Introduction
Ptosis, a common condition in clinical practice, is
characterized by a low-lying upper eyelid margin (1). The conjoint fascial sheath (CFS) is a
fibrous connective tissue located in the space between the superior
conjunctival levator palpebrae superioris muscle (LM) and the
anterior third of the superior rectus muscle (2). Since 2002, CFS suspension surgery has
been used to correct ptosis (3).
In CFS surgery, the CFS is fixed at the anterior one-third of the
tarsus so that the upper eyelid margin of the affected eye is
located at the upper edge of the cornea when looking straight ahead
in a sitting position to serve as a corrective role (4). This surgery is now recognized in
clinical practice due to good efficacy and a low number of
complications, such as lagophthalmos, exposure conjunctivitis and
hematoma in the eyebrow area (5).
However, a number of patients experience upper eyelid retraction
after surgery, and Sang et al (4) reported that the amount of upper
eyelid retraction was 0.21±0.07 mm 3 months after surgery. CFS
suspension alone lacks strong attachment points, so it cannot
maintain long-term tissue tension. The combination of the CFS and
LM to form a CFS + LM compound flap suspension on the tarsus can
provide the suspension force and an attachment point for the CFS
(5) to maintain long-term
postoperative outcomes, which is called CFS + LM complex suspension
surgery (6). A clinical study
revealed that the undercorrection and recurrence rates in a CFS +
LM complex suspension group were notably lower compared with those
in the simple CFS suspension group (7).
In pediatric patients, congenital ptosis not only
affects the appearance of the eye but also affects visual function
in severe cases because obstructions of the pupillary area can
cause visual dysfunction (1).
Therefore, the correction of congenital severe ptosis was the focus
of the present study. To the best of our knowledge, there have only
been a small number of studies documenting the correction of severe
congenital ptosis in children with CFS + LM complex suspension
(6-9).
Previous anatomical and histological studies have
reported that the CFS and LM are rich in collagen and elastic
fibers, but lack smooth muscle or skeletal muscle cells (10,11).
Elastic fibers and collagen fibers form the key structures that
maintain the elasticity of stress-bearing tissues, within which
elastin is the most important structural component (12). Furthermore, elastin expression in
the CFS has been previously reported to decrease with age (8). Clinically, the grade classification
of ptosis depends on LM strength, and doctors also determine the
method of surgery based on the LM strength (1). Therefore, the present study followed
up on a previous study (8) and
continued to investigate the association between elastin expression
and LM strength.
The present study aimed to measure the expression of
elastin in the CFS and LM tissues of children with unilateral
severe congenital ptosis with different LM strengths, and to
perform a postoperative evaluation of CFS + LM complex suspension.
The results of the present study may be beneficial for clarifying
the association between CFS/LM elasticity and LM strength, and may
explain why CFS + LM complex suspension surgery has more suspension
force compared with simple CFS suspension surgery. This information
may in turn be applied to provide a theoretical basis for
estimating the surgical volume of CFS + LM complex suspension for
the correction of severe congenital ptosis in children.
Materials and methods
General information
A total of 20 patients (20 eyes) with unilateral
severe congenital ptosis, aged 4-12 years, 15 males and 5 females,
underwent CFS + LM complex suspension surgery in Hebei Eye Hospital
(Xingtai, China) from June 2020 to February 2022. The average age
of the participants was 7.60±2.44 years. According to LM strength,
the patients were divided into the 0-1 mm group and the 2-3 mm
group (n=10/group). The LM strength was measured as follows: The
eyebrow arch was pressed while both eyes of the patient were
looking down as far as possible, then the patient was instructed to
look upwards, the distance that the upper eyelid margin moved was
observed and the value was recorded as the LM strength.
The present study was reviewed and approved by the
Ethics Committee of Hebei Eye Hospital (approval no. 2020KY013;
Xingtai, China). Written informed consent for participation was
obtained from the participant and the minor(s)' legal guardian, for
the publication of any potentially identifiable images or data
included.
Inclusion and exclusion criteria
Inclusion criteria: i) Patients with unilateral
severe congenital ptosis; ii) patients aged <14 years of age;
iii) patients with Bell's phenomenon before surgery; and iv)
patients without a history of eyelid surgery.
Exclusion criteria: i) Patients with genetic
syndromes, mainly including blepharophimosis-ptosis-epicanthus
inversus syndrome and Marcus Gunn jaw winking syndrome; ii)
acquired ptosis caused by trauma, oculomotor nerve palsy and
myasthenia gravis; and iii) other ocular and systemic diseases that
may affect the outcome of surgery, such as ocular inflammation,
ocular cyst, ocular tumor, coagulation dysfunction, immune system
disorders and infectious diseases.
Surgical technique
All the CFS + LM complex suspension surgeries were
performed under general anesthesia and by the same surgeon.
