|
1.
|
Nagadia R, Pandit P, Coman WB,
Cooper-White J and Punyadeera C: miRNAs in head and neck cancer
revisited. Cell Oncol (Dordr). 36:1–7. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Duvvuri U and Myers JN: Cancer of the head
and neck is the sixth most common cancer worldwide. Curr Probl
Surg. 46:114–117. 2009.PubMed/NCBI
|
|
3.
|
Chen YJ, Chang JT, Liao CT, et al: Head
and neck cancer in the betel quid chewing area: recent advances in
molecular carcinogenesis. Cancer Sci. 99:1507–1514. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
4.
|
Chang PM, Chen PM, Chu PY, et al:
Effectiveness of pharmacokinetic modulating chemotherapy combined
with cisplatin as induction chemotherapy in resectable locally
advanced head and neck cancer: phase II study. Cancer Chemother
Pharmacol. 63:9–17. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Chen MK, Su SC, Lin CW, Tsai CM, Yang SF
and Weng CJ: Cathepsin B SNPs elevate the pathological development
of oral cancer and raise the susceptibility to carcinogen-mediated
oral cancer. Hum Genet. 131:1861–1868. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Lou JL, Guo L, Zhao JQ and Wang SY:
Squamous cell carcinoma of cervical lymph nodes from an unknown
primary site: a retrospective analysis of treatment strategies and
prognosis. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 48:32–36.
2013.(In Chinese).
|
|
7.
|
Bose P, Brockton NT and Dort JC: Head and
neck cancer: from anatomy to biology. Int J Cancer. Feb
18–2013.(Epub ahead of print).
|
|
8.
|
Kubicek GJ, Kimler BF, Wang F, Reddy EK,
Girod DA and Williamson SK: Chemotherapy in head and neck cancer:
clinical predictors of tolerance and outcomes. Am J Clin Oncol.
34:380–384. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Rades D, Ulbricht T, Hakim SG and Schild
SE: Cisplatin superior to carboplatin in adjuvant radiochemotherapy
for locally advanced cancers of the oropharynx and oral cavity.
Strahlenther Onkol. 188:42–48. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Mandic R, Rodgarkia-Dara CJ, Krohn V,
Wiegand S, Grenman R and Werner JA: Cisplatin resistance of the
HNSCC cell line UT-SCC-26A can be overcome by stimulation of the
EGF-receptor. Anticancer Res. 29:1181–1187. 2009.PubMed/NCBI
|
|
11.
|
Sunwoo JB: A cisplatin-resistant
subpopulation of mesenchymal-like cells in head and neck squamous
cell carcinoma. Cell Cycle. 10:2834–2835. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Vyas A, Dandawate P, Padhye S, Ahmad A and
Sarkar F: Perspectives on new synthetic curcumin analogs and their
potential anticancer properties. Curr Pharm Des. 19:2047–2069.
2013.PubMed/NCBI
|
|
13.
|
Baliga MS, Joseph N, Venkataranganna MV,
Saxena A, Ponemone V and Fayad R: Curcumin, an active component of
turmeric in the prevention and treatment of ulcerative colitis:
preclinical and clinical observations. Food Funct. 3:1109–1117.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
14.
|
Hanai H and Sugimoto K: Curcumin has
bright prospects for the treatment of inflammatory bowel disease.
Curr Pharm Des. 15:2087–2094. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Li Y and Wang P: Neuroprotective effects
of curcumin. Zhongguo Zhong Yao Za Zhi. 34:3173–3175. 2009.(In
Chinese).
|
|
16.
|
Shishodia S: Molecular mechanisms of
curcumin action: gene expression. Biofactors. 39:37–55. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Noorafshan A and Ashkani-Esfahani S: A
review of therapeutic effects of curcumin. Curr Pharm Des.
19:2032–2046. 2013.PubMed/NCBI
|
|
18.
|
Zhang X, Chen LX, Ouyang L, Cheng Y and
Liu B: Plant natural compounds: targeting pathways of autophagy as
anti-cancer therapeutic agents. Cell Prolif. 45:466–476. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
19.
|
Ye MX, Li Y, Yin H and Zhang J: Curcumin:
updated molecular mechanisms and intervention targets in human lung
cancer. Int J Mol Sci. 13:3959–3978. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Saha S, Adhikary A, Bhattacharyya P, Das T
and Sa G: Death by design: where curcumin sensitizes drug-resistant
tumours. Anticancer Res. 32:2567–2584. 2012.PubMed/NCBI
|
|
21.
|
Gupta SC, Kismali G and Aggarwal BB:
Curcumin, a component of turmeric: from farm to pharmacy.
