Introduction
As a surgical method to preserve the bladder,
partial cystectomy can be used to achieve full-thickness resection
of the bladder wall and complete resection of bladder lesions, in
addition to ensuring adequate margins. In the 1950s, partial
cystectomy became widely used to treat muscle-invasive bladder
cancer (MIBC); however, due to its high recurrence rate (40–78%),
together with the development of controllable urinary diversion
technology and the application of total cystectomy with
preservation of nerves and prostate, radical cystectomy has become
the ‘gold standard’ for the treatment of MIBC (1–3).
However, study results from a 30-year period indicate that the
postoperative 5-year survival rate of radical cystectomy is only
40–60% (4). In addition, due to the
high perioperative mortality rate (1.5–4.2%) and incidence of
complications (67%) (5,6), which seriously affect the quality of
life following urinary diversion and damage the sexual function of
male patients after surgery, the ‘gold standard’ status for radical
cystectomy has been challenged.
A study (7) has shown
that ~50% of MIBC has dominant or occult local or distant
metastasis at the first diagnosis. For these patients whose
prognoses cannot be significantly improved by modified surgical
methods alone, combined treatment with radiotherapy and
chemotherapy is a useful complement to surgery. Therefore,
treatment with bladder preservation is likely to achieve similar
long-term efficacy to that of radical cystectomy and a higher
quality of life (8).
In 2008, Mak et al (9) indicated that the most common treatment
methods with bladder preservation included ‘thorough’ transurethral
resection of bladder tumor (TURBt), systemic chemotherapy (adjuvant
or neoadjuvant chemotherapy) and radiotherapy. However, traditional
TURBt has a blind zone and other deficiencies, such as the
incapability to access tumors in particular areas, and is a
challenging technique for the surgeon to master. Therefore, the
clearance of localized tumors in MIBC is <20% for TURBt alone,
and phase T3 tumors are rarely resected completely by TURBt
(10). Residual tumor and
pathological downstaging following TURBt is not uncommon (11). For patients with invasive bladder
cancer, TURBT alone can at most only reduce tumor burden, and
alleviate symptoms such as frequent urination, urgency with
urination and bloody urine; and ~50% of patients have distant
metastases postoperatively (6).
By contrast, partial cystectomy enables complete
resection of the full thickness of the lesion and ensures adequate
safety margins, with a low incidence of residual tumor. In
addition, the surgical procedure of partial cystectomy is
relatively simple. However, the traditional open partial cystectomy
surgery has several deficiencies such as high surgical risk, large
trauma, long postoperative recovery and an evident postoperative
scar. Laparoscopic surgery techniques have been developed since the
early 1990s, offering the possibility for the reduction of
complications in open surgery; with the unremitting effort of
clinicians, laparoscopic surgery has been developed from the
classic four-incision surgery (12)
to three-incision surgery (13) and
two-incision surgery (14), and
ultimately single-port surgery has successfully been achieved.
For single-port laparoscopic surgery, natural
orifice transumbilical surgery (NOTUS) is the most mature surgical
method. The incision of NOTUS is located in the umbilical region
where the incision is covered by the skin fold; therefore,
satisfactory cosmetic results can be achieved. Furthermore, NOTUS
has other advantages, including an absence of scarring, a superior
cosmetic effect, less postoperative pain, rapid recovery and a
lower incidence of trocar site hernia and infection. At present,
the range of single-port laparoscopic surgery encompasses kidney
cryotherapy, kidney biopsy, radical nephrectomy, single-port
transumbilical nephrectomy for living kidney transplantation
donors, sleeve gastrectomy, gastric banding surgery, right
hemicolectomy and other difficult surgeries (15–19).
Therefore, based on familiarity with single-port
laparoscopic renal cyst decompression and adrenalectomy, the
present authors attempted to apply the single-port laparoscopic
technique to partial cystectomy and the results obtained are
reported in the present study.
Materials and methods
Patient data
The study population included 30 patients who
underwent surgical treatment due to bladder cancer while admitted
to the Affiliated Hospital of the Academy of Military Medical
Sciences (Beijing, China) between June 2011 and July 2013 were
included in this study. The selected patients were diagnosed with
bladder cancer with total cystectomy indications. The patients
themselves and their families had expressly rejected total
cystectomy.
