Introduction
Preeclampsia is major cause of maternal morbidity
and mortality that is characterized by the development of
hypertension and proteinuria after 20 weeks of gestation (1) and complex disorders, including
placental and maternal components (2). Recent advances in genotyping technology
are likely to facilitate genome-wide association studies of
preeclampsia. Nucleated fetal erythrocytes, trophoblasts,
leukocytes and even fetal progenitors can cross the placenta
(3). Gussin et al (4) have shown that endothelial progenitor
cells (EPCs) are present in peripheral blood in the second
trimester. Moreover, Sugawara et al (5) demonstrated that the number of EPCs
increases in the second and third trimesters. Buemi et al
(6) observed that the number of
isolated EPCs gradually increases every trimester.
Free fetal DNA particles in maternal blood are
promising as an important means for the diagnosis of genetic
abnormalities of the fetus without invasive procedures.
Quantitative changes of cell-free fetal DNA in maternal blood as an
indicator for impending preeclampsia have been reported in numerous
studies. When the cell-free fetal DNA levels of 30 preeclamptic
patients were compared with those of healthy pregnant women, an
average 3.06-fold increase was observed (7).
CD34 is a transmembrane protein that is expressed in
1–4% of human bone marrow cells. These cells include pluripotent
hematopoietic stem cells and progenitors of each cell line
(8). In addition, CD34 is expressed
in the vascular endothelium of various organs. Fetal
CD34+ cells are detected in maternal blood during
pregnancy (9). Moreover, fetal
CD34+ cells are known to persist in the maternal
circulation even 27 years after delivery (10). CD133, also known as prominin-1, is a
protein expressed in hematopoietic stem and progenitor cells;
however, its function is not fully understood (11,12).
In the last 20 years, antibodies against CD34
(13) and CD133 (11,12) have
been widely used as markers for hematopoietic and progenitor cells
(14), and it has been shown that
CD34+ and CD133+ progenitor cells increase in
normal pregnancy and decrease in preeclampsia.
Adhesion molecules, including the EPC marker
CD34+, have been found in allogenic and xenogenic aortic
valve prostheses (15). Therefore,
in end-stage calcified aortic stenosis, the presence of EPCs
appears to be a biological hallmark, among others such as
inflammatory infiltration, heat shock protein (Hsp) homologues and
neoangiogenesis (16). Further
advances are expected from proteomic research. Comparisons of
protein patterns between healthy patients and those with disease
have been increasingly conducted in recent years to discover
markers of disease. Hsps are overexpressed in all organisms to
protect them from environmental stresses such as heat, oxidative
stress and ischemia (17). Hsp27 and
Hsp70 are well-known stress response proteins. Studies have shown
that Hsp70 levels in pregnant women are significantly higher than
those in healthy pregnant women (18,19). It
is also known that placental levels of Hsp27 in normal patients are
lower than those in patients with preeclampsia (20).
In the light of this information, the aim of the
present study was to evaluate cell free fetal DNA encoding CD34 and
CD133 in the maternal blood from randomly selected healthy pregnant
women in gestational week (GW) 12–14. During the follow-up, the
free fetal DNA levels of women who did and did not develop
preeclampsia were compared in order to investigate the possible
predictive role of CD34 and CD133 in preeclampsia. Hsp27 and Hsp70
heat shock protein levels were also compared between the two groups
of patients.
Materials and methods
Study design and sample
collection
This prospective study was conducted in 80
consecutive healthy pregnant women who were admitted to the
Obstetrics and Gynecology Clinic, Cerrahpasa Medical Faculty,
Istanbul University (Istanbul, Turkey). This study was approved by
the Cerrahpasa Medical Faculty Ethics Committee. Informed consent
was taken from every woman enrolled in the study. Multiple
pregnancies and any systemic diseases complicating pregnancy were
excluded. In order to increase the possibility of acquiring more
preeclamptic women, and also to prevent possible bias, only first
pregnancies were included.
During follow-up 8 women developed gestational
diabetes; 3 women developed pregnancy-induced hypertension; 2 women
developed pregnancy-induced cholestasis; 1 woman had a termination
of pregnancy at GW 19 and 1 woman withdrew from follow-up. The
studied was completed with 65 women. Six of the 65 women (9.2%)
developed preeclampsia.
Blood samples were taken from the pregnant women in
GW 12–14. Prior to any procedure, 5 ml maternal venous blood was
sampled and collected in an ethylenediaminetetraacetic tube.
Immediately after sampling, the plasma fraction was obtained by
centrifugation of the blood sample at 10,000 × g,4°C for 10 min and
500 µl from the supernatant layer was used. The diagnosis of
preeclampsia was made by measurement of ≥140 mmHg systolic blood
pressure and ≥90 mmHg diastolic pressure at least twice, with a ≥6
h interval between measurements; and ≥300 mg/24 h proteinuria or
1+ proteinuria in the dipstick test after GW 20 in a
woman who did not previously have hypertension or a renal disorder.
