Introduction
Radiotherapy is one of the main treatments for
locally advanced non-small cell lung cancer (LANSCLC). During
radiotherapy, normal lung tissue is inevitably irradiated, which
causes radiation injury to a greater or leser extent. It was
reported that 5–50% of patients irradiated for lung cancer suffer
from clinically significant symptomatic radiation pneumonitis (RP)
(1,2). Intensity modulated radiotherapy
(IMRT) reduces the dose at which normal tissues are irradiated and
reduces the risk of RP (3).
However, several studies revealed that 8–10% of patients with NSCLC
still develop RP after IMRT (4,5). The
pulmonary function of patients with LANSCLC is poorer than that of
patients with stage I or II NSCLC, thus RP occurs more easily.
Acute lung injury appears 1–3 months after radiotherapy, while
chronic lung damage (radiation fibrosis) evolves over 6–24 months
after radiotherapy (6).
At present, chest CT and X-ray are the main clinical
diagnostic methods for RP. However, they barely detect early
changes in pulmonary ventilation and blood flow. Thus, it is
necessary to evaluate early radioactive injury effectively.
Pulmonary function testing (PFT) is the main method to reflect the
ventilation function of the global lung, while lung perfusion
single photon emission computed tomography (SPECT) scanning is the
method to evaluate variation in blood flow.
In the present study, we aimed to develop a
quantitative method in order to reflect early change in perfusion
and to evaluate the change in ventilation function by PFT. At the
same time, we tried to explore the factors that caused these
changes.
Patients and methods
Patients
Twenty patients with LANSCLC were treated with IMRT
from July 2009 to August 2011 in Fujian Provincial Cancer Hospital.
Totally, there were 16 male patients and 4 female patients. The age
of patients was 38–68 years. The average age was 51.85±2.065 years.
Of them, 13 patients had a history of smoking and 7 patients never
smoked; 14 cases were central type lung cancer, while 6 cases were
peripheral type; 12 patients had been operated for lung cancer and
the others had no history of surgery. According to the patients’
condition, 7 patients received 1–2 cycles of concurrent
chemoradiotherapy based on platinum-containing drugs, and 13
patients received radiotherapy only. All of the patients underwent
lung perfusion SPECT scanning and PFT prior to and after
treatment.
Patient grouping
All of the patients were divided into two groups
according to the biological effective dose (BED). Grouping was
based on the NCCN Clinical Practice Guidelines in Oncology
(v.3.2011). The recommended dose of NCCN for NSCLC was 60–70 Gy; 60
Gy was approximately equal to our grouping criteria (BED=126,500
cGy).
Lung perfusion SPECT scanning and
quantification
Lung perfusion SPECT images were obtained based on a
dual-head γ camera (Infinia VC Hawkeye 4) equipped with a
low-energy and high-resolution collimator and a 4-slice spiral CT.
The instrument was produced by General Electric Company of America.
The imaging agents were 99mTc macroaggregated albumin (99mTc-MAA)
that was produced by the Guangdong Xi’ai Nucleus Pharmaceutical
Center, China.
Lung perfusion SPECT scanning included three
aspects: i) Sectional images of perfusion were taken. 99mTc-MAA
(185–370 kBq/5 ml) was administered by intravenous injection for
the patients in the supine position. The collimator was kept close
to the patients’ chest and both lungs were in the vision of the
camera. Each camera acquired thirty projection images over 180°
during 20 sec per projection as 128×128 matrices. The magnification
was 1.0. Patients were told to breathe calmly in order to reduce
interference of respiratory movement. ii) CT images were acquired.
