|
1
|
Lagacé F, Ghazawi FM, Le M, Rahme E, Savin
E, Zubarev A, Alakel A, Sasseville D, Moreau L, Meterissian S and
Litvinov IV: Analysis of incidence, mortality trends, and
geographic distribution of breast cancer patients in Canada. Breast
Cancer Res Treat. 178:683–691. 2019. View Article : Google Scholar
|
|
2
|
Ruppert AS, Dixon JG, Salles G, Wall A,
Cunningham D, Poeschel V, Haioun C, Tilly H, Ghesquieres H, Ziepert
M, et al: International prognostic indices in diffuse large B-cell
lymphoma: A comparison of IPI, R-IPI and NCCN-IPI. Blood.
135:2041–2048. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Li S, Xu HX, Wu CT, Wang WQ, Jin W, Gao
HL, Li H, Zhang SR, Xu JZ, Qi ZH, et al: Angiogenesis in pancreatic
cancer: Current research status and clinical implications.
Angiogenesis. 22:15–36. 2019. View Article : Google Scholar : PubMed/NCBI
|
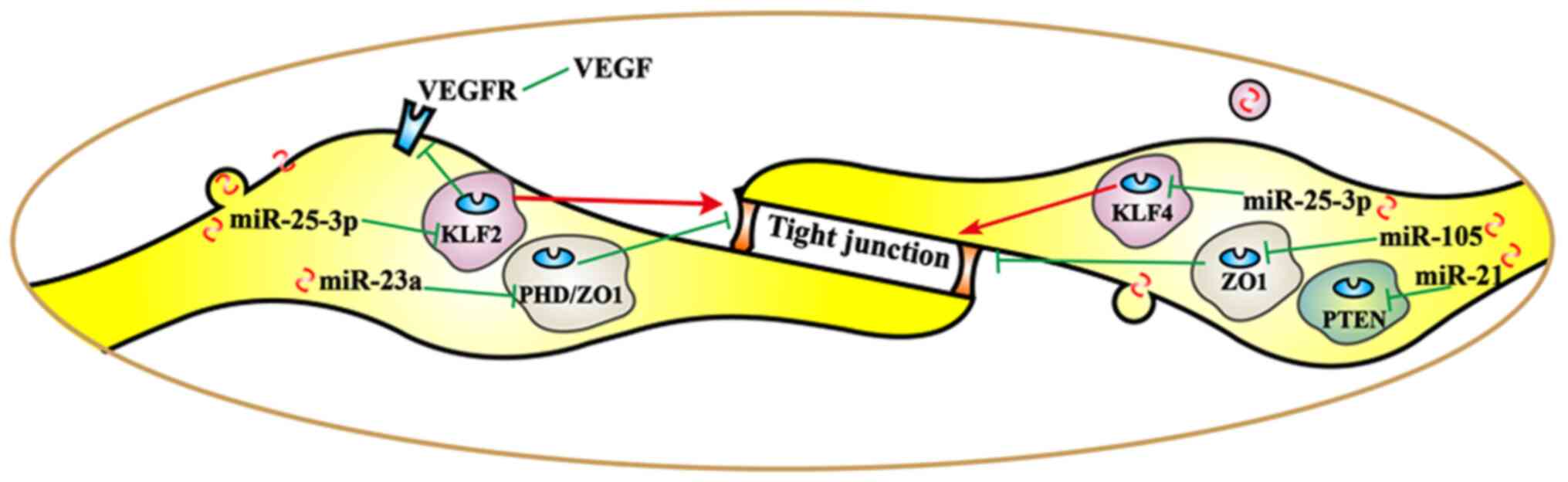
|
4
|
Orso F, Quirico L, Dettori D, Coppo R,
Virga F, Ferreira LC, Paoletti C, Baruffaldi D, Penna E and Taverna
D: Role of miRNAs in tumor and endothelial cell interactions during
tumor progression. Semin Cancer Biol. 60:214–224. 2020. View Article : Google Scholar : PubMed/NCBI
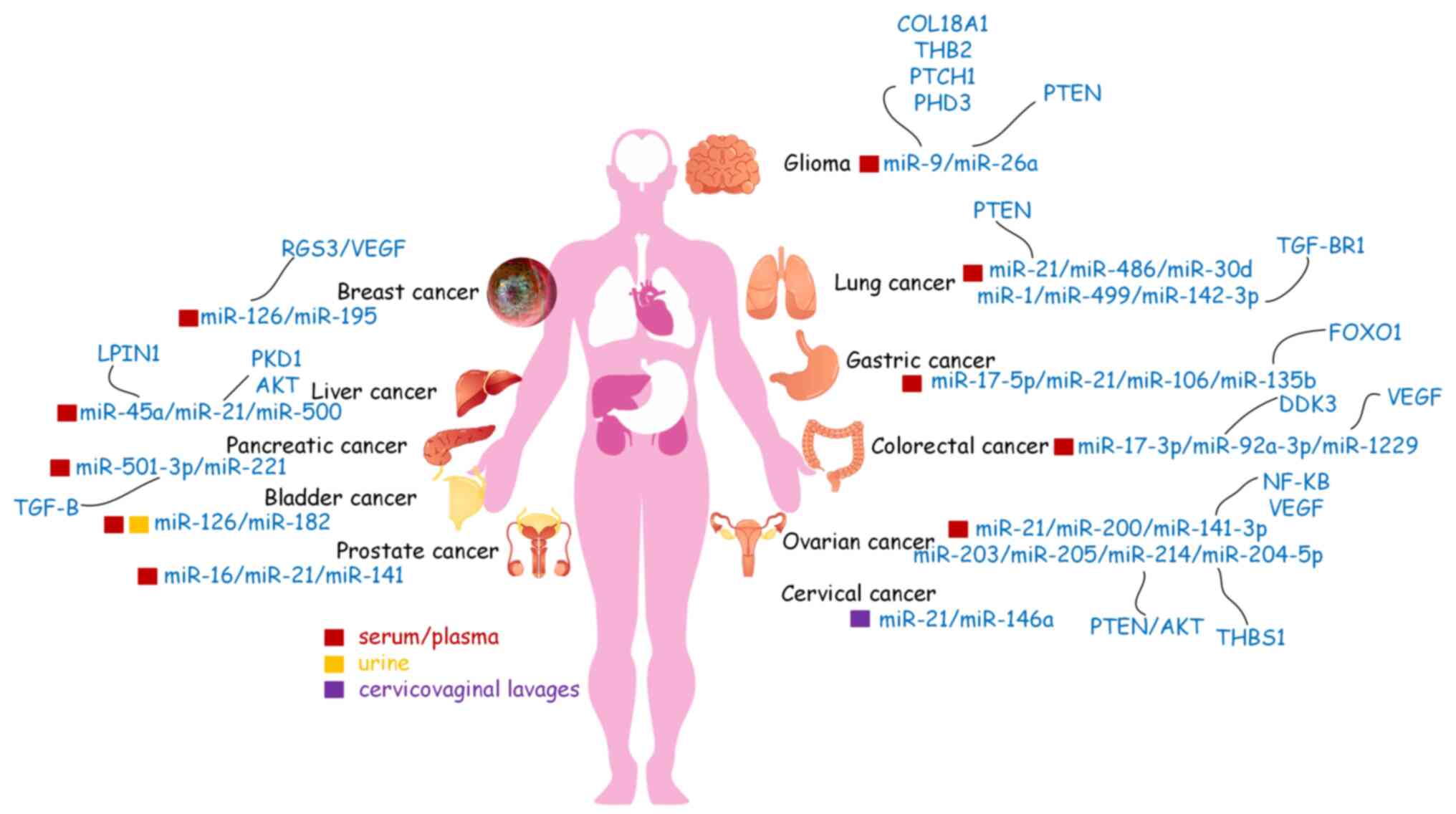
|
|
5
|
Bisgin H, Gong B, Wang Y and Tong W:
Evaluation of bioinformatics approaches for Next-Generation
sequencing analysis of microRNAs with a toxicogenomics study
design. Front Genet. 9:222018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lee YS and Dutta A: MicroRNAs in cancer.
Annu Rev Pathol. 4:199–227. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wang Y, Wang L, Chen C and Chu X: New
