Introduction
A burn is defined as damage to body tissue by heat,
chemicals, electricity, sunlight or radiation. Scalds from hot
liquids and steam, building fires and flammable liquids and gases
are the most common causes of burns. Another type of burn is an
inhalation injury, caused by inhaling smoke. There are three types
of burns: first-degree burns which only damage the outer layer of
skin, second-degree burns which damage the outer layer and the
layer beneath, and third-degree burns, which damage or destroy the
deepest layers of skin and the tissues underneath. Burns may cause
swelling, blistering, scarring, shock and mortality. They may lead
to infections due to the fact that the skin’s protective barrier is
damaged (1). Antibiotics are
capable of preventing or treating infections. An intracranial
hemorrhage (ICH) is a hemorrhage, or bleeding, within the skull.
Intracranial bleeding occurs when a blood vessel within the skull
ruptures or leaks. It may result from physical trauma (such as a
head injury) or have a non-traumatic cause (as occurs in a
hemorrhagic stroke) such as a ruptured aneurysm. Anticoagulant
therapy, used in the treatment of disorders of blood clotting, may
heighten the risk of intracranial hemorrhage (2). Intracranial hemorrhaging is a serious
medical emergency as the build-up of blood within the skull may
cause the intracranial pressure to increase, which may crush
delicate brain tissue or limit its blood supply (3). Severe increases in intracranial
pressure may lead to brain herniation, in which sections of the
brain are squeezed past structures in the skull. Multiple ICHs are
rare in severe burn patients and the pathogenesis remains unclear.
Computed tomography (CT) scans are a definitive tool for accurately
diagnosing ICHs (4). Medical
treatment and surgical therapy are available for ICH patients.
According to the condition of the patient, timely diagnosis and an
optimal choice of treatment methods are vital in order to achieve a
successful outcome. In recent years, the incidence of burns
complicated by intracranial hemorrhaging has rarely been mentioned
in the literature. In order to identify disease features and the
probable etiology and improve the prevention, diagnosis and
treatment of multiple ICHs following severe burns, we reviewed 16
cases from a total of 397 patients with severe burns complicated by
multiple ICHs who were admitted to the Third Xiangya Hospital of
Central South University (Changsha, China) from 1999 to 2010.
Patients and methods
General conditions
This study included 16 patients (5 females and 11
males), ranging from 30–56 years old (mean 45±6.70 years). All 16
patients were treated at a local hospital prior to being admitted
to the Third Xiangya Hospital of Central South University. Of these
patients, six were admitted to the hospital 7 days after having
received their burn injury, four on day eight, four on day 12, one
on day 18 and one on day 23. Upon admission, all 16 patients were
conscious and not in shock. Cranial CT scans of the brain revealed
no abnormalities. The total body surface area (TBSA) of the burn
wound was 60–70% in eight cases, 70–80% in four cases, 80–90% in
three cases and 95% in one case, an average of 70.5±10.64%. The
area of third-degree burns was <15% in ten cases, 15–20% in
three cases, 20–30% in two cases, and 30% in one case, with an
average of 18.38±7.01%. The study was approved by the Ethics
Committee of The Third Xiangya Hospital of Central South
University. Written informed consent was obtained from all
patients.
Hemorrhage following severe burns
Emergency CT examination, due to the sudden onset of
symptoms in the nervous system in all patients, confirmed
intracerebral hemorrhaging. On the eighth day following the burn,
eight patients presented with hemorrhaging, two patients presented
with hemorrhaging on day nine, three on day 15 and one each on days
20, 25 and 37. There were five cases of brainstem hemorrhaging,
nine cases of intracerebral hemorrhaging and two cases of
subarachnoid hemorrhaging. The volume of blood lost was <30 ml
in ten cases and >30 ml in six cases.
