Introduction
Angiogenesis, the multistep process by which novel
blood vessels develop from existing microvasculature in a variety
of physiological states, is an essential component in solid tumor
growth, invasion and metastatic pathways (1). As tumor angiogenesis is a promising
target for the development of novel anticancer therapies, >12
endogenous proteins that act as activators of tumor angiogenesis
have been identified (2). It is
well known that tumor-induced angiogenesis is regulated by vascular
endothelial growth factor (VEGF) and several other cytokines, such
as platelet-derived growth factor (PDGF) and fibroblast growth
factor (FGF), which are secreted by tumor cells. Among them, VEGF
and its corresponding tyrosine kinase receptors, which specifically
regulate endothelial proliferation, permeability and survival, are
known to be part of the most important signaling pathway in
physiological and pathological angiogenesis. The VEGF signaling
pathway is activated by the ligand-induced phosphorylation of VEGF
receptors. Blocking VEGFR phosphorylation using a kinase inhibitor
is expected to disrupt VEGF signaling pathways, resulting in
changes in tumor vasculature characteristics and growth. Therefore,
the blockade of this antiangiogenic mechanism may provide a useful
therapeutic strategy (3,4). Basic FGF (bFGF) is also a potent
angiogenic factor. bFGF has been shown to be a key regulator of
numerous physiological processes in adult organisms and is also
involved in tumoral angiogenesis. bFGF stimulates the release and
activity of collagenase, protease and integrins on the
extracellular membrane to form nascent microvascular networks.
Furthermore, bFGF has been shown to synergistically promote
VEGF-mediated tumor development and angiogenesis in mouse models,
suggesting that dual inhibition of VEGFR and FGFR pathways is an
attractive therapeutic approach (5,6). A
number of pharmacological antiangiogenic agents have been
investigated in clinical trials. Bevacizumab, a humanized
anti-VEGF-A monoclonal antibody, showed clinical benefit in
patients with metastatic colorectal cancer and was approved by the
USA Food and Drug Administration (FDA) in 2004 (7). More recently, sorafenib, an inhibitor
of multiple kinases, including VEGFR, PDGF receptor, c-kit, raf and
flt-3, showed benefits in patients with advanced hepatocellular
carcinoma (HCC) and was also approved for use in HCC by the USA FDA
in 2007 (8). These achievements
have validated the hypothesis that inhibition of angiogenesis may
be a strategy for cancer treatment.
Brivanib (BMS-582664; Bristol-Myers Squibb, New
York, NY, USA), a dual tyrosine kinase inhibitor with selectivity
against the key angiogenesis receptors VEGF-R2, FGF-R1 and FGF-R2,
is currently under development for the treatment of cancer as a
single agent as well as in combination with other cancer treatment
modalities. This compound is an orally available investigational
small molecule and predominantly undergoes oxidative hepatic
metabolism by CYP3A4 and CYP1A2 equally. The peak concentration of
brivanib in the plasma is reached after 1–2 h and it is primarily
eliminated in the feces (9). In
several tumor xenograft models, brivanib has shown significant
tumor growth inhibition when administered orally over multiple dose
levels, suggesting that it is effective in the treatment of HCC
(10,11).
High-resolution magic angle spinning magnetic
resonance spectroscopy (HR-MAS MRS), an ex vivo MRS
technique introduced in 1997, has recently become important for
analyzing metabolic profiles from intact tissue specimens that
contain information on the physiological and pathological status of
the tumor. Comparisons of HR-MAS MRS using small biopsies and
conventional high-resolution 1H MRS using perchloric
acid extracts have provided similar sensitivity and resolution
(12). Due to its closer and
realistic insights, the application of the HR-MAS MRS technique has
increasingly been utilized for the analysis of intact tissues,
predominantly in cancer research (13). Previous studies have shown that the
quantification of tumor metabolic changes with 1H HR-MAS
MRS, in conjunction with subsequent histopathology of the same
tumor specimen, supplements histopathological examination and
improves the accuracy in the diagnosis, characterization, and
evaluation of tumor progression in different tumors, including
prostate (14,15), brain (16), lung (17), breast (12), hepatic (10) and cervical tumors (18). Therefore, this study was designed
to investigate whether 1H HR-MAS MRS supplements
histopathological examination and provides quantitative metabolite
information for the analysis of the efficacy of brivanib treatment
in Hep3B tumor xenografts. Proliferation, apoptosis and
microvasculature, determined by histopathology, were also used as
measures for the effect of brivanib treatment.
Materials and methods
Tumor cell line
The Hep3B human hepatocellular carcinoma cell line
was purchased from the Korean Cell Line Bank (Seoul, Korea) and
cultured in minimal essential medium supplemented with 10% fetal
bovine serum, 1% ampicillin and 1% streptomycin. Cells were
cultured at 37°C in a humidified incubator containing 5%
CO2 and were passaged twice a week at a split ratio of
1:3. All the experiments were conducted with 70–80% confluent
cultures.