insights into the regulatory role of microRNA in tumor angiogenesis
and clinical implications. Mol Cancer. 17:222018. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hansen TB: Detecting agotrons in ago
CLIPseq Data. Methods Mol Biol. 1823:221–232. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
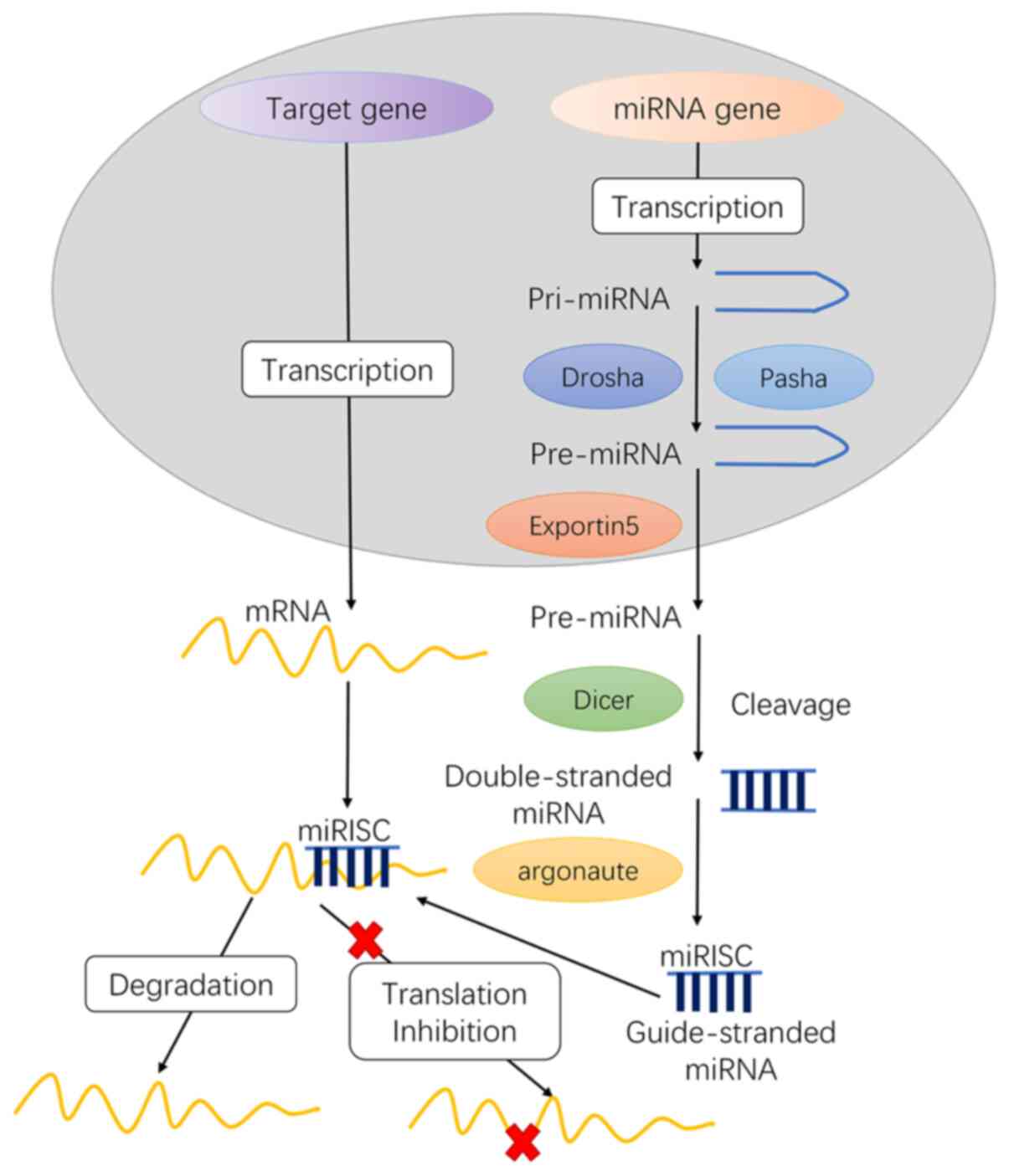
Vishnoi A and Rani S: MiRNA biogenesis and
regulation of diseases: An overview. Methods Mol Biol. 1509:1–10.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Denli AM, Tops BB, Plasterk RH, Ketting RF
and Hannon GJ: Processing of primary microRNAs by the
Microprocessor complex. Nature. 432:231–235. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Cheng L, Li F, Jiang Y, Yu H, Xie C, Shi Y
and Gong Q: Structural insights into a unique preference for 3′
terminal guanine of mirtron in Drosophila TUTase tailor. Nucleic
Acids Res. 47:495–508. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Michlewski G and Cáceres JF:
Post-transcriptional control of miRNA biogenesis. RNA. 25:1–16.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Leung DW, Cachianes G, Kuang WJ, Goeddel
DV and Ferrara N: Vascular endothelial growth factor is a secreted
angiogenic mitogen. Science. 246:1306–1309. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Goradel NH, Mohammadi N, Haghi-Aminjan H,
Farhood B, Negahdari B and Sahebkar A: Regulation of tumor
angiogenesis by microRNAs: State of the art. J Cell Physiol.
234:1099–1110. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Li R, Qi Y, Jiang M, Zhang T, Wang H, Wang