Dynamic changes in blood platelet levels
prior to and following cerebral hemorrhaging
One day prior to cerebral hemorrhaging, the platelet
levels reduced in all patients to 29–78 × 109/l
(43.7±9.8 ×109/l on average). Following treatment, five
patients exhibited a progressive decrease in platelet levels and
succumbed. The other 11 cases recovered to an average platelet
level of 7.5±1.6 × 109/l.
Clinical treatment and results
Following admission, all patients received
conventional treatment, such as anti-infection, nutritional support
and the changing of burn dressings. Following the appearance of
symptoms of intracerebral hemorrhaging, various supporting
treatments were performed according to the bleeding situation, such
as reducing the cranial pressure by fluid restriction, hemostasis,
platelet injection, cryotherapy or enrichment with erythrocytes.
The final result was that five of the 16 patients succumbed and 11
recovered. No significant difference in intracerebral bleeding was
exhibited between the deceased and surviving groups. There was no
marked difference (t<1, P>0.05) in the volume of blood lost
between the deceased (21.8±15.3 ml) and the surviving groups
(19.1±13.01 ml). When the intracerebral bleeding occurred, the
platelet count for the deceased group (46.6±12.2 ×109/l)
and the survival group (43.3±13.1 ×109/l) also exhibited
no significant difference (t<1, P>0.05). The platelet count
gradually and steadily reduced in the deceased group following
intracerebral bleeding. By contrast, the platelet count increased
from the third day following intracerebral bleeding in the
surviving group, and within a week the levels had recovered to
normal (7.5±1.6 × 109/l).
Case reports
Case 1
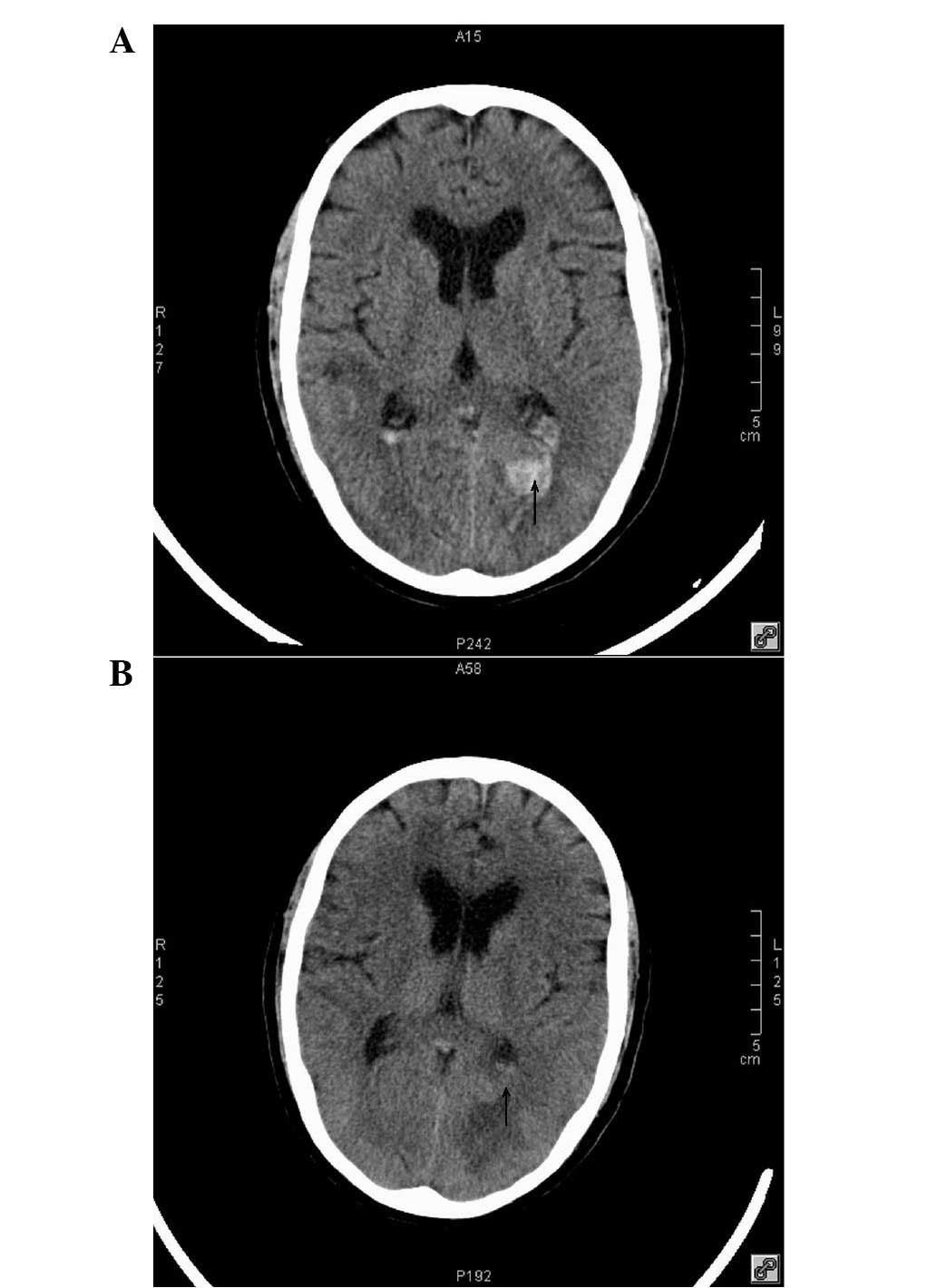
A 30-year-old male suffered complete body burns in a
boiler explosion. He was admitted to the hospital eight days later
and the diagnosis on admission was burns to 95% of the TBSA (3%
superficial second-degree burns, 77% deep second-degree burns and
15% third-degree burns) complicated with whole-body burn wound
sepsis. The patient had renal failure, anuria, an infection in both
lungs, heart failure and severe hypoxemia. The patient received
treatment with a ventilator, blood filtration, antibiotics,
nutritional support and dressing changes. On day 22 following
hospital admission, wound bleeding increased and airway and
gastrointestinal bleeding was observed. The platelet levels of the
patient were reduced to 41 ×109/l on day 24, giving an
activated partial thromboplastin time of 54.3 sec and a plasma
prothrombin time of 14.7 sec. The patient was in a light coma with
