Introduction
Enhanced external counterpulsation (EECP) was
developed in 1980 by Zheng in The First Affiliated Hospital of Sun
Yat-Sen University (Guangzhou, China). Following this, EECP has
been used to treat ischemic diseases such as coronary heart disease
and angina pectoris, following percutaneous coronary intervention,
transplantation and coronary artery bypass grafting, cerebral
arteriosclerosis, cerebral ischemia, embolism of retinal artery,
ischemic optic neuropathy, optic atrophy and hearing loss (1–4).
Patients with ocular ischemic diseases have been
previously treated with EECP and medication in the Department of
Ophthalmology, the First Affiliated Hospital of Sun Yat-Sen
University since 1985. In the present study, we retrospectively
analyzed the clinical data of 65 patients (92 eyes) with carotid
artery stenosis treated with EECP and medication.
Subjects and methods
Subjects
A total of 65 patients with carotid artery stenosis
examined between January, 2005 and May, 2009 were included in the
present study. This study was conducted in accordance with the
Declaration of Helsinki and was approved by the Ethics Committee of
the First Affiliated Hospital of Xinxiang Medical University
(Weihui, China). Written informed consent was obtained from all the
participants. There were 31 male and 34 female patients with a mean
age of 64.17±8.25 years (range, 29–86 years). Diagnoses were
confirmed by examination of visual acuity, slit lamp,
ophthalmoscope, field of vision, fluorescein fundus angiography
(FFA) test, intraocular pressure, visual evoked potential (VEP),
optical ultrasound, X-ray and carotid artery color Doppler
ultrasound. Patients diagnosed with ocular ischemic diseases were
included in this study, while patients with additional primary
ophthalmological conditions such as primary glaucoma,
iridocyclitis, retinal vein occlusion, high myopia, retinitis
pigmentosa, choroiditis, diabetic retinopathy, and other congenital
fundus abnormalities were excluded.
Methods
The clinical data of all the patients (n=65) were
retrospectively analyzed. Group A consisted of 31 patients (43
eyes) treated with EECP and medication, and group B consisted of 34
patients (49 eyes) treated with medication alone. The clinical
effect in the patients of the two groups was evaluated by comparing
the visual acuity, visual fields and optical hemodynamics.
Patient assessment
Patient assessment included examination of visual
acuity, field of vision (Zeiss 750 Visual Field Analyzer) and
optical hemodynamics prior to and following treatment. Color
Doppler ultrasound (Philips HD7) was used to examine ophthalmic
arterial hemodynamics with a frequency of 10 MHz. Hemodynamic
parameters in the ophthalmic artery of each patient were recorded,
including peak systolic blood flow velocity (Psv), end-diastolic
blood flow velocity (Edv), mean blood flow velocity (Vm),
resistance index (RI) and pulse index (PI). Each parameter was
measured three times and the mean value was used.
Treatment
The 31 patients (43 eyes) in group A were treated
with EECP and medication for 2 months. In group B, 34 patients (49
eyes) were treated with medication alone for 2 months for
regulation of blood pressure, regulation of blood sugar,
neurotrophy, anticoagulation and improvement of
microcirculation.
Thirty-one patients in group A were treated with
EECP once a day for 1 h, and the course of treatment lasted for a
half to 2 months. Balloon pumping pressure (0.35–0.4
MPa/cm2) utilized in younger patients whose course of
disease was <3 months were treated with EECP twice a day.
Patients who had who had undergone bypass surgery or had suffered
heart attack, severe heart failure, congestive heart disease,
aortic disease, aortic incompetence, abdominal aortic aneurysm
(aaa), severe peripheral vascular disease, frequent arrhythmia and
venous thrombosis, were excluded from group A.
Curative effect standards
Curative effect standards were applied when one of
the following conditions occurred: i) The patient could read a
minimum of three lines on a visual acuity chart, with visual fields
>10 b, and significant improvement with hemodynamic parameters
(P<0.01); ii) patients could read a minimum of two lines on the
visual acuity chart, with visual fields >5 b or improved
hemodynamic parameters (P<0.05); iii) patients did not exhibit
improved visual acuity, visual fields and optical hemodynamics
(5–7).