According to the LM strength, different surgical volumes were used
during the operation between the two groups: i) In the 0-1 mm
group, the separation height of the CFS + LM composite flap was 5-6
mm, where the upper eyelid margin was flat at the level of the
upper edge of the cornea; and ii) In the 2-3 mm group, the
separation height of the composite flap was 3-4 mm, such that the
upper eyelid margin covered the cornea by 0.5-1 mm.
The surgery was performed as follows: i) The
surgical incision was designed as a double eyelid line incision and
was marked in advance, and local anesthesia was administered to the
upper eyelid; ii) the skin was incised along the marked line,
before the tarsal plate and LM were separated and exposed; iii) the
orbicularis oculi and the LM aponeurosis were cut at a distance of
2 mm above the margin of the tarsal plate, and the LM aponeurosis
was separated from the Müller muscle and pulled ~5 mm over the
fornix to expose the CFS; iv) the CFS + LM composite flap was fixed
at the outer, intermediate and inner positions of the tarsal plate
with 5-0 absorbable thread, and the upper eyelid margin was flat at
the level of the upper edge of the cornea in the 0-1 mm group or
covered the cornea by 0.5-1 mm in the 2-3 mm group (any excess CFS
and LM tissues that were resected during surgery were collected,
cleaned and stored at -80˚C); and v) a 5-0 silk thread was used to
intermittently suture the skin incision and shape the double
eyelid.
The patients and their parents or guardians were
consulted preoperatively about the need for double eyelid
reconstruction of the other eye to maintain bilateral symmetry.
Western blotting
The CFS and LM specimens were removed from the
freezer, homogenized and lysed in RIPA buffer with protease and
phosphatase inhibitors (Beijing Solarbio Science & Technology
Co., Ltd.). The protein concentrations were measured using a BCA
protein assay (Beijing Solarbio Science & Technology Co.,
Ltd.). The protein samples (15 µg of protein per lane) were
separated by SDS-PAGE on 10% gels and were transferred onto PVDF
membranes, which were then blocked with 5% skimmed milk blocking
solution at room temperature for 1 h. The membranes were cut
between 63 and 48 kDa, and probed with rabbit anti-elastin
(1:1,000; Abcam; cat. no. ab23747) and mouse anti-β-actin (1:5,000;
Hangzhou Lianke Biotechnology, Co., Ltd.; cat. no. ab008-40)
antibodies and incubated overnight at 4˚C. The membranes were then
washed with TBST solution (0.05% Tween-20 used) and incubated with
HRP-conjugated goat anti-rabbit (cat. no. BA1054) and anti-mouse
(cat. no. BA1050) IgG secondary antibodies (1:5,000; Wuhan Boster
Biological Technology, Ltd.) at room temperature for 1 h. A
Superstar Enhanced Chemiluminescence (ECL) Reagent kit (Wuhan
Boster Biological Technology, Ltd.; cat. no. AR1170) was used to
detect the signals by X-ray film exposure. The gray values of the
protein bands were analyzed using ImageJ software (version 1.7.0;
National Institutes of Health) to determine the difference between
the target protein expression and the internal reference protein
expression. The ratio of the grayscale values of the bands was used
to indicate the relative expression level of the proteins.
Postoperative evaluation of curative
effects
The parameters of surgical outcomes included the
postoperative good correction rate, the degree of incomplete eyelid
closure and the incidence of complications. The patients returned
for follow-up at 1, 3 and 6 months postoperatively. The same
physician conducted the examination and analyzed the data.
Therapeutic effect indices: i) If the upper eyelid
covered the upper limbus of the cornea by 1-2 mm, it was considered
a ‘good correction’; ii) if the upper eyelid covered the upper
corneal limbus by >2 mm, it was considered an ‘undercorrection’;
iii) if the upper eyelid was located above the upper corneal
limbus, it was considered an ‘overcorrection’; iv) the upper eyelid
margin located at the preoperative level was considered a
‘relapse’. The postoperative good correction rate was then
calculated as the ratio of the number of patients with good
correction to the total number of patients.
For assessing the degree of incomplete eyelid
closure, the patient was instructed to close their eyes naturally,
before the unclosed distance between the upper and lower eyelid
margins was measured with a ruler to determine the degree of
incomplete eyelid closure.
For assessing the incidence of complications,
complications such as exposure keratitis, eyelid hematoma,
conjunctival prolapse, trichiasis and eyelid-ball separation, were
all recorded.
Statistical analysis
The data were analyzed using SPSS 20.0 statistical
software (IBM Corp.) and are presented as the means ± standard
deviation. Comparisons between two groups were performed using an
independent t-test. Comparisons between two tissues from the same
individual were determined by paired t-test. Categorical variables
were summarized as numbers and compared by Fisher exact probability
method. P<0.05 was considered to indicate a statistically
significant difference. Illustrator CS6 software (version 16.0.0;
Adobe Systems, Inc.) was used for assembling the figures.
