Introduction
Major surgery induces a high risk of postoperative
sepsis (1). With recent advances
in therapy in the medical and surgical fields, the postoperative
outcome has improved. Despite this progress, certain patients are
still at a high risk of infection, followed by morbidity and
mortality. Early markers of septic complications would be useful
for the diagnosis and therapeutic management of patients with
postoperative sepsis.
Cytokines are not only mediators of inflammation,
but also play an important role in the regulation of the immune
system. Reliable measurements of endogenous mediators, such as
tumor necrosis factor-α (TNF-α), interleukin-8 (IL-8) and
interleukin-10 (IL-10), have enabled us to clarify the pathway of
this inflammatory response, and thus are important in the clinical
setting (2).
TNF-α, a proinflammatory cytokine, is produced by
macrophages and monocytes. It is a potent activator of neutrophils
and endothelial cells, acting through two distinct TNF receptors.
IL-8, a proinflammatory cytokine released by cells, including
endothelial cells, monocytes and T cells, has been recognized as a
relevant activator of leukocytes, and is related to adult
respiratory distress syndrome (3).
IL-10 is a potent antiinflammatory cytokine that reduces neutrophil
adhesion to activated endothelial cells.
Acupuncture is a Chinese medicine treatment that
involves inserting needles into specific sites, known as acupoints,
on the body’s surface. The acupoints may be stimulated by different
methods, such as manual needling, the delivery of electrical
current or heat to the acupuncture needle, or by applying pressure
or laser-generated heat to the acupoint. Attenuation of the
inflammatory response reduces injury-induced immunosuppression and
is relevant to functional recovery (4).
The aim of our study was to observe the effect of
eletroacupuncture (EA) on cytokines and immune function and to
investigate whether point specificity was present in EA.
Materials and methods
Patient management
This study adopted a randomized, controlled trial
procedure, and 29 patients undergoing supratentorial craniotomy
were enrolled. The study protocol was approved by the Institutional
Review Board of Beijing Tiantan Hospital and written informed
consent was obtained from all patients. The patients were aged
between 18–60 years old, and the surgery had been assessed to be
grade 1–2 by the American Society of Anesthesiologists (ASA). The
following cases were excluded from this study: patients with
immune, renal or central nervous system dysfunction, patients with
congestive heart failure, exogenous hormone therapy (including
steroids), prior experience of acupuncture, pregnancy,
malnutrition, diabetes, malignancy, infection or inflammation.
No analgesics or tranquilizers were administered
prior to surgery. Once in surgery, the peripheral intravenous
infusion was initiated, and noninvasive blood pressure (NIBP),
heart rate (HR), oxygen pulse saturation (SpO2) and
bispectral index (BIS) were monitored. In group A, EA was applied
to Hegu (LI4), Waiguan (TE5), Jinme (BL63), Taichong (LR3), Zusanli
(ST36), Qiuxu (GB40), Tianzhu (BL10), Fengchi (GB20), Cuanzhu (BL2)
and Yuyao (EX-HN4) on the side with the craniotomy. The needles
were inserted to a depth of 0.75–1.5 cm at these acupoints. The
electroacupuncture stimulation (EAS) was delivered via a HANS
acupoint nerve stimulator (LH202H, Huawei Co., Ltd., Beijing,
China), with a disperse-dense wave, 2 Hz/100 Hz in frequency,
alternated once every 3 sec. The complete symmetric biphasic pulse
was adopted. The stimulation intensity was in accordance with the
maximal tolerance of patients and the EAS lasted from the induction
of anesthesia until the end of surgery.
Group C was a general anesthesia control group. In
this group, EA was not applied to patients, and other conditions
were the same as those of the other two groups.
Group S was a sham acupoints group. In this group,
EA was applied at 9 and 12 Cun above Kunlun (BL60), 7 and 10 Cun
above Taixi (KI3) and 7 and 9 Cun above Shenmen (HT7) on the side
with the craniotomy. The needles were inserted to a depth of
0.75–1.5 cm. EAS was delivered via a HANS acupoint nerve stimulator
(LH202H, Huawei Co., Ltd.), using a disperse-dense wave, 2 Hz/100
Hz in frequency, alternated once every 3 sec. The complete
symmetric biphasic pulse was adopted. The stimulation intensity was
in accordance with the maximal tolerance of patients and EAS lasted
from the induction of anesthesia until the end of surgery.
