|
1
|
Rodriguez-Morales AJ, Cardona-Ospina JA,
Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y,
Escalera-Antezana JP, Alvarado-Arnez LE, Bonilla-Aldana DK,
Franco-Paredes C, Henao-Martinez AF, et al: Clinical, laboratory
and imaging features of COVID-19: A systematic review and
meta-analysis. Travel Med Infect Dis. 34(101623)2020.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Ye Q, Wang B and Mao J: The pathogenesis
and treatment of the ‘Cytokine Storm’ in COVID-19. J Infect.
80:607–613. 2020.PubMed/NCBI View Article : Google Scholar
|
|
3
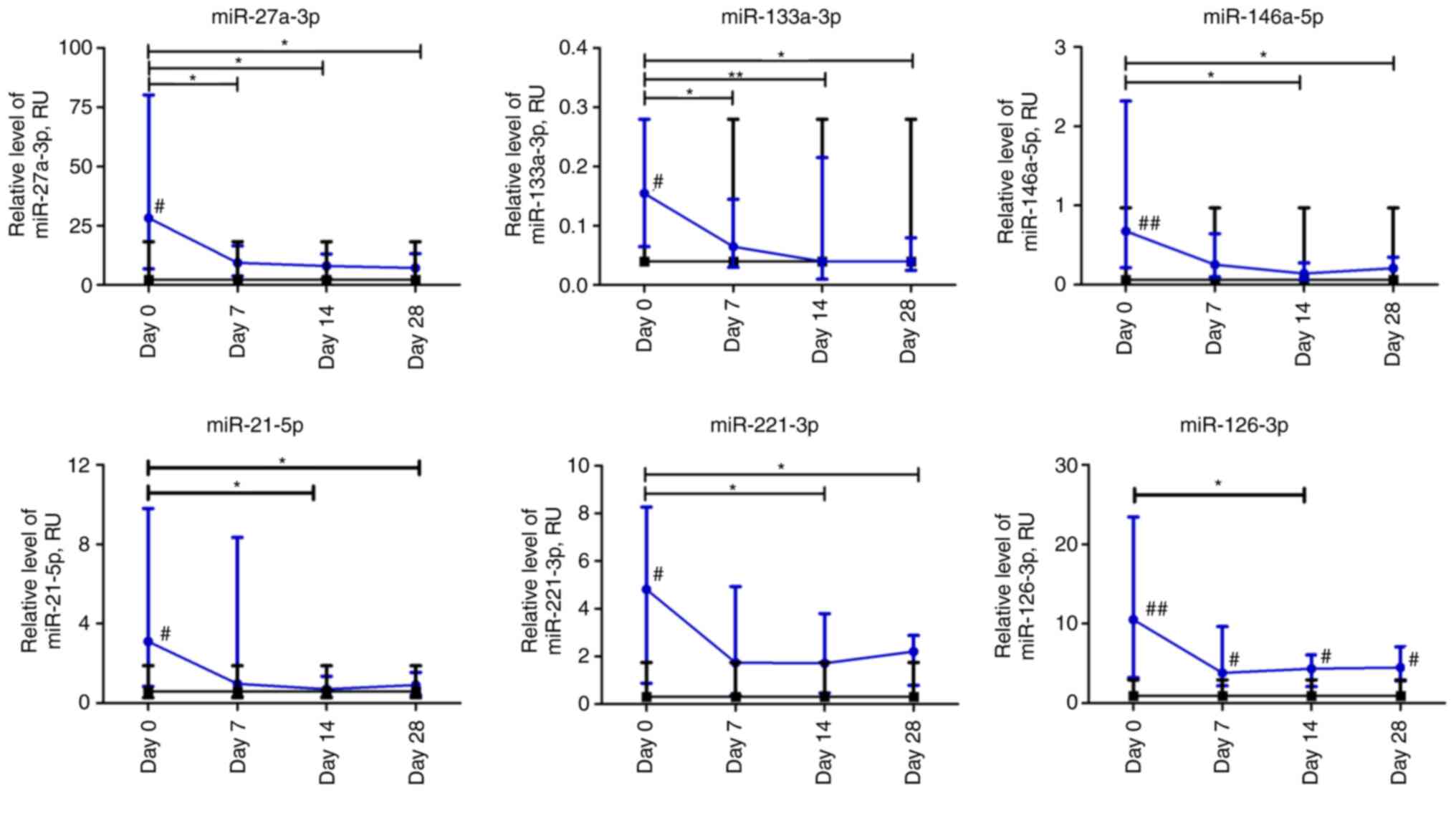
|
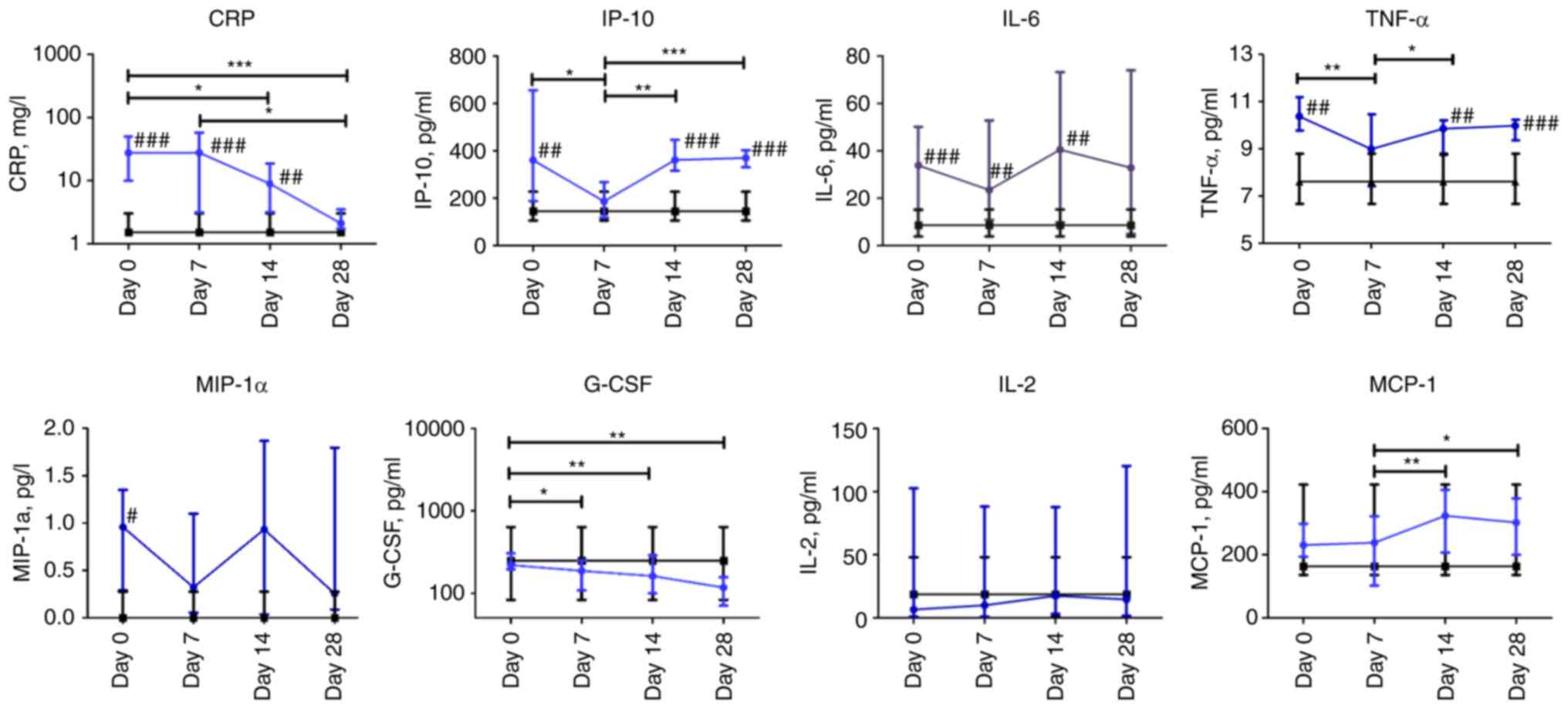
Chousterman BG, Swirski FK and Weber GF:
Cytokine storm and sepsis disease pathogenesis. Semin Immunopathol.
39:517–528. 2017.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Islam MT, Nasiruddin M, Khan IN, Mishra
SK, Kudrat-E-Zahan M, Riaz TA, Ali ES, Rahman MS, Mubarak MS,
Martorell M, et al: A perspective on emerging therapeutic
interventions for COVID-19. Front Public Health.
8(281)2020.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Puneet P, Moochhala S and Bhatia M:
Chemokines in acute respiratory distress syndrome. Am J Physiol
Lung Cell Mol Physiol. 288:L3–L15. 2005.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Bhatia M, Zemans RL and Jeyaseelan S: Role
of chemokines in the pathogenesis of acute lung injury. Am J Respir
Cell Mol Biol. 46:566–572. 2012.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Tomashefski JF Jr: Pulmonary pathology of
acute respiratory distress syndrome. Clin Chest Med. 21:435–466.