Statistical analysis
Statistical analysis was performed using SPSS v.14
(SPSS, Inc., Chicago, IL, USA). An independent sample t-test and
χ2 test were used to compare the differences between the
groups. Univariate and unconditional logistic stepwise regression
methods were used to adjust for confounding factors and analyze the
interactions between factors. Factors affecting outcome regarding
the disease were not considered.
Results
Types of ocular ischemic diseases of the
included patients
The types of ocular ischemic diseases of the
patients included in this study were ischemic optic nerve
disorders, ocular ischemic syndrome, retinal central (branch) vein
occlusion and external ophthalmoplegia (Table I).
 | Table ITypes of ocular ischemic diseases of
the included patients (n=65). |
Table I
Types of ocular ischemic diseases of
the included patients (n=65).
| Types of ocular
ischemic diseases | No. of patients | Constituent ratio
(%) |
|---|
| Ischemic optic nerve
disorders | 24 | 36.92 |
| Ocular ischemic
syndrome | 21 | 32.31 |
| Retinal central
(branch) vein occlusion | 12 | 18.46 |
| External
ophthalmoplegia | 8 | 12.31 |
| Total | 65 | |
Statistically significant differences
between groups A and B
All the patients with ocular ischemic diseases were
treated with EECP and medication for two mouths. The total
effective rate in group A was 86.05% (37 eyes), while the rate in
group B was 63.27% (31 eyes), indicating statistically significant
differences between groups A and B (χ2=2.238, P<0.05)
(Tables II–IV).
 | Table IIComparison of visual acuity prior to
and following treatment in the patients of group A. |
Table II
Comparison of visual acuity prior to
and following treatment in the patients of group A.
| Visual acuity
(m) |
|---|
|
|
|---|
| Time | LP | <0.1 | 0.1–0.3 | 0.4–0.9 | ≥1.0 |
|---|
| Prior to treatment,
n | 4 | 9 | 15 | 12 | 3 |
| Following treatment,
n | 2 | 5 | 13 | 17 | 6 |
 | Table IVComparison of curative effect between
groups A and B (mean ± standard deviation). |
Table IV
Comparison of curative effect between
groups A and B (mean ± standard deviation).
| Groups | No. of patients | No. of eyes | Effective no. of
eyes | Effective power
(%) |
|---|
| A | 31 | 43 | 37 | 86.05 |
| B | 34 | 49 | 31 | 63.27 |
The present study identified a close positive
correlation between the curative effect and the course of disease
in the patients of group A (R=0.719, P<0.05). The correlation
analysis revealed that the patients with a shorter course of
disease, exhibited an improved curative effect (Table V).
 | Table VAssociation between curative effect
and course of disease in the patients of group A. |
Table V
Association between curative effect
and course of disease in the patients of group A.
| Course of
disease | No. of eyes | Excellence, n | Effectiveness, n | Inefficiency, n |
|---|
| 4 days to 1
month | 8 | 6 | 2 | 0 |
| 2–3 months | 16 | 8 | 6 | 1 |
| 4–5 months | 5 | 2 | 2 | 1 |
| 6 months | 6 | 2 | 4 | 1 |
| 1–2 years | 4 | 1 | 2 | 1 |
| 5–10 years | 4 | 0 | 2 | 1 |
| Total | 43 | 19 | 18 | 5 |
Significantly reduced hemodynamic
parameters in the patients of group A
To investigate the curative effect mechanism of
EECP, we compared the hemodynamic parameters of all the patients
prior to and following treatment. The results showed that
ophthalmic artery perfusion of the patients in groups A and B was
improved. Parameters including Psv, Edv and RI of the patients in
group A were also reduced compared to those in patients of group B
(Table VI). Statistically
significant differences were observed between groups A and B
regarding hemodynamic parameters (χ2=4.935, 7.124;
5.478; P<0.05).