Plasma fractions were processed in the Molecular Diagnosis
Laboratory, Department of Molecular Biology and Genetics,
Cerrahpasa Medical Faculty, Istanbul University.
Maternal plasma fetal DNA processing
and quantitation
A 150-µl sample of plasma was used for each isolate.
An innuPREP virus DNA/RNA kit (Analytik Jena/Biometra, Germany) was
used for the isolation of fetal DNA from the maternal blood
according to the instructions of the manufacturer.
Gene sequences encoding CD34+ and
CD133+ surface antigens were used in order to
quantitatively measure the fetal DNA in the maternal blood; and a
gene sequence encoding glyceraldehyde phosphate dehydrogenase
(GAPDH), which is located in the autosomal region, was used as an
indicator of total DNA in the maternal blood since its expression
is constant at all times.
The primer sequences used for quantitative
polymerase chain reaction (qPCR) are shown in Table I. Platinum SYBR Green qPCR
SuperMix-UDG (Invitrogen Life Technologies, Carlsbad, CA, USA) was
used for the amplification and detection of DNA and a final primer
concentration of 250 nM was used as template for the isolation of
CD34 and CD133. Reactions were performed in a total volume of 25
µl.
 | Table I.Primer sequences used for qPCR. |
Table I.
Primer sequences used for qPCR.
| Gene | Sequence (5′-3′) |
|---|
| CD34 | F:
CCTGATGAATCGCCGCAGCTGGAGC |
|
| R:
CCTGGCCTCCACCGTTTT |
| GAPDH | F:
GAAGGTGAAGGTCGGAGT |
|
| R:
GAAGATGGTGATGGGATTTC |
| CD133 | F:
GGACCCATTGGCATTCTC |
|
| R:
CAGGACACAGCATAGAATAATC |
The qPCR consisted of 1 cycle of denaturation for 10
min at 95°C total followed by 50 cycles comprising denaturation for
30 sec at 95°C, binding for 1 min in 56°C and elongation for 1 min
at 72°C. The qPCR was performed using a Stratagene Mx3005P qPCR
system (Agilent Technologies, Santa Clara, CA, USA). qPCR results
of 8 healthy pregnant women were used for the calibration of CD34
and CD133 levels, and the results for the remaining women were
compared with the calibration values. Patients with results above
and below the calibration values for CD34 and CD133 genes were
identified for the preeclamptic and control groups. As the qPCR
efficiency was assumed to be 100%, a value of 2 was used during
calculation, instead of the 1.93 coefficient that is indicated in
the original formula. qPCR efficiencies were calculated using
slopes obtained from LightCycler software (Roche Diagnostics,
Basel, Switzerland). The corresponding qPCR efficiency (E) of one
cycle in the exponential phase was calculated according to the
equation: E = 10−1/slope.
Sodium dodecyl sulfate-polyacrylamide
gel electrophoresis (SDS-PAGE) and western blot analyses
Anti-Hsp27 monoclonal antibody (SPA-800), anti-Hsp70
monoclonal antibody (SPA-810) and horseradish peroxide
(HRP)-conjugated goat anti-mouse IgG secondary antibody (SAB-100)
were purchased from Stressgen Biotechnologies Corporation
(Victoria, Canada). The ECL Plus Western Blotting detection reagent
was purchased from Amersham (GE Healthcare, Piscataway, NJ, USA).
The bicinchoninic acid (BCA) assay kit was obtained from Pierce
(Thermo Fisher Scientific, Rockford, IL, USA). The other reagents
were obtained from Sigma-Aldrich (Chicago, IL, USA).
The protein concentration of each sample was
determined using the BCA kit. Bovine serum albumin was used as a
standard. For SDS-PAGE and western blot analysis, samples were
denatured in sample buffer containing 25 mM Tris-HCl (pH 6.8), 2%
SDS, 10% glycerol, 10% 2-mercaptoethanol and 0.002% bromphenol blue
and heating to boiling temperature for 3 min. Equal amounts of
proteins (100 µg/well) were analyzed by 10% SDS-PAGE. After
electrophoresis, proteins were transferred onto polyvinylidene
difluoride membranes using Bio-Rad Semi-Dry transfer apparatus
(Bio-Rad Laboratories, Inc., Hercules, CA, USA). Membranes were
blocked with 5% non-fat dry milk (in Tris-buffered saline and Tween
20) at room temperature for 1 h, and then incubated with the
primary antibodies anti-Hsp70 (dilution, 1:1,000) and anti-Hsp27
(dilution, 1:500) for 1 h at room temperature. The membrane was
then incubated with HRP-conjugated goat anti-mouse secondary
antibodies at a dilution of 1:5,000 for 1 h at room temperature.
