Introduction
Renal ischemia and reperfusion injury (IRI) is a
common cause of renal failure and often occurs in surgeries such as
kidney transplantation, renal artery angioplasty, partial
nephrectomy, accidental or iatrogenic trauma, hydronephrosis and
elective urological surgery (1,2). In
kidney transplantation, renal IRI can lead to acute kidney injury
(AKI), which is a syndrome with an abrupt loss of renal function
(3). It is also a significant
contributor to graft tubular atrophy and interstitial fibrosis, the
main cause of graft loss occurring more than one year after
transplantation (4).
Renal fibrosis is the major pathological change that
drives kidney diseases to the end stage (5), and is characterized by
glomerulosclerosis, tubulointerstitial fibrosis and tubular atrophy
and dilation. In previous studies, transforming growth factor-β1
(TGF-β1) has been identified to play a key role in renal tubular
interstitial fibrosis (6,7). TGF-β1 may initiate the transition
from renal tubular epithelial cells to myofibroblasts, which is
also the cellular source for extracellular matrix (ECM) deposition
(8). Smad7, an intracellular
signaling mediator of TGF-β family members, plays a pivotal role in
TGF-β1 signal transduction (9). A
large number of in vitro and in vivo studies have
found that Smad7 antagonizes TGF-β1 by degrading activated receptor
complexes (10,11).
Ozone oxidative preconditioning (OzoneOP) is a novel
treatment to protect organs from IRI and is relatively simple and
harmless. A few studies (12,13),
including one from authors of the present study (14), have focused on the protective
phenomenon of OzoneOP against inflammation, apoptosis and oxidative
stress in rat models of IRI. However, to the best of our knowledge,
there have been no reports concerning the role of OzoneOP in renal
fibrosis following IRI. In the present study, the role of OzoneOP
in ischemia-induced renal fibrosis was investigated. Moreover, the
IRI-associated molecules α-smooth muscle actin (α-SMA),
transforming growth factor (TGF)-β1 and Smad7 were tested to
determine whether and how OzoneOP affected the renal fibrosis.
Materials and methods
Animal preparation
All adult male Sprague Dawley rats (220–250 g) were
from the Center of Experimental Animals in the Medical College of
Wuhan University (Wuhan, China). This project was approved by the
Committee on the Ethics of Animal Experiments of Wuhan University,
and the procedures were carried out according to routine animal
care standards. All experimental procedures complied with the
Guidelines for the Care and Use of Laboratory Animals (National
Academy Press, 1996). Briefly, rats were anesthetized with
pentobarbital (45 mg/kg) and placed on a homeothermic table in
order to maintain the core body temperature at 37°C. A midline
laparotomy was made and right nephrectomy was performed.
Subsequently, the left kidney was subjected to 45 min of ischemia
followed by reperfusion.
The animals were divided into sham-operated (Sham),
IRI and OzoneOP groups. Each group contained 8 rats. In the Sham
group, the surgery involved only removal of the right kidney. In
the IRI and OzoneOP groups, the left kidney vessels were clamped
for 45 min followed by reperfusion. In the OzoneOP group, prior to
surgery, the rats received 15 OzoneOP treatments by rectal
insufflation (1 mg/kg), once a day, as previously described
(11). The ozone concentration was
50 μg/ml. At 8 weeks after IRI, the left kidneys were removed for
analysis and blood samples were collected for the detection of
blood urea nitrogen (BUN) and creatinine (Cr) levels.
Preservation of kidneys
The left kidney was removed under fully maintained
anesthesia. After removal, the kidney was fixed in 10%
phosphate-buffered formalin or immediately frozen, and stored at
−80°C for following experiments.
Serum assays
At 8 weeks after the surgery in each group, 1-ml
blood samples were taken and assays were performed according to the
instructions of commercially available creatinine and urea assay
kits (Nanjing Jiancheng Bioengineering Research Institute, Nanjing,
China). The absorbance was measured by spectrophotometry using a
Shimadzu UV-1700 spectrophotometer (Kyoto, Japan; absorbance
measured at 510 and 640 nm for the creatinine and urea assay kits,
respectively) and the concentrations of BUN and Cr were
calculated.