L and Han M: Primary tumor-secreted VEGF induces vascular
hyperpermeability in premetastatic lung via the occludin
phosphorylation/ubiquitination pathway. Mol Carcinog. 58:2316–2326.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Xu J, Xie L and Guo W: PDGF/PDGFR effects
in osteosarcoma and the ‘add-on’ strategy. Clin Sarcoma Res.
8:152018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
DeLisser HM, Christofidou-Solomidou M,
Strieter RM, Burdick MD, Robinson CS, Wexler RS, Kerr JS, Garlanda
C, Merwin JR, Madri JA and Albelda SM: Involvement of endothelial
PECAM-1/CD31 in angiogenesis. Am J Pathol. 151:671–677.
1997.PubMed/NCBI
|
|
18
|
Fang L, He Y, Liu Y, Ding H, Tong Y, Hu L,
Wang C, Zhang Y, Zheng X and Huang P: Adjustment of microvessel
area by stromal area to improve survival prediction in non-small
cell lung cancer. J Cancer. 10:3397–3406. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Hida K, Maishi N, Annan DA and Hida Y:
Contribution of tumor endothelial cells in cancer progression. Int
J Mol Sci. 19:12722018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zhang Y, Zhao HJ, Xia XR, Diao FY, Ma X,
Wang J, Gao L, Liu J, Gao C, Cui YG and Liu JY: Hypoxia-induced and
HIF1α-VEGF-mediated tight junction dysfunction in choriocarcinoma
cells: Implications for preeclampsia. Clin Chim Acta. 489:203–211.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Li L, Li JC, Yang H, Zhang X, Liu LL, Li
Y, Zeng TT, Zhu YH, Li XD, Li Y, et al: Expansion of cancer stem
cell pool initiates lung cancer recurrence before angiogenesis.
