Introduction
Congenital heart disease (CHD) is the most common
birth defect, affecting ~0.8% of live births worldwide (1,2). The
true incidence of CHD in China was ~11.1 per 1,000 live births,
which is higher than previously reported (3). Due to the an increasing absolute and
relative survival in children and young adults with CHD, brain
injury, as a potentially devastating complication of CHD, has
attracted increasing attention from neurologists and parents
(4). With improved surgical outcomes
and survival rates, children with CHD exhibit an increased risk of
developing neurodevelopmental deficits, which are characterized by
mild cognitive dysfunction, social interaction problems and
difficulties in core communication (4). Cognitive and global motor developments
of infants and children can be evaluated using the Bayley test,
which a reliable and widely applied test for growth restriction in
children aged 12 months (5). This
test was first described in 1969 by Bayley (6), and revised and standardized for the
Chinese population in 1993(7).
Amplitude-integrated electroencephalography (aEEG)
is used to identify seizures and abnormalities in the background
cerebral activity of infants in Neonatal Intensive Care Units
(NICU) (8). Continuous
electroencephalography (EEG) provides an image of the brain's
surface electrical activity and is a time-sensitive method of
detecting brain injury. For continuous bedside monitoring and
time-compressed background patterns, aEEG is a simpler and more
convenient tool that is used in the NICU for the assessment of
brain function in high-risk neonates, compared with a regular EEG
(9). In hypoxic ischemic
encephalopathy (HIE) and preterm infants, aEEG is helpful for
predicting the short-term outcome (10), as a continuous bedside monitor that
can indicate the abnormalities in cerebral activity immediately
(11). Additionally, aEEG is a
non-invasive and accurate approach that can assess
neurodevelopmental maturation and brain injuries in premature
infants, or in infants exhibiting cardiac arrest, extracorporeal
membrane oxygenation (ECMO) and ligation of patent ductus
arteriosus. A perioperative aEEG may be used as a tool to predict
clinical outcomes in infants undergoing heart surgery for CHD
(12). However, the role of aEEG in
the prediction of the outcomes of patients with CHD, following
surgery, remains largely undetermined. The current study aimed to
determine the effect of perioperative aEEG on neurodevelopmental
outcomes in infants with CHD.
Patients and methods
Patients
A retrospective cohort of 93 consecutively enrolled
infants (50 males, 43 females), born with CHD were enrolled in the
current study from Guangdong Provincial People's Hospital between
September 2015 and January 2017. For infants >3 months of age,
surgery is difficult and perioperative hemodynamics fluctuates
greatly. Additionally, the immune system is not fully developed
prior to 3 months of age. Therefore, infants are prone to infection
following cardiac surgery. The brain of infants prior to the age of
3 months is vulnerable to ischemia and hypoxia. Therefore, children
with CHD exhibit improved surgical outcomes, lower infection rates
and higher survival rates within 3 months after birth. Infants with
a genetic comorbidity or suspected syndromic disorder were excluded
from the current study (13). All
demographic, perioperative and cardiac measurements were collected
retrospectively from each patient. The ethnicity of the patient's
family and the family socioeconomic status were assessed. The
current study was approved by the ethical committee of Guangdong
Provincial People's Hospital, and written informed consent was
obtained from all parents.
Grouping
Grouping patients by the type of CHD is generally
accepted in the study of CHD development (12) or the analysis of the factors
influencing neurodevelopment, patients were classified according to
surgical factors, including surgery with or without orthopedic
surgery and palliative surgery, immediate thoracic closure
following surgery and delayed thoracic closure following surgery,
which is not a common grouping used in other randomized controlled
trial studies (grouping was based on disease classification and
surgical details).
Clinical characteristics
Patient data included gestational age, birth weight,
Apgar scores (14), cardiovascular
function, respiratory and multi-organ failure, neurologic
examination and neuroimaging data. The following information was
recorded in the current study: Period and method of surgery,
cardiopulmonary bypass time and aortic cross-clamping time. Simple
and complex CHD was categorized depending on Risk Adjustment in
Congenital Heart Surgery-1 (15,16),
which determined category 1 as simple CHD.
aEEG measurements
aEEG was monitored for 24 h prior to cardiac surgery
using an 8-channel EEG (NicoletOne monitor; CareFusion Corp;
Becton-Dickinson and Company). A total of 8 disposable,
self-adhesive, EEG scalp electrodes (Blue Sensor BRS-50 K AmbuTM
ECG electrode; Medicotest A/S) were used in a reduced montage
following the international 10-20 system (17). The clinician that performed the main
offline aEEG analyses was not involved in clinical care of the
patients. The 8-channel cross-brain aEEG trace was derived and
displayed at 6 cm/h on paper using a semi logarithmic scale to
assess and classify the aEEG background pattern. The channels were
also used to record EEG data to describe episodes of EEG seizures
in 10 sec epochs.
The interpretation of aEEG
aEEG is commonly used to evaluate background
pattern, seizure activity and sleep-wake cycles (18). aEEG traces were classified using
background voltage (19) and a
descriptive pattern. The aEEG recordings were categorized as 5
background patterns which were continuous normal voltage (CNV),
discontinuous normal voltage (DNV), or a combined third group of
the severe aEEG voltage pattern (SEVP), including burst suppression
(BS), continuous low voltage (CLV) or a flat trace (FT). For
outcome analysis, the 5 background patterns was categorized into
normal (CNV), mild abnormal (DNV transient and persistent) and
severely abnormal (BS, CLV and FT) (20). Sleep-wake cycling (SWC) refers to the
cyclic fluctuation in the amplitude and degree of discontinuity as
the neonate enters various stages of sleep or wakefulness (21). On the aEEG, SWC is reflected by the
presence of smooth sinusoidal variation, mostly in the minimal
amplitude. Periods of wider bandwidth represent discontinuous
activity during quiet sleep, whereas periods with a narrow
bandwidth represent more continuous activity when awake or during
active sleep (18). SWC was
categorized by occurrence: Absent, immature or developed (18). An electrographic seizure was defined
as an evolving repetitive stereotyped waveform, with a definite
onset, a peak and an end that lasted for ≥10 sec on raw EEG data
(18). Antiepileptic drugs
(Midazolam and Phenobarbital) were used to treat clinical seizures.
The results of continuous aEEG/EEG monitoring were examined
following patient discharge, by an external collaborator.
