Introduction
Coronary heart disease (CHD) with atherosclerosis
predominantly affects the inflammatory process, and remains to be a
major cause of morbidity and mortality worldwide (1). Several clinical studies are currently
underway in assessing various anti-inflammatory agents for the
treatment of atherosclerosis (2).
Recently, the CANTOS trial has demonstrated that anti-inflammatory
therapy targeting the interleukin (IL)-1β innate immunity pathway
reduced the risk of recurrent cardiovascular events in patients
with prior heart attack (3). In
addition, their previous findings indicated that high-sensitivity
C-reactive protein (hs-CRP) and IL-6 are associated with an
increased risk of cardiovascular events, independent of the
cholesterol level (4). Although
the specific mechanisms are unclear, several studies have
underlined the central role of inflammasomes, which act as integral
parts of the innate immune system during the process of
atherosclerosis (5–7).
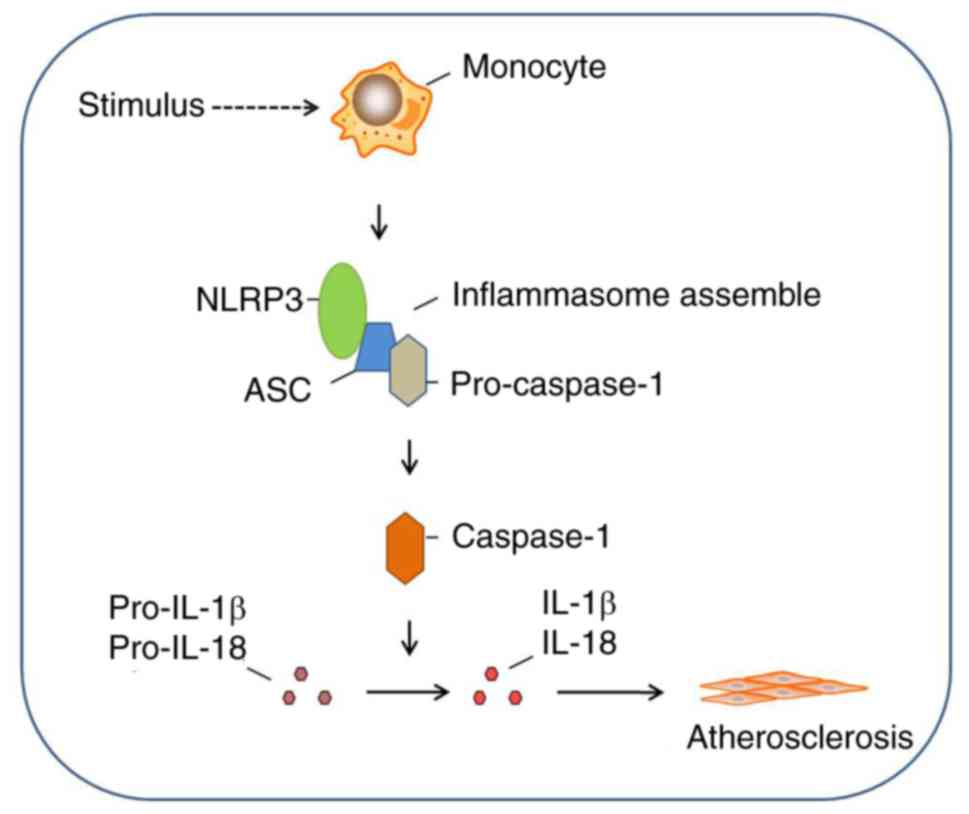
Nucleotide-binding oligomerization domain, leucine
rich repeat, and pyrin domain-containing protein 3 (NLRP3),
apoptosis-associated speck-like protein containing a CARD (ASC) and
caspase-1 constitute the main components of inflammasome-NLRP3
inflammasome (8). The NLRP3
inflammasome on activation forms a macromolecular protein complex
that regulates the activation of caspase-1 and production and
maturation of pro-inflammatory cytokines such as IL-1β and IL-18
(9). It can be activated by
various signals, wherein the cholesterol crystals act as a major
trigger and as a sustaining factor for atherogenic inflammation
through NLRP3 inflammasome and its induction of IL-1β (10).
Clinically, statins [HMG-CoA
(3-hydroxy-3-methylglutaryl-coenzyme A) reductase inhibitors] have
long been used for the treatment of CHD (11,12).
Statins can effectively stabilize or reverse atherosclerotic plaque
formation, improving prognosis, and reducing mortality and
morbidity by lowering the blood lipid levels and inhibiting the
inflammatory response (13).
Rosuvastatin is a relatively new drug that belongs to HMG-CoA
inhibitors. It has a safety and tolerability profile similar to or
better than that of commonly used doses of other statins (14). Rosuvastatin is associated with a
decrease in the levels of serum hs-CRP, which occurs independently
with the reduction of low-density lipoprotein cholesterol (LDL-C)
(15). Therefore, it is generally
used in clinics to prevent and treat CHD (16). However, research regarding the
correlation between NLRP3 inflammasome and rosuvastatin is hardly
available.
Thus, the present study aimed to determine whether
NLRP3 inflammasome was expressed in peripheral blood monocytes
(PBMCs) and correlated with IL-1β and IL-18 secretion in stable
angina pectoris (SAP) and acute myocardial infarction (AMI)
patients. In addition, the effect of rosuvastatin on the NLRP3
inflammasome signaling pathway was investigated in CHD in
vitro by utilizing a cell culture model to provide new insights
into the inflammatory pathogenesis and management of CHD.
Materials and methods
Study population
A total of 40 patients with stable SAP (n=20) and
AMI (n=20) admitted to our hospital for coronary angiography and
emergency percutaneous coronary intervention (PCI) from May 2017 to
April 2018 were enrolled. None of the participants were treated
with statins before. SAP was defined according to the
ACCF/AHA/ACP/AATS/PCNA/SCAI/STS Guidelines (17). AMI was diagnosed based on the
ESC/ACCF/AHA/WHF Third Universal Definition of myocardial
infarction (18). Patients with
clinical signs of acute infection, severe renal failure (serum
creatine levels >3 mg/dl) or rheumatoid disease, or suspected of
having a malignant or primary wasting disorder were excluded from
the present study. A total of 20 subjects with paroxysmal
supraventricular tachycardia (PSVT) admitted to our hospital for
radiofrequency ablation (RFCA) and exhibiting no evidence of CHD
upon history or physical examination were defined as the control
group (non-CHD group). Participants included in our study were aged
between 41 and 84 years, and utilization of samples was approved by
the Ethics Committee of The First Affiliated Hospital of Bengbu
Medical College (Bengbu, China) and written informed consent was
obtained from all subjects.
Blood samples
Peripheral blood samples were collected from all
patients in the morning after an overnight fast to obtain baseline
data. Plasma was separated by centrifugation at 2,500 × g for 15
min and was stored at −80°C until use.
Cell preparation
Peripheral blood mononuclear cells were isolated
from peripheral blood samples by Ficoll-Paque density gradient
centrifugation using lymphocyte separation medium (Sigma-Aldrich;
Merck KGaA). Isolated mononuclear cells were washed and centrifuged
twice with PBS lotion containing 3% fetal bovine serum (FBS) and 10
mM EDTA for 15 min at 400 × g at room temperature. Subsequently,
the peripheral blood mononuclear cells were resuspended at a final
concentration of 1.0×108 cells/ml and were isolated
using EasySep™ CD14+ antibody positive selection kit
(Stemcell Technologies, Inc.). The obtained PBMCs were washed with
PBS lotion containing 3% FBS and 10 mM EDTA three times. A final
concentration of 5.0×106 cells/ml of PBMCs were
incubated with 2.5 µl PE anti-human CD14 antibody (1:1,000; cat.
no. 12-0149-41; eBioscience; Thermo Fisher Scientific, Ltd.) at 4°C
for 30 min protected from light. A monoclonal antibody against
mouse IgG (1:1,000; cat. no. 10400C; Invitrogen; Thermo Fisher
Scientific, Ltd.) was used as the homologous control under the same
conditions. After washing thrice with PBS, the cells were
resuspended and the positive rate of CD14 was calculated by flow
cytometry.
Cell experiments
PBMCs from each group were cultured and proliferated
with RPMI-1640 culture medium containing 10% FBS (both from Thermo
Fisher Scientific, Inc.) and 50 U/ml rIL-2 (Sigma-Aldrich; Merck
KGaA) for 24 h in vitro. Then, the PBMCs were harvested and
equally divided into three portions. One portion was defined as the
untreated group (0 h) and collected directly for RNA and protein
extraction. The other two portions were sequentially cultured with
rosuvastatin for another 12 and 24 h, respectively, and were
defined as the 12 and 24-h groups. Rosuvastatin (Sigma-Aldrich;
Merck KGaA) was dissolved in DMSO at a stock solution of 20 mM and
stored in aliquots at −20°C as previously described (19).