Proc Natl Acad Sci USA. 115:E8948–E8957. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Okamoto T, Usuda H, Tanaka T, Wada K and
Shimaoka M: The functional implications of endothelial gap
junctions and cellular mechanics in vascular angiogenesis. Cancers.
11:2372019. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kalluri R and LeBleu VS: The biology,
function, and biomedical applications of exosomes. Science.
367:eaau69772020. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Sun Z, Shi K, Yang S, Liu J, Zhou Q, Wang
G, Song J, Li Z, Zhang Z and Yuan W: Effect of exosomal miRNA on
cancer biology and clinical applications. Mol Cancer. 17:1472018.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Tomasetti M, Lee W, Santarelli L and
Neuzil J: Exosome-derived microRNAs in cancer metabolism: Possible
implications in cancer diagnostics and therapy. Exp Mol Med.
49:e2852017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Hsu YL, Hung JY, Chang WA, Lin YS, Pan YC,
Tsai PH, Wu CY and Kuo PL: Hypoxic lung cancer-secreted exosomal
miR-23a increased angiogenesis and vascular permeability by
targeting prolyl hydroxylase and tight junction protein ZO-1.
Oncogene. 36:4929–4942. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Zeng Z, Li Y, Pan Y, Lan X, Song F, Sun J,
Zhou K, Liu X, Ren X, Wang F, et al: Cancer-derived exosomal
miR-25-3p promotes pre-metastatic niche formation by inducing
vascular permeability and angiogenesis. Nat Commun. 9:53952018.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
He L, Zhu W, Chen Q, Yuan Y, Wang Y, Wang
J and Wu X: Ovarian cancer cell-secreted exosomal miR-205 promotes
metastasis by inducing angiogenesis. Theranostics. 9:8206–8220.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Masoumi-Dehghi S, Babashah S and
Sadeghizadeh M: MicroRNA-141-3p-containing small extracellular
vesicles derived from epithelial ovarian cancer cells promote
endothelial cell angiogenesis through activating the JAK/STAT3 and
NF-κB signaling pathways. J Cell Commun Signal. 14:233–244. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Chen X, Mangala LS, Mooberry L, Bayraktar
E, Dasari SK, Ma S, Ivan C, Court KA, Rodriguez-Aguayo C, Bayraktar
R, et al: Identifying and targeting angiogenesis-related microRNAs
in ovarian cancer. Oncogene. 38:6095–6108. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Zhou Y, Ren H, Dai B, Li J, Shang L, Huang
J and Shi X: Hepatocellular carcinoma-derived exosomal miRNA-21
contributes to tumor progression by converting hepatocyte stellate
cells to cancer-associated fibroblasts. J Exp Clin Cancer Res.
37:3242018. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Zhao S, Li J, Zhang G, Wang Q, Wu C, Zhang
Q, Wang H, Sun P, Xiang R and Yang S: Exosomal miR-451a functions
as a tumor suppressor in hepatocellular carcinoma by targeting
LPIN1. Cell Physiol Biochem. 53:19–35. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Chen X, Yang F, Zhang T, Wang W, Xi W, Li
Y, Zhang D, Huo Y, Zhang J, Yang A and Wang T: MiR-9 promotes
tumorigenesis and angiogenesis and is activated by MYC and OCT4 in
human glioma. J Exp Clin Cancer Res. 38:992019. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Wang ZF, Liao F, Wu H and Dai J: Glioma
stem cells-derived exosomal miR-26a promotes angiogenesis of
microvessel endothelial cells in glioma. J Exp Clin Cancer Res.
38:2012019. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Bai M, Li J, Yang H, Zhang H, Zhou Z, Deng
T, Zhu K, Ning T, Fan Q, Ying G and Ba Y: MiR-135b delivered by
gastric tumor exosomes inhibits FOXO1 expression in endothelial
cells and promotes angiogenesis. Mol Ther. 27:1772–1783. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Lawson J, Dickman C, Towle R, Jabalee J,
Javer A and Garnis C: Extracellular vesicle secretion of miR-142-3p
from lung adenocarcinoma cells induces tumor promoting changes in
the stroma through cell-cell communication. Mol Carcinog.
58:376–387. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Yin Z, Ma T, Huang B, Lin L, Zhou Y, Yan
J, Zou Y and Chen S: Macrophage-derived exosomal microRNA-501-3p
promotes progression of pancreatic ductal adenocarcinoma through
the TGFBR3-mediated TGF-β signaling pathway. J Exp Clin Cancer Res.