Results
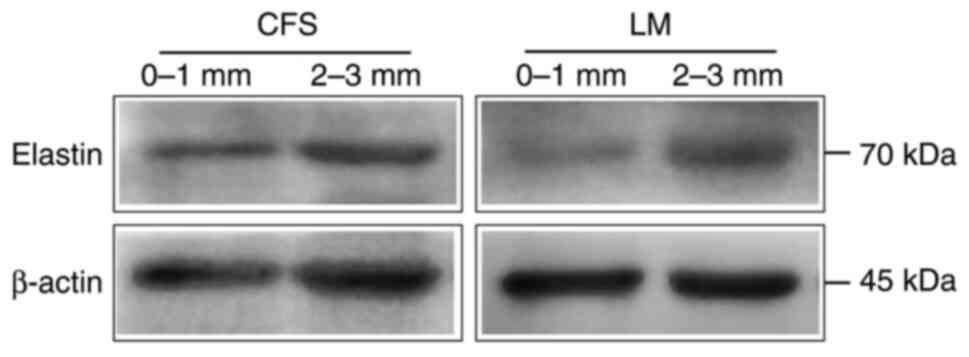
Comparison of elastin expression in
the CFS and LM between the groups
There were no significant differences in sex or age
between the two groups (Tables I
and II). Western blotting results
(Fig. 1; Table III) showed that compared with
that of the 0-1 mm group, the expression of elastin in the CFS of
the 2-3 mm group was increased, but the difference was not
statistically significant (P=0.125); however, the expression of
elastin in the LM of the 2-3 mm group was significantly increased
compared with that in the 0-1 mm group (P=0.021).
 | Table IComparison of the sex of the groups of
patients with different LM strengths (n=10). |
Table I
Comparison of the sex of the groups of
patients with different LM strengths (n=10).
| | Sex |
|---|
| Group | Male | Female |
|---|
| 0-1 mm | 7 | 3 |
| 2-3 mm | 8 | 2 |
| P-valuea | 1.000 | |
 | Table IIComparison of the age of the groups of
patients with different LM strengths (n=10). |
Table II
Comparison of the age of the groups of
patients with different LM strengths (n=10).
| Group | Age, years |
|---|
| 0-1 mm | 8.20±2.25 |
| 2-3 mm |
7.00±2.58a |
| t-value | 1.108 |
|
P-valuea | 0.283 |
 | Table IIIComparison of the expression of
elastin in the CFS and LM of the groups of patients with different
LM strengths (n=10). |
Table III
Comparison of the expression of
elastin in the CFS and LM of the groups of patients with different
LM strengths (n=10).
| Group | CFS | LM |
|---|
| 0-1 mm | 0.95±0.43 | 0.69±0.32 |
| 2-3 mm |
1.23±0.35a |
1.13±0.45a |
| t-value | -1.611 | -2.537 |
|
P-valuea | 0.125 | 0.021 |
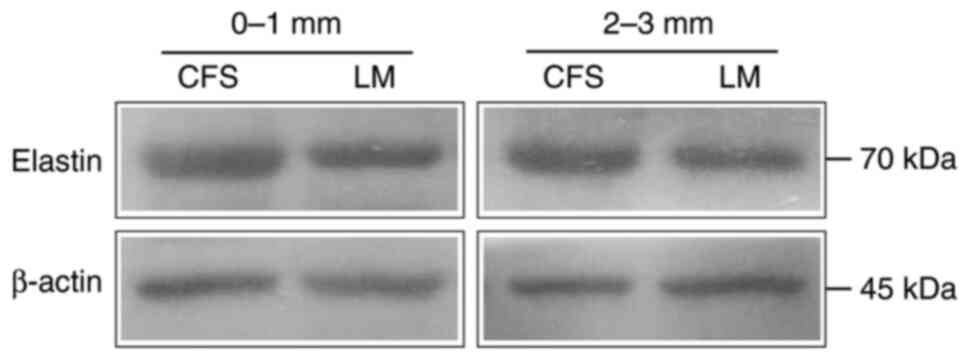
Comparison of elastin expression in the CFS and
LM within the groups. In both the 0-1 (P=0.005) and 2-3 mm
(P=0.009) groups, the expression level of elastin in the CFS was
significantly higher compared with that in the LM tissues (Fig. 2; Table IV).
 | Table IVComparison of the expression of
elastin in the CFS and LM of patients with the same LM strength
(n=10). |
Table IV
Comparison of the expression of
elastin in the CFS and LM of patients with the same LM strength
(n=10).