 | Table VIComparison of hemodynamic parameters
between groups A and B (mean ± standard deviation). |
Table VI
Comparison of hemodynamic parameters
between groups A and B (mean ± standard deviation).
| Group A (n=43) | Group B (n=49) |
|---|
|
|
|
|---|
| Index | Prior to
treatment | Following
treatment | t-value | P-value | Prior to
treatment | Following
treatment | t-value | P-value |
|---|
| Psv | 9.14±2.25 | 29.32±3.66 | 1.548 | 0.083 | 8.77±2.23 | 13.37±3.15 | 10.13 | <0.01 |
| Vm | 8.94±1.87 | 26.83±3.36 | 1.741 | 0.062 | 9.73±2.21 | 15.36±3.29 | 9.74 | <0.01 |
| RI | 1.17±0.08 | 0.34±0.11 | 1.275 | 0.121 | 1.35±0.13 | 0.68±0.14 | 9.37 | <0.01 |
Different types of ocular ischemic
diseases have different curative effects
The present study showed that different types of
ocular ischemic diseases had different curative effects. EECP had
optimum significant effectiveness in ischemic optic neuropathy.
Following treatment with EECP and medication for 2 months, no
improvement was observed in the visual acuity of patients with
clinical symptoms present for >6 months, while there was
significant improvement in visual fields and optical
hemodynamics.
None of the patients with ocular ischemic diseases
treated with EECP and medication in groups A and B exhibited any
complications during the therapeutic process.
Discussion
EECP is a non-invasive method used to assist
circulation, which improves diastolic augmentation and systolic
unloading via a pressurized air cuff around the legs of the
patient; cuff pressure was maintained at ~300 mmHg during diastole.
In the United States, this method has proven to be effective in
chronic angina, as confirmed by large-scale clinical trials
(8–11). Findings of those studies suggested
that the increase in coronary blood by EECP treatment occurs mainly
through diastolic augmentation, which is comparable to the effect
on the arterial system by intra-aortic balloon pumping (IABP),
although EECP also affects venous return. EECP is beneficial as it
can be immediately implemented and is non-invasive without risk of
bleeding or infection in contast to IABP. Thus, EECP may be useful
to improve circulation in patients with acute heart failure and
acute coronary syndrome. In patients with ocular ischemic diseases,
EECP induced diastolic augmentation comparable to that of IABP. By
contrast, EECP increased preload and the cardiac index (CI) with
increased venous return in contrast to IABP (11). In the present study, EECP was
performed in patients with ocular ischemic diseases, and the
changes in visual acuity, visual fields, as well as the hemodynamic
effects were observed in order to investigate the mechanism of EECP
and its effects on ocular ischemic diseases (12–14).
Before 1990, the mechanism of this treatment was
supposed to promote collateral circulation by increasing diastolic
pressure. In their study, Zheng et al identified and
confirmed that the flow shear stress was significantly increased
during EECP, regulating a series of reactions of shear stress
responsive elements, inducing vascular endothelial cell (VEC)
repair mechanism and improving VEC function, leading to inhibition
of the development of atherosclerosis. A new generation of EECP
device was designed based on the abovementioned advances which
aimed to promote the arterial flow shear stress more effectively
leading to vascular endothelium protection (15–17).
