Introduction
Congenital ectopia lentis (CEL) occurs in a variety
of genetic diseases, including Marfan syndrome (MFS), acromicric
dysplasia, geleophysic dysplasia 2 and Weill Marchesani syndrome.
Fibrillin-containing microfibrils are the major components of
zonular fibers, and disruption of zonular fibers causes ectopia
lentis. The fibrillin 1 (FBN1) gene, encoding fibrillin 1 protein,
is generally identified as being mutated in the majority of the
cases of ectopia lentis. Microfibrils in the extracellular matrix
are predominantly composed of FBN1 protein, and serve an important
role in incorporating elastin into elastic fibers. As a result,
FBN1 mutations are associated with impairments in protein synthesis
and secretion, leading subsequently to their improper incorporation
into the connective tissue (1).
It has been well established that transforming
growth factor β (TGFβ) is a potent stimulator of inflammation,
fibrosis and the activation of certain matrix metalloproteinases
(MMPs), which serve multiple essential roles, including in
fibrosis, proliferation and wound repair (2,3).
TGFβ1, β2 and β3 are crucial isoforms expressed in mammals that are
able to bind to the same receptor to elicit their biological
effects. TGFβ2, in particular, is essential in ocular physiological
and pathological processes, and is predominantly localized in
limbal epithelial cells and the ciliary body (4,5). In
addition, activation of the TGFβ signaling pathways may accelerate
the progression of aneurysms and encourage pneumothorax (collapsed
lung) in MFS. Given what is currently known about TGFβ, treatments
based upon restricting TGFβ signaling are currently undergoing
clinical trials (6,7).
Isogai et al (8) reported that TGFβ produced by cells
acts as a large latent complex that is able to bind to
extracellular matrix (ECM) proteins, such as fibrillin 1. Current
models have demonstrated that blockade of TGFβ by ECM chelating
ligand leads to an inhibition of its activation, thus limiting the
stimulation of its cell surface receptor. On the other hand, an
elevation in the levels of TGFβ may exert its detrimental effects
(with respect to MFS) through two distinct intracellular signaling
pathways: The canonical and non-canonical signal transduction
pathways (9–11).
Regarding the canonical signaling pathway, TGFβ and
its receptor binding complex are able to significantly enhance
Smad2 and/or Smad3 phosphorylation, and, once phosphorylated, these
proteins cause the recruitment of Smad4, its translocation to the
nucleus, and the transcription of Smad-dependent genes (12). On the other hand, TGFβ activates
non-canonical pathways, including the MAPK and JNK signaling
pathways, p38 and RhoA cascades, the first of which includes ERK
(13–15).
In mouse models, blocking JNK leads to a reduction
in the activity of MMPs, which serve an important role in MFS
pathology, indicating that JNK might be a therapeutic target
(16). In addition, inhibiting the
p38 MAPK pathway leads to a suppression in the levels of the MMPs.
Furthermore, ERK1/2 blockade was revealed to elevate the levels of
MMP inhibitors on cell membranes (17). TGFβ increases the expression levels
of elastase and numerous MMPs (18). As an elevated level of elastase is
able to promote elastin degradation, and MMPs can invoke a major
collapse in the elastic fibers, overexpression of these proteases
is able to reduce connective tissue elasticity, thereby
contributing to instability of the aortic wall. The association
between TGFβ and MMP expression has been well elucidated in the MFS
mouse model (19).
High concentrations of active TGFβ are able to
activate multiple intracellular signaling pathways that are
involved in the progression of MFS. However, the underlying
mechanisms have yet to be properly elucidated. The aim of the
present study was to investigate the expression levels of TGFβ and
MMPs in the aqueous humor of patients with CEL and congenital
cataracts (CC), and their potential correlation with the severity
of ectopic lentis.
Patients and methods
Patients and samples
An observational study was conducted on 17 patients
with CEL and 12 patients with CC. It was necessary that the
patients who applied to Zhongshan Ophthalmic Center, Sun Yat-sen
University of Medicine between January 2015 and December 2016 had
been diagnosed with either CEL or CC. Inclusion criteria included
the following: i) Diagnosed with CEL or CC, respectively; ii)
patient aged between 1 and 32 years; and iii) patients in the CEL
group had no other ocular diseases, such as CC or other congenital
anterior segment malformations, with the exception of the abnormal
lens position. Exclusion criteria included the following: i)
Previous intraocular surgery; ii) lens dislocation or cataract
caused by head trauma, ocular trauma or surgery; and iii) the
presence of inflammatory or infectious eye diseases, glaucoma, or
use of topical or systemic anti-inflammatory or anti-infectious
agents prior to screening. Aqueous humor samples were collected
during clear lens extraction or cataract surgery. A total of 17 CEL
patients with 21 eyes and 12 CC patients with 17 eyes were selected
for the study, in order to deduce whether the TGFβ2 and MMP levels
were related to the severity of the lens dislocation in patients
with CEL.
Ethics
This research was performed in accordance with The
Declaration of Helsinki and was approved by the Institutional
Review Board at the Zhongshan Ophthalmic Center, Sun Yat-sen
University of Medicine. Written informed consent was obtained from
each of the 6 adult subjects, and from the legal guardians of the
23 children, in accordance with The Declaration of Helsinki. All
participants provided informed consent for the publication of their
data, including images and examination results.
Analysis of the degree of lens
dislocation
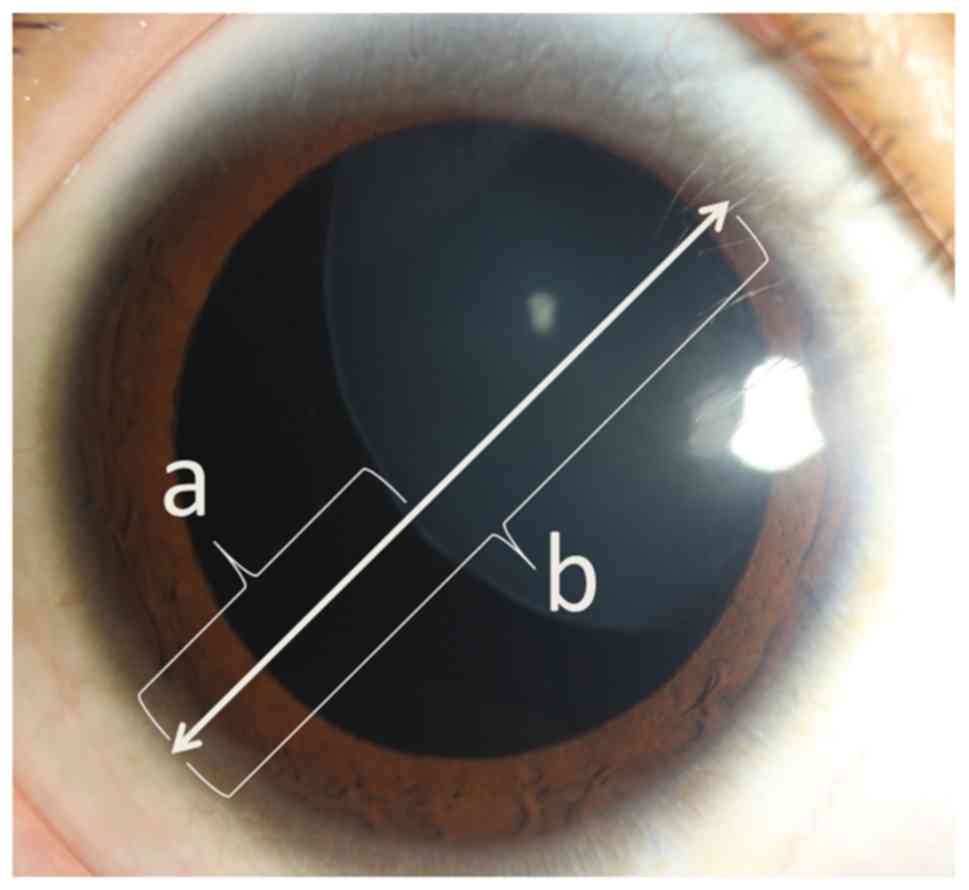
The degree of lens dislocation was defined by the
ratio of the distance from the lens edge to the pupil edge (a) and
the length of the white to white corneal diameter (i.e. the
horizontal distance between the borders of the corneal limbus) (b)
(Fig. 1). This was assessed on
anterior segment images from the hospital database of patients with
CEL. All the pupils of the patients were pharmacologically dilated
with 0.1 ml 0.5% tropicamide drops 30 min before examination.