Biofactors. 39:2–13. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22.
|
Gao W, Chan JY, Wei WI and Wong TS:
Anti-cancer effects of curcumin on head and neck cancers.
Anticancer Agents Med Chem. 12:1110–1116. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23.
|
Yallapu MM, Jaggi M and Chauhan SC:
Curcumin nanoformulations: a future nanomedicine for cancer. Drug
Discov Today. 17:71–80. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Varinska L, Mirossay L, Mojzisova G and
Mojzis J: Antiangogenic effect of selected phytochemicals.
Pharmazie. 65:57–63. 2010.PubMed/NCBI
|
|
25.
|
Basnet P and Skalko-Basnet N: Curcumin: an
anti-inflammatory molecule from a curry spice on the path to cancer
treatment. Molecules. 16:4567–4598. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26.
|
Haddad M, Sauvain M and Deharo E: Curcuma
as a parasiticidal agent: a review. Planta Med. 77:672–678. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
27.
|
Ji JL, Huang XF and Zhu HL: Curcumin and
its formulations: potential anti-cancer agents. Anticancer Agents
Med Chem. 12:210–218. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
28.
|
Shehzad A, Wahid F and Lee YS: Curcumin in
cancer chemoprevention: molecular targets, pharmacokinetics,
bioavailability, and clinical trials. Arch Pharm (Weinheim).
343:489–499. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
29.
|
Epstein J, Sanderson IR and Macdonald TT:
Curcumin as a therapeutic agent: the evidence from in vitro, animal
and human studies. Br J Nutr. 103:1545–1557. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
30.
|
Yallapu MM, Ebeling MC, Khan S, et al:
Novel curcumin loaded magnetic nanoparticles for pancreatic cancer
treatment. Mol Cancer Ther. May 23–2013.(Epub ahead of print).
|
|
31.
|
Pawar YB, Purohit H, Valicherla GR, et al:
Novel lipid based oral formulation of curcumin: development and
optimization by design of experiments approach. Int J Pharm.
436:617–623. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