RNA isolation and real-time reverse
transcriptase-polymerase chain reaction (RT-PCR)
Total RNA was extracted using TRIzol reagent
(Invitrogen; Thermo Fisher Scientific, Inc.) according to the
manufacturer's instructions. M-MLV reverse transcriptase (Promega
Corporation) was used to convert RNA into cDNA at 42°C for 60 min
following standard procedure. For real-time reverse
transcriptase-polymerase chain reaction (RT-PCR) quantification, 2
µl of cDNA reaction was amplified in a 20-µl standard RT-PCR
reaction. The PCR parameters were as follows: Denaturation at 94°C
for 5 min, followed by 40 amplification cycles at 94°C for 30 sec,
56°C for 60 sec, and 72°C for 40 sec, with the final cycle extended
to 10 min at 72°C, and termination at 4°C. The detection of β-actin
transcripts provided an internal control in RT-PCR, standardizing
the quantity of input cDNA. The quantitative RT-PCR amplification
products and the expression ratios of mRNA were determined using
the 2−ΔΔCq method (20)
for relative quantification. The primers used in the study are
listed in Table I.
 | Table I.Primers used in the present
study. |
Table I.
Primers used in the present
study.
| Gene | Sequence | Product size |
|---|
| NLRP3 |
|
Upstream |
F-5′-AAGCACCTGTTGTGCAATCTGAAG-3′ | 103 bp |
|
Downstream |
R-5′-GGGAATGGCTGGTGCTCAATAC-3′ |
|
| ASC |
|
Upstream |
F-5′-TGACGGATGAGCAGTACCAG-3′ | 151 bp |
|
Downstream |
R-5′-TCCTCCACCAGGTAGGACTG-3′ |
|
| Caspase-1 |
|
Upstream |
F-5′-GCCTGTTCCTGTGATGTGGA-3′ | 175 bp |
|
Downstream |
R-5′-TTCACTTCCTGCCCACAGAC-3′ |
|
| β-actin |
|
Upstream |
F-5′-CCTTCCTGGGCATGGAGTCCTG-3′ | 202 bp |
|
Downstream |
R-5′-GGAGCAATGATCTTGATCTTC-3′ |
|
Western blotting
Total proteins were extracted from PBMCs using RIPA
Lysis and Extraction Buffer (Thermo Fisher Scientific, Inc.). The
protein concentration was measured by BCA protein assay kit (Thermo
Fisher Scientific, Inc.). Equal amounts of proteins (20 µg per
lane) were loaded onto the gel and separated by SDS-polyacrylamide
gels with 10% (w/v) acrylamide, followed by electrophoresis and
blotting onto PVDF membranes (EMD Millipore). The membranes were
blocked in 5% nonfat milk for 30 min at room temperature and
co-incubated overnight with anti-NLRP3 (1:1,000; cat. no. 13158S;
Cell Signaling Technology, Inc.), anti-ASC (1:1,000; cat. no.
sc-514414; Santa Cruz Biotechnology, Inc.), anti-caspase-1
(1:1,000; cat. no. 3866S; Cell Signaling Technology, Inc.) and
anti-β-actin (cat. no. 8457S; Cell Signaling Technology, Inc.;
1:1,000) on a shaker at 4°C. After rinsing, the membranes were
co-incubated for 2 h with an alkaline phosphatase-labeled goat anti
rabbit secondary antibody (1:2,000; cat. no. 7054S; Cell Signaling
Technology, Inc.) on a shaker at room temperature. Following
additional rinsing, the membranes were treated with 5 ml BCIP/NBT
solution (Invitrogen; Thermo Fisher Scientific, Inc.) according to
the manufacturer's instructions. The Quantity One 1-D analysis
software version 4.6.3 (Bio-Rad Laboratories, Inc.) was used to
analyze the protein ladders. Protein expression levels were
normalized to those of internal controls (β-actin).
Enzyme-linked immunosorbent assay
(ELISA)
ELISA was used to determine the levels of IL-1β and
IL-18 according to the manufacturer's instructions (Cell Signaling
Technology, Inc.). Triplicated wells were set as samples and
standard references. The final absorbance values of proteins were
read by a microplate reader at 450 nm, while the means were used to
calculate IL-1β and IL-18 contents of corresponding samples based
on the established standard curves.
Statistical analysis
The numerical data were presented as the means ±
standard deviation (SD). Statistically significant differences
among the groups were evaluated by Student's t-test or one-way
analysis of variance (ANOVA) followed by the Bonferroni test, using
SPSS 21.0 software (IBM Corp.). Correlation analysis was performed
using Pearson's correlation. P-values <0.05 were considered to
be statistically significant.
Results
Baseline characteristics
Sixty participants were enrolled in this study and
were divided into three groups [SAP (n=20), AMI (n=20) and non-CHD
controls (n=20)]. No significant differences in age, sex, BMI,
smoking status, mononuclear count, lipoprotein A (LPA) level, urea
level, creatinine level and uric acid level were observed among the
three groups (P>0.05). However, total cholesterol (TC) level,
triglycerides (TG) level, high-density lipoprotein cholesterol
(HDL-C) level, LDL-C level, apolipoprotein B (Apo B) level and
alanine transaminase (ALT) level were significantly increased in
the SAP group compared to those in the control group (P<0.05),
while white blood cell (WBC) count, HDL-C, Apo A level, ALT level,
aspartate aminotransferase (AST) level and hs-CRP level were
significantly increased in the AMI group compared to those in the
control group (P<0.05). When compared to the SAP group, the WBC
count and levels of LDL-C, ALT, AST and hs-CRP in the AMI group
were revealed to be significant (P<0.05). The baseline
characteristics of the study population are presented in Table II.
 | Table II.Baseline laboratory indices of the
study group. |
Table II.
Baseline laboratory indices of the
study group.
|
| Control (n=20) | SAP (n=20) | AMI (n=20) |
|---|
| Age | 59.10±10.33 | 64.05±11.52 | 64.05±8.72 |
| BMI
(kg/m2) | 24.99±3.42 | 25.57±3.70 | 25.7310±3.13 |
| Male | 6 | 11 | 12 |
| Female | 14 | 9 | 8 |
| Smoking
history | 4/20 | 8/20 | 6/20 |
| CHD family
history | – | 5/20 | 6/20 |
| Hypertension | 7/20 | 12/20 | 10/20 |
| WBC
(×109/l) | 5.88±1.33 | 6.62±1.85 |
9.59±4.44a,b |
| Mononuclear
(×109/l) | 0.71±1.41 | 0.44±0.13 | 0.65±0.33 |
| TC (mmol/l) | 4.54±0.96 |
3.73±1.09a | 4.12±1.09 |
| TG (mmol/l) | 1.22±0.46 |
1.83±1.01a | 1.51±1.11 |
| HDL (mmol/l) | 1.21±0.29 |
0.97±0.25a |
0.97±0.25a,b |
| LDL (mmol/l) | 2.50±0.74 |
1.83±0.78a |
2.50±0.92b |
| Apo A (g/l) | 1.33±0.35 | 1.18±0.22 |
1.07±0.22a |
| Apo B (g/l) | 0.82±0.24 |
0.66±0.27a | 0.80±0.25 |
| LPA (mg/l) | 205.95±228.86 | 227.70±183.95 | 228.10±232.37 |
| ALT (U/l) | 17.35±8.80 |
27.85±16.99a |
42.25±16.92a,b |
| AST (U/l) | 21.50±4.48 | 27.20±11.44 |
146.40±132.90a,b |
| Urea (mmol/l) | 5.66±1.18 | 5.62±1.34 | 5.45±1.70 |
| Creatinine
(µmol/l) | 63.20±11.31 | 72.25±13.49 | 69.85±24.20 |
| hs-CRP (mg/l) | 1.24±1.37 | 3.34±5.74 |
24.27±31.08a,b |
| Uric acid
(umo1/l) | 296.10±88.46 | 299.85±70.12 | 297.00±86.183 |
Expression of NLRP3 inflammasome in
PBMCs
PBMCs isolated from SAP, AMI and control
participants were purified with CD14-antibody-conjugated beads, and
then were identified using fluorescence-activated cell sorting
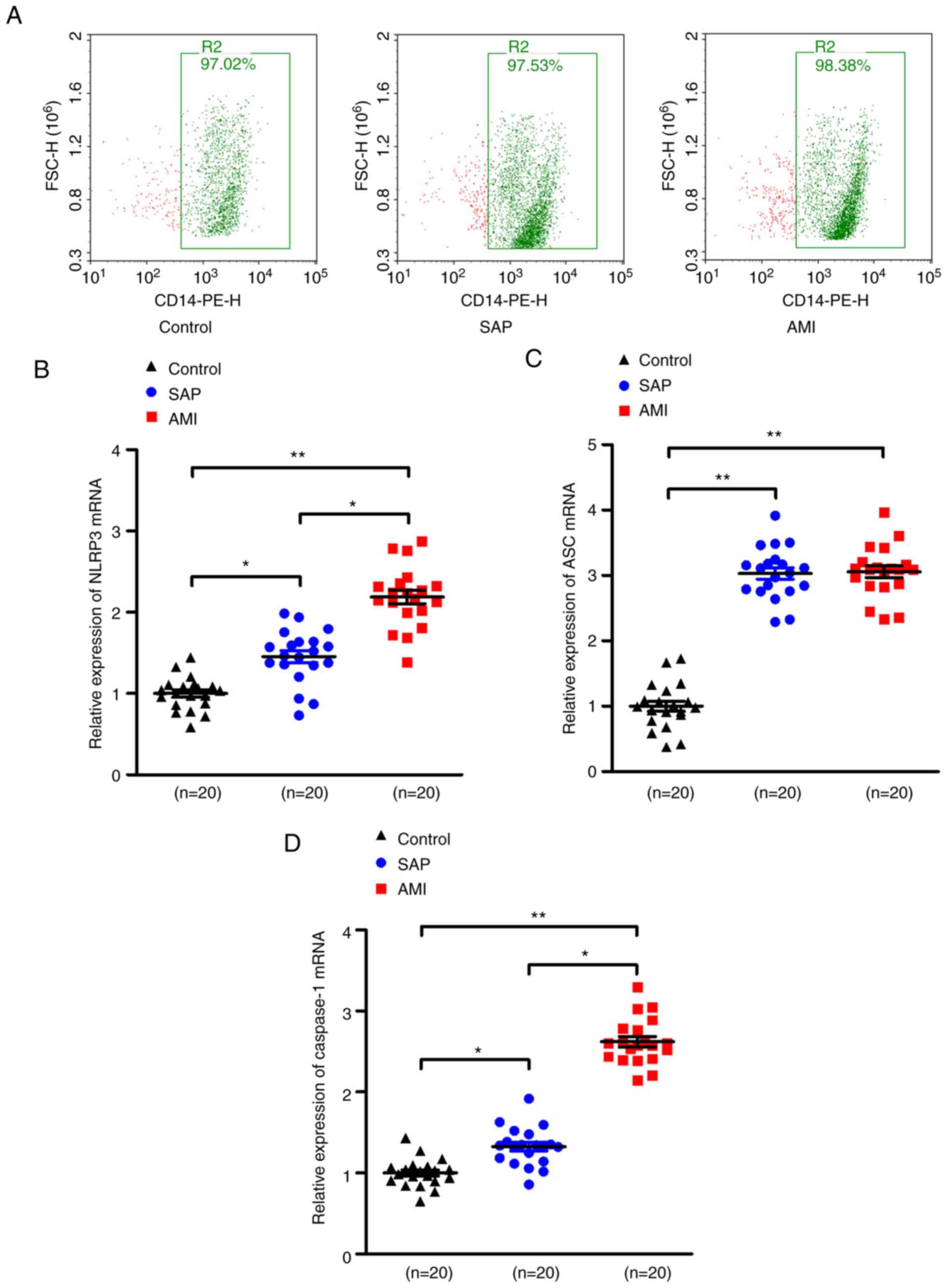
(FACS) as revealed in Fig. 1A.