38:3102019. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Yamada NO, Heishima K, Akao Y and Senda T:
Extracellular vesicles containing MicroRNA-92a-3p facilitate
partial Endothelial-Mesenchymal transition and angiogenesis in
endothelial cells. Int J Mol Sci. 20:44062019. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Hu HY, Yu CH, Zhang HH, Zhang SZ, Yu WY,
Yang Y and Chen Q: Exosomal miR-1229 derived from colorectal cancer
cells promotes angiogenesis by targeting HIPK2. Int J Biol
Macromol. 132:470–477. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Bazzoni G and Dejana E: Endothelial
cell-to-cell junctions: Molecular organization and role in vascular
homeostasis. Physiol Rev. 84:869–901. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Lesage J, Suarez-Carmona M,
Neyrinck-Leglantier D, Grelet S, Blacher S, Hunziker W, Birembaut
P, Noël A, Nawrocki-Raby B, Gilles C and Polette M: Zonula
occludens-1/NF-κB/CXCL8: A new regulatory axis for tumor
angiogenesis. FASEB J. 31:1678–1688. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Bhat AA, Uppada S, Achkar IW, Hashem S,
Yadav SK, Shanmugakonar M, Al-Naemi HA, Haris M and Uddin S: Tight
junction proteins and signaling pathways in cancer and
inflammation: A functional crosstalk. Front Physiol. 9:19422019.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Chao YC, Pan SH, Yang SC, Yu SL, Che TF,
Lin CW, Tsai MS, Chang GC, Wu CH, Wu YY, et al: Claudin-1 is a
metastasis suppressor and correlates with clinical outcome in lung
adenocarcinoma. Am J Respir Crit Care Med. 179:123–133. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Zhao L, Wang P, Liu Y, Ma J and Xue Y:
MiR-34c regulates the permeability of blood-tumor barrier via
MAZ-mediated expression changes of ZO-1, occludin, and claudin-5. J
Cell Physiol. 230:716–731. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Tornavaca O, Chia M, Dufton N, Almagro LO,
Conway DE, Randi AM, Schwartz MA, Matter K and Balda MS: ZO-1
controls endothelial adherens junctions, cell-cell tension,
angiogenesis, and barrier formation. J Cell Biol. 208:821–838.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Wu T, Hu H, Zhang T, Jiang L, Li X, Liu S,
Zheng C, Yan G, Chen W, Ning Y, et al: MiR-25 promotes cell
proliferation, migration, and invasion of Non-Small-Cell lung
cancer by targeting the LATS2/YAP signaling pathway. Oxid Med Cell
Longev. 2019:97197232019. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Liu B and Sun X: MiR-25 promotes invasion
of human non-small cell lung cancer via CDH1. Bioengineered.
10:271–281. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Xu FX, Su YL, Zhang H, Kong JY, Yu H and
Qian BY: Prognostic implications for high expression of MiR-25 in
lung adenocarcinomas of female non-smokers. Asian Pac J Cancer
Prev. 15:1197–1203. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Zhou W, Fong MY, Min Y, Somlo G, Liu L,
Palomares MR, Yu Y, Chow A, O'Connor ST, Chin AR, et al:
Cancer-secreted miR-105 destroys vascular endothelial barriers to
promote metastasis. Cancer Cell. 25:501–515. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Zhang L, Shen J, Cheng J and Fan X:
MicroRNA-21 regulates intestinal epithelial tight junction
permeability. Cell Biochem Funct. 33:235–240. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Cho HS, Han TS, Hur K and Ban HS: The
roles of Hypoxia-inducible factors and non-coding RNAs in
gastrointestinal cancer. Genes (Basel). 10:10082019. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Salinas-Vera YM, Marchat LA,
Gallardo-Rincón D, Ruiz-García E, Astudillo-De La Vega H,
Echavarría-Zepeda R and López-Camarillo C: AngiomiRs: MicroRNAs
driving angiogenesis in cancer (Review). Int J Mol Med. 43:657–670.
2019.PubMed/NCBI
|
|
53
|
Park JE, Dutta B, Tse SW, Gupta N, Tan CF,
Low JK, Yeoh KW, Kon OL, Tam JP and Sze SK: Hypoxia-induced tumor
exosomes promote M2-like macrophage polarization of infiltrating
myeloid cells and microRNA-mediated metabolic shift. Oncogene.
38:5158–5173. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Ren W, Hou J, Yang C, Wang H, Wu S, Wu Y,
Zhao X and Lu C: Extracellular vesicles secreted by hypoxia
pre-challenged mesenchymal stem cells promote non-small cell lung
cancer cell growth and mobility as well as macrophage M2
polarization via miR-21-5p delivery. J Exp Clin Cancer Res.
38:622019. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Zhang S, Zhang R, Xu R, Shang J, He H and
Yang Q: MicroRNA-574-5p in gastric cancer cells promotes
angiogenesis by targeting protein tyrosine phosphatase non-receptor
type 3 (PTPN3). Gene. 733:1443832020. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Yu P, Fan S, Huang L, Yang L and Du Y:
MIR210 as a potential molecular target to block invasion and
metastasis of gastric cancer. Med Hypotheses. 84:209–212. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Chen F, Chen J, Yang L, Liu J, Zhang X,
Zhang Y, Tu Q, Yin D, Lin D, Wong PP, et al: Extracellular
vesicle-packaged HIF-1α-stabilizing lncRNA from tumour-associated
macrophages regulates aerobic glycolysis of breast cancer cells.