Target-controlled infusion (TCI) of
propofol and sufentanil
The induction plasma concentration of propofol was 5
μg/ml, and that of sufentanil was 0.5 ng/ml. While the patient was
unconscious, the plasma concentration of propofol was reduced to
3.2 μg/ml and that of sufentanil to 0.3 ng/ml, and vecuronium
bromide 0.1 mg/kg was administered at the same time. After muscle
relaxation, tracheal intubation was performed. Mechanical
ventilation with pure oxygen was applied, 10 ml/kg in tidal volume,
12 times/min in respiratory frequency and 1 l/min in oxygen flow.
Vecuronium bromide (0.05 mg/kg) was intermittently administered
performed to maintain muscle relaxation. Sufentanil concentration
was adjusted to maintain the mean arterial pressure (MAP) and HR in
the basic range of +10% to −20%. In cases of hypotension (MAP
<20% of baseline), bradycardia (HR <50 beats/min) or
hypertension (MAP >10% of baseline values), 6 mg ephedrine, 0.5
mg atropine or 0.2–0.5 mg nicardipine was administered,
respectively.
Sampling
Blood samples were obtained at the following time
points: before anesthesia (T0), 4 h after induction of anesthesia
(T1), 1 day after surgery (T2) and 2 days after surgery (T3) in
SST™II advance tubes (Becton Dickinson, Oxford, UK) for cytokine
and immunoglobin concentration testing.
Multiplex cytometric bead assay
A cytometric bead assay kit (Becton Dickinson) was
employed to measure levels of TNF-α, IL-8, IL-10, IgM, IgA, and IgG
in plasma according to the manufacturer’s instructions.
Statistical analysis
The department of epidemiology and hygienic
statistics of Capital Medical University was responsible for data
input and statistical analysis. SPSS 13.0 statistical software was
adopted. Results are expressed as the mean ± SD. Data were analyzed
using repeated-measures analysis of variance and separate effect
analysis. In the analysis, Mauchly’s test was used to judge whether
there were correlations between the repeatedly measured data. When
P<0.05, we used Greenhouse-Geisser to correct the results.
Differences were considered to be statistically significant at
P<0.05. There were significant differences between group C and
group A or group C and group S for the baseline value of IgA and
IgM, so we used the D-value to T0 to compare the differences among
the three groups at the other time points.
Results
General condition
The randomized controlled trial had 29 participants,
and no subject withdrew from the trial. Patient characteristics and
surgical data are provided in Table
I. There were no differences in the arterial blood pressure or
HR among the groups prior to, during or after EAS. There was no
surgical morbidity or mortality.
 | Table IPatient characteristics and surgical
data. |
Table I
Patient characteristics and surgical
data.
| Group C | Group A | Group S |
|---|
| Gender
(male/female) | 5/5 | 5/4 | 4/6 |
| Age (years) | 42±10 | 43±9 | 39±7 |
| Weight (kg) | 67±10 | 65±9 | 68±11 |
| Height (cm) | 165±11 | 67±23 | 163±17 |
| Duration of surgery
(min) | 253±43 | 241±49 | 233±51 |
| ASA class (I/II) | 8/2 | 7/2 | 7/3 |
| Tumor type
(glioma/meningioma/other tumors) | 4/4/2 | 4/3/2 | 4/4/2 |
Comparison within the groups
IL-10 levels in peripheral blood increased
significantly compared with those at T0 at 1 and 2 days after
surgery in groups A and S, and 4 h after the induction of
anesthesia and 1 day after surgery in group C. The IL-8 levels in
peripheral blood increased significantly compared with those at T0
at 1 and 2 days after surgery in groups A and S. The IgA levels in
peripheral blood decreased significantly compared with those at T0
at 4 h after the induction of anesthesia, and 1 and 2 days after
surgery in group C (Table
II).
 | Table IILevels of cytokines and
immunoglobulins following surgery. |
Table II
Levels of cytokines and
immunoglobulins following surgery.
