|
1
|
Falk E: Pathogenesis of atherosclerosis. J
Am Coll Cardiol. 47:C7–C12. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Tedgui A and Mallat Z: Cytokines in
atherosclerosis: Pathogenic and regulatory pathways. Physiol Rev.
86:515–581. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Weber C and Noels H: Atherosclerosis:
Current pathogenesis and therapeutic options. Nat Med.
17:1410–1422. 2011. View
Article : Google Scholar
|
|
4
|
Lechner K, von Schacky C, McKenzie AL,
Worm N, Nixdorff U, Lechner B, Kränkel N, Halle M, Krauss RM and
Scherr J: Lifestyle factors and high-risk atherosclerosis: Pathways
and mechanisms beyond traditional risk factors. Eur J Prev Cardiol.
27:394–406. 2020. View Article : Google Scholar :
|
|
5
|
Shoeibi S: Diagnostic and theranostic
microRNAs in the pathogenesis of atherosclerosis. Acta Physiol
(Oxf). 228:e133532020. View Article : Google Scholar
|
|
6
|
Kunitomo M: Oxidative stress and
atherosclerosis. Yakugaku Zasshi. 127:1997–2014. 2007.In Japanese.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Li TT, Wang ZB, Li Y, Cao F, Yang BY and
Kuang HX: The mechanisms of traditional Chinese medicine underlying
the prevention and treatment of atherosclerosis. Chin J Nat Med.
17:401–412. 2019.PubMed/NCBI
|
|
8
|
Zarzycka B, Nicolaes GA and Lutgens E:
Targeting the adaptive immune system: New strategies in the
treatment of atherosclerosis. Expert Rev Clin Pharmacol. 8:297–313.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Wang C, Niimi M, Watanabe T, Wang Y, Liang
J and Fan J: Treatment of atherosclerosis by traditional Chinese
medicine: Questions and quandaries. Atherosclerosis. 277:136–144.
2018. View Article : Google Scholar
|
|
10
|
Vaidyanathan K and Gopalakrishnan S:
Nanomedicine in the diagnosis and treatment of atherosclerosis - a
systematic review. Cardiovasc Hematol Disord Drug Targets.
17:119–131. 2017. View Article : Google Scholar
|
|
11
|
Fasolo F, Di Gregoli K, Maegdefessel L and
Johnson JL: Non-coding RNAs in cardiovascular cell biology and
atherosclerosis. Cardiovasc Res. 115:1732–1756. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Varol C, Mildner A and Jung S:
Macrophages: Development and tissue specialization. Annu Rev
Immunol. 33:643–675. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Smigiel KS and Parks WC: Macrophages,
wound healing, and fibrosis: Recent insights. Curr Rheumatol Rep.
20:172018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Kuznetsova T, Prange KHM, Glass CK and de
Winther MPJ: Transcriptional and epigenetic regulation of
macrophages in atherosclerosis. Nat Rev Cardiol. 17:216–228. 2020.
View Article : Google Scholar :
|
|
15
|
Moore KJ and Tabas I: Macrophages in the
pathogenesis of atherosclerosis. Cell. 145:341–355. 2011.
View Article : Google Scholar :
|
|
16
|
Barrett TJ: Macrophages in atherosclerosis
regression. Arterioscler Thromb Vasc Biol. 40:20–33. 2020.
View Article : Google Scholar
|
|
17
|
Uccelli A, Moretta L and Pistoia V:
Mesenchymal stem cells in health and disease. Nat Rev Immunol.
8:726–736. 2008. View
Article : Google Scholar
|
|
18
|
Li J, Xue H, Li T, Chu X, Xin D, Xiong Y,
Qiu W, Gao X, Qian M, Xu J, et al: Exosomes derived from
mesenchymal stem cells attenuate the progression of atherosclerosis
in ApoE−/− mice via miR-let7 mediated infiltration and
polarization of M2 macrophage. Biochem Biophys Res Commun.
510:565–572. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kalluri R and LeBleu VS: The biology,
function, and biomedical applications of exosomes. Science.