Masson’s trichrome staining
Following fixation of the kidney in 10%
phosphate-buffered formalin, it was embedded with paraffin and cut
into 5-μm sections. The sections were deparaffinized and hydrated
gradually, and stained with Masson’s trichrome. Morphologic
assessments were observed by an experienced renal pathologist who
was unaware of the groups and treatments.
Immunohistochemistry
The expression of α-SMA was conducted by
immunohistochemical staining. Briefly, 5-μm sections were
deparaffinized, and endogenous peroxidase activity was blocked with
3% hydrogen peroxide at 37°C for 10 min. Then, the sections were
treated with 10% normal goat serum (Boster Biological Technology,
Ltd., Wuhan, China) in Tris-buffered saline (TBS) for 30 min at
37°C. Subsequently, they were incubated overnight at 4°C with a
rabbit polyclonal to α smooth muscle actin antibody (α-SMA;
dilution at 1:100 for immunohistochemistry; ab5694; Abcam,
Cambridge, MA, USA). After washing three times with
phosphate-buffered saline (PBS), these sections were incubated with
the secondary antibody (ZSGB-BIO Co., Beijing, China) for 30 min at
room temperature, followed by color reagent 3,3′-diaminobenzidine
(DAB). For the negative control group, the procedures were
performed with the exception of the addition of the primary
antibody.
Reverse transcription quantitative
polymerase chain reaction (RT-qPCR)
Total RNA was isolated using TRIzol reagent
(Invitrogen Life Technologies, Carlsbad, CA, USA) and the RNA
concentration was determined spectrophotometrically.
Single-stranded cDNA was synthesized using the cDNA synthesis kit
(Takara Bio Inc., Kyoto, Japan) according to the manufacturer’s
instructions. RT-qPCR was performed with the Platinum®
SYBR® Green qPCR SuperMix-UDG kit (Applied Biosystems,
Foster City, CA, USA). The primers used were as follows: α-SMA
forward, 5′-CAACCCCTATACAACCATCACAC-3′, and α-SMA reverse,
5′-CCCAAACTGCTTGCGTAACC-3′ (GenBank accession number NM_031005);
TGF-β1 forward, 5′-CTTTAGGAAGGACCTGGGTTG-3′, and TGF-β1 reverse
5′-GGTTGTGTTGGTTGTAGAGGG-3′ (GenBank accession number NM_021578);
Smad7 forward, 5′-GGCTTTCAGATTCCCAACTTC-3′, and Smad7 reverse,
5′-CGCCATCCACTTCCCTTGT-3′ (GenBank accession number NM_030858).
β-actin was used as a housekeeping gene. The data were presented as
a ratio of the gene to β-actin mRNA (sense:
5′-TGCTATGTTGCCCTAGACTTCG-3′ and antisense:
5′-GTTGGCATAGAGGTCTTTACGG-3′; GenBank accession number NM_031144).
The initial activation was at 95°C for 15 sec followed by 58°C for
20 sec and 72°C for 20 sec, cycling 40 times. The SLAN-96S
Real-Time PCR system (Shanghai Hongshi Medical Technology Co., Ltd,
Shanghai, China) was used. Three samples were used per assay.