Patients kept still in a supine position and breathed calmly. The
condition of scanning included voltage (140 kV), electric current
(2.5 mA), layer thickness (5 mm) and layer thickness of
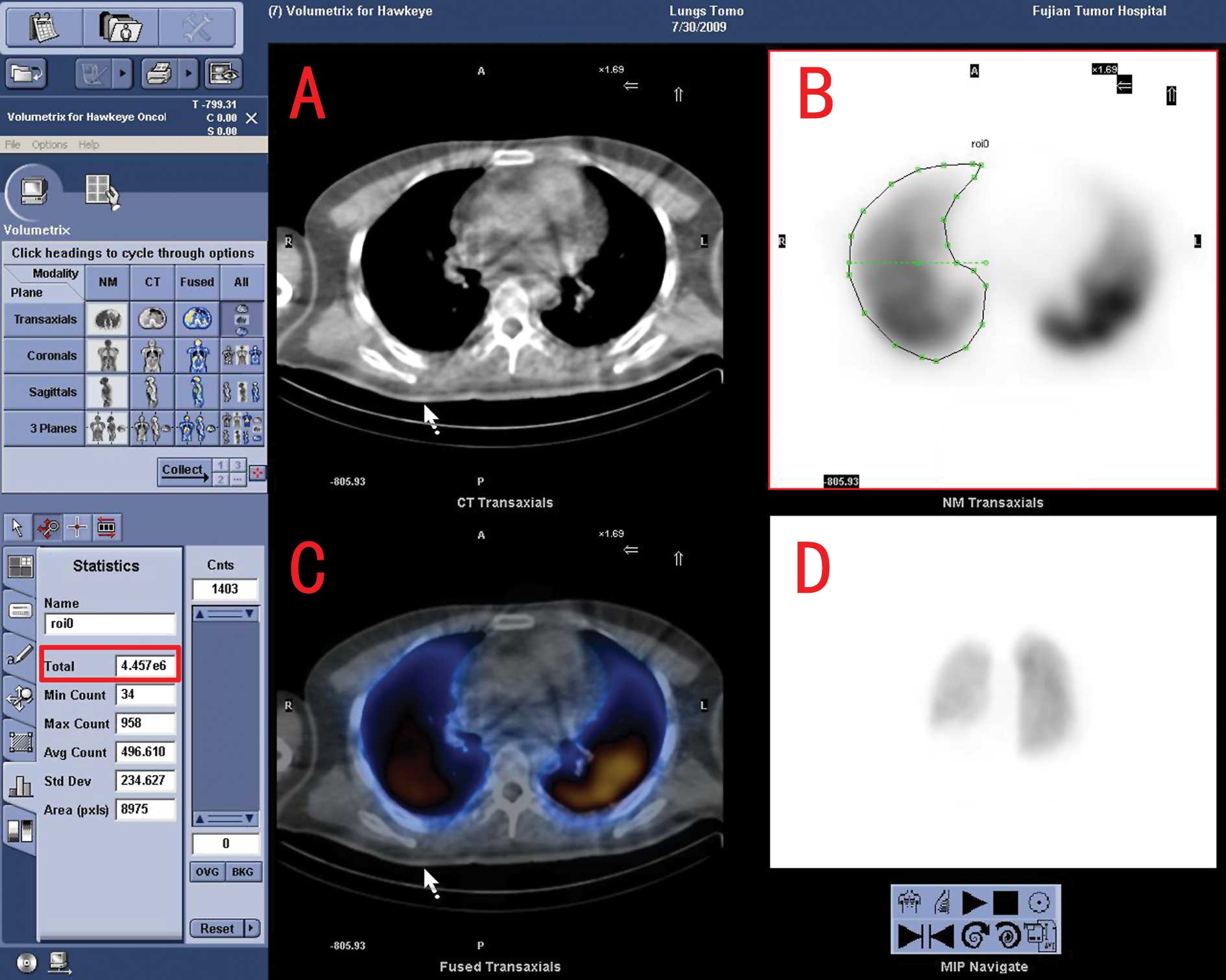
reconstruction (4 mm). iii) Image fusion was performed. Original
images were processed by GE Xeleris image fusion software (version
2.0). The fused image of the cross-section, sagittal section and
coronal section was acquired (Fig.
1).
The outline of the irradiated side lung was
delineated layer after layer from the apex to the base of the lung.
