Introduction
Spinal cord injury (SCI) is the most serious
complication of spinal injury. It frequently leads to dysfunction
of the limbs below the injury segment, with high incidence and
morbidity, but low mortality. SCI is also often associated with a
younger onset and high cost as patients may be unable to return to
their original health, which may affect their economic productivity
and also result in a high social cost (1,2). The
short- and long-term effects of modern medical treatments are not
ideal. SCI severely impairs the quality of life and brings a heavy
economic burden to society and the families of affected patients.
Identification of means to reduce SCI and promote post-operative
rehabilitation is one of the hotspots in current surgical research
(3,4). SCI triggers secondary injury through a
series of physiological and biochemical mechanisms, including
oxidative stress, excessive release of excitatory amino acids and
inflammatory response, so that lesions appear in intact tissue
around initial lesions, which further deepens the severity and
expands the scope of the injury (5).
Among these factors, oxidative stress may cause an imbalance
between reactive oxygen species and the anti-oxidant system, which
has an important role in the secondary injury component of SCI
(6). Prevention of oxidative stress
to reduce the degree of secondary injury has become a potential
strategy for the treatment of SCI (7).
Ginsenoside Rb1 (G-Rb1) is mainly derived from the
stem root and flower bud of Panax quinquefolius and Panax
notoginseng. A previous study indicated that G-Rb1 has
anti-oxidant effects, scavenges free radicals and improves the
body's immunity as mechanisms due to which it has been used for the
treatment of various traumatic diseases (8,9). Cheng
et al (10) demonstrated that
G-Rb1 reduces prostaglandin E2, NO2, matrix
metalloproteinase-13, cyclooxygenase-2, inducible nitric oxide
synthase (NOS), caspase-3 and poly(ADP ribose) polymerase levels,
thus preventing the interleukin-1-induced inflammatory response and
apoptosis of human articular chondrocytes. In study using a
hydrogen peroxide-induced human umbilical vein endothelial cell
model of aging, Liu et al (11) revealed that G-Rb1 promotes the
production of intracellular superoxide dismutase (SOD), reduces the
content of the lipid peroxidation product malondialdehyde (MDA) and
protects cells against oxidative stress-induced senescence. G-Rb1
adjusts the immune balance and scavenges free radicals, but it has
remained elusive whether it attenuates the oxidative stress injury
of the spinal cord through its anti-oxidant effect.
Nuclear factor erythroid 2-related factor 2
(Nrf2)/heme oxygenase (HO)-1 is considered to be the most important
anti-oxidant pathway. The key role of Nrf2/HO-1 in controlling
foreign bodies and oxidative damage has been confirmed in the
digestive, circulatory and nervous system, as well as in diseases
affecting the immune system. Activation of this pathway triggers
the production of corresponding anti-oxidant enzymes and phase-II
drug metabolism enzymes, thereby enhancing the ability of cells to
remove reactive oxygen species to maintain a redox balance and
reduce oxidative damage. It has been reported that G-Rb1 improves
organ injury induced by intestinal ischemia-reperfusion in C57BL/6J
mice by activating the Nrf2/HO-1 pathway (12). However, it has remained elusive
whether G-Rb1 exerts its protective effect against secondary SCI
via the endothelial (e)NOS/Nrf2/HO-1 signaling pathway. The aim of
the present study was to explore the specific implication of the
eNOS/Nrf2/HO-1 pathway in the effect of G-Rb1 on oxidative stress
injury of rat spinal cords as a possible mechanism of its
protective action.
Materials and methods
Animals
Sprague Dawley rats (n=40; 7 weeks old; 50% male and
50% female; weight, 220–260 g), were provided by the Experimental
Animal Division of the General Hospital of Shenyang Military Area
Command [Shenyang, China, rodent application license no. SYXK (Jun)
20120003; rodent production license no. SCXK (Army)20120001]. The
experiment was approved by the Experimental Animal Ethics Committee
of the General Hospital of Shenyang Military Area Command
(Shenyang, China). Animals were housed at a constant temperature
(22±1°C) with 50% humidity in a 12 h light/dark cycle. The rats had
ad libitum access to food and autoclaved water. Animals of
different sex were kept in separate cages.
Establishment of rat SCI model
The rat SCI model was established using Allen's
modified method (force, 25 g/cm; impact force, 10 g; fall height, 5
cm) (13,14). All animals were fasted for 12 h and
deprived of water for 4 h prior to surgery. Animals were maintained
warm during surgery. Rats were anesthetized by intraperitoneal
injection of 2% pentobarbital sodium (45 mg/kg) and then fixed in
the prone position on the operating table. A 2-cm incision was made
along the posterior midline of the spine and the muscle was bluntly
isolated, followed by laminectomy. The T10 chest segment was
exposed and injured with a heavy hammer (designed using Allen's
modified method; 25 gram cm force; impact force, 10 g; fall height,
5 cm) with a bottom diameter of 1.5 mm, resulting in moderate SCI
(15,16). The heavy hammer was removed
immediately after impact and the wound was sutured layer by
layer.
Groups and treatments
Rats were randomly divided into the sham operation
group (S group), SCI group, G-Rb1 treatment group (G-Rb1 group) and
SCI+G-Rb1+inhibitor L-name group (L-name group), with 10 rats in
each group (50% male and 50% female in each group). Rats in the S
group received laminectomy only; rats in G-Rb1 group were
intraperitoneally injected with G-Rb1 (10 mg/kg; Sigma-Aldrich;
Merck KGaA, Darmstadt, Germany) at 30 min after modeling and then
daily for 7 days. Rats in the SCI group were given an
intraperitoneal injection of an equal amount of normal saline and
rats in the L-name group were intraperitoneally injected with G-Rb1
(10 mg/kg) and given a tail vein injection of eNOS inhibitor L-name
at 30 min post modeling and then daily for 7 days (7 mg/kg; cat.
no. 51298-62-5; MedChemExpress, Monmouth Junction, NJ, USA).
Basso, Beattie and Bresnahan (BBB)
locomotor rating scale
The motor function of the hind limbs was evaluated
using the BBB method as previously described (17). The animals were observed according to
the standard BBB grading standards and the recovery of motor
function in the hind limbs was recorded. All observations were
performed simultaneously. Scoring criteria were as follows: 0–7
points, joint activity; 8–13 points, gait and coordination
function; 14–21 points, claw movement. The maximum score was 21
points and hind limb paralysis was scored as 0 points.
Sample collection and testing
The rats were euthanized using an overdose of 2%
pentobarbital sodium (120 mg/kg; intraperitoneal injection) at 24 h
after the last injection. Blood samples taken from the abdominal
aorta were centrifuged and stored at −80°C. Spinal cord tissue was
harvested from the injured area, of which one part was fixed in 10%
formalin, and another part was stored in liquid nitrogen.
ELISA
The changes of SOD (cat. no. SES134Ra), MDA (cat.
no. CEA597Ge), glutathione (GSH; cat. no. CEA294Ge) (all Wuhan USCN
Business Co., Ltd., Wuhan, China) and catalase (CAT; cat. no.
CSB-E13439r; Cloud-Clone Corp., Katy, TX, USA) in serum were
detected with an ELISA kit according to the manufacturer's
protocols. The optical density at 450 nm was measured using a
microplate reader (Bio-Rad 680; Bio-Rad Laboratories, Inc.,
Hercules, CA, USA) and the concentration was determined using a
standard curve.
H&E staining
Tissues were fixed in 10% formaldehyde for 24 h at
room temperature and then decalcified, dehydrated and permeabilized
using 50% xylene for 1 h and 100% xylene for 2 h. The tissues were
embedded in wax and sliced into 5-µm-thick sections using a
microtome. All of the following steps were performed at room
temperature. Sections were then dewaxed using xylene I for 15 min
and xylene II for 15 min, hydrated with absolute ethanol for 5 min,
90% ethanol for 2 min and 70% ethanol for 2 min. They were
subsequently mounted with 10% hematoxylin for 10 min,
differentiated with 1% hydrochloric acid and ethanol for 3–5 sec
and stained with 0.5% eosin for 1 min. Then they were dehydrated in
an alcohol gradient with xylene, cleared and mounted. Using a light
microscope, pathological changes in the spinal cord following
ginsenoside Rb1 treatment were observed.
Reverse transcription-quantitative
polymerase chain reaction (RT-qPCR) analysis
Primers were designed according to the sequences of
the eNOS, heat shock protein (HSP)90, Nrf2, HO-1 and NAD(P)H
quinone dehydrogenase 1 (Nqo1) genes listed in GenBank. The primers
were then synthesized in Shanghai Sangon Biotechnology Co., Ltd.
