Introduction
Following a burn, the skin loses its defensive
capacity, which predisposes it to infection and a series of
complications, such as burn sepsis and bacteremia, thus increasing
the mortality rate of patients (1). At present, with the development of
science and technology, an increasing number of treatment methods
are available for burns. Currently, the main treatment modality is
the application of autologous skin grafting. However, the healing
of split-thickness skin grafts (STSGs) following burn injury is
often accompanied by scar growth, leading to joint contracture
deformities and significantly affecting hand function (2). The present study observed that after
early allograft or xenograft coverage in patients with large
surface area deep second-degree burns on the dorsum of the hand,
thin intermediate thickness skin grafts (ITSGs), rather than full
thickness skin grafts (FTSGs), were used to repair the wounds, due
to the lack of skin source (3). In
patients who adhered to anti-scarring therapy and functional
exercises, no significant limitation of hand function was observed
during the long-term follow-ups (4). The misjudgment of tissue health
status and the residual of necrotic tissue in early stage surgical
treatment would directly affect the survival of skin grafts
(5,6). Thus, phased surgery circumvents those
problems, further improves functional reconstruction of the hand
following burns and increases the survival rate of skin grafts. The
present study attempted to determine the impact of phased skin
graft repair of wounds on patients with burns. Due to the variation
in damage to the donor area caused by the use of skin grafts of
varying thickness, the possibility of reducing the damage to the
donor site while preserving the functional recovery of the dorsum
of the hand was investigated. The present study also attempted to
analyze the effect of phased surgery on inflammatory indicators.
Patients with deep second-degree burns and indications for skin
grafting surgery were selected for the present study. As some
third-degree burns of the hand may be accompanied by exposed bone
and tendons, flap transfer repair is often required to ensure
function recovery. The survival rate of ITSGs over burn wounds was
lower compared with that of STSGs. Thin ITSGs on patients with deep
second-degree burns on the dorsum of the hand can improve the
survival rate, reduce damage to the donor area (7,8) and
cause no significant functional limitations following wound healing
with anti-scar therapy and exercise (9). In the present study, 64 patients with
deep second-degree burns on the dorsum of the hand admitted to
Guangzhou Red Cross Hospital between January 2020 and March 2023
were enrolled, and the safety and effectiveness of covering with
allogeneic (porcine) skin in phase I and then transplantation of
autologous thin ITSGs in phase II were analyzed.
Materials and methods
Patients
A total of 64 patients with dorsal hand burns
admitted to Guangzhou Red Cross Hospital (Guangzhou, China) between
January 2020 and March 2023 were enrolled in the present study.
This study complied with the ethical guidelines of the Declaration
of Helsinki and was approved by the Clinical Ethics Committee of
Guangzhou Red Cross Hospital (Guangzhou, China; approval no.
2021-153-01). All enrolled patients provided written informed
consent. The inclusion criteria were as follows: i) Complete data;
ii) diagnostic criteria for deep second-degree burns of the dorsal
hand with clear surgical indications; iii) first surgery at the
trauma location, admitted to the unit within 7 days from injury;
iv) high compliance and normal cognitive function; v) 2%≤ burn area
≤10%; vi) young-adult males aged 18-45 years (mean age, 33.1±2.4
years). The exclusion criteria were as follows: i) Abnormal
coagulation; ii) liver and kidney dysfunction; iii) malignant
tumors; iv) ulcers or severe infection symptoms at the burn site;
v) no third-degree burn trauma.
Methods
One week after the patients' injury, the allogeneic
(porcine) skin [artificial skin-genetically transfected porcine
skin (skin patch)] was used to cover the trauma during phase I
treatment. The allogeneic (porcine) skin was thawed and washed
repeatedly, and small holes were poked in it for drainage; the
necrotic scab on the back of the hand was excised and treated with
adequate hemostasis, followed by repeated rinsing with 0.5%
povidone iodine (PVP-I) and saline successively. After checking
that there was no active bleeding, the xenograft (pig) skin was
implanted according to the wound shape, and the edges were sutured
and fixed with finger compression dressing and immobilization.