The radioactive count of each layer was counted as X (Fig. 1). The total radioactive count of
the irradiated lung was counted as T1 (T1 =
X1+X2+X3+...Xn). The
mean of the irradiated side lung was counted as M
(M=T1/n). The top layer Xi and bottom layer
Xr of the irradiated area were confirmed according to
the IMRT plan. The total radioactive count of the irradiated area
was counted as T2 (T2 =
Xi+Xi+1+Xi+2+...Xr).
According to the calculation above, lung perfusion index (LPI) was
calculated (LPI = T2/M).
Pulmonary function testing (PFT)
PFT was performed on a lung function instrument
(Jaeger, version 4.6; Germany). Parameters of PFT included vital
capacity (VC), forced vital capacity (FVC), forced expiratory
volume in 1 sec (FEV1) and the percentage
(FEV1/FVC), maximum midexpiratory flow
(MMEF25–75) and carbon monoxide diffusing capacity
(DLCO). Patients received PFT before and after IMRT. The detection
conditions were kept consistent.
Statistical analysis
All of the parameters for PFT and LPI were analyzed
with matched t-test and all the results were represented as the
means ± standard deviation. Statistical significance was indicated
by p-values <0.05. The LPI of the radical dose (BED >126,500
cGy) group and the non-radical dose (BED ≤126,500 cGy) group was
analyzed by matched t-test. Statistical significance was indicated
also by p-values <0.05.
Linear correlation between the percentage of
irradiated area and LPI was performed to evaluate their
relationship. Correlation coefficient (r) and p-values were
obtained. The statistical software used was PASWStatistics18.
Results
Statistics of ungrouped data
The statistics of ungrouped data of lung perfusion
and PFT are shown in Table I.
 | Table I.Statistics of ungrouped data. |
Table I.
Statistics of ungrouped data.
| Parameters | Mean ± SD
| p-value |
|---|
| Pre-IMRT | Post-IMRT | |
|---|
| VC | 2.99±0.18 | 2.97±0.17 | 0.760 |
| FVC | 2.92±0.18 | 2.94±0.18 | 0.663 |
| FEV1 | 2.29±0.14 | 2.34±0.60 | 0.477 |
| FEV1/FVC
(%) | 78.89±1.44 | 80.32±1.72 | 0.311 |
| MMEF | 1.87±0.18 | 1.93±0.17 | 0.624 |
| DLCO | 5.94±0.32 | 5.82±0.34 | 0.576 |
| LPI | 31.76±3.20 | 32.87±3.02 | 0.135 |
Statistics of grouped data
After grouping by BED, the radical dose (BED
>126,500 cGy) group consisted of 10 patients, and the
non-radical dose (BED ≤126,500 cGy) group consisted of 10 patients.
According to the WHO criteria, the therapeutical effects of all the
patients were evaluated. In the radical dose group, 1 case was
evaluated as complete response (CR), 8 cases as partial response
(PR) and 1 case as no change (NC). In the non-radical dose group, 4
cases were evaluated as CR, 3 cases as PR and 3 cases as NC. The
two groups were analyzed with matched t-test. The results are shown
in Table II.
 | Table II.Statistics of LPI in the radical dose
and non-radical dose groups. |
Table II.
Statistics of LPI in the radical dose
and non-radical dose groups.