(Shanghai, China) and the sequences are listed in Table I.
 | Table I.Primer sequences used for polymerase
chain reaction. |
Table I.
Primer sequences used for polymerase
chain reaction.
| Gene | Upstream primer
sequence (5′-3′) | Downstream primer
sequence (5′-3′) |
|---|
| eNOS |
ACCGCCACACAGTAAATCCA |
TGCCAACAGGAAGCTGAGAG |
| HSP90 |
ACCAAGTCCCAGCTCACAAA |
TGGGGAGAAAGCAACCACTG |
| Nrf2 |
ATGAGTCGCTTGCCCTGG |
CTTGTTTTCCGTATTAAG |
| Nqo1 |
CTTGCTTTCCATCACCACCG |
GACGCTTCTTCCACCCTTCC |
| HO-1 |
AGCATGTTCCCAGGATG |
GCTCAATGTTGAGCACA |
| β-actin | CTG
TCCCTGTATGCCTCT |
ATGTCACGCACGATTTCC |
Spinal cord RNA was extracted using TRIzol (cat. no.
15596018; Invitrogen™; Thermo Fisher Scientific, Inc., USA) and
reverse transcribed into complementary DNA (cat. no. 4387406,
Invitrogen™, Thermo Fisher Scientific, Inc.) according to the
manufacturer's protocol. The composition of the reverse
transcription mixture was as follows: 10 µl 2X RT buffer mix, 1 µl
20X RT enzyme mix, 2 µl RNA sample and 7 µl nuclease-free
H2O. The reaction was performed at 37°C for 60 min. The
reaction was stopped by heating to 95°C for 5 min and holding at
4°C. This was followed by detection with a real-time PCR kit (iQ5;
Bio-Rad Laboratories, Inc.) in a real-time PCR system (RR820A;
Takara Bio, Inc., Otsu, Japan). The following thermocycling
conditions were used for RT-qPCR: Initial denaturation at 95°C for
30 sec; 40 cycles of PCR at 95°C for 5 sec and 60°C for 30 sec;
with a final dissociation stage at 95°C for 15 sec, 60°C for 1 min
and 95°C for 15 sec. The relative gene expression data was analyzed
with the 2∆∆Cq method (18).
Western blot analysis
Total tissue protein was extracted with a protein
extraction kit (cat. no. 78510; Thermo Fisher Scientific, Inc.) and
the protein concentration was determined by a bicinchoninic acid
protein quantification kit (cat. no. 23229; Thermo Scientific,
Inc.). Protein samples (30 µg/lane) were subjected to 10% SDS-PAGE
and transferred to polyvinylidene difluoride membranes (cat. no.
IB24002, Invitrogen; Thermo Fisher Scientific, Inc.). The samples
were incubated with 5% non-fat powdered milk with 100 ml
Tris-buffered saline with Tween-20 for 1 h, followed by incubation
with primary antibodies to eNOS (mouse monoclonal antibody; 1:1,500
dilution; cat. no. ab76198), HSP90 (1:10,000 dilution; cat. no.
ab203126), Nrf2 (1:1,000 dilution; cat. no. ab137550), Nqo1
(1:2,000 dilution; cat. no. ab217302) and HO-1 (1:1,000 dilution;
cat. no. ab82585) at 4°C overnight. Subsequently, membranes were
incubated with goat anti-mouse immunoglobulin (Ig) G H&L
horseradish peroxidase (HRP) conjugated (1:2,000 dilution; cat. no.
ab6789) or goat anti-rabbit IgG H&L HRP conjugated (1:2,000
dilution; cat. no. ab205718) secondary antibodies at 4°C for 2 h.
All primary and secondary antibodies were purchased from Abcam
(Cambridge, MA, USA) Subsequently, samples were developed with the
enhanced chemiluminescence method using Novex™ ECL
Chemiluminescent Substrate Reagent kit (cat. no. WP20005;
Invitrogen; Thermo Fisher Scientific, Inc.) for 1–2 min and
quantified with an automatic chemiluminescence imaging system
(Tanon 5200; Shanghai Tianneng Technology Co., Ltd., Shanghai,
China).
Immunohistochemical staining
Spinal cord tissues were dewaxed with xylene,
dehydrated with a gradient series of ethanols, incubated with 3%
hydrogen peroxide for 20 min at room temperature and washed three
times with PBS for 5 min each. The tissue was then blocked with 10%
goat serum (cat. no. ab7481; Abcam) for 30 min at room temperature.
The cells were incubated with antibodies against p-eNOS (1:400
dilution; cat. no. bs-13074R; BIOSS, Beijing, China) Nrf2 (1:100
dilution) in a humidified chamber at 4°C overnight, followed by
goat anti-rabbit IgG H&L HRP conjugated (1:2,000 dilution) for
30 min at room temperature. Immunoreactivity was then visualized
with diaminobenzidine (DAB; cat. no. DA1015) and haematoxylin (cat.
no. G1140) (both Beijing Solarbio Science & Technology Co.,
Ltd., Beijing, China) counterstaining was applied. The samples were
observed under a light microscope (magnification, ×200).
Statistical analysis
Values are expressed as the mean ± standard
deviation. Student's t-test was used to assess differences between
2 groups. One-way analysis of variance followed by Bonferroni's
post-hoc test was used assess differences among >2 groups. All
pairwise P-values are two-sided. P<0.05 was considered to
indicate a statistically significant difference. All data were
statistically analyzed using SPSS version 19.0 software (IBM Corp.,
Armonk, NY, USA).
Results
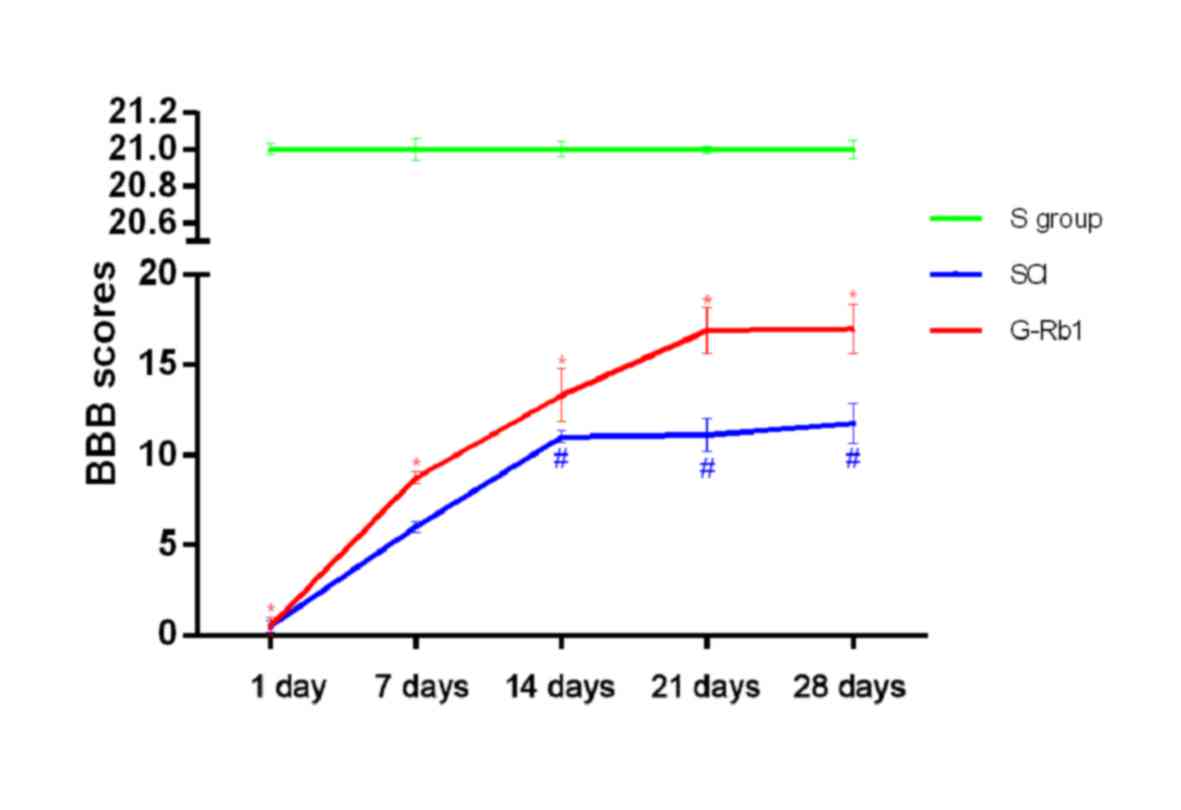
G-Rb1 improves the hind limb motor
function of SCI rats
All rats were released from the cage and conditioned
in an open space for 5 min, and the BBB test was performed and
recorded using camera monitoring. The evaluators were blinded to
the experimental grouping and treatment. The total score ranged
from 0–21 points. As presented in Fig.
