Introduction
Intradural extramedullary (IDEM) spinal tumors are
one of the most common intraspinal lesions that usually cause pain
or neurological deficit secondary to neural compression, the
majority of which are meningiomas (50%) and schwannomas (30%)
(1). For such lesions, surgery is
the preferred treatment, which mainly includes open spinal surgery
and minimally invasive spinal surgery (MISS) (2). Generally, traditional surgery for
IDEM spinal tumors uses an open approach, requiring a large
incision, bilateral paravertebral muscle stripping and extensive
bony resection for extensive laminectomy or additional facetectomy,
which leads to the risk and probability of numerous complications,
such as long-term pain, infection, cerebrospinal fluid leakage,
late spinal instability or kyphosis (3,4).
Given the shortcomings and limitations of the open approach, MISS
emerged and gradually replaced open spinal surgery, as it has the
characteristics of not damaging osseoligamentous structures and
muscles, reducing the occurrence of corresponding complications to
a large extent (5-7).
Moreover, previous study results (postoperative efficacy and
surgical complications) demonstrated that MISS is a safe and
effective surgical procedure for IDEM spinal tumor treatment
(8,9). In MISS, a microscope and endoscope
are used as auxiliary tools to observe and distinguish lesions from
normal tissues (10). In addition,
to further reduce the trauma-related instability and provide
operating space, tubular retractors (expandable or non-expandable)
have been successfully used in MISS (11). However, to the best of our
knowledge, there are few reports of pure endoscopic surgery with a
non-expandable tubular retractor for IDEM spinal lesions. The
present study reports 5 cases of IDEM spinal tumors that were
treated by pure endoscopic MISS with a non-expandable tubular
retractor, while retrospectively analyzing the procedure and
outcomes of this surgical technique.
Materials and methods
Patients
A total of 5 patients with IDEM spinal tumors who
underwent pure endoscopic MISS with a parallel non-expandable
tubular retractor system (BeiJing Fule) were retrospectively
analyzed between January 2019 and July 2020 in the Department of
Neurosurgery, Chongqing General Hospital (Chongqing, China). A
parallel non-expandable tubular retractor with a size of 22 mm was
utilized. This could be moved 20 mm up and down by fully separating
the multi-split space, meaning that the lamina could be exposed
within a range of ~60 mm (~2 vertebral levels). Therefore, the IDEM
tumors involving one or two vertebral levels were included in the
present study, while IDEM tumors involving >2 vertebral segments
were excluded. Table I shows the
preoperative conditions of the cases discussed in the present
report, including age, sex, tumor location, tumor size, clinical
symptoms and duration of symptoms. The patients' ages ranged from
46-76 years, with an average age of 61 years, and the group
included 3 men and 2 women. The preoperative evaluation consisted
of clinical examination and magnetic resonance imaging (MRI) of the
spine. The patients complained mainly of pain and/or neurological
deficit, presenting for 3-12 months. Specifically, 2 cases only
presented with a history of back pain, 2 cases presented with back
