Introduction
External beam radiotherapy (EBRT) is one of the most
commonly used primary treatment modalities for prostate cancer
(1). However, 24–80% of patients with
high-risk prostate cancer experience biochemical relapse after
definitive EBRT with or without androgen deprivation therapy
(2–7).
Current salvage therapies following primary EBRT include
prostatectomy, cryosurgery, brachytherapy and high-intensity
focused ultrasound (8). Although
salvage prostatectomy has resulted in promising outcomes, it is
generally recommended that it be considered only in young patients
without comorbidities and with low-risk prostate cancer. When a
patient presents with recurrent prostate cancer following
definitive EBRT and is deemed unfit for salvage prostatectomy, the
most appropriate management strategy is difficult to determine due
to the numerous limitations of current salvage therapies (9). Salvage re-irradiation for recurrent
prostate cancer after primary EBRT has been limited due to toxicity
to adjacent organs, particularly the rectum and bladder (10). Although, certain recent studies have
reported the effectiveness and safety of re-irradiation with
brachytherapy for locally relapsed prostate cancer, reports of
re-irradiation using EBRT are scarce (11,12). Thus,
in the present study, two cases of locally relapsed prostate cancer
following EBRT treated with re-irradiation using helical
tomotherapy are discussed. The present study was approved by the
ethics committee of Kyung Hee University Medical Center (Seoul,
Republic of Korea).
Case report
Case 1
A 68-year-old male with a prostate-specific antigen
(PSA) level of 15 ng/ml underwent a prostate biopsy and was
diagnosed with localized prostate cancer with a Gleason score of
2+3 in October 2004. Prostate magnetic resonance imaging (MRI) and
a bone scan showed organ confined prostate cancer. After a thorough
consultation with the patient, he decided to undergo EBRT due to a
history of cerebral infarction. A total dose of 72 Gy in 40
fractions was delivered to the prostate gland. After completion of
definitive EBRT, he complained of mild urinary urgency and
frequency, but these symptoms were controlled with anticholinergic
agents. Seventeen months following completion of EBRT, the
patient's PSA level decreased to 0.8 ng/ml. However, in April 2007
(2 years and 3 months after EBRT) his PSA level increased to 1.37
ng/ml, therefore, a repeat prostate biopsy was performed. Prostate
cancer with a Gleason score of 3+3 was diagnosed in one of eight
cores. Prostate MRI and PET-CT revealed no distant metastasis or
extra-prostatic tumor invasion. As the patient refused to undergo a
salvage prostatectomy, intermittent androgen deprivation therapy
was administered for 6 years. In 2013 (8 years and 6 months after
the initial diagnosis), during the resting period the patient's PSA
level reached 5.35 ng/ml within only 6 months. The patient
underwent a further prostate biopsy and 2 out of 12 cores showed
adenocarcinoma with a Gleason score of 4+4. However, prostate MRI
and a bone scan did not show periprostatic invasion or distant