Electrographic seizure activity (EA) was divided into the following
groups: i) No seizure; ii) a single seizure (SS), in which the
amplitude of a single waveform appeared suddenly and showed
persistent cerebral cortex activity; iii) recurrent seizure (RS),
in which a recurring amplitude indicated sudden and persistent
cerebral cortex activity. All patient reports were examined by a
neonatal neurological expert who was blinded from the patients'
diagnosis.
Surgical management
Cardiac surgery was performed by one group of
cardiac surgeons. The alphastat blood gas management was routinely
performed. In the majority of cardiac surgeries, normothermic or
mild hypothermic cardiopulmonary bypass (rectal temperature
>32˚C or 28-32˚C, respectively) was performed with a pump flow
rate of 100-150 ml/kg/min to achieve a mean arterial pressure of
40-50 mmHg (22,23). During arch repair, antegrade cerebral
perfusion, with a pump flow rate of -50 ml/kg/min was used, and the
mean arterial pressures were targeted at -40-50 mm Hg and were
measured in the right radial artery. Modified ultra-filtrations
were performed in all patients. Following surgery, patients
received milrinon (0.5-1 µg/kg/min) as an early postoperative
treatment combined with noradrenaline (0.05-1 µg/kg/min) and/or
adrenaline (0.01-0.5 µg/kg/min) to treat cardiac failure.
Postoperative analgesia included fentanyl (1-3 µg/kg/h within 3
days after surgery). Patients were given a Paracetamol drip, which
exhibits a smaller influence on the aEEG compared with intravenous
sedative/pain medications, to control pain when patients did not
require ventilation.
Follow-up
All 93 infants received a follow-up (at 6 months, 1
year, 1 a half years and 2 years) at the Child Development Clinic
of the Guangdong Provincial People's Hospital. At 1 year of age,
the Bayley Scales of Infant Development was used to provide a
mental development index (MDI) and psychomotor developmental index
(PDI). Cognitive and global motor development were evaluated using
the Bayley test, as previously described (6). The Bayley composite test scores are
scaled over a range of 50-150, with a mean of 100 and a standard
deviation (SD) of 16(7). Although
not considered to be an intelligence quotient test, the Bayley test
reliably identifies infants with developmental delays, as indicated
by scores of <68 (mean-2SD) on the cognitive or the global motor
composite scores. Tests were performed by one clinician who was
experienced in testing child development and was blinded to the
patients' diagnosis and surgical details.
Statistical analysis
Data were processed using SPSS 16.0 (SPSS, Inc.)
software and presented as the mean ± SD. Comparisons between groups
were performed using a student t-test and Bonferroni correction.
Variance analysis or a signed-rank test was used for comparison of
continuous variables and a χ2 test or Fisher's exact
test for dichotomous variables. Comparisons with the grade data
were performed using a Wilcoxon signed-rank test. Multiple linear
regression analysis was used to determine the influencing factors
of MDI and PDI. The β value or the regression coefficient, was
applied for regression analysis. β>0, indicated a positive
association between strain and independent variable, and β<0,
indicated a negative association. The inspection standard was
bilateral 0.05. P<0.05 was considered to indicate a
statistically significant difference.
Results
Clinical characteristics of
infants
The characteristics of patients are presented in
Table I. A total of 16 infants were
born at <37 weeks of gestation (27-36.6 weeks) and surgery in
these children was performed at term equivalent (>37 weeks of
gestation). Cardiac diagnoses were divided into four diagnostic
groups according to Clancy et al (24) (Table
II). A total of 5 children had >1 bypass surgery by the age
of 1 years old.
 | Table IPatient characteristics (n=93). |
Table I
Patient characteristics (n=93).
|
Characteristics | Value |
|---|
| Male sex, n
(%) | 50 (53.8%) |
| Gestational age
(weeks) | 38.18±2.799 |
| Birth weight
(g) |
2779.60±662.650 |
| Cyanotic CHD, n
(%) | 46 (49.5) |
| Complex CHD, n
(%) | 58 (62.4) |
| Age at surgery
(months) | 1.56±1.373 |
| Duration of
intensive care stay (day) | 27.31±12.319 |
| Emergency operation
(%) | 14 (15.05) |
| Corrective surgery
(%) | 88 (94.62) |
| CPB (min) | 114.11±68.545 |
| Aortic clamp time
(min) | 66.949±42.759 |
| Delayed sternal
closured (%) | 27 (29.03) |
| Mechanical
ventilation (day) | 8.022±8.106 |
 | Table IICardiac diagnoses and cardiac
class. |
Table II
Cardiac diagnoses and cardiac
class.
| Cardiac
diagnoses | Overall (n=93) | Class I (n=68) | Class II
(n=10) | Class III
(n=13) | Class IV (n=2) |
|---|
| TGA/IVS | 8 | 8 | 0 | 0 | 0 |
| TGA/VSD | 12 | 12 | 0 | 0 | 0 |
| TOF | 1 | 1 | 0 | 0 | 0 |
| TOF/PA | 1 | 0 | 0 | 1 | 0 |
| TAPVC | 9 | 9 | 0 | 0 | 0 |
| VSD without
IAA/coarctation | 30 | 30 | 0 | 0 | 0 |
| VSD with
IAA/coarctation | 10 | 0 | 10 | 0 | 0 |
| AVC defect | 0 | 0 | 0 | 0 | 0 |
| HLHS | 1 | 0 | 0 | 0 | 1 |
| Other functional
single ventricle | 13 | 0 | 0 | 12 | 1 |
| Other | 8 | 8 | 0 | 0 | 0 |
aEEG characteristics of the infants
with CHD preoperatively and postoperatively
A total of 45 infants were monitored using aEEG
preoperatively and 79 were monitored postoperatively. A total of 31
infants underwent preoperative and postoperative aEEG. The aEEG
results are presented in Table
III. Preoperatively, 82.2% infants indicated CNV (n=37) and
17.8% infants indicated DNV (n=8). A total of 2 infants exhibited
seizure activity on the aEEG. A total of 3 infants with
preoperative SS were found without postoperative seizure.