| Group | Before
anesthesia | 4 h after induction
of anesthesia | 1 day after
surgery | 2 days after
surgery |
|---|
| TNF (pg/ml) | Group C | 1.51±0.41 | 1.71±0.16 | 1.61±0.22 | 1.4±0.38 |
| Group A | 2.53±0.43 | 2.82±0.16 | 3.09±0.24 | 3.82±0.4 |
| Group S | 3.44±0.41 | 2.75±0.16 | 3.15±0.22 | 2.99±0.38 |
| IL-10 (pg/ml) | Group C | 1.28±0.21 | 4.83±1.32a | 3.97±1.04a | 1.66±0.53 |
| Group A | 2.53±0.22 | 3.16±1.4 | 7.18±1.1a | 5.69±0.56a |
| Group S | 2.82±0.21 | 3.04±1.32 | 6.36±1.04a | 4.01±0.53a |
| IL-8 (pg/ml) | Group C | 11.45±5.67 | 10.9±1.67 | 17.48±46.61 | 12.36±60.33 |
| Group A | 8.96±6.52 | 16.73±1.76 | 111.52±49.14ab | 228.61±63.59ab |
| Group S | 38.08±15.67 | 13.54±1.67 | 119.18±46.61ab | 174.28±60.33ab |
| IgM (g/l) | Group C | 1.47±0.11 | 1.16±0.1 | 1.29±0.13 | 1.38±0.12 |
| Group A | 0.19±0.11 | 0.19±0.11 | 0.19±0.14 | 0.18±0.13 |
| Group S | 0.32±0.11 | 0.26±0.1 | 0.3±0.13 | 0.26±0.12 |
| IgA (g/l) | Group C | 4.16±0.41 | 2.77±0.37a | 2.89±0.35a | 3.25±0.31a |
| Group A | 0.61±0.43 | 0.64±0.39b | 0.65±0.37b | 0.63±0.32 |
| Group S | 1.05±0.41 | 0.88±0.37b | 0.98±0.35b | 0.71±0.31 |
| IgG (g/l) | Group C | 0.53±0.08 | 0.47±0.07 | 0.44±0.08 | 0.45±0.07 |
| Group A | 0.42±0.08 | 0.42±0.08 | 0.42±0.09 | 0.41±0.08 |
| Group S | 0.46±0.08 | 0.46±0.07 | 0.46±0.08 | 0.46±0.07 |
Comparisons among the three groups
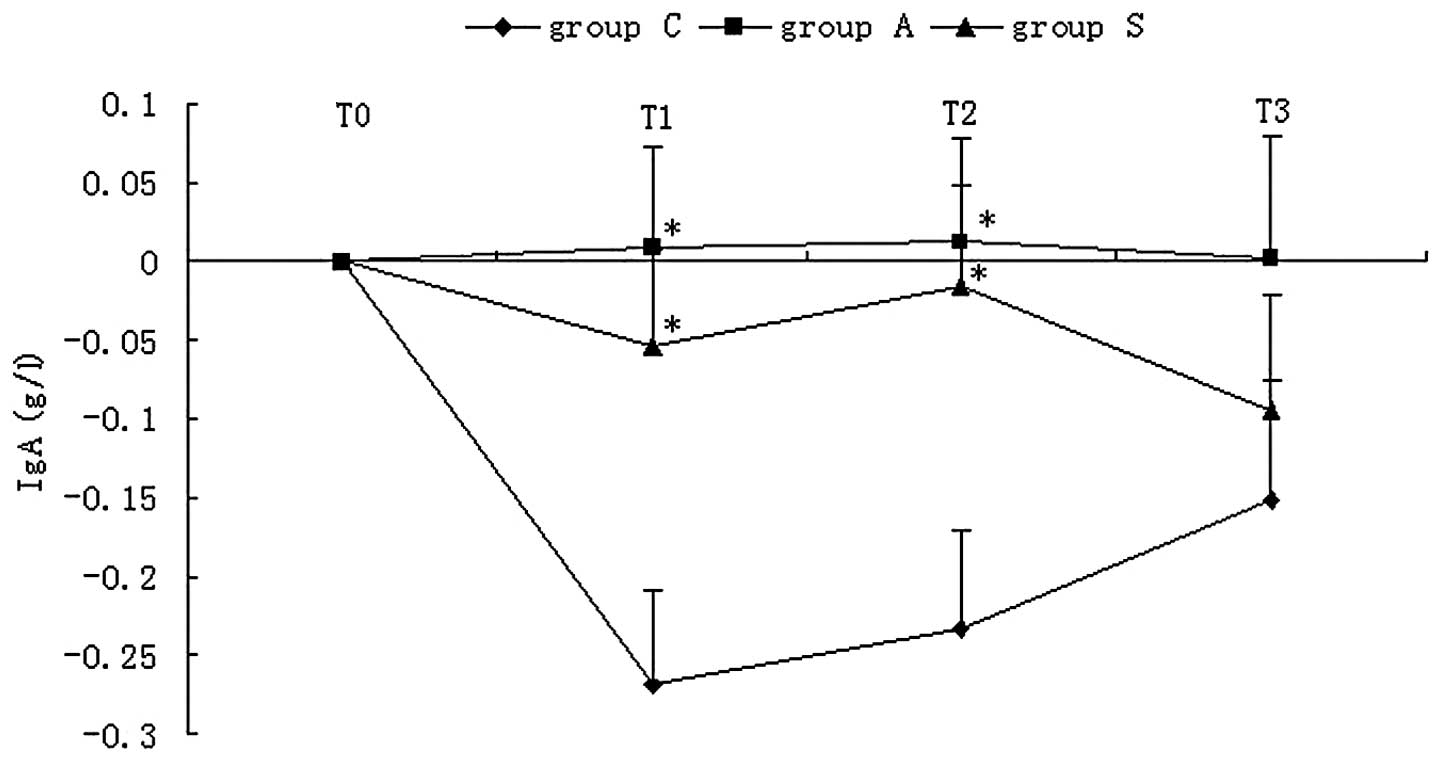
When comparing the levels of serum cytokines during
the craniotomy, we discovered that the peripheral blood IL-8 levels
in groups A and S increased significantly compared with that of
group C at 1 and 2 days after surgery (Table II). When comparing the levels of
serum immunoglobulin during the craniotomy, we observed that the
peripheral blood IgA levels in group C had decreased significantly
compared with those of groups A and S at 4 h after induction of
anesthesia and 1 day after surgery (Fig. 1).
Discussion
Surgery and the resultant stress response lead to a
suppression of immune function (5). The results of our study indicated
that EA improves the immune function suppressed by surgery. Our
study found that the peripheral blood IgA of patients in group C
decreased significantly compared with those of groups A and S 4 h
after the induction of anesthesia and 1 day after surgery. We also