metastasis. After a thorough consultation, the patient decided to
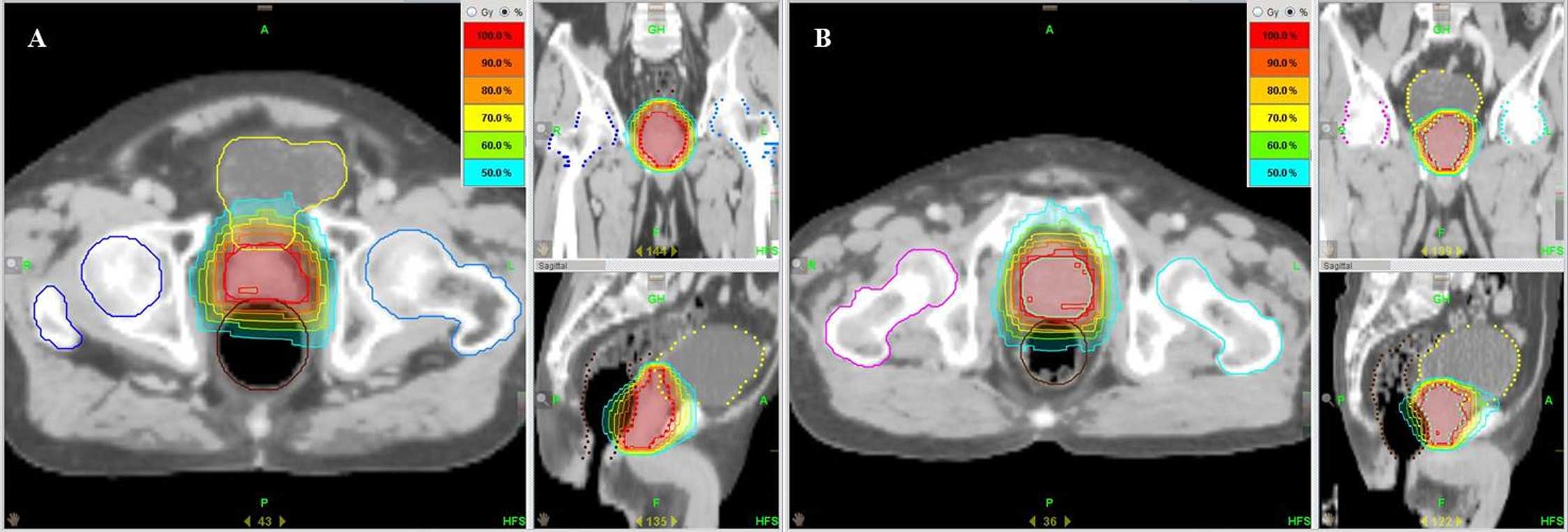
undergo tomotherapy. A total dose of 66 Gy in 30 fractions was
administered using tomotherapy (Fig.
1A). Following tomotherapy, the patient's PSA level decreased
to nadir and he did not experience any urologic problems.
Furthermore, there have been no rectal complications thus far.
Case 2
A 71-year-old male with a PSA level of 8.7 ng/ml was
diagnosed with Gleason score 3+3 prostate cancer in November 2006.
Extra-prostatic cancer was not detected by further imaging studies.
The patient received EBRT as he refused a radical prostatectomy. A
total dose of 77.4 Gy in 43 fractions was administered. Two years
after EBRT, his PSA level decreased to 1.4 ng/ml. However, it began
to increase and in January 2010 (2 years and 11 months after EBRT)
reached 2.6 ng/ml. The patient underwent repeat prostate biopsy,
which showed remaining cancer cells. A total dose of 69 Gy in 30
fractions was administered using tomotherapy (Fig. 1B). During the 4 years after
tomotherapy, the PSA level did not increase from nadir and no
rectal or urinary complications were reported.
Discussion
Salvage RT for cancer relapse after radical
prostatectomy is an attractive option as the possible complications
of RT associated with gastrointestinal (GI) or genitourinary (GU)
toxicity are minimal, as described in a previous study (10). However, salvage reirradiation is
considered a relative contraindication for recurrent prostate
cancer after definitive EBRT (10).
Recently Kishi et al (9)
reported a case of salvage brachytherapy for recurrent prostate
cancer after definitive EBRT. To minimize rectal toxicity, they
used a bolus injection of native-type hyaluronic acid gel, which
yielded promising oncologic and functional results. In another
retrospective study of 37 patients who received salvage
brachytherapy after definitive EBRT for prostate cancer, Aaronson
et al (13) reported that
brachytherapy provided prostate cancer control with an acceptable
rate of complications. In their study, 10 patients experienced GI
or GU complication. Functional outcomes and complications,
especially GI and GU complications, following radiation therapy are
graded from 1 to 4 (14). Only one
patient experienced grade 3 rectal hemorrhage, while others
experienced grade 2 complications that were managed conservatively.
A similar study of 15 patients, who underwent brachytherapy for the
treatment of recurrence after definitive EBRT, showed a biochemical
relapse-free survival rate of 60.2% 3 years after salvage
brachytherapy and all acute adverse events were grade 1 or 2
(12). Furthermore, Ramey and
Marshall (15) investigated 18
previous studies of salvage brachytherapy and concluded that
brachytherapy is a reasonable salvage option for patients with
local recurrence after primary EBRT for prostate cancer. Thus,
according to previous studies of salvage brachytherapy, which
described good oncologic outcomes with a tolerable rate of
complications, salvage RT using brachytherapy is an acceptable
treatment modality for the treatment of recurrent prostate cancer
after definitive EBRT.