The 30 patients included 18 males and 12 female
patients, with a mean age of 63.6 years (range, 45–81 years). The
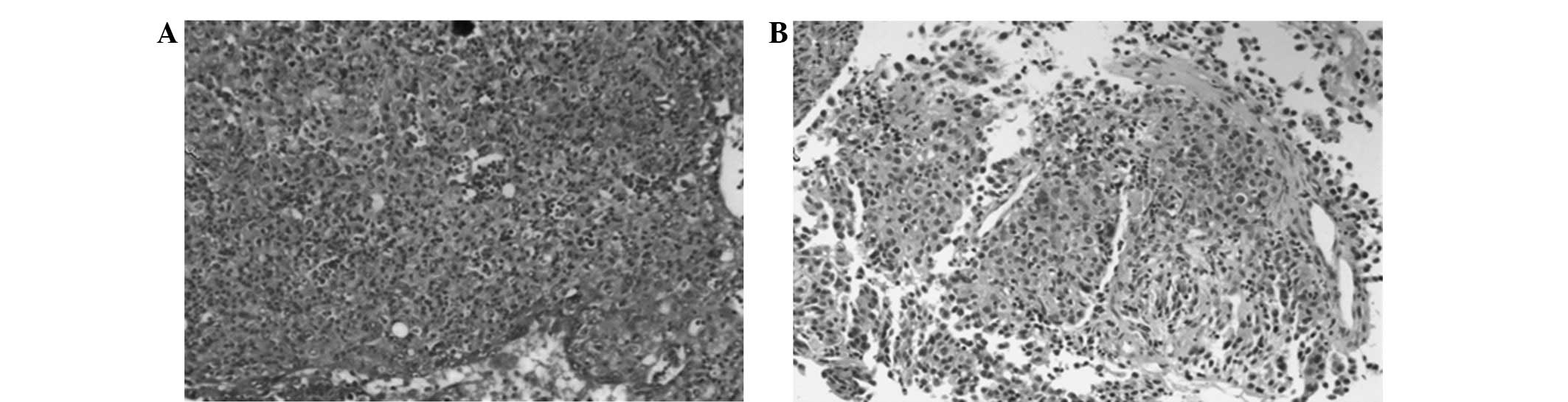
tumor stages were T2 in 11 cases and T3a in 19 cases. All patients
were confirmed by preoperative cystoscopy biopsy as having
high-grade invasive bladder cancer, with pathological grades of II
(16 cases) or III (14 cases; Fig.
1). The number of tumor lesions was 1–4, with a maximum tumor
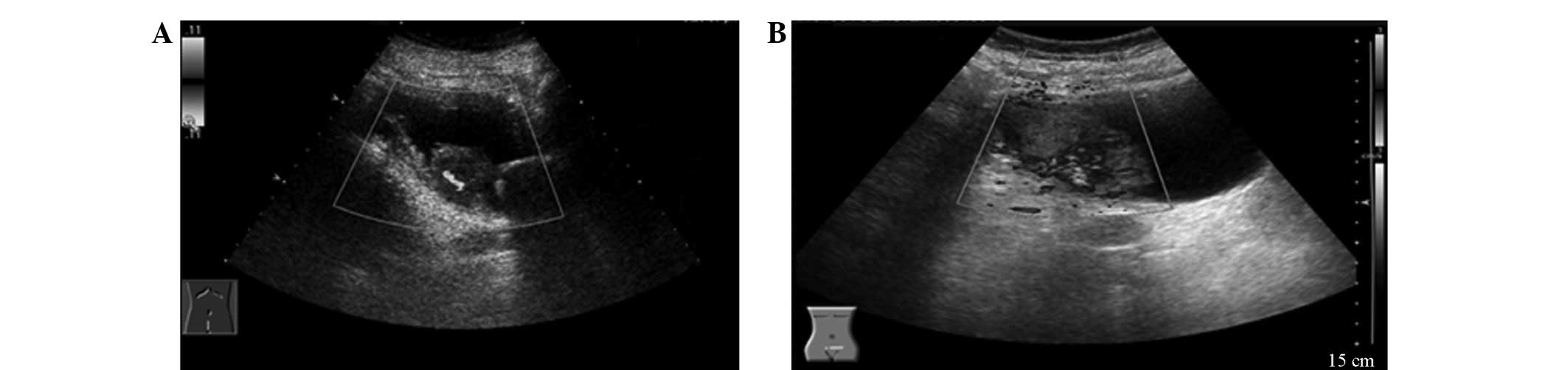
diameter of 4.5 cm. Systemic metastases were excluded by routine
chest radiograph, abdominal B-ultrasound, pelvic computed
tomography (CT) scan and whole body bone emission CT scan (Fig. 2). The patients all underwent
sequential therapy with bladder preservation.