Protein bands were detected by incubating the membranes with ECL
plus. Protein levels were quantitatively evaluated with ChemiDoc MP
and ImageLab 4.0.1 software (Bio-Rad).
Statistical analysis
Data are presented as means, standard deviations and
rates. Statistical analysis was performed using the t-test and
χ2 test. Correlation analyses were performed with the
Spearman correlation test. P<0.05 was considered statistically
significant. All statistical analyses were performed using the
Statistical Package for the Social Sciences (SPSS®) software
version 16.0 (SPSS, Inc., Chicago, IL, USA)
Results
Patient characteristics
At the initiation of the study, 80 women were
enrolled. Following a termination of pregnancy for one woman and
the withdrawal of one patient from follow-up, 78 women remained.
The incidence of preeclampsia in these women was 7% (6/78).
As mentioned in Materials and methods, 13 more women
were excluded because of pregnancy complications. A total of 65
pregnant women completed the study and fulfilled the inclusion
criteria. Samples from 8 women were used for the calibration of
CD34 and CD133 levels and, therefore, excluded from the statistical
calculations. During CD133 evaluation, the qPCR process was
unsuccessful in 7 cases. Statistical evaluations of CD34 and CD133
were performed for 57 and 50 women, respectively.
The mean age of the 57 women for whom qPCR
measurements were analyzed was 29.4±4.8 years. Among these 57
women, 6 (10.5%) developed preeclampsia. There was no significant
difference in the mean age of the preeclamptic and non-preeclamptic
women (29.6±4.6 vs. 28.1±6.1 years, respectively; P=0.485)
CD34 and CD133 expression
Expression levels of CD34 and CD133 in the two
groups were compared with the calibration results from 8 healthy
pregnant women. Among 57 women, CD34 expression was decreased in 30
(52.6%) and increased in 27 (47.4%) cases. Among 50 women, CD133
expression was decreased in 14 (28%) and increased in 36 (72%)
cases.
CD34 expression was compared between the
preeclamptic (n=6) and non-preeclamptic (n=51) groups. In the
preeclamptic group, CD34 expression was increased in 2 (33.3%) and
decreased in 4 (66.6%) women. In the non-preeclamptic group, CD34
expression was increased in 25 (49%) and decreased in 26 (51%)
women (P=0.467; Table II).
 | Table II.Comparison of CD34 expression between
the preeclamptic and non-preeclamptic groups. |
Table II.
Comparison of CD34 expression between
the preeclamptic and non-preeclamptic groups.
|
Expressiona | Preeclamptic
(n=6) | Non-preeclamptic
(n=51) |
P-valueb |
|---|
| Decreased | 4 | 26 | 0.467 |
| Increased | 2 | 25 |
|
CD133 expression was compared between the
preeclamptic (n=6) and non-preeclamptic (n=44) groups. In the
preeclamptic group, CD133 expression was increased in 4 (66.6%) and
decreased in 2 (33.3%) women. In the non-preeclamptic group, CD133
expression was increased in 32 (72%) and decreased in 12 (28%)
women (P=0.756; Table III).
 | Table III.Comparison of CD133 expression
between the preeclamptic and non-preeclamptic groups. |
Table III.
Comparison of CD133 expression
between the preeclamptic and non-preeclamptic groups.
|
Expressiona | Preeclamptic
(n=6) | Non-preeclamptic
(n=51) |
P-valueb |
|---|
| Decreased | 2 | 12 | 0.756 |
| Increased | 4 | 32 |
|
Spearman's correlation analysis showed that there
was no correlation between CD34 and CD133 (P=0.122; r=0.219).