1, on day 1, none of the rats in the SCI and G-Rb1 groups
scored higher than 2 points, indicating that the spinal cord was
seriously damaged and hind limb motor dysfunction was obvious. On
day 7 the motor function of the hind limbs in the G-Rb1 group was
significantly improved, with higher scores than those in the SCI
group (P<0.05).
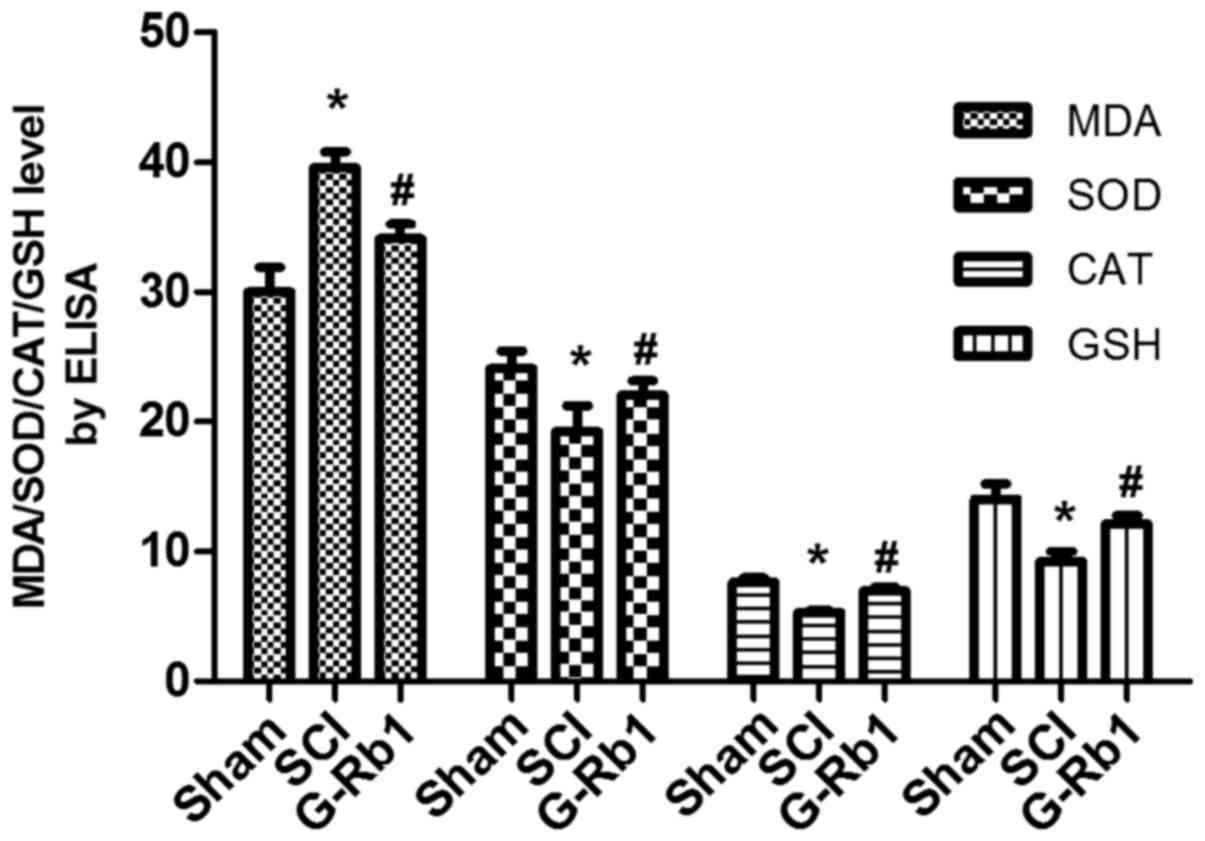
G-Rb1 attenuates SCI-induced changes
in the serum content of SOD, MDA, CAT and GSH
Compared with those in the S group, the levels of
MDA were significantly increased (P<0.05), and the levels of
SOD, CAT and GSH were significantly decreased in the SCI group
(P<0.05). G-Rb1 significantly decreased the levels of MDA, and
increased the levels of SOD, CAT and GSH compared with those in the
SCI group (P<0.05; Fig. 2).
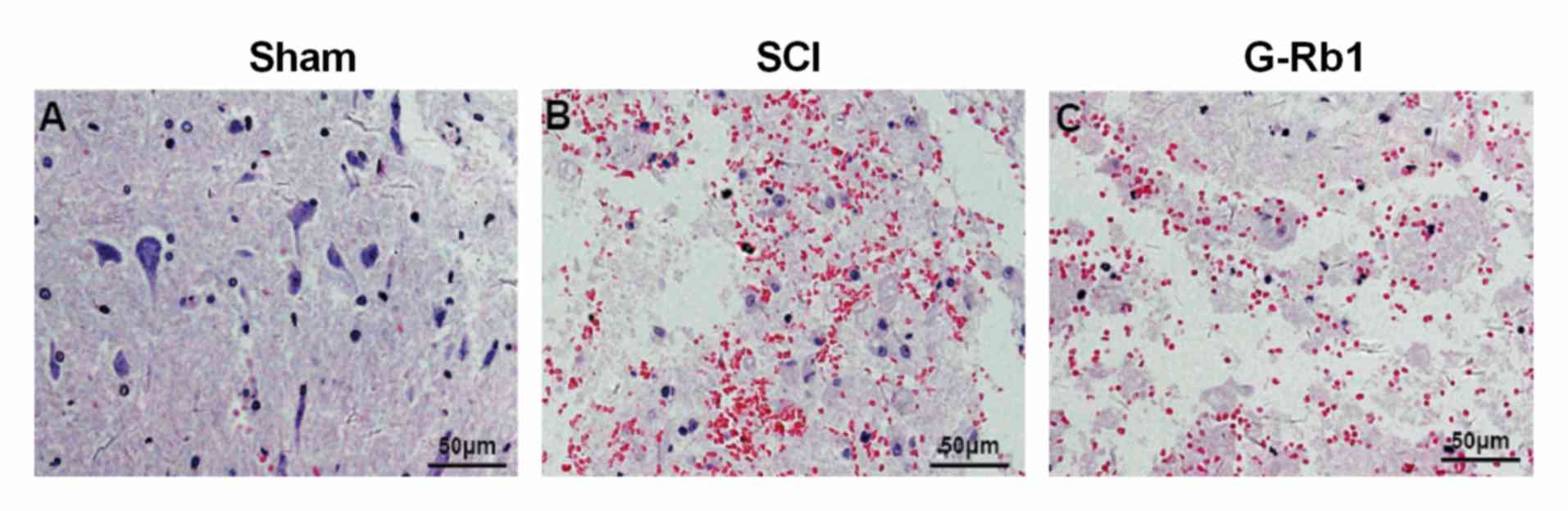
G-Rb1 attenuates SCI-induced
histopathological changes
Compared with the S group, the spinal cord tissue
displayed hemorrhage, neuronal degeneration/necrosis, as well as
mononuclear cell and lymphocyte infiltration in the SCI group. Of
note, G-Rb1 attenuated the hemorrhage, neuronal
degeneration/necrosis, as well as mononuclear cell and lymphocyte
infiltration compared with that in the SCI group (Fig. 3).