pain and lower limb numbness, and 1 case presented with back pain
and lower limb numbness and weakness. The preoperative MRI findings
of all patients were consistent with IDEM lesions, including 2
cases in the thoracic vertebrae and 3 cases in the lumbar (L)
vertebrae. According to the relationship between the spinal cord
and the tumor, the tumor locations were ventrolateral (n=1), dorsal
(n=1), dorsal lateral (n=1) and lateral (n=2). The tumor sizes were
35x15, 21x13, 18x7, 16x8 and 20x11 mm, respectively. Of the 5
examined tumors, 4 were within one vertebral level and 1 was within
two vertebral levels. All these tumors were suitable for endoscopic
surgery. The preoperative pain and neurological deficit were
evaluated by the visual analog scale (12) and the modified McCormick scale
(13), respectively, and indicated
that the pain score was between 6 and 10, while the neurological
deficit was graded as grade II in 4 cases and grade III in 1 case.
Initial clinical follow-up occurred at 3 and 6 months after
surgery. After 6 months of follow-up, visits were performed at
yearly intervals or more frequently when indicated.
 | Table IPreoperative characteristics of 5
patients. |
Table I
Preoperative characteristics of 5
patients.
| Case no. | Age, years | Sex | Tumor location | Tumor size, mm | Clinical
symptoms | Visual analog
scale | Modified McCormick
scale | Symptoms duration,
months |
|---|
| 1 | 55 | F | L2-L3,
ventrolaterala | 35x13 | Back pain, lower
limb numbness | 9 | II | 6 |
| 2 | 76 | F | T8-T9, dorsal | 21x13 | Back pain, lower
limb numbness and weakness | 10 | III | 6 |
| 3 | 67 | M | L1-L2, lateral | 18x7 | Back pain | 7 | II | 4 |
| 4 | 62 | M | L2, lateral | 16x8 | Back pain | 6 | II | 12 |
| 5 | 46 | M | T11-T12,
dorsolateral | 20x11 | Back pain, lower
limb numbness | 8 | II | 3 |
Surgical treatment
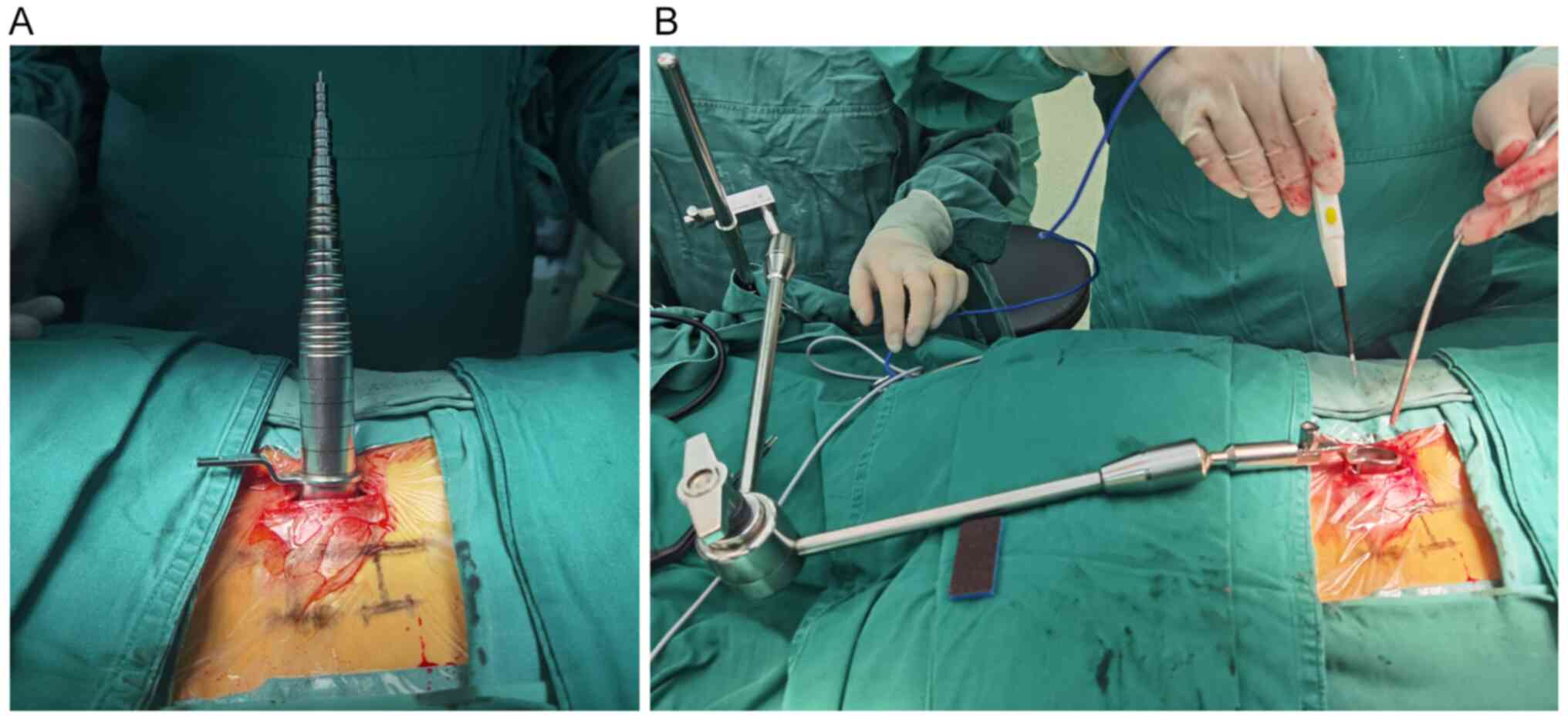
Under general anesthesia, the patient was placed in
a prone position. A 1.5- to 2-cm skin incision was made 2 cm
lateral to the midline, consistent with the tumor location on
C-Arm. The subcutaneous tissue was dissected to the muscle fascia
and paraspinal muscles, followed by blunt separation directly to
the lamina from the potential space among the paraspinal muscles.
Subsequently, tubular retractor devices were sequentially
introduced in this space (Fig.
1A). Finally, the tubular retractor was fixed on the operating
table using a flexible arm (Fig.
1B) and the appropriate position was ascertained under C-Arm,
which means that its angle could be slightly adjusted to eliminate
the tumor adjacent to the tube. Once the parallel non-expandable
tubular retractor system was set up, the surgeon operated using an
endoscope. Due to the advantages of flexible and convenient
operation and ease to adjust the visualization direction at any
time, hand-held endoscopes were often used to observe tumors and
formulate resection plans. When the surgeon needed to perform the
bimanual surgery, an assistant or a pneumatic arm held the
endoscope in one corner. Thus, these methods of controlling the
endoscope were used at different stages of the operation. The
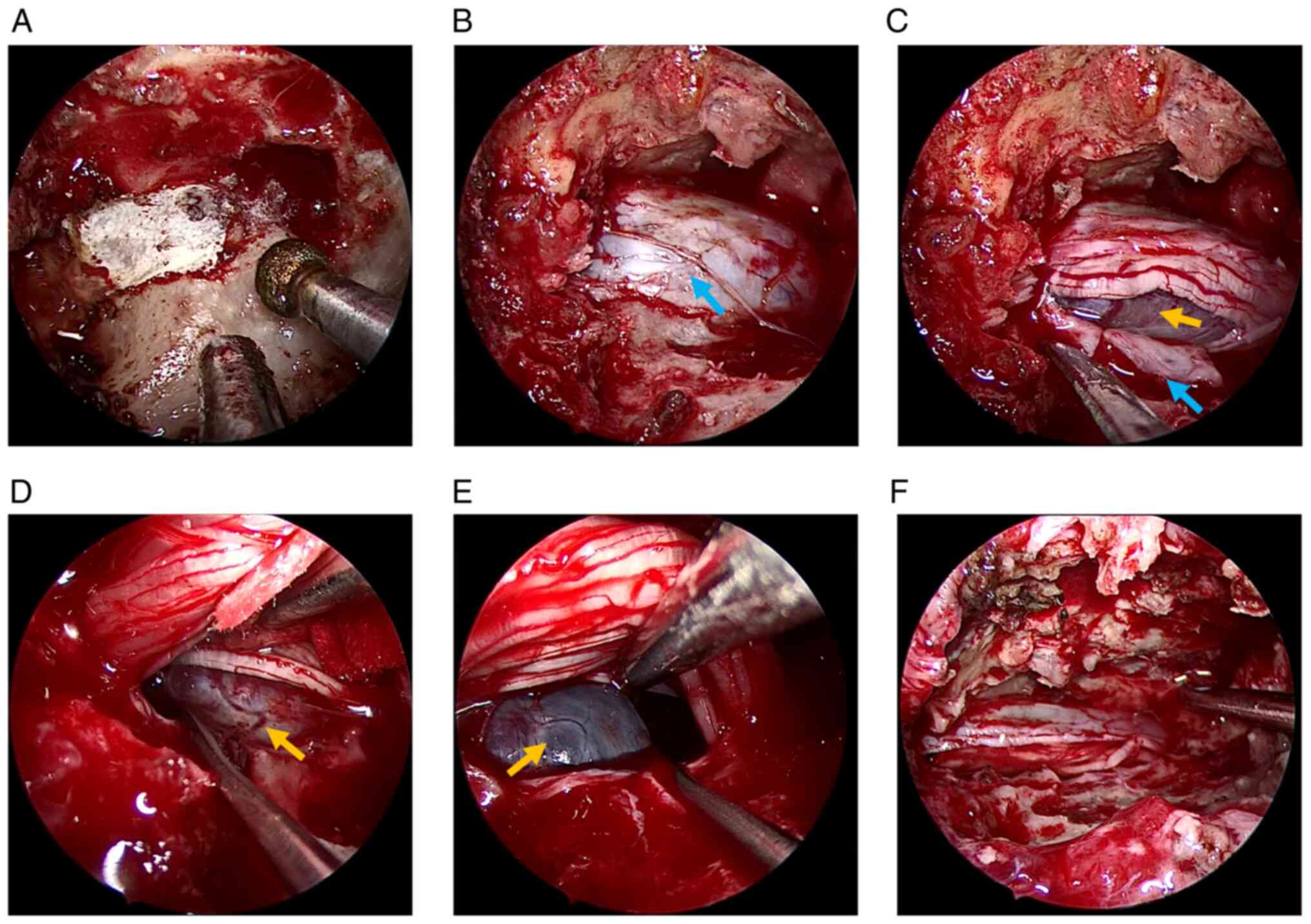
lamina or intervertebral space corresponding to the tumor was
exposed, and the lamina corresponding to the tumor was removed with
a high-speed drill and rongeur (Fig.