RT-PCR results revealed that the mRNA expression of NLRP3, ASC and
caspase-1 were significantly increased in SAP and AMI groups
compared to the control group (P<0.05). The significant
upregulation of the mRNA levels of the three indicators in the AMI
group was concurrently revealed when compared with the SAP group
(P<0.05, Fig. 1B-D). Similar
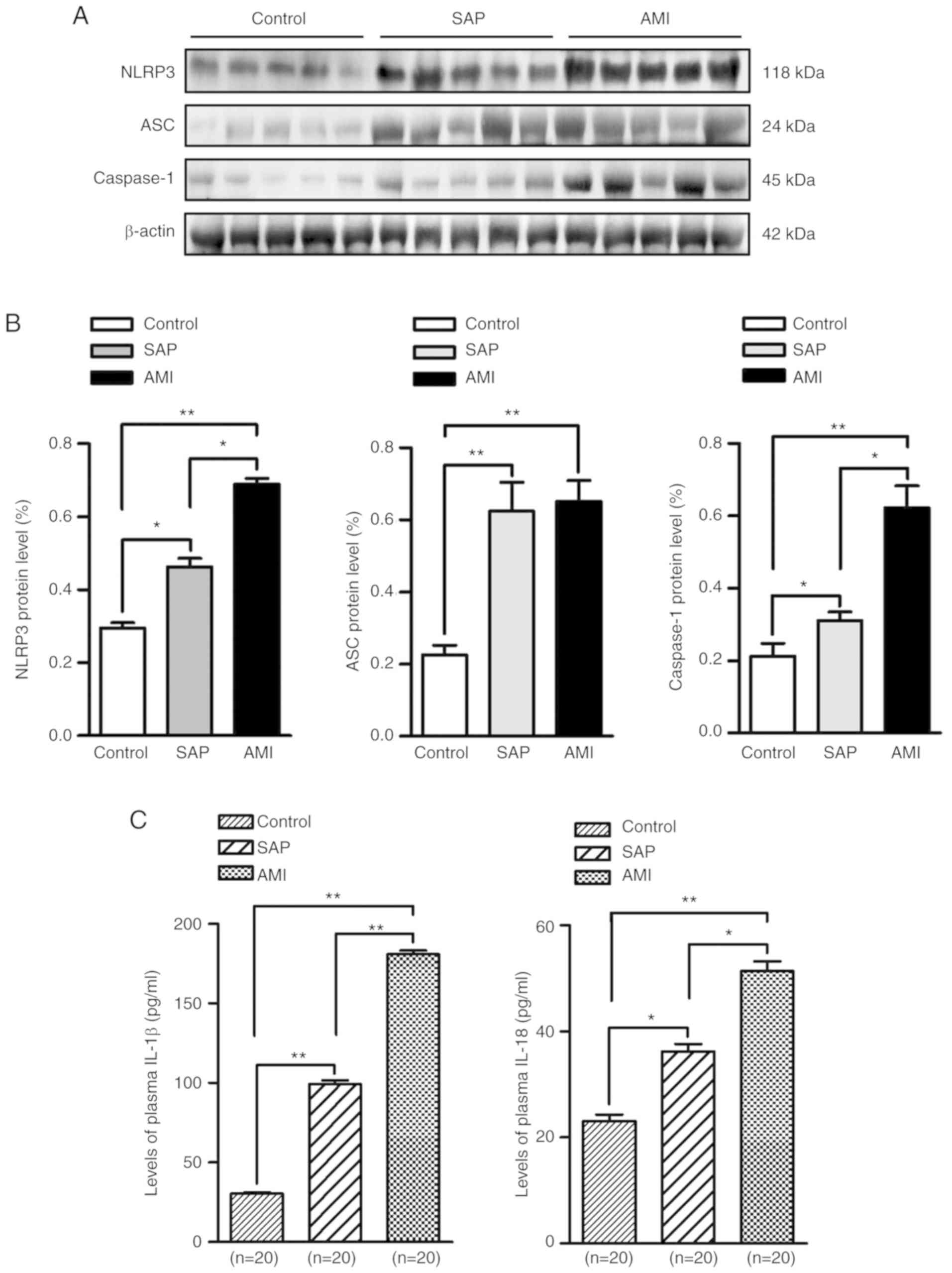
results were observed in the protein expression pattern of NLRP3
inflammasome, revealing a significant increase in the SAP and AMI
group compared to the control group, and the AMI group revealed an
increase compared with the SAP group (P<0.05, Fig. 2A and B).