Western blot
Total proteins were extracted, using RIPA buffer and
a protease inhibitor, and quantified using the bicinchoninic acid
method. Then, equivalent weights of protein (40 μg/lane) were
separated on 10% SDS-PAGE gels and transferred to a nitrocellulose
membrane. The membranes were blocked with 5% non-fat milk in
Tris-buffered saline and Tween 20 (TBST) buffer and then incubated
with the following rabbit anti-rat polyclonal primary antibodies:
α-SMA (1:1,000 dilution; Abcam; ab5694), TGF-β1 (1:1,000 dilution;
Santa Cruz Biotechnology, Inc.; sc146) and Smad7 (1:1,000 dilution;
Santa Cruz Biotechnology, Inc.; sc11392). Subsequently, after
washing twice with PBS, the membranes were incubated with secondary
antibody (ZSGB-BIO Co.) conjugated with horseradish peroxidase at
1:2,000 dilution. Specific bands were visualized using an Immobilon
Western Chemiluminescent HRP Substrate kit (Millipore, Darmstadt,
Germany).
Statistical analysis
Data were presented as the mean ± standard error of
the mean. The means of the different groups were compared using
one-way analysis of variance (ANOVA) and Student-Newman-Keuls
tests. Differences were considered statistically significant when
P<0.05.
Results
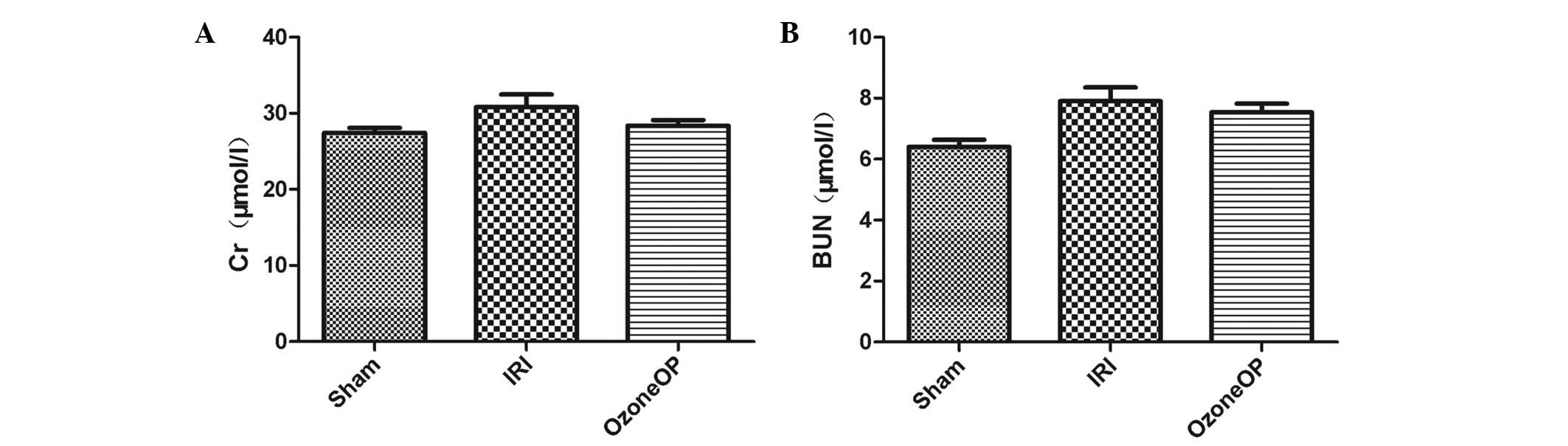
Long-term renal function outcomes
BUN and Cr levels were measured at 8 weeks following
IRI in rats that were treated with OzoneOP or were untreated. In
the IRI model, renal function was not altered significantly from
that in the Sham group and the preconditioning treatment with ozone
did not change these results (Fig.
1).