| LPI (mean ± SD)
| p-value |
|---|
| Pre-IMRT | Post-IMRT | |
|---|
| Non-radical dose
group | 27.32±3.14 | 29.54±3.13 | 0.025 |
| Radical dose
group | 36.20±5.39 | 36.19±5.14 | 0.993 |
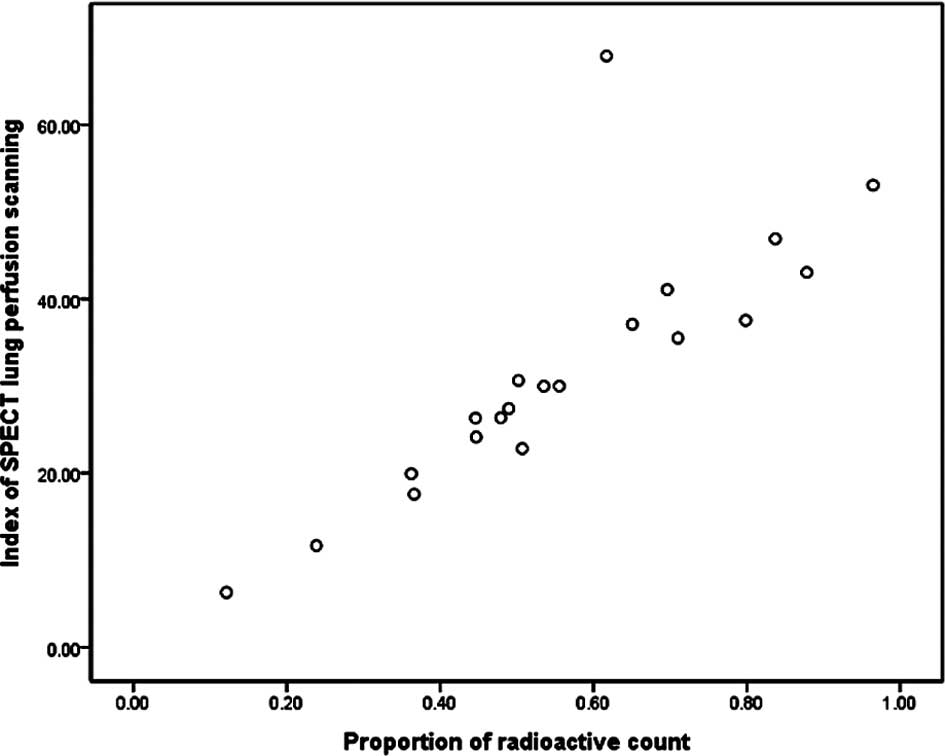
Linear correlation
As previously described, the total radioactive count
of the irradiated single lung was counted as T1. The
total radioactive count of the irradiated area was counted as
T2. Therefore, the percentage of the irradiated area was
described as P (P=T2/T1). The percentage of
the irradiated area and LPI were analyzed with linear correlation.
The result exhibited an excellent correlation between the
percentage and LPI, no matter whether this value was prior to or
after treatment (r=0.820 and r=0.823, respectively; p<0.001)
(Fig. 2).
Discussion
The main complications caused by radiotherapy for
lung cancer are acute radiation injury of the lung and radiation
pulmonary fibrosis. At present, the diagnosis of radiation-induced
lung injury mainly depends on symptomatology and image detection.
However, chest CT and X-ray barely detect early radiation injury.
Changes in ventilation and blood flow are usually discovered before
radiation injury develops into RP. Therefore, investigation of
these two aspects may have great significance for the early
evaluation of radiation injury.
PFT includes several parameters. VC and FVC reflect
the lung volume and total ventilatory function. FEV1 is
a measure of large- and medium-size airways, which is always
analyzed together with the percentage (FEV1/FVC).
Decreased FEV1 with a normal FEV1/FVC often
indicates a restrictive process, such as fibrosis (7), or reflects an acute exudative process
in the alveolar space (8).
MMEF25–75 stands for the average expiratory flow over
the middle half of the FVC and is considered to be a more sensitive
measure of small airway (bronchioles) narrowing than
FEV1. DLCO reflects the diffusing capacity through the
alveolar-capillary barrier. Since the function influenced first by
the radiation injury is blood gas exchange, DLCO is regarded as a
sensitive parameter for radiation injury. PFT is a test reflecting
the ventilation function of global lungs. In this study, none of
the parameters of PFT exhibited significant difference, as shown in
Table I, which may be due to the
fact that PFT was performed immediately after IMRT and some local
injury may not have yet appeared; it often takes several months for
parameters of PFT to manifest obvious changes. In studies that have
evaluated radiation injury by PFT, the follow-up period was 3–38
months. DLCO was found to be reduced by 5.7–14% and FEV1
was diminished by 1–7% (9–11). In a study by Miller et al,
parameters of PFT were continuously reduced during 2–8 years after
radiotherapy (11). Although there
was no significant difference in parameters of PFT in this study,
the results indicate that an early change in lung radiation injury
mainly reflects local injury. Lung perfusion SPECT scanning may be
more effective for the early diagnosis of radiation injury than
PFT.