Subsequently, two ophthalmologists and one non-ophthalmic physician
assessed the images.
Surgical technique
A single experienced surgeon (DYZ) performed the CEL
or CC operations in all cases. Topical 0.3% ofloxacin eye drop was
applied four times each day at 0.1 ml each time, for 3 days prior
to surgery. According to standard procedures, none of the patients
was in receipt of steroids prior to surgery.
Aqueous humor sampling
In the CEL and CC groups, the primary incision was
made under sterile conditions, and undiluted aqueous humor samples
(0.1–0.2 ml) were collected into a 30-gauge needle on a tuberculin
microsyringe. The samples were immediately frozen, and stored at
−80°C until measurements were made. All samples were collected
during the year 2016, and stored for 2–3 months under identical
conditions.
Multiplex analysis of cytokines in the
aqueous humor
All samples were assessed for the total protein
levels of TGFβ1, TGFβ2, TGFβ3 and MMP-1, −2, −3, −7, −8, −9, −10,
−12 and −13 using the Luminex system (Luminex xMAP®
technology; Bio-Rad Laboratories, Inc.) and commercially available
Bio-Plex Pro™ Human MMP (catalog number: 171AM001M, Bio-Rad
Laboratories, Inc.) and TGFβ (catalog number: 171W4001M, Bio-Rad
Laboratories, Inc.) assays. Each sample was measured twice. The
amount (in pg/ml) of TGFβ/MMPs present was quantified from the
standard curve of each measurement. The same aqueous humor sample
was measured in each plate as an internal control.
Statistical analysis
Every experiment was repeated twice. Statistical
analysis was performed using SPSS 13.0 software for Windows (SPSS,
Inc.). Some of the data values, which were not normally
distributed, were analyzed using the Kolmogorov-Smirnov test, and
the results are shown as the median and range (25th and 75th
percentiles) for continuous variables under these conditions,
including the expression levels of TGFβ/MMPs. The mean ± SD was
evaluated for normally distributed continuous variables, such as
the age of the patients. A nonparametric test (Mann-Whitney U test)
was used to compare abnormally distributed values of TGFβ/MMPs
among the different groups between males and females. The
proportions (percentages) of the qualitative variable of sex were
analyzed using Pearson's χ2 test. The Spearman
correlation coefficient method was used to analyze the correlation
between TGFβ/MMPs and the degree of lens dislocation, or between
TGFβ/MMPs and the age of the patients. P<0.05 was considered to
indicate a statistically significant difference.
Results
Demographic characteristics of 29
patients (38 eyes in total)
Aqueous humor samples were obtained from 38 eyes
from 29 subjects. A total of 17 CEL patients with 21 eyes (aged
12.76±9.37 years) and 12 CC patients with 17 eyes (aged 6.82±9.18
years) were randomized in the present study (Table I). No statistically significant
differences in either sex distribution or age were observed between
these two groups. Furthermore, the 17 CEL patients were analyzed
via standard echocardiography, and the presence of tricuspid
incompetence and aorto-sinus dilatation was identified in 23%
(4/17) and 35% (6/17) of the enrolled subjects, respectively;
tricuspid prolapse, ascending aorta extension, patent oval foramen
and ventriculus sinister diastolic function decrease were
identified in 5% (1/17) respectively. Only for 3 of the patients
were no apparent abnormalities identified in terms of cardiac
architecture and function. These patients in the CEL group had no
other ocular diseases, such as CC or other congenital anterior
segment malformations, except for the abnormal lens position.
 | Table I.Demographic characteristics of 29
patients (comprising 38 eyes in total) in the CEL and CC
groups. |
Table I.
Demographic characteristics of 29
patients (comprising 38 eyes in total) in the CEL and CC
groups.
| Characteristic | CEL group | CC group |
|---|
| Total no. of
subjects (no. of eyes) | 17 (21) | 12 (17) |
| Age, years; mean ±
SD (range) | 12.76±9.37
(5–32) | 6.82±9.18
(1–32) |
| Sex, M/F | 11/6 | 6/6 |
| Tricuspid prolapse,
n | 1 | – |
| Tricuspid
incompetence | 4 | – |
| Aorto-sinus
dilatation | 6 | – |
| Ascending aorta
extension | 1 | – |
| Patent oval
foramen | 1 | – |
| Ventriculus
sinister diastolic function decrease | 1 | – |
| Without heart
disease | 3 | – |
Levels of TGFβ1, −2 and −3
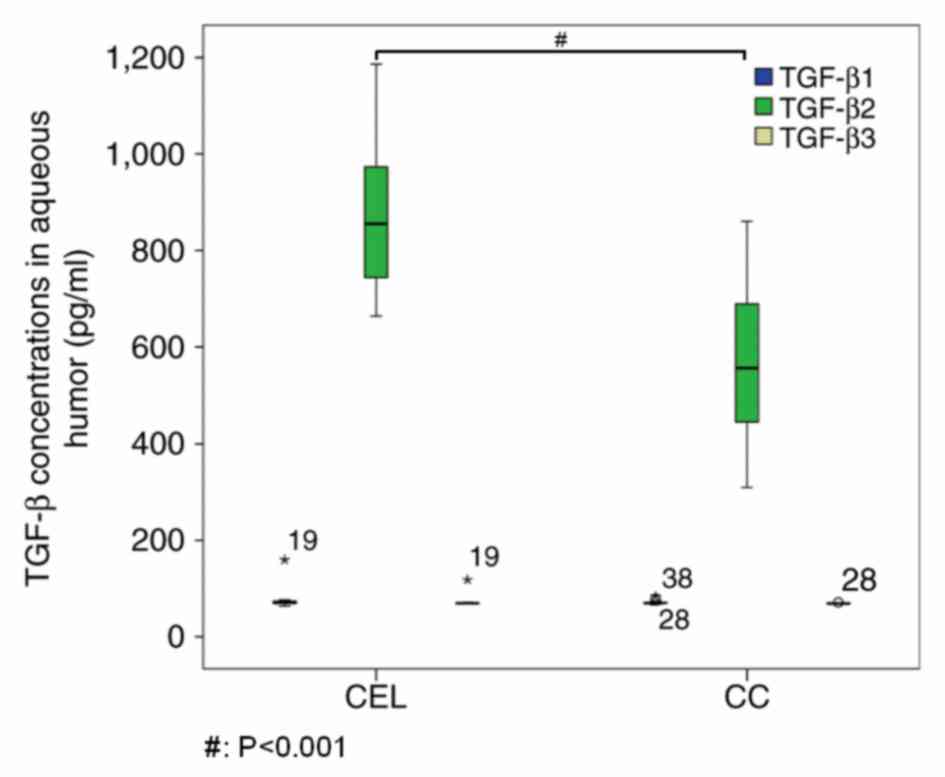
The difference between the TGFβ2 levels in the CEL
and CC groups was identified to be statistically significant
(P<0.001). The level of TGFβ2 in the CEL patients was 855.19
(744.33, 1,009.24) pg/ml, whereas it was 557.08 (438.24, 692.71)
pg/ml in the CC patients (P<0.001). However, the differences in
the levels of TGFβ1 and TGFβ3 in the two groups were not revealed
to be statistically significant (Table II and Fig. 2).