Helical tomotherapy, one of the newest conformal RT
modalities, employs helical intensity-modulated RT in which a
gantry 6-MV linear accelerator rotates continuously 360° around the
patient emitting tens of thousands of narrow beamlets providing an
integrated megavoltage computed tomography unit that permits
real-time verification of the patient's position during CT
stimulation and treatment. Helical tomotherapy planning has
numerous advantages, including a more conformal dose distribution
and decreased radiation dose to normal structures. Low rates of GI
and GU toxicity were observed in our previous study of 70 patients
with localized prostate cancer treated with hypofractionated
helical tomotherapy (16). In that
study, all complications of the GI and GU tracts were grade 0, 1 or
2, and either resolved spontaneously or could be managed with
medication or simple procedures, such as argon plasma coagulation.
In the present study, neither of the cases experienced
complications greater than grade 3. In case 1, analysis of dose
volume histograms (DVHs) for the initial and salvage RT plans
indicated that <50% of the rectal volume received >75 Gy,
with <10% receiving >120 Gy, and <5% receiving >130 Gy.
The DVHs also showed that <50% of the bladder volume received
>75 Gy, <10% received >100 Gy, and <5% received >115
Gy. In case 2, analysis of DVHs for the initial and salvage RT
plans showed that <50% of the rectal volume received >70 Gy,
with <10% receiving >110 Gy, and <5% receiving >120 Gy.
The DVHs also showed that <50% of the bladder volume received
>70 Gy, <10% received >110 Gy, and <5% received >125
Gy. Radiation doses to the rectum and bladder of these two patients
were high considering the tolerance dose of these organs. However,
doses delivered by helical tomotherapy to 50% of the rectal volume
were only 8.8 Gy and 2.7 Gy for case 1 and case 2, respectively and
the doses delivered to 50% of the bladder volume were 5.2 Gy and
2.2 Gy for case 1 and case 2, respectively. Furthermore, time
intervals from the first and second EBRT were 8 years 4 months and
3 years 4 months, respectively, which should have been enough time
to recover from mild complication following initial RT. To the best
of our knowledge, there is only one study regarding reirradiation
using EBRT. Vavassori et al (11) reported cases of reirradiation using
CyberKnife® for locally recurrent prostate cancer after primary
EBRT (median dose of 80 Gy). A total dose of 30 Gy in 5 fractions
was administered, and no patients experienced severe urinary or
rectal toxicity. Therefore, if it is possible to use a high
precision RT technique, salvage EBRT can be considered an
appropriate treatment option for locally recurrent prostate
cancer.
In conclusion, reirradiation was performed for
prostate cancer using helical tomotherapy, which resulted in a
promising outcome without urologic or rectal complications. Thus,
it suggests that helical tomotherapy may be a safe and effective
salvage treatment modality for locally recurrent prostate cancer
following definitive EBRT.
References
|
1
|
Grimm P, Billiet I, Bostwick D, Dicker AP,
Frank S, Immerzeel J, Keyes M, Kupelian P, Lee WR, Machtens S, et
al: Comparative analysis of prostate-specific antigen free survival
outcomes for patients with low, intermediate and high risk prostate
cancer treatment by radical therapy. BJU Int. 109:22–29. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Roach M III, Bae K, Speight J, Wolkov HB,
Rubin P, Lee RJ, Lawton C, Valicenti R, Grignon D and Pilepich MV:
Short-term neoadjuvant androgen deprivation therapy and
external-beam radiotherapy for locally advanced prostate cancer:
Long-term results of RTOG 8610. J Clin Oncol. 26:585–591. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bolla M, Collette L, Blank L, Warde P,
Dubois JB, Mirimanoff RO, Storme G, Bernier J, Kuten A, Sternberg
C, et al: Long-term results with immediate androgen suppression and
external irradiation in patients with locally advanced prostate
cancer (an EORTC study): A phase III randomised trial. Lancet.