367:eaau69772020. View Article : Google Scholar :
|
|
20
|
Sasaki R, Kanda T, Yokosuka O, Kato N,
Matsuoka S and Moriyama M: Exosomes and hepatocellular carcinoma:
From BENCH TO BEDside. Int J Mol Sci. 20:14062019. View Article : Google Scholar
|
|
21
|
Huang P, Wang L, Li Q, Tian X, Xu J, Xu J,
Xiong Y, Chen G, Qian H, Jin C, et al: Atorvastatin enhances the
therapeutic efficacy of mesenchymal stem cells-derived exosomes in
acute myocardial infarction via up-regulating long non-coding RNA
H19. Cardiovasc Res. 116:353–367. 2020. View Article : Google Scholar
|
|
22
|
Yue Y, Li YQ, Fu S, Wu YT, Zhu L, Hua L,
Lv JY, Li YL and Yang DL: Osthole inhibits cell proliferation by
regulating the TGF-β1/Smad/p38 signaling pathways in pulmonary
arterial smooth muscle cells. Biomed Pharmacother. 121:1096402020.
View Article : Google Scholar
|
|
23
|
Charles Richard JL and Eichhorn PJA:
Platforms for investigating lncRNA functions. SLAS Technol.
23:493–506. 2018.PubMed/NCBI
|
|
24
|
Tan J, Liu S, Jiang Q, Yu T and Huang K:
lncRNA-MIAT increased in patients with coronary atherosclerotic
heart disease. Cardiol Res Pract. 2019:62801942019. View Article : Google Scholar :
|
|
25
|
Liao J, Wang J, Liu Y, Li J and Duan L:
Transcriptome sequencing of lncRNA, miRNA, mRNA and interaction
network constructing in coronary heart disease. BMC Med Genomics.
12:1242019. View Article : Google Scholar
|
|
26
|
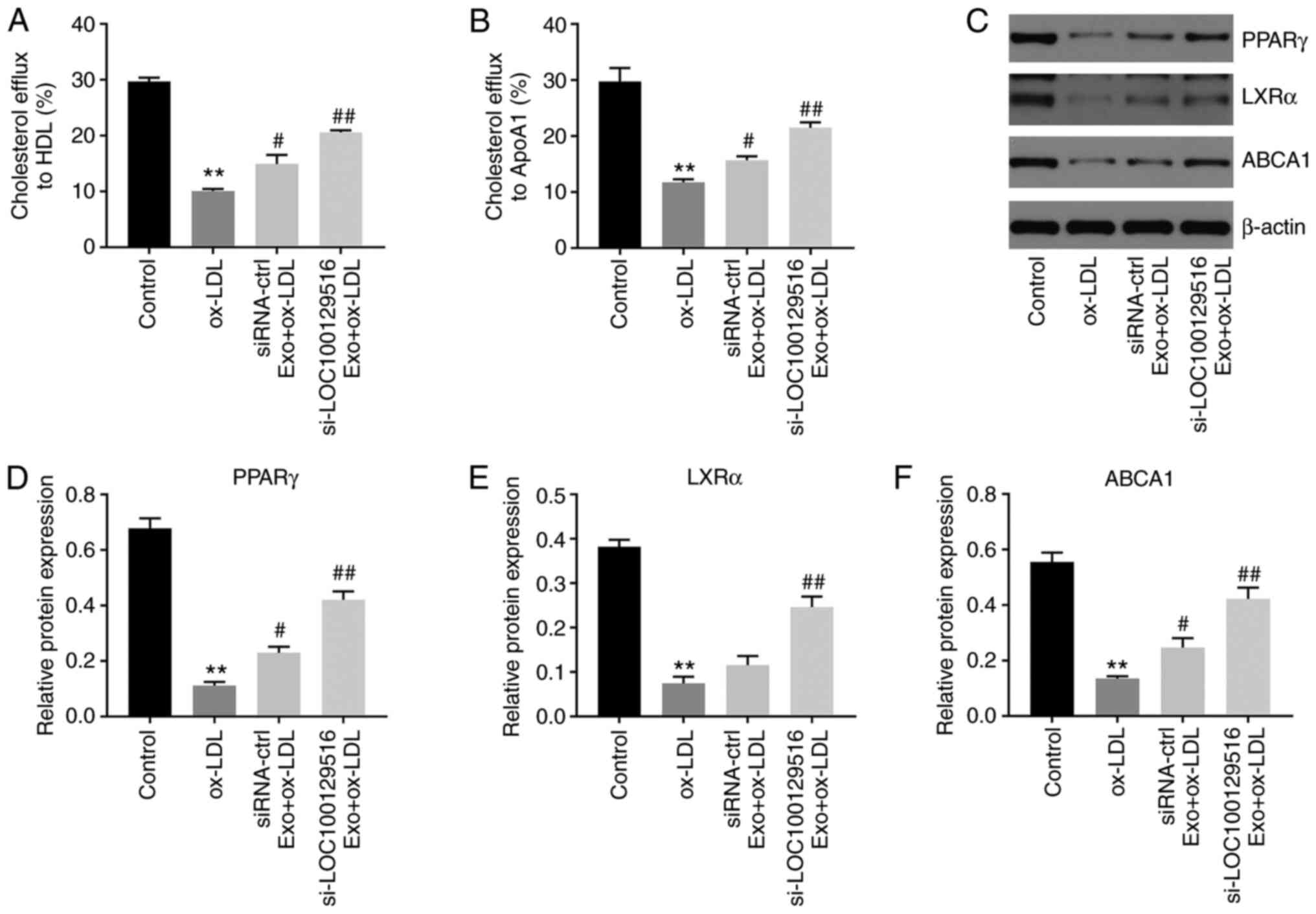
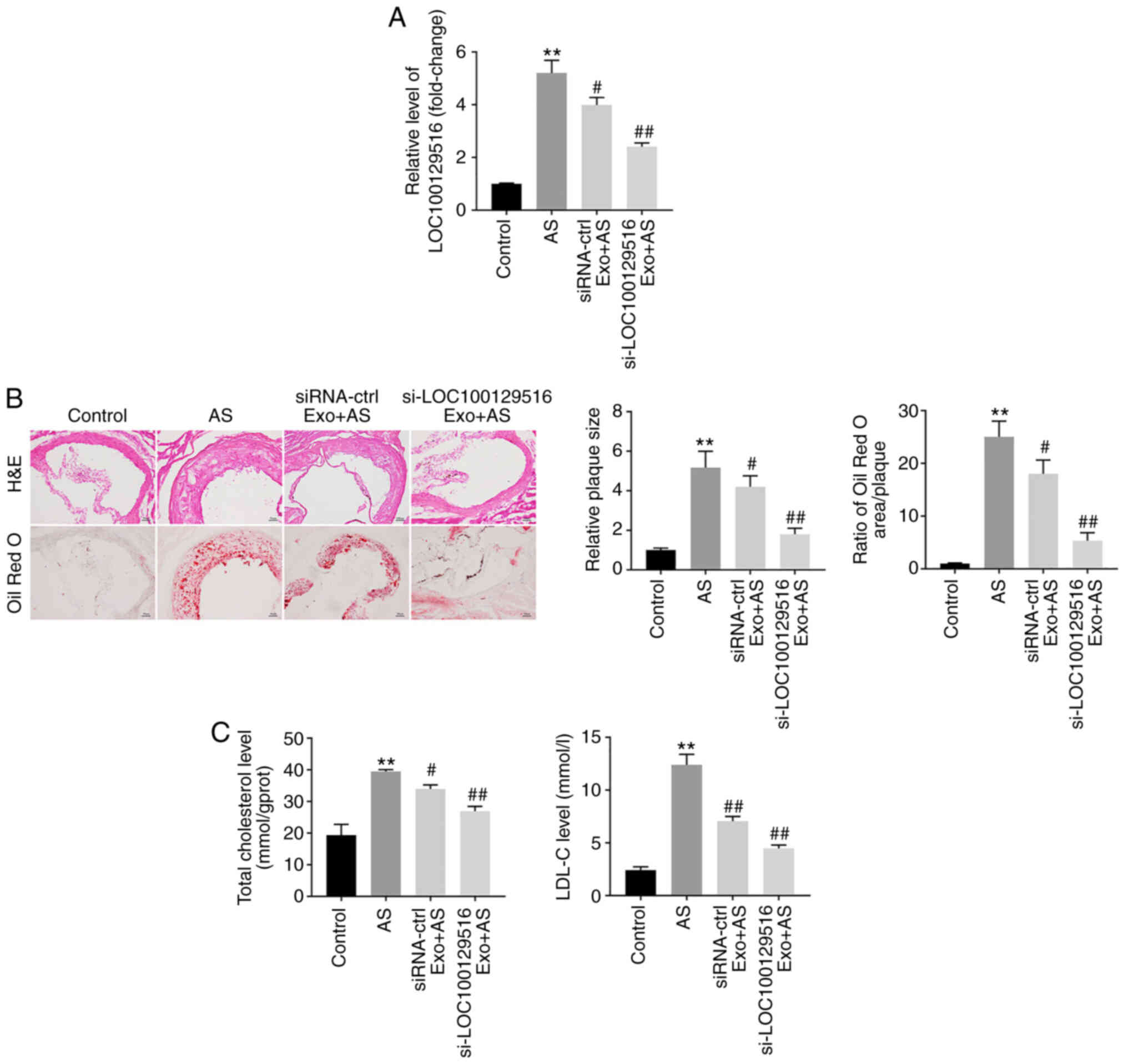
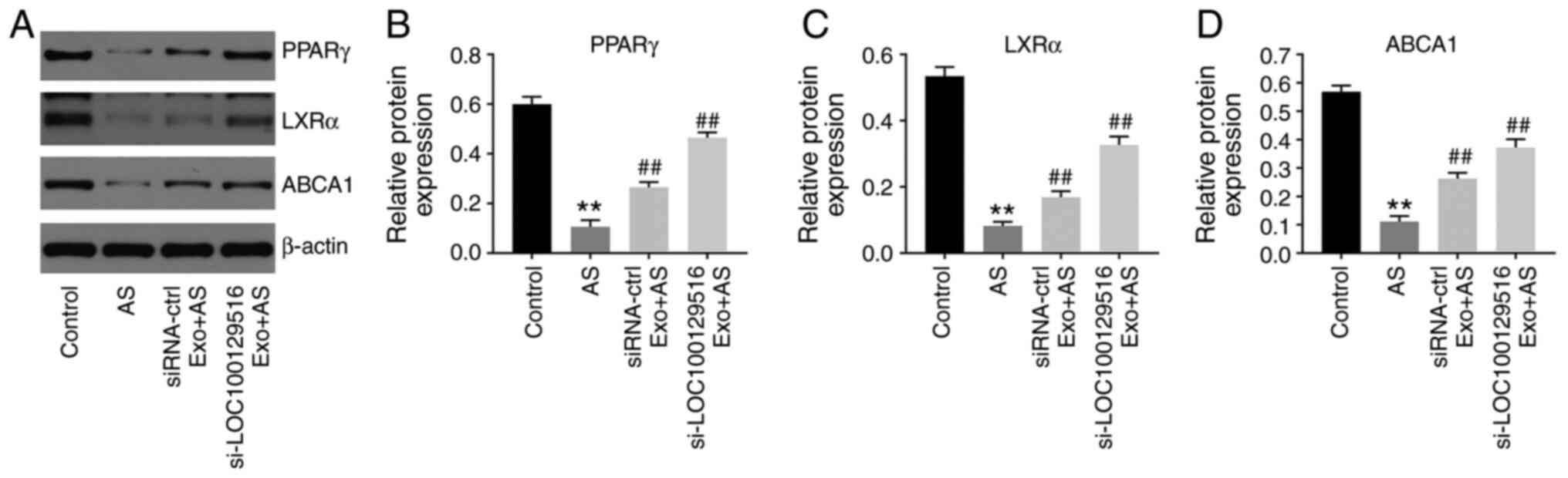
Lin XL, Hu HJ, Liu YB, Hu XM, Fan XJ, Zou
WW, Pan YQ, Zhou WQ, Peng MW and Gu CH: Allicin induces the
upregulation of ABCA1 expression via PPARγ/LXRα signaling in THP-1
macrophage-derived foam cells. Int J Mol Med. 39:1452–1460. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar
|
|
28
|
Cui Y, Fu S, Sun D, Xing J, Hou T and Wu
X: EPC-derived exosomes promote osteoclastogenesis through
lncRNA-MALAT1. J Cell Mol Med. 23:3843–3854. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
National Research Council Committee for
the Update of the Guide for the Care and Use of Laboratory Animals:
The National Academies Collection: Reports funded by National
Institutes of Health. Guide for the Care and Use of Laboratory
Animals. 8th edition. National Academies Press; Washington, DC:
2011
|
|
30
|
Shen S, Zheng X, Zhu Z, Zhao S, Zhou Q,
Song Z, Wang G and Wang Z: Silencing of GAS5 represses the
malignant progression of atherosclerosis through upregulation of
miR-135a. Biomed Pharmacother. 118:1093022019. View Article : Google Scholar
|
|
31
|
Guo Z, Zhao Z, Yang C and Song C: Transfer
of microRNA-221 from mesenchymal stem cell-derived extracellular
vesicles inhibits atherosclerotic plaque formation. Transl Res.