The included patients were randomly divided into two
groups, and were randomized by random numbers assigned by computer.
This study was conducted in accordance with the Declaration of
Helsinki. This study was conducted with approval from the Ethics
Committee of the Academy of Military Medical Sciences (Beijing,
China). Written informed consent was obtained from all
participants.
Single-port laparoscopic partial
cystectomy
The surgical instruments used included TriPort
(Olympus Corporation, Tokyo, Japan), an ultrasonic scalpel, 10-mm
30° laparoscope, 2-mm spring grasping forceps, needle holders,
curved electrocautery hook, 5-mm straight scissors and 5-mm washer
(Karl Storz GmbH & Co. KG, Tuttlingen Germany). The patient was
laid in a supine lithotomy position with the head at 30°, and the
location and size of the tumor was determined by cystoscopy, when
the operator stood at the patient's cephalic position and the
assistant stood at the contralateral position to the operator to
hold the cystoscope. When placing the single-port multi-channel
kit, a longitudinal skin incision was made 2 cm below the belly
button, and the skin fold was incised. The peritoneum was pushed
upward to expose the top of bladder. Under the surveillance of the
cystoscope and with maintenance of bladder filling, the top wall of
bladder was punctured and the single-port multi-channel kit was put
in place following positioning by fine needle puncture. The
cystoscope was then withdrawn, and an independent intake passage
was connected to a pneumoperitoneum apparatus (KARL STORZ Endoscopy
[Shanghai] Ltd., Beijing, China) to establish a gas-filled bladder
space with a pressure of 12–15 mmHg. The locations and sizes of
tumors in the bladder were observed after filling the bladder, and
the tumors were incised completely at about a distance of 1–2 cm
from the tumor basal margin up to the muscular layer of the bladder
using the electrocautery hook and ultrasonic scalpel. The bladder
incision was sutured using 2.0 absorbable suture lines if
necessary, and the surgical specimens were placed in specimen bags.
Following the surgery, the surgical wound and incision were soaked
and rinsed thoroughly with distilled water, and the bladder and
abdominal incision were closed layer by layer. An indwelling
urinary catheter was used for continuous bladder irrigation.
Open partial cystectomy
The patient was laid in a supine position, and a
central incision was made below the umbilicus with a length of ~15
cm. The skin, subcutaneous tissue and muscle layer were incised
layer by layer, and the peritoneum was bluntly dissected to expose
the bladder. The tissue surrounding the bladder was separated by a
combination of blunt and sharp dissection combined and the bladder
was incised. The tumors in the bladder were located and completely
resected at a distance of ~1 cm around the tumor. The excised
specimens were sent for pathological examination. The surgical
wound was rinsed with distilled water and saline, and an indwelling
urinary catheter was inserted. The bladder incision was
continuously sutured using 2.0 absorbable suture lines and embedded
using No. 1 silk after confirming that there was no active
hemorrhage in the bladder. An indwelling silicone drainage tube was
inserted beside the incision following the confirmation that there
was no urine leakage or hemorrhage, and the incision was closed
layer by layer.
Chemotherapy regimen
The systemic chemotherapy regimen (cisplatin plus
gemcitabine hydrochloride; GC regimen) was gemcitabine
hydrochloride 1 g/m2 (days 1, 8 and 15) and cisplatin 70
mg/m2 (day 2), with 3 weeks for 1 treatment course.
Cystoscopy, pelvic B ultrasound and pelvic CT were performed at
follow-up intervals (once every 3 months) to check for tumor
recurrence.
Statistical analysis
The results were recorded in EXCEL spreadsheets
(Microsoft, Seattle, WA USA) and analyzed using the SPSS software,
version 16.0 (SPSS Inc., Chicago, IL, USA). All result parameters
are expressed as mean ± standard deviation. A t-test was used to
analyze the difference level between the two groups. Perioperative
categorical data or complication results were analyzed by
non-parametric Whitney U test, χ2 test and Fisher's
exact test. P<0.05 was considered to indicate a statistically
significant difference.
Results
Patient characteristics
The 30 patients were randomized to an open surgery
group (group A) and laparoscopic surgery group (group B), with 15
patients in each group. All 30 patients were included in the
statistical analysis. The baseline characteristics of the two
groups included gender, mean age, clinical stage, pathological
stage, number of tumors and maximum tumor diameter. The baseline
characteristics were comparable between the two groups, and no
difference with statistical significance was observed (Table I).
 | Table I.Patient characteristics (mean ±
standard deviation, n=15 per group). |
Table I.