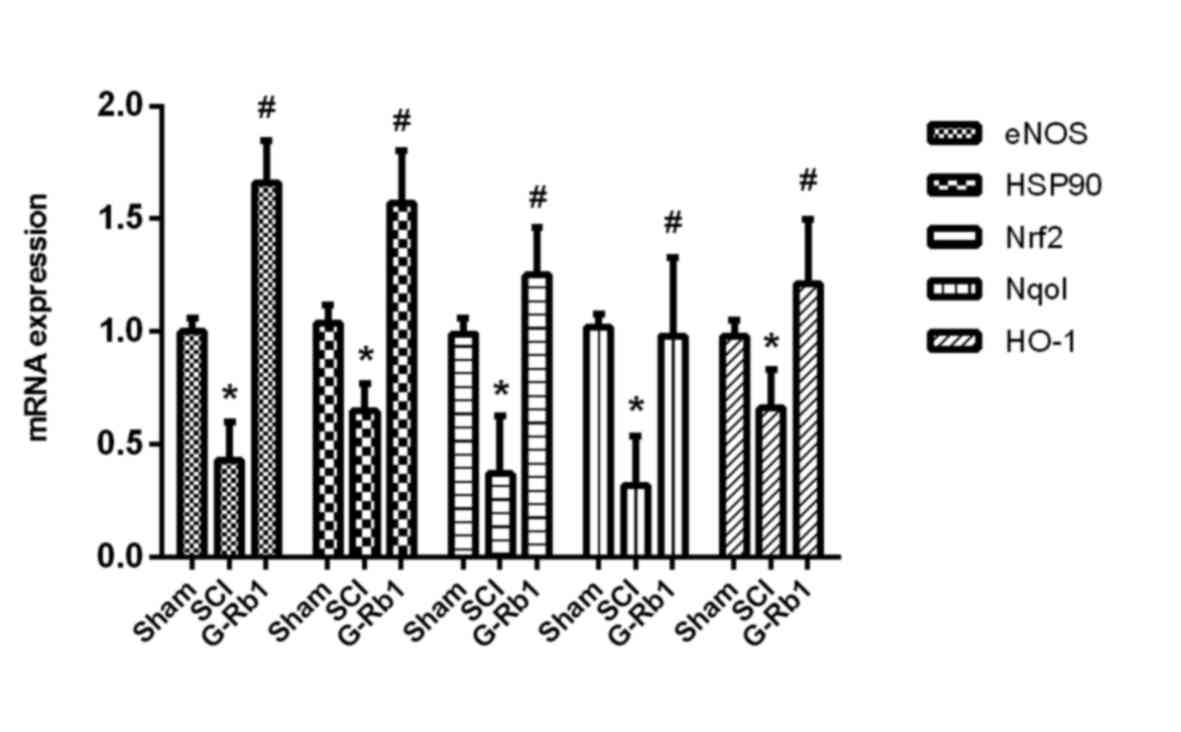
G-Rb1 modulates SCI-induced expression
of NOS, HSP90, Nrf2, Nqo1 and HO-1 mRNA
Compared with that in the S group, the expression of
NOS, HSP90, Nrf2, Nqo1 and HO-1 mRNA in spinal cord tissue of the
SCI group was significantly decreased (P<0.05). However, G-Rb1
significantly increased NOS, HSP90, Nrf2, Nqo1 and HO-1 mRNA
expression levels compared with that in the SCI group (P<0.05;
Fig. 4).
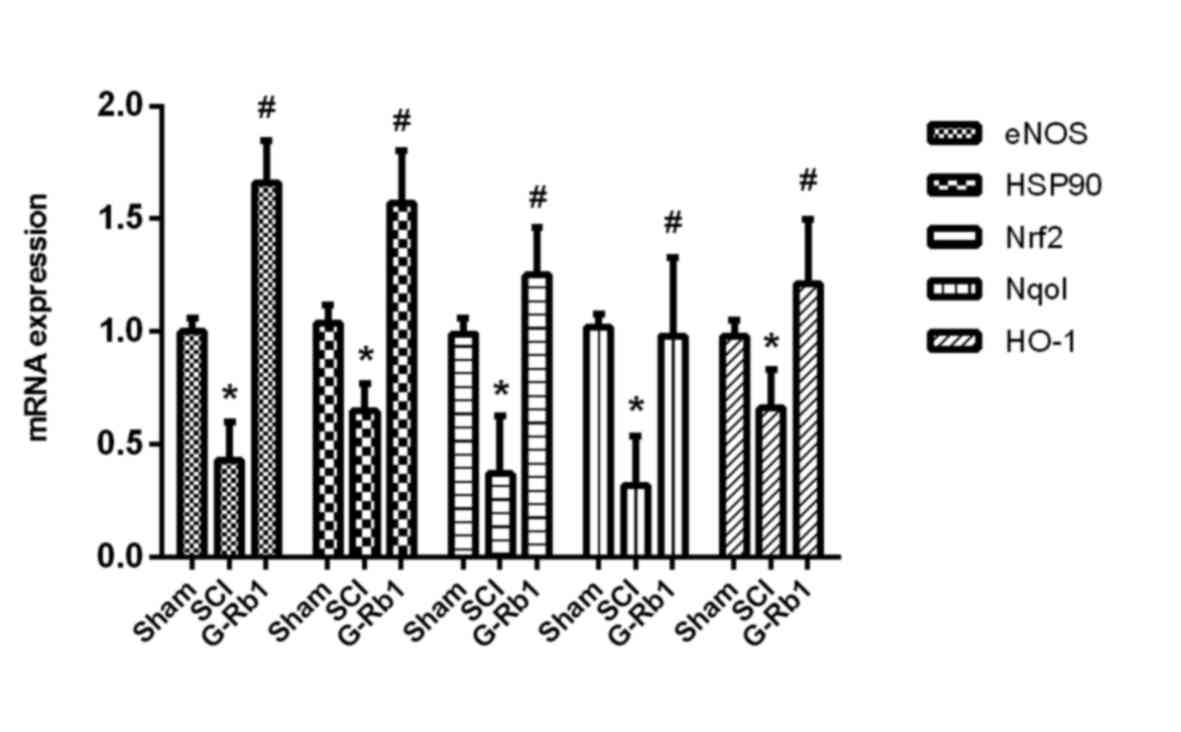 | Figure 4.mRNA expression of eNOS, HSP90, Nrf2,
Nqo1 and HO-1 after ginsenoside Rb1 treatment determined by reverse
transcription-quantitative polymerase chain reaction. *P<0.05
vs. S group; #P<0.05 vs. SCI group. S, sham; SCI,
spinal cord injury; HSP, heat shock protein; HO, heme oxygenase;
eNOS, endothelial nitric oxide synthase; Nrf2, nuclear factor
erythroid 2-related factor 2; G-Rb1, ginsenoside Rb-1; Nqo1,
NAD(P)H quinone dehydrogenase 1. |
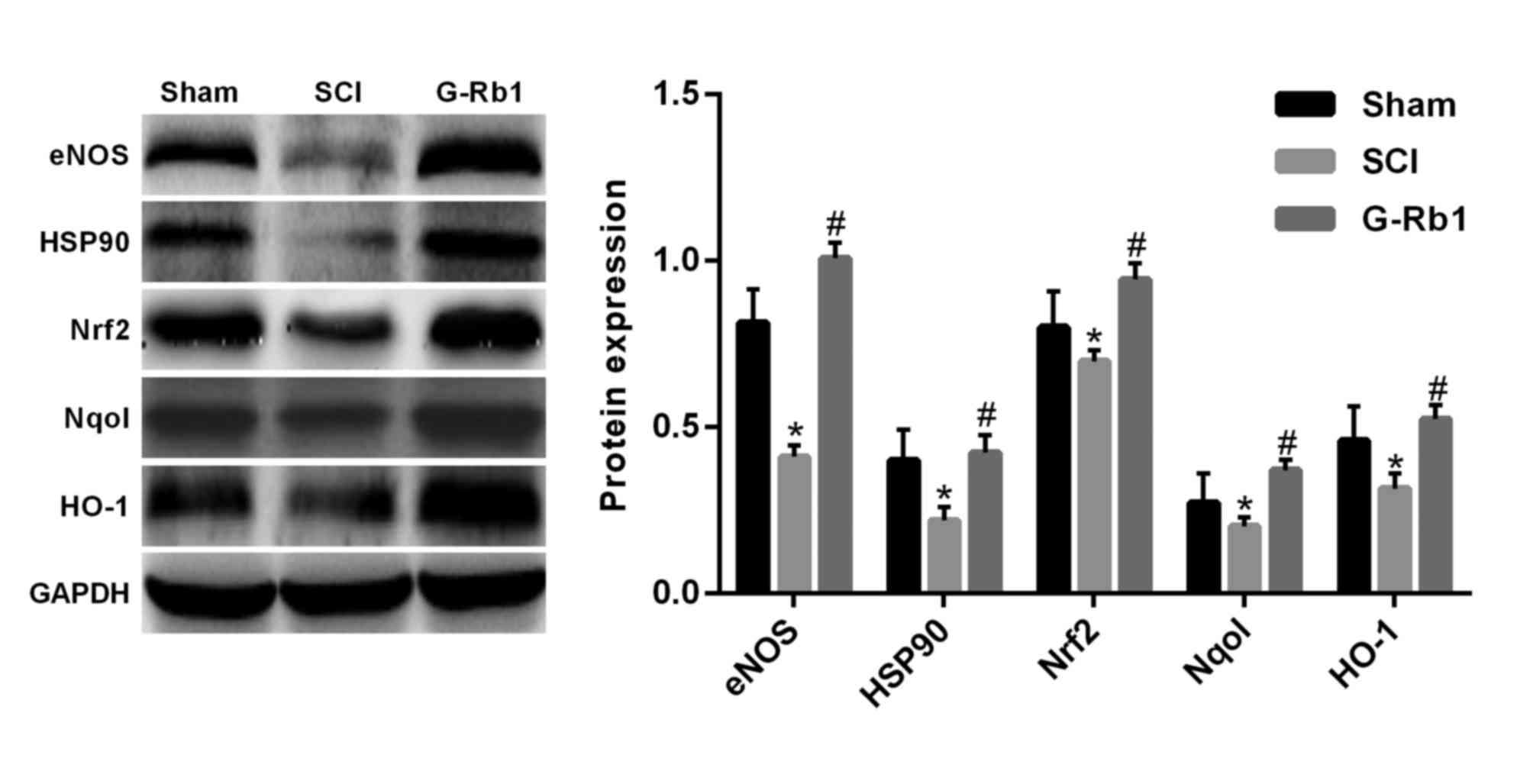