 | Table II.Aqueous humor TGFβ/MMP levels in
patients with CEL and CC. |
Table II.
Aqueous humor TGFβ/MMP levels in
patients with CEL and CC.
|
| CEL group Degree of
lens dislocation |
|
|
|---|
|
|
|
|
|
|---|
|
|
| TGFβ/MMP,
pg/ml | All | <0.4 | >0.4 | CC group | P-value |
|---|
| TGFβ1, median (P25,
P75) | 71.15 (68.62,
73.68) | 71.15 (68.87,
73.29) | 70.39 (68.62,
71.78) | 69.64 (67.36,
71.15) | 0.475 |
| TGFβ2, median (P25,
P75) | 855.19 (744.33,
1,009.24) | 749.94 (730.39,
796.44) | 954.09 (883.86,
1,121.05) | 557.08 (438.2,
692.71) |
<0.001a |
| TGFβ3, median (P25,
P75) | 69.57 (69.07,
69.98) | 69.67 (69.07,
69.92) | 69.57 (69.21,
69.98) | 69.07 (68.79,
69.57) | 0.49 |
| MMP-2, median (P25,
P75) | 552,803.83 | 561,063.74 | 541652.94 | 535,458.01 | 0.325 |
|
| (474,334.63,
676,702.56) | (549,706.36,
783,874.96) |
(476399.61,736999.94) | (394,626.45,
652,955.31) |
| MMP-3, median (P25,
P75) | 24,874.10
(12956.62, 36791.58) | 24,874.09
(12,956.62, 36,791.57) | 28,449.34
(14,820.54, 39,770.94) | 24,874.1
(12,956.62, 36,791.58) | 0.552 |
| MMP-7, median (P25,
P75) | 5,014.63 (4122.69,
6613.84) | 4,627.83 (3,731.67,
5,526.60) | 5,832.34 (4,628.28,
8,418.63) | 5,654.43 (3,953.61,
7,215.485) | 0.977 |
| MMP-8, median (P25,
P75) | 13,207.60
(8,327.02, 19,019.98) | 16,005.08
(8,437.79, 19,547.61) | 11,872.91
(9,209.54, 15,019.31) | 18,608.34
(13,065.12, 30,151.73) | 0.014a |
| MMP-9, median (P25,
P75) | 4,418.19 (4,018.74,
5,350.28) | 4,862.04 (4,174.08,
5,283.69) | 4,196.27 (4,085.31,
4,817.65) | 5,971.66 (4,773.27,
12,984.45) | 0.002a |
| MMP-10, median
(P25, P75) | 36,248.38
(29,234.96, 47,501.42) | 38,152.74
(32,483.39, 47,485.99) | 33,956.23
(29,234.96, 44,845.86) | 27,846.82
(21,557.86, 50,116.39) | 0.386 |
| MMP-12, median
(P25, P75) | 3,962.81 (2,975.89,
4,490.70) | 3,733.29 (3,159.50,
4,421.84) | 3,962.81 (3,320.17,
4,490.70) | 4,238.23 (3,733.29,
