Introduction
Colorectal cancer (CRC) is the third most common
cancer and the fourth most common cause of cancer-related mortality
worldwide. The most common curative therapy for colon cancer is
surgical resection. The survival rate of CRC patients correlates
with tumor stage and the 5-year relative survival is approximately
65% (1). However, patients with
advanced disease with unresectable metastatic lesions have a 5-year
survival of approximately 5% (1,2).
Several issues remain unsolved. For instance, effective treatment
modalities are rare in cases of patients with peritoneal
carcinomatosis, chemotherapy-resistant tumors and poor performance
status. Therefore, novel treatment modalities for such cases are
required.
Photodynamic therapy (PDT) was introduced
approximately 35 years ago. PDT consists of: systemic or topical
administration of a photosensitizer or metabolic precursor,
photoexcitation of the sensitizer by light in the visible
wavelength (400–750 nm) and tumor cell death induced by the release
of reactive oxygen species (ROS) (3,4). PDT
provides better selectivity for the targeting of tumors compared to
conventional chemo-and radiotherapy due to the preferential
accumulation of photosensitizers in tumors (3,4).
Photofrin® (Porfimer sodium) has received worldwide
regulatory approval as a photosensitizer and was the basis for the
growth of oncologic PDT (3,4). However, Photofrin requires
approximately 6 weeks of photosensitivity precautions (4). This side-effect has limited its use as
a photosensitizer for PDT.
Protoporphyrin IX (PpIX), synthesized from
5-aminolevulinic acid (ALA) in the mitochondria, is an intrinsic
and safe photosensitizer (3–5). PpIX
accumulates in several malignant tumors following 5-ALA
administration. This phenomenon is widely applicable for
photodynamic diagnosis (PDD) and PDT (3–5).
Recently, we reported the utility of lymph node metastasis
detection using 5-ALA administration in mouse models (6). One of the main advantages of ALA-PDT
is that PpIX is cleared from the body within 24–48 h subsequent to
systemic ALA administration (4).
Furthermore, 5-ALA is an endogenous agent that is part of the
regular diet. Therefore, ALA-PDT has the potential to avoid the
risk of prolonged phototoxicity associated with the conventional
photosensitizer, Photofrin (4).
ALA-PDT has been performed using lasers as light
sources at 635 nm. However, since lasers are large, complex and
expensive, PDT has not been widely used in clinical treatment. Over
the past decade, light-emitting diodes (LEDs), which are
inexpensive, stable, easy to operate, require little maintenance
and provide wide area illumination fields, have been used in PDT
instead of lasers (7,8). Therefore, ALA-PDT using LEDs has the
potential to rapidly become a useful treatment modality.
ALA-PDT is non-invasive and may be used in repeated
treatments and in combination with surgery, chemo- and radiotherapy
or other modalities. Over the past decade, investigators have
reported the effects of ALA-PDT in various tumor cells (9–16). In
dermatology, multicenter randomized controlled studies have
demonstrated the high efficacy of topical ALA-PDT for actinic
keratosis, Bowen’s disease and superficial basal cell carcinoma
(17–19). Although certain reports have
addressed the efficacy of ALA-PDT in CRC cells (20,21),
these were limited to in vitro studies. Therefore, the
objective of this study was to investigate the antitumor effect of
ALA-PDT using LEDs for the treatment of CRC cells in a xenograft
mouse model.
Materials and methods
Cell line and cell culture
The HT-29 human CRC cell line was purchased from the
American Type Culture Collection (Rockville, MD, USA). HT-29 cells
were grown in McCoy’s medium with 10% fetal bovine serum (FBS), 100
U/ml penicillin and 100 μg/ml streptomycin at 37°C in a
water-saturated atmosphere with 5% CO2/95% air.
Animals
Four-week-old female BALB/c mice were used in this
study. The mice were housed in groups, in plastic cages with
stainless-steel grid tops in an air-conditioned environment with a
12-h light-dark cycle and were provided with food and water ad
libitum. The animal experiments were conducted in accordance
with the institutional guidelines of the Kyoto Prefectural
University of Medicine, Kyoto, Japan.