G-Rb1 modulates SCI-induced expression
of NOS, HSP90, Nrf2, Nqo1 and HO-1 protein
Compared with that in the S group, the expression of
eNOS, HSP90, Nrf2, Nqo1 and HO-1 protein in the spinal cord tissue
of the SCI group was significantly decreased (P<0.05); however,
G-Rb1 significantly increased eNOS, HSP90, Nrf2, Nqo1 and HO-1
protein expression in the spinal cord compared with that in the SCI
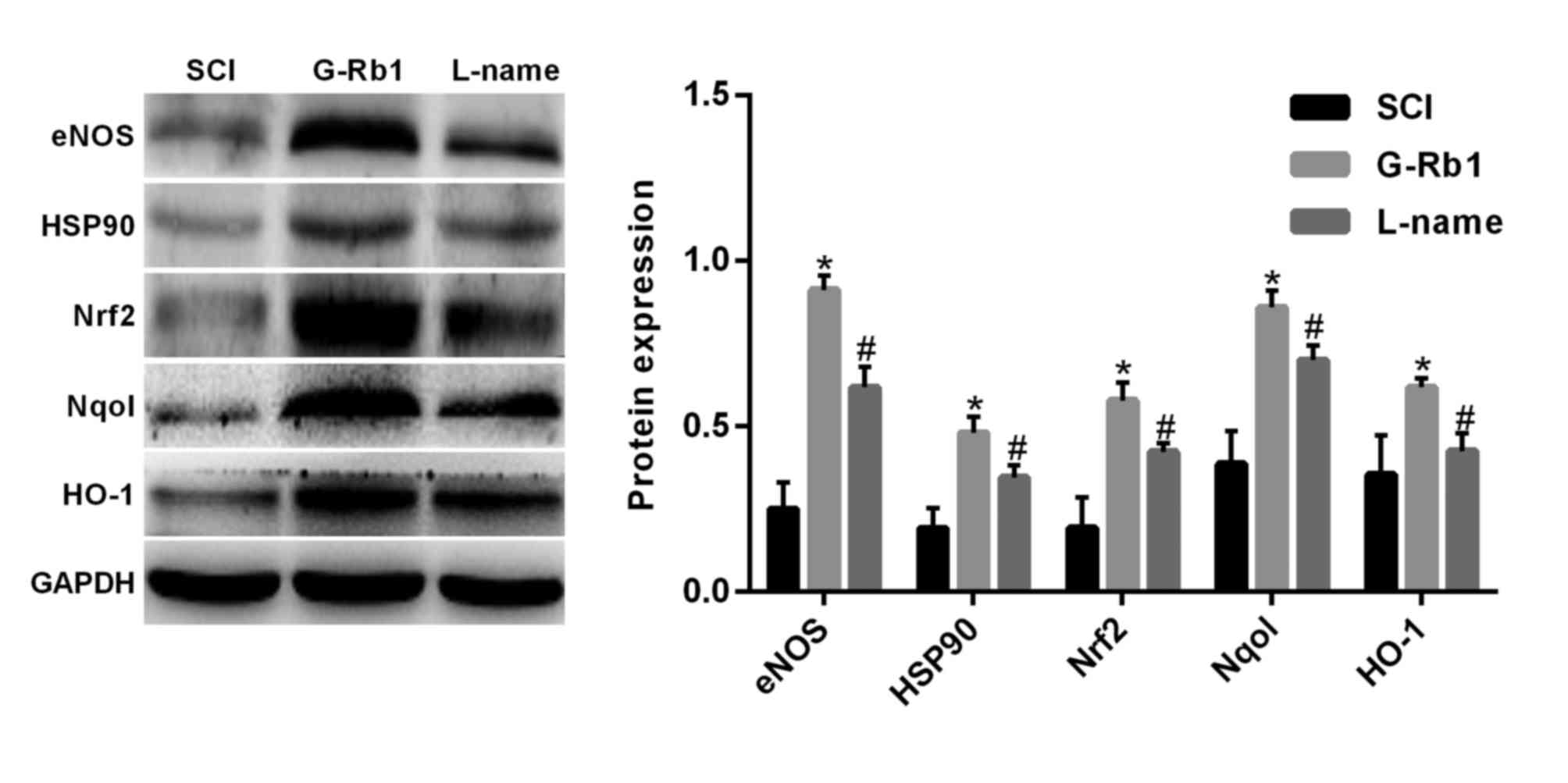
group (P<0.05) (Fig. 5). In order
to further demonstrate that the protective effect of G-Rb1 is
dependent on the eNOS/Nrf2/anti-oxidant response element (ARE)
pathway, rats subjected to SCI and receiving G-Rb1 were injected
with the eNOS inhibitor L-name. The results indicated that in this
L-name group, the expression of HSP90, Nrf2, Nqo1 and HO-1 was
significantly decreased compared with that in the G-Rb1 group
(P<0.05; Fig. 6). These results
may suggest that G-Rb1 attenuates oxidative stress in the spinal
cord via the eNOS/Nrf2/ARE signaling pathway.