2000.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Lyu P, Liu X, Zhang R, Shi L and Gao J:
The performance of chest CT in evaluating the clinical severity of
COVID-19 pneumonia: Identifying critical cases based on CT
characteristics. Invest Radiol. 55:412–421. 2020.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Zhao W, Zhong Z, Xie X, Yu Q and Liu J:
Relation between chest CT findings and clinical conditions of
coronavirus disease (COVID-19) pneumonia: A multicenter study. AJR
Am J Roentgenol. 214:1072–1077. 2020.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Wu J, Wu X, Zeng W, Guo D, Fang Z, Chen L,
Huang H and Li C: Chest CT findings in patients with coronavirus
disease 2019 and its relationship with clinical features. Invest
Radiol. 55:257–261. 2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Alon R, Sportiello M, Kozlovski S, Kumar
A, Reilly EC, Zarbock A, Garbi N and Topham DJ: Leukocyte
trafficking to the lungs and beyond: Lessons from influenza for
COVID-19. Nat Rev Immunol. 21:49–64. 2020.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Zemans RL, Colgan SP and Downey GP:
Transepithelial migration of neutrophils: Mechanisms and
implications for acute lung injury. Am J Respir Cell Mol Biol.
40:519–535. 2009.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Zhang L, Yan X, Fan Q, Liu H, Liu X, Liu Z
and Zhang Z: D-dimer levels on admission to predict in-hospital
mortality in patients with Covid-19. J Thromb Haemost.
18:1324–1329. 2020.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Li H, Xiang X, Ren H, Xu L, Zhao L, Chen
X, Long H, Wang Q and Wu Q: Serum amyloid A is a biomarker of
severe Coronavirus disease and poor prognosis. J Infect.
80:646–655. 2020.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Gao L, Jiang D, Wen XS, Cheng XC, Sun M,
He B, You LN, Lei P, Tan XW, Qin S, et al: Prognostic value of
NT-proBNP in patients with severe COVID-19. Respir Res.
21(83)2020.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Al Balushi A, Al Shekaili J, Al Kindi M,
Ansari Z, Al-Khabori M, Khamis F, Ambusaidi Z, Al Balushi A, Al
Huraizi A, Al Sulaimi S, et al: Immunological predictors of disease
severity in patients with COVID-19. Int J Inf Dis. 110:83–92.
2021.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Sidiropoulou P, Docea AO, Nikolaou V,
Katsarou MS, Spandidos DA, Tsatsakis A, Calina D and Drakoulis N:
Unraveling the roles of vitamin D status and melanin during
COVID-19 (Review). Int J Mol Med. 47:92–100. 2021.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Hussain T, Zhao D, Shah SZA, Wang J, Yue
R, Liao Y, Sabir N, Yang L and Zhou X: MicroRNA 27a-3p regulates
antimicrobial responses of murine macrophages infected by
mycobacterium avium subspecies paratuberculosis by targeting
interleukin-10 and TGF-β-activated protein kinase 1 binding protein
2. Front Immunol. 11(1915)2018.PubMed/NCBI View Article : Google Scholar
|
|
19
|
de Gonzalo-Calvo D, Benitez ID, Pinilla L,
Carratala A, Moncusi-Moix ANNA, Gort-Paniello C, Molinero M,
González J, Torres G, Bernal M, et al: Circulating microRNA
profiles predict the severity of COVID-19 in hospitalized patients.
Transl Res. 236:147–159. 2021.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Lev S, Gottesman T, Levin GS, Lederfein D,
Berkov E, Diker D, Zaidman A, Nutman A, Ber AI, Angel A, et al:
Observational cohort study of IP-10's potential as a biomarker to
aid in inflammation regulation within a clinical decision support
protocol for patients with severe COVID-19. PLoS One.
16(e0245296)2021.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Iannetta M, Buccisano F, Fraboni D,
Malagnino V, Campogiani L, Teti E, Spalliera I, Rossi B, Di Lorenzo
A, Palmieri R, et al: Baseline T-lymphocyte subset absolute counts
can predict both outcome and severity in SARS-CoV-2 infected
patients: A single center study. Sci Rep. 11(12762)2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Deng R, Wang C, Ye Y, Gou L, Fu Z, Ye B,
Shao F, Zhang X, Fu W, Xiao J, et al: Clinical manifestations of
blood cell parameters and inflammatory factors in 92 patients with
COVID-19. Ann Transl Med. 9(62)2021.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Shi H, Wang W, Yin J, Ouyang Y, Pang L,
Feng Y, Qiao L, Guo X, Shi H, Jin R and Chen D: The inhibition of
IL-2/IL-2R gives rise to CD8 + T cell and lymphocyte decrease
through JAK1-STAT5 in critical patients with COVID-19 pneumonia.