Cancer-bearing mouse model
HT-29 cells (0.5×106) were inoculated
subcutaneously in 100 μl of phosphate-buffered saline (PBS) into
the flanks of nude mice under general anesthesia. One week later,
the longest diameter of the xenograft tumor was between 3 and 5 mm.
The mice were then divided into a treatment and a control group.
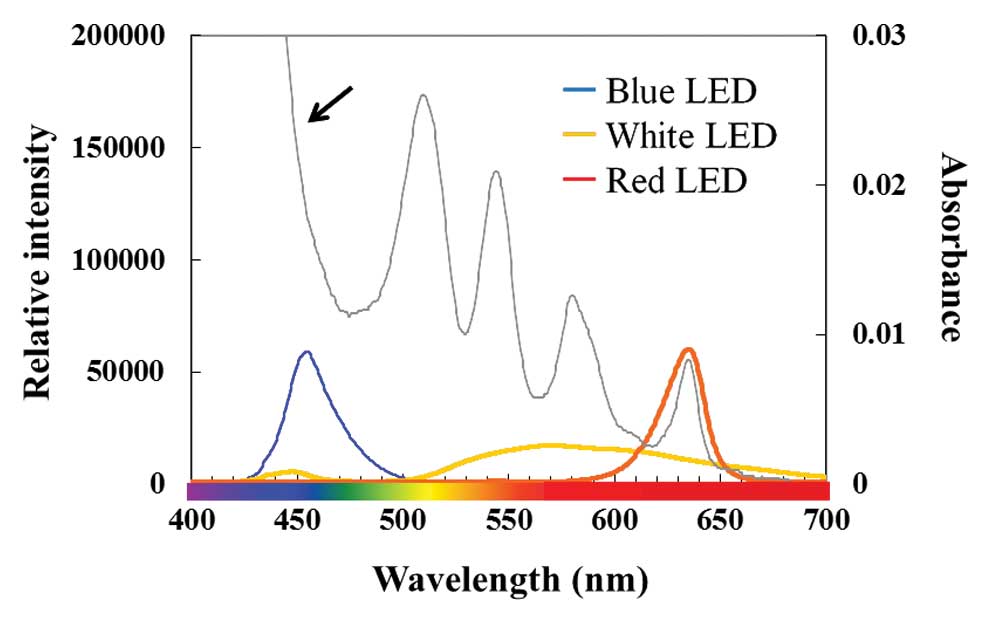
The treatment group consisted of 3 subgroups: the blue LED (peak
wavelength, 456 nm), the white LED and the red LED (635 nm) groups
(Fig. 1). These LED irradiation
units were provided by SBI Pharmaceuticals Co., Ltd. (Tokyo,
Japan). The control group and treatment subgroups comprised 6 mice
each.
Light sources for photodynamic
therapy
Cultured cell plates and inoculated mice were
exposed to the 3 types of LED lights (Fig. 1). Light intensity was measured using
a photo-radiometer.
Photodynamic therapy in vitro
HT-29 cells (5×104 cells/0.1 ml) were
seeded in 96-well plates and placed in an incubator at 37°C for 24
h. The medium was then replaced with medium containing 1 mM 5-ALA
(Cosmo Bio International, Tokyo, Japan) (6,15).
Three hours later, the 5-ALA-containing medium was replaced with
PBS. Cells were irradiated with 3 types of LED at a measured
fluence rate of 16 mW/cm2 and fluence of 3.0
J/cm2. PBS was replaced with fresh medium immediately
subsequent to irradiation. The control group was not exposed to ALA
administration or LED irradiation. Twenty-four hours later, cell
viability was determined using the
3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT)
assay (15). Sample absorbances
were read on a MaxLine Microplate Reader equipped with a 550-nm
filter. Five separate experiments were performed.
Photodynamic therapy in vivo
Nude mice in the treatment group received an
intraperitoneal injection of 250 mg/kg of 5-ALA (6,16).