Xenograft tumor model and brivanib
treatment
Male athymic BALB/c nu/nu mice (age, 7 weeks) were
purchased from Orient Bio (Seoul, Korea) and maintained in a
specific pathogen-free mouse colony at the Laboratory Animal
Research Center, Samsung Biomedical Research Institute (SBRI;
Seoul, Korea). The mice were maintained in accordance with
guidelines of the Association for Assessment and Accreditation of
Laboratory Animal Care International (Guide for the Care and Use of
Laboratory Animals), and all murine studies were reviewed and
approved by the Institutional Animal Care and Use Committee of SBRI
(approved proposal #S-B1-002). Ectopic xenograft tumors were
established by subcutaneous injection of 5×106 Hep3B
cells in a total volume of 0.1 ml serum-free medium into the right
thigh under anesthetic using 1.5% isoflurane, 70% N2O
and 30% O2. Tumor volume was estimated using caliper
measurements and calculated using the equation v = π/6 × a × b × c,
where a, b and c are caliper measurements of tumor length, width
and depth, respectively. Tumor development was followed in
individual animals every other day by sequential caliper
measurements. When the tumor volume reached ~50–70 mm3,
the mice were randomized into two groups and brivanib therapy was
initiated. Brivanib was obtained from Bristol-Myers Squibb and
prepared as a suspension in vehicle (70% polyethylene glycol 400)
for oral administration to xenografted tumor-bearing mice. In the
treated group (n=8), mice were treated daily with oral
administration of brivanib at 90 mg/kg body weight for 18 days. In
the control group (n=7), mice were treated daily with an equivalent
volume of vehicle. On day 18 following treatment, the mice were
sacrificed and the tumors were removed. The tumor tissues were
sharply excised and fixed in 10% neutral-buffered formalin for
histological analysis or snap-frozen in liquid nitrogen prior to
storage at −80°C for immediate ex vivo HR-MAS MRS data
acquisition.
Immunohistochemistry and terminal
deoxynucleotidyl transferase dUTP nick end-labeling (TUNEL)
assay
Formalin-fixed, paraffin-embedded samples were
sliced into 4-μm sections, deparaffinized in xylene, rehydrated in
graded alcohol and transferred to 0.01 M phosphate-buffered saline
(PBS, pH 7.4). For immunohistochemical localization of Ki-67 (a
marker for cell proliferation) and CD31 (a marker for tumor
microvascularity) in the sections, heat-induced epitope retrieval
was performed with citrate buffer (pH 6.0; Dako, Carpinteria, CA,
USA) for 5 min at 121°C to identify hidden antigen epitopes and the
sections were then cooled to room temperature. Endogenous
peroxidase was blocked by incubating slides with 3% hydrogen
peroxide in PBS for 30 min at room temperature. Subsequent to
washing in PBS, sections were treated with serum-free blocking
solution (Dako) for 20 min at room temperature to block
non-specific binding. Subsequently, the sections were incubated
with Ki-67 rabbit polyclonal antibody (1/200; Dako) or CD31 mouse
monoclonal antibody (1/150; BD Biosciences, Erembodegem, Belgium)
for 60 min at room temperature. The sections were then washed in
PBS and incubated for 30 min at room temperature with horseradish
peroxidase-labeled polymer conjugated secondary antibodies against
rabbit IgG (Dako). The color reaction was developed using the
ready-to-use DAB (3,3′-diaminobenzidine) substrate-chromogen
solution (Dako) for 5 min and then washed with distilled water.
Sections were lightly counterstained with Mayer’s hematoxylin for
30 sec prior to dehydration and mounting.
Apoptotic cell death was assessed using a TUNEL
assay with a commercially available apoptosis detection kit
(ApopTag® Peroxidase In Situ Apoptosis Detection Kit;
Millipore, Temecula, CA, USA) according to the manufacturer’s
instructions. Briefly, following routine deparaffinization,
rehydration and blocking of endogenous peroxidase with 3% hydrogen
peroxide in PBS for 10 min at room temperature, the tissue sections
were digested with 20 μg/ml proteinase K in PBS for 15 min at room
temperature. Subsequent to washing in PBS buffer, equilibration
buffer was applied to the sections for 1 min at room temperature
and the sections were then incubated with working strength terminal
deoxynucleotidyl transferase (TdT) enzyme for 60 min at 37°C in a
humidity chamber. The reaction was terminated in Working Strength
Stop/Wash buffer for 30 min at room temperature. After washing in
PBS, the sections were covered with anti-digoxigenin-peroxidase for
30 min at room temperature. The color reaction was developed using
DAB substrate chromogen solution for 5 min and the sections were
washed with distilled water and lightly counterstained with Mayer’s
hematoxylin for 30 sec. All the sections were stained with
hematoxylin and eosin for histological analysis.
Cell proliferation was determined by calculating the
number of Ki-67-positive cell nuclei and the apoptotic cell death
was determined by counting the number of TUNEL-positive cells in at
least five randomly selected high-power fields (magnification,
×200). Microvessel density (MVD) was also determined by calculating
the number of individual microvessels stained with CD31, the
endothelial cell surface marker in tumor areas without necrosis, as
described in our previous study (19).
1H HR-MAS MR spectroscopy
Prior to the 1H HR-MAS MRS data
acquisition, the tumor samples were cut to fit a MAS rotor and
flushed with deuterium oxide (D2O) to remove the
residual blood and water. The samples were inserted into a
pre-weighed zirconium HR-MAS rotar (50 μl, 4-mm diameter) and
weighed. The average tissue sample content was 7–9 mg. For chemical
shift reference, TSP
(3′-trimethylsilylpropionate-2,2,3,3-d4) sodium salt was
dissolved in D2O at a concentration of 1 mM. The
remaining volume of the rotor was filled with D2O to
ensure consistent spinning and each sample was transferred into the
HR-MAS probe. The HR-MAS studies were conducted on a Bruker Avance
400 MHz vertical-bore spectrometer (Bruker BioSpin GmbH,
Rheinstetten, Germany) equipped with a 4-mm HR-MAS
1H/13C probe with a z-gradient aligned with
the magic angle axis using the standard 5000 Hz spinning rate for
the magnetic field strength. Spectra were obtained at 4°C.
