Introduction
Patients with urinary diversion may exhibit various
complications, including upper urinary tract changes (i.e.,
hydronephrosis or contracted kidney), urinary infections and
urolithiasis, and renal dysfunction is often observed (1–5).
Over the past decade, the disease concept of chronic kidney disease
(CKD) has been advocated and renal dysfunction resulting from
urinary diversion should be considered to be an indication of CKD
(6–9). It has been reported that the
prevalence of renal failure varies widely (10–60%) among cohorts
with urinary intestinal diversion (1,5,10),
possibly due to inconsistencies in the methods utilized to define
renal dysfunction. These studies differ in their definitions of
renal failure; renal deterioration and morphological deterioration
of the kidney are used synonymously, while the etiology of renal
failure is often unknown. In the present study, renal dysfunction
was investigated in patients with ileal conduit urinary diversion
using the estimated glomerular filtration rate (eGFR), which is a
more universal method. A cross-sectional study was performed on the
renal function of ileal conduit diversion patients and the
prevalence of CKD and risk factors for decreased eGFR was
studied.
Patients and methods
Study design
A cross-sectional study was performed in patients
with ileal conduit urinary diversion.
Patients
A total of 102 outpatients who had undergone ileal
conduit diversion for bladder cancer between April 1979 and March
2011 at Osaka City University Hospital (Osaka, Japan) were studied.
The subjects were selected from the total population of patients
who had undergone ileal conduit urinary diversion (n=370). Out of
the 370 patients, 268 were excluded based on the exclusion criteria
which were: subjects with incomplete follow-up (including deceased
cases), post-nephrectomy, severe urinary tract infection, chronic
glomerulonephritis, chronic inflammatory disease, metastasis or
recurrence of bladder cancer or other malignant diseases. Table I shows the characteristics of the
102 patients with ileal conduit diversion.
 | Table ICharacteristics of ileal conduit
diversion patients with or without CKD and healthy subjects. |
Table I
Characteristics of ileal conduit
diversion patients with or without CKD and healthy subjects.
| Variable | Total (n=102) | Without CKD
(n=42) | With CKD (n=60) | P-valuea | Healthy subjects
(n=63) |
|---|
| Age (years), mean ±
SD | 69.1±8.9 | 65.1±9.3 | 72.5±6.8 | <0.0001 | 68.0±8.1 |
| Gender (males), n
(%) | 79 (77.5) | 32 (76.2) | 47 (78.3) | NS | 43 (68.3) |
| Hypertension, n
(%) | 37 (36.3) | 8 (19.0) | 29 (48.3) | 0.005 | 16 (25.4) |
| Diabetes mellitus, n
(%) | 16 (15.7) | 5 (11.9) | 10 (16.7) | NS | 6 (9.5) |
| Dyslipidemia, n
(%) | 18 (17.6) | 4 (9.5) | 14 (23.3) | NS | 22 (34.9) |
| Post-operative
duration (years), mean ± SD | 9.4±5.5 | 7.9±3.1 | 10.3±6.6 | 0.031 | - |
| Hydronephrosis, n
(%) | 24 (23.5) | 2 (4.8) | 22 (36.7) | <0.0001 | - |
| Pre-operative
hydronephrosis, n (%) | 9 (8.8) | 1 (2.4) | 8 (13.3) | 0.011 | - |
| Post-operative
hydronephrosis, n (%) | 15 (14.7) | 1 (2.4) | 14 (23.3) | 0.001 | - |
| Past history of
pyelonephritis, n (%) | 33 (32.4) | 7 (16.7) | 24 (40.0) | 0.021 | - |
| Urolithiasis, n
(%) | 14 (13.7) | 2 (4.8) | 12 (20.0) | 0.039 | - |
| eGFR (ml/min/1.73
m2), mean ± SD | 62.3±22.0 | 78.0±15.7 | 50.6±17.3 | <0.0001 | 78.4±22.1 |
| Proteinuria, n
(%) | 26 (25.5) | 0 (0) | 26 (43.3) | <0.0001 | 2 (3.2) |
| CKD, n (%) | 60 (58.8) | - | - | - | 11 (17.5) |
The control group consisted of 63 age- and
gender-matched healthy subjects who voluntarily underwent
multiphasic health screening, including a physical examination,
electrocardiography, chest X-ray, liver and renal function tests
and blood glucose and lipid tests, at Ohno Memorial Hospital
between April 2008 and March 2009. Informed consent was obtained
from all patients and control volunteers prior to their
participation in the study, which was approved by the human ethics
committee of Osaka City University Hospital (Osaka, Japan).