| Group | In 0-1 mm | In 2-3 mm |
|---|
| CFS | 1.33±0.41 | 1.54±0.62 |
| LM |
0.70±0.39a |
0.95±0.34a |
| t-value | 3.656 | 3.305 |
|
P-valuea | 0.005 | 0.009 |
Therapeutic effects. Within 6 months after
surgery, there were 9 patients (9 eyes) exhibiting good correction
and 1 patient (1 eye) with undercorrection in the 0-1 mm CFS + LM
group, yielding a 90% correction rate (Table V). In the 2-3 mm group, the good
correction rate of CFS + LM complex suspension surgery was 100%
(Table V). In addition, there were
no overcorrections or relapses in the two groups at the end of
follow-up (Table V).
 | Table VCurative effect within 6 months after
surgery (n=10). |
Table V
Curative effect within 6 months after
surgery (n=10).
| Group | Good
correction |
Undercorrection | Overcorrection | Relapse | Correction
rate |
|---|
| 0-1 mm | 9 | 1 | 0 | 0 | 90% |
| 2-3 mm | 10 | 0 | 0 | 0 | 100% |
Degree of incomplete eyelid closure. A total
of 6 months after surgery, the degree of incomplete eyelid closure
in the 2-3 mm group was significantly lower compared with that in
the 0-1 mm group (P=0.048; Table
VI), indicating that patients with an LM strength of 2-3 mm,
but not 0-1 mm, have improved closing function of the eyelid after
surgery.
 | Table VIUnclosed distance between the upper
and lower eyelid margins in the two groups at 6 months after
surgery (n=10). |
Table VI
Unclosed distance between the upper
and lower eyelid margins in the two groups at 6 months after
surgery (n=10).
| Group | Distance, mm |
|---|
| 0-1 mm | 1.80±0.63 |
| 2-3 mm |
1.20±0.63a |
| t-value | 2.121 |
|
P-valuea | 0.048 |
Incidence of complications. During the
6-month follow-up period, conjunctival prolapse was observed in 3
patients (3 eyes), including 2 patients in the 0-1 mm group and 1
patient in the 2-3 mm group (Table
VII). Those patients recovered after fixation of the prolapsed
conjunctiva to the corresponding eyelid with a vertical mattress
suture using 3-0 silk threads, which were removed after 14 days.
Other postoperative complications, such as exposure keratitis,
eyelid hematoma, trichiasis, and separation of the eyelid from the
eyeball, did not occur after CFS + LM complex suspension surgery,
as shown in Table VII.
 | Table VIIComplications in the two groups
during the whole follow-up period (n=10). |
Table VII
Complications in the two groups
during the whole follow-up period (n=10).
| Group | Exposure
keratitis | Eyelid
hematoma | Conjunctival
prolapse | Trichiasis | Eyelid-ball
separation | Total
complications |
|---|
| 0-1 mm | 0 | 0 | 2 | 0 | 0 | 2 |
| 2-3 mm | 0 | 0 | 1 | 0 | 0 | 1 |
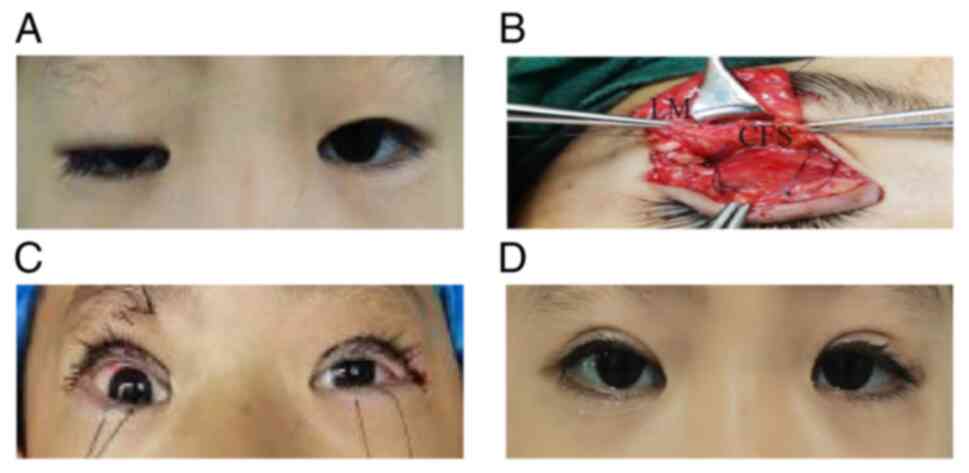
Presentation of representative patients. In
order to observe the postoperative effect of CFS + LM complex
suspension for correction of severe congenital ptosis, two patients
are presented.
Case presentation from the 0-1 mm group. An
8-year-old male patient was diagnosed with severe congenital ptosis
of the right eye. The LM strength was 0 mm in the right eye and 11
mm in the left eye. The superior rectus muscles of both eyes were
functional and Bell's sign was positive. CFS + LM complex
suspension of the right eye and double eyelid reconstruction of the
left eye were performed. Based on the evaluation of the height of
the palpebral fissure, the contour of the eyelid margin and the
formation of the double eyelid crease, it was concluded that the
postoperative appearance was satisfactory (Fig. 3).