Two spectra were obtained for each sample, as
previously described (12). A
standard single-pulse spectrum (zgpr; Bruker BioSpin GmbH) with
suppression of the water signal was obtained following 3 sec of
water presaturation and a 60° flip angle over a sweep width of 20
ppm. Thereafter, a Carr-Purcell-Meiboom-Gill (CPMG) spin-echo
experiment (cpmgpr; Bruker BioSpin GmbH) was performed using 2 sec
of water suppression prior to a 90° excitation pulse. The free
induction decay was collected into 64 K points during 2.72 sec, and
32 transients were collected. A total of 128 transients over a
frequency region of 16.7 ppm were collected into 32 K points,
resulting in an acquisition time of 1.64 sec. Spectra were
Fourier-transformed into 128K after 0.3 Hz exponential line
broadening. A linear baseline correction was applied, and chemical
shifts were calibrated to the TSP peak at 0 ppm.
Statistical analysis
Hep3B xenograft tumor volume and the HR-MAS MRS
metabolite concentration were compared by the Mann-Whitney U test,
and quantification of Ki-67-, CD31- and TUNEL-positive reactions
were compared using the unpaired Student’s t-test. P<0.05 was
considered to indicate a statistically significant difference.
Results
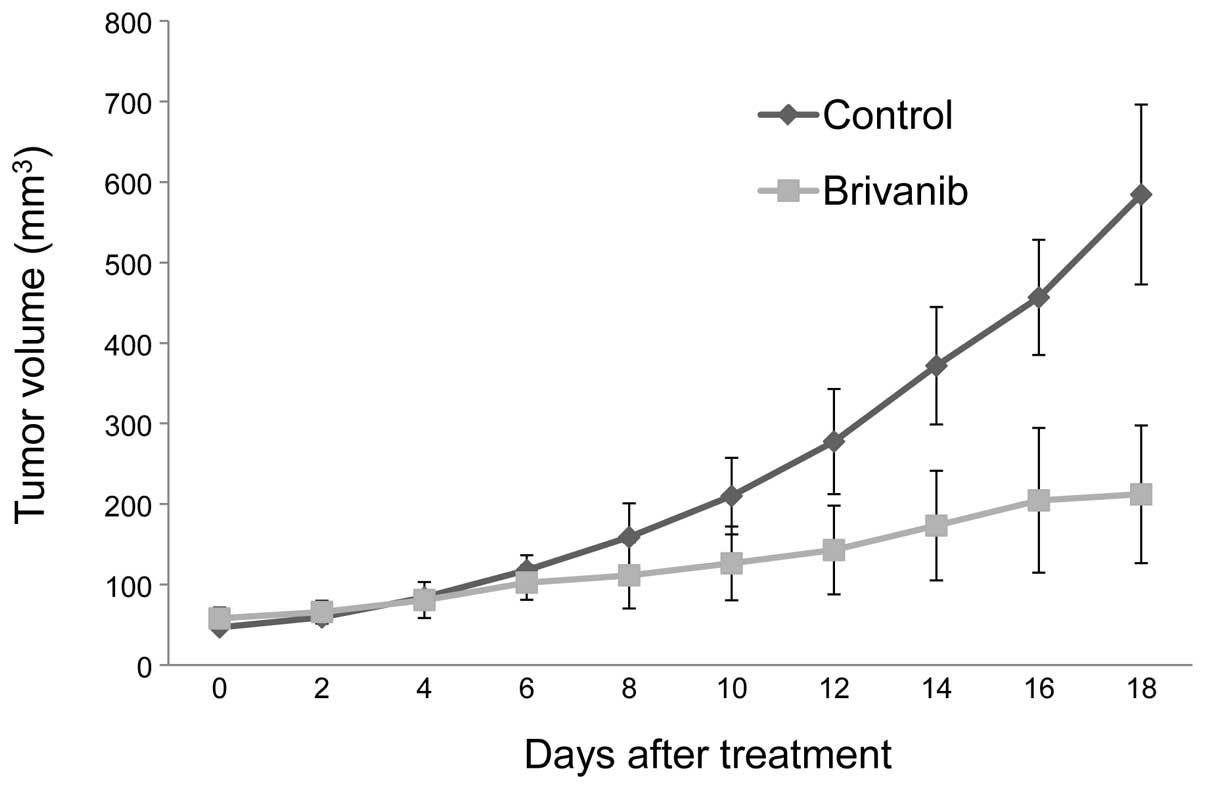
In vivo tumor xenograft growth
inhibition
The antitumor activity of brivanib was investigated
in a Hep3B human hepatocellular carcinoma xenograft model in
athymic nude mice. Tumor growth was assessed according to tumor
volume. As shown in Fig. 1,
treatment with brivanib at a daily dose of 90 mg/kg body weight
markedly reduced tumor growth, suggesting that brivanib is
effective in xenografted Hep3B tumors. Statistically significant
tumor growth inhibition was observed on the sixth day following
treatment between the two groups (P<0.05). The mean tumor volume
in vehicle-treated mice was 584.4±111.6 mm3 (mean ± SD)
on the 18th day following treatment, while that in brivanib-treated
mice only reached 212.2±85.5 mm3 (64% reduction compared
with vehicle; P<0.05). During the study, the antitumor activity
observed with brivanib treatment was not associated with any overt
toxicity as judged by the lack of significant changes in body
weight between the two groups (data not shown).