Lung perfusion SPECT scanning is a functional
imaging modality. It reflects changes in local blood flow. It is
more sensitive to detect radiation-induced lung injury than CT and
X-ray (7). Theuws et al
reported that it was more common to note change caused by
radiotherapy in perfusion scanning than in CT (12). At present, lung perfusion SPECT
scanning is reported mainly according to the visual inspection of
the physician. This method is inevitably influenced by the doctor’s
subjective judgement, therefore it is difficult to measure early
subtle variations in perfusion.
Several studies have attempted to quantify SPECT
images by radioactive count. These studies indicate that the
radioactive count is an available quantitative method for SPECT
images (13–15). As described above, this study
calculated LPI through radioactive count. LPI related the blood
flow of the irradiated area and global single lung. After linear
correlation analysis, LPI and the percentage of the irradiated area
exhibited an excellent correlation (Fig. 2). Thus, we hypothesized that LPI
reflects the distribution of blood within and outside the
irradiated area. In order to explore the reason for these changes,
we evaluated the therapeutic effect using WHO criteria.
In the non-radical dose group, 4 cases were
evaluated as CR, 3 cases as PR and 3 cases as NC. The tumor size of
7 cases markedly decreased. Reduction in tumor size releases
compression to normal lung tissue, which may allow a portion of the
perfusion defect region restored blood flow. Munley et al
hypothesized that the area with poor perfusion caused by tumor
compression could recover after therapy (16). Non-radical dose group receives
lower dose radiotherapy than the radical dose group. The technique
of IMRT guarantees the dose of the target while protecting normal
lung tissue (3). Therefore,
radiotherapy has little influence on the non-irradiated area. In
the tumor mass, the percentage of the irradiated area throughout
the global single lung becomes larger after IMRT. This explained
the increase in LPI in this study. Of course, it must be pointed
out that the increase in LPI is just an increase in proportion, but
not an increase in global lung perfusion. The total radioactive
count decreases. In the radical dose group, large-dose radiation
damages both the blood flow of the irradiated area and that of the
non-irradiated area. Although tumor size in most cases is reduced
markedly, the recovery of blood flow is insignificant against the
damage of large-dose radiation. In the mass, post-IMRT LPI did not
exhibit significant difference with pre-IMRT LPI.
Many studies have confirmed that radiotherapy causes
a defect in blood flow (12,17,18).
However, few studies have focused on the change in percentage of
the irradiated area’s perfusion in global perfusion. This study
indicates that the percentage may predict the recovery of blood
flow in lung tissue around the tumor, which will provide a basis
for the prevention of lung function after radiotherapy. By
comparison of the two groups in this study, the factor of dose
significantly affected the radiation-induced pulmonary toxicity.
Radical dose radiotherapy also damaged the normal lung tissue,
while it inhibited cancer growth and invasion. Miller et al
observed bronchial stenosis following high-dose external-beam RT
(74–86 Gy) (19). Several studies
have probed the relationship between dose and radiation injury
through dose response curves (DRC), and these studies indicate that
reduction in local blood flow is proportional to the increase in
dose (20–22). Another two studies previously
reported that dose-dependent reductions in perfusion were noted as
early as 1.5 months after radiotherapy and peaked by approximately
6 months (23,24). In this study, the perfusion
scanning was performed immediately after IMRT. Therefore, the
result only displayed the difference between radical dose and
non-radical dose, whereas it did not display any correlation
between dose and reduction in perfusion.