Postoperative anti-infection treatment was provided, and the phase
II surgery was performed 7 days after the completion of the phase I
surgery. The suture at the edge of the xenograft (porcine) skin was
removed, the xenograft was carefully separated to avoid tearing the
newly formed granulation tissue. Careful observation was made to
check for any remaining necrotic tissue or residual xenograft. The
wound surface was lightly scraped to induce slight bleeding,
followed by repeated rinsing with 0.5% PVP-I and normal saline.
Once there was no active bleeding, the size of the dorsal hand
wound was measured, and a large thin ITSGs (~0.45 mm thick) was
harvested from the anterior lateral aspect of the contralateral
thigh. The graft was implanted according to the shape of the wound,
and the edges were sutured for fixation. Finger compression on
dressing and immobilization, as well as postoperative
anti-infection treatment, were performed. The dressings were
removed after 7 days.
Observation indices
The wound healing time was calculated from the
beginning of the post-injury period. 7-day survival and infection
rates following phase II skin grafting: The survival rate was
calculated as a percentage of the grafting area, with no dressing
change considered as 100% survival. The complications were as
follows: i) Infection rate on the first dressing removal for trauma
culture after stage II surgery, with the detection of bacteria or
fungi considered as 100% infection; ii) displacement of skin
pieces: Comparison of intraoperative grafts appeared to be
displaced; iii) subcutaneous blood accumulation: Incomplete
hemostasis or uneven pressure led to subcutaneous blood
accumulation, followed by skin piece inactivation; iv) inflammatory
index: Fasting venous blood was taken 2 days before and after phase
I surgery, and 2 days before and after phase II surgery, and the
levels of white blood cell (WBC), C-reactive protein (CRP) and IL-6
were measured. v) Vancouver Scar Scale (VSS) at the 6-month
postoperative follow-up, where 0-5 was considered significantly
effective, 6-10 effective and 11-15 ineffective [the effective
rate=(the number of significant cases + the number of effective
cases)/total cases x100] (10).
vi) At the 6-month postoperative follow-up, the satisfaction
questionnaire was used to assess patient satisfaction: >85
points, very satisfied; 65-85 points, satisfied; <65 points,
unsatisfied [satisfaction=number of (very satisfied + satisfied)
cases/total number of cases x100] (11).
Statistical analysis
Data were processed using SPSS 24.0 statistical
software (IBM Corp.). ANOVA with repeated measures was used for
comparisons among multiple time points, and Bonferroni's post-hoc
test was used for post-hoc test. P<0.05 was considered to
indicate a statistically significant difference.
Results
Wound healing time
The mean healing time was 21.94 days, with 23 cases
undergoing phase I surgery 7 days after injury, 21 cases undergoing
phase I surgery 8 days after injury, 16 cases undergoing phase I
surgery 9 days after injury, 2 cases undergoing phase I surgery 10
days after injury, 1 case undergoing phase I surgery 11 days after
injury, and 1 case undergoing phase I surgery 12 days after injury.
The patients who underwent surgery 10-12 days after injury were all
transferred to the Guangzhou Red Cross Hospital 5-7 days after
injury, and the remaining patients were admitted to the Guangzhou
Red Cross Hospital immediately after injury or within 2 days from
injury.