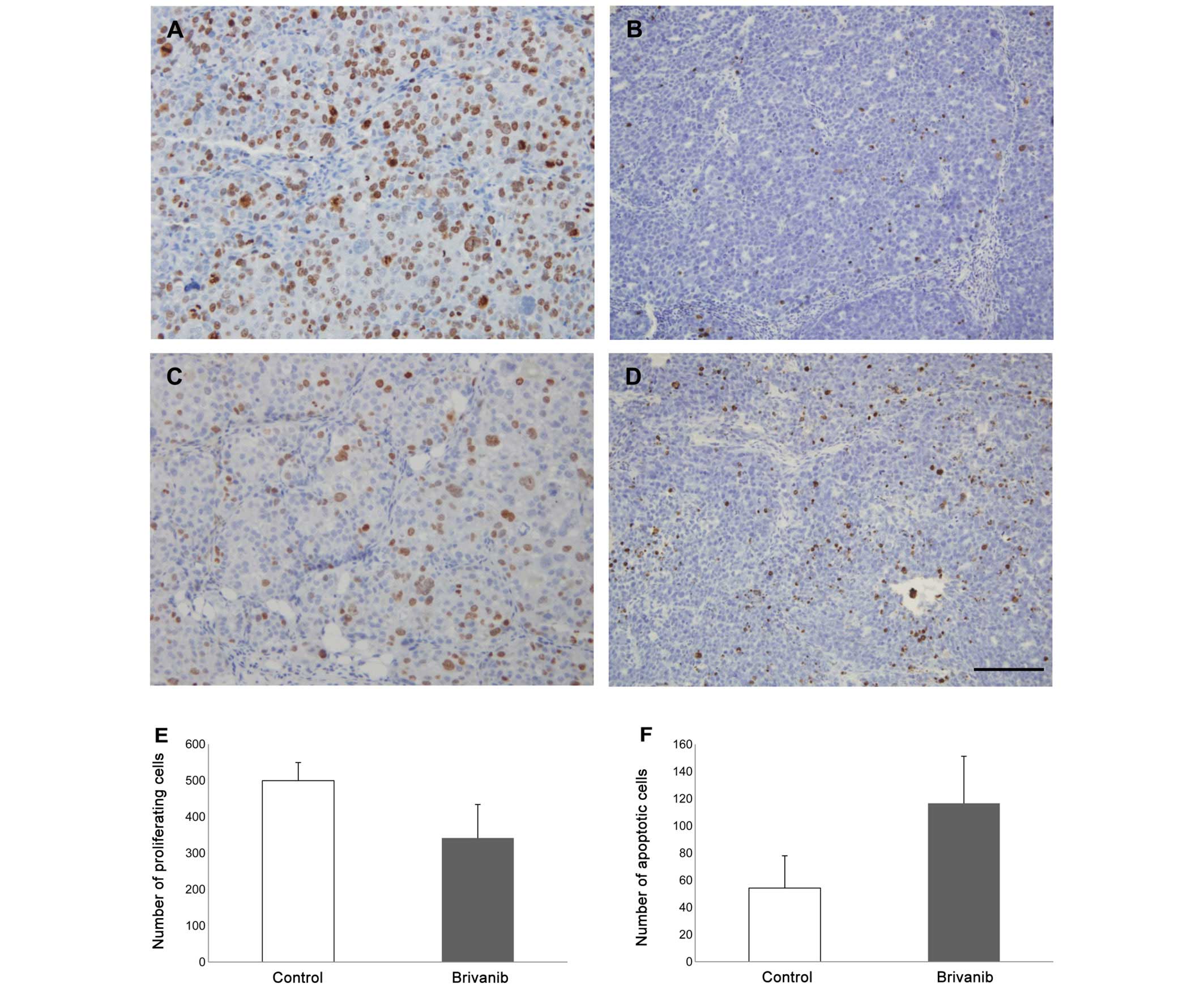
Effects on cell proliferation and
apoptosis
Based on the results with regard to in vivo
tumor growth inhibition, the antiproliferative effects of brivanib
at the cell level were assessed by quantifying tumor cell
proliferation measured by immunohistochemical staining for Ki-67
and apoptosis analyzed by a TUNEL assay 18 days following
treatment, as described in Materials and methods. Quantitative
analysis was performed on a total of 15 mice (n=7 control and n=8
treated). As expected, the mean number of Ki-67-positive tumor
cells was substantially decreased, while the mean number of
TUNEL-positive cells, which was inversely related to
Ki-67-positivity, was significantly increased in brivanib-treated
tumor cells (Fig. 2A–D). As shown
in Fig. 2E and F, the mean number
of Ki-67-positive tumor cells (proliferating cells) in
vehicle-treated mice was 499.33±50.05, but that in brivanib-treated
mice was 341.51±92.32 (32% reduction compared with vehicle;
P<0.05), while the mean number of TUNEL-positive cells
(apoptotic cells) was 54.20±23.76 in vehicle-treated mice and
116.53±34.67 (54% increase compared with vehicle; P<0.05) in
brivanib-treated mice. These observations suggested that the
antitumor activity of brivanib in Hep3B xenografts may be
attributed to the inhibition of cell proliferation and the
induction of apoptotic cell death.