Cell Death Dis. 11(429)2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Liao M, Liu Y, Yuan J, Wen Y, Xu G, Zhao
J, Cheng L, Li J, Wang X, Wang F, et al: Single-cell landscape of
bronchoalveolar immune cells in patients with COVID-19. Nat Med.
26:842–844. 2020.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Clinical management of severe acute
respiratory infection when novel coronavirus (nCoV) infection is
suspected [Internet]. [cited 2021 Jul 25]. Available from:
https://www.who.int/publications/i/item/10665-332299.
|
|
26
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408.
2001.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Büttner L, Aigner A, Fleckenstein FN,
Hamper CM, Jonczyk M, Hamm B, Scholz O and Böning G: Diagnostic
value of initial chest CT findings for the need of ICU
treatment/intubation in patients with COVID-19. Diagnostics
(Basel). 10(929)2020.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Liu J, Li S, Liu J, Liang B, Wang X, Wang
H, Li W, Tong Q, Yi J, Zhao L, et al: Longitudinal characteristics
of lymphocyte responses and cytokine profiles in the peripheral
blood of SARS-CoV-2 infected patients. EBioMedicine.
55(102763)2020.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu
Y, Zhang L, Fan G, Xu J, Gu X, et al: Clinical features of patients
infected with 2019 novel coronavirus in Wuhan, China. Lancet.
395:497–506. 2020.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Lax SF, Skok K, Zechner P, Kessler HH,
Kaufmann N, Koelblinger C, Vander K, Bargfrieder U and Trauner M:
Pulmonary arterial thrombosis in COVID-19 with fatal outcome:
Results from a prospective, single-center, clinicopathologic case
series. Ann Intern Med. 173:350–361. 2020.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Xu Z, Shi L, Wang Y, Zhang J, Huang L,
Zhang C, Liu S, Zhao P, Liu H, Zhu L, et al: Pathological findings
of COVID-19 associated with acute respiratory distress syndrome.
Lancet Respir Med. 8:420–422. 2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Marté JL, Toney NJ, Cordes L, Schlom J,
Donahue RN and Gulley JL: Original research: Early changes in
immune cell subsets with corticosteroids in patients with solid
tumors: Implications for COVID-19 management. J Immunother Cancer.
8(e001019)2020.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Abdin SM, Elgendy SM, Alyammahi SK,
Alhamad DW and Omar HA: Tackling the cytokine storm in COVID-19,
challenges and hopes. Life Sci. 257(118054)2020.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Tomić S, Đokić J, Stevanović D, Ilić N,
Gruden-Movsesijan A, Dinić M, Radojević D, Bekić M, Mitrović N,
Tomašević R, et al: Reduced expression of autophagy markers and
expansion of myeloid-derived suppressor cells correlate with poor T
cell response in severe COVID-19 patients. Front Immunol.
22(614599)2021.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Deng Z, Zhang M, Zhu T, Zhili N, Liu Z,
Xiang R, Zhang W and Xu Y: Dynamic changes in peripheral blood
lymphocyte subsets in adult patients with COVID-19. Int J Infect
Dis. 98:353–358. 2020.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Riley JL: PD-1 signaling in primary T
cells. Immunol Rev. 229:114–125. 2009.PubMed/NCBI View Article : Google Scholar
|
|
37
|
Pyzik A, Grywalska E, Matyjaszek-Matuszek
B, Smoleń A, Pyzik D and Roliński J: Frequencies of PD-1-positive T
CD3+CD4+, T CD3+CD8+ and B CD19+ lymphocytes in female patients
with Graves' disease and healthy controls-preliminary study. Mol
Cell Endocrinol. 448:28–33. 2017.PubMed/NCBI View Article : Google Scholar
|
|
38
|
Nascimbeni M, Shin EC, Chiriboga L,
Kleiner DE and Rehermann B: Peripheral CD4(+)CD8(+) T cells are
differentiated effector memory cells with antiviral functions.
Blood. 104:478–486. 2004.PubMed/NCBI View Article : Google Scholar
|
|
39
|
Overgaard NH, Jung JW, Steptoe RJ and
Wells JW: CD4+/CD8+ double-positive T cells: More than just a
developmental stage? J Leukoc Biol. 97:31–38. 2015.PubMed/NCBI View Article : Google Scholar
|
|
40
|
Yang X, Dai T, Zhou X, Qian H, Guo R, Lei
L, Zhang X, Zhang D, Shi L, Cheng Y, et al: Naturally activated
adaptive immunity in COVID-19 patients. J Cell Mol Med.
