Introduction
The identification of the primary tumor in patients
presenting with cerebral metastasis is mandatory in order to plan a
proper treatment strategy. Unfortunately, in certain instances, the
primary tumor remains occult even after a extensive and scrupulous
diagnostic work-up (1,2).
Esophageal cancer was well described at the
beginning of the 19th century, and the first successful resection
was performed by Torek in 1913 (3).
The overall incidence of the disease is highest in males >50
years old. Brain metastases have been reported in only 1.7–3.6% of
all patients with different types of esophageal cancer (4,5), while
brain metastasis as the presenting form of esophageal carcinoma is
highly uncommon (6). The present
study reports the case of a patient with a carcinoma of unknown
primary origin (CUP) who presented with a cerebral metastasis,
without extra-neurological symptoms. The CUP was subsequently
diagnosed as a esophageal carcinoma. Written informed consent was
obtained from the patient.
Case report
A 69-year-old male patient was referred to the
Neurological Centre of Latium (NCL) in July 2011 due to rapidly
progressing right-hand apraxia and agraphia and recent reoccurring
headaches. The patient was a heavy smoker (>40 pack years) and
had a history of alcohol abuse. A physical examination indicated
right, upper-limb prevailing hemiparesis [American Spinal Injury
Association (ASIA) impairment scale, grade 1]. Furthermore, right
dysmetria, adiadochokinesia and somatesthesic disturbance were
present.
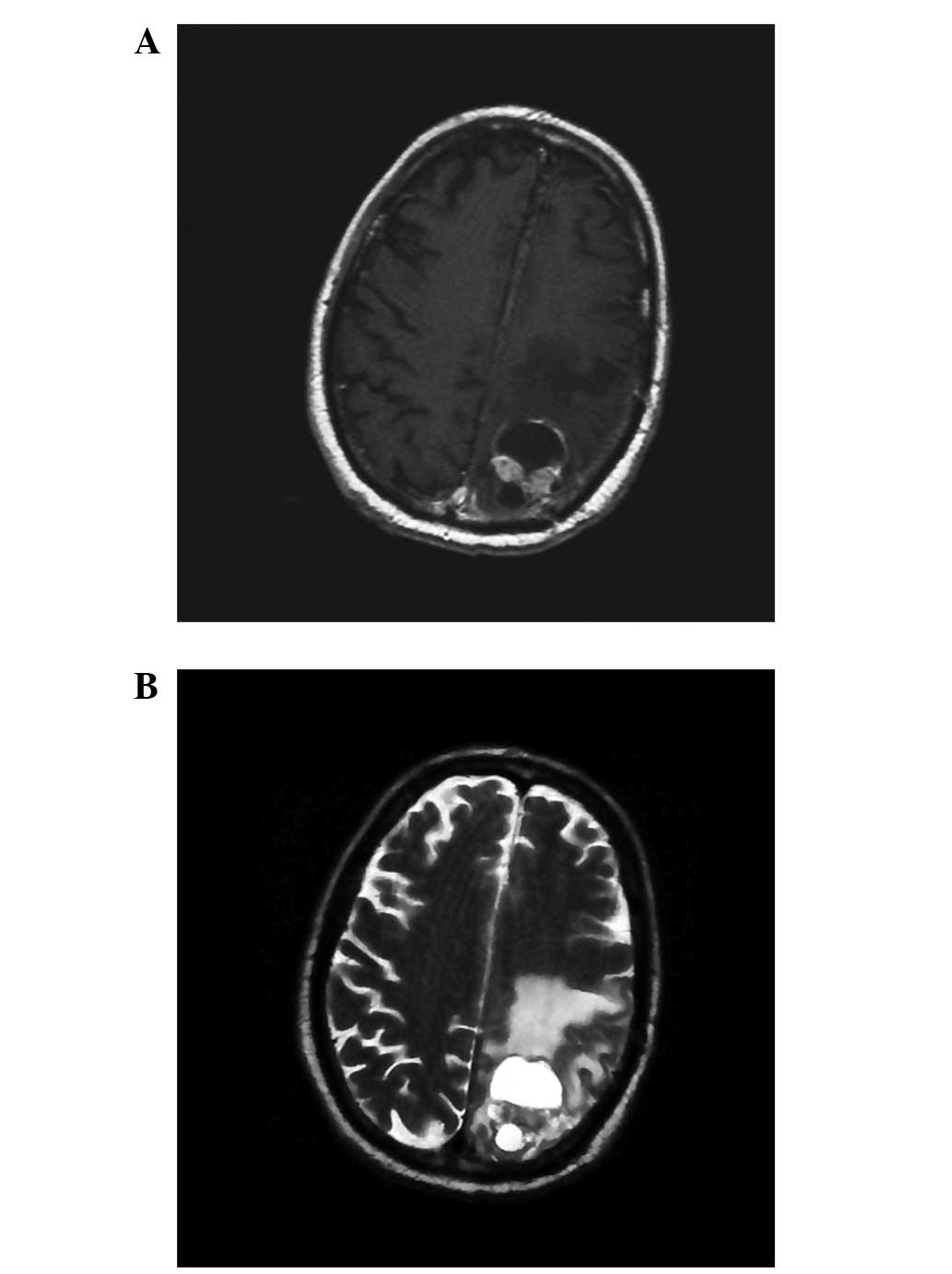
An imaging work-up included computerized tomography
(CT) scanning and brain magnetic resonance imaging (MRI), which
indicated a low-density, contrast-enhancing subcortical lesion that
was localized in the proximity of the left motor area, with
perifocal edema and flattened sulci (Fig. 1). Whole-body completion CT scans
were uneventful, thus leading to the diagnosis of a high-grade,
primitive glial neoplasm.