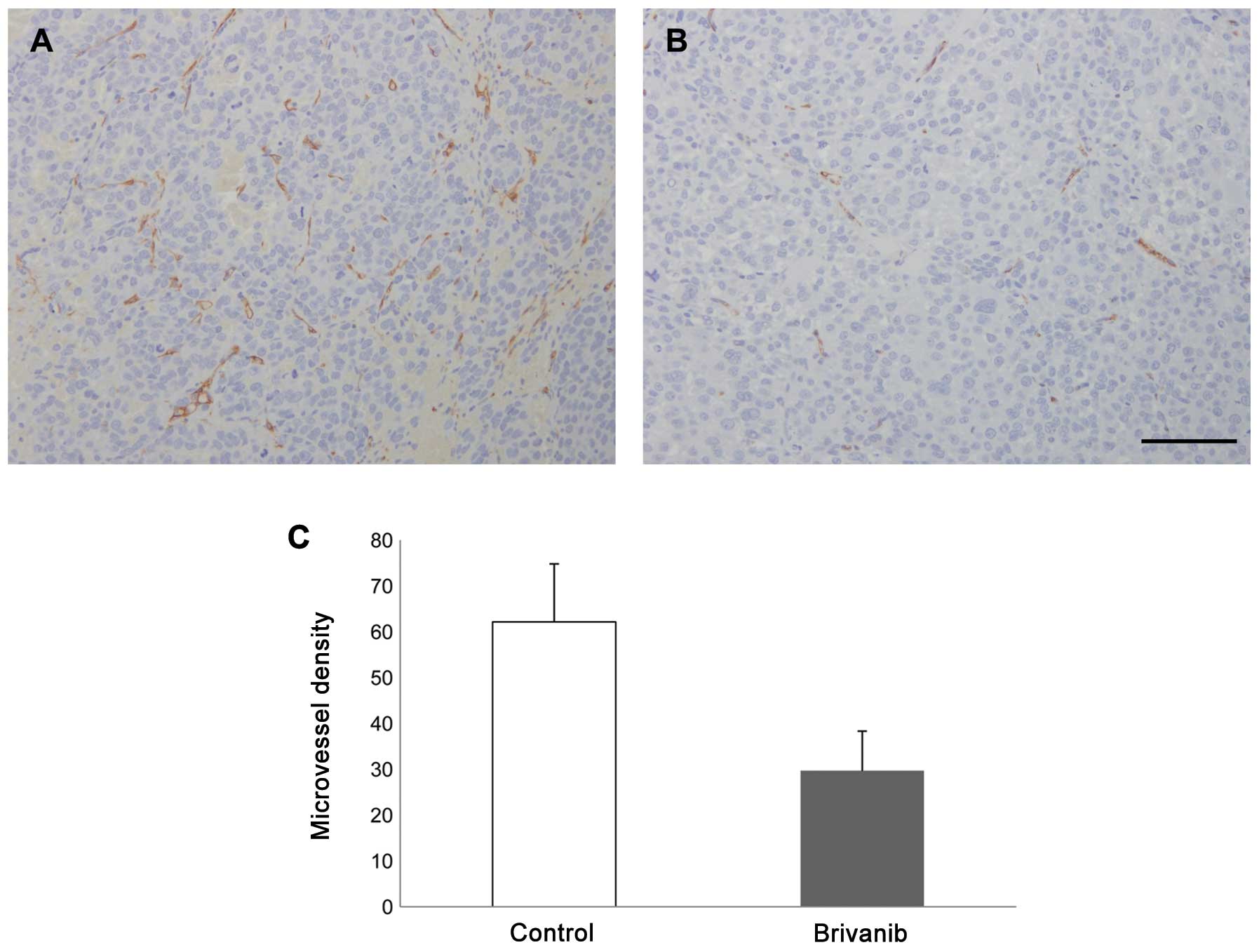
Effect on MVD
The specific effects of brivanib on tumor
microvasculature from vehicle-treated and brivanib-treated animals
were immunohistochemically analyzed with CD31 antibody reactivity
in vascular tumor areas without necrosis. As shown in Fig. 3, tumor microvessels were
significantly reduced in tumor tissue from brivanib-treated mice
compared with tumor tissue from vehicle-treated mice. MVD in
vehicle-treated mice was 58.51±13.37 18 days following treatment,
but that in brivanib-treated mice was 28.42±8.26. There was a
significant reduction in brivanib-treated tumor MVD compared with
the vehicle-treated tumor (51% reduction; P<0.05). These results
are consistent with the hypothesis that targeting tumor-associated
angiogenesis is a primary mechanism of antitumor activity of
brivanib in the Hep3B xenograft model.
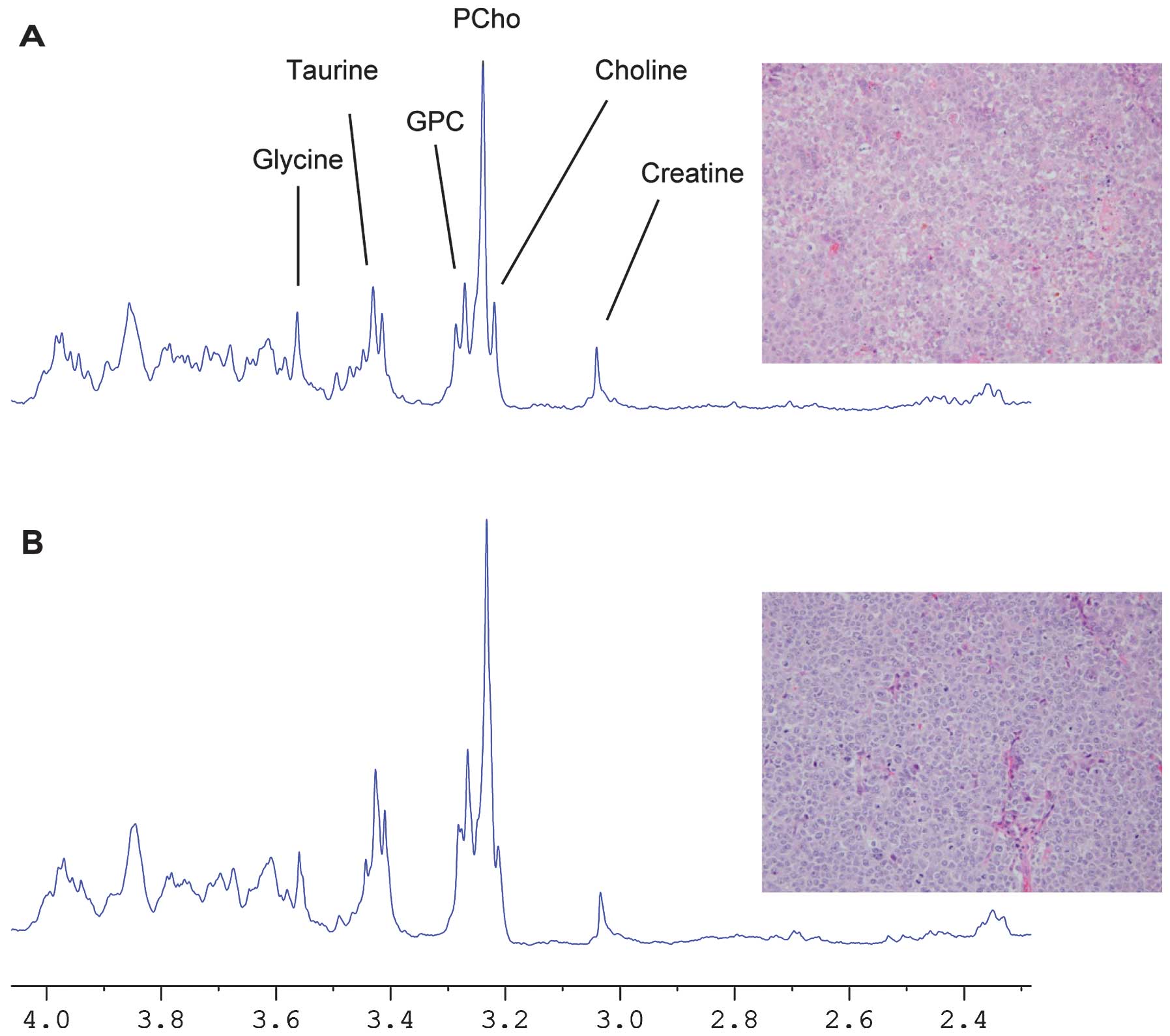
1H HR-MAS MR spectroscopy
To investigate the effect of brivanib treatment on
xenografted Hep3B tumor metabolism, 1H HR-MAS MRS was
used as described in Materials and methods. Representative
1H HR-MAS spectra from a control and a treated tumor are
shown in Fig. 4 with assignments
for the majority of the metabolites, including glycine (3.56 ppm),
taurine (3.42 ppm), glycerophosphocholine (GPC, 3.23 ppm),
phosphocholine (PCho, 3.21 ppm), choline (Cho, 3.19 ppm) and
creatine (3.04 ppm). As shown in the results, the HR-MAS MRS
analyses demonstrated significant differences in the
choline-containing metabolic profiles (Cho, PCho and GPC) between
vehicle-treated control mice (n=7) and brivanib-treated mice (n=8).
The choline-containing metabolites tended to decrease in
brivanib-treated tumor tissues. The concentration of PCho, which
was the largest peak in the two groups was 6.56±1.28 μmol/g in the
vehicle-treated control mice and 5.54±0.97 μmol/g in the
brivanib-treated mice, while the concentration of GPC was 3.49±0.82
μmol/g in the vehicle-treated control mice and 2.45±0.18 μmol/g in
the brivanib-treated mice (P<0.05, Mann-Whitney U test).
Discussion
In the present study, 1H HR-MAS and
histopathology were used to investigate the effects of treatment
with brivanib in a human HCC xenograft. As shown in the results,
brivanib, a novel, dual tyrosine kinase inhibitor with selectivity
against VEGF and FGF receptors, effectively inhibited tumor growth
in Hep3B xenografts and was associated with the inhibition of
angiogenesis, increased apoptosis and inhibition of cell
proliferation.
Generally, HCC tumors are hypervascularized,
suggesting that they may be particularly vulnerable to angiogenesis
inhibition (20). Several
endogenous proangiogenic factors and modulators are expressed in
HCC, and studies have indicated that they may be involved in HCC
pathogenesis. A number of studies have indicated that VEGF and
basic FGF are important proangiogenic factors that are central in
the progression of HCC by promoting tumor angiogenesis and
subsequent growth and metastasis (21,22).
VEGF is considered to be one of the most important angiogenic
factors involved in HCC vascularization. Elevated expression of