Postoperatively, discontinuous normal voltage was detected in 5
(6.3%) infants, and continuous normal voltage was detected in 74
(93.7%) infants. A total of 3 infants exhibited seizure activity on
the postoperative aEEG without seizure activity on the preoperative
aEEG. One of the 3 infants also had symptomatic seizures and was
treated with phenobarbital (10 mg/kg/day) and the magnetic
resonance imaging was normal (Table
III).
 | Table IIIPreoperative and postoperative aEEG
characteristics of infants with CHD (n=93). |
Table III
Preoperative and postoperative aEEG
characteristics of infants with CHD (n=93).
|
Characteristics | Preoperative
(n=45) | Postoperative
(n=79) |
|---|
| Background n
(%) |
|
Normal | 37 (82.2) | 74 (93.7) |
|
Mild
abnormal | 8 (17.8) | 5 (6.3) |
|
Severe
abnormal | 0 (0) | 0 (0) |
| SWC n (%) | | |
|
Developed | 9(20) | 35 (44.3) |
|
Immature | 34 (75.6) | 41 (51.9) |
|
Absent | 2 (4.4) | 3 (3.8) |
| Seizure n (%) | | |
|
No | 43 (95.6) | 76 (96.2) |
|
SS | 1 (2.2) | 2 (2.5) |
|
RS | 1 (2.2) | 1 (1.3) |
MDI and PDI in infants with CHD
All 93 infants were examined at the mean age of
10.54 months. The mean MDI was 96.483±21.997, and PDI was
87.763±21.584 (data not shown). PDI was significantly lower than
the normal values of 100 (P<0.001), with no significant
differences observed for MDI (P=0.127) (Table IV). The mean of MDI and PDI in
cyanotic CHD was compared with acyanotic CHD (MDI, 93.00±21.422 vs.
99.89±22.244; PDI, 84.50±20.397 vs. 90.96±22.443, data not shown).
The mean of MDI and PDI was lower compared with complex and simple
CHD (MDI, 94.45±20.649 vs. 99.86±23.993; PDI, 86.81±19.617 vs.
89.34±24.725, data not shown). However, the differences were not
statistically significant.
 | Table IVMDI and PDI in infants with CHD and
the average of the normal population (100). The BSID (Chinese City)
was standardized in 15 cities and defined normal value in general
population was 100(9). |
Table IV
MDI and PDI in infants with CHD and
the average of the normal population (100). The BSID (Chinese City)
was standardized in 15 cities and defined normal value in general
population was 100(9).
| | 95% CI of the
difference |
|---|
| | t | df | P-value | Mean
difference | Lower | Upper |
|---|
| MDI | -1.542 | 92 | 0.127 | -3.51613 | -8.0463 | 1.0141 |
| PDI | -5.467 | 92 |
<0.001a | -12.23656 | -16.6818 | -7.7913 |
Risk factors for abnormal MDI and
PDI
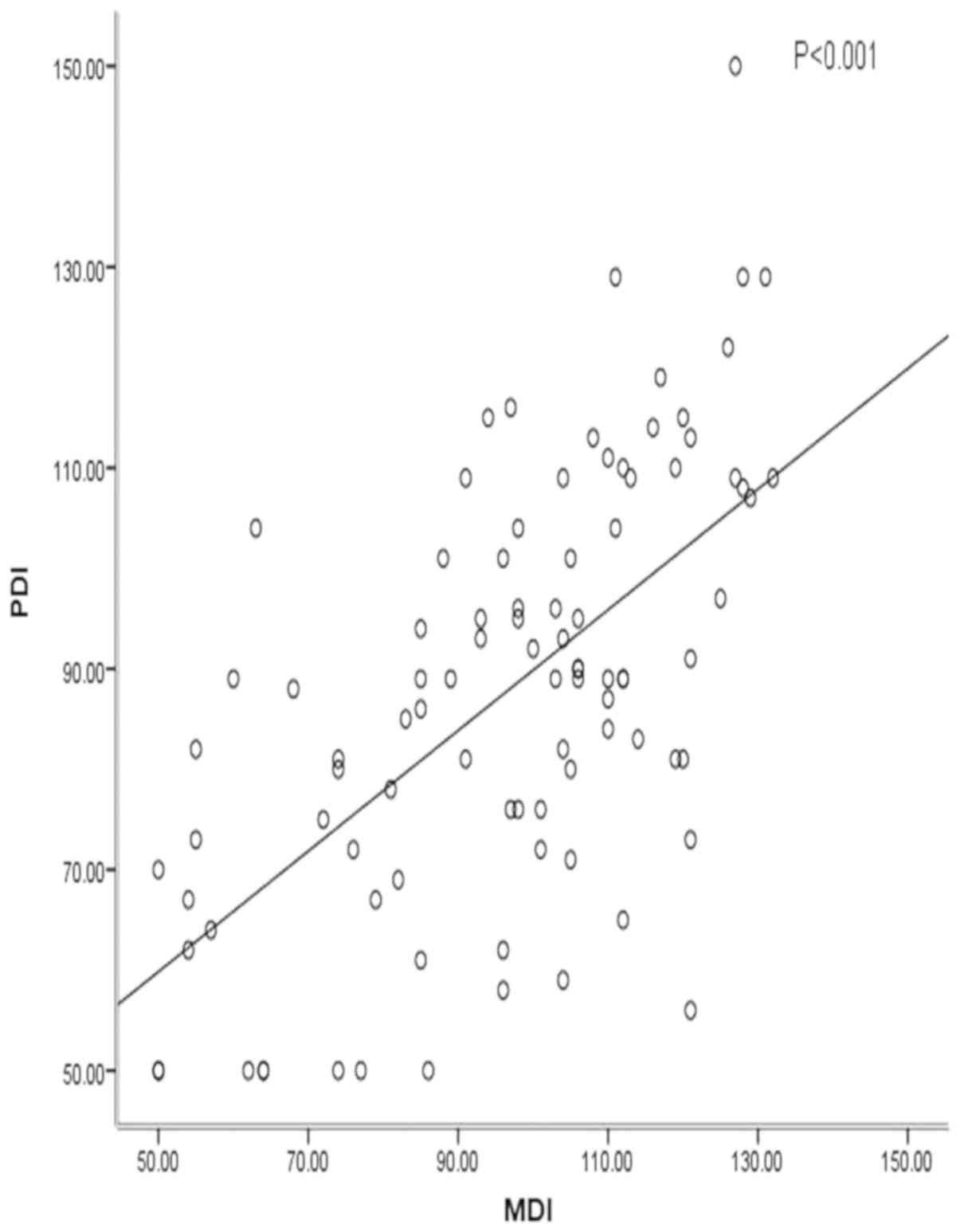
According to univariate linear regression and
multivariate linear regression, the results demonstrated a positive
linear association between PDI and MDI (β=0.929; 95% CI: Lower,
0.556; upper, 1.301; Fig. 1;
Table V). A negative linear
association between length of intensive care stay and PDI was
observed (β=-0.577; 95% CI: Lower, -0.874; upper, -0.279; Table VI), and CPB was the protective
factor of PDI (β=11.956; 95% CI: Lower, 0.845; upper, 23.068;
Table VI). The PDI of surgery with
CPB was significantly higher than that of surgery without CPB
(P=0.035; data not shown). The PDI of infants with mild behavioral
problems was significantly lower compared with infants exhibiting
no behavioral problems (β=-10.605; 95% CI: Lower, -18.546; upper,
-2.664; P=0.01; Table VI).