2A). The extent of bone resection was determined by the needs
of each lesion based on the bony anatomical landmarks that were
identified preoperatively and verified intraoperatively using
C-Arm. The hemilaminectomy was usually applied. Exceptionally, for
ventral tumors, the ipsilateral facet needs to be resected to gain
space for tumor exposure. A small portion of the lower part of the
ligamentum flavum was removed, exposing the dura over the mass
lesion (Fig. 2B). Subsequently,
the dura was opened and widened using scissors, and the lateral
dura margin was contracted with 5-0 Prolene sutures to expose the
tumor (Fig. 2C). The cephalic part
of the tumor was loosened from the surrounding neural tissues using
a dissector and the tumor was removed (Fig. 2D). After adjusting the parallel
non-expandable tubular retractor angle, the caudal part of the
tumor was loosened using the same aforementioned method (Fig. 2E) and the tumor was completely
removed (Fig. 2F). It was noted
that during the resection of lumbar meningioma, the brain cotton
was used to separate the tumor from the cauda equina nerve to
provide protection to the nerve. Next, the spinous process base was
removed to create more space for repairing the dura. With the
assistance of an endoscope, the dura mater was sutured as
previously described by Parihar et al (14). If there had been a risk of
cerebrospinal fluid leakage, an absorbable artificial dura mater
would have been used for further dura mater watertight closure.
Finally, the skin was closed with a single suture.
Pathological examination
Surgically resected tumor tissues were detected by
routine pathological examination, using H&E staining. Tumor
specimens were first fixed with 4% formaldehyde solution at room
temperature for 24 h and then embedded and fixed in paraffin. The
specimens were then cut into 4-µm sections and deparaffinized in
xylene at 60˚C for 2 h. Subsequently, at room temperature, the
sections were stained with 0.5% hematoxylin for 3 min, followed by
0.5% eosin for 3 min. Subsequently, the stained sections were
observed under a light microscope to obtain microphotographs of the
histopathology.
Results
Surgical outcomes
All patients underwent a successful pure endoscopic
MISS with a parallel non-expandable tubular retractor. Table II shows the intraoperative and
postoperative conditions, including blood loss, the extent of tumor
resection, pathology, clinical symptoms (at 3-month follow-up),
complications and follow-up time. The mean blood loss was ~47 ml,
the maximum blood loss was 70 ml and the minimum blood loss was 35
ml. Postoperative MRI demonstrated that a gross total resection
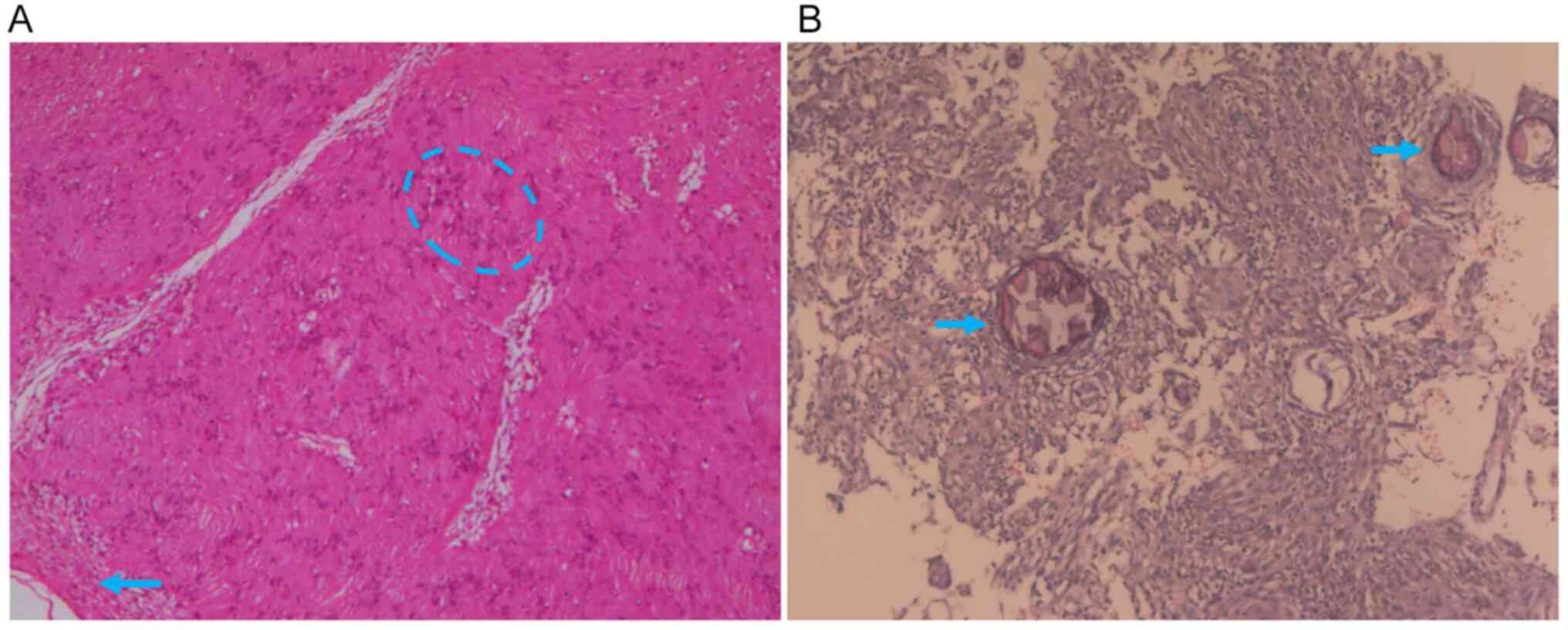
(GTR) had been achieved in all cases. The pathological analysis