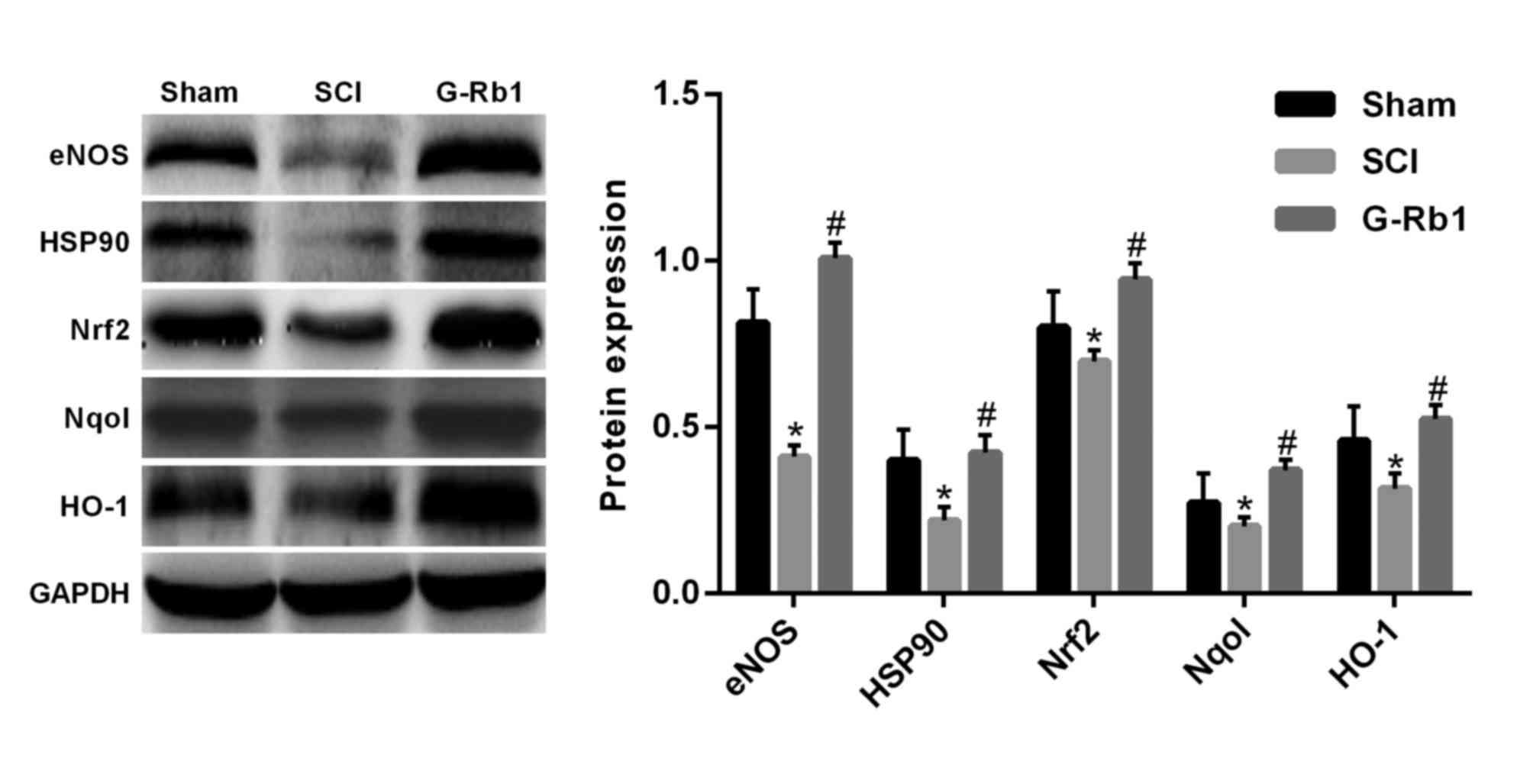 | Figure 5.Expression of eNOS, HSP90, Nrf2, Nqo1
and HO-1 protein determined by western blot analysis. *P<0.05
vs. S group; #P<0.05 vs. SCI group. S, sham; SCI,
spinal cord injury; HSP, heat shock protein; HO, heme oxygenase;
eNOS, endothelial nitric oxide synthase; Nrf2, nuclear factor
erythroid 2-related factor 2; G-Rb1, ginsenoside Rb-1; Nqo1,
NAD(P)H quinone dehydrogenase 1. |
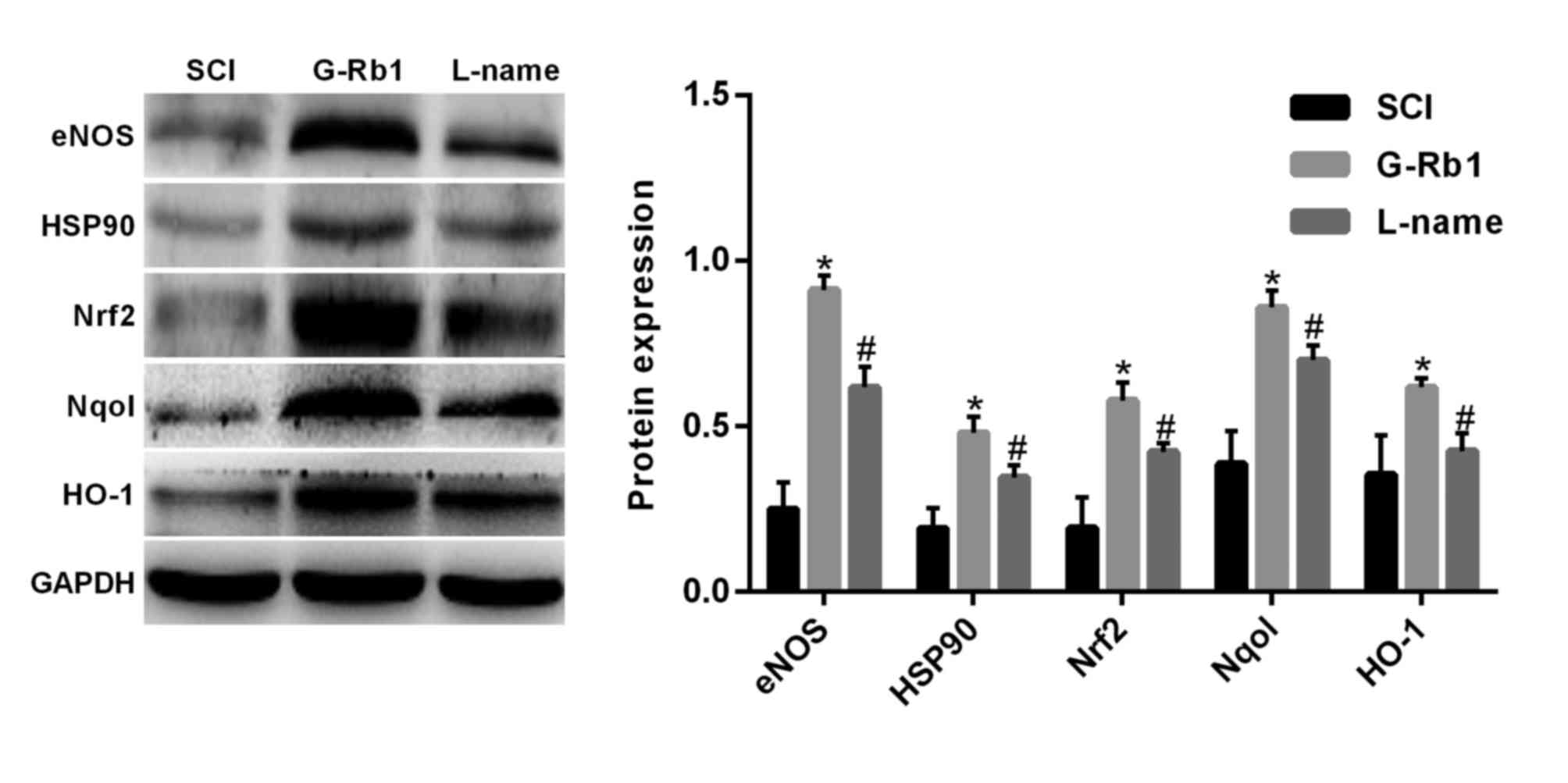 | Figure 6.Effect of L-name on the expression of
eNOS, HSP90, Nrf2, Nqo1 and HO-1 in a rat model of SCI. *P<0.05
vs. S group; #P<0.05 vs. SCI group. S, sham; SCI,
spinal cord injury; HSP, heat shock protein; HO, heme oxygenase;
eNOS, endothelial nitric oxide synthase; Nrf2, nuclear factor
erythroid 2-related factor 2; G-Rb1, ginsenoside Rb-1; Nqo1,
NAD(P)H quinone dehydrogenase 1. |
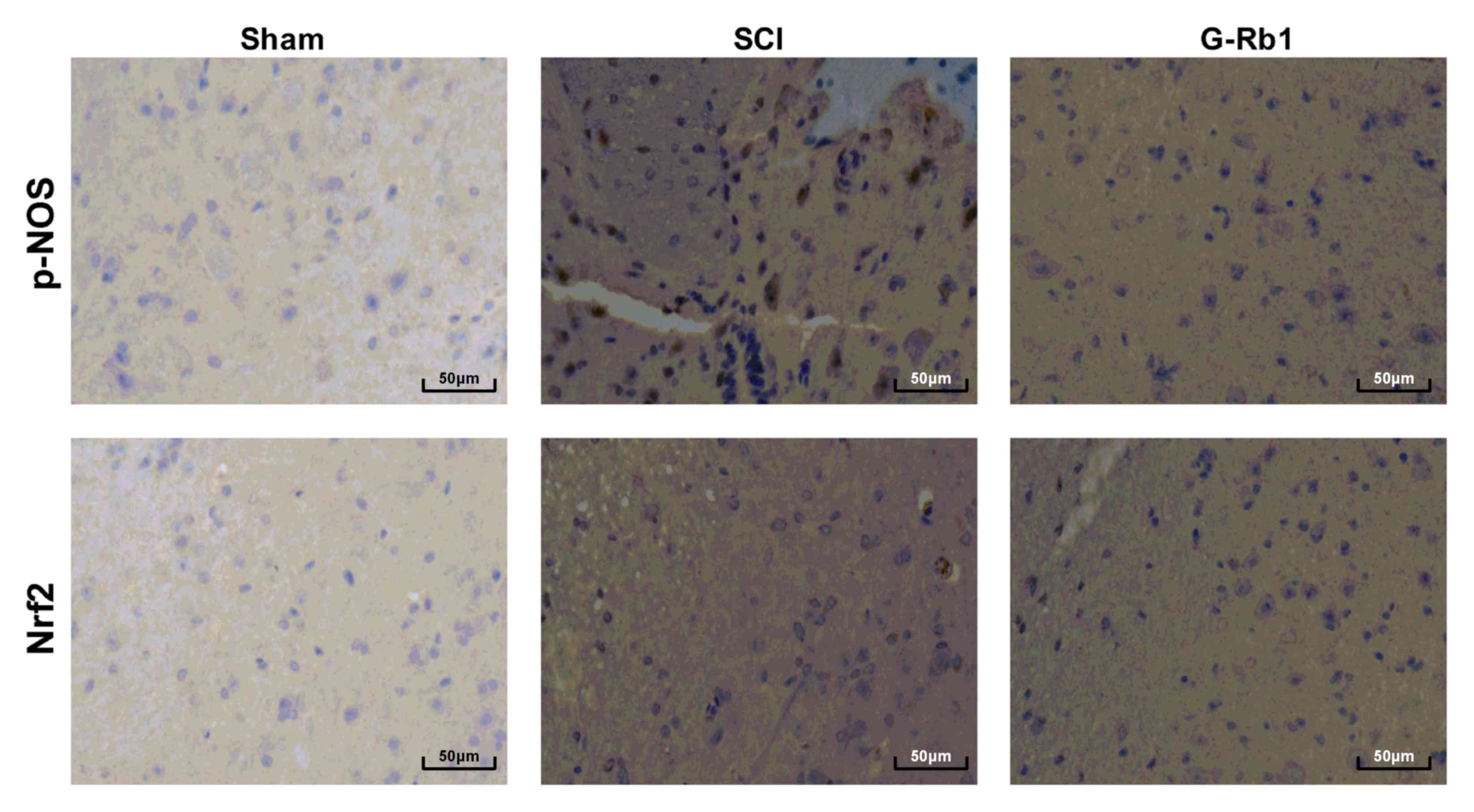
Effect of G-Rb1 on the expression of
p-eNOS and Nrf2 protein post SCI
Immunohistochemical analysis indicated that compared
with that in the S group, the level of p-eNOS in the spinal cord
tissue of the SCI group was notably increased and the level of Nrf2
was notably decreased. Compared with those in the SCI group the
p-eNOS level was markedly increased and the Nrf2 level was markedly
decreased in the G-Rb1 group (Fig.
7).
Discussion
SCI may trigger oxidative stress, change membrane
permeability, and induce lysosomal disintegration and cell
necrosis, resulting in secondary damage to the spinal cord. The
present study indicated that compared with the control group,
spinal cord function scores of SCI rats were significantly
decreased, neuronal degeneration and necrosis were present, the
levels of MDA in serum were significantly increased, SOD, CAT and
GSH protein expression was significantly decreased, and eNOS/Nrf2
protein expression was significantly decreased. Of note, G-Rb1
significantly increased the hind limb function score, reduced the
MDA content, increased SOD, CAT and GSH content, and upregulated
eNOS/Nrf2 protein expression in SCI rats.
MDA is a metabolite of lipid peroxidation, and its
content reflects the degree of lipid peroxidation in vivo,
as well as indirectly reflects the degree of cell damage caused by
oxygen free radicals. SOD and CAT are important anti-oxidant
enzymes, which scavenge oxygen free radicals generated in the
process of tissue and cell metabolism, thus protecting the body
from oxidative stress injury, and their activity indirectly
reflects the anti-oxidant capacity of the body. Therefore, it is
important to monitor the activity of MDA, SOD and CAT in spinal
cord tissue of SCI rats in order to observe their oxidative stress
status (19). In the present study,
the MDA content was significantly increased, while SOD, CAT and GSH
protein expression was significantly decreased, and the levels of
eNOS, p-eNOS, HSP90, Nrf2 and Nqo1 were decreased. In the resting
state, the redox sites of eNOS are occupied by caveolin (CAV)-1 and
eNOS is inactivated; when the cells are stimulated by external
signals, the intracellular Ca2+ concentration increases,
and calmodulin and HSP90 occupy the CAV-1 binding sites on eNOS,
leading to the dissociation of eNOS from CAV-1 and eNOS is
activated (20–22). Nrf2 is an important transcription
factor, which reduces reactive oxygen species and promotes the
body's resistance to harmful external stimuli. Under physiological
conditions, Kelch-like ECH-associated protein 1 (Keap1) in the
cytoplasm is linked to Nrf2 to inactivate it (23–25).
Upregulation of eNOS results in increased nitrosylation of Keap1.
Nrf2 detaches from Keap1 and is thereby activated, and translocates
into the nucleus, where it recognizes and binds to a series of