32.
|
Gupta NK and Dixit VK: Bioavailability
enhancement of curcumin by complexation with phosphatidyl choline.
J Pharm Sci. 100:1987–1995. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
33.
|
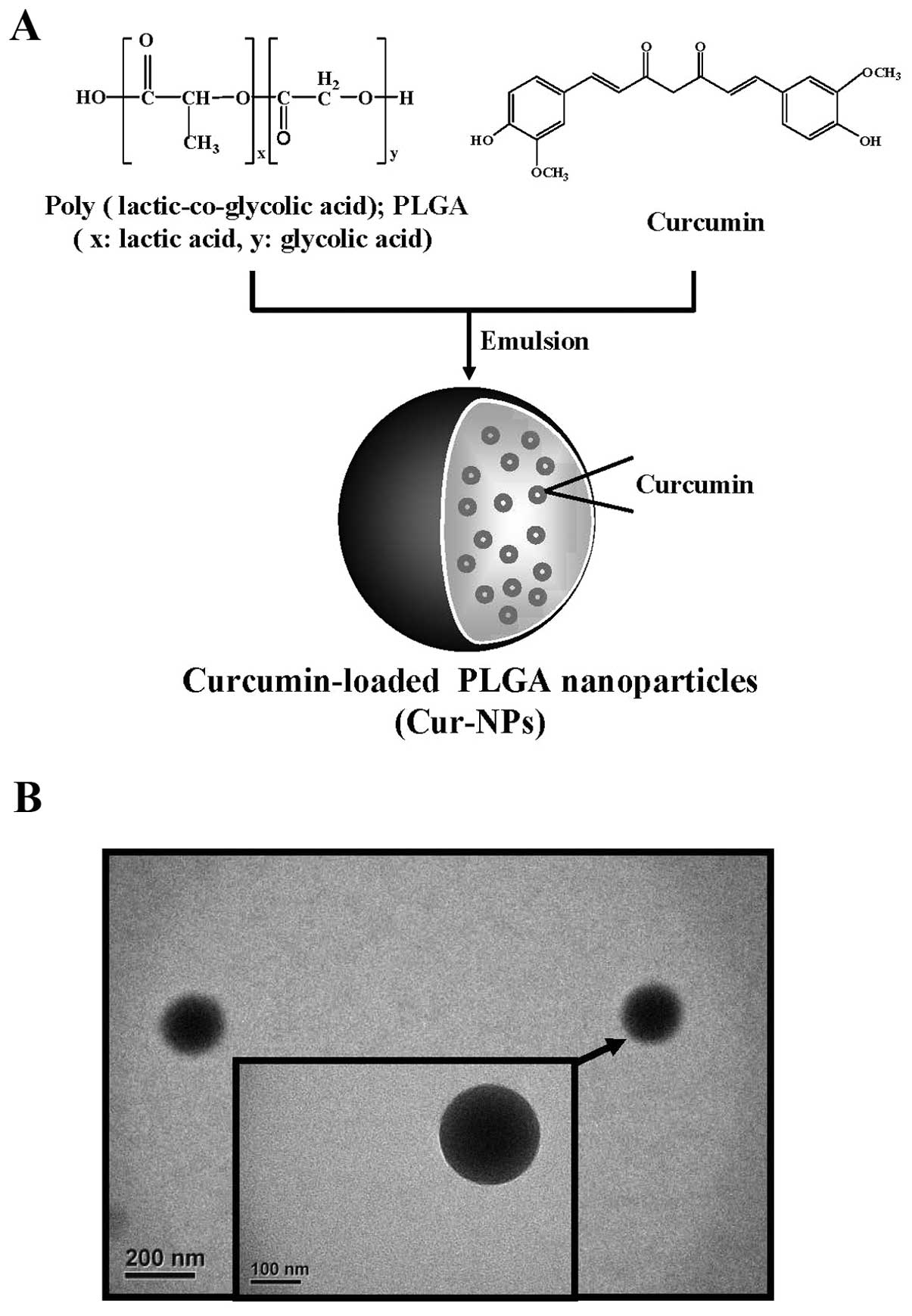
Verderio P, Bonetti P, Colombo M, Pandolfi
L and Prosperi D: Intracellular drug release from curcumin-loaded
PLGA nanoparticles induces G2/M block in breast cancer cells.
Biomacromolecules. 14:672–682. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
34.
|
Tsai YM, Chang-Liao WL, Chien CF, Lin LC
and Tsai TH: Effects of polymer molecular weight on relative oral
bioavailability of curcumin. Int J Nanomed. 7:2957–2966. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
35.
|
Doggui S, Sahni JK, Arseneault M, Dao L
and Ramassamy C: Neuronal uptake and neuroprotective effect of
curcumin-loaded PLGA nanoparticles on the human SK-N-SH cell line.
J Alzheimers Dis. 30:377–392. 2012.PubMed/NCBI
|
|
36.
|
Das M and Sahoo SK: Folate decorated dual
drug loaded nanoparticle: role of curcumin in enhancing therapeutic
potential of nutlin-3a by reversing multidrug resistance. PLoS One.
7:e329202012. View Article : Google Scholar : PubMed/NCBI
|
|
37.
|
Xie X, Tao Q, Zou Y, et al: PLGA
nanoparticles improve the oral bioavailability of curcumin in rats:
characterizations and mechanisms. J Agric Food Chem. 59:9280–9289.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
38.
|
Bansal SS, Goel M, Aqil F, Vadhanam MV and
Gupta RC: Advanced drug delivery systems of curcumin for cancer
chemoprevention. Cancer Prev Res (Phila). 4:1158–1171. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
39.
|
Jain AK, Das M, Swarnakar NK and Jain S:
Engineered PLGA nanoparticles: an emerging delivery tool in cancer
therapeutics. Crit Rev Ther Drug Carrier Syst. 28:1–45. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
40.
|
Berginc K, Trontelj J, Basnet NS and
Kristl A: Physiological barriers to the oral delivery of curcumin.
Pharmazie. 67:518–524. 2012.PubMed/NCBI
|
|
41.