226:83–95. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Yu XH, Zhang DW, Zheng XL and Tang CK:
Cholesterol transport system: An integrated cholesterol transport
model involved in atherosclerosis. Prog Lipid Res. 73:65–91. 2019.
View Article : Google Scholar
|
|
33
|
Ertek S: High-density lipoprotein (HDL)
dysfunction and the future of HDL. Curr Vasc Pharmacol. 16:490–498.
2018. View Article : Google Scholar
|
|
34
|
Kennedy MA, Barrera GC, Nakamura K, Baldán
A, Tarr P, Fishbein MC, Frank J, Francone OL and Edwards PA: ABCG1
has a critical role in mediating cholesterol efflux to HDL and
preventing cellular lipid accumulation. Cell Metab. 1:121–131.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Talbot CPJ, Plat J, Ritsch A and Mensink
RP: Determinants of cholesterol efflux capacity in humans. Prog
Lipid Res. 69:21–32. 2018. View Article : Google Scholar
|
|
36
|
Wang H, Yang Y, Sun X, Tian F, Guo S, Wang
W, Tian Z, Jin H, Zhang Z and Tian Y: Sonodynamic therapy-induced
foam cells apoptosis activates the phagocytic
PPARγ-LXRα-ABCA1/ABCG1 pathway and promotes cholesterol efflux in
advanced plaque. Theranostics. 8:4969–4984. 2018. View Article : Google Scholar :
|
|
37
|
Mao MJ, Hu JP, Wang C, Zhang YY and Liu P:
Effects of Chinese herbal medicine Guanxinkang on expression of
PPARγ-LXRα-ABCA1 pathway in ApoE-knockout mice with
atherosclerosis. Zhong Xi Yi Jie He Xue Bao. 10:814–820. 2012.In
Chinese. View Article : Google Scholar
|
|
38
|
Li Y, Shi G, Han Y, Shang H, Li H, Liang
W, Zhao W, Bai L and Qin C: Therapeutic potential of human
umbilical cord mesenchymal stem cells on aortic atherosclerotic
plaque in a high-fat diet rabbit model. Stem Cell Res Ther.
12:4072021. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Kirwin T, Gomes A, Amin R, Sufi A, Goswami
S and Wang B: Mechanisms underlying the therapeutic potential of
mesenchymal stem cells in atherosclerosis. Regen Med. 16:669–682.
2021. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Hashem RM, Rashed LA, Abdelkader RM and
Hashem KS: Stem cell therapy targets the neointimal smooth muscle
cells in experimentally induced atherosclerosis: Involvement of
intracellular adhesion molecule (ICAM) and vascular cell adhesion
molecule (VCAM). Braz J Med Biol Res. 54:e108072021. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Zhang X, Huang F, Li W, Dang JL, Yuan J,
Wang J, Zeng DL, Sun CX, Liu YY, Ao Q, et al: Human gingiva-derived
mesenchymal stem cells modulate monocytes/macrophages and alleviate
atherosclerosis. Front Immunol. 9:8782018. View Article : Google Scholar
|
|
42
|
Chen S, Zhou H, Zhang B and Hu Q: Exosomal
miR-512-3p derived from mesenchymal stem cells inhibits oxidized
low-density lipoprotein-induced vascular endothelial cells
dysfunction via regulating Keap1. J Biochem Mol Toxicol. 35:1–11.