5,110.39) | 0.221 |
| MMP-13, median
(P25, P75) | 2,682.62 (2,243.78,
3,034.13) | 2,682.62 (2,316.88,
3,004.82) | 2,594.83 (2,375.38,
2,814.41) | 2,624.07 (2,448.49,
2,887.65) | 0.929 |
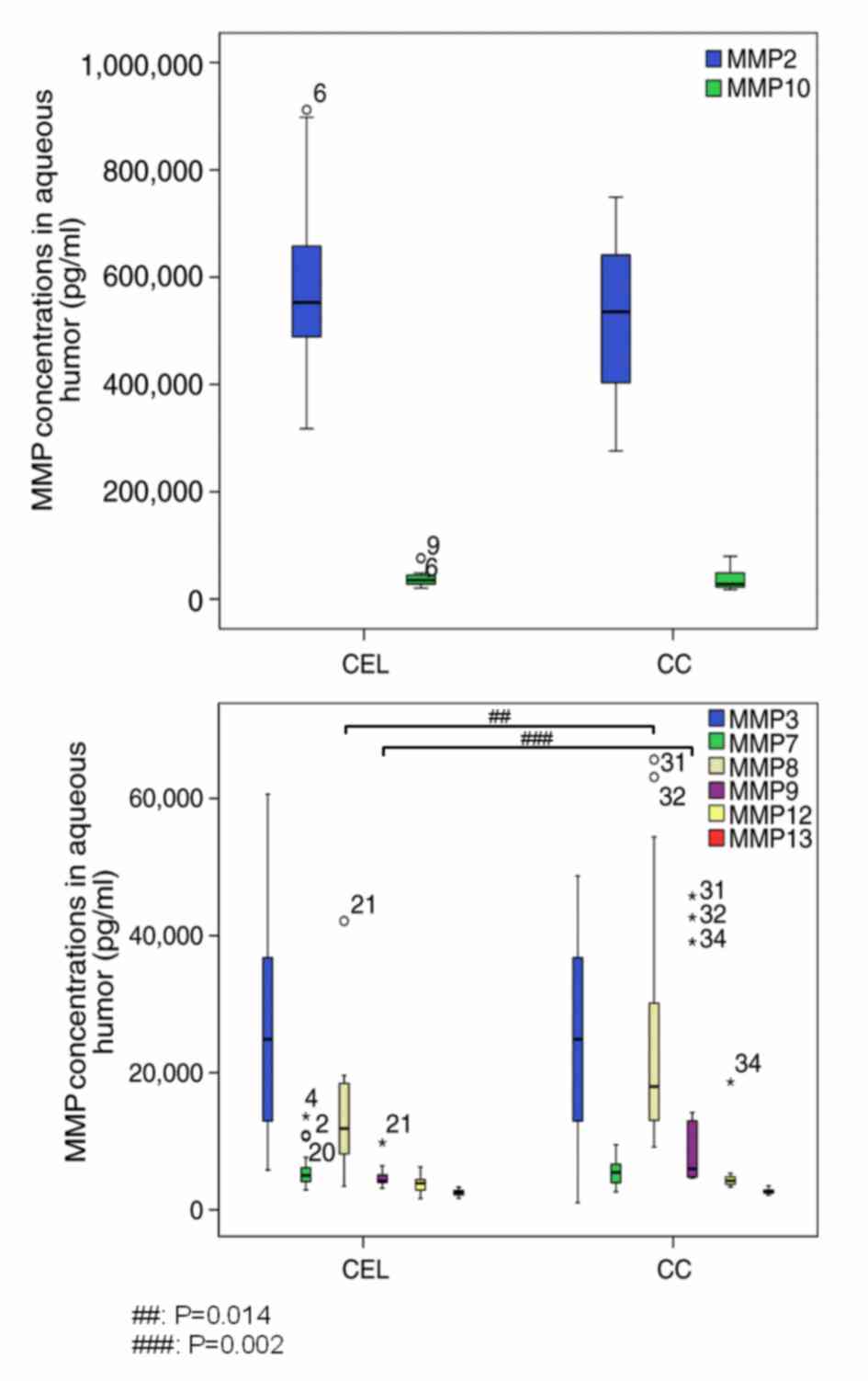
Levels of MMP1,-2,-3,-7,-8,-9,-10,-12
and −13
MMP-1 could not be detected in the majority of the
aqueous humor samples in the two groups. The differences identified
for MMP-2, −3, −7, −10, −12 and −13 in the two groups did not reach
the level of statistical significance (Table II and Fig. 3). The Mann-Whitney U test
demonstrated that the levels of MMP-2 and MMP-10 in the aqueous
humor from the patients with CEL were higher compared with those
from the patients with CC, although, again, this did not reach the
level of statistical significance (P=0.325 and P=0.386,
respectively). However, the levels of MMP-8 and MMP-9 in the
aqueous humor of patients with CEL were significantly lower
compared with those in the CC patients (P=0.014 and P=0.002;
Table II and Fig. 3).
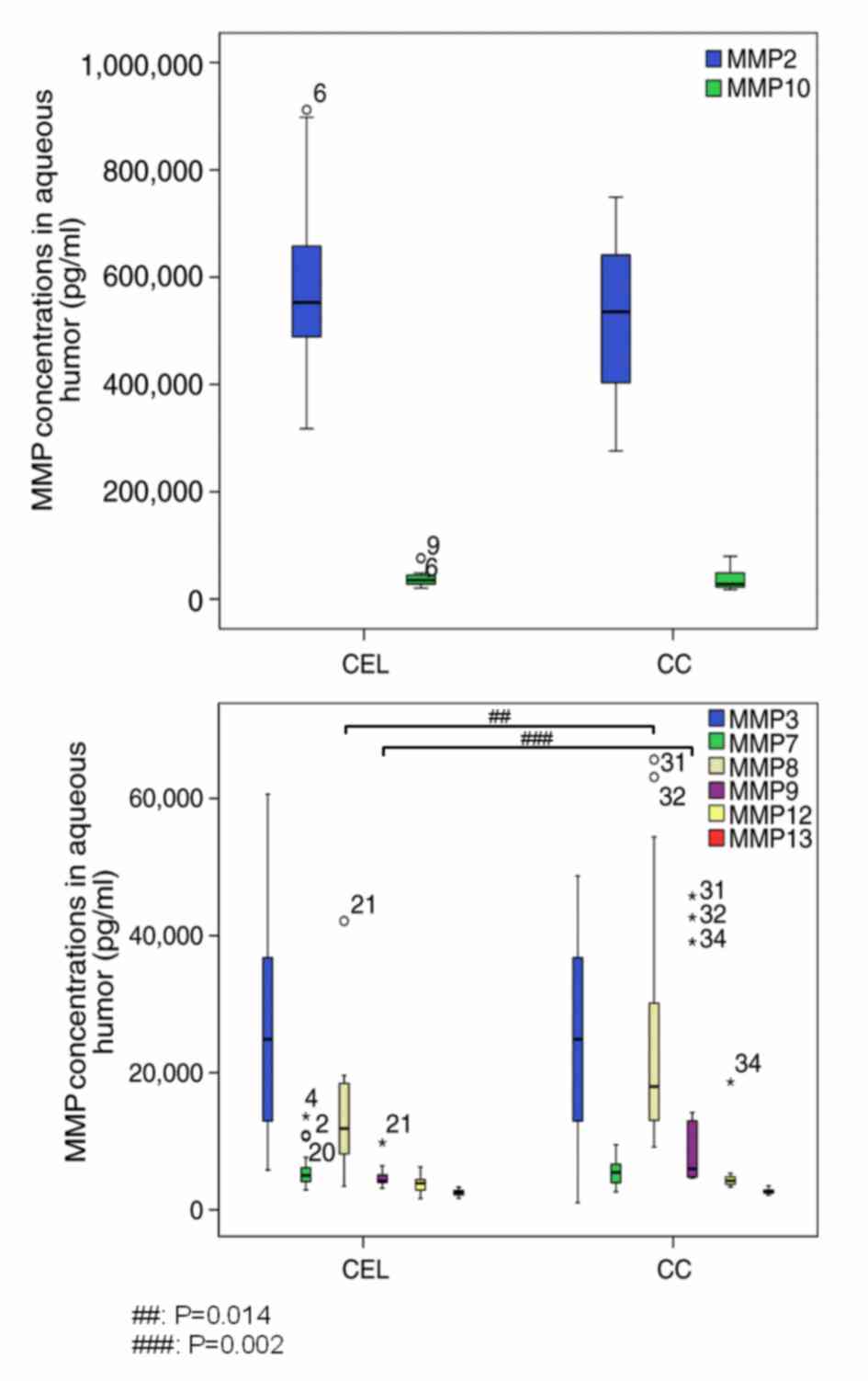 | Figure 3.Aqueous humor MMP levels in patients
with CEL and CC. MMPs levels in the aqueous humor from 29 patients
(38 eyes) in the CEL and CC groups were measured with Luminex
xMAP® Technology by using commercially available
Bio-Plex Pro™ Human MMP assays. The Mann-Whitney U test
demonstrated that the levels of MMP-2 and MMP-10 in the aqueous
humor in the patients with CEL were higher compared with those in
the patients with CC, although, this did not reach the level of
statistical significance (P=0.325 and P=0.386, respectively).
However, the levels of MMP-8 and MMP-9 in the aqueous humor of
patients with CEL were significantly lower compared with those in
the CC patients (MMP-8: ##P=0.014 and MMP-9:
###P=0.002). The differences in MMP-2, −3, −7, −10, −12
and −13 in the two groups were not statistically significant.