24:12457–12463. 2020.PubMed/NCBI View Article : Google Scholar
|
|
41
|
Kalfaoglu B, Almeida-Santos J, Tye CA,
Satou Y and Ono M: T-cell hyperactivation and paralysis in severe
COVID-19 infection revealed by single-cell analysis. Front Immunol.
11(589380)2020.PubMed/NCBI View Article : Google Scholar
|
|
42
|
Chen X, Huang J, Huang Y, Chen J, Huang Y,
Jiang X and Shi Y: Characteristics of immune cells and cytokines in
patients with coronavirus disease 2019 in Guangzhou, China. Hum
Immunol. 81:702–708. 2020.PubMed/NCBI View Article : Google Scholar
|
|
43
|
Neidleman J, Luo X, Frouard J, Xie G, Gill
G, Stein ES, McGregor M, Ma T, George AF, Kosters A, et al:
SARS-CoV-2-Specific T cells exhibit phenotypic features of helper
function, lack of terminal differentiation, and high proliferation
potential. Cell Rep Med. 1(1000081)2020.PubMed/NCBI View Article : Google Scholar
|
|
44
|
Wang W, Xiang HP, Wang HP, Zhu LX and Geng
XP: CD4 + CD25 + CD127 high cells as a negative predictor of
multiple organ failure in acute pancreatitis. World J Emerg Surg.
12(7)2017.PubMed/NCBI View Article : Google Scholar
|
|
45
|
Kalfaoglu B, Almeida-Santos J, Tye CA,
Satou Y and Ono M: T-cell dysregulation in COVID-19. Biochem
Biophys Res Commun. 538:204–210. 2021.PubMed/NCBI View Article : Google Scholar
|
|
46
|
Hanna SJ, Codd AS, Gea-Mallorqui E,
Scourfield DO, Richter FC, Ladell K, Borsa M, Compeer EB, Moon OR,
Galloway SAE, et al: T cell phenotypes in COVID-19-a living review.
Oxf Open Immunol. 2(iqaa007)2021.PubMed/NCBI View Article : Google Scholar
|
|
47
|
Kusnadi A, Ramírez-Suástegui C, Fajardo V,
Chee SJ, Meckiff BJ, Simon H, Pelosi E, Seumois G, Ay F, Vijayanand
P and Ottensmeier CH: Severely ill COVID-19 patients display
impaired exhaustion features in SARS-CoV-2-reactive CD8+ T cells.
Sci Immunol. 6(eabe4782)2021.PubMed/NCBI View Article : Google Scholar
|
|
48
|
Peng Y, Mentzer AJ, Liu G, Yao X, Yin Z,
Dong D, Dejnirattisai W, Rostron T, Supasa P, Liu C, et al: Broad
and strong memory CD4+ and CD8+ T cells induced by SARS-CoV-2 in UK
convalescent individuals following COVID-19. Nat Immunol.
21:1336–1345. 2020.PubMed/NCBI View Article : Google Scholar
|
|
49
|
Neagu M, Calina D, Docea AO, Constantin C,
Filippini T, Vinceti M, Drakoulis N, Poulas K, Nikolouzakis TK,
Spandidos DA and Tsatsakis A: Back to basics in COVID-19: Antigens
and antibodies-completing the puzzle. J Cell Mol Med. 25:4523–4533.
2021.PubMed/NCBI View Article : Google Scholar
|
|
50
|
De Biasi S, Meschiari M, Gibellini L,
Bellinazzi C, Borella R, Fidanza L, Gozzi L, Iannone A, Lo Tartaro
D, Mattioli M, et al: Marked T cell activation, senescence,
exhaustion and skewing towards TH17 in patients with COVID-19
pneumonia. Nat Commun. 11(3434)2020.PubMed/NCBI View Article : Google Scholar
|
|
51
|
Qin C, Zhou L, Hu Z, Zhang S, Yang S, Tao
Y, Xie C, Ma K, Shang K, Wang W and Tian DS: Dysregulation of
immune response in patients with COVID-19 in Wuhan, China. Clin
Infect Dis. 71:762–768. 2020.PubMed/NCBI View Article : Google Scholar
|
|
52
|
Wang F, Hou H, Luo Y, Tang G, Wu S, Huang
M, Liu W, Zhu Y, Lin Q, Mao L, et al: The laboratory tests and host
immunity of COVID-19 patients with different severity of illness.