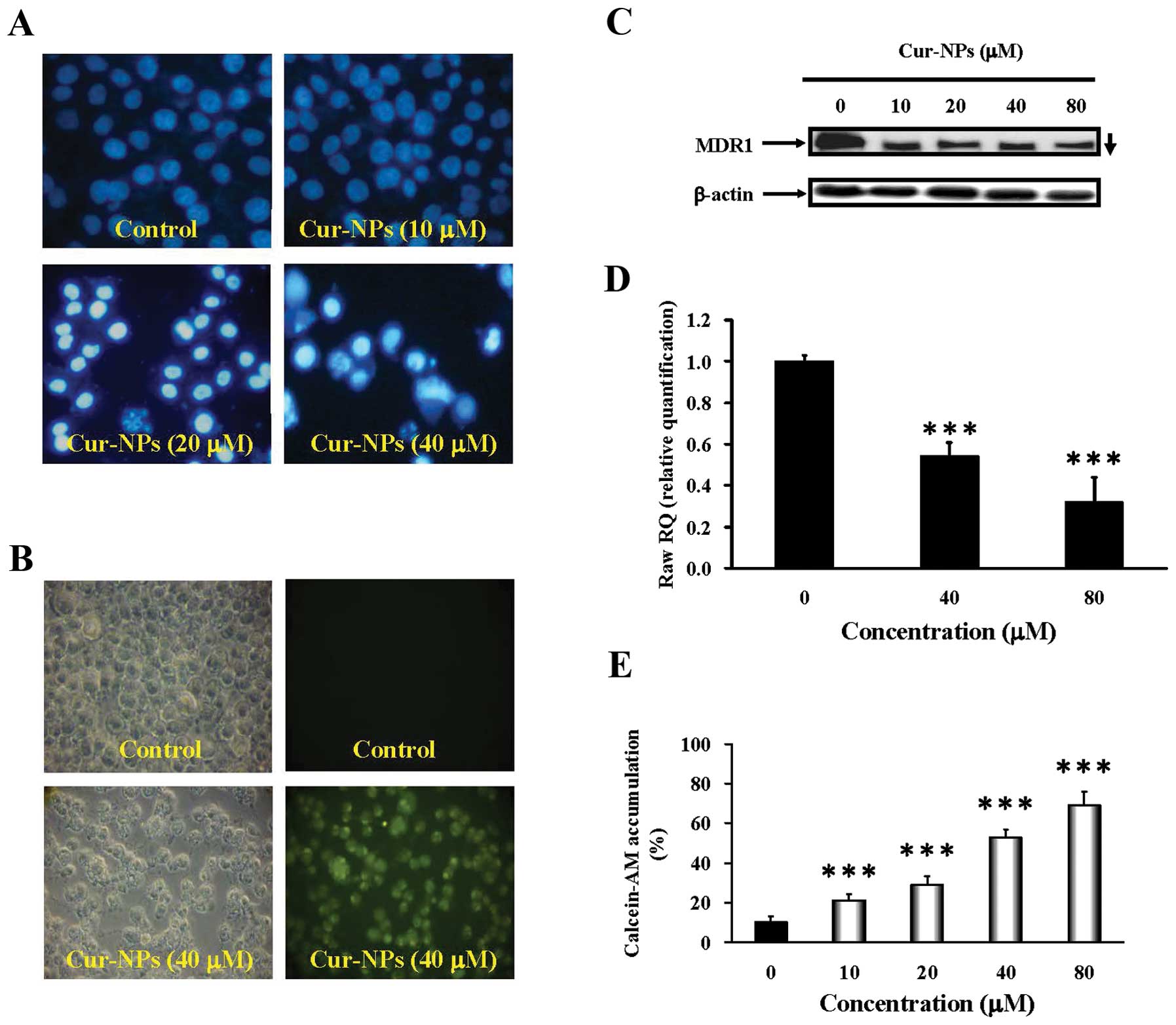
|
Shukla S, Zaher H, Hartz A, Bauer B, Ware
JA and Ambudkar SV: Curcumin inhibits the activity of ABCG2/BCRP1,
a multidrug resistance-linked ABC drug transporter in mice. Pharm
Res. 26:480–487. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
42.
|
Yue GG, Cheng SW, Yu H, et al: The role of
turmerones on curcumin transportation and P-glycoprotein activities
in intestinal Caco-2 cells. J Med Food. 15:242–252. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
43.
|
Zhou S, Lim LY and Chowbay B: Herbal
modulation of P-glycoprotein. Drug Metab Rev. 36:57–104. 2004.