AREs. As downstream events, ARE then activates the expression of
certain corresponding phase-II detoxification enzyme genes, induces
the expression of SOD, CAT, GSH, leading to the clearance and
metabolism of free radicals (11).
Nqo1 is one of Nrf2-driven downstream target genes that is involved
in anti-oxidant stress injury (26,27).
Activated eNOS regulates the Nrf2/HO-1 signaling pathway, increases
the expression of anti-oxidant enzymes, and reduces the incidence
of cardiovascular disease. Studies have indicated that small doses
of tert-butyl hydroquinone activate Nrf2, upregulate the expression
of anti-oxidant enzymes and regulate oxidative damage of nerve
cells (28,29). In the early stage of fluorosis,
expression of anti-oxidant enzymes, including SOD, CAT and GSH-Px
is upregulated by activation of the Nrf2/HO-1 pathway, enhancing
the ability of cells to resist oxidative stress and reduce the
production of oxygen free radicals (30). Sulforaphane and carnosic acid
contribute to the activation of Nrf2/HO-1, effectively reducing the
binding of 4-hydroxynonenal to mitochondria, and inhibiting
oxidative stress (25). Therefore,
the Nrf2-mediated anti-oxidant response has a crucial role in
functional recovery after SCI (31,32).
The pharmacological effects of ginseng include
regulation of the central nervous system, enhancement of physical
strength, reduction of fatigue and improvement of the metabolism.
G-Rb1 as the major active component of ginseng scavenges oxygen
free radicals, blocks calcium overload in nerve cells, improves
energy metabolism and maintains neuronal cell integrity (33,34). Sun
et al (33) have reported
that after intestinal ischemia-reperfusion, the renal MDA content
in rats was increased and SOD levels were decreased, while G-Rb1
can reduced oxidative stress injury by activating the Nrf2/HO-1
pathway. Hwang et al (34)
have demonstrated that G-Rb1 effectively reduces
6-hydroxydopamine-induced oxidative stress injury in human
dopaminergic cells by activating Nrf2/HO-1. In the present study,
G-Rb1 significantly increased the hind limb function score,
decreased the content of MDA, increased the content of SOD, CAT and
GSH, and enhanced the expression of eNOS, HSP90, Nrf2 and Nqo1
protein in SCI rats. The mechanisms may include scavenging of free
radicals, improvement of anti-oxidant enzyme activity and blocking
of lipid peroxidation to protect cells from oxidative stress
injury, thus maintaining the physiological function of the spinal
cord tissue.
In conclusion, the present study demonstrated that
G-Rb1 significantly increased the hind limb function score,
decreased the MDA content, increased the SOD, CAT and GSH content,
and upregulated eNOS/Nrf2 protein expression in SCI rats, which
exerted an obvious protective effect against oxidative stress
injury, and the underlying mechanism may be associated with the
eNOS/Nrf2/HO-1 pathway.
Acknowledgements
Not applicable.
Funding
This study was supported by the Scientific and
technological project in Liaoning Province (No. 2014225012).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
XL, XG and LX conceived and designed the study,
acquired data, interpreted the results and drafted the manuscript.
LX also contributed to the acquisition of funding and support. XL,
MY, YZ, HY and YW performed the experiments. LX and YX analyzed the
data. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The study was approved by the Experimental Animal
Ethics Committee of the General Hospital of Shenyang Military Area
Command (Shenyang, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Mitchell R, Harvey L, Stanford R and Close
J: Health outcomes and costs of acute traumatic spinal injury in
New South Wales, Australia. Spine J. 2017.(Epub Ahead of Print).