JCI Insight. 5(e137799)2020.PubMed/NCBI View Article : Google Scholar
|
|
53
|
Chen G, Wu D, Guo W, Cao Y, Huang D, Wang
H, Wang T, Zhang X, Chen H, Yu H, et al: Clinical and immunological
features of severe and moderate coronavirus disease 2019. J Clin
Invest. 130:2620–2629. 2020.PubMed/NCBI View Article : Google Scholar
|
|
54
|
Yang J, Zhang E, Zhong M, Yang Q, Hong K,
Shu T, Zhou D, Xiang J, Xia J, Zhou X, et al: Longitudinal
characteristics of t cell responses in asymptomatic SARS-CoV-2
infection. Virol Sin. 35:838–841. 2020.PubMed/NCBI View Article : Google Scholar
|
|
55
|
Sanchez-Cerrillo I, Landete P, Aldave B,
Sanchez-Alonso S, Sanchez-Azofra A, Marcos-Jimenez A, Avalos E,
Alcaraz-Serna A, de Los Santos I, Mateu-Albero T, et al:
Differential redistribution of activated monocyte and dendritic
cell subsets to the lung associates with severity of COVID-19.
medRxiv. 2020(20100925)2020.PubMed/NCBI View Article : Google Scholar
|
|
56
|
Leng Z, Zhu R, Hou W, Feng Y, Yang Y, Han
Q, Shan G, Meng F, Du D, Wang S, et al: Transplantation of ACE2-
mesenchymal stem cells improves the outcome of patients with
COVID-19 pneumonia. Aging Dis. 11:216–228. 2020.PubMed/NCBI View Article : Google Scholar
|
|
57
|
Fujita S, Seino KI and Sato K, Sato Y,
Eizumi K, Yamashita N, Taniguchi M and Sato K: Regulatory dendritic
cells act as regulators of acute lethal systemic inflammatory
response. Blood. 107:3656–3664. 2006.PubMed/NCBI View Article : Google Scholar
|
|
58
|
Boor PPC, Metselaar HJ, Mancham S, Tilanus
HW, Kusters JG and Kwekkeboom J: Prednisolone suppresses the
function and promotes apoptosis of plasmacytoid dendritic cells. Am
J Transplant. 6:2332–2341. 2006.PubMed/NCBI View Article : Google Scholar
|
|
59
|
Shin KS, Jeon I, Kim BS, Kim IK, Park YJ,
Koh CH, Song B, Lee JM, Lim J, Bae EA, et al: Monocyte-derived
dendritic cells dictate the memory differentiation of CD8+ T cells
during acute infection. Front Immunol. 10(1887)2019.PubMed/NCBI View Article : Google Scholar
|
|
60
|
Calina D, Sarkar C, Arsene AL, Salehi B,
Docea AO, Mondal M, Islam MT, Zali A and Sharifi-Rad J: Recent
advances, approaches and challenges in targeting pathways for
potential COVID-19 vaccines development. Immunol Res. 68:315–324.
2020.PubMed/NCBI View Article : Google Scholar
|
|
61
|
Aldridge JR Jr, Moseley CE, Boltz DA,
Negovetich NJ, Reynolds C, Franks J, Brown SA, Doherty PC, Webster
RG and Thomas PG: From the cover: TNF/iNOS-producing dendritic
cells are the necessary evil of lethal influenza virus infection.
Proc Natl Acad Sci USA. 106:5306–5311. 2009.PubMed/NCBI View Article : Google Scholar
|
|
62
|
Iijima N, Mattei LM and Iwasaki A:
Recruited inflammatory monocytes stimulate antiviral Th1 immunity
in infected tissue. Proc Natl Acad Sci USA. 108:284–289.
2011.PubMed/NCBI View Article : Google Scholar
|
|
63
|
Haroun RAH, Osman WH and Eessa AM:
Interferon-γ-induced protein 10 (IP-10) and serum amyloid A (SAA)
are excellent biomarkers for the prediction of COVID-19 progression
and severity. Life Sci. 269(119019)2021.PubMed/NCBI View Article : Google Scholar
|
|
64
|
Wang G, Wu C, Zhang Q, Wu F, Yu B, Lv J,
Li Y, Li T, Zhang S, Wu C, et al: C-reactive protein level may
predict the risk of COVID-19 aggravation. Open Forum Infect Dis.
7(ofaa153)2020.PubMed/NCBI View Article : Google Scholar
|
|
65
|
Chen W, Zheng KI, Liu S, Yan Z, Xu C and
Qiao Z: Plasma CRP level is positively associated with the severity
of COVID-19. Ann Clin Microbiol Antimicrob. 19(18)2020.PubMed/NCBI View Article : Google Scholar
|
|
66
|
Mardani R, Namavar M, Ghorbi E, Shoja Z,
Zali F, Kaghazian H, Aghasadeghi MR, Sadeghi SA, Sabeti S, Darazam
IA, et al: Association between serum inflammatory parameters and
the disease severity in COVID-19 patients. J Clin Lab Anal.