Hsp27 and Hsp70 expression
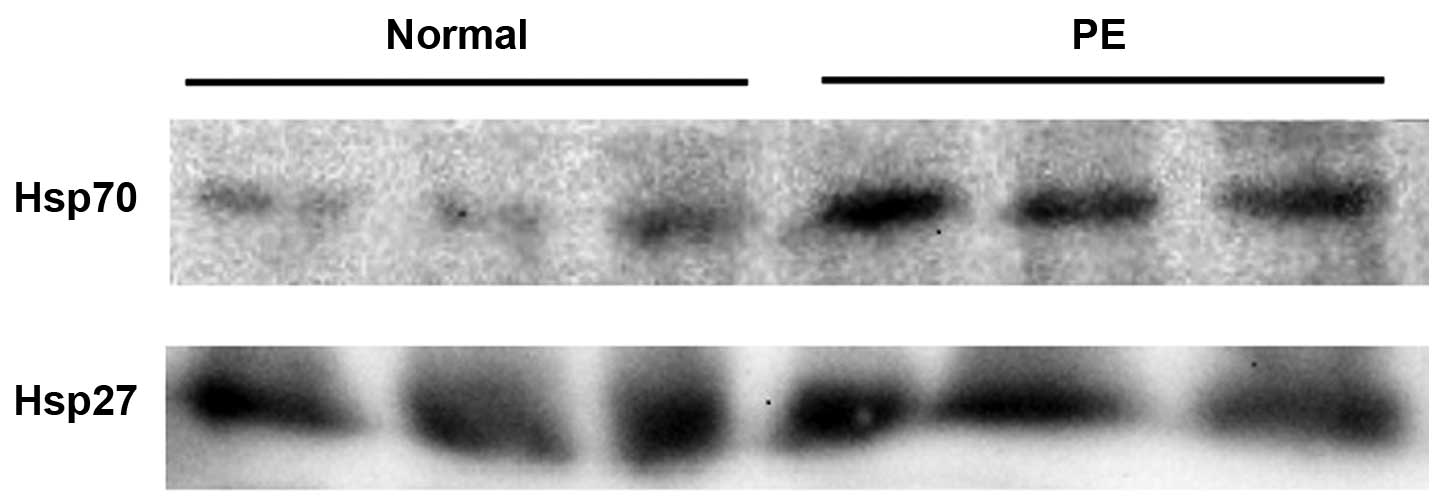
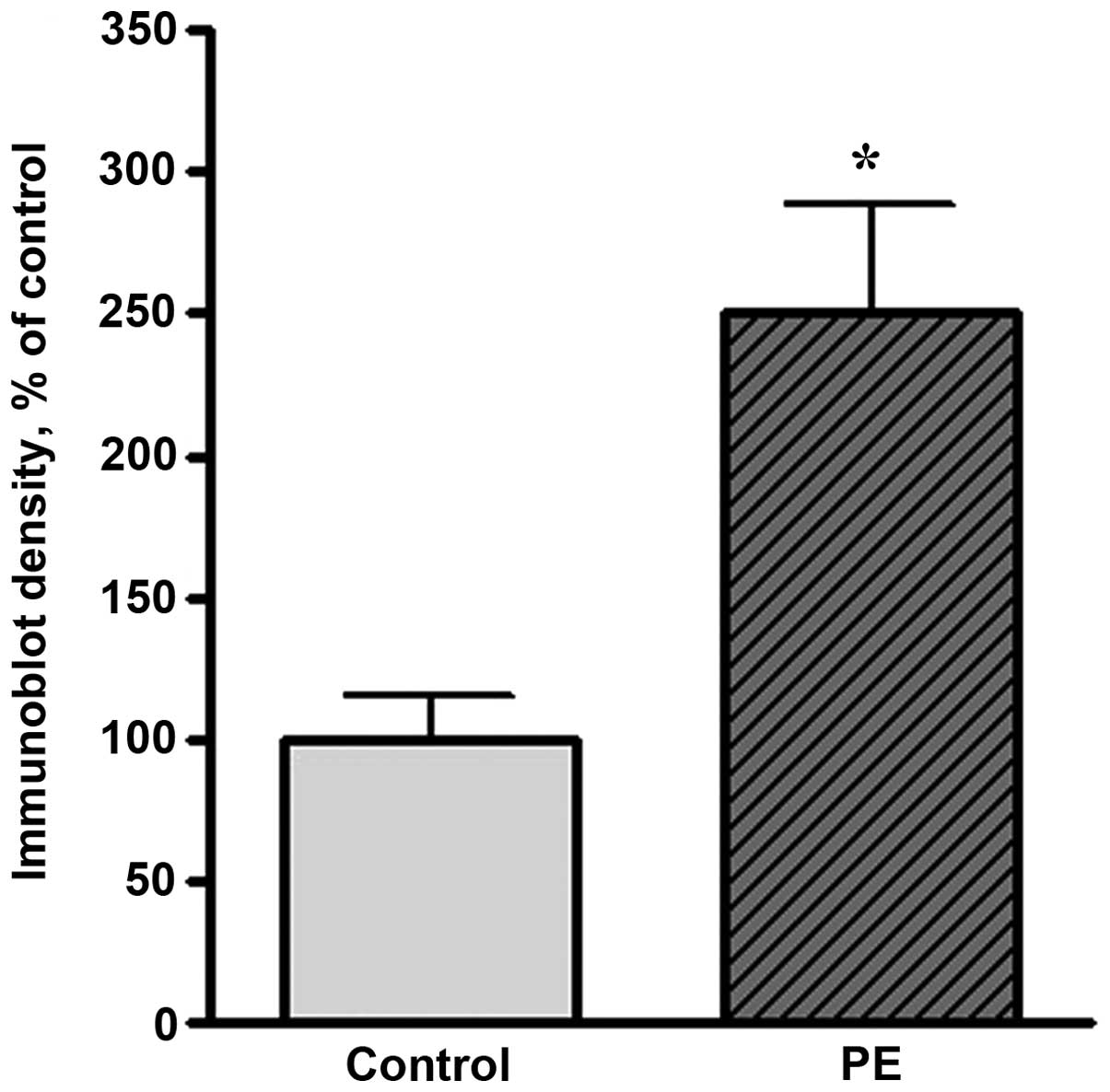
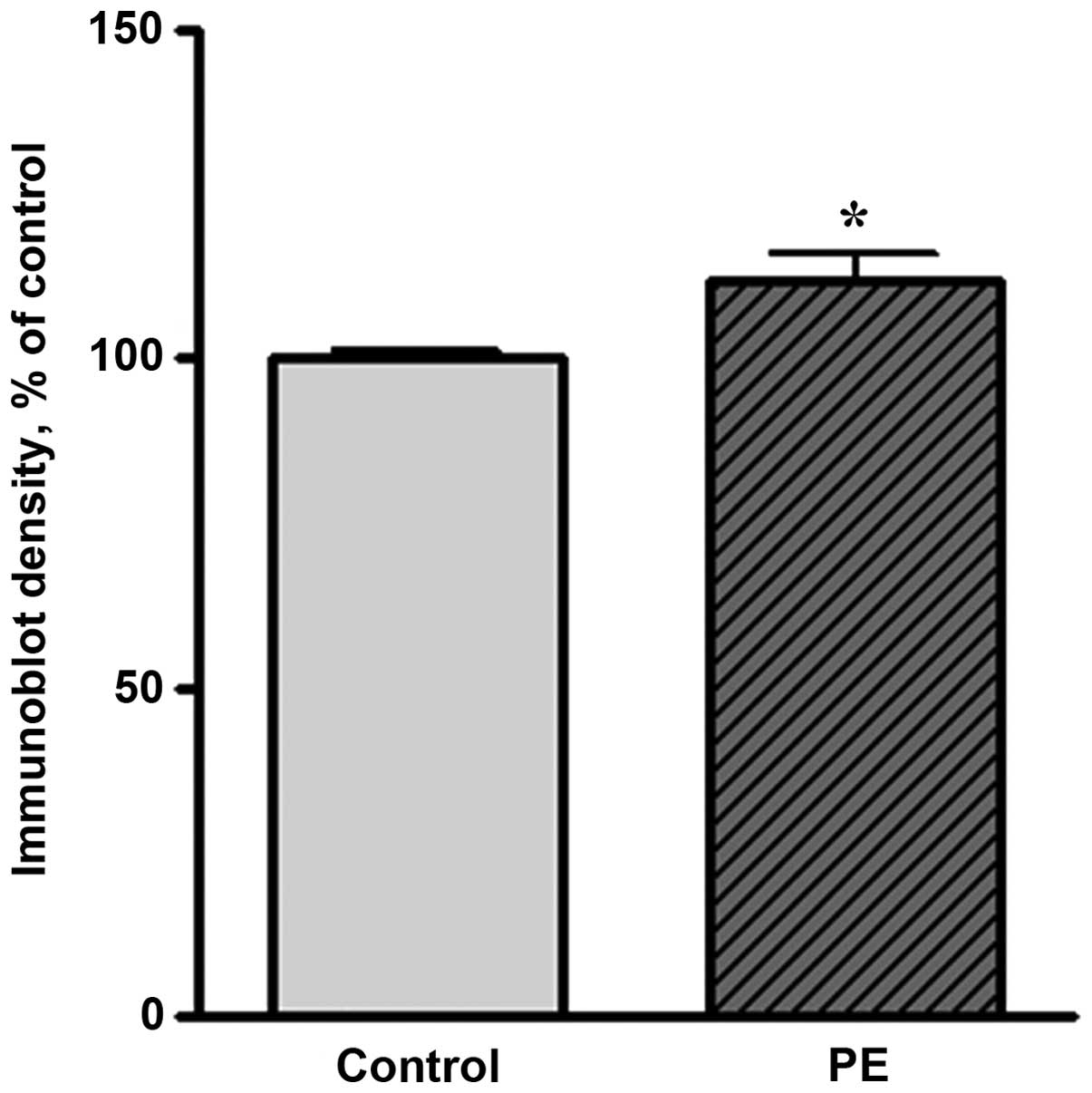
Western blot analysis showed that the expression
levels of Hsp27 and Hsp70 were markedly increased in preeclamptic
women compared with healthy pregnant women. A representative
western blot result is shown in Fig.
1. The level of Hsp70 in preeclamptic women was significantly
increased compared with that in healthy pregnant women (by 150%,
P<0.05; Fig. 2). The Hsp27 level
was increased by 11% of the control level in preeclamptic women
(Fig. 3).
Discussion
In recent studies concerning the pathophysiology of
preeclampsia, the idea that an altered balance of angiogenic
[vascular endothelial growth factor (VEGF) and placental growth
factor (PlGF)] and antiangiogenic [soluble fms-like tyrosine
kinase-1 (sFlt-1) and soluble endoglin (sEng)] factors may play
role in the pathogenesis of preeclampsia gained importance.