 | Table VMultivariate linear regression
analysis of the influencing factors of MDI. |
Table V
Multivariate linear regression
analysis of the influencing factors of MDI.
| | 95% CI of
regression coefficient |
|---|
| Influencing
factor | β | t | P-value | Lower | Upper |
|---|
| PDI | 0.929 | 5.261 |
<0.001a | 0.556 | 1.301 |
| Cyanotic CHD | 17.218 | 2.385 | 0.029a | 1.984 | 32.451 |
 | Table VIMultivariate linear regression
analysis of influencing factors of PDI. |
Table VI
Multivariate linear regression
analysis of influencing factors of PDI.
| | 95% CI of
regression coefficient |
|---|
| Influencing
factor | β | t | P-value | Lower | Upper |
|---|
| MDI | 0.497 | 6.397 |
<0.001a | 0.342 | 0.652 |
| Length of ICU | -0.577 | -3.861 |
<0.001a | -0.874 | -0.279 |
| Surgery with
CPB | 11.956 | 2.142 | 0.035a | 0.845 | 23.068 |
| Mild behavioral
problem | -10.605 | -2.658 | 0.01a | -18.546 | -2.664 |
| Severe behavioral
problem | -4.784 | -0.645 | 0.521 | -19.54 | 9.973 |
Association between perioperative aEEG
and neurodevelopmental outcomes
The association between perioperative aEEG and
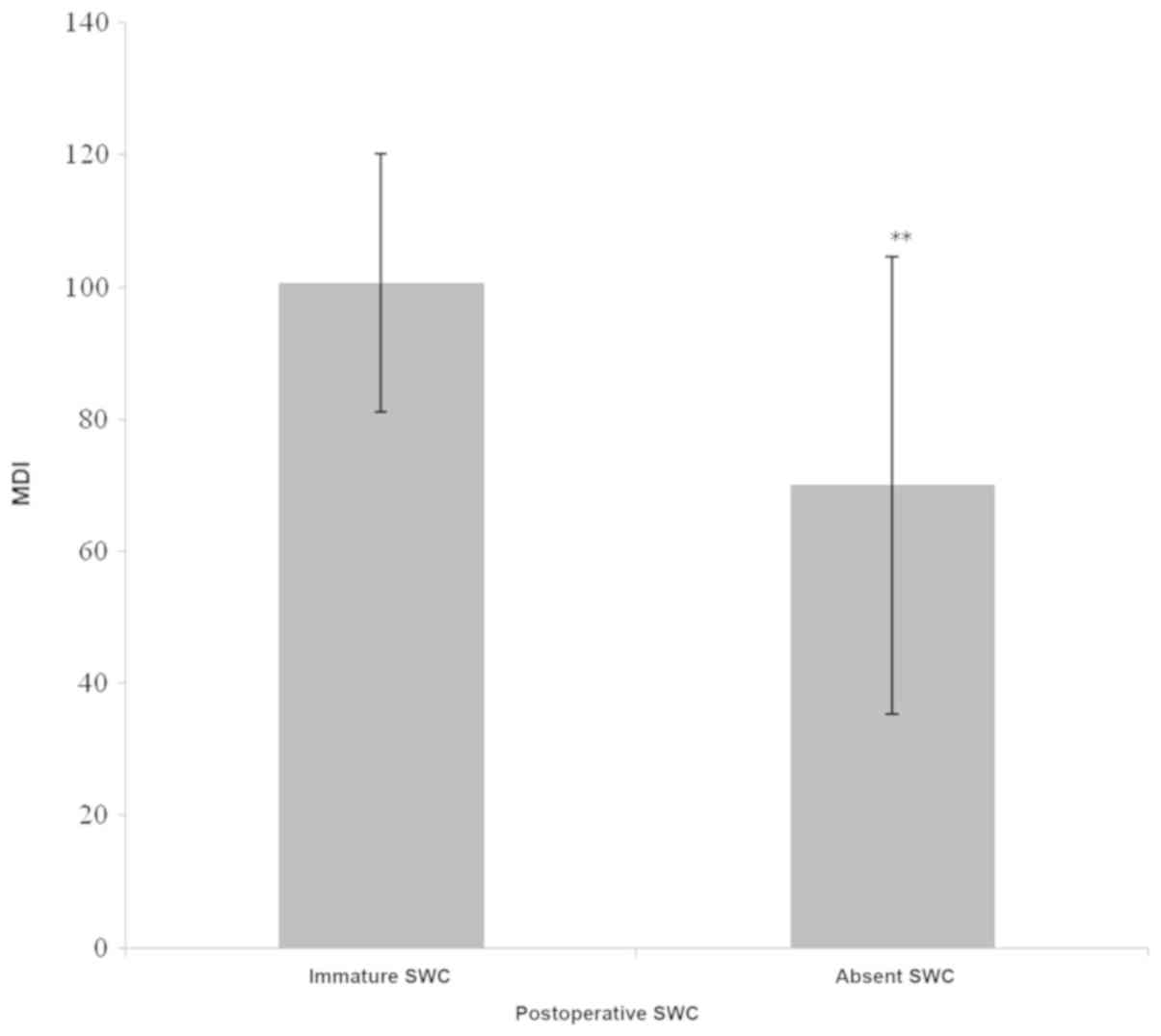
neurodevelopmental outcomes was subsequently examined. A
significant difference of MDI was demonstrated among groups with
developed, immature or absent postoperative SWC (t=3.984; P=0.023;
Table VII). Using the Bonferroni
method for further comparisons, infant MDI, with absent
postoperative SWC (70.00±34.641) was indicated to be significantly
lower compared with immature postoperative SWC MDI (100.65±19.572;
P<0.001; Fig. 2). Additionally,
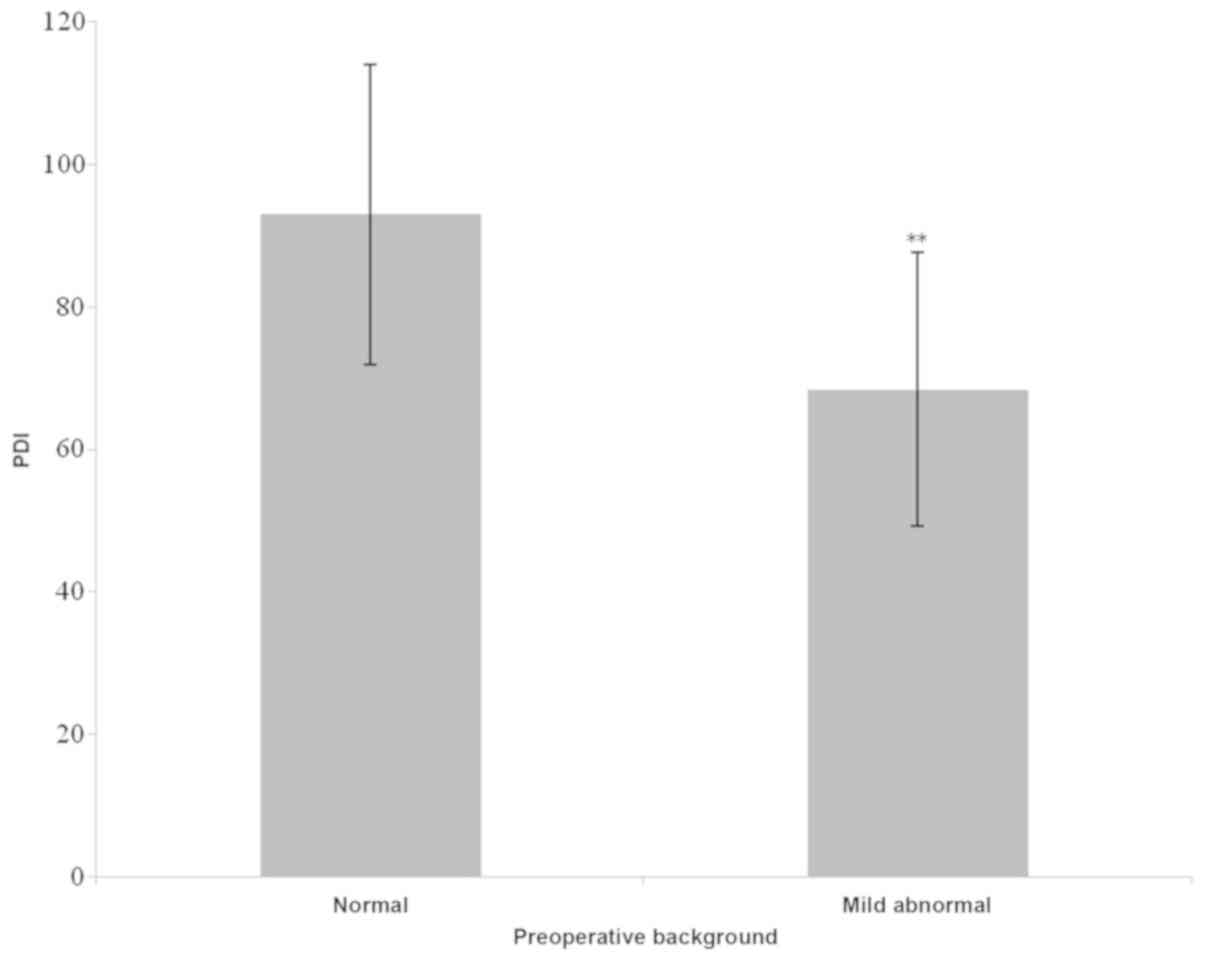
infants with mild abnormal exhibited a significantly lower PDI