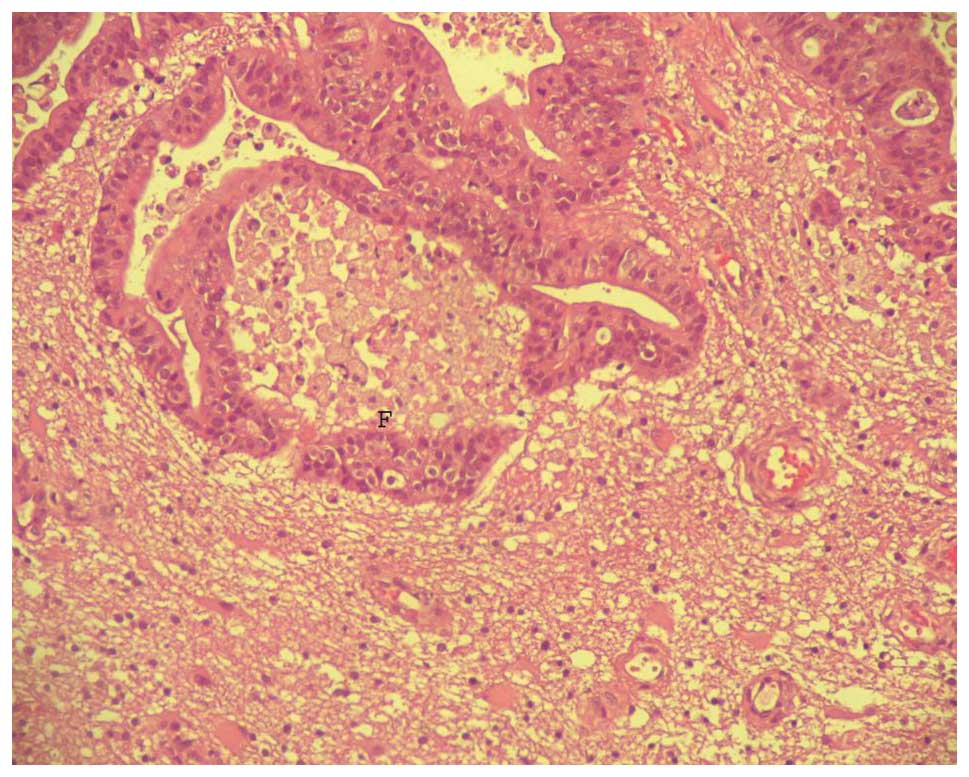
The patient underwent microsurgical resection of the
mass via a trans-sulcal approach. The histology was conclusive for
a well-differentiated adenocarcinoma (Fig. 2). The staining pattern obtained
following immunochemical analysis suggested a primary tumor arising
from the digestive tract [thyroid transcription factor 1-negative
(TTF1−) and carcinoembryonic antigen-positive
(CEA+)].
Once discharged, the patient was scheduled for a
complete oncological work-up that included a whole-body positron
emission tomography (PET) scan and digestive tract endoscopy. The
esophagogastroduodenoscopy revealed a flat, whitish area extending
for ~2 cm in the longitudinal axis lying on the lower third of the
thoracic esophagus, extending to the submucosa. No evidence of
enlarged regional lymph nodes was present (cT2N0M1). The patient
refused further surgical procedures and was scheduled for
whole-brain and local radiotherapy and chemotherapy treatments. The
protocol that was used consisted of a fractionated 50 Gy dose (2
Gy/day) and concurrent chemotherapy, including paclitaxel and
cisplatin. An antiblastic therapy protocol was accomplished with a
favorable course, despite an episode of non-fatal toxicity
occurring subsequent to 2 months (transient leukopenia and
pneumonia).