pupillary asymmetry (left pupil 2 mm, right 4 mm). CT revealed
multiple patchy areas of high density, particularly in the right
temporal lobe. The bleeding lesion was irregular and 2.5 ml in
size. There were no abnormalities in the ventricle and cistern.
Following symptomatic treatment and fiber bronchoscopy for airway
congestion, platelet injection, cryoprecipitation and packed
erythrocyte infusion, the patient began to recover on day 29, with
a platelet level of 112 ×109/l. On day 43, CT
reexamination revealed hematoma absorption (Fig 1). On day 50, the patient exhibited a
marked improvement and was transferred to a general ward. The
patient received multiple skin grafts and was discharged 3 months
later.
Case 2
A 54-year-old male, was admitted to hospital for a
cough and throat pain 23 days after receiving alkali burns to the
entire body. The diagnosis on admission was burns to 80% of the
TBSA (20% superficial second-degree burns, 30% deep second-degree
burns and 30% third-degree burns) complicated by burn wound sepsis
and lung infection. Hypoproteinemia, anemia and a severely low
platelet count were observed, the patient received wound dressings,
escharectomy, antibiotic treatment, packed erythrocyte infusion,
platelet injection and nutritional support. On day 12 following
admission, the patient complained of a severe headache and
dizziness, and his platelet level was found to be 38 ×
109/l. The CT revealed cerebral hemorrhaging in the left
occipital lobe, subarachnoid hemorrhaging and slight ventricular
hemorrhaging. On day 14, a place of bleeding in the right lower
limb appeared and CT revealed a new lesion in the right parietal
lobe, however, a lumbar puncture revealed that the cerebral spinal
fluid was normal. On day 16, the place of bleeding in the right
lower limb was aggravated and CT revealed a new lesion in the left
parietal lobe with an improvement to the subarachnoid and
ventricular hemorrhages. On day 18, the patient fell
unconsciousness with intermittent, paroxysmal, generalized tetanic
spasms. CT revealed no changes in the left parietal lobe
hemorrhage, but reductions in the right occipital lobe,
subarachnoid and ventricular hemorrhages were observed. The
platelet level was 108 ×109/l. On day 20 the patient
regained consciousness, presenting with first-degree muscle
strength in the right lower limb. On day 47, CT revealed a
significant improvement to the hemorrhage of the left occipital
lobe (Fig. 2). Further symptomatic
treatments, including wound dressing, antibiotics, decompression
and nutritional support, led to the patient being discharged three
months later.