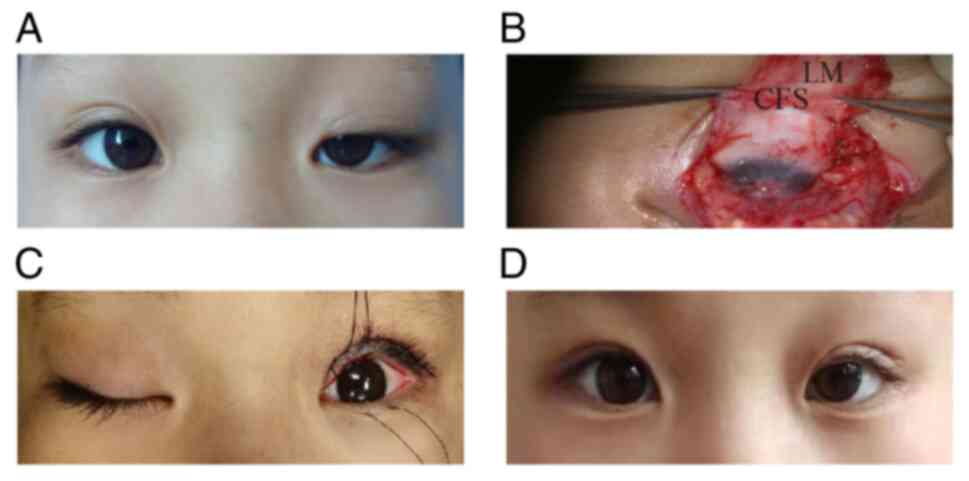
Case presentation from the 2-3 mm group. A
5-year-old female patient was diagnosed with severe congenital
ptosis of the left eye. The LM strength was 2 mm in the left eye
and 12 mm in the right eye. The superior rectus muscles of both
eyes were functional and Bell's sign was positive. CFS + LM complex
suspension of the left eye was performed and the effect of
postoperative correction was satisfactory (Fig. 4). The results demonstrated that
both patients with severe congenital ptosis with different LM
strength were corrected by surgery without complications.
Discussion
Ptosis is a common ophthalmic condition in which the
upper eyelid cannot be lifted, which can be due to congenital,
acquired LM dysfunction or loss of function (13,14).
Clinically, ptosis can be divided into three grades, namely mild,
moderate and severe, according to LM strength and position of the
upper eyelid margin (15). Severe
ptosis means that LM strength is <4 mm and the upper eyelid
margin covers the pupil by ≥50% (16). Due to the abnormal obscuration of
the optical axis by the upper eyelid at birth, children with severe
congenital ptosis are at serious risk of form-deprivation amblyopia
and refractive errors, especially in unilateral cases (17-19).
At present, severe congenital ptosis is typically
corrected with frontalis muscle suspension surgery (20). The method is to connect the
frontalis muscle with the tarsus, and use the strength of the
frontalis muscle to lift up the eyelids (21). However, certain complications, such
as incomplete eyelid closure, undercorrection and postoperative
keratitis, are common (21). The
main reason for these is that the direction of the traction force
of the frontal muscle during the correction of ptosis is vertical
upward, which changes the direction of the physiological force of
the upper eyelids (6,22). Over the past decade, CFS suspension
surgery has attracted considerable attention (23,24).
The safety, therapeutic and cosmetic effects of CFS suspension
surgery have been reported to be significantly superior compared
with those of traditional frontalis muscle suspension (4,25-26).
In addition, these results have been found to be closely associated
with the anatomical characteristics of the CFS. Previous anatomical
studies have shown that the CFS is attached to the superior
conjunctival fornix and is comprised of the fascia between the LM
and the superior rectus muscle (2,27).
When the eyeball looks upward and the upper eyelid is lifted, the
CFS, LM and superior rectus muscle exert a synergistic effect
(28). Therefore, the CFS is a
dynamic structure that is involved in lifting the upper eyelid.
This anatomical advantage of the CFS reduces the resistance during
eye closure after CFS suspension surgery, and therefore reduces
postoperative upper eyelid hysteresis to achieve good therapeutic
and cosmetic effects (22).
Furthermore, the correction of ptosis by CFS suspension is proposed
to be more effective at aligning with the physiological lifting of
the upper eyelid and is therefore safer, which to some extent
compensates for the shortcomings of frontalis muscle suspension
(29).
With the development of surgery, CFS + LM complex
suspension surgery is becoming increasingly common for correcting
severe congenital ptosis in children, since this surgical method
has been documented to achieve superior therapeutic effects
compared with those exerted by simple CFS suspension and frontalis
muscle suspension (7,9). Previous histological studies have
revealed that the CFS and LM are rich in collagen fibers and
elastic fibers, which may explain why the CFS and LM are elastic
and why CFS + LM complex suspension surgery can be used for severe
blepharoptosis (8,10,11).