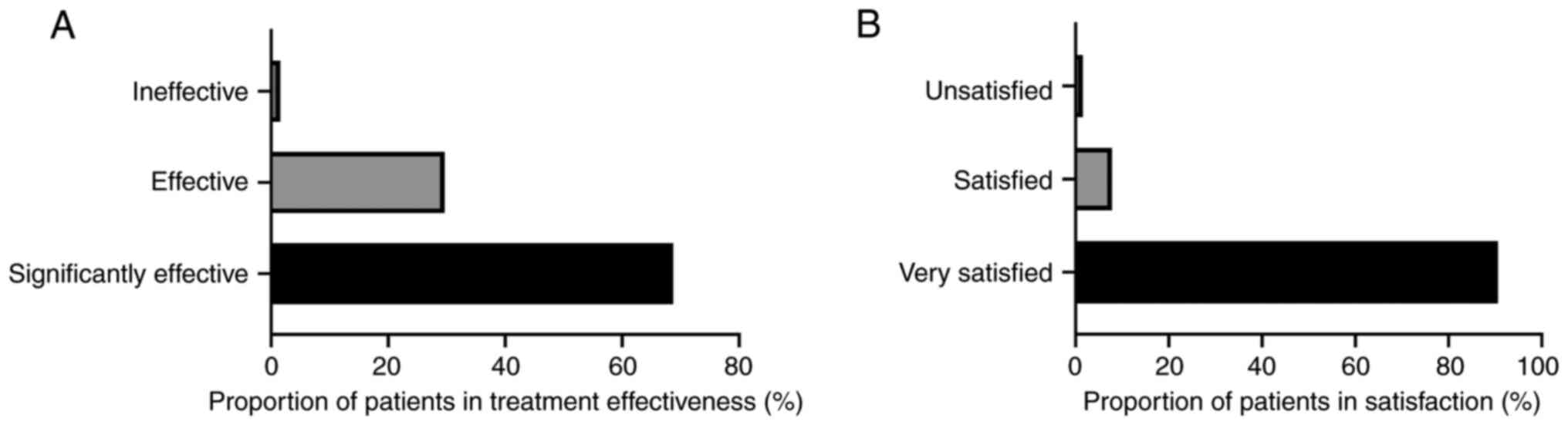
Complication rate, treatment effect
and patient satisfaction
The survival rate of all 64 surgical patients was
>95%, with a survival rate of 98.66%, and no patients presented
with skin fragment displacement, pressure inactivation or
infection. According to the VSS, 44 cases were considered
significantly effective (score, 0-5), 19 cases were considered
effective (score, 6-10), and 1 case was considered ineffective
(score, 11-15), with an effectiveness rate of 98.44%. In addition,
58 surgical patients were very satisfied, 5 surgical patients were
satisfied and 1 surgical patient was dissatisfied, with a
satisfaction rate of 98.43% (Fig.
1).
Observation of infection and
inflammatory indices
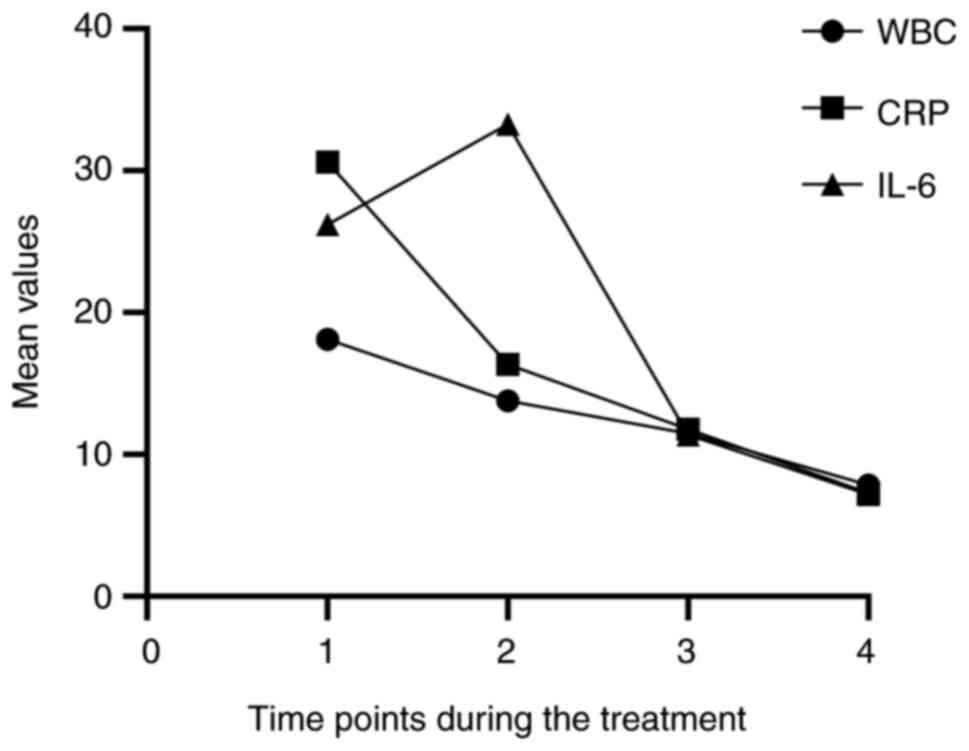
The levels of inflammatory markers WBC, CRP and IL-6
in 64 patients exhibited a decreasing trend at the four time-points
(2 days before and after phase I surgery, and 2 days before and
after phase II surgery) (Fig. 2).