View Article : Google Scholar
|
|
44.
|
Gosepath EM, Eckstein N, Hamacher A, et
al: Acquired cisplatin resistance in the head-neck cancer cell line
Cal27 is associated with decreased DKK1 expression and can
partially be reversed by overexpression of DKK1. Int J Cancer.
123:2013–2019. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
45.
|
Shih YH, Chang KW, Hsia SM, et al: In
vitro antimicrobial and anticancer potential of hinokitiol against
oral pathogens and oral cancer cell lines. Microbiol Res.
168:254–262. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
46.
|
Mathew A, Fukuda T, Nagaoka Y, et al:
Curcumin loaded-PLGA nanoparticles conjugated with Tet-1 peptide
for potential use in Alzheimer’s disease. PLoS One.
7:e326162012.PubMed/NCBI
|
|
47.
|
Luz PP, Magalhaes LG, Pereira AC, Cunha
WR, Rodrigues V and Andrade ESML: Curcumin-loaded into PLGA
nanoparticles: preparation and in vitro schistosomicidal activity.
Parasitol Res. 110:593–598. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
48.
|
Anand P, Nair HB, Sung B, et al: Design of
curcumin-loaded PLGA nanoparticles formulation with enhanced
cellular uptake, and increased bioactivity in vitro and superior
bioavailability in vivo. Biochem Pharmacol. 79:330–338. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
49.
|
Koppolu B, Rahimi M, Nattama S, Wadajkar A
and Nguyen KT: Development of multiple-layer polymeric particles
for targeted and controlled drug delivery. Nanomedicine. 6:355–361.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
50.
|
Chang CM, Chang PY, Tu MG, et al:
Epigallocatechin gallate sensitizes CAL-27 human oral squamous cell
carcinoma cells to the anti-metastatic effects of gefitinib
(Iressa) via synergistic suppression of epidermal growth factor
receptor and matrix metalloproteinase-2. Oncol Rep. 28:1799–1807.
2012.
|
|
51.
|
Tsai SC, Lu CC, Lee CY, et al: AKT
serine/threonine protein kinase modulates bufalin-triggered
intrinsic pathway of apoptosis in CAL 27 human oral cancer cells.
Int J Oncol. 41:1683–1692. 2012.PubMed/NCBI
|
|
52.
|
Yallapu MM, Othman SF, Curtis ET, et al:
Curcumin-loaded magnetic nanoparticles for breast cancer
therapeutics and imaging applications. Int J Nanomed. 7:1761–1779.
2012.PubMed/NCBI
|
|
53.
|
Tsai SC, Yang JS, Peng SF, et al: Bufalin
increases sensitivity to AKT/mTOR-induced autophagic cell death in
SK-HEP-1 human hepatocellular carcinoma cells. Int J Oncol.
41:1431–1442. 2012.PubMed/NCBI
|
|
54.
|
Mozaffarieh M, Konieczka K, Hauenstein D,
Schoetzau A and Flammer J: Half a pack of cigarettes a day more
than doubles DNA breaks in circulating leukocytes. Tob Induc Dis.
8:142010. View Article : Google Scholar : PubMed/NCBI
|
|
55.
|
Kuo TC, Yang JS, Lin MW, et al: Emodin has
cytotoxic and protective effects in rat C6 glioma cells: roles of
Mdr1a and nuclear factor kappaB in cell survival. J Pharmacol Exp
Ther. 330:736–744. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
56.
|
Huang WW, Tsai SC, Peng SF, et al:
Kaempferol induces autophagy through AMPK and AKT signaling
molecules and causes G2/M arrest via downregulation of CDK1/cyclin
B in SK-HEP-1 human hepatic cancer cells. Int J Oncol.