Surgical technique
An ileal segment 15 to 20 cm in length was selected
10 to 15 cm from the ileocecal valve. The ureteral-ileal
anastomoses were performed separately by 2 running sutures using
the Nesbit technique and were stented with 7- or 8-Fr catheters for
7 to 10 days. The ileal segment was anastomosed to the anterior
abdominal wall in a nipple-to-stoma fashion.
Definition of CKD
In all patients, serum creatinine levels were
measured periodically during follow-up and the serum creatinine
concentration levels obtained at the patients’ previous visit were
used for statistical analysis (mean time from surgery, 9.4±5.5
years; range, 1.8–31.7 years). The eGFR was calculated using the
equation of the Japanese Society of Nephrology as follows: 194 x
age−0.287 x serum creatinine−1.094, including
a correction factor of 0.739 for females (11). In the present study, CKD was
primarily defined as having an eGFR of <60 ml/min/1.73
m2 or eGFR of ≥60 ml/min/1.73 m2 with
proteinuria. Proteinuria was defined as a urinary protein level of
≥1 (∼≥30 mg/dl) in the dipstick test using a spontaneously and
freshly voided urine sample, persisting for at least 3 months.
Risk factors
To evaluate the clinical risk factors, the age and
presence or absence of hypertension, diabetes mellitus,
dyslipidemia, cardiovascular disease and hydronephrosis were
investigated. Hypertension was defined as: i) the administration of
antihypertensive agents and/or a history of this disorder; ii) a
systolic blood pressure >140 mmHg; or iii) a diastolic blood
pressure >90 mmHg. Diabetes mellitus was defined by: i) the
administration of insulin or oral antidiabetic agents; or ii) prior
diagnosis according to the Report of the Expert Committee on the
Diagnosis and Classification of Diabetes Mellitus of the American
Diabetes Association (12).
Dyslipidemia was defined as a low-density lipoprotein cholesterol
level >140 mg/dl, triglyceride >150 mg/dl and high-density
lipoprotein cholesterol <40 mg/dl or had undergone medical
treatment for hyperlipidemia. Blood samples were obtained following
overnight fasting. The diagnosis of pyelonephritis was based on
clinical manifestations, body temperature, laboratory test results
and imaging data [plain X-ray, ultrasonography and computed
tomography (CT)]. Urolithiasis was diagnosed in patients with a
history of urolithiasis, as well as those who had no symptoms but
were observed to have stone formation in their follow-up CT.
Hydronephrosis was diagnosed using ultrasonography, drip infusion
pyelography or CT.
Statistical analysis
The data are expressed as percentages or as the
means ± standard deviation (SD), where appropriate. Differences
between the groups were examined using the Student’s t-test or
Mann-Whitney U test. Changes within each group were evaluated using
the paired Student’s t-test. Categorical variables were compared
using the Chi-square test. Multiple logistic regression analysis
was performed to assess the effect of the variables on the presence
of CKD, while dummy variables were used to assess the presence of
hypertension, diabetes mellitus, dyslipidemia, urolithiasis,
hydronephrosis and pyelonephritis (1 = presence, 0 = absence).
In order to determine the association between
hydronephrosis and the presence of CKD, several methods were used
to define hydronephrosis in the logistic regression analysis.
According to the variables, model 1 contained patients with a past
history of hydronephrosis, including prior to surgery, model 2
contained patients with pre-operative hydronephrosis and model 3
contained those with post-operative hydronephrosis. A value of
P<0.05 was considered to indicate a statistically significant
difference. These tests were performed using the Stat View V
Statistical System (SAS Institute Inc., Cary, NC, USA).
Results
Demographics and characteristics of the
ileal conduit diversion patients with or without CKD and healthy
subjects
Table I shows the
characteristics of the 102 patients with ileal conduit diversion
and the 63 healthy control subjects. The prevalence of CKD was
significantly higher in the ileal conduit diversion patients
compared with the healthy subjects [60 patients (58.8%) vs. 11
healthy subjects (17.5%), P<0.0001].
The mean age of the patients with CKD was greater
than that of the patients without CKD (P<0.0001). The mean
post-operative duration of the patients with CKD was longer than
that of the patients without CKD (P=0.031).