Carotid artery stenosis is a leading cause of
ischemic stroke and patients usually present to neurological
clinics with stroke symptoms of hemiplegia and homonymous
hemianopia (18). An increasing
number of patients with carotid artery stenosis have presented to
ophthalmological clinics due to eye discomfort. Therefore, such
patients who have carotid artery stenosis accompanied by ocular
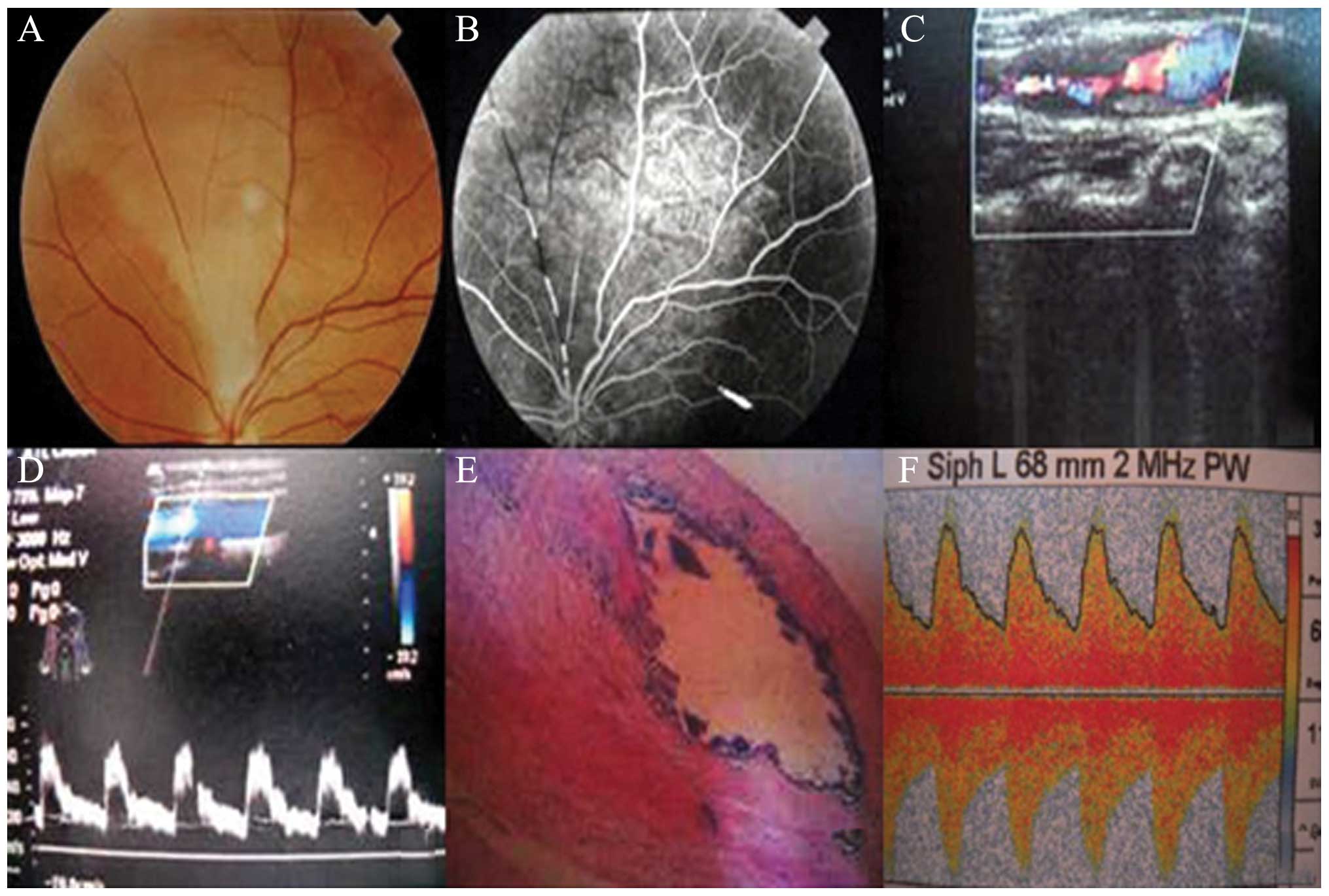
ischemic presentations have received increasing attention (Fig. 1) (16,19,25).