VEGF is associated with histopathologic tumor grade, postoperative
recurrence, poor prognosis and tumor microvessel density in HCC
(23). Overexpression of bFGF is
also detected in patients with HCC. Basic FGF stimulates the
release and activity of collagenases, proteases and integrins on
the extracellular membrane to form nascent microvascular networks.
Furthermore, bFGF has been shown to synergistically increase
VEGF-mediated HCC development and angiogenesis (24,25).
Due to the complex interactions among tumor cells, the invading
stroma and novel blood vessels, therapeutic antiangiogenic agents
that target a single angiogenic molecule have shown limited
efficacy in clinical trials (26,27).
Thus, the dual inhibition of VEGF and FGF signaling pathways, which
promote angiogenesis and metastasis may be a novel antiangiogenic
therapeutic strategy in HCC. Therefore, brivanib, a dual inhibitor
of VEGFR and FGFR tyrosine kinases was administered in an HCC
xenograft model in the present study.
In several tumor xenograft models, the daily
administration of brivanib induced significant tumor growth
inhibition. Brivanib has shown significant dose-dependent tumor
growth inhibition in breast, colon and lung xenograft models
(11). However, the exact
mechanisms by which brivanib treatment induces growth inhibition
are not well understood. Brivanib may prevent the tumor mass from
expanding by disrupting the supply of nutrients and growth factors
to the tumor cells. In addition, results of previous in
vitro and in vivo studies have shown that brivanib
affects the host endothelium (9,11).
In a preclinical study, brivanib significantly suppressed tumor
growth in six HCC xenograft lines when orally administered once
daily (10). Consistent with
results from other studies, the results of the present study have
demonstrated that the daily administration of brivanib
significantly inhibited the growth of Hep3B xenografts. Brivanib
therapy decreased tumor growth by 64%. Immunohistochemical analyses
demonstrated that treatment with brivanib exhibited a significant
effect on the inhibition of cell proliferation and induction of
apoptosis in tumors compared with the vehicle-treated control,
suggesting that brivanib results in apoptosis of the Hep3B
xenograft tumor. The results of the present study also showed that
the marked reduction in MVD with brivanib therapy compared with
vehicle-treated control is noteworthy, as a decrease in tumor
vessel density induced by antiangiogenic agents is expected to
reduce tumor perfusion and thereby oxygen delivery. The balance
between the proangiogenic and antiangiogenic molecules released by
tumor cells and surrounding host cells determines the intense tumor
vascularization. Previous studies have demonstrated that
VEGF-positive tissue was associated with a high MVD expression,
whereas VEGF-negative tissue demonstrated a low expression of MVD,
suggesting a positive correlation between VEGF and MVD (28). This result suggests that the potent
antiangiogenic activity of brivanib is the primary mechanism of the
inhibition of tumor growth in a Hep3B xenograft animal model.