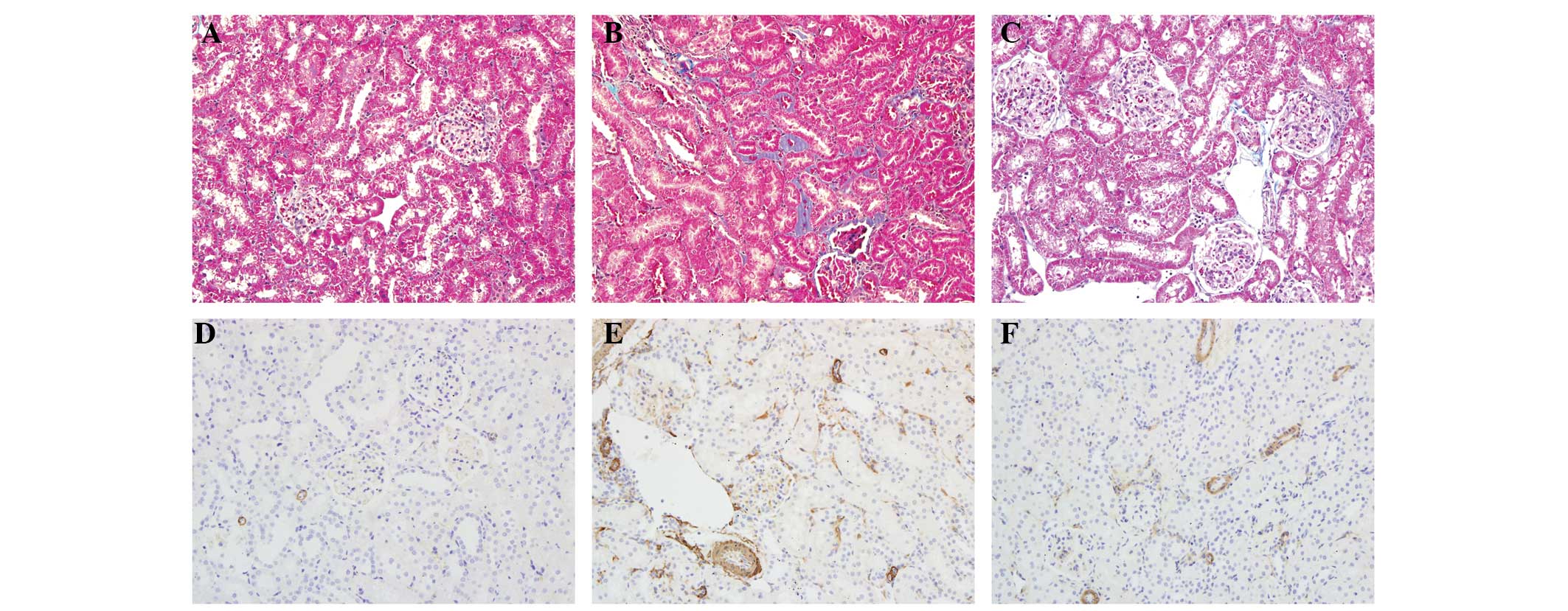
Morphologic features
Morphologic features were evaluated using Masson’s
trichrome staining (Fig. 2A–C). In
the Sham group, it revealed little deposition of collagen in the
renal cortical tissue sections; however, a significant increase in
tubulointerstitial collagen deposition was observed in rats
subjected to IRI. In the OzoneOP group, an increase in collagen
staining compared with that in the Sham group was observed;
however, the staining was less than that observed in the IRI
group.
Localization of the expression of
α-SMA
The localization of α-SMA was observed by
immunohistochemistry. Staining revealed that α-SMA was rarely found
in the Sham group. However, in the IRI group, renal tissues were
strongly positive for α-SMA expression, which was mainly localized
in the injured renal tubular epithelial cells, tubulointerstitium
and vascular smooth muscle. The α-SMA expression in the OzoneOP
group was reduced compared with that in the IRI group (Fig. 2D–F).