At the last follow-up at 14 months post-surgery, the
patient was alive and well (Karnofsky index, >90). A
neurological examination revealed amelioration of the motor
function of the right hand and arm, with a positive impact on the
quality of life physical domain, in spite of the development of a
minor depressive syndrome. The patient was alive at 16 months after
the initial diagnosis and, to date, no local or distant tumor
recurrence has been documented.
Discussion
The diagnosis of a brain metastasis is usually made
during the routine follow-up examinations of patients with a known
type of cancer. In the case of a CUP presenting with brain
metastases, either a neurosurgeon or a neurologist are consulted
prior to the oncologist. The incidence of brain metastasis of
unknown primary origin is almost equal to that of cerebral
metastases where the primary cancer is known (1,7).
Moreover, a CUP will remain unknown for a period of time for the
majority of the cases despite complete radiological and
instrumental assessments (7).
Common contrast-enhancing malignant tumors of the
brain are glioblastoma multiforme (GBMs), anaplastic astrocytomas
(AAs), metastases and lymphomas, all of which are often
characterized by similar conventional CT and MRI findings (8). However, metastatic tumors of the brain
may exhibit different signal intensities on diffusion-weighted MRI
(DWI) depending on their histology and cellularity. In fact, the
signal intensity on DWI may predict the histology of the metastases
(9), since well-differentiated
adenocarcinomas tend to be hypointense, while small and large cell
neuroendocrine tumors usually show hyperintensity (9,10).
However, a study by Takeshima et al(11) suggested that the MRI findings of a
cystic tumor with a thin enhancing rim may alert the clinician to
the possibility of a metastatic brain tumor from the esophagus,
particularly when a high-risk population is considered.
Patients with a newly detected brain mass and no
history of other tumors, usually undergo extensive and expensive
diagnostic testing to identify the primary neoplasm prior to the
selection of a biopsy site. In this situation, a neurosurgical
procedure may be considered as the most appropriate step to be
taken in order to provide a definitive diagnosis, and also to avoid
the unnecessary waste of time and resources. By contrast, it should
be noted that esophageal cancer often lacks distinctive
morphological characteristics leading to the potential unsuccessful
identification of the site of origin by routine histological
examination (12). Therefore,
routine cancer screenings, such as whole-body PET and conventional
diagnostic modalities (CT and/or MRI), are of fundamental value in
detecting unknown primary tumors in inaccessible locations
(13).
Esophageal cancer is a highly lethal disease with an
extremely poor 5-year survival rate regardless of the stage of the
disease. In 2008, esophageal cancer had an estimated annual
incidence rate of 19.2/100,000 for males and 4.2/100,000 for
females, who are exposed to a lower risk compared with males
(14). At the time of diagnosis,
~50% of patients have metastatic disease and the majority of
patients with localized esophageal cancer will develop metastases,
despite potentially curative local therapy. The most common sites
of distant recurrence, in order of frequency, are the lymph nodes
(45%), liver (35%), lung (20%), cervical/supraclavicular lymph
nodes (18%), bone (10%), adrenal (5%) and peritoneum (2%), while
the incidence of brain metastasis is only 1.5% (15). Brain metastases have been reported
in only 1.7–3.6% of all patients with different types of esophageal
cancer (4,5,15).
Patients with metastatic esophageal cancer have a median survival
time of 6 months. The median patient age at the time of the
diagnosis of brain metastasis was >60 years. The longest median
survival time observed following the diagnosis of brain metastasis
(9.6 months) occurred in patients with single brain lesions who
underwent resection and received whole-brain radiotherapy (16,17).
There was a trend toward a worse survival in
patients with liver metastases and patients in recursive
partitioning analysis (RPA) class II–III vs. RPA class I. Moreover
the reported 5-year survival rate ranges from 20 to 36% subsequent
to intentionally curative surgery due to a high rate of either
local or distant recurrence. The distant metastasis rate has been
reported to be 26% within 20 months after radical surgery.
Hematoxylin and eosin staining is one of the most effective
predictors of survival in esophageal cancer due to the number of
lymph node metastases detected using this technique (18,19).
The case reported in the present study is
exceptional due to the patient’s prolonged, disease-free survival,
the excellent response (to date) to non-surgical treatment of the
primary disease and the clinical presentation resembling a brain
glioma, which made the post-operative search for the primary tumor
a challenge. Radical surgery on the brain lesion, even though
located in an eloquent area, resulted in improvement to the
presenting neurological deficits and represented the basis for a
proper oncological assessment and successful management.