Furthermore, the CFS tissue of children has significantly higher
elastin expression compared with that of adolescents and adults
(8). Higher elastin content
indicates an improved elasticity of the CFS and CFS + LM complex,
providing structural support for the use of CFS + LM complex in
pediatric patients. However, elastin expression in the CFS and LM
of pediatric patients with severe ptosis with different LM
strengths requires further exploration. To address this issue, the
present study measured and analyzed the relationship between the
expression levels of elastin and the surgical volume necessary to
accurately implement CFS + LM complex suspension surgery in
children with severe congenital ptosis.
It was found that in the 2-3 mm group, elastin
expression in the LM was significantly higher compared with that in
the 0-1 mm group, suggesting that the function of the LM is
superior in this group, due to higher elastin content, where the
two factors are positively associated. However, there was no
significant difference in the expression levels of elastin in the
CFS between the two groups. These results potentially provide a
theoretical basis for choosing the appropriate volume for ptosis
correction surgery according to LM strength. In the present study,
the standard surgical volume used for patients with LM strengths in
the range of 0-1 mm was a separation height of the CFS + LM complex
of 5-6 mm, and the upper eyelid margin was flat at the level of the
upper edge of the cornea. For patients with LM strengths in the
range of 2-3 mm, the surgical volume was a separation height of the
composite flap of 3-4 mm, and the upper eyelid margin covered the
cornea by 0.5-1 mm.
Furthermore, elastin expression in the CFS was found
to be significantly higher compared with that in the LM in both the
1-2 and 2-3 mm groups, suggesting that the elasticity of the CFS
was superior compared with that of the LM, especially in patients
with severe ptosis with higher LM strength. Elastin is the most
important structural component of elastic fibers, and its content
can reflect the elasticity of the tissue (30). It is therefore possible that the
CFS has a high content of elastin, whereas the LM may also contain
a certain degree of elastin that is superimposed with the CFS in
pediatric patients with severe congenital ptosis, consistent with
the findings of a previous study (11). The LM firmly adheres to the orbital
apex, towards which it exerts strong suspending force and traction
(31). Combined with the
histological evidence, the CFS + LM complex had good elasticity,
flexibility and traction, which rendered the postoperative upper
eyelid position more stable.
In the present study, the postoperative follow-up
duration was 6 months. The good correction rate, the degree of
incomplete eyelid closure and the incidence of complications were
then recorded. Within 6 months after surgery, the correction rate
of the 2-3 mm group was 100%. In the 0-1 mm group, 1 patient (1
eye) experienced mild undercorrection, yielding a 90% correction
rate. The reason for this undercorrection may be excessive
retraction caused by early postoperative eye movement or suture
loosening. In terms of incomplete closure, the degree of eyelid
closure in the 2-3 mm group was higher compared with that in the
1-2 mm group, suggesting that the increased LM strength is
conducive to eyelid closure. In terms of surgical complications,
conjunctival prolapse is a common complication of CFS + LM complex
suspension surgery (6). Of the 20
patients enrolled to the present study, 3 patients (3 eyes)
experienced upper fornix conjunctival prolapse within 1 week after
surgery. The main cause was that the upper fornix conjunctival
tissue developed edema postoperatively and detached from the
suspensory ligament due to gravity. However, these patients
recovered after the fixation of the prolapsed conjunctiva to the
corresponding eyelid. Other postoperative complications, such as
exposure keratitis, eyelid hematoma, trichiasis, and eyelid-ball
separation, did not occur. The clinical observation results of this
study suggest that CFS + LM complex suspension surgery is safe and
effective.
Congenital ptosis is mainly caused by the lack of LM
development, resulting in difficulty lifting the upper eyelid
(14). It has previously been
proposed that LM strength represents LM function and its damage
degree (32,33). Consistent with this hypothesis, in
the present study LM strength and its elastin content were found to
be positively associated. From a clinical point of view, when the
muscle strength of LM is 2-3 mm in patients with severe ptosis, it
indicates that the elastic fibers are functioning adequately, since
the expression level of elastin is high. By contrast, when the
muscle strength is 0-1 mm, the expression level of elastin is low.
However, from the perspective of molecular mechanisms, additional
evidence is needed. In subsequent studies, morphological staining
and structural analysis of the tissues is required.
In conclusion, the results of the present study
suggested that elastin expression in the CFS was higher compared
with that in the LM of children with severe congenital ptosis and
that elastin expression in the LM may be positively associated with
LM strength. However, elastin expression in the CFS had no clear
association with LM function. Therefore, adjusting the operation
volume in CFS + LM complex suspension surgery according to LM
strength appears feasible, which can achieve satisfactory
postoperative results in the correction of severe congenital ptosis
in children.
Acknowledgements
Not applicable.