revealed schwannoma (Fig. 3A) in 3
cases and meningioma (Fig. 3B) in
2 cases. After the operation, all patients improved significantly
and there were no procedure-related postoperative complications,
such as cerebrospinal fluid leakage, wound hematoma or vertebral
segment instability. All patients were followed up for 6-40 months,
with a mean follow-up time of 25.2 months. At the initial 3-month
follow-up the pain symptoms were significantly reduced or had even
disappeared. The neurological status was grade I in 4 cases and
grade II in 1 case; therefore, it had improved by one grade in all
patients. Only one patient (case 2) still had mild lower limb
weakness, which was due to the tight adhesion between the extensive
basal meningioma and dura mater. However, this returned to normal
in the subsequent follow-up. In the present case series, all
patients achieved good outcomes without serious complications, such
as long-term pain, infection, cerebrospinal fluid leakage, late
spinal instability or kyphosis.
 | Table IIOutcome data of 5 patients. |
Table II
Outcome data of 5 patients.
| Case no. | Blood loss, ml | Extent of
resection | Pathology | Postoperative
symptoms | Visual analog
scale | Modified McCormick
scale | Complications | Follow-up time,
months |
|---|
| 1 | 50 | GTR | Schwannoma | None | 0 | I | None | 40 |
| 2 | 70 | GTR | Meningioma | Lower limb
weakness | 2 | II | None | 31 |
| 3 | 40 | GTR | Schwannoma | None | 0 | I | None | 19 |
| 4 | 35 | GTR | Schwannoma | None | 0 | I | None | 6 |
| 5 | 40 | GTR | Meningioma | None | 0 | I | None | 30 |
Illustrative case
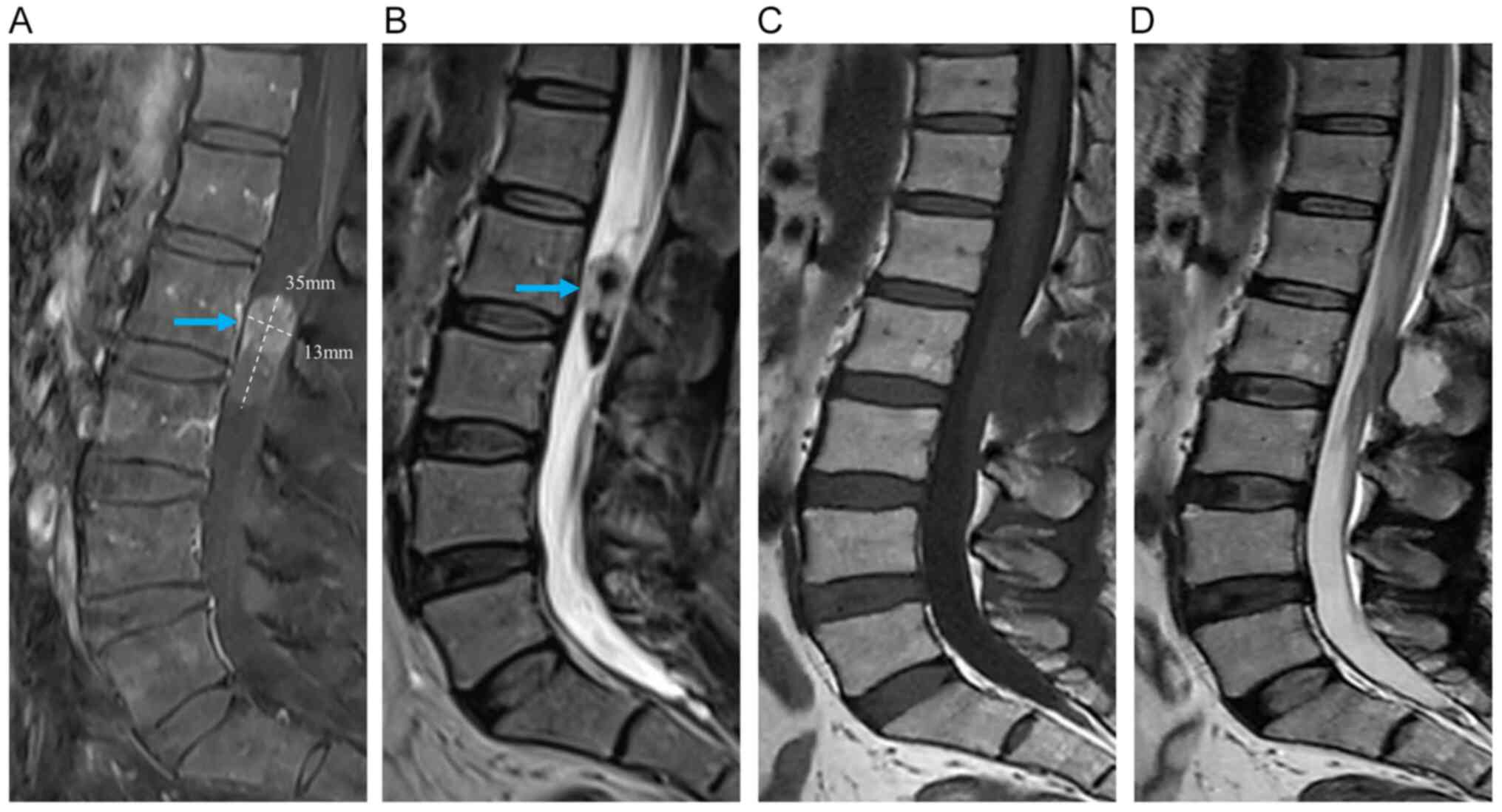
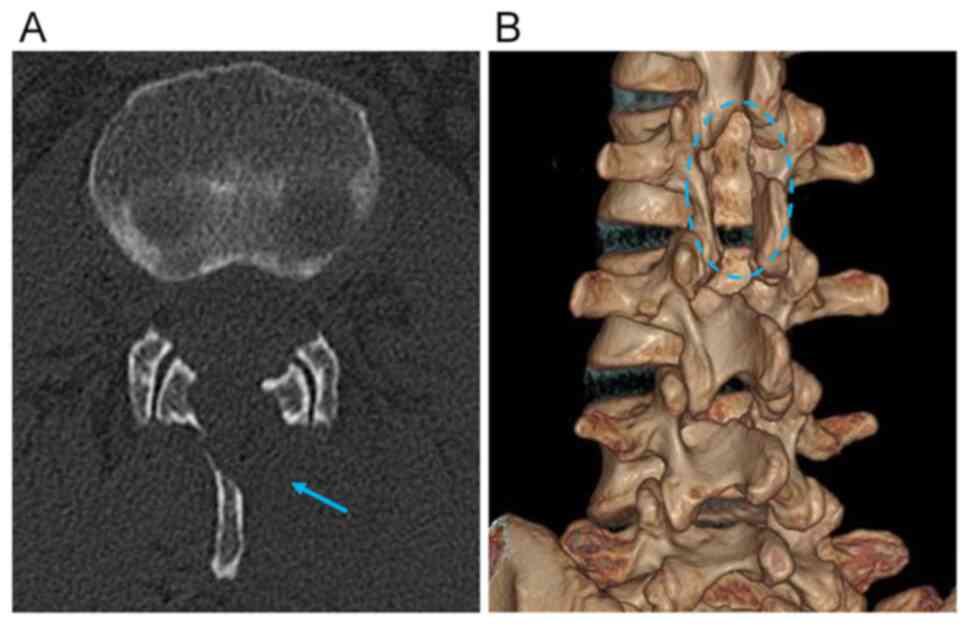
A 55-year-old female patient (case 1) presented with
a 6-month history of back pain and lower limb numbness. On
examination, there was no weakness of the limbs and no
bowel/bladder symptoms. MRI revealed an IDEM lesion at the L2-3
level (Fig. 4A and B). The patient underwent pure endoscopic
MISS with a parallel non-expandable tubular retractor and
postoperative imaging revealed that a GTR of all the lesions had
been achieved (Fig. 4C and
D). Postoperative computed
tomography scans revealed laminectomy defects (Fig. 5A and B). Pathological analysis showed the
Antoni B zone featuring hypocellularity in the myxoid stroma via
H&E staining, which confirmed a schwannoma (Fig. 3A). Postoperatively, the patient
experienced good pain relief. The patient's modified McCormick
scale at 3 months improved from II to I. No spinal instability or
kyphosis occurred during the follow-up.
Discussion
Due to the advantages of little tissue damage and
fast recovery time, MISS for the resection of IDEM spinal tumors
has been valued and favored by surgeons (15,16).
The key auxiliary devices in MISS are retractors and lighting