EECP has been used in ischemic disease such as
retinal arterial obstruction, ischemic optic neuropathy and optic
atrophy in the Department of Ophthalmology, the First Affiliated
Hospital of Sun Yat-Sen University, and has been proven to have a
significant curative effect. Optic nerves are the nerve endings of
cerebrum. During the process of optic atrophy, some optic nerve
fibers are reversible, and their function improves with prompt
recovery of blood supply. EECP can oppress limbs during the
relaxation period, increase the blood flow of carotid and vertebral
arteries, as well as increase the volume of blood flow of the
ophthalmic artery. EECP simultaneously increases the perfusion
pressure of posterior ciliary arteries and blood supply of the
optic nerve, decreases ischemia and the poor supply of oxygen in
the optic nerve. As a result, EECP gradually improves the visual
function, and significantly improves the visual acuity and field of
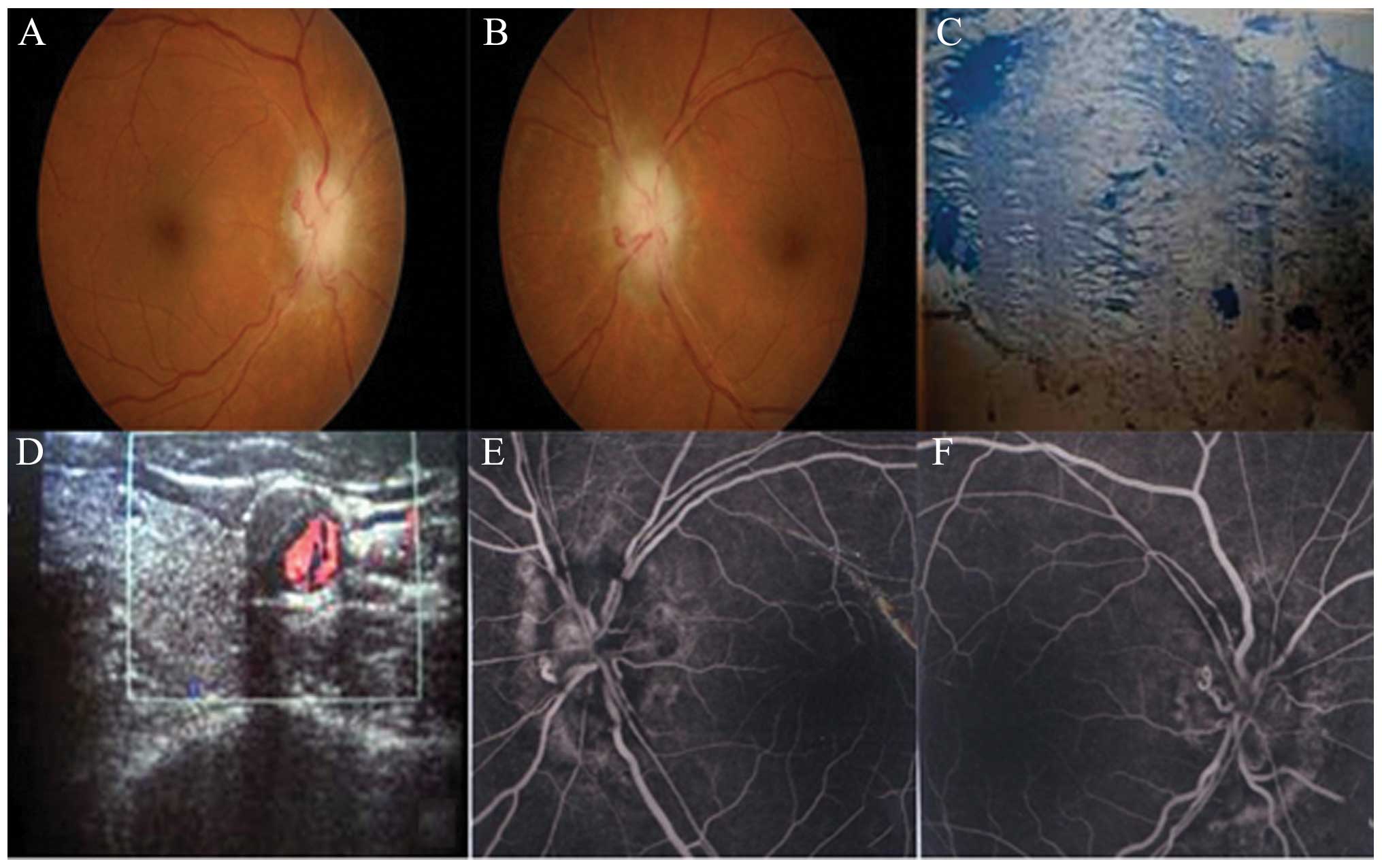
vision of patients (Fig. 2)
(17,20,25).