Lung perfusion SPECT scanning is a method to
evaluate local pulmonary function, while PFT is a method for global
function. The combination of the two methods may be helpful for
diagnosing radiation-induced lung injury earlier. Marks et
al found that SPECT was useful in models for predicting
radiation-induced changes in PFT (25). Fan et al found a significant
correlation between local perfusion and global pulmonary function
(26). However, current PFT is
unable to determine early radiation injury.
In conclusion, the quantitative method of lung
perfusion SPECT scanning evaluates changes in perfusion early in
LANSCLC patients receiving a non-radical dose (BED ≤126,500 cGy)
IMRT. The current method of PFT is not able to evaluate the early
change in global lung function, since time is a contributing factor
for radiation-induced lung injury. Methodology of PFT should be
investigated to improve sensitivity. In addition, a larger sample
and longer-term studies are required to provide a basis for the
early diagnosis of radiation injury.
Acknowledgements
This study was supported by the Nature
Science Foundation of Fujian province (No. 2008J0268). The authors
express special appreciation for the technical support to Dr Lin
Duanyu, Department of Nuclear Medicine, Fujian Provincial Cancer
Hospital Affiliated to Fujian Medical University, and also for her
assistance in the measurements.
References
|
1.
|
Mehta V: Radiation pneumonitis and
pulmonary fibrosis in non-small-cell lung cancer: pulmonary
function, prediction, and prevention. Int J Radiat Oncol Biol Phys.
63:5–24. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Marks LB, Yu X, Vujaskovic Z, et al:
Radiation-induced lung injury. Semin Radiat Oncol. 13:333–345.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Murshed H, Liu HH, Liao Z, et al: Dose and
volume reduction for normal lung using intensity-modulated
radiotherapy for advanced-stage non-small-cell lung cancer. Int J
Radiat Oncol Biol Phys. 58:1258–1267. 2004.PubMed/NCBI
|
|
4.
|
Sura S, Gupta V, Yorke E, et al:
Intensity-modulated radiation therapy (IMRT) for inoperable
non-small cell lung cancer: the Memorial Sloan-Kettering Cancer
Center (MSKCC) experience. Radiother Oncol. 87:17–23. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
5.
|
Yom SS, Liao Z, Liu HH, et al: Initial
evaluation of treatment-related pneumonitis in advanced-stage
non-small-cell lung cancer patients treated with concurrent
chemotherapy and intensity-modulated radiotherapy. Int J Radiat
Oncol Biol Phys. 68:94–102. 2007. View Article : Google Scholar
|
|
6.
|
Graves PR, Siddiqui F, Anscher MS, et al:
Radiation pulmonary toxicity: from mechanisms to management. Semin
Radiat Oncol. 20:201–207. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7.
|
Ghafoori P, Marks LB, Vujaskovic Z, et al:
Radiation-induced lung injury. Assessment, management, and
prevention. Oncology (Williston Park). 22:37–47. 2008.PubMed/NCBI
|
|
8.
|
Spyropoulou D, Leotsinidis M, Tsiamita M,
et al: Pulmonary function testing in women with breast cancer
treated with radiotherapy and chemotherapy. In Vivo. 23:867–872.
2009.PubMed/NCBI
|
|
9.
|
Allen AM, Henning GT, Ten Haken RK, et al:
Do dose-volume metrics predict pulmonary function changes in lung
irradiation? Int J Radiat Oncol Biol Phys. 55:921–929.
2003.PubMed/NCBI
|
|
10.
|
De Jaeger K, Seppenwoolde Y, Boersma LJ,
et al: Pulmonary function following high-dose radiotherapy of
non-small-cell lung cancer. Int J Radiat Oncol Biol Phys.
55:1331–1340. 2003.PubMed/NCBI
|
|
11.
|
Miller KL, Zhou SM, Barrier RC Jr, et al:
Long-term changes in pulmonary function tests after definitive
radiotherapy for lung cancer. Int J Radiat Oncol Biol Phys.