WBC levels were significantly different among the four time-points
(P<0.001), and the WBC 2 days after phase II surgery was
significantly lower than the level at the other three time-points
(P<0.001). There was a significant difference in CRP among the
four time-points (P<0.001), and the CRP of patients 2 days after
phase II surgery was significantly lower than that of the other
three time-points (P<0.001). There was no statistical difference
in IL-6 among the four time-points (P=0.160) (Table I, Table II and Table III).
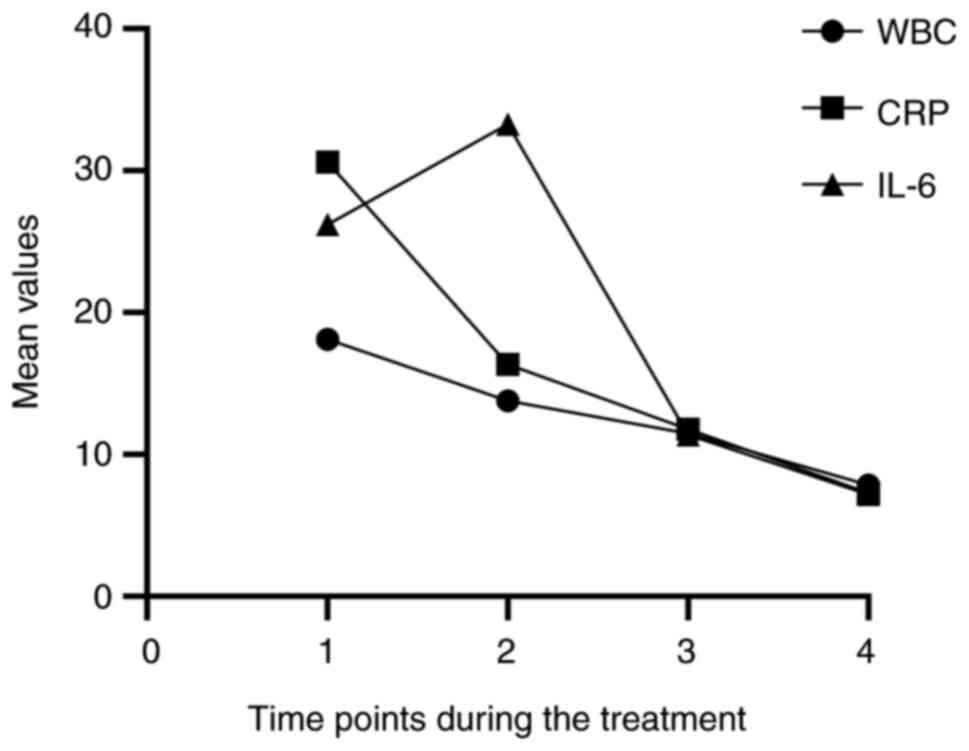 | Figure 2Temporal changes in the mean of three
inflammatory markers (WBC, CRP, IL-6). The change in the mean
values of the three inflammatory markers over time is shown. It can
be found that the three inflammatory markers gradually decreased
with time. Time points 1,2,3,4, represent 2 days before and after
phase I surgery, and 2 days before and after phase II surgery,
respectively. WBC, white blood cell; CRP, C-reactive protein. |
 | Table IRepeated measurement of WBC of
patients at 2 days before and after phase I surgery and 2 days
before and after phase II surgery. |
Table I
Repeated measurement of WBC of
patients at 2 days before and after phase I surgery and 2 days
before and after phase II surgery.