Nat Cell Biol. 21:498–510. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Liu L, Wang Y, Bai R, Yang K and Tian Z:
MiR-186 inhibited aerobic glycolysis in gastric cancer via HIF-1α
regulation. Oncogenesis. 6:e3182017. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Shivdasani RA: MicroRNAs: Regulators of
gene expression and cell differentiation. Blood. 108:3646–3653.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Bielenberg DR and Zetter BR: The
contribution of angiogenesis to the process of metastasis. Cancer
J. 21:267–273. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Landskroner-Eiger S, Moneke I and Sessa
WC: MiRNAs as modulators of angiogenesis. Cold Spring Harb Perspect
Med. 3:a0066432013. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Dimova I, Popivanov G and Djonov V:
Angiogenesis in cancer-general pathways and their therapeutic
implications. J BUON. 19:15–21. 2014.PubMed/NCBI
|
|
63
|
Chen X, Xu X, Pan B, Zeng K, Xu M, Liu X,
He B, Pan Y, Sun H and Wang S: MiR-150-5p suppresses tumor
progression by targeting VEGFA in colorectal cancer. Aging (Albany
NY). 10:3421–3437. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Mao Z, Xu B, He L and Zhang G: PVT1
promotes angiogenesis by regulating miR-29c/Vascular endothelial
growth factor (VEGF) signaling pathway in non-small-cell lung
cancer (NSCLC). Med Sci Monit. 25:5418–5425. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Yang F, Shao C, Wei K, Jing X, Qin Z, Shi
Y, Shu Y and Shen H: MiR-942 promotes tumor migration, invasion,
and angiogenesis by regulating EMT via BARX2 in non-small-cell lung
cancer. J Cell Physiol. 234:23596–23607. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Gao LM, Zheng Y, Wang P, Zheng L, Zhang
WL, Di Y, Chen LL, Yin XB, Tian Q, Shi SS and Xu SF:
Tumor-suppressive effects of microRNA-181d-5p on non-small-cell
lung cancer through the CDKN3-mediated Akt signaling pathway in
vivo and in vitro. Am J Physiol Lung Cell Mol Physiol.
316:L918–L933. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Zhang Y, Chen Z, Feng L, Jiang P, Li X and
Wang X: Ionizing Radiation-inducible microRNA-21 induces
angiogenesis by directly targeting PTEN. Asian Pac J Cancer Prev.
20:1587–1593. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Liu H, Chen Y, Li Y, Li C, Qin T, Bai M,
Zhang Z, Jia R, Su Y and Wang C: MiR-195 suppresses metastasis and
angiogenesis of squamous cell lung cancer by inhibiting the
expression of VEGF. Mol Med Rep. 20:2625–2632. 2019.PubMed/NCBI
|
|
69
|
Hong Z, Hong C, Ma B, Wang Q, Zhang X, Li
L, Wang C and Chen D: MicroRNA-126-3p inhibits the proliferation,
migration, invasion, and angiogenesis of triple-negative breast
cancer cells by targeting RGS3. Oncol Rep. 42:1569–1579.
2019.PubMed/NCBI
|
|
70
|
Alhasan L: MiR-126 modulates angiogenesis
in breast cancer by targeting VEGF-A-mRNA. Asian Pac J Cancer Prev.
20:193–197. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Zhao Z, Li L, Du P, Ma L, Zhang W, Zheng
L, Lan B, Zhang B, Ma F, Xu B, et al: Transcriptional
Downregulation of miR-4306 serves as a new therapeutic target for
triple negative breast cancer. Theranostics. 9:1401–1416. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Hunter S, Nault B, Ugwuagbo KC, Maiti S
and Majumder M: Mir526b and Mir655 promote tumour associated
angiogenesis and lymphangiogenesis in breast cancer. Cancers
(Basel). 11:9382019. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Lin X, Qiu W, Xiao Y, Ma J, Xu F, Zhang K,
Gao Y, Chen Q, Li Y, Li H and Qian A: MiR-199b-5p suppresses tumor
angiogenesis mediated by vascular endothelial cells in breast
cancer by targeting ALK1. Front Genet. 10:13972019. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Chen X, Zeng K, Xu M, Liu X, Hu X, Xu T,
He B, Pan Y, Sun H and Wang S: P53-induced miR-1249 inhibits tumor
growth, metastasis, and angiogenesis by targeting VEGFA and HMGA2.
Cell Death Dis. 10:1312019. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Lin M, Zhang Z, Gao M, Yu H, Sheng H and
Huang J: MicroRNA-193a-3p suppresses the colorectal cancer cell
proliferation and progression through downregulating the PLAU
expression. Cancer Manag Res. 11:5353–5363. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Fang Y, Sun B, Wang J and Wang Y: MiR-622
inhibits angiogenesis by suppressing the CXCR4-VEGFA axis in
colorectal cancer. Gene. 699:37–42. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Fan X, Liu M, Tang H, Leng D, Hu S, Lu R,
Wan W and Yuan S: MicroRNA-7 exerts antiangiogenic effect on
colorectal cancer via ERK signaling. J Surg Res. 240:48–59. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Chen P, Guo H, Wu X, Li J, Duan X, Ba Q
and Wang H: Epigenetic silencing of microRNA-204 by Helicobacter
pylori augments the NF-κB signaling pathway in gastric cancer
development and progression. Carcinogenesis. 41:430–441. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Shi Y, Huang X, Chen G, Wang Y, Liu Y, Xu
W, Tang S, Guleng B, Liu J and Ren J: MiR-632 promotes gastric
cancer progression by accelerating angiogenesis in a TFF1-dependent
manner. BMC Cancer. 19:142019. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Dai J, Wei R, Zhang P and Kong B:
Overexpression of microRNA-195-5p reduces cisplatin resistance and
angiogenesis in ovarian cancer by inhibiting the PSAT1-dependent
GSK3β/β-catenin signaling pathway. J Transl Med. 17:1902019.