According to this theory, the antiangiogenic factor sFlt-1 is
released from the hypoxic placenta. VEGF interacts with its
receptor on cell membranes where it exerts its effects via Flt-1;
VEGF is a strong angiogenic factor and causes vasodilatation.
sFlt-1 is the soluble and, therefore, detectable form of Flt-1, and
is found in maternal serum. sFlt-1 is an antiangiogenic factor that
shows antagonistic effects against VEGF and PlGF by binding to them
in the serum (21).
Eng is the co-receptor of transforming growth factor
(TGF)-β1 and TGF-β3, and is widely expressed in vascular
endothelium and syncytiotrophoblasts. The TGF-β1 signaling pathway
contains CD34 and CD133. The soluble form of Eng, sEng, is an
antiangiogenic factor and inhibits the TGF-β1 pathway (21,22).
The present study focused on two different genes
that have the potential to be markers for preeclampsia.
CD34-expressing cells are precursors of hematopoietic and
endothelial cell lines and are known to be regulators of
angiogenesis (23,24). The other marker, CD133, was first
defined in the neuroepithelial stem cells of mice (25); its function is not well established,
although it is considered to play a role in angiogenesis. In the
human body, CD133 is known to be an antigenic marker expressed in
hematopoietic stem and progenitor cells (11,12).
In preeclamptic women, free fetal DNA levels
increase 3-fold compared with those in healthy pregnant women
(7,12,26–28).
Zhong et al (29) suggested
that DNA levels were higher in early-onset (<34 GW) preeclampsia
compared with late onset (>34 GW) preeclampsia and healthy
pregnant women; this finding was attributed to placental damage.
Sifakis et al (30) evaluated
the serum samples of pregnant women at GWs 11–13 and showed that
the levels of fetal DNA fragments were significantly higher in
early onset compared with late onset preeclampsia. In the present
study, the aim was to go a step further by evaluating the potential
predictive value of CD34 and CD133. Therefore, only healthy
pregnant women at GW 12–14 were enrolled.
The amount of free fetal DNA in the maternal serum
of healthy pregnant women has been shown to increase with
increasing gestational age (31).
Moreover, the ratio of fetal DNA to total free DNA has been shown
to increase every trimester, although total free DNA remains
unaffected by gestational age (32).
In the present study, in the non-preeclamptic group,
also denoted as the healthy group, CD34 was decreased in 26 (51%)
and increased in 25 (49%) of 51 women; CD133 was decreased in 12
(28%) and increased in 32 (72%) of 44 women. In the preeclamptic
group, CD34 expression was increased in 2 (33.3%) and decreased in
4 (66.6%); whereas CD133 expression was increased in 4 (66.6%) and
decreased in 2 (33.3%). There was no significant difference between
preeclamptic and non-preeclamptic women, neither in CD34 nor in
CD133 expression. Spearman's correlation analysis showed that there
was no correlation between CD34 and CD133.
Luppi et al (14) detected that circulating
CD34+ and CD133+ progenitor cells were
increased in normal pregnancy and decreased in preeclamptic women.
By contrast, Matsubara et al (33) showed that the number of
CD34+, CD133+ and VEGF2+ cells in
the maternal circulation increased with increasing gestational age,
and that there was no significant difference in the number of these
cells between preeclamptic and non-preeclamptic women. Buemi et
al (6) suggested that the number
of CD133+ and VEGF2+ endothelial progenitor
cells in the maternal circulation increased with increasing
gestational age, and that women with gestational hypertension had
higher levels of the latter cells when compared with healthy
pregnant women.
CD34 and CD133 are expressed by a small fraction of
fetal cells in the fetal circulation. However in the present study,
in maternal circulation CD34 was amplified in 65 women and CD133
was amplified in 57 women by qPCR. Gene expression was evaluated by
comparison with a calibration value obtained from the analysis of a
set of samples from 8 healthy pregnant women selected from the
study group. CD34 expression was decreased in 30 (52.6%) and
increased in 27 (47.4%) of the 57 pregnant women, and CD133
expression was decreased in 14 (28%) and increased in 36 (72%) of
50 pregnant women.
Studies have demonstrated the presence of EPCs
including CD34 and CD133 in different types of atherosclerosis
(34,35) and in allogeneic and xenogeneic aortic
valve prostheses. Endothelial cell dysfunction has been suggested
to be a part of a wider maternal inflammatory reaction that is
responsible for the clinical syndrome of preeclampsia (36). The preeclamptic pregnancy is the most
studied among pregnancy-specific complications due to its strong
association stress which can result into endothelial dysfunction.