However, MMP-1 could not be detected in the aqueous humor samples
in either group. MMP, matrix metalloproteinase; CEL, congenital
ectopia lentis; CC, congenital cataract. |
Relationship between TGFβ/MMPs and the
degree of lens dislocation in the CEL group
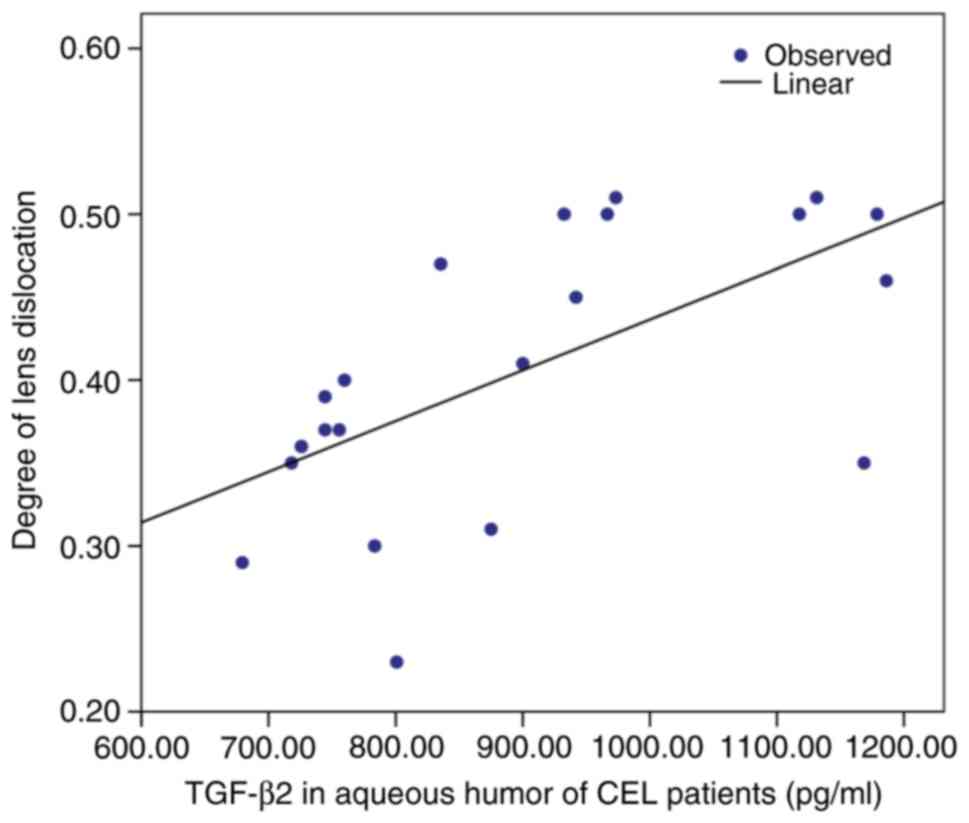
The Spearman correlation test revealed that there
was a significant positive correlation between the TGFβ2 level and
the degree of lens dislocation (r2=0.379, P=0.003;
Fig. 4). By contrast, no
significant correlation was identified between the degree of lens
dislocation and the levels of TGFβ1 and β3/MMP-2, −3, −7, −8, −9,
−10, −12 and −13 (Table III;
TGFβ1, P=0.263; TGFβ3, P=0.571; MMP-2, P=0.238; MMP-3, P=0.98;
MMP-7; P=0.989; MMP-8; P=0.552; MMP-9, P=0.638; MMP-10, P=0.726;
MMP-12, P=0.812; and MMP-13, P=0.853).
 | Table III.Association between the levels of
TGFβ/MMPs and degree of lens dislocation variable in CEL group and
also association between the levels of TGFβ/MMPs and age in CEL and
CC groups. |
Table III.
Association between the levels of
TGFβ/MMPs and degree of lens dislocation variable in CEL group and
also association between the levels of TGFβ/MMPs and age in CEL and
CC groups.
|
| Degree of lens
dislocation variable | Age |
|---|
|
|
|
|
|---|
|
| R | P-value | R | P-value |
|---|
| TGFβ1 | 0.014 | 0.263 | 0.008 | 0.592 |
| TGFβ2 | 0.379 | 0.003 | 0.298 | <0.001 |
| TGFβ3 | 0.017 | 0.571 | 0.01 | 0.547 |
| MMP2 | 0.086 | 0.238 | 0.01 | 0.56 |
| MMP3 | 0.000 | 0.98 | 0.008 | 0.597 |
| MMP7 | 0.000 | 0.989 | 0.003 | 0.736 |
| MMP8 | 0.019 | 0.552 | 0.083 | 0.079 |
| MMP9 | 0.012 | 0.638 | 0.05 | 0.178 |
| MMP10 | 0.007 | 0.726 | 0.016 | 0.453 |
| MMP12 | 0.002 | 0.812 | 0.039 | 0.232 |
| MMP13 | 0.003 | 0.853 | 0.08 | 0.085 |
Relationship between TGFβ/MMPs and age
in the CEL and CC groups
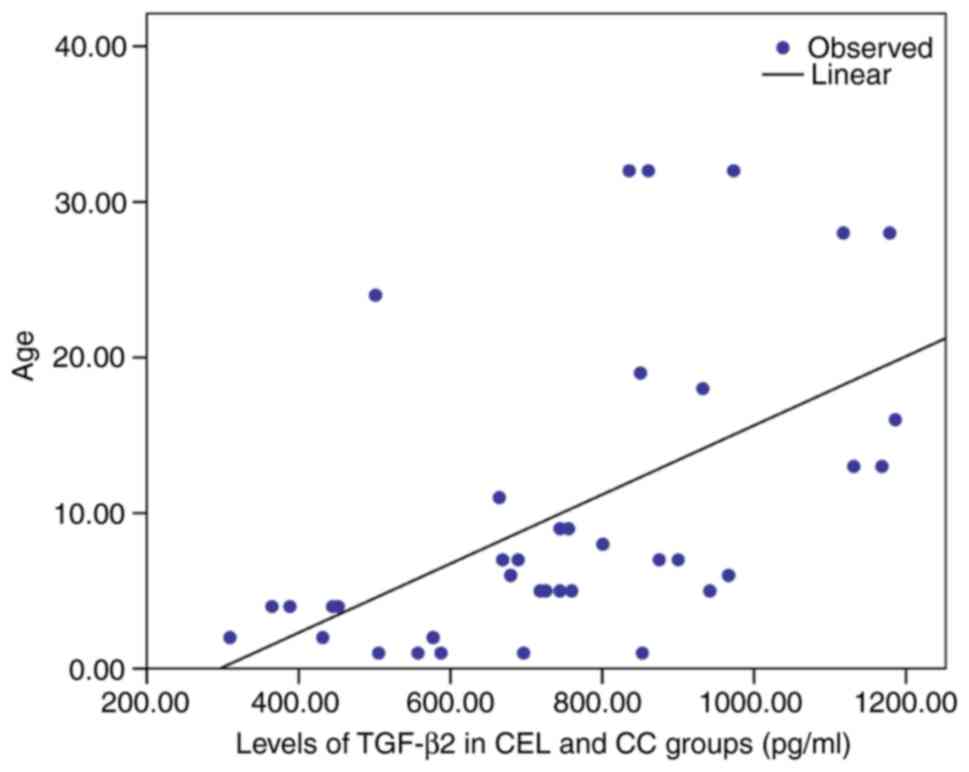
The Spearman correlation test revealed that TGFβ2
was positively correlated with age (r2=0.298,
P<0.001; Fig. 5).