vision systems. The tubular retractor technique plays an important
role in MISS and has been demonstrated to be a viable alternative
to traditional laminectomy. In the study performed by Dhandapani
and Karthigeyan (17), retractors
were classified as non-tubular or tubular, the latter being further
divided into expandable tubular and non-expandable retractors,
where the non-expandable retractors could be further divided into
convergent and parallel retractors. Compared with the non-tubular
retractor, the tubular retractor has the advantage of less damage
to surgery-related tissues while maintaining structural and
functional integrity, thus it has become and has been recognized as
a mainstream tool (18).
Furthermore, compared with the non-expandable tubular retractor,
the retraction mechanism of the expandable tubular retractor is
dynamic, which may also lead to more tissue damage (18). Dahlberg et al (19) described the minimally invasive
microsurgical resection of primary intradural spinal tumors using
an expandable tubular retraction system. Nzokou et al
(20) reported on the minimally
invasive removal of thoracic and lumbar spinal tumors using a
non-expandable tubular retractor. Balasubramanian et al
(21) reported a large series of
spinal tumors operated by the keyhole technique using a
non-expandable tubular retractor. Undeniably, compared with
traditional open surgery, the tubular retractor technique suffers
from poor exposure of the intraspinal field. However, auxiliary
lighting vision systems, such as microscopes and endoscopes, can
overcome this deficiency to some extent. As for the auxiliary
lighting vision systems, at present, the visualization of most MISS
primarily relies on the microscope and occasionally on the
endoscope (22-24).
With the development of endoscopic technology, the endoscope has
been widely used and recognized in neurosurgery due to its
excellent intraoperative visualization. Previously, a number of
cases (n≥5 per study) using MISS to treat IDEM spinal lesions have
been reported and the surgical method used a pure endoscope with a
retractor (as shown in Table
III). Caballero-García et al (25) described the use of an endoscope and
a Caspar system in MISS for IDEM spinal tumors. Similarly, Zeng
et al (26) reported
endoscopic MISS surgery for the removal of IDEM spinal lesions with
a Williams retractor. Dhandapani and Karthigeyan (17) mainly used the X-tube and Quadrant
retractor in pure endoscopic MISS to remove IDEM spinal lesions. In
the aforementioned literature, the Caspar system and Williams
retractor belong to the non-tubular retractor system, whereas the
X-tube and Quadrangle retractor belong to the expandable tubular
retractor system, which may cause uncertain damage to patients.