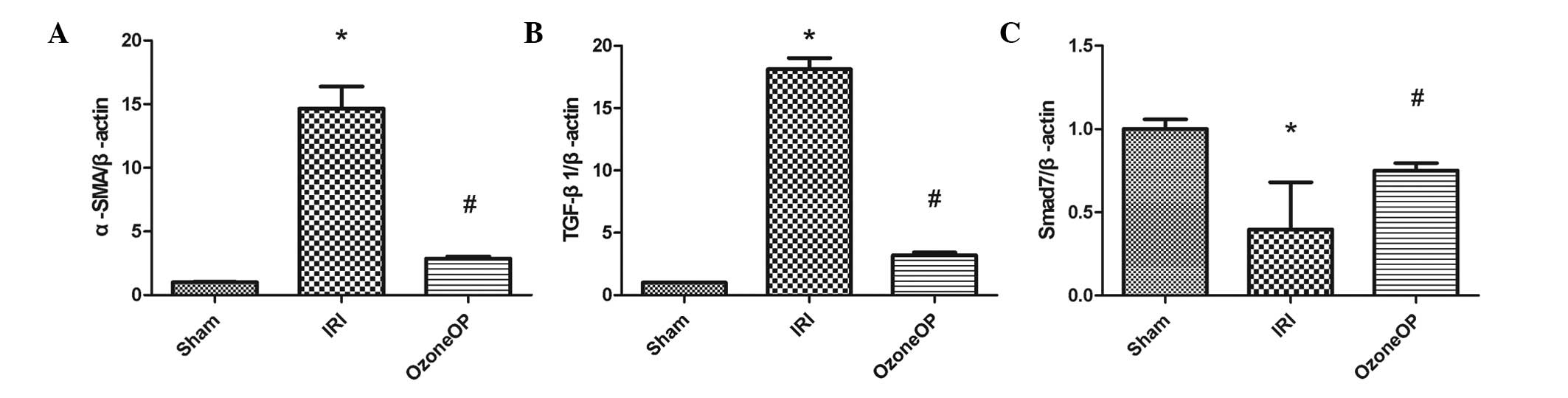
RT-qPCR analysis
To investigate the mRNA levels of α-SMA, TGF-β1 and
Smad7, RT-qPCR analyses were conducted. The expression levels of
α-SMA, TGF-β1 and Smad7 relative to β-actin were determined. The
mRNA levels of α-SMA and TGF-β1 were significantly greater in the
IRI group than in the Sham group. However, OzoneOP treatment
inhibited their expression following renal IRI. The mRNA level of
Smad7 was reduced in rats subjected to IRI compared with that in
the Sham group, and OzoneOP attenuated the reduction (Fig. 3).
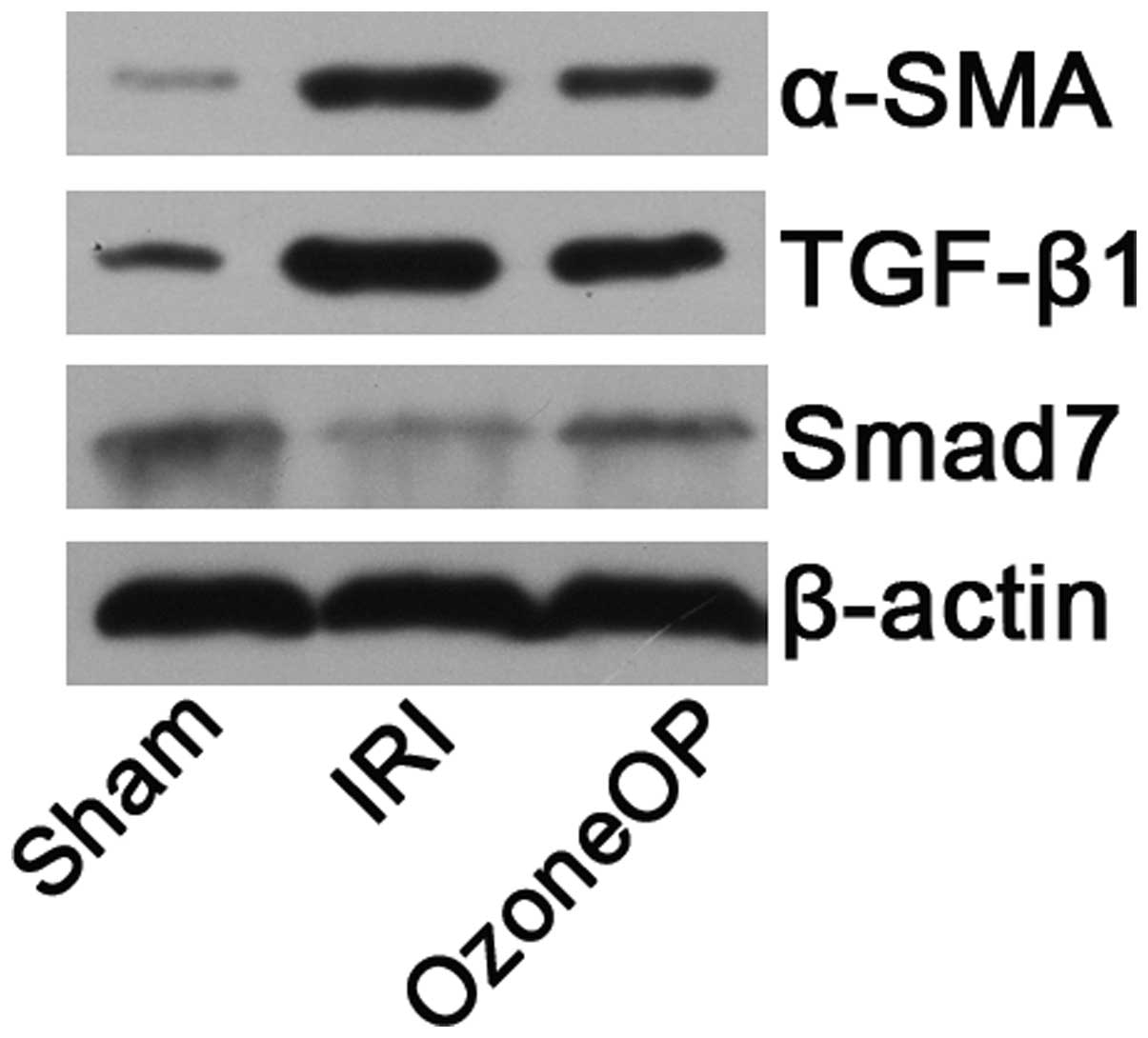
Western blot analysis
The results of western blot corroborated the RT-qPCR
findings. The expression levels of α-SMA and TGF-β1 were
upregulated in the IRI and OzoneOP groups when compared with those
in the Sham group. However, OzoneOP attenuate the expression
induced by IRI. Smad7 expression was downregulated in rats
subjected to IRI compared with that in the Sham group. However, in
the OzoneOP group, the expression level of Smad7 was clearly
greater than that observed in the IRI group (Fig. 4).
Discussion
Ozone has been investigated as a novel treatment for
a number of diseases (15,16). In one study, it was demonstrated
that ozone had protective anti-apoptosis and anti-inflammatory
effects in an animal model of organ IRI (14). Ozone may be used therapeutically to
protect organs from IRI and is relatively simple and harmless. It
has also been shown to improve the functioning of organs subjected
to IRI by inducing them to adapt to slight and transient oxidative
stresses, resulting in improvements of endogenous antioxidant
systems (17).
IRI is of significant interest to researchers due to
its impact on such organs as the kidney, liver and heart. It is the
leading antigen-independent factor contributing to the development
of chronic allograft loss, which is the foremost cause of graft
loss occurring more than one year after kidney transplantation
(18). In addition, it is also a
crucial contributor to renal fibrosis, which is characterized by
glomerulosclerosis, rarefaction of the glomerular and peritubular
capillaries, and tubulointerstitial fibrosis (19). The long-term inflammation elicited
by IRI can result in fibrosis. Therefore, it is essential to find
alternative strategies to counteract the development of fibrotic
tissue. In a previous study, we demonstrated that OzoneOP has renal
protective effects associated with its anti-apoptosis and
anti-inflammatory properties (14). In the present study, the aim was to
investigate whether OzoneOP could have a beneficial effect in
preventing the development of renal fibrosis following IRI and to
elucidate the underlying mechanism.