View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Lu J, Xu Y, Wei X, Zhao Z, Xue J and Liu
P: Emodin inhibits the epithelial to mesenchymal transition of
epithelial ovarian cancer cells via ILK/GSK-3β/Slug signaling
pathway. Biomed Res Int. 2016:62532802016. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Salinas-Vera YM, Gallardo-Rincón D,
García-Vázquez R, Hernández-de la Cruz ON, Marchat LA,
González-Barrios JA, Ruíz-García E, Vázquez-Calzada C,
Contreras-Sanzón E, Resendiz-Hernández M, et al: HypoxamiRs
profiling identify miR-745 as a regulator of the early stages of
vasculogenic mimicry in SKOV3 ovarian cancer cells. Front Oncol.
9:3812019. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Mu HQ, He YH, Wang SB, Yang S, Wang YJ,
Nan CJ, Bao YF, Xie QP and Chen YH: MiR-130b/TNF-α/NF-κB/VEGFA loop
inhibits prostate cancer angiogenesis. Clin Transl Oncol.
22:111–121. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Zhang P, Yang X, Wang L, Zhang D, Luo Q
and Wang B: Overexpressing miR-335 inhibits DU145 cell
proliferation by targeting early growth response 3 in prostate
cancer. Int J Oncol. 54:1981–1994. 2019.PubMed/NCBI
|
|
85
|
He Q, Zhao L, Liu X, Zheng J, Liu Y, Liu
L, Ma J, Cai H, Li Z and Xue Y: MOV10 binding circ-DICER1 regulates
the angiogenesis of glioma via miR-103a-3p/miR-382-5p mediated ZIC4
expression change. J Exp Clin Cancer Res. 38:92019. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Li C, Wang X and Song Q: MicroRNA 885-5p
inhibits hepatocellular carcinoma metastasis by repressing AEG1.
Onco Targets Ther. 13:981–988. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Zhang S, Li G, Liu C, Lu S, Jing Q, Chen
X, Zheng H, Ma H, Zhang D, Ren S, et al: MiR-30e-5p represses
angiogenesis and metastasis by directly targeting AEG-1 in squamous
cell carcinoma of the head and neck. Cancer Sci. 111:356–368. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Niu J, Li Z and Li F: Overexpressed
microRNA-136 works as a cancer suppressor in gallbladder cancer
through suppression of JNK signaling pathway via inhibition of
MAP2K4. Am J Physiol Gastrointest Liver Physiol. 317:G670–G681.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Fan B, Jin Y, Zhang H, Zhao R, Sun M, Sun
M, Yuan X, Wang W, Wang X, Chen Z, et al: MicroRNA-21 contributes
to renal cell carcinoma cell invasiveness and angiogenesis via the
PDCD4/c-Jun (AP-1) signalling pathway. Int J Oncol. 56:178–192.
2020.PubMed/NCBI
|
|
90
|
Wang H, Peng R, Wang J, Qin Z and Xue L:
Circulating microRNAs as potential cancer biomarkers: The advantage
and disadvantage. Clin Epigenetics. 10:592018. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Ali Syeda Z, Langden SSS, Munkhzul C, Lee
M and Song SJ: Regulatory mechanism of MicroRNA expression in
cancer. Int J Mol Sci. 21:17232020. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Hammouz RY, Kołat D, Kałuzińska Ż,
Płuciennik E and Bednarek AK: MicroRNAs: Their role in metastasis,
angiogenesis, and the potential for biomarker utility in bladder
carcinomas. Cancers (Basel). 13:8912021. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Tipanee J, Di Matteo M, Tulalamba W,
Samara-Kuko E, Keirsse J, Van Ginderachter JA, Chuah MK and
VandenDriessche T: Validation of miR-20a as a tumor suppressor gene
in liver carcinoma using hepatocyte-specific hyperactive piggyBac
transposons. Mol Ther Nucleic Acids. 19:1309–1329. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Rosenfeld N, Aharonov R, Meiri E,
Rosenwald S, Spector Y, Zepeniuk M, Benjamin H, Shabes N, Tabak S,
Levy A, et al: MicroRNAs accurately identify cancer tissue origin.