Hypertension, hydronephrosis, pre-operative
hydronephrosis, post-operative hydronephrosis, pyelonephritis and
urolithiasis were more prevalent in the patients with CKD (P=0.005,
<0.0001, 0.011, 0.001, 0.021, 0.039, respectively). No
significant differences were observed in the other factors between
the patients with and without CKD. The prevalence of CKD with an
eGFR of <60 ml/min/1.73 m2 among the patients aged
≥50 years was 47.5% (47/99).
Temporal changes in eGFR following
urinary diversion
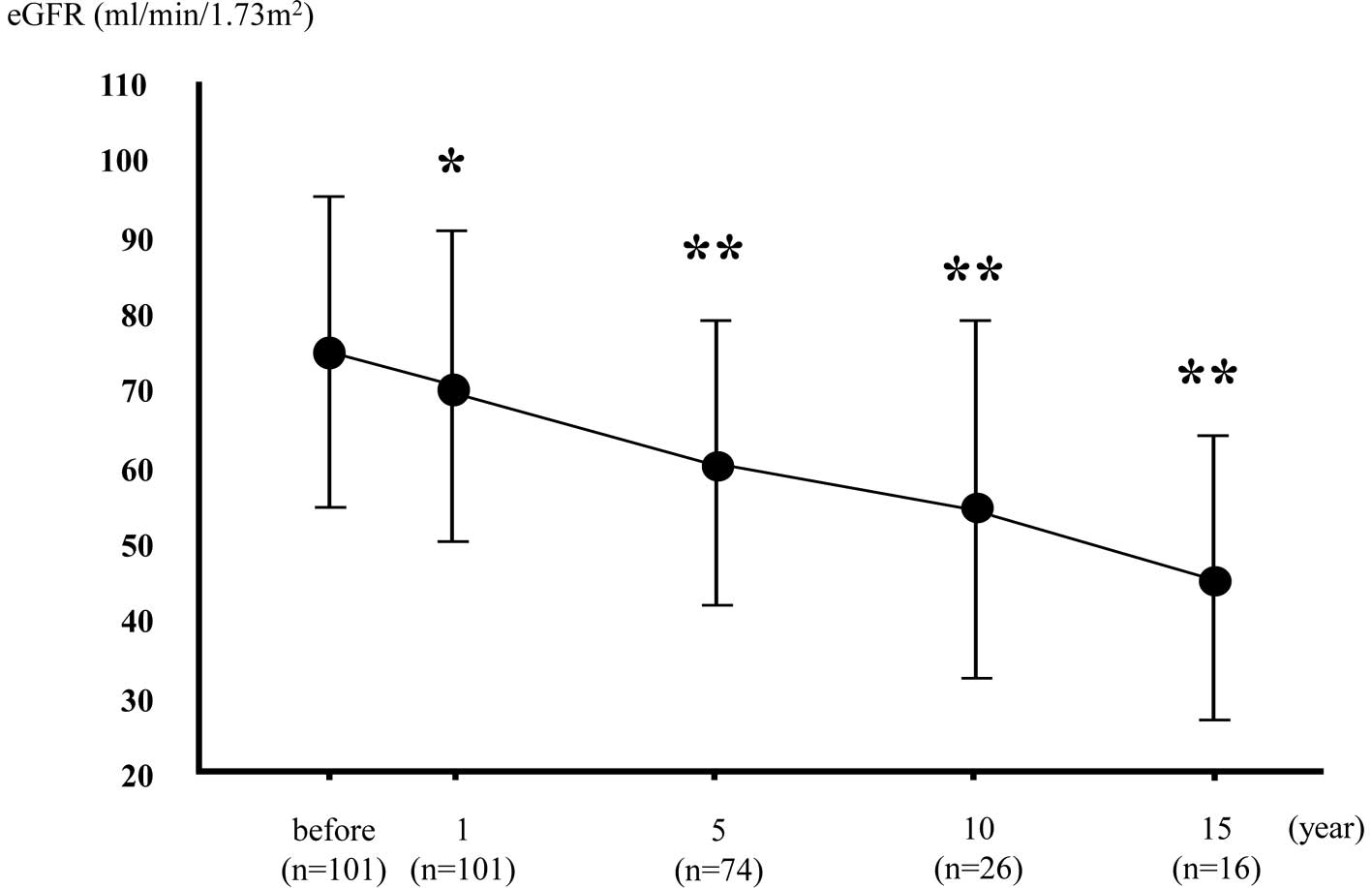
The mean eGFR values prior to surgery and at 1, 5,
10 and 15 years after surgery for the patients with ileal conduit
diversion are shown in Fig. 1 (the
cut-off value was 15 years due to the low number patients after 20
years). The mean decrease in eGFR per year for the patients with
urinary diversion was 0.95±2.0 ml/min/1.73 m2.