compared with CNV (t=2.87; P=0.0064; Table VIII; Fig. 3). A single infant with preoperative
SS without postoperative EA exhibited a poor outcome at 1 year (MDI
80, PDI 84, data not shown). A total of 2 infants with
postoperative SS also exhibited a poor outcome (MDI 79, PDI 67; MDI
97, PDI 116, respectively, data not shown). These three infants
both included in the cyanotic CHD group. A single infant with
postoperative RS and symptomatic seizure with VSD exhibited lower
PDI but normal MDI (94, 110, respectively, data not shown). Due to
the small number of patients which indicated seizure activity pre-
or postoperation (only 4 children), a significant difference was
not revealed between seizure and clinical characteristics. These
data were not shown. A close association was indicated between
perioperative aEEG and neurodevelopmental outcomes.
 | Table VIIAssociation of MDI and perioperative
aEEG. |
Table VII
Association of MDI and perioperative
aEEG.
| aEEG
characteristics | MDI (mean ±
SD) | F/t | P-value |
|---|
| Preoperative
background | | 1.96 | 0.0561 |
|
Normal | 99.19±22.552 | | |
|
Mild
abnormal | 80.57±25.448 | | |
| Preoperative
SWC | | 0.555 | 0.578 |
|
Developed
SWC | 102.22±25.680 | | |
|
Immature
SWC | 94.50±23.685 | | |
|
Absent
SWC | 106.50±7.778 | | |
| Postoperative
background | | 1.01 | 0.3139 |
|
Normal | 95.05±21.605 | | |
|
Mild
abnormal | 104.20±23.658 | | |
| Postoperative
SWC | | 3.984 | 0.023a |
|
Developed
SWC | 91.94±21.349 | | |
|
Immature
SWC | 100.65±19.572 | | |
|
Absent
SWC | 70.00±34.641 | | |
 | Table VIIIAssociation of PDI and perioperative
aEEG. |
Table VIII
Association of PDI and perioperative
aEEG.