Patient characteristics (mean ±
standard deviation, n=15 per group).
| Parameters | Open surgery | Laparoscopy | P-value |
|---|
| Age (years) |
64.600±8.943 |
62.533±10.501 | 0.5663 |
| Number of tumors
(n) |
2.133±0.990 |
2.200±0.862 | 0.8455 |
| Volume of tumors
(cm) |
2.667±0.900 |
2.633±0.743 | 2.8 |
| Follow-up duration
(months) |
9.600±2.586 |
9.000±2.268 | 0.5048 |
Perioperative situation and
follow-up
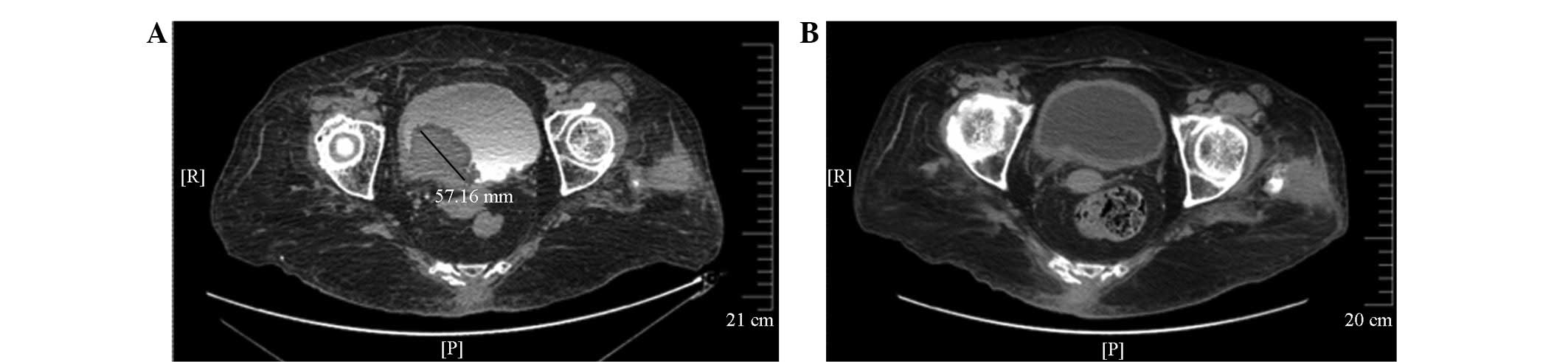
The recurrence rate for the two groups during
follow-up was 3/15 and 3/15 for groups A and B, respectively
(Table II). Although there was no
significant difference in overall survival rate and the incidence
of surgical incision infection between the two groups, the degree
of bleeding was notably higher in group A compared with group B
(Table II and Fig. 3). The incidence of early
postoperative frequent urination was notably higher in group A
compared with group B (4 patients in group A and 2 patients in
group B), but the incidence rate between the two groups showed no
significant difference (P=0.36). The symptom of frequent urination
in group A was mostly relieved in 1 month after surgery, although
in 1 patient the symptom was relieved 3 months after surgery.
According to the Clavien-Dindo classification (20) of surgical complications, no
significant difference was observed in the category and level of
complications between the two groups. All 30 patients successfully
completed the scheduled chemotherapy regimen During follow-up,
bladder function was sustained and no tumor recurrence was detected
(Fig. 3). All the patients
experienced a high quality of life. None of the patients had severe
hematological toxic reactions during chemotherapy, and the
complications were improved following symptomatic treatments. The
hematological toxic reactions included: 8 cases of grade I; 3 cases
of grade II, 2 cases of grade III; and 2 cases of grade IV in group
A; and 7 cases of grade I, 4 cases of grade II, 3 cases of grade
III and 1 case of grade IV in group B (Table II).
 | Table II.Follow-up data for the two groups
(n=15 per group). |
Table II.