| WBC (<10) | Mean | Standard
deviation | F value | P-value |
|---|
| 2 days prior phase I
surgery | 18.1280 | 2.63841 | 508.365 | <0.001 |
| 2 days post phase I
surgery | 13.7917 | 1.80955 | | |
| 2 days prior phase II
surgery | 11.4744 | 1.34734 | | |
| 2 days post phase II
surgery | 7.8480 | 1.31109 | | |
 | Table IIRepeated measurements of CRP of
patients at 2 days before and after phase I surgery, and 2 days
before and after phase II surgery. |
Table II
Repeated measurements of CRP of
patients at 2 days before and after phase I surgery, and 2 days
before and after phase II surgery.
| CRP (<7) | Mean | Standard
deviation | F value | P-value |
|---|
| 2 days prior phase I
surgery | 30.6020 | 19.83975 | 81.672 | <0.001 |
| 2 days post phase I
surgery | 16.3586 | 5.04698 | | |
| 2 days prior phase II
surgery | 11.7677 | 2.77063 | | |
| 2 days post phase II
surgery | 7.2847 | 2.27631 | | |
 | Table IIIRepeated measurements of patients'
IL-6 at 2 days before and after phase I surgery, and 2 days before
and after phase II surgery. |
Table III
Repeated measurements of patients'
IL-6 at 2 days before and after phase I surgery, and 2 days before
and after phase II surgery.
| IL-6 (<7) | Mean | Standard
deviation | F value | P-value |
|---|
| 2 days prior phase I
surgery | 26.2131 | 15.20918 | 2.018 | 0.160 |
| 2 days post phase I
surgery | 33.2956 | 137.06445 | | |
| 2 days prior phase II
surgery | 11.3713 | 2.27474 | | |
| 2 days post phase II
surgery | 7.1795 | 2.02553 | | |
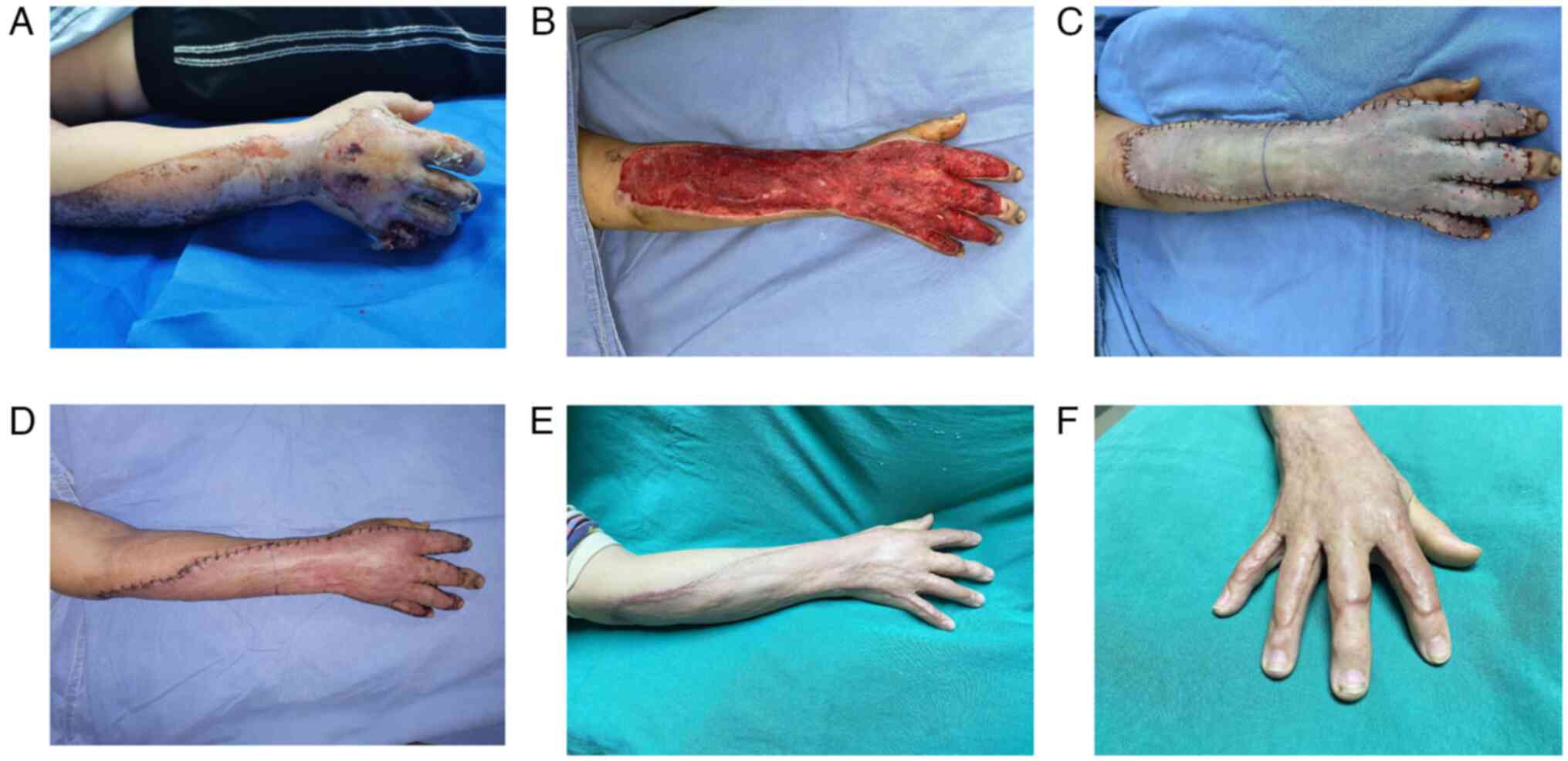
One typical case
A male patient aged 31 years was scalded on his
right forearm and right dorsum due to hot plastic dumping, and was
treated with anti-infection and local dressing change on the wound
following the injury. The patient was transferred to Guangzhou Red
Cross Hospital (Guangdong, China) 2 days after the injury and was
administered silver sulfadiazine cream and Vaseline oil gauze with
finger dressing. The dressing was replaced on alternate days. At 9
days after the injury, the patient underwent phase I debridement
and xenograft skin coverage treatment, and the dressing was changed
on alternate days. Then, 7 days after the surgery, the patient
underwent phase II debridement and autologous thin ITSG. The
dressing was removed 7 days after the surgery, and all the skin