A number of HR-MAS MRS approaches have demonstrated
altered tumor metabolic profiles for treated tumors, in conjunction
with subsequent histopathology of the same tumor specimen, which
supports histopathological examination and improves the accuracy in
the diagnosis, characterization, and evaluation of tumor
progression in different tumors (12,16,17).
In this study, 1H HR-MAS MRS was used to investigate how
brivanib treatment influences the metabolic profiles of Hep3B
xenografts. As shown in the results, the 1H HR-MAS MR
spectra were dominated by choline, creatine and taurine in the
region above 3 ppm. The 1H HR-MAS spectra show
significantly higher levels of PCho and GPC in the vehicle-treated
control tumors, supporting the hypothesis that brivanib treatment
induces changes in metabolism. It has been previously observed that
the choline metabolites that are regulated by several signaling
pathways are important in phospholipid metabolism and these choline
metabolites increase with tumor malignancy (29,30).
The in vivo choline metabolite signal is dependent upon the
cellular concentrations of GPC, PCho and Cho. Several biochemical
studies have suggested that PCho is a precursor as well as a
breakdown product of the predominant membrane component
phosphatidylcholine, whereas GPC is solely a membrane breakdown
product (31). In accordance with
previous studies, the decreased choline-containing metabolites as a
therapeutic response to brivanib in the present 1H
HR-MAS MRS results may be due to decreased cell density, which is
in agreement with histopathology showing decreased cell
proliferation and increased apoptotic cell death.
In conclusion, this study has shown that the
vascular targeting agent brivanib is highly efficacious in Hep3B
xenograft and is associated with an inhibition of angiogenesis,
increased apoptosis and inhibition of cell proliferation.
Furthermore, the results suggested that the additional information
obtained by HR-MAS MRS metabolic profiling may be a feasible tool
for evaluating the therapeutic response and supporting
histopathological analysis through the quantification of altered
metabolic profiles following treatment with therapeutic agents.
Acknowledgements
This study was conducted with the support of a grant
(to D.I.C.) from the Korean Healthcare Technology R&D Project,
Ministry for Health, Welfare and Family Affairs, Korea (grant no:
A102142).
References
|
1
|
Folkman J: What is the evidence that
tumors are angiogenesis dependent? J Natl Cancer Inst. 82:4–6.
1990. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ferrara N: Vascular endothelial growth
factor as a target for anticancer therapy. Oncologist. 9(Suppl 1):
2–10. 2004. View Article : Google Scholar
|
|
3
|
Hicklin DJ and Ellis LM: Role of the
vascular endothelial growth factor pathway in tumor growth and
angiogenesis. J Clin Oncol. 23:1011–1027. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kerbel RS: Tumor angiogenesis. N Engl J
Med. 358:2039–2049. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Presta M, Dell’Era P, Mitola S, Moroni E,
Ronca R and Rusnati M: Fibroblast growth factor/fibroblast growth
factor receptor system in angiogenesis. Cytokine Growth Factor Rev.
16:159–178. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Turner N and Grose R: Fibroblast growth
factor signalling: from development to cancer. Nat Rev Cancer.
10:116–129. 2010. View
Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hurwitz H, Fehrenbacher L, Novotny W,
Cartwright T, Hainsworth J, Heim W, Berlin J, Baron A, Griffing S,
Holmgren E, Ferrara N, Fyfe G, Rogers B, Ross R and Kabbinavar F:
Bevacizumab plus irinotecan, fluorouracil, and leucovorin for
metastatic colorectal cancer. N Engl J Med. 350:2335–2342. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Cheng AL, Kang YK, Chen Z, Tsao CJ, Qin S,
Kim JS, Luo R, Feng J, Ye S, Yang TS, et al: Efficacy and safety of
sorafenib in patients in the Asia-Pacific region with advanced
hepatocellular carcinoma: a phase III randomised, double-blind,
placebo-controlled trial. Lancet Oncol. 10:25–34. 2009. View Article : Google Scholar
|
|
9
|
Diaz-Padilla I and Siu LL: Brivanib
alaninate for cancer. Expert Opin Investig Drugs. 20:577–586. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Huynh H, Ngo VC, Fargnoli J, Ayers M, Soo
KC, Koong HN, Thng CH, Ong HS, Chung A, Chow P, Pollock P, Byron S
and Tran E: Brivanib alaninate, a dual inhibitor of vascular
endothelial growth factor receptor and fibroblast growth factor
receptor tyrosine kinases, induces growth inhibition in mouse
models of human hepatocellular carcinoma. Clin Cancer Res.