Hsp70 and Hsp27 are well-known stress response proteins expressed
under various pathological conditions, including trauma, and focal
or global ischemia (37). The
present study demonstrated that Hsp70 and Hsp27 proteins were
increased in preeclamptic women. Based on these findings, the
increase in EPCs correlates with the increase of Hsps, but CD34 and
CD133 changes depending on preeclampsia groups. With the
statistical analysis of qPCR results for CD34 and CD133, the
increase in EPCs correlates with the increase of Hsps, but CD34 and
CD133 changed in the preeclampsia groups.
In conclusion, the changes in CD34 and CD133 DNA in
preeclamptic compared with non-preeclamptic women remain unclear.
The results of this study revealed that the levels of CD34 did not
change in preeclampsia; however, it is striking that the level of
CD133 expression was increased in 72% of all pregnant women.
Acknowledgements
The study was funded by the Research Fund of
Istanbul University (Project no: 20411 and UDP-32968).
References
|
1
|
Roberts JM and Cooper DW: Pathogenesis and
genetics of preeclampsia. Lancet. 357:53–56. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Salonen Ros H, Lichtenstein P, Lipworth L
and Cnattingius S: Genetic effects on the liability of developing
pre-eclampsia and gestational hypertension. Am J Med Genet.
4:256–260. 2000. View Article : Google Scholar
|
|
3
|
Nguyen Huu S, Dubernard G, Aractingi S and
Khosrotehrani K: Feto-maternal cell trafficking: A transfer of
pregnancy associated progenitor cells. Stem Cell Rev. 2:111–116.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gussin HA, Bischoff FZ, Hoffman R and
Elias S: Endothelial precursor cells in the peripheral blood of
pregnant women. J Soc Gynecol Invest. 9:357–361. 2002. View Article : Google Scholar
|
|
5
|
Sugawara J, Mitsui-Saito M, Hoshiai T,
Hayashi C, Kimura Y and Okamura K: Circulating endothelial
progenitor cells during human pregnancy. J Clin Endocrinol Metab.
90:1845–1848. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Buemi M, Allegra A, D'Anna R, et al:
Concentration of circulating endothelial progenitor cells (EPC) in
normal pregnancy and in pregnant women with diabetes and
hypertension. Am J Obstet Gynecol. 196:68.e1–68.e6. 2007.
View Article : Google Scholar
|
|
7
|
Zeybek YG, Günel T, Benian A, Aydınlı K
and Kaleli S: Clinical evaluations of cell-free fetal quantities in
pre-eclamptic pregnancies. J Obstet Gynaecol Res. 39:632–640. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Satterthwaite AB, Burn TC, Le Beau MM and
Tenen DG: Structure of the gene encoding CD34, a human
hematopoietic stem cell antigen. Genomics. 12:788–794. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Davey DA and MacGillivray I: The
classification and definition of the hypertensive disorders of
pregnancy. Am J Obstet Gynecol. 158:892–898. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bianchi DW, Zickwolf GK, Weil GJ,
Sylvester S and DeMaria MA: Male fetal progenitor cells persist in
maternal blood for as long as 27 years postpartum. Proc Natl Acad
Sci USA. 93:705–708. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Miraglia S, Godfrey W, Yin AH, et al: A
novel five-transmembrane hematopoietic stem cell antigen:
Isolation, characterization, and molecular cloning. Blood.
90:5013–5021. 1997.PubMed/NCBI
|
|
12
|
Yin AH, Miraglia S, Zanjani ED, et al:
AC133, a novel marker for human hematopoietic stem and progenitor
cells. Blood. 90:5002–5012. 1997.PubMed/NCBI
|
|
13
|
Ariga H, Ohto H, Busch MP, et al: Kinetics
of fetal cellular and cell-free DNA in the maternal circulation
during and after pregnancy: Implications for noninvasive prenatal
diagnosis. Transfusion. 41:1524–1530. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Luppi P, Powers RW, Verma V, Edmunds L,
Plymire D and Hubel CA: Maternal circulating
CD34+VEGFR-2+ and
CD133+VEGFR-2+ progenitor cells increase
during normal pregnancy but are reduced in women with preeclampsia.
Reprod Sci. 17:643–652. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Wilhelmi MH, Mertsching H, Wilhelmi M,
Leyh R and Haverich A: Role of inflammation in allogeneic and
xenogeneic heart valve degeneration: Immunohistochemical evaluation
of inflammatory endothelial cell activation. J Heart Valve Dis.
12:520–526. 2003.PubMed/NCBI
|
|
16
|
Mazzone A, Epistolato MC, De Caterina R,
et al: Neoangiogenesis, T-lymphocyte infiltration, and heat shock
protein-60 are biological hallmarks of an immunomediated
inflammatory process in end-stage calcified aortic valve stenosis.
J Am Coll Cardiol. 43:1670–1676. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Papp E, Nardai G, Söti C and Csermely P:
Molecular chaperones, stress proteins and redox homeostasis.