grafts were well established. The patient was satisfied with the
result, and his hand function recovered almost completely (Fig. 3).
Discussion
Burns, which can lead to damage to the skin mucosa
and deep tissues, are one of the most common occurrences in
surgical practice. There is now a consensus for early surgical
treatment of deep burn wounds, with the functional recovery of the
hand being particularly important for patients. For deep
second-degree burn wounds on the hand, the traditional surgical
approach is FTSGs or ITSGs after incision, to ensure the hand
function recovers. Skin grafting of burn patients belongs to
contaminated surgery thus the grafting area of the patients is easy
to become infected and causing its inactivation. Simultaneous phase
I skin grafting may lead to misjudgment of the tissue health
status, residual necrotic tissue or the excision of too much normal
tissue. In addition, it is often the case that some necrotic tissue
left behind might lead to the inability of all skin grafts to be
viable in phase I. In a previous study, the necrotic tissue was
removed as thoroughly as possible during phase I surgery and
cleared again during phase II surgery (based on the condition of
the wound), leading to a reduction of the occurrence of
inflammatory reactions and residual necrotic tissues affecting the
survival of the skin grafts and improving the survival rate of the
skin grafts (12). The results of
the present study showed that the treatment of allogeneic skin
coverage after early debridement and scabbing, followed by
autologous thin ITSGs in phase II to repair deep second-degree
burns on the dorsum of the hand, achieved improved results in terms
of attenuating scar formation, restoring hand function and
improving appearance following wound healing with high
satisfaction.
In general, patients with burns experience large
changes in body functions with a significant inflammatory response,
which can lead to a significant imbalance of inflammatory factors.
Continuous inflammatory response during this period can affect hand
function, and the pathologically proliferative contracture of the
scar following healing may also result in a local inflammatory
response that further affects dorsal hand function (13,14).