noted that the IL-10 and IL-8 levels in peripheral blood were
increased significantly compared with those at T0 at 1 day and 2
days after surgery in groups A and S.
IgG may have a significant protective function
(6). IgG is important in bacterial
and viral defense; therefore, it may be advantageous in preventing
postoperative infection. A previous study reported that IgG was
modulated in obese women treated with EA compared with women
treated with placebo EA and restricted diet only (7); however, there was no observed
difference amongst the three groups in our study.
Another study investigated the application of EA in
70 volunteers, and observed changes in immunoglobulin levels in the
serum, saliva and gingival sulcus fluid (8). The results of the study showed that
30 min and 24 h after acupuncture treatment, saliva IgA levels were
significantly increased in volunteers whose IgA levels had
previously been low. When acupuncture was applied daily for 2
weeks, the study observed that saliva IgA levels were increased
significantly by ~20% compared with the baseline value. This is
similar to the results from our own study.
Kho et al observed 29 male patients during
and 6 days after upper abdominal surgery, and changes in IgA, IgM
and IgG levels in the peripheral blood were recorded. The surgery
was performed under two different anesthetic techniques (9): group 1 received acupuncture and small
doses of fentanyl and group 2 received moderate doses of fentanyl.
After surgery, the level of immunoglobulin decreased in the two
groups. IgA and IgG recovered by the sixth day after surgery in the
two groups, and IgM recovered by the fourth day. Acupuncture and
transcutaneous stimulation analgesia in patients undergoing major
abdominal surgery did not affect the immune system, which was
measured by the concentrations of immunoglobulin either during or
after surgery. In our study, we observed that peripheral blood IgA
of the patients in group C had decreased significantly compared
with those of groups A and S 4 h after the induction of anesthesia
and 1 day after surgery, which showed that EA in patients
undergoing supratentorial craniotomy may affect the immune system
as measured by the concentrations of immunoglobulins.