Funding
Funding: The present study was sponsored by the Natural Science
Foundation of Beijing Municipality (grant no. 7194249), the Beijing
Outstanding Talent Training Foundation (grant no.
2018000021469G208) and the Xingtai City Science and Technology Key
Research and Development Project (grant no. 2023ZZ053 and
2023ZZ059).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
PB was responsible for the study conceptualization,
the surgical operation and manuscript review. XJ was responsible
for designing and performing experiments, and for the writing and
editing of the manuscript. ZL was responsible for the methodology
and data analysis. JS was responsible for the follow-up examination
and data acquisition. RP and MW were responsible for the literature
search and data interpretation. HW, HZ and SL were responsible for
data collection. PB and XJ confirm the authenticity of all the raw
data. All authors read and approved the final manuscript.
Ethics approval and consent to
participate
The present study adheres to the tenets of The Code
of Ethics of the World Medical Association (Declaration of
Helsinki) for research involving humans and was reviewed and
approved by the Ethics Committee of Hebei Eye Hospital (approval
no. 2020KY013; Xingtai, China). Written informed consent for
participation was obtained from the participant and the minor(s)'
legal guardian, for the publication of any potentially identifiable
images or data included in this article.
Patient consent for publication
Written informed consent for publication of their
clinical details and clinical images was obtained from the legal
guardian of the participants aged <18 years.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Finsterer J: Ptosis: Causes, presentation,
and management. Aesthetic Plast Surg. 27:193–204. 2003.PubMed/NCBI View Article : Google Scholar
|
|
2
|
Hwang K, Shin YH and Kim DJ: Conjoint
fascial sheath of the levator and superior rectus attached to the
conjunctival fornix. J Craniofac Surg. 19:241–245. 2008.PubMed/NCBI View Article : Google Scholar
|
|
3
|
Holmstrom H and Santanelli F: Suspension
of the eyelid to the check ligament of the superior fornix for
congenital blepharoptosis. Scand J Plast Reconstr Surg Hand Surg.
36:149–156. 2002.PubMed/NCBI View Article : Google Scholar
|
|
4
|
Sang PF, Fang MS, Li X, Liu C and Xi Q:
Treatment of severe ptosis by conjoint fascial sheath suspension.
Biomed Res Int. 19(1837458)2021.PubMed/NCBI View Article : Google Scholar
|
|
5
|
Yue Q, Fu A and Wang TL: Efficacy and
safety of surgical procedures for congenital moderate and severe
Blepharoptosis: A network meta-analysis. J Craniofac Surg.
34:2363–2368. 2023.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Shi J, Liu Z, Li Y, Song L, Li Y, Yang J,
Pang R, Zhang H, Xiao L and Bai P: Efficacy of combined conjoint
fascial sheath and levator muscle composite flap suspension for
congenital severe ptosis. Plast Reconstr Surg Jul: 25, 2023 (Epub
ahead of print). doi: 10.1097/PRS.0000000000010947, 2023.
|
|
7
|
Shi JH, Liu S and Liu ZC: Effect of the
novel combined fascial sheath and levator palpebrae muscle
composite flap suspension for congenital severe blepharoptosis. Chi
J Aesthet Med. 29:23–27. 2020.(In Chinese).
|
|
8
|
Liu Z, Jia X, Pang R, Wang H, Shi J and
Bai P: Research on the expression of elastin in the conjoint
fascial sheath for the correction of severe unilateral congenital
blepharoptosis. BMC Ophthalmol. 22(256)2022.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Xing Y, Wang X, Cao Y, Ding X, Lin M, Li J
and Fan X: Modified combined fascial sheath and levator muscle
complex suspension with Müller muscle preservation on treating
severe congenital ptosis. Ann Plast Surg. 82:39–45. 2019.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Li B, Yang J, Wu W, Chai C, Gu Z, He Z,
Tan Z, Cheng S, Lu P and Zeng L: Anatomical and histological study
of the conjoint fascial sheath of the levator and superior rectus
for ptosis surgery. Ophthalmic Plast Reconstr Surg. 36:617–620.
2020.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Pang RH, Wang J and Shi JH: Pathological
and clinical observation of conjoint fascial sheath in severe
ptosis. J Pract Med. 37:1641–1644. 2021.
|
|
12
|
Mithieux SM and Weiss AS: Elastin. Adv
Protein Chem. 70:437–461. 2005.PubMed/NCBI View Article : Google Scholar
|
|
13
|
Harvey DJ, Iamphongsai S and Gosain AK:
Unilateral congenital blepharoptosis repair by anterior levator
advancement and resection: An educational review. Plast Reconstr
Surg. 126:1325–1331. 2010.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Patel K, Carballo S and Thompson L:
Ptosis. Dis Mon. 63:74–79. 2017.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Harvey DJ, Iamphongsai S and Gosain AK:
Unilateral congenital blepharoptosis repair by anterior levator
advancement and resection: An educational review. Plast Reconstr
Surg. 126:1325–1331. 2010.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Qiu Y, Sun D, Pan P, Jin Y, Cai L, Yang J,
Lin D and Liu F: Conjoint fascial sheath suspension for severe
blepharoptosis through palpebral margin incision. Aesthetic Plast
Surg. 46:2301–2309. 2022.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Griepentrog GJ, Diehl N and Mohney BG:
Amblyopia in childhood eyelid ptosis. Am J Ophthalmol.