In general, allogeneic skin coverage following phase I surgical
debridement can reduce the release of inflammatory mediators and
establish a good foundation for autologous skin grafts in phase II,
which is conducive to the functional recovery of the dorsum of the
hand. With regard to the effect on the inflammatory response of
patients, WBC, CRP and IL-6 gradually decreased at the four
time-points (2 days before and after phase I surgery, and 2 days
before and after phase II surgery) and the WBC and CRP levels of
patients at the four time-points were statistically different in
the present study. Various factors influence the systemic
inflammatory response, with the severity of the burn often being
the most important factor. The inflammatory response tends to
diminish with time following the injury. Surgical trauma can be an
aggravating factor, but the removal of necrotic tissue and
effective coverage are also mitigating factors. In the present
study, only the patients with 2%≤ burn area ≤10% were selected in
an attempt to minimize the complications caused by severe burns;
however, there were patients with only 3% burn area who had the
higher inflammatory response indexes in the 2 days before phase I
surgery, so the sample size and the variety of inflammatory indices
still need to be increased for further observation. By analyzing
only the currently available data, phased surgical repair treatment
was able to reduce the inflammatory response of patients and
maintain the balance between each factor, which can enhance
treatment efficacy and improve prognosis (15).
Deep burns in functional areas are often repaired
using FTSGs/ITSGs, possibly due to the low prevalence of regular
anti-scarring therapy and functional exercise (16). However, in the Burns and Plastic
Department of Guangzhou Red Cross Hospital, burn patients are
routinely administered anti-scar treatment and functional exercise
after wound healing. In the present study, all patients had regular
follow-up visits for anti-scar treatment and functional exercises.
This could have been one of the factors that aided the healing of
hand function via thin ITSGs transplantation (17).
The present study indicated that patients with deep
second-degree burns of the hand are not significantly dysfunctional
following clinical wound repair using thin ITSGs transplantation
plus adherence to anti-scarring therapy and functional exercises.
The authors look forward to conducting more relevant retrospective
analyses and extended studies in the future. Based only on the
currently available data, phase I allogeneic (porcine) skin grafts
and phase II autologous thin ITSGs in patients with deep
second-degree burns on the dorsum of the hand are ideal for
treatment, as they can significantly reduce inflammatory reaction
and improve patient prognosis. Following regular anti-scarring
treatment and functional exercises, hand function was restored in
the present study with satisfactory results.
Acknowledgements
Not applicable.
Funding
Funding: The present study was supported by 2023 city-school
(college) enterprise joint funding project (grant no.
2023A03J0526), New Exploration of sepsis target Therapy Research
project by China Red Cross Foundation, Medical Empowerment Public
Welfare Special Fund (grant no. HSZH202200909), Guangdong Yiyang
Health Charity Foundation, 2022 Charity and public welfare Medical
Clinical Research Project, (grant no. JZ2022008) and Guangzhou
Science and Technology Project (grant no. 202102010046).
Availability of data and materials
The data generated in the present study may be
requested from the corresponding author.
Authors' contributions
JES and SMS wrote the manuscript and contributed to
the data analysis and interpretation. SSJ, GL and ZZ collected data
and information of the case, and confirmed the authenticity of all
the raw data. WHL and SYZ designed research and approved the final
version of the manuscript. All authors read and approved the final
manuscript.
Ethics approval and consent to
participate
The present study was complied with the ethical
guidelines of the Declaration of Helsinki and was approved by the
Clinical Ethics Committee of Guangzhou Red Cross Hospital (approval
no. 2021-153-01) Written informed consent was obtained from all the
participants.
Patient consent for publication
Consent for publication was obtained from the
patients.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Guchlerner M, Brockmann MA and Pitz S:
Periocular necrobiotic xanthogranuloma with mono- and biclonal
gammopathy. Klin Monbl Augenheilkd. 237:41–45. 2020.PubMed/NCBI View Article : Google Scholar : (In German).
|
|
2
|
Wang KA, Wu GS, Sun Y and Xia ZF: Advances
in the research of prevention and treatment of postburn
contractures of hand. Zhonghua Shao Shang Za Zhi. 33:58–61.