Prior to 45 min of ischemia, certain rats received
15 ozone preconditioning treatments by rectal insufflation, and
subsequently, they underwent reperfusion for up to 8 weeks.
Although renal function showed no significant differences among all
groups, the results of Masson’s trichrome staining showed that IRI
induced a significant increase in tubulointerstitial collagen
deposition in rats subjected to IRI. However, this pathologic
finding of renal fibrosis was significantly ameliorated by OzoneOP.
In addition, previous studies have confirmed that OzoneOP is able
to reduce the short-term inflammatory response following organ IRI
(12,14). In the current study, observation of
Masson’s trichrome staining revealed extensive inflammatory cell
infiltration in the IRI group. However, inflammatory cells were
sparsely distributed in the OzoneOP group. These results indicate
that OzoneOP suppresses long-term inflammation and thereby
attenuates the development of renal fibrosis.
TGF-β1 has been demonstrated to be not only a
multipurpose cytokine but also a crucial inducer of renal fibrosis
(20). It increases ECM deposition
by enhancing the synthesis of ECM proteins and inducing the
protease inhibitors blocking their degradation (21). Using animal models, increased
expression of TGF-β1 has been found to be universal in various
kinds of chronic kidney disease. The results of in vitro
studies are also in accordance with those of in vivo
studies. TGF-β1 may induce interstitial fibroblasts and tubular
epithelial cells to undergo epithelial-to-mesenchymal transition
(EMT) to become matrix-producing fibrogenic cells. The expression
of α-SMA parallels that of TGF-β1. α-SMA is often expressed during
EMT and it has been viewed as a marker of ‘activated’ fibroblasts.
As mediators of TGF-β1 family members, Smad proteins are important
molecules in its signal transduction pathway (22,23).
In the present study, it was found that the expression of TGF-β1
and α-SMA was upregulated in the IRI and OzoneOP groups due to IRI;
however, the changes induced by IRI were attenuated significantly
in the OzoneOP group. Furthermore, the expression of Smad7 in the
IRI group showed a significant reduction when compared with that in
the Sham group, and OzoneOP markedly inhibited this reduction. This
indicates that OzoneOP affects the expression of TGF-β1/Smad7 and
thereby exerts protective effects against the renal fibrosis
induced by IRI.
To the best of our knowledge, the present study is
the first to demonstrate that OzoneOP is able to protect the
ischemic kidney against renal fibrosis. This protective effect may
be achieved via modulation of the TGF-β1/Smad7 pathway. Therefore,
these findings reveal the potential role of ozone as a novel
therapeutic option against ischemic renal fibrosis.
Acknowledgements
This study was supported in part by the National
Natural Science Foundation of China (Grant No. 30901494) and
Natural Science Foundation of Hubei Province (Grant No.
2013CFB226).
References
|
1
|
Yun Y, Duan WG, Chen P, et al: Ischemic
postconditioning modified renal oxidative stress and lipid
peroxidation caused by ischemic reperfusion injury in rats.
Transplant Proc. 41:3597–3602. 2009. View Article : Google Scholar
|
|
2
|
Barri YM, Sanchez EQ, Jennings LW, et al:
Acute kidney injury following liver transplantation: definition and
outcome. Liver Transpl. 15:475–483. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Schrier RW, Wang W, Poole B and Mitra A:
Acute renal failure: definitions, diagnosis, pathogenesis, and
therapy. J Clin Invest. 114:5–14. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Nankivell BJ, Borrows RJ, Fung CL, et al:
The natural history of chronic allograft nephropathy. N Engl J Med.
349:2326–2333. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Cook HT: The origin of renal fibroblasts
and progression of kidney disease. Am J Pathol. 176:22–24. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Li R, Chung AC, Dong Y, et al: The
microRNA miR-433 promotes renal fibrosis by amplifying the
TGF-β/Smad3-Azin1 pathway. Kidney Int. 84:1129–1244.