In a previous study, rats received EA at the Zusanli
(ST36) and Neiguan (PC6) acupoints, or electrical stimulation at
sham points, for 30 min prior to stimulation with either 5 mg/kg
LPS intravenously or normal saline (10). Plasma cytokines were assessed 240
min after either LPS or normal saline injection. The results
demonstrated that EA pretreatment significantly decreased
LPS-induced plasma TNF-α and IL-1β levels and increased the plasma
IL-10 level. The findings suggested that EA pretreatment at the
ST36 and PC6 acupoints attenuated the LPS-induced inflammatory
response. However, our study demonstrated that the IL-8 levels in
groups A and S were significantly increased when compared with that
of group C at 1 and 2 days after surgery. This showed that EA is
also an injury to the body as well as an advantage.
Numerous acupuncture studies use a sham acupoints
group as a control group, but it has been found that sham acupoints
have similar effects to those of true acupoints. Furthermore, the
results of pain-related studies have not supported the concept of
point specificity (11). However,
certain studies evaluating the response to stimulation of multiple
points on the body surface have shown that point-specific actions
are present. Therefore, the existence of point specificity in
acupuncture remains controversial. In our study, we observed that
there was no difference between groups A and S for IL-8 and IgA
levels, which confirms that point specificity in EA was not
present.
Our study indicated that EA, in addition to its
analgesic effects, prevented the decrease of immunoglobulin after
surgery. The study also suggested that the stimulation of
non-acupoints elicits effects similar to those of stimulation of
true acupoints. Further studies in this area are required in order
to detect the mechanisms. Acupuncture-drug combined anesthesia
should be used to partially improve immune suppression after
surgery.
Acknowledgements
This project was supported by the National Key Basic
Research Program; the program title was “Basic Research on Clinical
Acupuncture Analgesia” (2007CB512500). The title of the subprogram
was “Study on the Mechanism of Acupuncture Anesthesia for
Craniotomy” (2007 CB 512503).
References
|
1
|
Wan S and Yim A: Cytokines in myocardial
injury: impact on cardiac surgical approach. Eur J Cardiothoracic
Surg. 16(Suppl 1): S107–S111. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Giomarelli P, Scolletta S, Borrelli E and
Biagioli B: Myocardial and lung injury after cardiopulmonary
bypass: role of interleukin (IL)-10. Ann Thorac Surg. 76:117–123.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Patrick DA, Moore FA, Moore EE, Biffl WL,
Sauaia A and Barnett CC Jr: Jack A. Barney Resident Research Award
winner. The inflammatory profile of interleukin-6, interleukin-8,
and soluble intercellular adhesion molecule-1 in post-injury
multiple organ failure. Am J Surg. 172:425–431. 1996. View Article : Google Scholar
|
|
4
|
Hall GM, Peerbhoy D, Shenkin A, Parker CJ
and Salmon P: Relationship of the functional recovery after hip
arthroplasty to the neuroendocrine and inflammatory responses. Br J
Anaesth. 87:537–542. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yokoyama M, Itano Y, Mizobuchi S,
Nakatsuka H, Kaku R, Takashima T and Hirakawa M: The effects of
epidural block on the distribution of lymphocyte subsets and
natural-killer cell activity in patients with and without pain.
Anesth Analg. 92:463–469. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Brandtzaeg P: Structure, synthesis and
external transfer of mucosal immunoglobulins. Ann Immunol.
124:417–438. 1973.PubMed/NCBI
|
|
7
|
Cabioglu MT, Ergene N, Surucu HS, Çelik HH
and Findik D: Serum IgG, IgA, IgM, and IgE levels after
electroacupuncture and diet therapy in obese women. Am J Chin Med.
35:955–965. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Yang MM, Ng KK, Zeng HL and Kwok JSL:
Effect of acupuncture on immunoglobulins of serum, saliva and
gingival sulcus fluid. Am J Chin Med. 1:89–94. 1989. View Article : Google Scholar
|
|
9
|
Kho HG, Van Egmond, Eijk RJ and Kapteyns
WM: Lack of influence of acupuncture and transcutaneous stimulation
on the immunoglobulin levels and leucocyte counts following
upper-abdominal surgery. Eur J Anaesthesiol. 8:39–45.
1991.PubMed/NCBI
|
|
10
|
Gu G, Zhang Z, Wang G, Han F, Han L, Wang
K, Liu J and Li W: Effects of electroacupuncture pretreatment on
inflammatory response and acute kidney injury in endotoxaemic rats.
J Int Med Res. 39:1783–1797. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Choi EM, Jiang F and Longhurst JC: Point
specificity in acupuncture. Chinese Medicine. 7:42012. View Article : Google Scholar : PubMed/NCBI
|