Discussion
Burn injuries are often followed by a profound
hypermetabolic response that may last long after the injury was
initially sustained (5). The
hypermetabolic response is responsible for devastating muscle and
protein catabolism, insulin resistance and cardiac dysfunction that
may last for months and marked growth retardation which may impede
proper development (6). Patients
have supraphysiologic metabolic rates, multi-organ dysfunction and
increased levels of inflammatory cytokines and acute phase proteins
(7). This response may lead to
alterations in the consciousness of the burn patients.
Burn patients with sepsis are often mentioned in the
literature, but those with burns concurrent with intracranial
lesions are often neglected. Cho et al reported a study of
patients who had strokes following burns (8). Physical examination is challenging to
complete in burns patients. The observation of pupillary changes in
patients with facial burns is difficult, as the eyelids undergo
serious edema; furthermore, it is not easy to perform a
pathological and neurological examination of the facial wounds of a
burns patient as they are covered thickly with layers of scar
tissue.
Multiple ICHs are rare in severe burn patients and
the pathogenesis remains unclear. There have been reports that the
consumption of blood platelets, fibrinogen, plasmin and blood
coagulation factor by the burned tissue and the disseminated
intravascular coagulation (DIC) process may contribute to
intracerebral hemorrhaging (9).
Cho et al (8) hypothesized
that wound infection and sepsis are the main reasons for shock
following a burn. According to the cases we examined, intracranial
hemorrhaging occurred during the infection period of shock. All
patients had serious wound sepsis, with a low platelet count and
blood coagulation disorders prior to the intracerebral
hemorrhaging. Five patients (cases 12–16) succumbed; despite the
administration of a platelet infusion, their platelet counts had
been progressively decreasing. In the other 11 surviving cases, the
blood platelet count rose slowly following treatment with a
platelet infusion and blood filtration. Therefore, we believe that
the direct cause of multiple intracranial hemorrhaging in patients
with severe burns is a sharp decline in the platelet count and
blood coagulation disorders, and its indirect causes are systemic
sepsis and wound sepsis. As the patients were hospitalized in
hospitals with insufficient medical facilities, we consider that
the informal treatment and medication may be the cause of wound
infection and sepsis, indirectly leading to intracerebral
hemorrhaging.
Patients with a large burn area present with
thrombocytopenia and blood coagulation disorders easily. The rapid
consumption of platelets is a concern, but the main concerns in the
middle-late stage are serious infections and the direct absorption
of toxins leading to the rapid decline of platelet levels.
Inflammation is a defense mechanism against damaging
factors such as severe trauma and infection which may activate
blood coagulation leading to blood clotting and microcirculation
disorders and even organ dysfunction (8). However, the mechanism is complex and
the correlation between the two remains unclear (10). During an inflammatory reaction,
inflammation mediators are released which activate blood
coagulation and consume mass clotting factors through the
‘waterfall sample cascade’ which may lead to blood coagulation
disorders (11–13). In serious wounds, bacteria and
external toxins are absorbed into the bloodstream; in the current
study, Staphylococcus aureus was cultured from the surface
of the wound in six cases and from blood cultures in two cases .