155:1125–1128. 2013.PubMed/NCBI View Article : Google Scholar
|
|
18
|
Hsia NY, Wen LY, Chou CY, Lin CL, Wan L
and Lin HJ: Increased risk of refractive errors and amblyopia among
children with ptosis: A nationwide population-based study. J Clin
Med. 11(2334)2022.PubMed/NCBI View Article : Google Scholar
|
|
19
|
Bremond-Gignac D: Unilateral ptosis in
children. Rev Prat. 70:993–996. 2020.PubMed/NCBI(In French).
|
|
20
|
Bee YS, Tsai PJ, Lin MC and Chu MY:
Factors related to amblyopia in congenital ptosis after frontalis
sling surgery. BMC Ophthalmol. 18(302)2018.PubMed/NCBI View Article : Google Scholar
|
|
21
|
Lee JH and Kim YD: Surgical treatment of
unilateral severe simple congenital ptosis. Taiwan J Ophthalmol.
8:3–8. 2018.PubMed/NCBI View Article : Google Scholar
|
|
22
|
Bing L: Progress in the operative therapy
of congenital blepharoptosis. J Tissue Engineering and
Reconstructive Surgery. 13:279–282. 2017.
|
|
23
|
Wang H, Liu L and Wang ZJ: Conjoint
fascial sheath suspension for early correction of severe
blepharoptosis after double-eyelid blepharoplasty. Br J Oral
Maxillofac Surg. 58:966–969. 2020.PubMed/NCBI View Article : Google Scholar
|
|
24
|
Zhou J, Chen W, Qi Z and Jin X: Minimally
invasive conjoint fascial sheath suspension for blepharoptosis
correction. Aesthetic Plast Surg. 43:956–963. 2019.PubMed/NCBI View Article : Google Scholar
|
|
25
|
Zhao YN, Ge HG and Shen QL: Comparative
study on conjoint fascial sheath suspension and the simple
frontalis muscle suspension for moderate or severe ptosis. Int Eye
Sci. 17:1790–1792. 2017.
|
|
26
|
Pan XH, Wei T, Wang XD and Xu C: Clinical
efficacy of conjoint fascial sheath suspension and frontalis muscle
suspension in treating moderate or severe congenital ptosis and the
effects on ocular surface and refractive status. Exp Ther Med.
20:3278–3284. 2020.PubMed/NCBI View Article : Google Scholar
|
|
27
|
Hwang K: Surgical anatomy of the upper
eyelid relating to upper blepharoplasty or blepharoptosis surgery.
Anat Cell Biol. 46:93–100. 2013.PubMed/NCBI View Article : Google Scholar
|
|
28
|
Zhuang W, Fang S, Fan H, Zhu W, Chen Y,
Tang W, Liu C, Liu X, Zhang Z, Xing X and Yang C: Anatomical study
of the extraocular check ligament system. J Plast Reconstr Aesthet
Surg. 72:2017–2026. 2019.PubMed/NCBI View Article : Google Scholar
|
|
29
|
Li Y, Wang HX and Bai P: Changes of ocular
surface before and after treatment of blepharoptosis with combined
fascial sheath suspension and frontal muscle flap suspension. J
Craniofac Surg. 32:e698–e701. 2021.PubMed/NCBI View Article : Google Scholar
|
|
30
|
Vindin H, Mithieux SM and Weiss AS:
Elastin architecture. Matrix Biol. 84:4–16. 2019.PubMed/NCBI View Article : Google Scholar
|
|
31
|
Ng SK, Chan W, Marcet MM, Kakizaki H and
Selva D: Levator palpebrae superioris: An anatomical update. Orbit.
32:76–84. 2013.PubMed/NCBI View Article : Google Scholar
|
|
32
|
Pereira LS, Hwang TN, Kersten RC, Ray K
and McCulley TJ: Levator superioris muscle function in involutional
Blepharoptosis. Am J Ophthalmol. 145:1095–1098. 2008.PubMed/NCBI View Article : Google Scholar
|
|
33
|
Lai HT, Weng SF, Chang CH, Huang SH, Lee
SS, Chang KP and Lai CS: Analysis of levator function and ptosis
severity in involutional Blepharoptosis. Ann Plast Surg. 78 (Suppl
23):S58–S60. 2017.PubMed/NCBI View Article : Google Scholar
|