Parihar et al (14)
reported a series of cases that underwent MISS for the resection of
IDEM spinal tumors using an endoscope combined with a
non-expandable tubular retractor and the gross total resection of
tumor has been achieved with minor blood loss in all patients. It
is worth noting that the retractor used by Parihar et al
(14) was a Destandau retractor
system, which belongs to the convergent non-expandable tubular
retractors, while the retractor used in the present study was a
parallel non-expandable tubular retractor. Indeed, compared with a
convergent retractor, the parallel retractor can provide more
available space, making it more suitable for an endoscope and for
removing larger lesions (17).
 | Table IIIPrevious studies (n≥5 cases per
study) recording pure endoscope and retractor treatment for an
intradural extramedullary spinal tumor. |
Table III
Previous studies (n≥5 cases per
study) recording pure endoscope and retractor treatment for an
intradural extramedullary spinal tumor.
| First author/s,
year | No. of cases | Retractor
system | GTR rate, % | (Refs.) |
|---|
| Parihar et
al, 2017 | 18 | Convergent
non-expandable tubular retractor | 100 | (14) |
| Dhandapani and
Karthigeyan, 2018 | 16 | Expandable tubular
retractor; convergent non-expandable tubular retractor | 100 | (17) |
| Caballero-García
et al, 2022 | 10 | Non-tubular
retractor | 100 | (25) |
| Zeng et al,
2022 | 20 | Non-tubular
retractor | 100 | (26) |
| Present study | 5 | Parallel
non-expandable tubular retractor | 100 | - |
For IDEM spinal tumors, an endoscope can provide
better visualization than a microscope (27). With the assistance of an adjustable
angle tubular retractor, endoscopic visualization can be further
expanded. Most importantly, the endoscope is allowed to enter the
surgical area for close observation of panoramic visualization,
which has great advantages, especially for ventral or ventrolateral
lesions, in avoiding more invasive surgical approaches, such as
anterior or anterolateral approaches (28,29).
However, the endoscope can only provide two-dimensional images,
which requires long-term training, experience accumulation and
intraoperative instrument feedback to reconstruct three-dimensional
(3D) images, putting forward higher requirements for surgeons
(30). Although the microscope can
provide 3D visualization, it is far away from the surgical area,
which leads to serious light attenuation and cannot provide a
close-up view of surgical details or panoramic visualization
(26). These two auxiliary
lighting vision systems have their advantages and limitations, and
both have been proven to be effective and safe. Therefore, the
choice of endoscope or microscope depends on the surgeon's
preference.
Although the MISS under a microscope or an endoscope
is relatively safe and effective, it is undeniable that it still
has certain limitations. Soriano-Sánchez et al (31) reviewed the current indications and
contraindications of microscope-assisted MISS for the treatment of
IDEM lesions and considered that the key factors for the
microscopic approach were tumor location, size, histology and
spinal instability. For the endoscopic approach, although the tumor
location is not strictly required, the tumor size is a particularly
critical limiting factor. Especially for large tumors, even if
expandable tubular retractors with adjustable angles and endoscopes
with excellent visualization are used, it is impossible to reach
all parts of the tumor, and this greatly increases the risk of
bleeding and nerve damage. In general, to ensure the safety of the
surgery, a pure endoscopic approach using an expandable tubular
retractor is recommended for tumors within two vertebral levels
(14). Hence, the endoscopy
approach is indicated for no more than 2 vertebral segments. It is
difficult for the endoscopic approach to remove some tumors with
specific locations and histology, such as ventral meningioma
(32). The ventral meningioma
usually has a wide base and limited surgical space, which makes it
vulnerable to spinal cord injury due to repeated traction (33). Therefore, for ventral meningioma,
the endoscopic approach is not recommended, while traditional open
surgery is recommended. Other ventral tumors or meningiomas at
other locations (lateral, medial, or posterior) can be removed by
the endoscopic approach (32). In
addition, the endoscopic approach will increase the difficulty of
repairing the dura mater and of achieving hemostasis (17). The bimanual technique is essential
for hemostasis and the suturing of the dura. In the endoscopic
approach, however, the limited available space in endoscopic
surgery will increase the difficulty of using the bimanual
technique, which is also a limitation of endoscopic methods
(34). Furthermore, the method of
using an endoscope with a non-expandable tubular retractor requires
that the surgeon should have experience in both spinal surgery and
endoscopic visualization.
In addition, postoperative complications are also an
important concern for surgeons and patients. Tumialán et al
(35) considered the correlation
between the amount of bone resection and the risk of secondary
spinal deformity and instability after IDEM lesion resection.
Therefore, for MISS, controlling the degree of bone resection and
avoiding unnecessary bone resection are key factors to minimize the
risk of postoperative instability. In the present study, a
hemilaminectomy was usually applied. However, for ventral tumors,
the ipsilateral facet needs to be resected to gain space for tumor
exposure and an additional pedicle screw fixation is required after
tumor removal. Recently, Duff et al (36) reported the image merges tailored
access resection technique (37)
under the guidance of 3D fluoroscopy for the resection of spinal
intradural lesions. In this study (36), the planned intraoperative
neuronavigation was used to optimize tumor access and expose the
tumor, which may further refine and reduce bone resection.
The current study reported a patient series with
IDEM spinal tumors treated via pure endoscopic MISS with a parallel
non-expandable tubular retractor, in which the patients achieved
good outcomes. All patients improved significantly in the
postoperative period and had no serious postoperative
complications, which is comparable with the results of previous
studies (14,17,25,26).