Biofactors. 17:249–257. 2013. View Article : Google Scholar
|
|
18
|
Molvarec A, Prohászka Z, Nagy B, Szalay J,
Füst G, Karádi I and Rigó J Jr: Association of elevated serum
heat-shock protein 70 concentration with transient hypertension of
pregnancy, preeclampsia and superimposed preeclampsia: A
case-control study. J Hum Hypertens. 20:780–786. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Fukushima A, Kawahara H, Isurugi C, et al:
Changes in serum levels of heat shock protein 70 in preterm
delivery and preeclampsia. J Obstet Gynaecol Res. 31:72–77. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Shin JK, Jeong YT, Jo HC, et al: Increased
interaction between heat shock protein 27 and mitogen-activated
protein kinase (p38 and extracellular signal-regulated kinase) in
pre-eclamptic placentas. J Obstet Gynaecol Res. 35:888–894. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Cunningham FG, Leveno KJ, Bloom SL, Hauth
JC, Gilstrap LC III and Wenstrom KD: Hypertensive disorders in
pregnancyWilliams Obstetrics. 22nd. McGraw Hill; New York: pp.
761–808. 2005
|
|
22
|
Lindheimer MD, Roberts JM and Cunningham
FG: Prevention of preeclampsia and eclampsiaChesley's Hypertensive
Disorders in Pregnancy. 3rd. Elsevier (Academic Press); San Diego,
CA: pp. 213–226. 2009
|
|
23
|
Majka M, Janowska-Wieczorek A, Ratajczak
J, et al: Numerous growth factors, cytokines, and chemokines are
secreted by human CD34+ cells, myeloblasts,
erythroblasts, and megakaryoblasts and regulate normal
hematopoiesis in an autocrine/paracrine manner. Blood.
97:3075–3085. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Peichev M, Naiyer AJ, Pereira D, et al:
Expression of VEGFR-2 and AC133 by circulating human
CD34+ cells identifies a population of functional
endothelial precursors. Blood. 95:952–958. 2000.PubMed/NCBI
|
|
25
|
Jászai J, Fargeas CA, Florek M, Huttner WB
and Corbeil D: Focus on molecules: Prominin-1 (CD133). Exp Eye Res.
85:585–586. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lo YM, Zhang J, Leung TN, Lau TK, Chang AM
and Hjelm NM: Rapid clearance of fetal DNA from maternal plasma. Am
J Hum Genet. 64:218–224. 1999. View
Article : Google Scholar : PubMed/NCBI
|
|
27
|
Hahn S, Gupta AK, Troeger C, et al:
Disturbances in placental immunology: Ready for therapeutic
interventions? Springer Semin Immunopathol. 27:477–493. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Carty DM, Delles C and Dominiczak AF:
Novel biomarkers for predicting preeclampsia. Trends Cardiovasc
Med. 18:186–194. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Zhong XY, Gebhardt S, Hillermann R, Tofa
KC, Holzgreve W and Hahn S: Parallel assessment of circulatory
fetal DNA and corticotropin-releasing hormone mRNA in early- and
late-onset preeclampsia. Clin Chem. 51:1730–1733. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Sifakis S, Zaravinos A, Maiz N, Spandidos
DA and Nicolaides KH: First-trimester maternal plasma cell-free
fetal DNA and preeclampsia. Am J Obstet Gynecol. 201:472.e1–472.e7.
2009. View Article : Google Scholar
|
|
31
|
Horinek A, Korabecna M, Panczak A, et al:
Cell-free fetal DNA in maternal plasma during physiological single
male pregnancies: Methodology issues and kinetics. Fetal Diagn
Ther. 24:15–21. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Pomyje J, Zivný J, Sefc L, Plasilová M,
Pytlík R and Necas E: Expression of genes regulating angiogenesis
in human circulating hematopoietic cord blood
CD34+/CD133+ cells. Eur J Haematol.
70:143–150. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Matsubara K, Abe E, Matsubara Y, Kameda K
and Ito M: Circulating endothelial progenitor cells during normal
pregnancy and pre-eclampsia. Am J Reprod Immunol. 56:79–85. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Bauriedel G, Jabs A, Skowasch D, et al:
Dendritic cells in neointima formation after rat carotid balloon
injury. Coordinated expression with anti-apoptotic Bcl-2 and HSP47
in arterial repair. J Am Coll Cardiol. 42:930–938. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Banchereau J, Briere F, Caux C, et al:
Immunobiology of dendritic cells. Annu Rev Immunol. 18:767–811.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Ekambaram P: HSP70 expression and its role
in preeclamptic stress. Indian J Biochem Biophys. 48:243–255.
2011.PubMed/NCBI
|
|
37
|
Shin JK, Jeong YT, Jo HC, et al: Increased
interaction between heat shock protein 27 and mitogen-activated
protein kinase (p38 and extracellular signal-regulated kinase) in
pre-eclamptic placentas. J Obstet Gynaecol Res. 35:888–894. 2009.
View Article : Google Scholar : PubMed/NCBI
|