Esophageal carcinoma rarely presents with an
isolated brain metastasis. In such cases, other than a careful
assessment aimed to discover the unknown primary origin, removal of
the lesion must be considered in order to treat the presenting
symptoms and obtain a rapid histological diagnosis. Further studies
are warranted in order to assess whether progression of the primary
disease may be accelerated by post-surgical stress. This hypothesis
should also be investigated against the potential benefits in terms
of an improved quality of life and the advantages of a shorter
diagnostic time.
References
|
1
|
Mueller WC, Spector Y, Edmonston TB, et
al: Accurate classification of metastatic brain tumors using a
novel microRNA-based test. Oncologist. 16:165–174. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Campos S, Davey P, Hird A, et al: Brain
metastasis from an unknown primary, or primary brain tumour? A
diagnostic dilemma. Curr Oncol. 16:62–66. 2009.PubMed/NCBI
|
|
3
|
Torek F: The operative treatment of
carcinoma of the oesophagus. Ann Surg. 61:384–405. 1915. View Article : Google Scholar
|
|
4
|
Smith RS and Miller RC: Incidence of brain
metastasis in patients with esophageal carcinoma. World J
Gastroenterol. 17:2407–2410. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Agrawal R, Shukla P, Shukla V and Chauhan
A: Brain metastasis from esophageal carcinoma. J Cancer Res Ther.
5:137–139. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ogawa K, Toita T, Sueyama H, et al: Brain
metastases from esophageal carcinoma: natural history, prognostic
factors, and outcome. Cancer. 94:759–764. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Pavlidis N and Fizazi K: Carcinoma of
unknown primary (CUP). Crit Rev Oncol Hematol. 69:271–278. 2009.
View Article : Google Scholar
|
|
8
|
Spallone A, Nardi R and Silipo P:
Diagnosis of pineal area tumors using computer tomography. Zh Vopr
Neirokhir Im N N Burdenko. 6:16–20. 1980.(In Russian).
|
|
9
|
Maier SE, Sun Y and Mulkern RV: Diffusion
imaging of brain tumors. NMR Biomed. 23:849–864. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Hayashida Y, Hirai T, Morishita S, et al:
Diffusion-weighted imaging of metastatic brain tumors: comparison
with histologic type and tumor cellularity. AJNR Am J Neuroradiol.
27:1419–1425. 2006.PubMed/NCBI
|
|
11
|
Takeshima H, Kuratsu J, Nishi T, et al:
Metastatic brain tumours from esophageal carcinoma: neuro-imaging
and clinicopathological characteristics in Japanese patients. Acta
Neurochir (Wien). 143:31–36. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Giordana MT, Cordera S and Boghi A:
Cerebral metastases as first symptom of cancer: a
clinico-pathologic study. J Neurooncol. 50:265–273. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Regelink G, Brouwer J, de Bree R, et al:
Detection of unknown primary tumours and distant metastases in
patients with cervical metastases: value of FDG-PET versus
conventional modalities. Eur J Nucl Med Mol Imaging. 29:1024–1030.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lambert R: Endoscopy in screening for
digestive cancer. World J Gastrointest Endosc. 4:518–525. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Rice TW, Khuntia D, Rybicki LA, et al:
Brain metastases from esophageal cancer: a phenomenon of adjuvant
therapy? Ann Thorac Surg. 82:2042–2049. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Go PH, Klaassen Z, Meadows MC and
Chamberlain RS: Gastrointestinal cancer and brain metastasis: a
rare and ominous sign. Cancer. 117:3630–3640. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Posner MC, Forastiere AA and Minsky BD:
Cancer of the esophagus. Cancer Principles & Practice of
Oncology. De Vita VT Jr, Hellman S and Rosenberg SA: 7th edition.
Lippincott Williams & Wilkins; Philadelphia: pp. 861–909.
2005
|
|
18
|
Takeno S, Yamashita SI, Yamamoto S, et al:
Number of metastasis-positive lymph node stations is a simple and
reliable prognostic factor following surgery in patients with
esophageal cancer. Exp Ther Med. 4:1087–1091. 2012.
|
|
19
|
Waterman TA, Hagen JA, Peters JH,
DeMeester SR, Taylor CR and Demeester TR: The prognostic importance
of immunohistochemically detected node metastases in resected
esophageal adenocarcinoma. Ann Thorac Surg. 78:1161–1169. 2004.
View Article : Google Scholar : PubMed/NCBI
|