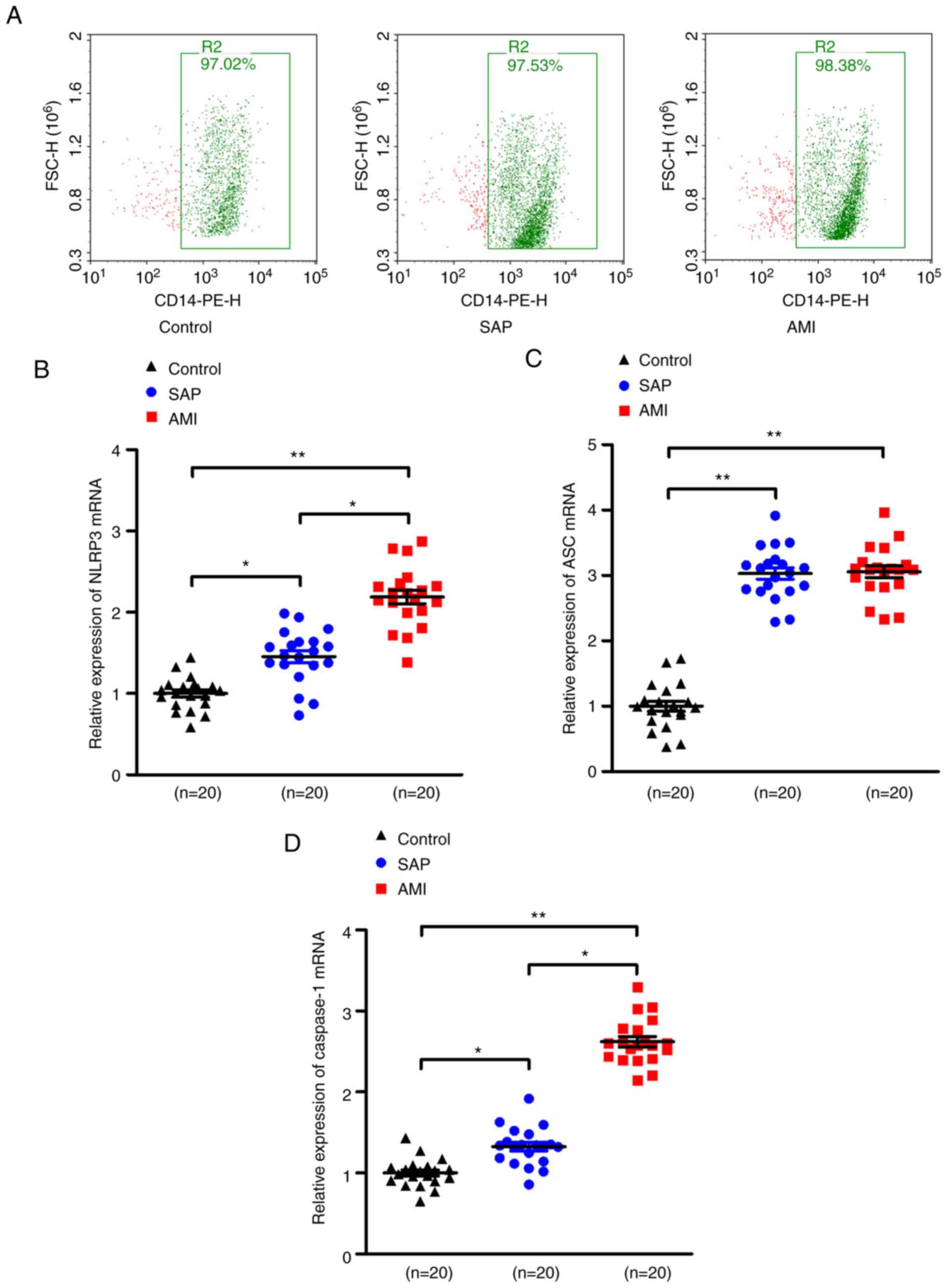 | Figure 1.Upregulation of NLRP3 inflammasome
mRNA levels in PBMCs in patients with SAP and AMI, compared with
non-CHD controls. (A) PBMCs were isolated from peripheral blood and
the positive rate of CD14 was calculated to be ≥95% of PBMCs by
flow cytometry. RT-PCR assays were performed to quantify the mRNA
levels of (B) NLRP3, (C) ASC and (D) caspase-1 in PBMCs of each
group. *P<0.05; **P<0.01. NLRP3, nucleotide-binding
oligomerization domain, leucine rich repeat, and pyrin
domain-containing protein 3; PBMCs, peripheral blood monocytes;
SAP, stable angina pectoris; AMI, acute myocardial infarction; CHD,
coronary heart disease; ASC, apoptosis-associated speck-like
protein containing a CARD. |
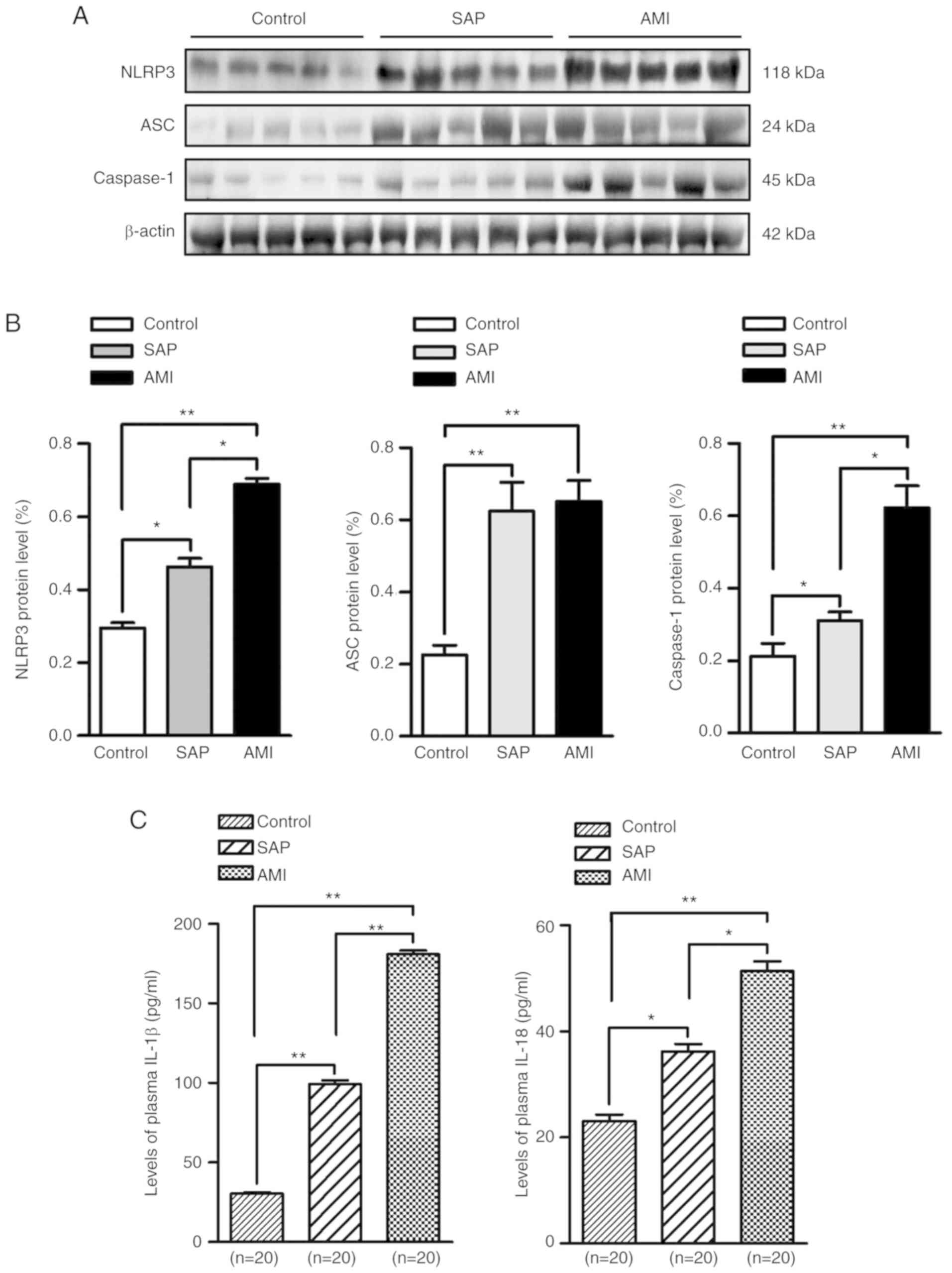 | Figure 2.Increase in protein expression levels
of NLRP3 inflammasome and secretion of its downstream interleukins
in PBMCs of patients with SAP and AMI, compared with non-CHD
controls. (A) Western blotting was used to detect the protein
expression of NLRP3, ASC and caspase-1 in PBMCs of each group. (B)
Quantitative results are illustrated for the three indicators using
western blot analysis. (C) Plasma levels of IL-1β and IL-18 from
each group were measured by ELISA. *P<0.05; **P<0.01. NLRP3,
nucleotide-binding oligomerization domain, leucine rich repeat, and
pyrin domain-containing protein 3; PBMCs, peripheral blood
monocytes; SAP, stable angina pectoris; AMI, acute myocardial
infarction; CHD, coronary heart disease; ASC, apoptosis-associated
speck-like protein containing a CARD; ELISA, enzyme-linked
immunosorbent assay. |
Measurement of IL-1β and IL-18 in
plasma
As revealed in Fig.
2C, there was a significant increase in the secretion of IL-1β
and IL-18 in the SAP and AMI groups compared to the controls
(P<0.05). In addition, a significant upregulation in the
concentrations of the two cytokines was observed in the AMI group,
compared with the SAP group (P<0.05).
Correlations of IL-1β and IL-18 levels
with inflammatory markers
The correlations of cytokines IL-1β and IL-18 with
plasma levels of the indicated inflammatory markers in a total of
60 subjects were analyzed. The results revealed that both WBC count
and hs-CRP level were positively correlated with IL-1β and IL-18
concentrations, WBC count (r=0.484; P<0.05) and hs-CRP
level (r=0.442; P<0.05) with IL-1β, WBC count
(r=0.365; P<0.05) and hs-CRP level (r=0.293;
P=0.023) with IL-18. However, there were no significant
correlations between mononuclear count, Apo A level, Apo B level,
or LPA level with IL-1β and IL-18 concentrations (Table III).
 | Table III.Correlation of inflammatory markers
with IL-1β and IL-18. |
Table III.