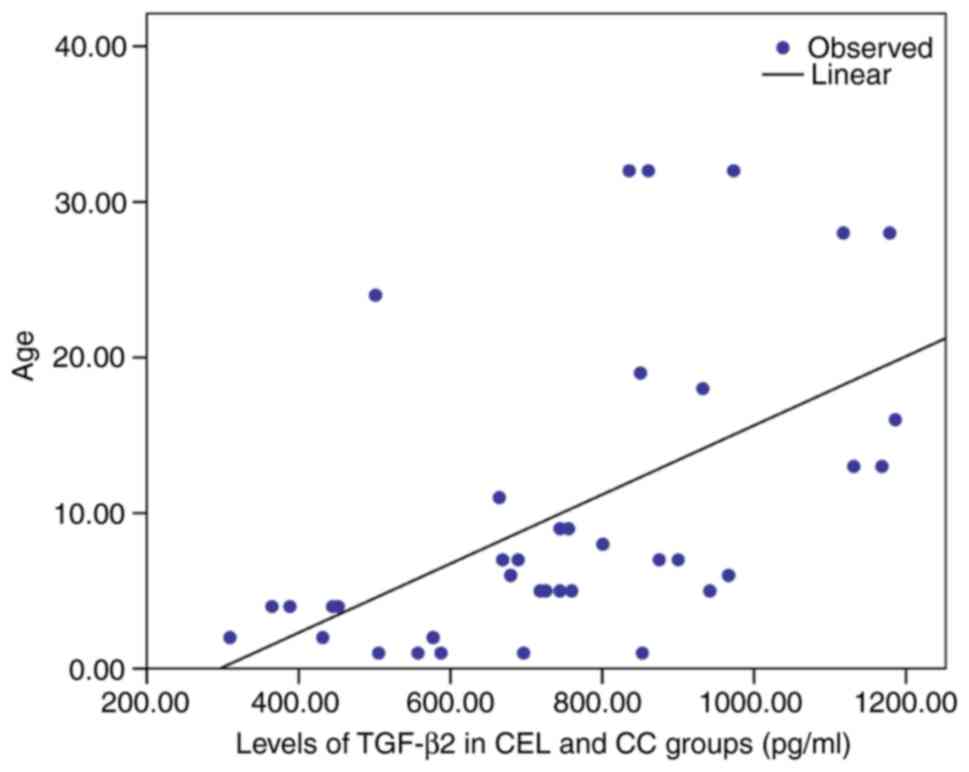 | Figure 5.Correlation between TGFβ2
concentration and age in patients with CEL and CC. MMP and TGFβ2
levels in the aqueous humor from 29 patients (38 eyes) in the CEL
and CC groups were measured with Luminex xMAP®
Technology by using commercially available Bio-Plex Pro™ Human MMP
and TGFβ assays. Spearman correlation test showed that TGFβ2 were
positively correlated with the age (r2=0.298;
P<0.001). No significant correlation was found between the age
and TGFβ1 and 3, MMP-2, −3, −7, −8, −9, −10, −12 and 13 levels.
MMP, matrix metalloproteinase; TGFβ, transforming growth factor β;
CEL, congenital ectopia lentis; CC, congenital cataract. |
However, the correlation identified between age and
the levels of TGFβ1 and β3, and MMP-2, −3, −7, −8, −9, −10, −12 and
−13 did not reach the level of statistical significance (Table III; TGFβ1, P=0.592; TGFβ3,
P=0.547; MMP-2, P=0.56; MMP-3, P=0.597; MMP-7, P=0.736; MMP-8,
P=0.079; MMP-9, P=0.178; MMP-10, P = 0.453; MMP-12, P=0.232; and
MMP-13, P=0.085).
Discussion
To the best of the authors' knowledge, the present
study is the first to confirm that the expression levels of TGFβ2
in the aqueous humor of patients with CEL is associated with the
severity of ectopia lentis, suggesting the important role of TGFβ
and MMPs in the pathological process of CEL.
MFS is characterized as a hereditary disorder with
various symptoms, including skeletal, cardiovascular and ocular
systems (20). CEL is one of the
most commonly identified ocular disorders identified in people with
MFS. It is well-recognized that reduced or mutant forms of
fibrillin 1, which induces increased levels of TGFβ activation, is
the precise factor that results in the different clinical features
(13). Furthermore, the abnormal
homeostasis resulting from overexpression of MMP-2 and MMP-9 leads
to a slow deterioration of both the elastin fibers and other
components of the ECM (21). The
aforementioned reports established that TGFβ signaling is able to
accelerate the progression of aneurysms and pneumothorax in
patients diagnosed with MFS. Therefore, the present hypothesis was
that TGFβ signaling may also drive ectopia lentis.
To validate this hypothesis, multiplex bead
immunoassays were performed to confirm the levels of TGFβ and MMPs
in the aqueous humor. It was identified that the concentration of
TGFβ2 was significantly increased in CEL patients compared with the
control groups, and a significant association was identified
between the levels of TGFβ2 in the aqueous humor of patients with
CEL and the severity of CEL, indicating that the signaling pathways
mediated by TGFβ serve a crucial role in the architecture and
function of the zonular fibers.
It has been previously shown that TGFβ is secreted
as a large latent complex that consists of TGFβ, its binding
protein and latency-associated peptide (22). Fibrillin 1, which is characterized
as an isomer of latent TGFβ binding proteins, is able to
specifically bind to the TGFβ latent complex. TGFβ signaling is
initiated by binding of TGFβ to its receptors, activating its
downstream signaling cascades by releasing the mature TGFβ that is
regulated by proteases or MMPs (23).
Previously, researchers have focused on the
canonical and non-canonical TGFβ signaling pathways, due to the
important roles they serve in aneurysms (16). On the basis of their results, the
present hypothesis was that a deficiency of fibrillin 1 in the
patients with CEL may inhibit matrix sequestration of the large
latent complex of TGFβ, subsequently rendering this cytokine more
prone to activation. Furthermore, TGFβ signaling may be involved in
the regulation of MMPs, causing CEL.
TGFβ is classified as an upstream mediator of matrix
metabolism, and MMPs are considered important factors in the
progression of aneurysms in patients with MFS (24). However, the role of TGFβ/MMPs in
ectopia lentis progression is yet to be properly elucidated. The
present study revealed that aqueous humor samples from patients
with CEL exhibited levels of MMP-2 and −10 that were higher
compared with those in patients with CC, although the level of
statistical significance was not attained. Interestingly, the
levels of MMP-8 and MMP-9 in the aqueous humor of the CEL patients
were significantly lower compared with those in the CC patients.
Since no healthy persons were included in the present study as a
control group, it was not possible to conclude that the levels of
MMPs in the aqueous humor of the CEL patients were higher than
those normally identified in the general population. However, the
levels of MMP-8 and MMP-9 in the aqueous humor of CC patients were
significantly higher, suggesting that MMPs may be an unknown factor
involved in CC.