14:6146–6153. 2008. View Article : Google Scholar
|
|
11
|
Marathe PH, Kamath AV, Zhang Y, D’Arienzo
C, Bhide R and Fargnoli J: Preclinical pharmacokinetics and in
vitro metabolism of brivanib (BMS-540215), a potent VEGFR2
inhibitor and its alanine ester prodrug brivanib alaninate. Cancer
Chemother Pharmacol. 65:55–66. 2009. View Article : Google Scholar
|
|
12
|
Sitter B, Lundgren S, Bathen TF, Halgunset
J, Fjosne HE and Gribbestad IS: Comparison of HR MAS MR
spectroscopic profiles of breast cancer tissue with clinical
parameters. NMR Biomed. 19:30–40. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Beckonert O, Coen M, Keun HC, Wang Y,
Ebbels TM, Holmes E, Lindon JC and Nicholson JK: High-resolution
magic-angle-spinning NMR spectroscopy for metabolic profiling of
intact tissues. Nat Protoc. 5:1019–1032. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Cheng LL, Burns MA, Taylor JL, He W,
Halpern EF, McDougal WS and Wu CL: Metabolic characterization of
human prostate cancer with tissue magnetic resonance spectroscopy.
Cancer Res. 65:3030–3034. 2005.PubMed/NCBI
|
|
15
|
Swanson MG, Zektzer AS, Tabatabai ZL,
Simko J, Jarso S, Keshari KR, Schmitt L, Carroll PR, Shinohara K,
Vigneron DB and Kurhanewicz J: Quantitative analysis of prostate
metabolites using 1H HR-MAS spectroscopy. Magn Reson
Med. 55:1257–1264. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Erb G, Elbayed K, Piotto M, Raya J,
Neuville A, Mohr M, Maitrot D, Kehrli P and Namer IJ: Toward
improved grading of malignancy in oligodendrogliomas using
metabolomics. Magn Reson Med. 59:959–965. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Rocha CM, Barros AS, Gil AM, Goodfellow
BJ, Humpfer E, Spraul M, Carreira IM, Melo JB, Bernardo J, Gomes A,
Sousa V, Carvalho L and Duarte IF: Metabolic profiling of human
lung cancer tissue by 1H high resolution magic angle
spinning (HRMAS) NMR spectroscopy. J Proteome Res. 9:319–332. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sitter B, Bathen T, Hagen B, Arentz C,
Skjeldestad FE and Gribbestad IS: Cervical cancer tissue
characterized by high-resolution magic angle spinning MR
spectroscopy. MAGMA. 16:174–181. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yang J, Kim JH, Im GH, Heo H, Yoon S, Lee
J, Lee JH and Jeon P: Evaluation of antiangiogenic effects of a new
synthetic candidate drug KR-31831 on xenografted ovarian carcinoma
using dynamic contrast enhanced MRI. Korean J Radiol. 12:602–610.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Frenette C and Gish R: Targeted systemic
therapies for hepatocellular carcinoma: clinical perspectives,
challenges and implications. World J Gastroenterol. 18:498–506.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Miura H, Miyazaki T, Kuroda M, Oka T,
Machinami R, Kodama T, Shibuya M, Makuuchi M, Yazaki Y and Ohnishi
S: Increased expression of vascular endothelial growth factor in
human hepatocellular carcinoma. J Hepatol. 27:854–861. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Torimura T, Sata M, Ueno T, Kin M, Tsuji
R, Suzaku K, Hashimoto O, Sugawara H and Tanikawa K: Increased
expression of vascular endothelial growth factor is associated with
tumor progression in hepatocellular carcinoma. Hum Pathol.
29:986–991. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Moon WS, Rhyu KH, Kang MJ, Lee DG, Yu HC,
Yeum JH, Koh GY and Tarnawski AS: Overexpression of VEGF and
angiopoietin 2: a key to high vascularity of hepatocellular
carcinoma? Mod Pathol. 16:552–557. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Hsu PI, Chow NH, Lai KH, Yang HB, Chan SH,
Lin XZ, Cheng JS, Huang JS, Ger LP, Huang SM, Yen MY and Yang YF:
Implications of serum basic fibroblast growth factor levels in
chronic liver diseases and hepatocellular carcinoma. Anticancer
Res. 17:2803–2809. 1997.PubMed/NCBI
|
|
25
|
Mise M, Arii S, Higashituji H, Furutani M,
Niwano M, Harada T, Ishigami S, Toda Y, Nakayama H, Fukumoto M,
Fujita J and Imamura M: Clinical significance of vascular
endothelial growth factor and basic fibroblast growth factor gene
expression in liver tumor. Hepatology. 23:455–464. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Adams J, Huang P and Patrick D: A strategy
for the design of multiplex inhibitors for kinase-mediated
signalling in angiogenesis. Curr Opin Chem Biol. 6:486–492. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Laird AD and Cherrington JM: Small
molecule tyrosine kinase inhibitors: clinical development of
anticancer agents. Expert Opin Investig Drugs. 12:51–64. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Li W, Liu ML, Cai JH, Tang YX, Zhai LY and
Zhang J: Effect of the combination of a cyclooxygenase-1 selective
inhibitor and taxol on proliferation, apoptosis and angiogenesis of
ovarian cancer in vivo. Oncol Lett. 4:168–174.
2012.PubMed/NCBI
|
|
29
|
Jensen LR, Huuse EM, Bathen TF, Goa PE,
Bofin AM, Pedersen TB, Lundgren S and Gribbestad IS: Assessment of
early docetaxel response in an experimental model of human breast
cancer using DCE-MRI, ex vivo HR MAS, and in vivo 1H
MRS. NMR Biomed. 23:56–65. 2010. View
Article : Google Scholar : PubMed/NCBI
|
|
30
|
Moestue S, Sitter B, Bathen TF, Tessem MB
and Gribbestad IS: HR MAS MR spectroscopy in metabolic
characterization of cancer. Curr Top Med Chem. 11:2–26. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Seierstad T, Røe K, Sitter B, Halgunset J,
Flatmark K, Ree AH, Olsen DR, Gribbestad IS and Bathen TF:
Principal component analysis for the comparison of metabolic
profiles from human rectal cancer biopsies and colorectal
xenografts using high-resolution magic angle spinning 1H
magnetic resonance spectroscopy. Mol Cancer. 7:332008. View Article : Google Scholar
|