Univariate logistic regression analysis
for factors associated with CKD
Univariate logistic regression analysis was
performed to examine the correlation between CKD and risk factors
in the patients with ileal conduit diversion (Table II). The presence of CKD was
significantly associated with older age, longer post-operative
duration, the presence of hypertension, a past history of
hydronephrosis, post-operative hydronephrosis and urolithiasis.
 | Table IIUnivariate logistic regression
analysis of factors associated with CKD in patients with ileal
conduit diversion. |
Table II
Univariate logistic regression
analysis of factors associated with CKD in patients with ileal
conduit diversion.
| Variable | Unit increase | OR (95% CI) | P-value |
|---|
| Age | 1 year | 1.14 (1.07–1.22) | <0.0001 |
| Gender (males vs.
females) | | 1.13 (0.44–2.89) | 0.888 |
| Post-operative
durations | 1 year | 1.10 (1.01–1.20) | 0.039 |
| Hypertension
(presence vs. absence) | | 3.98 (1.58–9.99) | 0.003 |
| Diabetes mellitus
(presence vs. absence) | | 1.20 (0.40–3.60) | 0.745 |
| Dyslipidemia
(presence vs. absence) | | 2.89 (0.88–9.52) | 0.081 |
| Past history of
hydronephrosis (presence vs. absence) | | 11.58
(2.55–52.64) | 0.0015 |
| Pre-operative
hydronephrosis (presence vs. absence) | | 6.31
(0.76–52.50) | 0.089 |
| Post-operative
hydronephrosis (presence vs. absence) | | 9.94
(2.11–46.85) | 0.004 |
| Past history of
pyelonephritis (presence vs. absence) | | 2.44 (0.99–6.01) | 0.052 |
| Urolithiasis
(presence vs. absence) | | 5.00
(1.06–23.67) | 0.043 |
Multivariate logistic regression analysis
for factors associated with CKD
Multiple logistic regression analysis was performed
to examine the factors associated with the presence of CKD,
independent of the other factors (Table III). Each multiple model included
the unmodifiable basic clinical factors (age, gender,
post-operative duration and diabetes mellitus) and the significant
factors (hypertension, urolithiasis and hydronephrosis) obtained
from the univariate analysis. Models 1 to 3 included a past history
of hydronephrosis, pre-operative hydronephrosis and post-operative
hydronephrosis, respectively, as variables for hydronephrosis. In
these models, older age and the presence of hypertension,
urolithiasis, a past history of hydronephrosis and post-operative
hydronephrosis were indicated to be independent and significant
factors associated with the presence of CKD, whereas the presence
of pre-operative hydronephrosis was of borderline significance.
 | Table IIIMultiple logistic regression analysis
of factors associated with CKD in patients with ileal conduit
diversion. |
Table III
Multiple logistic regression analysis
of factors associated with CKD in patients with ileal conduit
diversion.
| Variable | Unit increase | Model 1 OR (95%
CI) | Model 2 OR (95%
CI) | Model 3 OR (95%
CI) |
|---|
| Age | 1 year | 1.16
(1.07–1.26)c | 1.16
(1.07–1.25)c | 1.17
(1.08–1.27)c |
| Gender (males vs.
females) | | 0.89 (0.23–3.49) | 0.92
(0.26–3.31) | 0.85
(0.23–3.08) |
| Post operative
durations | 1 year | 1.06
(0.94–1.19) | 1.05
(0.94-.18) | 1.06
(0.95–1.19) |
| Hypertension
(presence vs. absence) | | 4.03
(1.20–13.56)a | 4.70
(1.46–15.03)b | 4.26
(1.31–13.78)a |
| Diabetes mellitus
(presence vs. absence) | | 0.63
(0.16–2.49) | 0.65
(0.18–2.37) | 0.62
(0.17–2.32) |
| Urolithiasis
(presence vs. absence) | | 15.76
(1.93–129.04)a | 13.45
(1.83–98.69)a | 14.35
(1.73–119.09)a |
| Past history of
hydronephrosis (presence vs. absence) | | 21.85
(2.22–214.83)b | - | - |
| Pre-operative
hydronephrosis (presence vs. absence) | | - | 32.14
(0.38–2720.88) | - |
| Post-operative
hydronephrosis (presence vs. absence) | | - | - | 15.41
(1.16–204.98)a |
Discussion
In the present study, we investigated: i) the
prevalence of CKD; ii) the temporal changes in post-operative eGFR;
and iii) the clinical factors associated with the presence of CKD
in patients with ileal conduit urinary diversion. The prevalence of
CKD was significantly higher in the ileal conduit diversion
patients compared with the healthy subjects. The mean decrease in
eGFR per year for the patients with urinary diversion was 0.95±2.0
ml/min/1.73 m2. Multiple logistic regression analysis
revealed that the independent and significant factors associated
with the presence of CKD included older age and the presence of
hypertension, urolithiasis and a past history of
hydronephrosis.