MMPs and their tissue inhibitors are all expressed
in the aqueous humor with or without age-associated cataracts
(25). Upon a review of the
relevant literature, no studies reporting that MMPs in the aqueous
humor are relevant to CC were identified. Some findings have
indicated that lens cells may synthesize MMPs upon certain
injuries, such as cataract surgery or oxidative stress (26–28).
It has been documented that TGFβ drives anterior
subcapsular cataract formation due to the increasing levels of
MMP-2 and MMP-9, thereby promoting the development of posterior
capsule opacification (29–33).
Researchers have previously observed that the level of MMP-9
activity varies in different types of cataracts (34). It has been demonstrated that the
level of MMP-9 activity in lens epithelial cells increases with the
age of patients with age-associated cataract (34). However, MMP proteins are not only
secreted by ciliary non-pigment epithelial cells in the aqueous
humor (35). It has been reported
that scleral fibroblasts (36),
uveal melanocytes (37), ciliary
muscle cells (38–40), trabecular cells (41,42)
and retinal pigment epithelial cells (43–45)
are able to produce MMPs and secrete or exchange them to the
aqueous humor. The changes in the MMP expression levels may result
from the homeostatic mechanism of various cells in the aqueous
humor. Therefore, the levels of MMPs in the aqueous humor of CEL
patients may or may not serve a key role in the disintegration of
zonular fibers, and further studies are required to explore the
role of MMPs in ectopia lentis.
A limitation of the present study was that these
samples were not compared with age-matched control healthy persons,
due to ethical reasons. On the other hand, active inflammatory
factors in the aqueous humor in the eyes of cadavers are degraded
slowly, because the protein in the aqueous humor of cadavers is
easy to dissolve and inactivate. Due to the age factor, CC patients
were included to provide a study contrast. Besides, the only
accurate information about congenital ectopia lentis available was
a general diagnosis, with no genetic information due to economic or
technical reasons. Therefore, it was not possible to make the
diagnosis of MFS. The small number of patients enrolled also
limited the results, and further studies are required that include
a larger number of subjects.
In conclusion, the findings in the present study
indicated that TGFβ signaling activation may promote the
progression of CEL. These findings may support targeting TGFβ
signaling as a potential therapy to prevent the complications in
patients with MFS that arise from CEL.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Science and
Technology Planning Project of Guangdong Province (grant no.
2014A020212106) and the National Natural Science Foundation (grant
no. NSFC 81873673).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
QC, BX, GJ and DZ conceived and designed the
experiments. BX performed the experiments. BZ, MC and KW analyzed
the data. JiL, YW, JuL and YZ contributed
reagents/materials/analysis tools, and helped perform the
experiments and acquired data. QC, BX, GJ and CAY wrote the paper.
CAY analyzed and interpreted the patient data regarding the
standard echocardiography and was a major contributor in writing
the manuscript.
Ethics approval and consent to
participate
This research was performed in accordance with The
Declaration of Helsinki and was approved by the Institutional
Review Board at the Zhongshan Ophthalmic Center, Sun Yat-sen
University of Medicine. Written informed consent was obtained from
each of the 6 adult subjects, and from the legal guardians of the
23 children, in accordance with The Declaration of Helsinki.
Patient consent for publication
All participants provided informed consent for the
publication of their data, including images and examination
results.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Dietz H: Marfan syndrome. In: Adam MP,
Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Stephens K and Amemiya
A (eds). GeneReviews. University of Washington, Seattle, Bookshelf
ID. NBK13352017.
|
|
2
|
Shi Y and Massagué J: Mechanisms of
TGF-beta signaling from cell membrane to the nucleus. Cell.
113:685–700. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Tandon A, Tovey JC, Sharma A, Gupta R and
Mohan RR: Role of transforming growth factor Beta in corneal
function, biology and pathology. Curr Mol Med. 10:565–578. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pervan CL, Lautz JD, Blitzer AL, Langert
KA and Stubbs EB Jr: Rho GTPase signaling promotes constitutive
expression and release of TGF-β2 by human trabecular meshwork
cells. Exp Eye Res. 146:95–102. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ochiai Y and Ochiai H: Higher
concentration of transforming growth factor-beta in aqueous humor
of glaucomatous eyes and diabetic eyes. Jpn J Ophthalmol.
46:249–253. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Habashi JP, Judge DP, Holm TM, Cohn RD,
Loeys BL, Cooper TK, Myers L, Klein EC, Liu G, Calvi C, et al:
Losartan, an AT1 antagonist, prevents aortic aneurysm in a mouse
model of Marfan syndrome. Science. 312:117–121. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Neptune ER, Frischmeyer PA, Arking DE,
Myers L, Bunton TE, Gayraud B, Ramirez F, Sakai LY and Dietz HC:
Dysregulation of TGF-beta activation contributes to pathogenesis in
Marfan syndrome. Nat Genet. 33:407–411. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Isogai Z, Ono RN, Ushiro S, Keene DR, Chen
Y, Mazzieri R, Charbonneau NL, Reinhardt DP, Rifkin DB and Sakai
LY: Latent transforming growth factor beta-binding protein 1
interacts with fibrillin and is a microfibril-associated protein. J
Biol Chem. 278:2750–2757. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hynes RO: The extracellular matrix: Not
just pretty fibrils. Science. 326:1216–1219. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Gomez D, Coyet A, Ollivier V, Jeunemaitre
X, Jondeau G, Michel JB and Vranckx R: Epigenetic control of
vascular smooth muscle cells in Marfan and non-Marfan thoracic
aortic aneurysms. Cardiovasc Res. 89:446–456. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Mu Y, Gudey SK and Landström M: Non-Smad
signaling pathways. Cell Tissue Res. 347:11–20. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kang JS, Liu C and Derynck R: New
regulatory mechanisms of TGF-beta receptor function. Trends Cell
Biol. 19:385–394. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Derynck R and Zhang YE: Smad-dependent and
Smad- independent pathways in TGF-beta family signalling. Nature.
425:577–584. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lee MK, Pardoux C, Hall MC, Lee PS,
Warburton D, Qing J, Smith SM and Derynck R: TGF-beta activates Erk
MAP kinase signalling through direct phosphorylation of ShcA. EMBO
J. 26:3957–3967. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Yamashita M, Fatyol K, Jin C, Wang X, Liu
Z and Zhang YE: TRAF6 mediates Smad-independent activation of JNK
and p38 by TGF-beta. Mol Cell. 31:918–924. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Holm TM, Habashi JP, Doyle JJ, Bedja D,
Chen Y, van Erp C, Lindsay ME, Kim D, Schoenhoff F, Cohn RD, et al:
Noncanonical TGFβ signaling contributes to aortic aneurysm
progression in Marfan syndrome mice. Science. 332:358–361. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Gomes LR, Terra LF, Wailemann RA, Labriola
L and Sogayar MC: TGF-β1 modulates the homeostasis between MMPs and
MMP inhibitors through p38 MAPK and ERK1/2 in highly invasive
breast cancer cells. BMC cancer. 12:262012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Chung AW, Au-Yeung K, Sandor GG, Judge DP,
Dietz HC and van-Breemen C: Loss of elastic fiber integrity and
reduction of vascular smooth muscle contraction resulting from the
upregulated activities of matrix metalloproteinase-2 and −9 in the
thoracic aortic aneurysm in Marfan syndrome. Circ Res. 101:512–522.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Wang Y, Ait-Oufella H, Herbin O, Bonnin P,
Ramkhelawon B, Taleb S, Huang J, Offenstadt G, Combadière C, Rénia
L, et al: TGF-beta activity protects against inflammatory aortic
aneurysm progression and complications in angiotensin II-infused
mice. J Clin Invest. 120:422–432. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Haneline M and Lewkovich GN: A narrative
review of pathophysiological mechanisms associated with cervical
artery dissection. J Can Chiropr Assoc. 51:146–157. 2007.PubMed/NCBI
|
|
21
|
Nataatmadja M, West J and West M:
Overexpression of transforming growth factor-beta is associated
with increased hyaluronan content and impairment of repair in
Marfan syndrome aortic aneurysm. Circulation 114 (1 Suppl).