Follow-up data for the two groups
(n=15 per group).
| Variable | Open surgery, n
(%) | Laparoscopic surgery,
n (%) | P-value |
|---|
| Tumor recurrence | 3/15 (20) | 3/15 (20) | 1.0000 |
| Frequent
urination | 4/15 (26.7) | 2/15 (13.3) | 0.3613 |
| Incision
infection | 3/15 (20) | 0/15 (0) | 0.0679 |
| Grade I hematological
toxicity | 8/15 (53.3) | 7/15 (46.7) | 0.715 |
| Grade II
hematological toxicity | 3/15 (20) | 4/15 (26.7) | 0.0614 |
| Grade III
hematological toxicity | 2/15 (13.3) | 3/15 (20) | 0.0162 |
| Grade IV
hematological toxicity | 2/15 (13.3) | 1/15 (6.7) | 0.0060 |
Follow-up data and postoperative
complications
Perioperative data are summarized in Table III. The duration of surgery was
significantly longer in group B than in group A; however, the
amount of surgical blood loss, the duration of postoperative
urinary catheter and drainage pipe indwelling and hospital stay
were significantly greater in group A than in group B.
 | Table III.Perioperative data (mean ± standard
deviation, n=15 per group). |
Table III.
Perioperative data (mean ± standard
deviation, n=15 per group).
| Variable | Open surgery | Laparoscopic
surgery | P-value |
|---|
| Duration of surgery
(min) |
90.333±16.740 |
105.333±11.255 | 0.0075 |
| Surgical blood loss
(ml) |
182.000±59.546 |
49.333±14.864 | <0.0001 |
| Duration of drainage
(days) |
4.067±1.387 |
1.20±0.941 | 0.0002 |
| Duration of urinary
catheterization (days) |
7.333±0.900 |
3.800±0.775 | 0.0000 |
| Hospital stay
(days) |
7.267±1.033 |
5.800±1.699 | 0.0080 |
Discussion
Over the past decade, as the understanding of
bladder cancers, particularly of muscle-invasive bladder cancers,
has deepened, it has been realized that bladder cancer is a
systemic disease that cannot be cured by local surgical treatment
alone (7). Combination treatment
with radiotherapy and chemotherapy is an effective method of
improving the long-term survival of invasive bladder cancer
following surgery (8).
Zhang et al (21) performed a retrospective analysis of
the treatment and follow-up results of 136 cases of MIBC in
Shanghai Ruijin Hospital between 2002 and 2007. It was observed
that the 5-year cancer-specific survival rate was higher in the
patients that underwent partial cystectomy than in those who
underwent radical cystectomy (68 vs. 55%, respectively; P=0.033),
and the 5-year cancer-specific survival rate in all MIBC patients
was 65%. The mean cancer-specific survival times in all MIBC cases
and the partial and radical cystectomy groups were 49.9, 52.6 and
40.4 months, respectively; 75 and 90% of local recurrence occurred
between 16 and 32 months after surgery, respectively.
In 2004, Holzbeierlein et al (22) summarized the results of 58 patients
with MIBC treated with partial cystectomy in the Memorial
Sloan-Kettering Cancer Center from 1995 to 2001, and observed that
the progressive recurrence-associated risk factors included
concomitant carcinoma in situ (CIS) [odds ratio (OR)=7.05]
and positive regional nodes (OR=4.38). In 2006, Kassouf et
al (23) reported that
pathological staging was associated with recurrence, and the
history of superficial bladder cancer was associated with clinical
staging and progressive recurrence.
In 2008, Smadlone et al (24) reported the results of 25 patients
with MIBC who received partial cystectomy from 1995 to 2005. The
mean follow-up duration was 45.3 months (8–118 months), and the
5-year cancer-specific survival rate was 84%. During the follow-up
period, the recurrence rate was 28%, of which 8% was superficial
recurrence and 20% was progress recurrence. The tumor volume was
the only risk factor that was found to be associated with
recurrence. The treatment of MIBC with partial cystectomy remains a
controversial topic, with the focus of controversy lying in the
appropriate indications. The indications for the treatment of MIBC
with partial cystectomy recommended in the 2011 edition of the US
NCCN bladder cancer treatment guidelines are: Single T2 tumor with
appropriate location and not associated with CIS. The proportion of
clinical cases of MIBC meeting this stringent standard is <5%
(21). However, this surgical
indication can be relaxed if sequential treatment with partial
cystectomy combined with the GC regimen is used. In the present
study, the recurrence rate was not significantly different between
the open surgery group and the laparoscopic surgery group based on
1-year follow-up data (3/15 vs. 3/15, respectively). The majority
of the recurrence in these patients was local recurrence, which is
consistent with the results of Zhang et al (21). The primary risk factors for
recurrence of bladder cancer are the primary tumor size and tumor
pathological grade.