Correlation of inflammatory markers
with IL-1β and IL-18.
|
| IL-1β | IL-18 |
|---|
|
|
|
|
|---|
| Variables | r | P-value | r | P-value |
|---|
| WBC | 0.484 |
<0.001a | 0.365 | 0.005a |
| Mononuclear | 0.025 | 0.849 | 0.020 | 0.878 |
| hs-CRP | 0.442 |
<0.001a | 0.293 | 0.023a |
| Apo A | −0.350 | 0.006a | −0.021 | 0.063 |
| Apo B | −0.039 | 0.765 | −0.053 | 0.686 |
| LPA | 0.048 | 0.717 | 0.059 | 0.656 |
Effect of rosuvastatin on NLRP3
inflammasome and downstream cytokines in PMBCs in vitro
PBMCs isolated from each group were cultured and
proliferated as described in Materials and methods. Western
blotting and real-time RT-PCR were performed to detect the
expression of NLRP3, ASC, and caspase-1 in PBMCs. ELISA was
performed to assess IL-1β and IL-18 levels in the supernatants. The
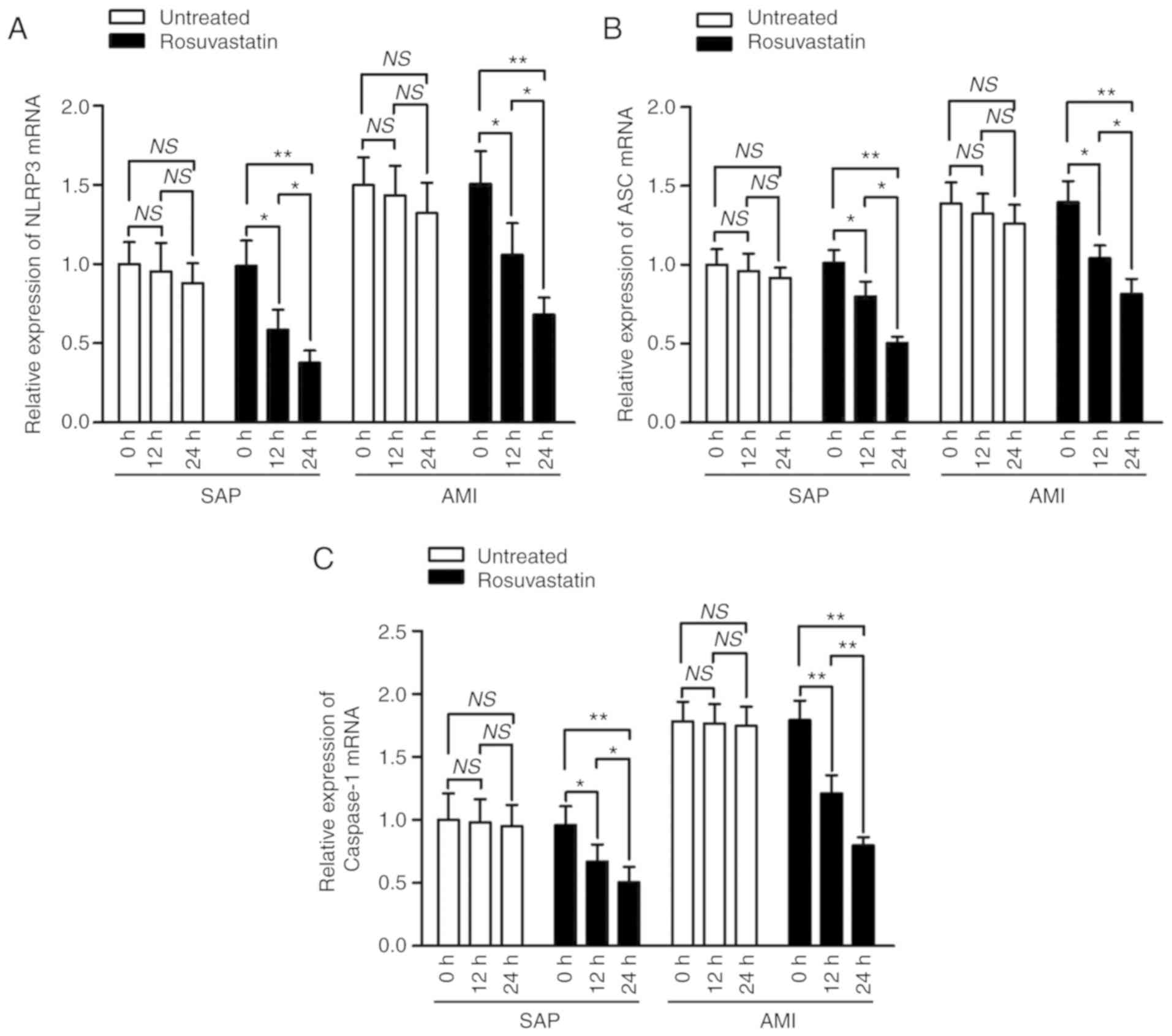
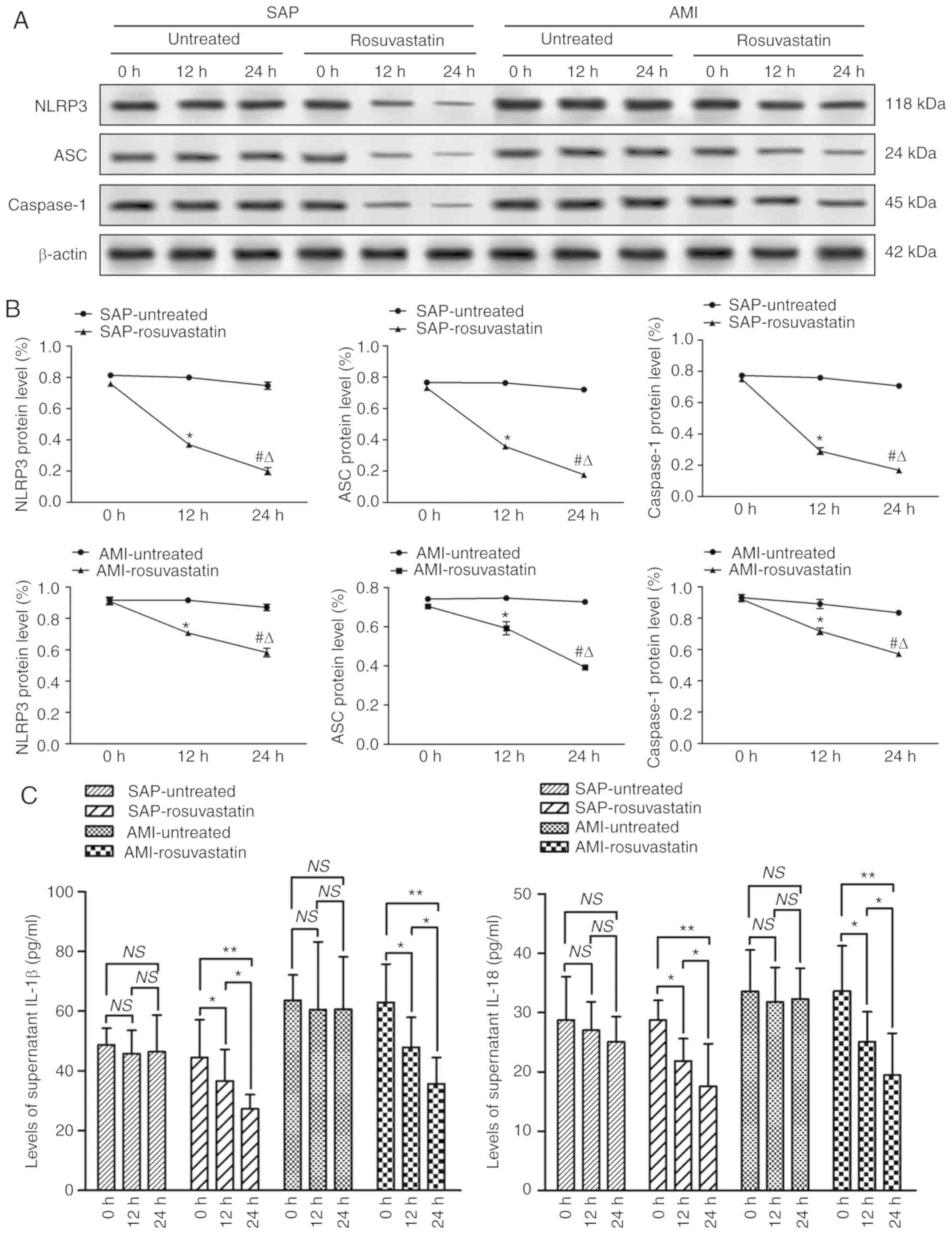
results revealed that the mRNA and protein expression of NLRP3, ASC
and caspase-1 were downregulated in the 12 and 24-h groups treated
with rosuvastatin compared to the untreated groups of PBMCs from
either SAP or AMI patients in vitro (P<0.05), and more
significant decrease was observed in the 24-h group compared to the
12-h group (P<0.05) (Figs. 3
and 4A and B). Similar results
were also observed for the expression of IL-1β and IL-18 in the
supernatants of untreated groups, and the rosuvastatin group
treated for 12 and 24 h (Fig.
4C).