Therefore, pure endoscopic MISS with a parallel non-expandable
tubular retractor may be an effective and safe surgical strategy
for IDEM spinal tumor resection. However, the present study is
limited by the relatively small sample size. In further work,
further cases will be recorded to increase the number of samples to
further verify the surgical method.
The current study reported 5 cases of IDEM spinal
tumors treated by pure endoscopic MISS with a parallel
non-expandable tubular retractor, and summarized the surgical
procedure and outcomes. A GTR was achieved in all cases. After the
operation, all cases were significantly improved without serious
postoperative complications. The results of the current series
demonstrated that for IDEM spinal tumors, pure endoscopic MISS with
a parallel non-expandable tubular retractor may be an effective and
safe surgical strategy. Moreover, this surgical strategy has the
advantage of causing low amounts of trauma, less bleeding and fewer
postoperative reactions. Admittedly, despite these advantages, pure
endoscopic technology has also some limitations such as the
difficulty in the removal of a large tumor and a steep learning
curve.
Acknowledgements
Not applicable.
Funding
Funding: No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
GZ, BJ, PW, CX, HJ, JL, CT, XT and NW participated
in the conception and design of the study and data acquisition. GZ
participated in drafting and writing the manuscript. BJ critically
revised the paper. NW ensured that questions related to the
integrity of any part of the work were appropriately investigated
and resolved. GZ, BJ, PW, CX, HJ, JL, CT, XT and NW confirm the
authenticity of all the raw data. All authors have read and
approved the final manuscript.
Ethics approval and consent to
participate
The Ethics Committee of Chongqing General Hospital
waived the requirement for additional ethical review as this report
is retrospective and not based on any specific patient priorities,
experiences or preferences. Informed consent for participation in
the study or use of the medical data was obtained from the
patients. The patients provided permission to publish the features
of their cases and the identity of the patients has been
protected.
Patient consent for publication
Written informed consent was obtained from the
patient for publication of this manuscript and any accompanying
images.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Ottenhausen M, Ntoulias G, Bodhinayake I,
Ruppert FH, Schreiber S, Förschler A, Boockvar JA and Jödicke A:
Intradural spinal tumors in adults-update on management and
outcome. Neurosurg Rev. 42:371–388. 2019.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Wong AP, Lall RR, Dahdaleh NS, Lawton CD,
Smith ZA, Wong RH, Harvey MJ, Lam S, Koski TR and Fessler RG:
Comparison of open and minimally invasive surgery for
intradural-extramedullary spine tumors. Neurosurg Focus.
39(E11)2015.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Lu DC, Chou D and Mummaneni PV: A
comparison of mini-open and open approaches for resection of
thoracolumbar intradural spinal tumors. J Neurosurg Spine.
14:758–764. 2011.PubMed/NCBI View Article : Google Scholar
|
|
4
|
McGirt MJ, Garcés-Ambrossi GL, Parker SL,
Sciubba DM, Bydon A, Wolinksy JP, Gokaslan ZL, Jallo G and Witham
TF: Short-term progressive spinal deformity following laminoplasty
versus laminectomy for resection of intradural spinal tumors:
Analysis of 238 patients. Neurosurgery. 66:1005–112.
2010.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Haji FA, Cenic A, Crevier L, Murty N and
Reddy K: Minimally invasive approach for the resection of spinal
neoplasm. Spine (Phila Pa 1976). 36:E1018–E1026. 2011.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Zong S, Zeng G, Du L, Fang Y, Gao T and
Zhao J: . Treatment results in the different surgery of intradural
extramedullary tumor of 122 cases. PLoS One.
9(e111495)2014.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Raygor KP, Than KD, Chou D and Mummaneni
PV: Comparison of minimally invasive transspinous and open
approaches for thoracolumbar intradural-extramedullary spinal
tumors. Neurosurg Focus. 39(E12)2015.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Gandhi RH and German JW: Minimally
invasive approach for the treatment of intradural spinal pathology.
Neurosurg Focus. 35(E5)2013.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Iacoangeli M, Gladi M, Di Rienzo A, Dobran
M, Alvaro L, Nocchi N, Maria LG, Somma D, Colasanti R and Scerrati
M: Minimally invasive surgery for benign intradural extramedullary
spinal meningiomas: Experience of a single institution in a cohort
of elderly patients and review of the literature. Clin Interv
Aging. 7:557–564. 2012.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Banczerowski P, Czigléczki G, Papp Z,
Veres R, Rappaport HZ and Vajda J: Minimally invasive spine
surgery: Systematic review. Neurosurg Rev. 38:11–26.
2015.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Sharif S, Shaikh Y and Peev N: Minimally
invasive spinal surgery: How to keep out of trouble. World
Neurosurg. 119:517–526. 2018.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Ohnhaus EE and Adler R: Methodological
problems in the measurement of pain: A comparison between the
verbal rating scale and the visual analogue scale. Pain. 1:379–384.
1975.PubMed/NCBI View Article : Google Scholar
|
|
13
|
McCormick PC, Torres R, Post KD and Stein
BM: Intramedullary ependymoma of the spinal cord. J Neurosurg.
72:523–532. 1990.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Parihar VS, Yadav N, Yadav YR, Ratre S,
Bajaj J and Kher Y: Endoscopic management of spinal intradural
extramedullary tumors. J Neurol Surg A Cent Eur Neurosurg.
8:219–226. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Goldstein CL, Macwan K, Sundararajan K and
Rampersaud YR: Perioperative outcomes and adverse events of
minimally invasive versus open posterior lumbar fusion:
Meta-analysis and systematic review. J Neurosurg Spine. 24:416–427.
2016.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Fontes RB, Wewel JT and O'Toole JE:
Perioperative cost analysis of minimally invasive vs open resection
of intradural extramedullary spinal cord tumors. Neurosurgery.
78:531–539. 2016.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Dhandapani S and Karthigeyan M:
‘Microendoscopic’ versus ‘pure endoscopic’ surgery for spinal
intradural mass lesions: A comparative study and review. Spine J.