This stimulates the release of a variety of inflammation mediators,
causing a marked increase in platelet adhesion and the clumping
together of platelets to form large numbers of tiny white
thrombuses in the circulation when blood coagulation increases. The
tiny blood clots cause a series of pathological physiology
reactions such as thrombocytopenia, a reduction in fibrinogen, an
increase in the activity of dissolved fibrinogen, serious bleeding
and coagulant function failure. Six cases exhibited level I
coagulant function failure the day prior to intracerebral
haemorrhaging, and two cases who succumbed had level II coagulant
function failure (14). When
coagulant function failure occurs in patients with serious burns,
it is preceded by gastrointestinal and skin mucous membrane
bleeding. Therefore, when platelets are being infused and the
filter is not capable of maintaining the platelet levels, there is
a risk of intracranial hemorrhaging.
In certain patients, the decision to conduct an
emergency CT examination was made due to the sudden onset of
clinical symptoms such as headache and hemiplegia. Diagnosis was
determined according to clinical manifestations such as an altered
mental state and a pupillary change, CT scans and laboratory data.
The majority of patients with burns appear to have a sudden
alteration to their mental state when their symptoms improve; when
symptoms such as severe headache, nausea and vomiting appear in
patients, this is a warning sign. Head CT examinations established
the amount of bleeding and whether the blood loss was stable; this
allowed us to decide whether to continue with a more conservative
treatment or to proceed with surgery according to the specific
circumstances of each patient. In CT imaging, shadowing due to
increased flake density (Fig. 1)
or focal density (Fig. 2) is
common.
In a previous study, we examined stroke diagnoses in
elderly burn patients (15). Burns
causing intracerebral hemorrhaging appear initially with the
bleeding of skin mucous membranes and gastrointestinal and internal
organs prior to intracerebral hemorrhaging; therefore we should pay
particular attention to severe wound bleeding, hematemesis or blood
in the stools. During the burn infection period, the platelet count
should be checked often as a sudden drop in the platelet level is a
useful diagnostic indicator of systemic infections. For simple
stroke patients, a marked reduction in the platelet levels and skin
mucous membrane and internal bleeding are not generally observed
prior to intracranial hemorrhaging.
For burn patients with intracranial hemorrhaging,
prevention is preferable to treatment, as the long-term use of
antibiotics may cause double fungal infections which may lead to
increased morbidity and mortality (16). In general, strategies to prevent
infection, such as early excision and grafting, aggressive
anti-microbial therapy, including the use of colistin, and early
enteral feedings improve the survival rate (17–18).
In the current study, two the of 16 cases underwent early
escharectomies, leading to a significant improvement in body and
wound infections. Treatment for intracranial hemorrhaging should be
initiated as soon as the diagnosis is confirmed, with platelet
infusions, hemostasis, decompression, blood filtration, antibiotics
and nutritional support. Key to successful treatment are
controlling the platelet levels via hemostasis, non-heparinized
blood filtration and effective anti-inflammatory treatment to
prevent platelets counts from dropping further.
The role of surgical treatment for these patients
requires further study. Conservative treatment is usually
recommended due to the fact that treating sporadic or multiple
hemorrhages with surgery is complex. We performed conservative
treatment in all sixteen cases, with success in eleven cases
(68.75% success rate). Large hemorrhages or unlimited bleeding
require surgery to clean the intracranial edema and reduce
intracranial pressure: for basal ganglia hemorrhage >30 ml,
surgery should be timely and a minimally invasive intraoperative
puncture hematoma or a small bone window to clear hematoma should
be selected; for cerebellar hemorrhage >10 ml or combined with
hydrocephalus, surgery may be considered; if the lobes are bleeding
then conservative treatment should be provided.
The incidence of particularly severe burns
accompanied by multiple intracranial hemorrhaging is not high. In
recent years, it has been rarely mentioned in the literature.
Although the patient survival rate for severe burns patients also
undergoing multiple intracranial hemorrhaging is low and treatment
costs are high, if the patients are provided with sufficient
attention and positive symptomatic treatment then there is a good
chance of a successful treatment.