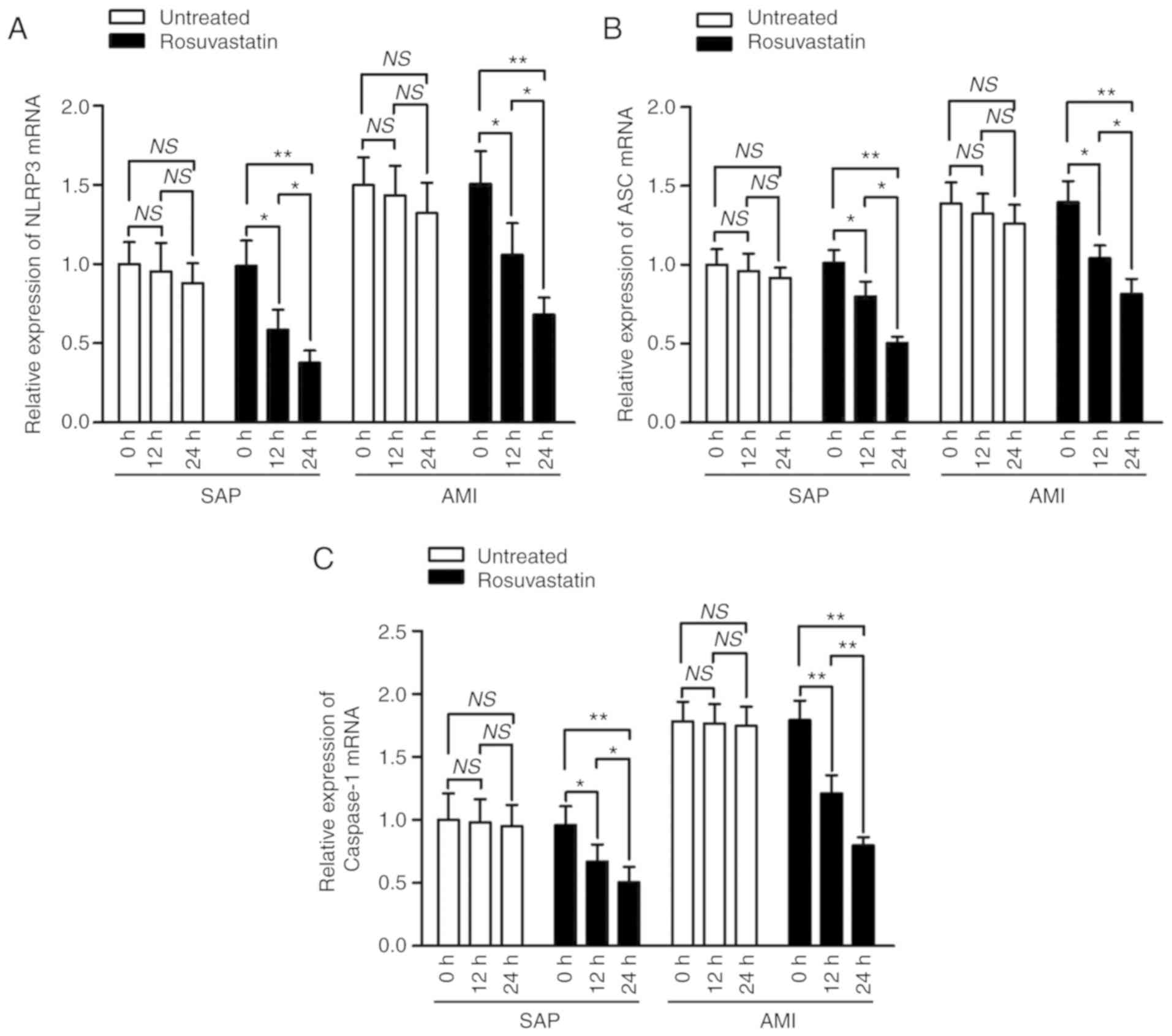 | Figure 3.Effect of rosuvastatin on NLRP3
inflammasome mRNA levels in PBMCs in vitro. PBMCs were
isolated from the peripheral blood of patients with non-CHD, SAP
and AMI, respectively, followed by proliferation and treatment with
rosuvastatin at a concentration of 20 µM for the indicated
time-points. RT-PCR assay was performed to investigate the
influence of rosuvastatin on the mRNA levels of (A) NLRP3, (B) ASC
and (C) caspase-1 in PBMCs of each group. *P<0.05; **P<0.01.
NLRP3, nucleotide-binding oligomerization domain, leucine rich
repeat, and pyrin domain-containing protein 3; PBMCs, peripheral
blood monocytes; CHD, coronary heart disease; SAP, stable angina
pectoris; AMI, acute myocardial infarction; ASC,
apoptosis-associated speck-like protein containing a CARD; NS, not
significant. |
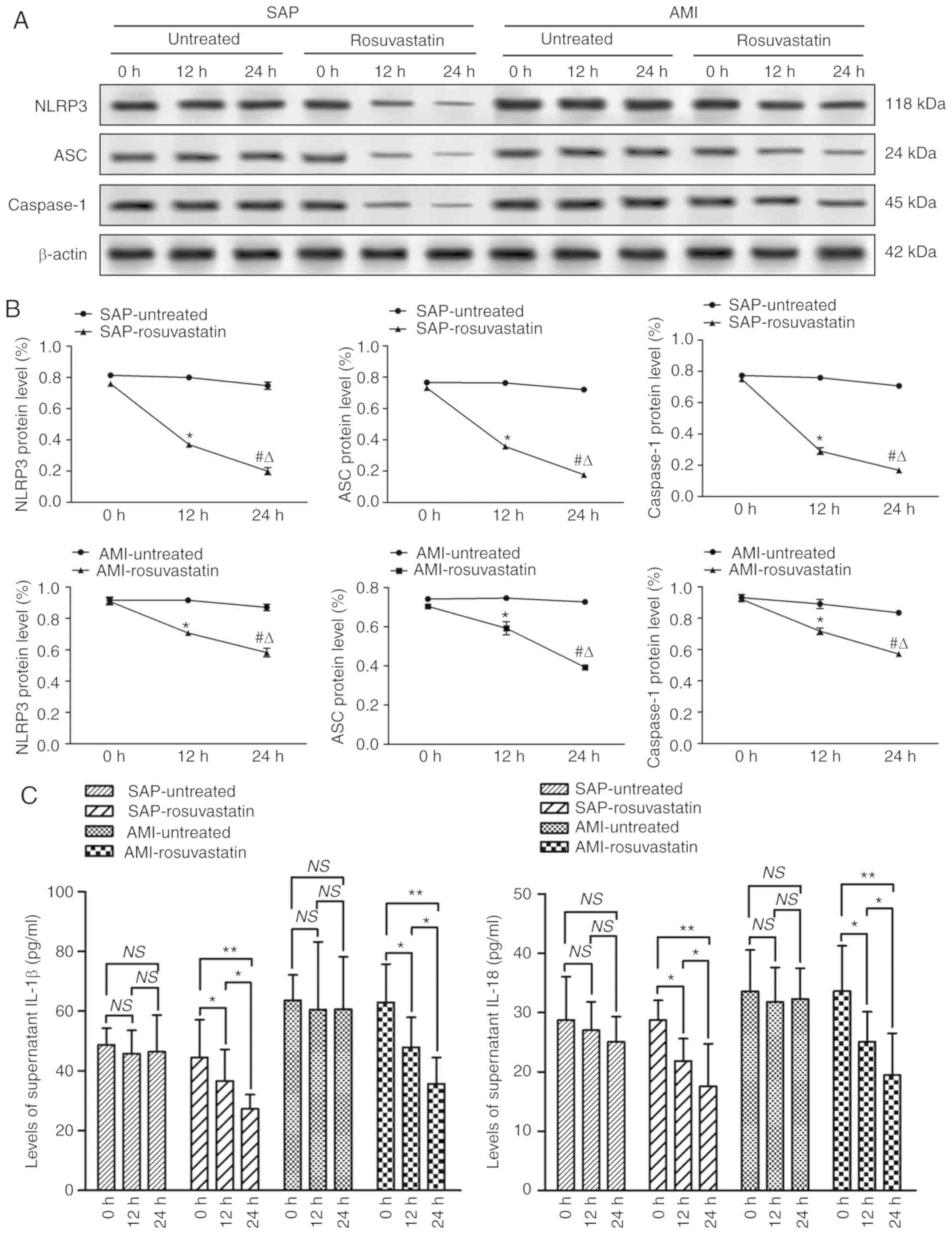 | Figure 4.Effect of rosuvastatin on protein
expression levels of NLRP3 inflammasome in PBMCs and secretion of
its downstream cytokines in supernatants in vitro. PBMCs
were isolated from the peripheral blood of patients with non-CHD,
SAP and AMI, respectively, followed by proliferation and treatment
with rosuvastatin at a concentration of 20 µM for the indicated
time-points. (A) Western blotting was conducted to analyze the
influence of rosuvastatin on the protein levels of NLRP3, ASC and
caspase-1 in PBMCs of each group. (B) Quantitative results for
modulating the protein expression of the aforementioned three
indicators by rosuvastatin are illustrated. (C) Modulation of IL-1β
and IL-18 secretion in the supernatants by rosuvastatin of each
group was measured by ELISA. *P<0.05, **P<0.01 and
#P<0.05 (compared to the 0-h group);
ΔP<0.05 (compared to the 12-h group). NLRP3,
nucleotide-binding oligomerization domain, leucine rich repeat, and
pyrin domain-containing protein 3; PBMCs, peripheral blood
monocytes; CHD, coronary heart disease; SAP, stable angina
pectoris; AMI, acute myocardial infarction; ASC,
apoptosis-associated speck-like protein containing a CARD; NS, not
significant. |
Discussion
Cardiovascular disease is still considered to be the
leading cause of deaths and illnesses worldwide (1). Atherosclerosis is widely perceived as
the pathological basis of CHD including SAP and AMI, wherein the
cholesterol deposition incites a progressive macrophage-dominated
inflammatory response. Until recently, the molecular basis of these
inflammatory responses in atherosclerotic lesions was not clearly
understood. In the present study, PBMCs were isolated and the
expression levels of NLRP3 inflammasome and its downstream
cytokines from SAP and AMI patients were identified, and the effect
of rosuvastatin during this process was investigated. The results
revealed that NLRP3, ASC and caspase-1 were highly expressed in
PBMCs along with its downstream cytokines IL-1β and IL-18 in SAP
and AMI patients when compared to non-CHD controls. Rosuvastatin at
a concentration of 20 µM for 12 and 24 h led to a significant
decrease in the expression of NLRP3 inflammasome and its downstream
mediators in vitro in a time-dependent manner.