42:2069–2077. 2013.PubMed/NCBI
|
|
57.
|
Lan YH, Chiang JH, Huang WW, et al:
Activations of both extrinsic and intrinsic pathways in HCT 116
human colorectal cancer cells contribute to apoptosis through
p53-mediated ATM/Fas signaling by Emilia sonchifolia
extract, a folklore medicinal plant. Evid Based Complement Alternat
Med. 2012:1781782012.PubMed/NCBI
|
|
58.
|
Lin C, Tsai SC, Tseng MT, et al: AKT
serine/threonine protein kinase modulates baicalin-triggered
autophagy in human bladder cancer T24 cells. Int J Oncol.
42:993–1000. 2013.
|
|
59.
|
Taurin S, Nehoff H, Diong J, Larsen L,
Rosengren RJ and Greish K: Curcumin-derivative nanomicelles for the
treatment of triple negative breast cancer. J Drug Target. May
16–2013.(Epub ahead of print).
|
|
60.
|
Yen FL, Wu TH, Tzeng CW, Lin LT and Lin
CC: Curcumin nanoparticles improve the physicochemical properties
of curcumin and effectively enhance its antioxidant and
antihepatoma activities. J Agric Food Chem. 58:7376–7382. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
61.
|
Anand P, Kunnumakkara AB, Newman RA and
Aggarwal BB: Bioavailability of curcumin: problems and promises.
Mol Pharm. 4:807–818. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
62.
|
Yallapu MM, Dobberpuhl MR, Maher DM, Jaggi
M and Chauhan SC: Design of curcumin loaded cellulose nanoparticles
for prostate cancer. Curr Drug Metab. 13:120–128. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
63.
|
Yin HT, Zhang DG, Wu XL, Huang XE and Chen
G: In vivo evaluation of curcumin-loaded nanoparticles in a A549
xenograft mice model. Asian Pac J Cancer Prev. 14:409–412. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
64.
|
Misra R and Sahoo SK: Coformulation of
doxorubicin and curcumin in poly(D,L-lactide-co-glycolide)
nanoparticles suppresses the development of multidrug resistance in
K562 cells. Mol Pharm. 8:852–866. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
65.
|
Pramanik D, Campbell NR, Das S, et al: A
composite polymer nanoparticle overcomes multidrug resistance and
ameliorates doxorubicin-associated cardiomyopathy. Oncotarget.
3:640–650. 2012.
|
|
66.
|
Ganta S, Devalapally H and Amiji M:
Curcumin enhances oral bioavailability and anti-tumor therapeutic
efficacy of paclitaxel upon administration in nanoemulsion
formulation. J Pharm Sci. 99:4630–4641. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
67.
|
Ganta S and Amiji M: Coadministration of
Paclitaxel and curcumin in nanoemulsion formulations to overcome
multidrug resistance in tumor cells. Mol Pharm. 6:928–939. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
68.
|
Punfa W, Yodkeeree S, Pitchakarn P,
Ampasavate C and Limtrakul P: Enhancement of cellular uptake and
cytotoxicity of curcumin-loaded PLGA nanoparticles by conjugation
with anti-P-glycoprotein in drug resistance cancer cells. Acta
Pharmacol Sin. 33:823–831. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
69.
|
Cort A, Ozdemir E, Timur M and Ozben T:
Effects of curcumin on bleomycininduced oxidative stress in
malignant testicular germ cell tumors. Mol Med Rep. 6:860–866.
2012.PubMed/NCBI
|
|
70.
|
Misra J, Chanda D, Kim DK, et al: Curcumin
differentially regulates endoplasmic reticulum stress through
transcriptional corepressor SMILE (small heterodimer
partner-interacting leucine zipper protein)-mediated inhibition of
CREBH (cAMP responsive element-binding protein H). J Biol Chem.
286:41972–41984. 2011. View Article : Google Scholar
|
|
71.
|
Wahl H, Tan L, Griffith K, Choi M and Liu
JR: Curcumin enhances Apo2L/TRAIL-induced apoptosis in
chemoresistant ovarian cancer cells. Gynecol Oncol. 105:104–112.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
72.
|
Dilnawaz F, Singh A and Sahoo SK:
Transferrin-conjugated curcumin-loaded superparamagnetic iron oxide
nanoparticles induce augmented cellular uptake and apoptosis in
K562 cells. Acta Biomater. 8:704–719. 2012. View Article : Google Scholar
|