With the application of laparoscopy in urology and
the improvement of intraluminal suture techniques, laparoscopic
techniques have been applied in cystectomy or partial cystectomy.
It has been confirmed in clinical practice that these two types of
procedure are technically feasible, with several advantages such as
reduced trauma, less blood loss, mild postoperative pain, shorter
hospital stay, better surgical field appearance and rapid recovery
with the resumption of normal daily activities (25). Conventional partial cystectomy
surgery requires the use of 3–5 channels, which requires numerous
skin incisions, provides poor cosmetic results and has a relatively
high risk of peritoneal implantation. To further reduce trauma,
improve cosmetic results and reduce tumor metastasis during the
surgical procedure, a single-port laparoscopic technique has been
proposed. Single-port multi-channel operating systems and special
instruments, such as flexible endoscopy, grasping forceps, scissors
and needle holders, have been successfully developed and have laid
the foundation for single-hole multi-channel laparoscopic
techniques (16,26).
In 2006, Chen et al (27) reported 8 cases of bladder cancer that
were successfully treated by intraperitoneal laparoscopic partial
cystectomy, with a mean surgery time of 230 min, mean blood loss
volume of 300 ml and mean hospital stay of 7 days. No
intraoperative and postoperative complications occurred. Two
patients had local recurrence and distant metastasis 12 and 14
months after surgery, respectively. Conservative treatment was
provided. The other 6 cases had no tumor recurrence and distant
metastasis during the 8–22 month follow-up period.
Based on the mastery of single-port laparoscopy for
renal cyst decortication and adrenalectomy, single-port
laparoscopic partial cystectomy has been conducted in the
Affiliated Hospital of the Academy of Military Medical Sciences.
The postoperative results have been satisfactory, with a duration
of surgery of 90–120 min (mean, 105.3 min), intraoperative bleeding
volume of 20–70 ml (mean, 49.3 ml), and mean hospital stay of 5.8
days. The wound drainage tube was removed on the day following the
surgery, and the urethral catheter was removed within 5 days after
surgery.
In the surgical procedure, it was recognized that
single-port laparoscopic partial cystectomy has unique advantages
for the treatment of bladder cancer. Firstly, the bladder was
filled with gas via the top of the bladder using a pneumoperitoneum
apparatus, which avoided interference with the abdominal organs and
reduced intestinal adhesion and wound complications. The gas-filled
bladder acted as a retractor, which facilitated the manipulation of
the instruments and resulted in improved surgical efficiency. In
addition, the gas-filled bladder had a beneficial role in
hemostasis, by compression of the bladder wall to reduce the
bleeding that is the main problem of open TURBt. Secondly, the
majority of the laparoscopic surgery procedure was conducted under
direct vision, with which the blind zone of traditional open
surgery and TURBt could be effectively observed and treated. By
aspirating urine and intraoperative bleeding through a urinary
catheter in the bladder and using barbed absorbable suture
techniques, the duration of surgery was reduced. Thirdly, the
extension and depth of surgical resection were comparable to those
of traditional open surgery, and it was possible to confirm the
intraoperative bleeding site, conduct effective hemostasis, and
conduct intraluminal suturing for resected sites. Following an
initial attempt, it was also found that compared with conventional
laparoscopy or other intraluminal surgeries such as transurethral
resection of the prostate, the transvesical single-port
laparoscopic partial cystectomy surgery was relatively challenging,
and the learning curve was relatively long requiring special
training and the use of certain flexible instruments to
successfully complete the surgery. The duration of surgery was
longer when larger tumors were resected, and when complete
resection of the tumor tissue was expected, it was necessary to
appropriately expand the incision or cut the tissue prior to
removal of the tumor.
With regard to the procedures used in the surgery,
the following recommendations are made based on experience: i) The
bladder puncture site should avoid the peritoneum to reduce the
impact on the abdominal viscera; ii) the placement of the
single-port kit should be conducted under the direct vision of the
cystoscope, with maintenance of satisfactory bladder filling; iii)
the use of a 5-mm integrated endoscope can reduce the interference
of the surgery by the instruments; iv) the ureteral open position
should be confirmed prior to the resection of the bladder tumor to
avoid injury; v) mastery of the intraluminal suture technique is
necessary; vi) ureteral reimplantation should be considered if the
distance from the tumor base to the ureteral orifice is <l cm,
or in cases of accidental ureter damage; vii) for large resection
tissue blocks, a morcellator can be used or the tissue can be split
into smaller pieces prior to the removal of the tissue.