| aEEG
characteristic | PDI (mean ±
SD) | F/t | P-value |
|---|
| Preoperative
background | | 2.87 | 0.0064a |
|
Normal | 92.97±21.005 | | |
|
Mild
abnormal | 68.43±19.217 | | |
| Preoperative
SWC | | 2.18 | 0.126 |
|
Developed
SWC | 102.44±23.975 | | |
|
Immature
SWC | 85.91±21.268 | | |
|
Absent
SWC | 82.50±9.192 | | |
| Postoperative
background | | -0.95 | 0.3435 |
|
Normal | 88.30±21.806 | | |
|
Mild
abnormal | 79.60±20.070 | | |
| Postoperative
SWC | | 2.936 | 0.059 |
|
Developed
SWC | 83.86±21.756 | | |
|
Immature
SWC | 92.51±20.839 | | |
|
Absent
SWC | 68.00±17.088 | | |
Predictive value of the perioperative
aEEG on neurodevelopmental outcomes
The predictive value of the perioperative aEEG
results on neurodevelopmental outcomes was assessed in 31 infants
that underwent pre- and postoperative aEEG using Wilcoxon
signed-rank test. The comparison of pre- and postoperative aEEG
suggested that infant brain function exhibited no changes following
surgery (Table IX). The PDI
(68.43±19.217) of infants with mild abnormal preoperative
background pattern was significantly lower compared with normal
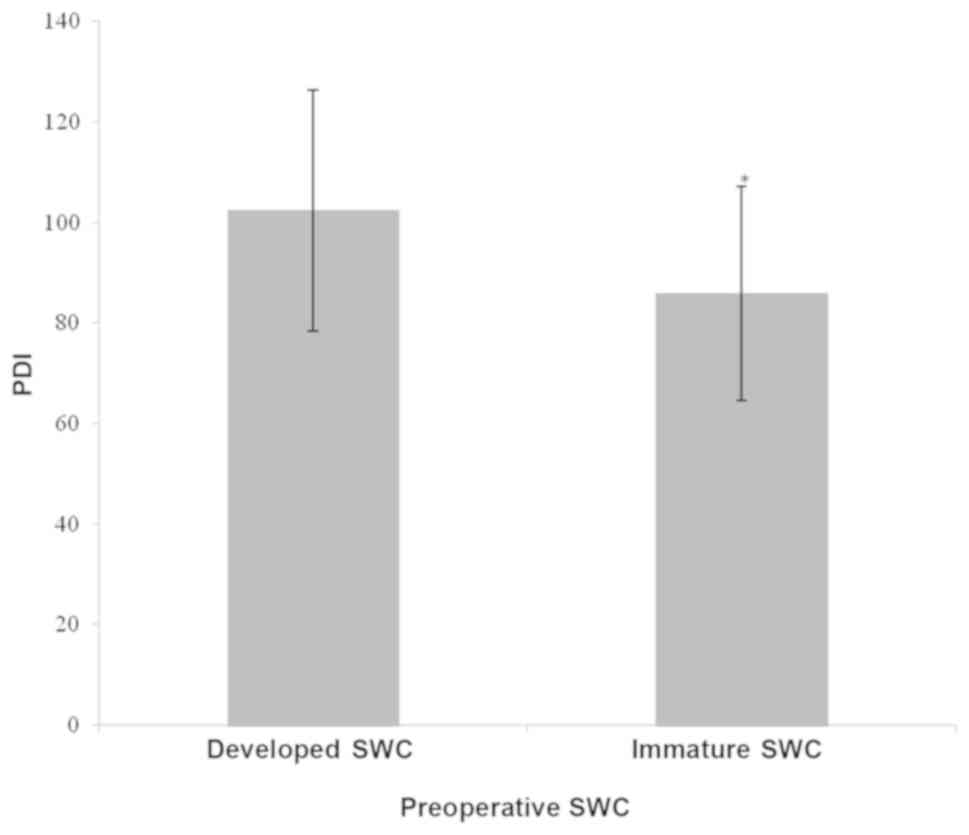
preoperative background pattern (92.97±21.005; P=0.013; Table VIII; Fig. 4). PDI (85.08±21.431) of infants with
immature preoperative SWC was significantly lower compared with
normal preoperative SWC (105.14±21.162; P=0.037; P<0.05;
Table VIII; Fig. 4). These results suggested that the
perioperative aEEG may serve as a predictor of neurodevelopmental
outcomes.
 | Table IXChanges between pre- and
postoperative aEEG (n=31). |
Table IX
Changes between pre- and
postoperative aEEG (n=31).
| Perioperative
aEEG | n | Z | P-value |
|---|
| Background
pattern | | 0.378 | 0.705 |
|
Better | 4 | | |
|
No
change | 24 | | |
|
Worse | 3 | | |
| SWC | | 1.508 | 0.132 |
|
Better | 8 | | |
|
No
change | 20 | | |
|
Worse | 3 | | |
| Seizure | | 0 | 1.000 |
|
Better | 1 | |
|
No
change | 29 | | |
|
Worse | 1 | | |
Discussion
The aim of the current study was to determine the
predictive value of pre- and postoperative aEEG on the 1-year
neurodevelopmental outcome in children who underwent a CHD
operation. This information is important as imaging studies fail to
indicate a relationship between preoperative cranial ultrasound
findings and neurodevelopmental outcomes, or between perioperative
brain injuries detected on cerebral magnetic resonance (25). In the current study, the
perioperative aEEG was strongly associated with neurodevelopmental
outcomes at 1 year of age and was independent of confounding
factors. The results of the current study extend and support the
findings of a previous study conducted by Gunn et al
(26), which demonstrated similar
background pattern changes in relation to surgery, and indicated an
association between postoperative background pattern abnormalities
and a poorer neurodevelopmental outcomes at 2 years of age.
The majority of infants in the current study (80.6%)
exhibited a normal background pattern, with 19.4% exhibiting DNV.
An increasing number of infants with cyanotic CHD or complex CHD
exhibited significantly abnormal preoperative SWC, which was
contradictory to a study performed by ter Horst et al
(20) that demonstrated that SWC was
equal between infants with cyanotic and acyanotic CHD.
A total of 6.3% of infants exhibited an abnormal
background pattern. The percentage of DNV was smaller in
postoperative aEEG compared with preoperative aEEG, indicating that
brain function of infants with CHD can be improved following
surgery. This is consistent with the results of a previous study on
perioperative aEEG in 73 infants with CHD. The reason for the
smaller number of DNV was the improvement of oxygen delivery and
cerebral perfusion following surgery. The improvement is consistent
with the study by Anastasia Dimitropoulos which indicated that a
postoperative acquired brain injury was less frequent than
preoperative injury (41% preoperative vs. 30% postoperative)
(27). However, the improvement of
cerebral activity was not observed in 31 infants who underwent both
pre- and post-operative aEEG. Another study (28) reported that MRI-defined white matter
injuries before and after surgery were similar. A proportion of
infants in the present study, who were transferred from a basic
hospital, usually exhibited unfavorable situations prior to surgery
and also may have worse brain function. Therefore, a large cohort
clinical study is required to confirm this finding.
EA was present in 2 (4.4%) infants preoperatively
and in 3 (3.8%) infants postoperatively. Three infants exhibited
cyanotic CHD, which is consistent with the study of Gunn et
al (26), demonstrating that
perioperative seizures are common in infants undergoing Norwood
operations. Additionally, these findings are also in accordance
with the study of Dimitropoulos et al (27), which indicated that lower
preoperative oxygen saturation is a risk factor for brain injury.
However, EA was demonstrated to be more frequent in infants with
acyanotic CHD (20).