2017.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|
|
3
|
Li G, Li YY and Sun JE: Comparison of the
efficacy of allogeneic (porcine) skin covering followed by
second-stage implantation method and normal one-stage implantation
method in the treatment of refractory wounds. Modern Diagnosis
Ther. 30:2790–2792. 2019.
|
|
4
|
Argirova M and Hadzhiyski O: Acute dorsal
hand burns in children. Ann Burns Fire Disasters. 19:22–25.
2006.PubMed/NCBI
|
|
5
|
Ciudad P, Date S, Orfaniotis G, Dower R,
Nicoli F, Maruccia M, Lin SP, Chuang CY, Chuang TY, Wang GJ and
Chen HC: Delayed grafting for banked skin graft in lymph node flap
transfer. Int Wound J. 14:125–129. 2017.PubMed/NCBI View Article : Google Scholar
|
|
6
|
Snelling CF: Delayed skin graft
application following burn scar release of the face and hand. Ann
Plast Surg. 10:349–358. 1983.PubMed/NCBI View Article : Google Scholar
|
|
7
|
Sun L and Patel AJ: Outcomes of split vs.
full-thickness skin grafts in scalp reconstruction in outpatient
local anaesthetic theatre. Scars Burn Heal.
7(20595131211056542)2021.PubMed/NCBI View Article : Google Scholar
|
|
8
|
Kanapathy M and Mosahebi A: Comparative
study on the donor site aesthetic outcome between epidermal graft
and split-thickness skin graft. Int Wound J. 16:354–359.
2019.PubMed/NCBI View Article : Google Scholar
|
|
9
|
Chan QE, Barzi F, Harvey JG and Holland
AJ: Functional and cosmetic outcome of full-versus split-thickness
skin grafts in pediatric palmar surface burns: A prospective,
independent evaluation. J Burn Care Res. 34:232–236.
2013.PubMed/NCBI View Article : Google Scholar
|
|
10
|
Baryza MJ and Baryza GA: The vancouver
scar Scale: An administration tool and its interrater reliability.
J Burn Care Rehabil. 16:535–538. 1995.PubMed/NCBI View Article : Google Scholar
|
|
11
|
Alsaif A, Karam M, Hayre A, Abul A,
Aldubaikhi A and Kahlar N: Full thickness skin graft versus split
thickness skin graft in paediatric patients with hand burns:
Systematic review and meta-analysis:. Burns. 49:1017–1027.
2022.PubMed/NCBI View Article : Google Scholar
|
|
12
|
Xu Z, Zhang Z, Wang B, Sun Y, Guo Y, Gao W
and Qin G: The application of delayed skin grafting combined
traction in severe joint cicatricial contracture. Zhonghua Zheng
Xing Wai Ke Za Zhi. 30:424–427. 2014.PubMed/NCBI(In Chinese).
|
|
13
|
Hong YK, Chang YH, Lin YC, Chen B, Guevara
BEK and Hsu CK: Inflammation in wound healing and pathological
scarring. Adv Wound Care (New Rochelle). 12:288–300.
2023.PubMed/NCBI View Article : Google Scholar
|
|
14
|
Zhang D, Li B and Zhao M: Therapeutic
strategies by regulating interleukin family to suppress
inflammation in hypertrophic scar and keloid. Front Pharmacol.
12(667763)2021.PubMed/NCBI View Article : Google Scholar
|
|
15
|
Enomoto A, Shimoide T, Kinoshita Y,
Sukedai M and Hamada S: Application of an oral appliance for
endotracheal tube fixation in facial burn patients. Br J Oral
Maxillofac Surg. 59:127–128. 2021.PubMed/NCBI View Article : Google Scholar
|
|
16
|
Flores O, Tyack Z, Stockton K and Paratz
JD: The use of exercise in burns rehabilitation: A worldwide survey
of practice. Burns. 46:322–332. 2019.PubMed/NCBI View Article : Google Scholar
|
|
17
|
Peng H, Liang PF and Wang :
Influences of different rehabilitative methods on function of hands
and psychological anxiety of patients with deeply burned hands
retaining denatured dermis and grafting large autologous skin.
Zhonghua Shao Shang Za Zhi. 33:272–276. 2017.PubMed/NCBI View Article : Google Scholar : (In Chinese).
|