PubMed/NCBI
|
|
2
|
Moshi H, Sundelin G, Sahlen KG and Sorlin
A: Traumatic spinal cord injury in the north-east
Tanzania-describing incidence, etiology and clinical outcomes
retrospectively. Global health Action. 10:13556042017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bothig R, Fiebag K, Thietje R,
Faschingbauer M and Hirschfeld S: Morbidity of urinary tract
infection after urodynamic examination of hospitalized SCI
patients: The impact of bladder management. Spinal Cord. 51:70–73.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pannek J: Editorial Note on: Morbidity of
urinary tract infection after urodynamic examination of
hospitalized SCI patients: The impact of bladder management. Spinal
Cord. Sep 18–2012.(Epub Ahead of Print).
|
|
5
|
Borges TJ, Lang BJ, Lopes RL and Bonorino
C: Modulation of alloimmunity by heat shock proteins. Front
Immunol. 7:3032016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ren J, Fan C, Chen N, Huang J and Yang Q:
Resveratrol pretreatment attenuates cerebral ischemic injury by
upregulating expression of transcription factor Nrf2 and HO-1 in
rats. Neurochem Res. 36:2352–2362. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Chini MG, Malafronte N, Vaccaro MC,
Gualtieri MJ, Vassallo A, Vasaturo M, Castellano S, Milite C, Leone
A, Bifulco G, et al: Identification of limonol derivatives as heat
shock protein 90 (Hsp90) Inhibitors through a multidisciplinary
approach. Chemistry. 22:13236–13250. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Dong X, Zheng L, Lu S and Yang Y:
Neuroprotective effects of pretreatment of ginsenoside Rb1 on
severe cerebral ischemia-induced injuries in aged mice: Involvement
of anti-oxidant signaling. Geriatr Gerontol Int. 17:338–345. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Chen W, Guo Y, Yang W, Zheng P, Zeng J and
Tong W: Involvement of connexin40 in the protective effects of
ginsenoside Rb1 against traumatic brain injury. Cell Mol Neurobiol.
36:1057–1065. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cheng W, Wu D, Zuo Q, Wang Z and Fan W:
Ginsenoside Rb1 prevents interleukin-1 beta induced inflammation
and apoptosis in human articular chondrocytes. Int Orthop.
37:2065–2070. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Liu DH, Chen YM, Liu Y, Hao BS, Zhou B, Wu
L, Wang M, Chen L, Wu WK and Qian XX: Rb1 protects endothelial
cells from hydrogen peroxide-induced cell senescence by modulating
redox status. Biol Pharm Bull. 34:1072–1077. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Gurcan O, Gurcay AG, Kazanci A, Senturk S,
Bodur E, Karaca EU, Turkoglu OF and Bavbek M: Effect of asiatic
acid on the treatment of spinal cord injury: An Experimental study
in rats. Turk Neurosurg. 27:259–264. 2017.PubMed/NCBI
|
|
13
|
Mo YP, Yao HJ, Lv W, Song LY, Song HT,
Yuan XC, Mao YQ, Jing QK, Shi SH and Li ZG: Effects of
electroacupuncture at governor vessel acupoints on neurotrophin-3
in rats with experimental spinal cord injury. Neural Plast.
2016:23718752016. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Armstrong HK, Koay YC, Irani S, Das R and
Nassar ZD: Australian Prostate Cancer BioResource, Selth LA,
Centenera MM, McAlpine SR and Butler LM: A novel class of Hsp90
C-terminal modulators have pre-clinical efficacy in prostate tumor
cells without induction of a heat shock response. Prostate.
76:1546–1559. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Allen AR: Surgery of experimental lesion
of spinal cord equivalent to crush injury of fracture dislocation
of spinal column. J American Med Asso lvii. 878–880. 1962.
|
|
16
|
Allen AR and Reginald A: Remarks on the
histopathological changes in the spinal cord due to impact. An
experimental study. J Nervous Mental Dis. 41:141–147. 1914.
View Article : Google Scholar
|
|
17
|
Basso DM, Beattie MS and Bresnahan JC: A
sensitive and reliable locomotor rating scale for open field
testing in rats. J Neurotrauma. 12:1–21. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Oh JH, Hyun JY and Varshavsky A: Control
of Hsp90 chaperone and its clients by N-terminal acetylation and
the N-end rule pathway. Proc Natl Acad Sci USA. 114:E4370–E4379.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Krzemien-Ojak L, Goral A, Joachimiak E,
Filipek A and Fabczak H: Interaction of a novel chaperone PhLP2A
with the heat shock protein Hsp90. J Cell Biochem. 118:420–429.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Bryan HK, Olayanju A, Goldring CE and Park
BK: The Nrf2 cell defence pathway: Keap1-dependent and -independent
mechanisms of regulation. Biochem Pharmacol. 85:705–717. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kang CH, Kim MJ, Seo MJ, Choi YH, Jo WS,
Lee KT, Jeong YK and Kim GY:
5-Hydroxy-3,6,7,8,3′4′-hexamethoxyflavone inhibits nitric oxide
production in lipopolysaccharide-stimulated BV2 microglia via NF-κB
suppression and Nrf-2-dependent heme oxygenase-1 induction. Food
Chem Toxicol. 57:119–125. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Terazawa R, Akimoto N, Kato T, Itoh T,
Fujita Y, Hamada N, Deguchi T, Iinuma M, Noda M, Nozawa Y and Ito
M: A kavalactone derivative inhibits lipopolysaccharide-stimulated
iNOS induction and NO production through activation of Nrf2
signaling in BV2 microglial cells. Pharmacol Res. 71:34–43. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kim HJ, Zheng M, Kim SK, Cho JJ, Shin CH,
Joe Y and Chung HT: CO/HO-1 induces NQO-1 expression via Nrf2
activation. Immune Netw. 11:376–382. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Li WC, Jiang DM, Hu N, Qi XT, Qiao B and
Luo XJ: Lipopolysaccharide preconditioning attenuates
neuroapoptosis and improves functional recovery through activation
of Nrf2 in traumatic spinal cord injury rats. Int J Neurosci.
123:240–247. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Li J, Johnson D, Calkins M, Wright L,
Svendsen C and Johnson J: Stabilization of Nrf2 by tBHQ confers
protection against oxidative stress-induced cell death in human
neural stem cells. Toxicol Sci. 83:313–328. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Rubiolo JA, Mithieux G and Vega FV:
Resveratrol protects primary rat hepatocytes against oxidative
stress damage: Activation of the Nrf2 transcription factor and
augmented activities of antioxidant enzymes. Eur J Pharmacol.
591:66–72. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zhang J, Zhang Y, Liang C, Wang N, Zheng H
and Wang J: Choline supplementation alleviates fluoride-induced
testicular toxicity by restoring the NGF and MEK expression in
mice. Toxicol Appl Pharmacol. 310:205–214. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Miller DM, Singh IN, Wang JA and Hall ED:
Administration of the Nrf2-ARE activators sulforaphane and carnosic
acid attenuates 4-hydroxy-2-nonenal-induced mitochondrial
dysfunction ex vivo. Free Radic Biol Med. 57:1–9. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Duan W, Zhang R, Guo Y, Jiang Y, Huang Y,
Jiang H and Li C: Nrf2 activity is lost in the spinal cord and its
astrocytes of aged mice. In Vitro Cell Dev Biol Anim. 45:388–397.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ohashi R, Yan S, Mu H, Chai H, Yao Q, Lin
PH and Chen C: Effects of homocysteine and ginsenoside Rb1 on
endothelial proliferation and superoxide anion production. J Surg
Res. 133:89–94. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Xie XS, Liu HC, Yang M, Zuo C, Deng Y and
Fan JM: Ginsenoside Rb1, a panoxadiol saponin against oxidative
damage and renal interstitial fibrosis in rats with unilateral
ureteral obstruction. Chin J Integr Med. 15:133–140. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Sun Q, Meng QT, Jiang Y and Xia ZY:
Ginsenoside Rb1 attenuates intestinal ischemia reperfusion induced
renal injury by activating Nrf2/ARE pathway. Molecules.
17:7195–7205. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Hwang YP and Jeong HG: Ginsenoside Rb1
protects against 6-hydroxydopamine-induced oxidative stress by
increasing heme oxygenase-1 expression through an estrogen
receptor-related PI3K/Akt/Nrf2-dependent pathway in human
dopaminergic cells. Toxicol Appl Pharmacol. 242:18–28. 2010.
View Article : Google Scholar : PubMed/NCBI
|