The results of the current study indicated that
poorer PDI at 1 year was associated with an abnormal preoperative
aEEG background pattern and SWC, and the same association was
observed between poorer MDI at 1 year and abnormal postoperative
SWC. This finding is consistent with the study by Gunn et al
(12), in which an abnormal
background pattern was associated with poorer neurodevelopmental
outcome at 2 years of age. The significance of the DNV background
pattern, as a potential negative outcome predictor, has been
emphasized by Mulkey et al (29), in which DNV was considered to be
mildly abnormal. Gunn et al (12) and Latal et al (30) demonstrated that a delayed recovery of
SWC was associated with a poorer neurodevelopmental outcome in
children with CHD. Considering the effect of sedative and pain
relief drugs is difficult to avoid, the current study did not
collect an intraoperative aEEG measurement. Therefore, preoperative
aEEG may be a marker for a more complicated and severe clinical
course and may independently predict neurodevelopmental
outcome.
A total of 3.1 and 5.7% of all infants with proven
pre- and postoperative seizure activity were indicated on the aEEG,
respectively, and perioperative seizures may easily occur in
cyanotic CHD patients. These results were lower compared with other
studies, which reported a postoperative prevalence of ~11-19% using
either continuous electroencephalography recordings or aEEG
(31). However, this result is
similar to a previous study indicating a number of 6.7% (32). Accordingly, the prevalence of
postoperative seizures was higher in a group of neonates following
surgical correction of a congenital aortic arch obstruction
(33). Therefore, the differences in
the prevalence of aEEG seizures may be explained by the time of
aEEG monitoring.
Postoperative seizures are a risk factor for poor
neurodevelopmental outcomes in newborns with transposition of the
great arteries (28) and for other
types of CHD (34). Algra et
al (31) demonstrated that
postoperative seizures on aEEG were associated with new cerebral
injuries and worsening motor outcomes at 2 years of age. In the
present study, a weak association was indicated between
perioperative seizures and poorer motor outcome at 1 year of age,
which was consistent with two patient cohorts in which
perioperative seizures were not associated with early
neurodevelopmental outcome (35).
In the current study, a pre- and postoperative aEEG
was not performed in all participants, as the patients may have
been in the different department prior to surgery. Because only
patients were in a severe situation before surgery were managed in
NICU and could undergo both pre- and postoperative aEEG.
Additionally, molecular level changes pre- and postoperative aEEG
were not assessed in the current study, and this should be
investigated in future research.
In conclusion, children with CHD who underwent
cardiac surgery before 3 months of age exhibited delayed
neurodevelopmental outcomes, and aEEG is a useful tool for
predicting the neurodevelopmental outcomes in infants undergoing
heart surgery.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JG designed the study and wrote the manuscript. SL
and YS collected the data from the patients. YL, CC and BW
performed the experiment. JZ and YY analyzed the data. As the
corresponding author of the article, SH performed the literature
research, revised the manuscript and gave final approval of the
version to be published. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The current study was approved by the ethical
committee of Guangdong Provincial People's Hospital, and written
informed consent was obtained from all parents of the patients.
Patient consent for publication
Not applicable.
Competing interests
The author declare that they have no competing
interest.
References
|
1
|
Mandalenakis Z, Rosengren A, Skoglund K,
Lappas G, Eriksson P and Dellborg M: Survivorship in children and
young adults with congenital heart disease in Sweden. JAMA Intern
Med. 177:224–230. 2017.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Matthiesen NB, Henriksen TB, Gaynor JW,
Agergaard P, Bach CC, Hjortdal VE and Østergaard JR: Congenital
heart defects and indices of fetal cerebral growth in a nationwide
cohort of 924 422 liveborn infants. Circulation. 133:566–575.
2016.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Qu Y, Liu X, Zhuang J, Chen G, Mai J, Guo
X, Ou Y, Chen J, Gong W, Gao X, et al: Incidence of congenital
heart disease: The 9-year experience of the Guangdong registry of
congenital heart disease, China. PLoS One.
11(e0159257)2016.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Massaro AN, El-Dib M, Glass P and Aly H:
Factors associated with adverse neurodevelopmental outcomes in
infants with congenital heart disease. Brain Dev. 30:437–446.
2008.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Komur M, Ozen S, Okuyaz C, Makharoblıdze K
and Erdogan S: Neurodevelopment evaluation in children with
congenital hypothyroidism by Bayley-III. Brain Dev. 35:392–397.
2013.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Kono Y, Yonemoto N, Kusuda S, Hirano S,
Iwata O, Tanaka K and Nakazawa J: Developmental assessment of VLBW
infants at 18 months of age: A comparison study between KSPD and
Bayley III. Brain Dev. 38:377–385. 2016.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Luo XR, Yang ZW and Wan GB: National
Collaboration Group. Revision of bailey infant and child
development scale in China (City Edition). Chin J Clin Psychol.
1:71–75. 1993.
|
|
8
|
Massaro AN, Tsuchida T, Kadom N, El-Dib M,
Glass P, Baumgart S and Chang T: aEEG evolution during therapeutic
hypothermia and prediction of NICU outcome in encephalopathic
neonates. Neonatology. 102:197–202. 2012.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Davis AS, Gantz MG, Do B, Shankaran S,
Hamrick SE, Kennedy KA, Tyson JE, Chalak LF, Laptook AR, Goldstein
RF, et al: Serial aEEG recordings in a cohort of extremely preterm
infants: Feasibility and safety. J Perinatol. 35:373–378.
2015.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Fogtmann EP, Plomgaard AM, Greisen G and
Gluud C: Prognostic accuracy of electroencephalograms in preterm
infants: A systematic review. Pediatrics.
139(e20161951)2017.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Rakshasbhuvankar A, Paul S, Nagarajan L,
Ghosh S and Rao S: Amplitude-integrated EEG for detection of
neonatal seizures: A systematic review. Seizure. 33:90–98.
2015.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Gunn JK, Beca J, Hunt RW, Olischar M and
Shekerdemian LS: Perioperative amplitude-integrated EEG and
neurodevelopment in infants with congenital heart disease.
Intensive Care Med. 38:1539–1547. 2012.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Homsy J, Zaidi S, Shen Y, Ware JS, Samocha
KE, Karczewski KJ, DePalma SR, McKean D, Wakimoto H, Gorham J, et
al: De novo mutations in congenital heart disease with
neurodevelopmental and other congenital anomalies. Science.
350:1262–1266. 2015.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Iliodromiti S, Mackay DF, Smith GC, Pell
JP and Nelson SM: Apgar score and the risk of cause-specific infant
mortality: A population-based cohort study. Lancet. 384:1749–1755.