Atherosclerosis is an inflammatory condition that
involves both acute and chronic components. Recent insights
indicated that innate immune cells play a vital role in the
pathogenesis of atherosclerosis (21). Atherosclerotic plaque development
in the arterial wall is characterized by infiltration of monocytes
(22). Circulating monocytes
initially adhere to the activated endothelium, then infiltrate into
the vessel wall via endothelial cell junction, form lesional
macrophages, and then participate decisively in the development and
exacerbation of atherosclerosis. The inflammatory cytokines are
secreted to modify the endothelial function, proliferation of
vascular smooth muscle cell (VSMCs), degradation of collagen, and
thrombosis (23). The
inflammasomes are innate immune system receptors/sensors that are
formed in response to infectious microbes and molecules derived
from host proteins (24). It is a
cytoplasmic macromolecular protein complex that contains multiple
proteins, which is formed in response to danger-associated
molecular patterns (DAMPs) or pathogen-associated molecular
patterns (PAMPs), and serves as a molecular platform for activation
of cysteine protease caspase-1 (25). NLRP3 inflammasome is one of the
most studied inflammasomes, and involved in the process of sterile
inflammation (26).
It is well known that an array of exogenous and
endogenous stimuli can activate NLRP3 inflammasome, and the
underlying precise mechanism remains unclear. However, several
common upstream pathways have been identified including potassium
(K+) efflux (27), the
generation of mitochondrial reactive oxygen species (ROS) (28), and cathepsin release as a result of
phagolysosomal membrane destabilization (29). NLRP3 activation forms a complex,
which has been revealed to regulate the activation of caspase-1 and
promote the production of inflammatory cytokines, such as IL-1β and
IL-18 (30). Clinical studies have
revealed that the increase in IL-1β and IL-18 levels is related to
clinical severity in patients with CHD (31,32).
In recent years, NLRP3 inflammasome has been considered as a novel
player in myocardial infarction (33). Animal experiments were performed to
identify whether inflammasome activation of cardiac fibroblasts
remains essential for myocardial ischemia/reperfusion injury
(34). Consistent with this, a
study revealed that inhibition of NLRP3 inflammasome limited the
inflammatory injury following myocardial ischemia-reperfusion in a
mouse model (35). Therefore,
NLRP3 inflammasome and associated IL-1β release are considered as
potential biomarkers of conventional cardiovascular risk (36). CRP, as an important inflammatory
mediator, is able to directly participate in the pathogenesis of
atherosclerosis by activating endothelial cells and promoting the
inflammatory component of atherosclerosis (37,38).
Moreover, the circulating level of hs-CRP was also revealed to be
strongly associated with the clinical setting of unstable angina
pectoris (39,40). In the present study, peripheral
blood was collected from patients within 12 h after an attack of
AMI, and emergency PCI was applied to testify and treat the target
lesion. It was revealed that WBC count, levels of hs-CRP, NLRP3
inflammasome and its downstream cytokines IL-1β and IL-18 were all
significantly increased in patients with AMI when compared to
non-CHD controls. Expression of key factors of the NLRP3
inflammasome signaling pathway were also observed to be enhanced in
SAP patients.
Furthermore, it was determined that IL-1β and IL-18
content revealed a correlation with WBC count and the level of
hs-CRP. These findings revealed an inflammatory response in
coronary artery occlusion, especially in the process of AMI
characterized by a greater and a more marked activation of
inflammation. The results that the increase in either hs-CRP level
or WBC count in SAP patients was not significant enough when
compared to non-CHD controls also support the notion. In light of
this evidence, it is proposed that the stimulated PBMCs orchestrate
the activation of NLRP3 inflammasome. This was due to the
upregulation of the expression of NLRP3, ASC, caspase-1, and their
downstream mediators, leading to atherosclerotic progression
(Fig. 5).
The elevated blood cholesterol levels, or more
precisely the LDL-C levels, are generally recognized as a major
risk factor and are causally linked to the pathogenesis of
atherosclerosis (41).
Rosuvastatin has been extensively used for the treatment of
hyperlipidemia and CHD, and is mainly referred due to its benefit
to stabilization and regression of atherosclerotic plaques, which
thus avoids or improves cardiovascular events. Recently,
rosuvastatin was also reported to have the ability to decrease the
number of inflammatory cells in atherosclerotic plaques and possess
other anti-inflammatory properties (42). The potential relationship between
rosuvastatin and NLRP3 inflammasome in coronary artery disease
(CAD) has been documented by previous studies (8,43),
however, SAP and AMI represent different stages of development of
coronary atherosclerosis with different pathophysiological
processes, and their underlying molecular mechanisms are far from
complete.
In the present study, CD14+ monocytes
were cultured and treated with rosuvastatin at different
time-points in vitro, and it was revealed that these
indicators were significantly downregulated in a time-dependent
manner in patients with SAP and AMI. However, in patients without
CHD, the effect of rosuvastatin exhibited no significant results.
These findings indicated an activation of the NLRP3 inflammasome
signaling pathway during the inflammatory process of
atherosclerosis. Rosuvastatin could partially reverse the
activation of this pathway in different stages of atherogenesis,
particularly in the development of stable plaques including plaque
rupture. Based on the aforementioned findings, the present study
confirmed the anti-inflammatory effect of rosuvastatin, which was
independent of lipid-level lowering.
In summary, it was revealed that PBMCs from patients
with either SAP or AMI have a higher expression of NLRP3
inflammasome and its downstream cytokines, and activation of these
indicators revealed a correlation particularly in AMI patients.
Rosuvastatin exhibited desirable inhibitory effects on the
activation of the NLRP3 inflammasome signaling pathway in a
time-dependent manner. These findings indicated NLRP3 inflammasome
as a potential target in the inflammatory process that leads to
atherosclerosis, and provided a new pharmacological role of
rosuvastatin as an anti-inflammatory drug for CHD including SAP and
AMI.
Acknowledgements
Not applicable.
Funding
The present study was supported by a grant from the
Natural Science Research Key Project of Education Office of Anhui
Province (grant no. KJ2018A0242), and an internal grant from Bengbu
Medical College (grant no. BYKY1672).
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author upon reasonable
request.
Authors' contributions
JZ, SW, SH and HW designed the experiments. JZ, SW
and HL performed the experiments. JZ, ML and XG analyzed the data.
JZ, SW and SH wrote the manuscript. JZ and HW revised the
manuscript. All authors read, reviewed and approved the final
manuscript.
Ethics approval and consent to
participate
The utilization of samples was approved by the
Ethics Committee of The First Affiliated Hospital of Bengbu Medical
College (Bengbu, China) and written informed consent was obtained
from all subjects.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Benjamin EJ, Blaha MJ, Chiuve SE, Cushman
M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C,
et al: Heart disease and stroke statistics-2017 update: A report
from the American heart association. Circulation. 135:e146–e603.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Welsh P, Grassia G, Botha S, Sattar N and
Maffia P: Targeting inflammation to reduce cardiovascular disease
risk: A realistic clinical prospect? Br J Pharmacol. 174:3898–3913.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ridker PM, Everett BM, Thuren T, MacFadyen
JG, Chang WH, Ballantyne C, Fonseca F, Nicolau J, Koenig W, Anker
SD, et al: Antiinflammatory therapy with canakinumab for
atherosclerotic disease. N Engl J Med. 377:1119–1131. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ridker PM, Hennekens CH, Buring JE and
Rifai N: C-reactive protein and other markers of inflammation in
the prediction of cardiovascular disease in women. N Engl J Med.
342:836–843. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Duewell P, Kono H, Rayner KJ, Sirois CM,
Vladimer G, Bauernfeind FG, Abela GS, Franchi L, Nuñez G, Schnurr
M, et al: NLRP3 inflammasomes are required for atherogenesis and
activated by cholesterol crystals. Nature. 464:1357–1361. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kingsbury SR, Conaghan PG and McDermott
MF: The role of the NLRP3 inflammasome in gout. J Inflamm Res.
4:39–49. 2011.PubMed/NCBI
|
|
7
|
Toldo S, Mezzaroma E, Mauro AG, Salloum F,
Van Tassell BW and Abbate A: The inflammasome in myocardial injury
and cardiac remodeling. Antioxid Redox Signal. 22:1146–1161. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Satoh M, Tabuchi T, Itoh T and Nakamura M:
NLRP3 inflammasome activation in coronary artery disease: Results
from prospective and randomized study of treatment with
atorvastatin or rosuvastatin. Clin Sci (Lond). 126:233–241. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Schroder K, Zhou R and Tschopp J: The
NLRP3 inflammasome: A sensor for metabolic danger? Science.