In their study, Costa et al(21) reported that EECP can promote ramus
anastomoticus of retinal ischemia ischemic zone open and collateral
circulation formation, improve retinal blood stream, ultimately
leading to the treatment of optic atrophy. The present study has
shown that there was significant improvement in patients with optic
atrophy treated with EECP combined with drugs.
The present study also identified a close positive
correlation between curative effect and course of disease in the
patients of group A (R=0.719, P<0.05). Correlation analysis
revealed that the patients with a shorter course of disease
exhibited an improved curative effect. Consequently, early
diagnosis and intervention are needed in patients with ocular
ischemic diseases. Significant improvement in visual acuity and
visual fields was observed in some patients with optic atrophy with
symptoms present for >1 year, following treatment with EECP and
medication for several months. The color of video disc also changed
from pallor to reddish when under examination using an
ophthalmoscope. Therefore, even low-vision patients with long-term
optic atrophy may benefit from EECP.
Results of the present study have shown that there
was significant improvement in the visual acuity, visual fields and
optical hemodynamics of the patients in group A, where
statistically significant differences were observed between groups
A and B. Moreover, this study demonstrated that patients with
ocular ischemic diseases can be treated with EECP 1 or 2 times/day,
for 1 h each time, initially at a course of treatment of half a
month, and subsequently for >1 month. Younger patients exhibited
an improved curative effect compared to older patients, since they
had higher diastolic blood pressure when treated with EECP.
Therefore, younger patients with ocular ischemic diseases can be
treated with EECP 2 times/day using an ophthalmoscope.
The present study has shown that EECP is safe and
effective, and that it can be used to treat various conditions
apart from hemorrhagic disease, severe hypertension, aortic
incompetence, thrombophlebitis and glaucoma. Early intervention may
therefore be effective in the treatment of carotid artery stenosis
and reduce the incidence of ophthalmic and cerebral complications
when treated with EECP combined with drugs (22–24).
References
|
1
|
Zheng ZS: The past, present and future of
external counterpulsation. J Sun Yat-Sen Univ Med Sci. 27:602–604.
2006.(In Chinese).
|
|
2
|
Lu L, Wu WK, Zheng ZS, et al: Effects of
external counterpulsation on renin-angiotensin system and
hemodynamics in dogs with myocardial ischemia. Chin J Pathophysiol.
17:804–807. 2002.(In Chinese).
|
|
3
|
Chen XL, Liu TT, Yu ZH, et al: Enhanced
external counterpulsation improved no-reflow phenomena in
myocardium after percutaneous coronary intervention. Chin J
Hypertens. 16:712–715. 2008.(In Chinese).
|
|
4
|
Lawrence PF and Oderich GS: Ophthalmologic
findings as predictors of carotid artery disease. Vasc Endovascular
Surg. 36:415–424. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Takaki Y, Nagata M, Shinoda K, et al:
Severe acute ocular ischemia associated with spontaneous internal
carotid artery dissection. Int Ophthalmol. 28:447–449. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wang YL, Zhao L, Huang YX, et al: Clinical
characteristics of ocular ischemia syndrome. Zhonghua Yan Ke Za
Zhi. 45:1080–1083. 2009.(In Chinese).
|
|
7
|
Liu SR, Luo RJ, Li XM, et al: Analysis of
ocular ischemic diseases caused by carotid artery stenosis. Chin J
Ocul Fund Dis. 26:310–313. 2010.(In Chinese).
|
|
8
|
Li MY and Li CM: Effectiveness of external
counterpulsation in the treatment of optic atrophy. Chin J Rehabil
Med. 18:101–102. 2003.
|
|
9
|
Wu GF, Du ZM, Hu C, et al: Angiogenic
effects of long-term enhanced external counterpulsation in a dog
model of myocardial infarction. Am J Physiol Heart Circ Physiol.