2014.PubMed/NCBI View Article : Google Scholar
|
|
15
|
O'Brien SM, Clarke DR, Jacobs JP, Jacobs
ML, Lacour-Gayet FG, Pizarro C, Welke KF, Maruszewski B, Tobota Z,
Miller WJ, et al: An empirically based tool for analyzing mortality
associated with congenital heart surgery. J Thorac Cardiovasc Surg.
138:1139–1153. 2009.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Lacour-Gayet F, Clarke D, Jacobs J, Comas
J, Daebritz S, Daenen W, Gaynor W, Hamilton L, Jacobs M,
Maruszsewski B, et al: The Aristotle score: A complexity-adjusted
method to evaluate surgical results. Eur J Cardiothorac Surg.
25:911–924. 2004.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Tekgul H, Bourgeois BF, Gauvreau K and
Bergin AM: Electroencephalography in neonatal seizures: Comparison
of a reduced and a full 10/20 montage. Pediatr Neurol. 32:155–161.
2005.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Shah NA and Wusthoff CJ: How to use:
Amplitude-integrated EEG (aEEG). Arch Dis Child Educ Pract Ed.
100:75–81. 2015.PubMed/NCBI View Article : Google Scholar
|
|
19
|
al Naqeeb N, Edwards AD, Cowan FM and
Azzopardi D: Assessment of neonatal encephalopathy by
amplitude-integrated electroencephalography. Pediatrics.
103:1263–1271. 1999.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Horst HJ, Mud M, Roofthooft MT and Bos AF:
Amplitude integrated electroencephalographic activity in infants
with congenital heart disease before surgery. Early Hum Dev.
86:759–764. 2010.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Fogtmann EP, Plomgaard AM, Greisen G and
Gluud C: Prognostic accuracy of electroencephalograms in preterm
infants: A systematic review. Pediatrics. 139(pii:
e20161951)2017.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Latal B, Wohlrab G, Brotschi B, Beck I,
Knirsch W and Bernet V: Postoperative amplitude-integrated
electroencephalography predicts four-year neurodevelopmental
outcome in children with complex congenital heart disease. J
Pediatr. 178(55-60.e1)2016.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Drury PP, Gunn AJ, Bennet L,
Ganeshalingham A, Finucane K, Buckley D and Beca J: Deep
hypothermic circulatory arrest during the arterial switch operation
is associated with reduction in cerebral oxygen extraction but no
increase in white matter injury. J Thorac Cardiovasc Surg.
146:1327–1333. 2013.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Clancy RR, Sharif U, Ichord R, Spray TL,
Nicolson S, Tabbutt S, Wernovsky G and Gaynor JW: Electrographic
neonatal seizures after infant heart surgery. Epilepsia. 46:84–90.
2005.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Bertholdt S, Latal B, Liamlahi R, Pretre
R, Scheer I, Goetti R, Dave H, Bernet V, Schmitz A, von Rhein M, et
al: Cerebral lesions on magnetic resonance imaging correlate with
preoperative neurological status in neonates undergoing
cardiopulmonary bypass surgery. Eur J Cardiothorac Surg.
45:625–632. 2014.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Gunn JK, Beca J, Penny DJ, Horton SB,
d'Udekem YA, Brizard CP, Finucane K, Olischar M, Hunt RW and
Shekerdemian LS: Amplitude-integrated electroencephalography and
brain injury in infants undergoing Norwood-type operations. Ann
Thorac Surg. 93:170–176. 2012.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Dimitropoulos A, McQuillen PS, Sethi V,
Moosa A, Chau V, Xu D, Brant R, Azakie A, Campbell A, Barkovich AJ,
et al: Brain injury and development in newborns with critical
congenital heart disease. Neurology. 81:241–248. 2013.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Bellinger DC, Wypij D, Rivkin MJ, DeMaso
DR, Robertson RL Jr, Dunbar-Masterson C, Rappaport LA, Wernovsky G,
Jonas RA and Newburger JW: Adolescents with d-transposition of the
great arteries corrected with the arterial switch procedure:
Neuropsychological assessment and structural brain imaging.
Circulation. 124:1361–1369. 2011.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Mulkey SB, Yap VL, Bai S, Ramakrishnaiah
RH, Glasier CM, Bornemeier RA, Schmitz ML and Bhutta AT:
Amplitude-integrated EEG in newborns with critical congenital heart
disease predicts preoperative brain magnetic resonance imaging
findings. Pediatr Neurol. 52:599–605. 2015.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Latal B, Kellenberger C, Dimitropoulos A,
Hagmann C, Balmer C, Beck I and Bernet V: Can preoperative cranial
ultrasound predict early neurodevelopmental outcome in infants with
congenital heart disease? Dev Med Child Neurol. 57:639–644.
2015.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Algra SO, Schouten AN, Jansen NJ, van
Oeveren W, Haas F, Groenendaal F, Lemmers PM, van Haastert IC, Toet
MC and de Vries LS: Perioperative and bedside cerebral monitoring
identifies cerebral injury after surgical correction of congenital
aortic arch obstruction. Intensive Care Med. 41:2011–2012.
2015.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Juan G, Suixin L, Shaoru H, Yunxia S,
Yumei L, Yuan R, Chen C and Bi W: Postoperative brain functions in
infants with critical congenital heart disease via aEEG. Chin J
Thoracic Cardiovascular Surg. 34:581–585. 2018.
|
|
33
|
Gaynor JW, Nicolson SC, Jarvik GP,
Wernovsky G, Montenegro LM, Burnham NB, Hartman DM, Louie A, Spray
TL and Clancy RR: Increasing duration of deep hypothermic
circulatory arrest is associated with an increased incidence of
postoperative electroencephalographic seizures. J Thorac Cardiovasc
Surg. 130:1278–1286. 2005.PubMed/NCBI View Article : Google Scholar
|
|
34
|
von Rhein M, Dimitropoulos A,
Valsangiacomo Buechel ER, Landolt MA and Latal B: Risk factors for
neurodevelopmental impairments in school-age children after cardiac
surgery with full-flow cardiopulmonary bypass. J Thorac Cardiovasc
Surg. 144:577–583. 2012.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Gaynor JW, Jarvik GP, Bernbaum J, Gerdes
M, Wernovsky G, Burnham NB, D'Agostino JA, Zackai E,
McDonald-McGinn DM, Nicolson SC, et al: The relationship of
postoperative electrographic seizures to neurodevelopmental outcome
at 1 year of age after neonatal and infant cardiac surgery. J
Thorac Cardiovasc Surg. 131:181–249. 2006.PubMed/NCBI View Article : Google Scholar
|