327:296–300. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rajamäki K, Lappalainen J, Oörni K,
Välimäki E, Matikainen S, Kovanen PT and Eklund KK: Cholesterol
crystals activate the NLRP3 inflammasome in human macrophages: A
novel link between cholesterol metabolism and inflammation. PLoS
One. 5:e117652010. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
No authors listed, . Randomised trial of
cholesterol lowering in 4444 patients with coronary heart disease:
The scandinavian simvastatin survival study (4S). Lancet.
344:1383–1389. 1994.PubMed/NCBI
|
|
12
|
Ridker PM, Danielson E, Fonseca FA, Genest
J, Gotto AM Jr, Kastelein JJ, Koenig W, Libby P, Lorenzatti AJ,
MacFadyen JG, et al: Rosuvastatin to prevent vascular events in men
and women with elevated C-reactive protein. N Engl J Med.
359:2195–2207. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Schwartz GG, Olsson AG, Ezekowitz MD, Ganz
P, Oliver MF, Waters D, Zeiher A, Chaitman BR, Leslie S and Stern
T; Myocardial Ischemia Reduction with Aggressive Cholesterol
Lowering (MIRACL) Study Investigators, : Effects of atorvastatin on
early recurrent ischemic events in acute coronary syndromes: The
MIRACL study: A randomized controlled trial. JAMA. 285:1711–1718.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zacà V, Rastogi S, Imai M, Wang M, Sharov
VG, Jiang A, Goldstein S and Sabbah HN: Chronic monotherapy with
rosuvastatin prevents progressive left ventricular dysfunction and
remodeling in dogs with heart failure. J Am Coll Cardiol.
50:551–557. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ren Y, Zhu H, Fan Z, Gao Y and Tian N:
Comparison of the effect of rosuvastatin versus
rosuvastatin/ezetimibe on markers of inflammation in patients with
acute myocardial infarction. Exp Ther Med. 14:4942–4950.
2017.PubMed/NCBI
|
|
16
|
Karlson BW, Nicholls SJ, Lundman P, Barter
PJ and Palmer MK: Modeling statin-induced reductions of
cardiovascular events in primary prevention: A VOYAGER
meta-Analysis. Cardiology. 140:30–34. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Fihn SD, Gardin JM, Abrams J, Berra K,
Blankenship JC, Dallas AP, Douglas PS, Foody JM, Gerber TC,
Hinderliter AL, et al: 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS
guideline for the diagnosis and management of patients with stable
ischemic heart disease: Executive summary: A report of the American
college of cardiology foundation/American heart association task
force on practice guidelines, and the American College of
physicians, American association for thoracic surgery, preventive
cardiovascular nurses association, society for cardiovascular
angiography and interventions, and society of thoracic surgeons.
Circulation. 126:3097–3137. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Thygesen K, Alpert JS, Jaffe AS, Simoons
ML, Chaitman BR, White HD; Joint ESC/ACCF/AHA/WHF Task Force for
the Universal Definition of Myocardial Infarction, ; Katus HA,
Lindahl B, Morrow DA, et al: Third universal definition of
myocardial infarction. Circulation. 126:2020–2035. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Giampietro C, Lionetti MC, Costantini G,
Mutti F, Zapperi S and La Porta CA: Cholesterol impairment
contributes to neuroserpin aggregation. Sci Rep. 7:436692017.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Marchant DJ, Boyd JH, Lin DC, Granville
DJ, Garmaroudi FS and McManus BM: Inflammation in myocardial
diseases. Circ Res. 110:126–144. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Weber C and Soehnlein O: ApoE controls the
interface linking lipids and inflammation in atherosclerosis. J
Clin Invest. 121:3825–3827. 2011. View
Article : Google Scholar : PubMed/NCBI
|
|
23
|
Husain K, Hernandez W, Ansari RA and
Ferder L: Inflammation, oxidative stress and renin angiotensin
system in atherosclerosis. World J Biol Chem. 6:209–217. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Guo H, Callaway JB and Ting JP:
Inflammasomes: Mechanism of action, role in disease, and
therapeutics. Nat Med. 21:677–687. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Martinon F, Burns K and Tschopp J: The
inflammasome: A molecular platform triggering activation of
inflammatory caspases and processing of proIL-beta. Mol Cell.
10:417–426. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Lamkanfi M and Dixit VM: Mechanisms and
functions of inflammasomes. Cell. 157:1013–1022. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Muñoz-Planillo R, Kuffa P, Martinez-Colón
G, Smith BL, Rajendiran TM and Núñez G: K+ efflux is the
common trigger of NLRP3 inflammasome activation by bacterial toxins
and particulate matter. Immunity. 38:1142–1153. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Alfonso-Loeches S, Ureña-Peralta JR,
Morillo-Bargues MJ, Oliver-De La Cruz J and Guerri C: Role of
mitochondria ROS generation in ethanol-induced NLRP3 inflammasome
activation and cell death in astroglial cells. Front Cell Neurosci.
8:2162014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Hornung V, Bauernfeind F, Halle A, Samstad
EO, Kono H, Rock KL, Fitzgerald KA and Latz E: Silica crystals and
aluminum salts activate the NALP3 inflammasome through phagosomal
destabilization. Nat Immunol. 9:847–856. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Toldo S and Abbate A: The NLRP3
inflammasome in acute myocardial infarction. Nat Rev Cardiol.
15:203–214. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Galea J, Armstrong J, Gadsdon P, Holden H,
Francis SE and Holt CM: Interleukin-1 beta in coronary arteries of
patients with ischemic heart disease. Arterioscler Thromb Vasc
Biol. 16:1000–1006. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Blankenberg S, Tiret L, Bickel C, Peetz D,
Cambien F, Meyer J and Rupprecht HJ; AtheroGene Investigators, :
Interleukin-18 is a strong predictor of cardiovascular death in
stable and unstable angina. Circulation. 106:24–30. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Takahashi M: NLRP3 inflammasome as a novel
player in myocardial infarction. Int Heart J. 55:101–105. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kawaguchi M, Takahashi M, Hata T, Kashima
Y, Usui F, Morimoto H, Izawa A, Takahashi Y, Masumoto J, Koyama J,
et al: Inflammasome activation of cardiac fibroblasts is essential
for myocardial ischemia/reperfusion injury. Circulation.
123:594–604. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Toldo S, Marchetti C, Mauro AG, Chojnacki
J, Mezzaroma E, Carbone S, Zhang S, Van Tassell B, Salloum FN and
Abbate A: Inhibition of the NLRP3 inflammasome limits the
inflammatory injury following myocardial ischemia-reperfusion in
the mouse. Int J Cardiol. 209:215–220. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Bullón P, Cano-García FJ, Alcocer-Gómez E,
Varela-López A, Roman-Malo L, Ruiz-Salmerón RJ, Quiles JL,
Navarro-Pando JM, Battino M, Ruiz-Cabello J, et al: Could
NLRP3-inflammasome be a cardiovascular risk biomarker in acute
myocardial infarction patients? Antioxid Redox Signal. 27:269–275.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Verma S, Buchanan MR and Anderson TJ:
Endothelial function testing as a biomarker of vascular disease.
Circulation. 108:2054–2059. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Szmitko PE, Wang CH, Weisel RD, de Almeida
JR, Anderson TJ and Verma S: New markers of inflammation and
endothelial cell activation: Part I. Circulation. 108:1917–1923.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Yip HK, Wu CJ, Hang CL, Chang HW, Yang CH,
Hsieh YK, Fang CY, Fu M, Yeh KH and Chen MC: Levels and values of
inflammatory markers in patients with angina pectoris. Int Heart J.
46:571–581. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Fiechter M, Ghadri JR, Jaguszewski M,
Siddique A, Vogt S, Haller RB, Halioua R, Handzic A, Kaufmann PA,
Corti R, et al: Impact of inflammation on adverse cardiovascular
events in patients with acute coronary syndromes. J Cardiovasc Med
(Hagerstown). 14:807–814. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Ference BA, Ginsberg HN, Graham I, Ray KK,
Packard CJ, Bruckert E, Hegele RA, Krauss RM, Raal FJ, Schunkert H,
et al: Low-density lipoproteins cause atherosclerotic
cardiovascular disease. 1. Evidence from genetic, epidemiologic,
and clinical studies. A consensus statement from the European
atherosclerosis society consensus panel. Eur Heart J. 38:2459–2472.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Tousoulis D, Andreou I, Tsiatas M, Miliou
A, Tentolouris C, Siasos G, Papageorgiou N, Papadimitriou CA,
Dimopoulos MA and Stefanadis C: Effects of rosuvastatin and
allopurinol on circulating endothelial progenitor cells in patients
with congestive heart failure: The impact of inflammatory process
and oxidative stress. Atherosclerosis. 214:151–157. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Altaf A, Qu P, Zhao Y, Wang H, Lou D and
Niu N: NLRP3 inflammasome in peripheral blood monocytes of acute
coronary syndrome patients and its relationship with statins. Coron
Artery Dis. 26:409–421. 2015. View Article : Google Scholar : PubMed/NCBI
|