Acknowledgements
This study was supported by the the
program for New Century Excellent Talents in University
(NCET-11-0527) and fundamental research funds for the central
universities (2011JQ028).
References
|
1.
|
Fu Y, Xie B, Ben D, et al: Pathogenic
alteration in severe burn wounds. Burns. 38:90–94. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2.
|
Kushner D: Mild traumatic brain injury:
toward understanding manifestations and treatment. Arch Intern Med.
158:1617–1624. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
3.
|
Zhu H, Li F, Zou M, et al: Experimental
high-altitude intracerebral hemorrhage in minipigs: histology,
behavior and itracranial pressure in a double-injection model. Acta
Neurochir (Wien). 155:655–661. 2013. View Article : Google Scholar
|
|
4.
|
Lee J, Evans CS, Singh N, et al: Head
computed tomography utilization and intracranial hemorrhage rates.
Emerg Radiol. Dec 19–2012.(Epub ahead of print).
|
|
5.
|
Hart DW, Wolf SE, Mlcak R, et al:
Persistence of muscle catabolism after severe burn. Surgery.
128:312–319. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
6.
|
Gauglitz GG, Herndon DN, Kulp GA, Meyer WJ
III and Jeschke MG: Abnormal insulin sensitivity persists up to
three years in pediatric patients post-burn. J Clin Endocrinol
Metab. 94:1656–1664. 2009.PubMed/NCBI
|
|
7.
|
Jeschke MG, Chinkes DL, Finnerty CC, et
al: Pathophysiologic response to severe burn injury. Ann Surg.
248:387–401. 2008.PubMed/NCBI
|
|
8.
|
Cho SJ, Minn YK and Kwon KH: Stroke after
burn. Cerebrovasc Dis. 24:261–263. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
9.
|
Winkelman MD and Galloway PG: Central
nervous system complications of thermal burns. A postmortem study
of 139 patients. Medicine (Baltimore). 71:271–283. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
10.
|
Huisse MG, Pease S, Hurtado-Nedelec M, et
al: Leukocyte activation: The link between inflammation and
coagulation during heatstroke. A study of patients during the 2003
heat wave in Paris. Crit Care Med. 36:2288–2295. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11.
|
Marshall JC: Inflammation, coagulopathy,
and the pathogenesis of multiple organ dysfunction syndrome. Crit
Care Med. 29:S99–S106. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
12.
|
Schouten M, Wiersinga WJ, Levi M and van
der Poll T: Inflammation, endothelium, and coagulation in sepsis. J
Leukoc Biol. 83:536–545. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13.
|
Pawlinski R, Pedersen B, Erlich J and
Mackman N: Role of tissue factor in haemostasis, thrombosis,
angiogenesis and inflammation: Lessons from low tissue factor mice.
Thromb Haemost. 92:444–450. 2004.PubMed/NCBI
|
|
14.
|
Cho SJ, Minn YK and Kwon KH: Stroke after
burn. Cerebrovasc Dis. 24:261–263. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15.
|
Xie HQ, Zhou JD, Nie XM, et al: HSP70
inhibits burn serum-induced apoptosis of cardiomyocytes via
mitochondrial and membrane death receptor pathways. J Burn Care
Res. 29:512–518. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16.
|
Murray CK, Loo FL, Hospenthal DR, et al:
Incidence of systemic fungal infection and related mortality
following severe burns. Burns. 34:1108–1112. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17.
|
Cox RA, Mlcak RP, Chinkes DL, et al: Upper
airway mucus deposition in lung tissue of burn trauma victims.
Shock. 29:356–361. 2008.PubMed/NCBI
|
|
18.
|
Rosanova M, Epelbaum C, Noman A, et al:
Use of colistin in a pediatric burn unit in Argentina. J Burn Care
Res. 30:612–615. 2009. View Article : Google Scholar : PubMed/NCBI
|