The overall prevalence of CKD in the ileal conduit
diversion patients was 58.8% (60/102), which was significantly
higher compared with that of the healthy subjects (17.5%, 11/63;
Table I). In the Japanese
population aged 50 years or older, the prevalence of CKD with an
eGFR less than 60 ml/min/1.73 m2 was previously reported
to be 18.6% (13). In the present
study, among the subjects aged 50 and over, the prevalence of CKD
with an eGFR less than 60 ml/min/1.73 m2 was 47.5%
(47/99). These findings indicated a higher prevalence of CKD in
ileal conduit diversion cohorts compared with the age-matched
general population, suggesting that ileal conduit urinary diversion
may be a risk factor for CKD. Furthermore, the mean yearly decrease
in eGFR of the patients was 0.95 ml/min/1.73 m2
(Fig. 1), which was approximately
3 times that of previously reported Japanese subjects at 0.36
ml/min/1.73 m2 (14).
Although it is well-known that renal deterioration is a common
complication in ileal conduit diversion patients (1–10),
this is the first study to reveal the prevalence of CKD.
In the present study, logistic regression analysis
revealed that older age and the presence of hypertension,
urolithiasis and a past history of hydronephrosis were the
independent and significant factors associated with the presence of
CKD (Tables II and III). The results indicating that age and
hypertension are clinical risk factors associated with CKD in the
ileal conduit urinary diversion patients are consistent with those
from previous studies in general populations (15–17).
It has also been reported that urolithiasis represents a
significant and independent risk factor for CKD in the general
population (18), which is
consistent with the results of the present study for the patients
with the ileal conduit urinary diversion.
Hydronephrosis is a well-known risk factor for CKD,
which may cause CKD in ileal conduit diversion patients as well as
in cohorts without urinary diversion. The findings of the present
study revealed a past history of hydronephrosis in 23.5% of the
patients, of which 8.9% exhibited pre-operative hydronephrosis and
14.9% exhibited post-operative hydronephrosis. Singh et al
(3) reported upper urinary tract
dilatation in 34% of patients and Madersbacher et al
(1) reported that, following ileal
conduit diversion, morphological/functional or pre-operative upper
urinary tract pathology deterioration occurred in 35/131 (27%)
patients. These findings are partially consistent with those of the
present study. Multivariate logistic regression analysis indicated
that hydronephrosis was a significant risk factor for the presence
of CKD in the ileal conduit urinary diversion patients (Tables II and III). Pre-operative hydronephrosis was
associated with the presence of CKD to some extent, but
post-operative hydronephrosis was more strongly associated
(Table III). This may be since
renal function may be improved by urinary diversion in renal
dysfunction caused by pre-operative urinary obstruction
(hydronephrosis) if the kidney function is not impaired as a result
of the non-functioning kidney due to chronic obstruction. Ileal
conduit urinary diversion is a low pressure reservoir in which
outflow is not obstructed, but it may cause hydronephrosis due to
the non-physiological attachment of the ureter, anastomotic
stricture, stomal stenosis and urolithiasis. Therefore, periodic
monitoring following surgery is necessary and when hydronephrosis
occurs, it is important to use appropriate monitoring to prevent
CKD.
The present study had certain limitations. Firstly,
due to the cross-sectional design, the findings do not necessarily
indicate causality, but this point may be further elucidated in
future longitudinal studies. Secondly, CKD was investigated only in
patients with ileal conduit urinary diversion; therefore, further
studies are required to elucidate CKD in the patients with other
urinary diversion techniques.