The following subjects remain controversial in
laparoscopic partial cystectomy: The risk of intra-abdominal tumor
implantation; urine leakage and ureteral injury; and bladder tumor
recurrence. However, these risks of surgery can be avoided by the
use of single-port laparoscopy. The laparoscopic technique
described in the present study used an extraperitoneal approach,
which avoided the flowing of urine into the abdominal cavity. In
addition, filling the bladder with water to observe the peritoneal
position and fully separating the peritoneum is conducive to
bladder suturing. Cystoscopy performed during the surgery to
determine the location of the tumor and select the optimum puncture
site prevents penetration of the tumor tissue and reduces puncture
channel transfer. With monitoring by laparoscopy, the tumor can be
completely resected using an electrocautery hook and ultrasonic
scalpel; thus, the surgery may be conducted precisely and with
minimal damage. Furthermore, under the pressure of the
pneumoperitoneum, the bladder mucosa can be fully developed, so
that during the surgical procedure it is possible to fully observe
the bladder mucosa. For smaller tumors in the bladder and tumors
missed by cystoscopic examination, electrocautery gasification can
be conducted using an electrocautery hook, and for tumors on the
side-wall of the bladder, a ureteral catheter can be inserted
during surgery to prevent damage of the ureteral orifice. During
surgery, 2.0 absorbable suture lines can be used, depending on the
circumstances, for continuous full-thickness suturing of the
bladder, followed by injection supercharging of the bladder to
observe whether there is any leakage of urine. In order to reduce
the implantation of tumor cells in the extraperitoneal space, the
incised tumor specimens should be placed in a specimen bag as
quickly as possible, and the extraperitoneal space should be soaked
in distilled water for 10 min prior to suturing the bladder. The
patients in this study had no peritoneal damage, the specimens were
all complete, >1.5 cm and the bladder healed well without any
urine leakage or ureteral damage. The drainage tubes were removed
24–48 h after surgery.
In summary, transvesical single-port laparoscopic
partial cystectomy has been found to be a safe, effective and
feasible surgical method following its initial application in
bladder surgery. This surgical method not only is advantageous
compared with open surgery and transurethral surgery, but also
compensates for the deficiencies of these two traditional surgical
methods. The single-port laparoscopic method is not only minimally
invasive (less invasive, with better cosmetic results than ordinary
multiple-port laparoscopy), but also avoids the risk of water
intoxication that traditional transurethral surgery has, in
addition to the deficiencies of incompletely tumor resection and
poorer long-term efficacy. Based on experience in China and
overseas, it is considered that with regard to the ‘gold standard’
status of radical cystectomy for the treatment of MIBC, in
appropriate cases of MIBC, surgery with bladder preservation is a
practical and significant method for improving the quality of life
and reducing the risk of surgery for patients. As a simple and safe
surgical method, with few complications that enables the
preservation of the bladder, single-port laparoscopic partial
cystectomy has unique advantages, which are worthy of further
exploration and may be recommended for wider use. Due to the
current results being from a small sample at a single center,
further controlled clinical studies with a long-term follow-up are
required to confirm the clinical efficacy.
References
|
1
|
Lindahl F, Jørgensen D and Egvad K:
Partial cystectomy for transitional cell carcinoma of the bladder.
Scand J Urol Nephrol. 18:125–129. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Resnick MI and O'Conor VJ Jr: Segmental
resection for carcinoma of the bladder: Review of 102 patients. J
Urol. 109:1007–1010. 1973.PubMed/NCBI
|
|
3
|
Novick AC and Stewart BH: Partial
cystectomy in the treatment of primary and secondary carcinoma of
the bladder. J Urol. 116:570–574. 1976.PubMed/NCBI
|
|
4
|
Oosterlinck W, Lobel B, Jakse G, Malmström
PU, Stockle M and Sternberg C: European Association of Urology
(EAU) Working Group on Oncological Urology: Guidelines on bladder
cancer. Eur Urol. 41:105–112. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Shabsigh A, Korets R, Vora KC, et al:
Defining early morbidity of radical cystectomy for patients with
bladder cancer using a standardized reporting methodology. Eur
Urol. 55:164–174. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ramani VA, Maddineni SB, Grey BR and
Clarke NW: Differential complication rates following radical
cystectomy in the irradiated and nonirradiated pelvis. Eur Urol.
57:1058–1063. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Merseburger AS, Matuschek I and Kuczyk MA:
Bladder preserving strategies for muscle-invasive bladder cancer.