2021. View Article : Google Scholar
|
|
43
|
Yang Y, Ye Y, Su X, He J, Bai W and He X:
MSCs-derived exosomes and neuroinflammation, neurogenesis and
therapy of traumatic brain injury. Front Cell Neurosci. 11:552017.
View Article : Google Scholar :
|
|
44
|
Yu C, Tang W, Lu R, Tao Y, Ren T and Gao
Y: Human adipose-derived mesenchymal stem cells promote lymphocyte
apoptosis and alleviate atherosclerosis via miR-125b1-3p/BCL11B
signal axis. Ann Palliat Med. 10:2123–2133. 2021. View Article : Google Scholar
|
|
45
|
Wang H, Gong H, Liu Y and Feng L:
Relationship between lncRNA-Ang362 and prognosis of patients with
coronary heart disease after percutaneous coronary intervention.
Biosci Rep. 40:BSR202015242020. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Mao Q, Liang XL, Zhang CL, Pang YH and Lu
YX: lncRNA KLF3-AS1 in human mesenchymal stem cell-derived exosomes
ameliorates pyroptosis of cardiomyocytes and myocardial infarction
through miR-138-5p/Sirt1 axis. Stem Cell Res Ther. 10:3932019.
View Article : Google Scholar :
|
|
47
|
Li H, Han S, Sun Q, Yao Y, Li S, Yuan C,
Zhang B, Jing B, Wu J, Song Y and Wang H: Long non-coding RNA
CDKN2B-AS1 reduces inflammatory response and promotes cholesterol
efflux in atherosclerosis by inhibiting ADAM10 expression. Aging
(Albany NY). 11:1695–1715. 2019. View Article : Google Scholar
|
|
48
|
Meng XD, Yao HH, Wang LM, Yu M, Shi S,
Yuan ZX and Liu J: Knockdown of GAS5 inhibits atherosclerosis
progression via reducing EZH2-mediated ABCA1 transcription in
ApoE−/− mice. Mol Ther Nucleic Acids. 19:84–96. 2020.
View Article : Google Scholar
|
|
49
|
Zhang ZZ, Chen JJ, Deng WY, Yu XH and Tan
WH: CTRP1 decreases ABCA1 expression and promotes lipid
accumulation through the miR-4245p/FoxO1 pathway in THP-1
macrophage-derived foam cells. Cell Biol Int. Jul 20–2021, Epub
ahead of print https://doi.org/10.1002/cbin.11666. View Article : Google Scholar
|
|
50
|
Moradi-Chaleshtori M, Shojaei S,
Mohammadi-Yeganeh S and Hashemi SM: Transfer of miRNA in
tumor-derived exosomes suppresses breast tumor cell invasion and
migration by inducing M1 polarization in macrophages. Life Sci.
282:1198002021. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Zhao R, Feng J and He G: miR-613 regulates
cholesterol efflux by targeting LXRα and ABCA1 in PPARγ activated
THP-1 macrophages. Biochem Biophys Res Commun. 448:329–334. 2014.
View Article : Google Scholar
|
|
52
|
Xu Y, Lai F, Xu Y, Wu Y, Liu Q, Li N, Wei
Y, Feng T, Zheng Z, Jiang W, et al: Mycophenolic acid induces
ATP-binding cassette transporter A1 (ABCA1) expression through the
PPARγ-LXRα-ABCA1 pathway. Biochem Biophys Res Commun. 414:779–782.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Gu HF, Li N, Xu ZQ, Hu L, Li H, Zhang RJ,
Chen RM, Zheng XL, Tang YL and Liao DF: Chronic unpredictable mild
stress promotes atherosclerosis via HMGB1/TLR4-mediated
downregulation of PPARγ/LXRα/ABCA1 in ApoE−/− mice.
Front Physiol. 10:1652019. View Article : Google Scholar
|
|
54
|
Wang S, Zhang X, Liu M, Luan H, Ji Y, Guo
P and Wu C: Chrysin inhibits foam cell formation through promoting
cholesterol efflux from RAW264.7 macrophages. Pharm Biol.
53:1481–1487. 2015. View Article : Google Scholar : PubMed/NCBI
|