Nat Biotechnol. 26:462–469. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Søkilde R, Vincent M, Møller AK, Hansen A,
Høiby PE, Blondal T, Nielsen BS, Daugaard G, Møller S and Litman T:
Efficient identification of miRNAs for classification of tumor
origin. J Mol Diagn. 16:106–115. 2014. View Article : Google Scholar
|
|
96
|
Yang Y, Guo Z, Chen W, Wang X, Cao M, Han
X, Zhang K, Teng B, Cao J, Wu W, et al: M2 macrophage-derived
exosomes promote angiogenesis and growth of pancreatic ductal
adenocarcinoma by targeting E2F2. Mol Ther. 29:1226–1238. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Caporali A and Emanueli C: MicroRNA
regulation in angiogenesis. Vascul Pharmacol. 55:79–86. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Szajnik M, Czystowska-Kuźmicz M, Elishaev
E and Whiteside TL: Biological markers of prognosis, response to
therapy and outcome in ovarian carcinoma. Expert Rev Mol Diagn.
16:811–826. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Taylor DD and Gercel-Taylor C: MicroRNA
signatures of tumor-derived exosomes as diagnostic biomarkers of
ovarian cancer. Gynecol Oncol. 110:13–21. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Qattan A, Intabli H, Alkhayal W, Eltabache
C, Tweigieri T and Amer SB: Robust expression of tumor suppressor
miRNA's let-7 and miR-195 detected in plasma of Saudi female breast
cancer patients. BMC Cancer. 17:7992017. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Hu X, Fan J, Duan B, Zhang H, He Y, Duan P
and Li X: Single-molecule catalytic hairpin assembly for rapid and
direct quantification of circulating miRNA biomarkers. Anal Chim
Acta. 1042:109–115. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Tsujiura M, Ichikawa D, Komatsu S,
Shiozaki A, Takeshita H, Kosuga T, Konishi H, Morimura R, Deguchi
K, Fujiwara H, et al: Circulating microRNAs in plasma of patients
with gastric cancers. Br J Cancer. 102:1174–1179. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Zhou Q, Liu J, Quan J, Liu W, Tan H and Li
W: MicroRNAs as potential biomarkers for the diagnosis of glioma: A
systematic review and meta-analysis. Cancer Sci. 109:2651–2659.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Hu Z, Chen X, Zhao Y, Tian T, Jin G, Shu
Y, Chen Y, Xu L, Zen K, Zhang C and Shen H: Serum microRNA
signatures identified in a genome-wide serum microRNA expression
profiling predict survival of non-small-cell lung cancer. J Clin
Oncol. 28:1721–1726. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Rabinowits G, Gerçel-Taylor C, Day JM,
Taylor DD and Kloecker GH: Exosomal microRNA: A diagnostic marker
for lung cancer. Clin Lung Cancer. 10:42–46. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Yamamoto Y, Kosaka N, Tanaka M, Koizumi F,
Kanai Y, Mizutani T, Murakami Y, Kuroda M, Miyajima A, Kato T and
Ochiya T: MicroRNA-500 as a potential diagnostic marker for
hepatocellular carcinoma. Biomarkers. 14:529–538. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Sabo AA, Birolo G, Naccarati A, Dragomir
MP, Aneli S, Allione A, Oderda M, Allasia M, Gontero P, Sacerdote
C, et al: Small Non-Coding RNA profiling in plasma extracellular
vesicles of bladder cancer patients by next-generation sequencing:
Expression levels of miR-126-3p and piR-5936 increase with higher
histologic grades. Cancers (Basel). 12:15072020. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Xie F, Li Y, Wang M, Huang C, Tao D, Zheng
F, Zhang H, Zeng F, Xiao X and Jiang G: Circular RNA BCRC-3
suppresses bladder cancer proliferation through miR-182-5p/p27
axis. Mol Cancer. 17:1442018. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Tanaka Y, Kamohara H, Kinoshita K,
Kurashige J, Ishimoto T, Iwatsuki M, Watanabe M and Baba H:
Clinical impact of serum exosomal microRNA-21 as a clinical
biomarker in human esophageal squamous cell carcinoma. Cancer.
119:1159–1167. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Liu J, Sun H, Wang X, Yu Q, Li S, Yu X and
Gong W: Increased exosomal microRNA-21 and microRNA-146a levels in
the cervicovaginal lavage specimens of patients with cervical
cancer. Int J Mol Sci. 15:758–773. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Park NJ, Zhou H, Elashoff D, Henson BS,
Kastratovic DA, Abemayor E and Wong DT: Salivary microRNA:
Discovery, characterization, and clinical utility for oral cancer
detection. Clin Cancer Res. 15:5473–5477. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
El-Daly SM, Morsy SM, Medhat D, El-Bana
MA, Latif YA, Omara EA, Awadallah JR and Gamal-Eldeen AM: The
diagnostic efficacy of circulating miRNAs in monitoring the early
development of colitis-induced colorectal cancer. J Cell Biochem.
120:16668–16680. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Ng EK, Chong WW, Jin H, Lam EK, Shin VY,
Yu J, Poon TC, Ng SS and Sung JJ: Differential expression of
microRNAs in plasma of patients with colorectal cancer: A potential
marker for colorectal cancer screening. Gut. 58:1375–1381. 2009.
View Article : Google Scholar : PubMed/NCBI
|