Curr Opin Urol. 18:513–518. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Solsona E, Climent MA, Iborra I, et al:
Bladder preservation in selected patients with muscle-invasive
bladder cancer by complete transurethral resection of the bladder
plus systemic chemotherapy: Long-term follow-up of a phase 2
nonrandomized comparative trial with radical cystectomy. Eur Urol.
55:911–919. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mak RH, Zietman AL, Heney NM, Kaufman DS
and Shipley WU: Bladder preservation: Optimizing radiotherapy and
integrated treatment strategies. BJU Int. 102:1345–1353. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Merseburger AS and Kuczyk MA: The value of
bladder-conserving strategies in muscle-invasive bladder carcinoma
compared with radical surgery. Curr Opin Urol. 17:358–362. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Divrik RT, Sahin AF, Yildirim U, Altok M
and Zorlu F: Impact of routine second transurethral resection on
the long-term outcome of patients with newly diagnosed pT1
urothelial carcinoma with respect to recurrence, progression rate
and disease-specific survival: A prospective randomised clinical
trial. Eur Urol. 58:185–190. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Bauer O, Devroey P, Wisanto A, Gerling W,
Kaisi M and Diedrich K: Small diameter laparoscopy using a
microlaparoscope. Hum Reprod. 10:1461–1464. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Leggett PL, Bissell CD, Churchman-Winn R
and Ahn C: Three-port microlaparoscopic cholecystectomy in 159
patients. Surg Endosc. 15:293–296. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kagaya T: Laparoscopic cholecystectomy via
two ports, using the ‘Twin-Port’ system. J Hepatobiliary Pancreat
Surg. 8:76–80. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kaouk JH, Haber GP, Goel RK, et al:
Single-port laparoscopic surgery in urology: Initial experience.
Urology. 71:3–6. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kaouk JH and Palmer JS: Single-port
laparoscopic surgery: initial experience in children for
varicocelectomy. BJU Int. 102:97–99. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Reavis KM, Hinojosa MW, Smith BR and
Nguyen NT: Single-laparoscopic incision transabdominal surgery
sleeve gastrectomy. Obes Surg. 18:1492–1494. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Nguyen NT, Hinojosa MW, Smith BR and
Reavis KM: Single laparoscopic incision transabdominal (SLIT)
surgery-adjustable gastric banding: A novel minimally invasive
surgical approach. Obes Surg. 18:1628–1631. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Remzi FH, Kirat HT, Kaouk JH and Geisler
DP: Single-port laparoscopy in colorectal surgery. Colorectal Dis.
10:823–826. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Tokunaga M, Kondo J, Tanizawa Y, Bando E,
Kawamura T and Terashima M: Postoperative intra-abdominal
complications assessed by the Clavien-Dindo classification
following open and laparoscopy-assisted distal gastrectomy for
early gastric cancer. J Gastrointest Surg. 16:1854–1859. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhang M, Tao R, Zhang C and Shen Z:
Lymphovascular invasion and the presence of more than three tumors
are associated with poor outcomes of muscle-invasive bladder cancer
after bladder-conserving therapies. Urology. 76:902–907. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Holzbeierlein JM, Lopez-Corona E, Bochner
BH, et al: Partial cystectomy: A contemporary review of the
Memorial Sloan-Kettering Cancer Center experience and
recommendations for patient selection. J Urol. 172:878–881. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kassouf W, Swanson D, Kamat AM, et al:
Partial cystectomy for muscle invasive urothelial carcinoma of the
bladder: A contemporary review of the M. D. anderson cancer center
experience. J Urol. 175:2058–2062. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Smaldone MC, Jacobs BL, Smaldone AM and
Hrebinko RL Jr: Long-term results of selective partial cystectomy
for invasive urothelial bladder carcinoma. Urology. 72:613–616.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Chapron C, Dubuisson JB, Jacob S,
Fauconnier A and Da Costa Vieira M: Laparoscopy and bladder
endometriosis. Gynecol Obstet Fertil. 28:232–237. 2000.(In French).
PubMed/NCBI
|
|
26
|
Gill IS, Canes D, Aron M, et al: Single
port transumbilical (E-NOTES) donor nephrectomy. J Urol.
180:637–641. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Chen X, Qi L, Chen HQ, Qi F, Liu HY and
Chen XX: Laparoscopic partial cystectomy. Zhong Guo Nei Jing Za Zhi
She. 12:456–457. 2006.(In Chinese).
|