In conclusion, we revealed an increased prevalence
of CKD in patients with ileal conduit urinary diversion, suggesting
the need for improved management of hypertension, urolithiasis and
hydronephrosis following surgery. Cancer control is indisputably
the most important consideration in the prognosis of patients
following total cystectomy, but given the high incidence of CKD,
active monitoring of functional/morphological renal changes should
be considered to prevent CKD following urinary diversion.
Acknowledgements
This study was supported by grants
from the Osaka Medical Research Foundation for Incurable
Diseases.
References
|
1
|
Madersbacher S, Schmidt J, Eberle JM, et
al: Long-term outcome of ileal conduit diversion. J Urol.
169:985–990. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Neal DE: Complications of ileal conduit
diversion in adults with cancer followed up for at least five
years. Br Med J (Clin Res Ed). 290:1695–1697. 1985.PubMed/NCBI
|
|
3
|
Singh G, Wilkinson JM and Thomas DG:
Supravesical diversion for incontinence: a long-term follow-up. Br
J Urol. 79:348–353. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sullivan JW, Grabstald H and Whitmore WF
Jr: Complications of ureteroileal conduit with radical cystectomy:
review of 336 cases. J Urol. 124:797–801. 1980.PubMed/NCBI
|
|
5
|
Shimko MS, Tollefson MK, Umbreit EC,
Farmer SA, Blute ML and Frank I: Long-term complications of conduit
urinary diversion. J Urol. 185:562–567. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Foley RN, Murray AM, Li S, et al: Chronic
kidney disease and the risk for cardiovascular disease, renal
replacement, and death in the United States Medicare population,
1998 to 1999. J Am Soc Nephrol. 16:489–495. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Go AS, Chertow GM, Fan D, McCulloch CE and
Hsu CY: Chronic kidney disease and the risks of death,
cardiovascular events, and hospitalization. N Engl J Med.
351:1296–1305. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sarnak MJ, Levey AS, Schoolwerth AC, et
al: Kidney disease as a risk factor for development of
cardiovascular disease: a statement from the American Heart
Association Councils on Kidney in Cardiovascular Disease, High
Blood Pressure Research, Clinical Cardiology, and Epidemiology and
Prevention. Circulation. 108:2154–2169. 2003. View Article : Google Scholar
|
|
9
|
Shlipak MG, Sarnak MJ, Katz R, et al:
Cystatin C and the risk of death and cardiovascular events among
elderly persons. N Engl J Med. 352:2049–2060. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Koch MO, McDougal WS, Hall MC, Hill DE,
Braren HV and Donofrio MN: Long-term metabolic effects of urinary
diversion: a comparison of myelomeningocele patients managed by
clean intermittent catheterization and urinary diversion. J Urol.
147:1343–1347. 1992.
|
|
11
|
Matsuo S, Imai E, Horio M, et al: Revised
equations for estimated GFR from serum creatinine in Japan. Am J
Kidney Dis. 53:982–992. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Report of the Expert Committee on the
Diagnosis and Classification of Diabetes Mellitus. Diabetes Care.
20:1183–1197. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Imai E, Horio M, Watanabe T, et al:
Prevalence of chronic kidney disease in the Japanese general
population. Clin Exp Nephrol. 13:621–630. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Imai E, Horio M, Yamagata K, et al: Slower
decline of glomerular filtration rate in the Japanese general
population: a longitudinal 10-year follow-up study. Hypertens Res.
31:433–441. 2008.PubMed/NCBI
|
|
15
|
Chen N, Wang W, Huang Y, et al:
Community-based study on CKD subjects and the associated risk
factors. Nephrol Dial Transplant. 24:2117–2123. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Shulman NB, Ford CE, Hall WD, et al:
Prognostic value of serum creatinine and effect of treatment of
hypertension on renal function. Results from the hypertension
detection and follow-up program The Hypertension Detection and
Follow-up Program Cooperative Group. Hypertension. 13:I80–I93.
1989. View Article : Google Scholar
|
|
17
|
Walker WG, Neaton JD, Cutler JA, Neuwirth
R and Cohen JD: Renal function change in hypertensive members of
the Multiple Risk Factor Intervention Trial. Racial and treatment
effects The MRFIT Research Group. JAMA. 268:3085–3091. 1992.
View Article : Google Scholar
|
|
18
|
Rule AD, Bergstralh EJ, Melton LJ 3rd, Li
X, Weaver AL and Lieske JC: Kidney stones and the risk for chronic
kidney disease. Clin J Am Soc Nephrol. 4:804–811. 2009. View Article : Google Scholar : PubMed/NCBI
|