I371–I377. 2006.
|
|
22
|
Chaudhry SS, Cain SA, Morgan A, Dallas SL,
Shuttleworth CA and Kielty CM: Fibrillin-1 regulates the
bioavailability of TGFbeta1. J Cell Biol. 176:355–367. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
ten-Dijke P and Arthur HM: Extracellular
control of TGFbeta signalling in vascular development and disease.
Nat Rev Mol Cell Biol. 8:857–869. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Nataatmadja M, West M, West J, Summers K,
Walker P, Nagata M and Watanabe T: Abnormal extracellular matrix
protein transport associated with increased apoptosis of vascular
smooth muscle cells in marfan syndrome and bicuspid aortic valve
thoracic aortic aneurysm. Circulation. 108 (Suppl 1):II329–II334.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Di-Girolamo N, Verma MJ, McCluskey PJ,
Lloyd A and Wakefield D: Increased matrix metalloproteinases in the
aqueous humor of patients and experimental animals with uveitis.
Curr Eye Res. 15:1060–1068. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Sachdev NH, Di-Girolamo N, Nolan TM,
McCluskey PJ, Wakefield D and Coroneo MT: Matrix metalloproteinases
and tissue inhibitors of matrix metalloproteinases in the human
lens: Implications for cortical cataract formation. Invest
Ophthalmol Vis Sci. 45:4075–4082. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Tamiya S, Wormstone IM, Marcantonio JM,
Gavrilovic J and Duncan G: Induction of matrix metalloproteinases 2
and 9 following stress to the lens. Exp Eye Res. 71:591–597. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Seomun Y, Kim J, Lee EH and Joo CK:
Overexpression of matrix metalloproteinase-2 mediates phenotypic
transformation of lens epithelial cells. Biochem J. 358:41–48.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Dwivedi DJ, Pino G, Banh A, Nathu Z,
Howchin D, Margetts P, Sivak JG and West-Mays JA: Matrix
metalloproteinase inhibitors suppress transforming growth
factor-beta-induced subcapsular cataract formation. Am J Pathol.
168:69–79. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
de-Iongh RU, Wederell E, Lovicu FJ and
McAvoy JW: Transforming growth factor-beta-induced
epithelial-mesenchymal transition in the lens: A model for cataract
formation. Cells Tissues Organs. 179:43–55. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Li J, Tang X and Chen X: Comparative
effects of TGF-β2/Smad2 and TGF-β2/Smad3 signaling pathways on
proliferation, migration, and extracellular matrix production in a
human lens cell line. Exp Eye Res. 92:173–179. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Sinpitaksakul SN, Pimkhaokham A,
Sanchavanakit N and Pavasant P: TGF-beta1 induced MMP-9 expression
in HNSCC cell lines via Smad/MLCK pathway. Biochem Biophys Res
Commun. 371:713–718. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Yao J, Yang W, Liu Y, Sun YX and Jiang Q:
Dexamethasone inhibits TGF-β2-induced migration of human lens
epithelial cells: implications for posterior capsule opacification
prevention. Mol Med Rep. 5:1509–1513. 2012.PubMed/NCBI
|
|
34
|
Alapure BV, Praveen MR, Gajjar D, Vasavada
AR, Rajkumar S and Johar K: Matrix metalloproteinase-9 activity in
human lens epithelial cells of cortical, posterior subcapsular, and
nuclear cataracts. J Cataract Refract Surg. 34:2063–2067. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Rösch S, Ramer R, Brune K and Hinz B:
R(+)-methanandamide and other cannabinoids induce the expression of
cyclooxygenase-2 and matrix metalloproteinases in human
nonpigmented ciliary epithelial cells. J Pharmacol Exp Ther.
316:1219–1228. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
McBrien NA, Lawlor P and Gentle A: Scleral
remodeling during the development of and recovery from axial myopia
in the tree shrew. Invest Ophthalmol Vis Sci. 41:3713–3719.
2000.PubMed/NCBI
|
|
37
|
Chu SC, Hu DN, Yang SF, Yang PY, Hsieh YS,
Huang SM, Yu G and McCormick SA: Uveal melanocytes produce matrix
metalloproteinases-2 and −9 in vitro. Pigment Cell Res. 17:636–642.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Weinreb RN and Lindsey JD:
Metalloproteinase gene transcription in human ciliary muscle cells
with latanoprost. Invest Ophthalmol Vis Sci. 43:716–722.
2002.PubMed/NCBI
|
|
39
|
Oh DJ, Martin JL, Williams AJ, Peck RE,
Pokorny C, Russell P, Birk DE and Rhee DJ: Analysis of expression
of matrix metalloproteinases and tissue inhibitors of
metalloproteinases in human ciliary body after latanoprost. Invest
Ophthalmol Vis Sci. 47:953–963. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Lan YQ, Zhang C, Xiao JH, Zhuo YH, Guo H,
Peng W and Ge J: Suppression of IkappaBalpha increases the
expression of matrix metalloproteinase-2 in human ciliary muscle
cells. Mol Vis. 15:1977–1987. 2009.PubMed/NCBI
|
|
41
|
Alexander JP, Samples JR, Van-Buskirk EM
and Acott TS: Expression of matrix metalloproteinases and inhibitor
by human trabecular meshwork. Invest Ophthalmol Vis Sci.
32:172–180. 1991.PubMed/NCBI
|
|
42
|
Pang IH, Hellberg PE, Fleenor DL, Jacobson
N and Clark AF: Expression of matrix metalloproteinases and their
inhibitors in human trabecular meshwork cells. Invest Ophthalmol
Vis Sci. 44:3485–3493. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Bandyopadhyay M and Rohrer B: Matrix
metalloproteinase activity creates pro-angiogenic environment in
primary human retinal pigment epithelial cells exposed to
complement. Invest Ophthalmol Vis Sci. 53:1953–1961. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Zeng A, Zeng S, Cheng Y and Xiao Q:
Modulation of matrix metalloproteinase and TIMP-1 expression by
TGF-beta1 in cultured human RPE cells. J Huazhong Univ Sci
Technolog Med Sci. 26:363–365. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Christian PG, Harkin DG, Rayner C and
Schmid KL: Comparative effects of posterior eye cup tissues from
myopic and hyperopic chick eyes on cultured scleral fibroblasts.
Exp Eye Res. 107:11–20. 2013. View Article : Google Scholar : PubMed/NCBI
|