360:103–106. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Horwitz EM, Bae K, Hanks GE, Porter A,
Grignon DJ, Brereton HD, Venkatesan V, Lawton CA, Rosenthal SA,
Sandler HM, et al: Ten-year follow-up of radiation therapy oncology
group protocol 92-02: A phase III trial of the duration of elective
androgen deprivation in locally advanced prostate cancer. J Clin
Oncol. 26:2497–2504. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Pilepich MV, Winter K, Lawton CA, Krisch
RE, Wolkov HB, Movsas B, Hug EB, Asbell SO and Grignon D: Androgen
suppression adjuvant to definitive radiotherapy in prostate
carcinoma-long-term results of phase III RTOG 85-31. Int J Radiat
Oncol Biol Phys. 61:1285–1290. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Denham JW, Steigler A, Lamb DS, Joseph D,
Turner S, Matthews J, Atkinson C, North J, Christie D, Spry NA, et
al: Short-term neoadjuvant androgen deprivation and radiotherapy
for locally advanced prostate cancer: 10-year data from the TROG
96.01 randomised trial. Lancet Oncol. 12:451–459. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
D'Amico AV, Manola J, Loffredo M, Renshaw
AA, DellaCroce A and Kantoff PW: 6-month androgen suppression plus
radiation therapy vs radiation therapy alone for patients with
clinically localized prostate cancer: A randomized controlled
trial. JAMA. 292:821–827. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Heidenreich A, Bastian PJ, Bellmunt J,
Bolla M, Joniau S, van der Kwast T, Mason M, Matveev V, Wiegel T,
Zattoni F and Mottet N: European Association of Urology: EAU
guidelines on prostate cancer. Part II: Treatment of advanced,
relapsing and castration-resistant prostate cancer. Eur Urol.
65:467–479. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kishi K, Sato M, Shirai S, Sonomura T and
Yamama R: Reirradiation of prostate cancer with rectum
preservation: Eradicative high-dose-rate brachytherapy with natural
type hyaluronate injection. Brachytherapy. 11:144–148. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Zelefsky MJ, Levin EJ, Hunt M, Yamada Y,
Shippy AM, Jackson A and Amols HI: Incidence of late rectal and
urinary toxicities after three-dimensional conformal radiotherapy
and intensity-modulated radiotherapy for localized prostate cancer.
Int J Radiat Oncol Biol Phys. 70:1124–1129. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Vavassori A, Jereczek-Fossa BA, Beltramo
G, De Cicco L, Fariselli L, Bianchi LC, Possanzini M, Bergantin A,
DeCobelli O and Orecchia R: Image-guided robotic radiosurgery as
salvage therapy for locally recurrent prostate cancer after
external beam irradiation: Retrospective feasibility study on six
cases. Tumori. 96:71–75. 2010.PubMed/NCBI
|
|
12
|
Shimbo M, Inoue K, Koike Y, Katano S and
Kawashima K: Salvage I seed implantation for prostate cancer with
postradiation local recurrence. Urol Int. 90:294–300. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Aaronson DS, Yamasaki I, Gottschalk A,
Speight J, Hsu IC, Pickett B, Roach M III and Shinohara K: Salvage
permanent perineal radioactive-seed implantation for treating
recurrence of localized prostate adenocarcinoma after external beam
radiotherapy. BJU Int. 104:600–604. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Budäus L, Bolla M, Bossi A, Cozzarini C,
Crook J, Widmark A and Wiegel T: Functional outcomes and
complications following radiation therapy for prostate cancer: A
critical analysis of the literature. Eur Urol. 61:112–127. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ramey SJ and Marshall DT: Re-irradiation
for salvage of prostate cancer failures after primary radiotherapy.
World J Urol. 31:1339–1345. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kong M, Hong SE and Chang SG:
Hypofractionated helical tomotherapy (75 Gy at 2.5 Gy per fraction)
for localized prostate cancer: long-term analysis of
gastrointestinal and genitourinary toxicity. Onco Targets Ther.
7:553–566. 2014. View Article : Google Scholar : PubMed/NCBI
|