18:1592–1602. 2018.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Wu J, Zhang C, Lu K, Li C and Zhou Y: A
Novel inextensible endoscopic tube versus traditional extensible
retractor system in single-level minimally invasive transforaminal
lumbar interbody fusion: A prospective observation study. Pain
Physician. 22:E587–E599. 2019.PubMed/NCBI
|
|
19
|
Dahlberg D, Halvorsen CM, Lied B and
Helseth E: Minimally invasive microsurgical resection of primary,
intradural spinal tumours using a tubular retraction system. Br J
Neurosurg. 26:472–475. 2012.PubMed/NCBI View Article : Google Scholar
|
|
20
|
Nzokou A, Weil AG and Shedid D: Minimally
invasive removal of thoracic and lumbar spinal tumors using a
non-expandable tubular retractor. J Neurosurg Spine. 19:708–715.
2013.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Balasubramanian SC, Nair AR, Saphiya NN,
Madan A and Mathews SS: Minimally invasive resection of spinal
tumors with tubular retractor: Case series, surgical technique, and
outcome. World Neurosurg. 149:e612–e621. 2021.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Zhu YJ, Ying GY, Chen AQ, Wang LL, Yu DF,
Zhu LL, Ren YC, Wang C, Wu PC, Yao Y, et al: Minimally invasive
removal of lumbar intradural extramedullary lesions using the
interlaminar approach. Neurosurg Focus. 39(E10)2015.PubMed/NCBI View Article : Google Scholar
|
|
23
|
Mannion RJ, Nowitzke AM, Efendy J and Wood
MJ: Safety and efficacy of intradural extramedullary spinal tumor
removal using a minimally invasive approach. Neurosurgery.
68:208–216. 2011.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Formo M, Halvorsen CM, Dahlberg D,
Brommeland T, Fredø H, Hald J, Scheie D, Langmoen IA, Lied B and
Helseth E: Minimally invasive microsurgical resection of primary,
intradural spinal tumors is feasible and safe: A consecutive series
of 83 Patients. Neurosurgery. 82:365–371. 2018.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Caballero-García J, Linares-Benavides YJ,
Leitão ULS, Aparicio-García C and López-Sánchez M: Minimally
invasive removal of extra- and intradural spinal tumors using full
endoscopic visualization. Global Spine J. 12:121–129.
2022.PubMed/NCBI View Article : Google Scholar
|
|
26
|
Zeng W, Jiang H, He S, Zhang Y, Yu B, Wang
H and Wang C: Comparison of neuroendoscopic and microscopic surgery
for unilateral hemilaminectomy: Experience of a single institution.
Front Surg. 9(823770)2022.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Ying GY, Yao Y, Shen F, Wu ZY, Chen CM and
Zhu YJ: Percutaneous endoscopic removal of cervical foraminal
schwannoma via interlaminar approach: A case report. Oper Neurosurg
(Hagerstown). 14:1–5. 2018.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Özkan N, Dammann P, Chen B, Schoemberg T,
Schlamann M, Sandalcioglu IE and Sure U: Operative strategies in
ventrally and ventrolaterally located spinal meningiomas and review
of the literature. Neurosurg Rev. 36:611–619. 2013.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Telfeian AE, Choi DB and Aghion DM:
Transforaminal endoscopic surgery under local analgesia for ventral
epidural thoracic spinal tumor: Case report. Clin Neurol Neurosurg.
134:1–3. 2015.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Minamide A, Yoshida M, Yamada H, Nakagawa
Y, Maio K, Kawai M and Iwasaki H: Clinical outcomes of
microendoscopic decompression surgery for cervical myelopathy. Eur
Spine J. 19:487–493. 2010.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Soriano-Sánchez JA, Soto García ME,
Soriano Solís S, Rodríguez García M, Trejo Huerta P, Sánchez
Escandón O, Flores Soria ER and Romero-Rangel JAI: Microsurgical
resection of intraspinal benign tumors using non-expansile tubular
access. World Neurosurg. 133:e97–e104. 2020.PubMed/NCBI View Article : Google Scholar
|
|
32
|
El-Hajj VG, Pettersson-Segerlind J,
Fletcher-Sandersjöö A, Edström E and Elmi-Terander A: Current
knowledge on spinal meningiomas-surgical treatment, complications,
and outcomes: A systematic review and meta-analysis (Part 2).
Cancers (Basel). 14(6221)2022.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Tola S, De Angelis M, Bistazzoni S,
Chiaramonte C, Esposito V and Paolini S: Hemilaminectomy for spinal
meningioma: A case series of 20 patients with a focus on ventral-
and ventrolateral lesions. Clin Neurol Neurosurg. 148:35–41.
2016.PubMed/NCBI View Article : Google Scholar
|
|
34
|
Kravtsov MN, Manukovsky VA, Mirzametov SD,
Malysheva OV, Averyanov DA and Svistov DV: Percutaneous
transforaminal full-endoscopic removal of neurinoma of the fifth
lumbar nerve root with intraoperative neuromonitoring: A case
report. Front Surg. 9(877974)2022.PubMed/NCBI View Article : Google Scholar
|
|
35
|
Tumialán LM, Theodore N, Narayanan M,
Marciano FF and Nakaji P: Anatomic basis for minimally invasive
resection of intradural extramedullary lesions in thoracic spine.
World Neurosurg. 109:e770–e777. 2018.PubMed/NCBI View Article : Google Scholar
|
|
36
|
Duff JM, Omoumi P, Bobinski L, Belouaer A,
Plaza Wuthrich S, Zanchi F and Maduri R: Transtubular image-guided
surgery for spinal intradural lesions: Techniques, results, and
complications in a consecutive series of 60 patients. J Neurosurg
Spine: 1-9, 2022 doi: 10.3171/2021.10.SPINE211168 (Epub ahead of
print).
|
|
37
|
Maduri R, Bobinski L and Duff JM: Image
merge tailored access resection (IMTAR) of spinal intradural
tumors. Technical report of 13 cases. World Neurosurg. 98:594–602.
2017.PubMed/NCBI View Article : Google Scholar
|