2013.PubMed/NCBI
|
|
7
|
Ni H, Chen J, Pan M, et al: FTY720
prevents progression of renal fibrosis by inhibiting renal
microvasculature endothelial dysfunction in a rat model of chronic
kidney disease. J Mol Histol. 44:693–703. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Zeisberg M, Maeshima Y, Mosterman B and
Kalluri R: Renal fibrosis. Extracellular matrix microenvironment
regulates migratory behavior of activated tubular epithelial cells.
Am J Pathol. 160:2001–2008. 2002.
|
|
9
|
Zhang X, Yang J, Li Y and Liu Y: Both Sp1
and Smad participate in mediating TGF-beta1-induced HGF receptor
expression in renal epithelial cells. Am J Physiol Renal Physiol.
288:F16–F26. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nakao A, Afrakhte M, Morén A, et al:
Identification of Smad7, a TGFbeta-inducible antagonist of TGF-beta
signalling. Nature. 389:631–635. 1997. View
Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ren ZP, Sun LP, Xia YC and Tong QX: Effect
of the protease inhibitor MG132 on the transforming growth
factor-β/Smad signaling pathway in HSC-T6 cells. J Huazhong Univ
Sci Technolog Med Sci. 33:501–504. 2013.
|
|
12
|
Ajamieh HH, Menendez S, Martinez-Sanchez
G, et al: Effects of ozone oxidative preconditioning on nitric
oxide generation and cellular redox balance in a rat model of
hepatic ischaemia-reperfusion. Liver Int. 24:55–62. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ajamieh HH, Berlanga J, Merino N, et al:
Role of protein synthesis in the protection conferred by
ozone-oxidative-preconditioning in hepatic ischaemia/reperfusion.
Transpl Int. 18:604–612. 2005. View Article : Google Scholar
|
|
14
|
Chen H, Xing B, Liu X, et al: Ozone
oxidative preconditioning inhibits inflammation and apoptosis in a
rat model of renal ischemia/reperfusion injury. Eur J Pharmacol.
581:306–314. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Martinez-Sanchez G, Al-Dalain SM, Menendez
S, et al: Therapeutic efficacy of ozone in patients with diabetic
foot. Eur J Pharmacol. 523:151–161. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
León Fernández OS, Pantoja M, Díaz Soto
MT, et al: Ozone oxidative post-conditioning reduces oxidative
protein damage in patients with disc hernia. Neurol Res. 34:59–67.
2012.PubMed/NCBI
|
|
17
|
Leon OS, Menendez S, Merino N, et al:
Ozone oxidative preconditioning: a protection against cellular
damage by free radicals. Mediators Inflamm. 7:289–294. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Feitoza CQ, Goncalves GM, Semedo P, et al:
Inhibition of COX 1 and 2 prior to renal ischemia/reperfusion
injury decreases the development of fibrosis. Mol Med. 14:724–730.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Weng X, Shen H, Kuang Y, et al: Ischemic
postconditioning inhibits the renal fibrosis induced by
ischemia-reperfusion injury in rats. Urology. 80:481–484. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Liu Y: Renal fibrosis: new insights into
the pathogenesis and therapeutics. Kidney Int. 69:213–217. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Border WA and Noble NA: TGF-beta in kidney
fibrosis: a target for gene therapy. Kidney Int. 51:1388–1396.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kellenberger T, Krag S, Danielsen CC, et
al: Differential effects of Smad3 targeting in a murine model of
chronic kidney disease. Physiol Rep Dec. 1:e001812013.PubMed/NCBI
|
|
23
|
Wang Y1, Zhang Z, Shen H, Lu Y, Li H, Ren
X and Wu G: TGF-beta1/Smad7 signaling stimulates renal
tubulointerstitial fibrosis induced by AAI. J Recept Signal
Transduct Res. 28:413–428. 2008. View Article : Google Scholar : PubMed/NCBI
|