36(e24162)2022.PubMed/NCBI View Article : Google Scholar
|
|
67
|
Peruzzi B, Bencini S, Capone M, Mazzoni A,
Maggi L, Salvati L, Vanni A, Orazzini C, Nozzoli C, Morettini A, et
al: Quantitative and qualitative alterations of circulating myeloid
cells and plasmacytoid DC in SARS-CoV-2 infection. Immunology.
161:345–353. 2020.PubMed/NCBI View Article : Google Scholar
|
|
68
|
Mangano C and Oliva BM: Relationship
between lymphocyte subsets values and C-reactive protein in
COVID-19 patients. Cytometry A. 99:462–465. 2021.PubMed/NCBI View Article : Google Scholar
|
|
69
|
Tyurin AV, Salimgareeva MK, Miniakhmetov
IR, Khusainova RI, Samorodov A, Pavlov VN and Kzhyshkowska J:
Correlation of the imbalance in the circulating lymphocyte subsets
with c-reactive protein and cardio-metabolic conditions in patients
with COVID-19. Front Immunol. 13(856883)2022.PubMed/NCBI View Article : Google Scholar
|
|
70
|
Meizlish ML, Pine AB, Bishai JD, Goshua G,
Nadelmann ER, Simonov M, Chang CH, Zhang H, Shallow M, Bahel P, et
al: A neutrophil activation signature predicts critical illness and
mortality in COVID-19. Blood Adv. 5:1164–1177. 2021.PubMed/NCBI View Article : Google Scholar
|
|
71
|
Hasanvand A: COVID-19 and the role of
cytokines in this disease. Inflammopharmacology. 30:789–798.
2022.PubMed/NCBI View Article : Google Scholar
|
|
72
|
Tavakkoli M, Wilkins CR, Mones JV and
Mauro MJ: A novel paradigm between leukocytosis, G-CSF secretion,
neutrophil-to-lymphocyte ratio, myeloid-derived suppressor cells,
and prognosis in non-small cell lung cancer. Front Oncol.
9(295)2019.PubMed/NCBI View Article : Google Scholar
|
|
73
|
Miles B: G-CSF in Covid-19 patients:
Increased need for mechanical ventilation and inferior 60-day
survival. Supportive Care in Cancer [Internet]. 2022 Jun 1 [cited
2022 Sep 15];30:S77-S77. Available from: https://doi.org/10.1007/s00520-022-07099-y.
|
|
74
|
Chen Y, Wang J, Liu C, Su L, Zhang D, Fan
J, Yang Y, Xiao M, Xie J, Xu Y, et al: IP-10 and MCP-1 as
biomarkers associated with disease severity of COVID-19. Mol Med.
26(97)2020.PubMed/NCBI View Article : Google Scholar
|
|
75
|
Pons MJ, Ymaña B, Mayanga-Herrera A, Sáenz
Y, Alvarez-Erviti L, Tapia-Rojas S, Gamarra R, Blanco AB, Moncunill
G and Ugarte-Gil MF: Cytokine profiles associated with worse
prognosis in a hospitalized peruvian COVID-19 cohort. Front
Immunol. 12(700921)2021.PubMed/NCBI View Article : Google Scholar
|
|
76
|
Tjan LH, Furukawa K, Nagano T, Kiriu T,
Nishimura M, Arii J, Hino Y, Iwata S, Nishimura Y and Mori Y: Early
differences in cytokine production by severity of coronavirus
disease 2019. J Infect Dis. 223:1145–1149. 2021.PubMed/NCBI View Article : Google Scholar
|
|
77
|
Yang AP, Li HM, Tao WQ, Yang XJ, Wang M,
Yang WJ and Liu JP: Infection with SARS-CoV-2 causes abnormal
laboratory results of multiple organs in patients. Aging (Albany
NY). 12:10059–10069. 2020.PubMed/NCBI View Article : Google Scholar
|
|
78
|
Liu Y, Tan W, Chen H, Zhu Y, Wan L, Jiang
K, Guo Y, Tang K, Xie C, Yi H, et al: Dynamic changes in lymphocyte
subsets and parallel cytokine levels in patients with severe and
critical COVID-19. BMC Infect Dis. 21(79)2021.PubMed/NCBI View Article : Google Scholar
|
|
79
|
Leisman DE, Ronner L, Pinotti R, Taylor
MD, Sinha P, Calfee CS, Hirayama AV, Mastroiani F, Turtle CJ,
Harhay MO, et al: Cytokine elevation in severe and critical
COVID-19: A rapid systematic review, meta-analysis, and comparison
with other inflammatory syndromes. Lancet Respir Med. 8:1233–1244.