56:611–615. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Theuws JC, Kwa SL, Wagenaar AC, et al:
Dose-effect relations for early local pulmonary injury after
irradiation for malignant lymphoma and breast cancer. Radiother
Oncol. 48:33–43. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Kim S, Kim HK, Kang DY, et al:
Intra-operative sentinel lymph node identification using a novel
receptor-binding agent (technetium-99m neomannosyl human serum
albumin, 99mTc-MSA) in stage I non-small cell lung cancer. Eur J
Cardiothorac Surg. 37:1450–1456. 2010. View Article : Google Scholar
|
|
14.
|
Zhang WJ, Zheng R, Zhao LJ, et al: Utility
of SPECT lung perfusion scans in assessing early changes in
pulmonary function of patients with lung cancer after radiotherapy.
Ai Zheng. 23:1180–1184. 2004.PubMed/NCBI
|
|
15.
|
Ahn BC, Kim HJ, Lee SW, et al: New
quantitative method for bone tracer uptake of temporomandibular
joint using Tc-99m MDP skull SPECT. Ann Nucl Med. 23:651–656. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Munley MT, Marks LB, Hardenbergh PH, et
al: Functional imaging of normal tissues with nuclear medicine:
applications in radiotherapy. Semin Radiat Oncol. 11:28–36. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Curran WJ Jr, Moldofsky PJ and Solin LJ:
Observations on the predictive value of perfusion lung scans on
post-irradiation pulmonary function among 210 patients with
bronchogenic carcinoma. Int J Radiat Oncol Biol Phys. 24:31–36.
1992. View Article : Google Scholar
|
|
18.
|
Boersma LJ, Damen EM, de Boer RW, et al:
Estimation of overall pulmonary function after irradiation using
dose-effect relations for local functional injury. Radiother Oncol.
36:15–23. 1995. View Article : Google Scholar
|
|
19.
|
Miller KL, Shafman TD, Anscher MS, et al:
Bronchial stenosis: an underreported complication of high-dose
external beam radiotherapy for lung cancer. Int J Radiat Oncol Biol
Phys. 61:64–69. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
20.
|
Marks LB, Munley MT, Spencer DP, et al:
Quantification of radiation-induced regional lung injury with
perfusion imaging. Int J Radiat Oncol Biol Phys. 38:399–409. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
21.
|
Zhang J, Ma J, Zhou S, et al:
Radiation-induced reductions in regional lung perfusion: 0.1-12
year data from a prospective clinical study. Int J Radiat Oncol
Biol Phys. 76:425–432. 2010.PubMed/NCBI
|
|
22.
|
Kong FM, Frey KA, Quint LE, et al: A pilot
study of [18F]fluorodeoxyglucose positron emission tomography scans
during and after radiation-based therapy in patients with non
small-cell lung cancer. J Clin Oncol. 25:3116–3123. 2007.
|
|
23.
|
Theuws JC, Seppenwoolde Y, Kwa SL, et al:
Changes in local pulmonary injury up to 48 months after irradiation
for lymphoma and breast cancer. Int J Radiat Oncol Biol Phys.
47:1201–1208. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
24.
|
Woel RT, Munley MT, Hollis D, et al: The
time course of radiation therapy-induced reductions in regional
perfusion: a prospective study with >5 years of follow-up. Int J
Radiat Oncol Biol Phys. 52:58–67. 2002.PubMed/NCBI
|
|
25.
|
Marks LB, Hollis D, Munley M, et al: The
role of lung perfusion imaging in predicting the direction of
radiation-induced changes in pulmonary function tests. Cancer.
88:2135–2141. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
26.
|
Fan M, Marks LB, Lind P, et al: Relating
radiation-induced regional lung injury to changes in pulmonary
function tests. Int J Radiat Oncol Biol Phys. 51:311–317. 2001.
View Article : Google Scholar : PubMed/NCBI
|