290:H248–H254. 2006.PubMed/NCBI
|
|
10
|
Wu GF, Du ZM, Hu CH, et al: Microvessel
angiogenesis induced by enhanced external counterpulsation in
chronic experiment infarct model. J Card Fail. 8:S262002.
|
|
11
|
Taguchi I, Ogawa K, Kanaya T, Matsuda R,
Kuga H and Nakatsugawa M: Effects of enhanced external
counterpulsation on hemodynamics and its mechanism. Circ J.
68:1030–1034. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Shea ML, Conti CR and Arora RR: An update
on enhanced external counterpulsation. Clin Cardiol. 28:115–118.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Loh PH, Louis AA, Windram J, et al: The
immediate and long-term outcome of enhanced external
counterpulsation in treatment of chronic stable refractory angina.
J Intern Med. 259:276–284. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lawson WE, Hui JCK, Kennard ED, et al:
Two-year outcomes in patients with mild refractory angina treated
with enhanced external counterpulsation. Clin Cardiol. 29:69–73.
2006.PubMed/NCBI
|
|
15
|
Amselem L, Montero J, Diaz-Llopis M,
Pulido JS, Bakri SJ, Palomares P and Garcia-Delpech S: Intravitreal
bevacizumab (Avastin) injection in ocular ischemic syndrome. Am J
Ophthalmol. 144:122–124. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Malhotra R and Gregory-Evans K: Management
of ocular ischemic syndrome. Br J Ophthahnol. 184:1428–1431. 2000.
View Article : Google Scholar
|
|
17
|
Karacostas D, Terzidou C, Voutas S, Rafou
J, Artemis N and Georgiadis N: Isolated ocular ischemic syndrome
with no cerebral involvement in common carotid artery occlusion.
Eur J Ophthalmol. 11:97–101. 2001.PubMed/NCBI
|
|
18
|
Chen CS and Miller NR: Ocular ischemic
syndrome: review of clinical presentation, etiology, investigation,
and management. Compr Ophthalmol Update. 8:17–28. 2007.PubMed/NCBI
|
|
19
|
Albers GW, Hart RG, Lutsep HL, Newell DW
and Sacco RL: Addendum to the supplement to the guidelines for the
management of transient ischemic attacks. Stroke. 31:10012000.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wolintz RJ: Carotid endarterectomy for
ophthalmic manifestations: is it ever indicated? J Neuroophthalmol.
25:299–302. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Costa VP, Kuzniec S, Molnar LJ, Cerri GG,
Puech-Leão P and Carvalho CA: The effects of carotid endarterectomy
on the retrobulbar circulation of patients with severe occlusive
carotid artery disease. An investigation by color Doppler imaging.
Ophthalmology. 106:306–310. 1999. View Article : Google Scholar
|
|
22
|
Sivalingam A, Brown GC and Magargal LE:
The ocular ischemic syndrome. III Visual prognosis and the effect
of treatment. Int Ophthalmol. 15:15–20. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Pecold-Stepniewska H, Karolczak-Kulesza M,
Wasilewicz R, Krasiński Z and Kulesza J: Glaucoma and ocular
ischemic syndrome - case report. Klin Oczna. 106:258–260. 2004.(In
Polish).
|
|
24
|
Klijn CJ, Kappelle LJ, van Schooneveld MJ,
Hoppenreijs VP, Algra A, Tulleken CA and van Gijn J: Venous stasis
retinopathy in symptomatic carotid artery occlusion: prevalence,
cause, and outcome. Stroke. 33:695–701. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Luo R, Liu S, Li X, Zhuo Y and Tian Z:
Fifty-eight cases of ocular ischemic diseases caused by carotid
artery stenosis. Chin Med J. 123:2662–2665. 2010.PubMed/NCBI
|