2020.PubMed/NCBI View Article : Google Scholar
|
|
80
|
Han H, Ma Q, Li C, Liu R, Zhao L, Wang W,
Zhang P, Liu X, Gao G, Liu F, et al: Profiling serum cytokines in
COVID-19 patients reveals IL-6 and IL-10 are disease severity
predictors. Emerg Microbes Infect. 9:1123–1130. 2020.PubMed/NCBI View Article : Google Scholar
|
|
81
|
Lambert KA, Roff AN, Panganiban RP,
Douglas S and Ishmael FT: MicroRNA-146a is induced by inflammatory
stimuli in airway epithelial cells and augments the
anti-inflammatory effects of glucocorticoids. PLoS One.
13(e0205434)2018.PubMed/NCBI View Article : Google Scholar
|
|
82
|
Taganov KD, Boldin MP, Chang KJ and
Baltimore D: NF-κB-dependent induction of microRNA miR-146, an
inhibitor targeted to signaling proteins of innate immune
responses. Proc Natl Acad Sci USA. 103:12481–12486. 2006.PubMed/NCBI View Article : Google Scholar
|
|
83
|
Zeng Z, Gong H, Li Y, Jie K, Ding C, Shao
Q, Liu F, Zhan Y, Nie C, Zhu W and Qian K: Upregulation of miR-146a
contributes to the suppression of inflammatory responses in
LPS-induced acute lung injury. Exp Lung Res. 39:275–282.
2013.PubMed/NCBI View Article : Google Scholar
|
|
84
|
Donyavi T, Bokharaei-Salim F, Baghi HB,
Khanaliha K, Janat-Makan MA, Karimi B, Nahand JS, Mirzaei H,
Khatami A, Garshasbi S, et al: Acute and post-acute phase of
COVID-19: Analyzing expression patterns of miRNA-29a-3p, 146a-3p,
155-5p, and let-7b-3p in PBMC. Int Immunopharmacol.
97(107641)2021.PubMed/NCBI View Article : Google Scholar
|
|
85
|
Garg A, Seeliger B, Derda AA, Xiao K,
Gietz A, Scherf K, Sonnenschein K, Pink I, Hoeper MM, Welte T, et
al: Circulating cardiovascular microRNAs in critically ill COVID-19
patients. Eur J Heart Fail. 23:468–475. 2021.PubMed/NCBI View Article : Google Scholar
|
|
86
|
Meng G, Wei J, Wang Y, Qu D and Zhang J:
MiR-21 regulates immunosuppression mediated by myeloid-derived
suppressor cells by impairing RUNX1-YAP interaction in lung cancer.
Cancer Cell Int. 20(495)2020.PubMed/NCBI View Article : Google Scholar
|
|
87
|
Wang T, Jiang L, Wei X, Dong Z, Liu B,
Zhao J, Wang L, Xie P, Wang Y and Zhou S: Inhibition of miR-221
alleviates LPS-induced acute lung injury via inactivation of
SOCS1/NF-κB signaling pathway. Cell Cycle. 18:1893–1907.
2019.PubMed/NCBI View Article : Google Scholar
|
|
88
|
Xu P, Xin J, Song L, Chen Y, Ma J, Liu L,
Qi Z, Pan X and Zhou S: Serum miR-133 as a potential biomarker in
acute cerebral infarction patients. Clin Lab. 66:1923–1928.
2020.PubMed/NCBI View Article : Google Scholar
|
|
89
|
Huang J, Zhu L, Qiu C, Xu X, Zhang L, Ding
X, Liao Q, Xu J and Zhang X: MicroRNA miR-126-5p enhances the
inflammatory responses of monocytes to lipopolysaccharide
stimulation by suppressing cylindromatosis in chronic HIV-1
Infection. J Virol. 5:e02048–e02016. 2017.PubMed/NCBI View Article : Google Scholar
|
|
90
|
Fogel O, Tinggaard AB, Fagny M, Sigrist N,
Roche E, Leclere L, Deleuze JF, Batteux F, Dougados M,
Miceli-Richard C and Tost J: Deregulation of microRNA expression in
monocytes and CD4+ T lymphocytes from patients with axial
spondyloarthritis. Arthritis Res Ther. 21(51)2019.PubMed/NCBI View Article : Google Scholar
|