Five hours later, mice were irradiated with LEDs at a measured
fluence rate of 96 mW/cm2 and fluence of 32
J/cm2. The 3 types of LEDs described above were used in
this study. The control group was not exposed to ALA administration
or LED irradiation. ALA-PDT was repeated 3 times at weekly
intervals. Three weeks after the initial treatment, the mice were
sacrificed under general anesthesia and tumors were removed
(16). Removed tumor weights were
measured (16).
Statistical analysis
Differences in tumor weight and cell viability among
the groups were analyzed using the non-parametric Mann-Whitney U
test. P<0.05 was considered to indicate a statistically
significant difference.
Results
Efficacy of ALA-PDT using LEDs for the
treatment of CRC in vitro
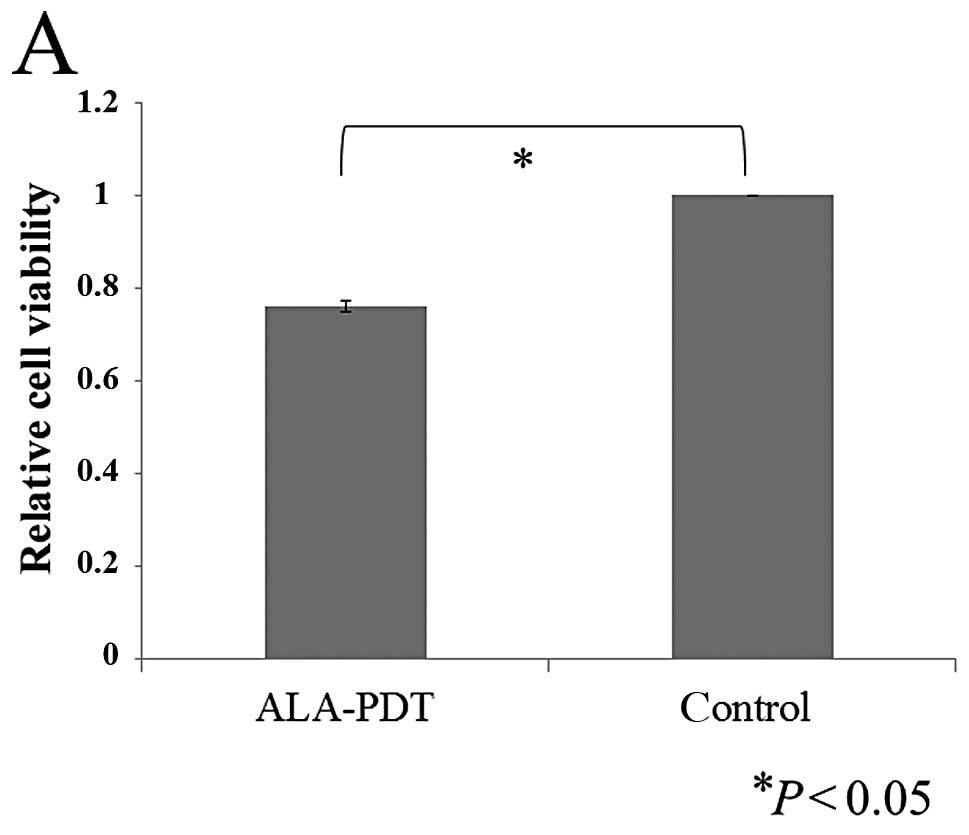
First, the efficacy of ALA-PDT in the HT-29 cell
line was evaluated. Red LEDs (peak wavelength, 635 nm) were used in
this study since 635 nm is applied for conventional ALA-PDT
(4). The cell viability of HT-29
cells was significantly lower in the group treated with ALA-PDT
using red LED compared to the control group (P<0.05) (Fig. 2A). Moreover, increasing light doses
resulted in significant reductions in cell viability (Fig. 2B). These results indicate that
ALA-PDT using red LEDs is effective in treating human colon cancer
cells and that the antitumor effects are dependent on fluence.
Types of LEDs that are most suitable for
ALA-PDT in HT-29
Fig. 1 shows the
correlation between the absorption spectrum for PpIX and emission
spectrum of the 3 types of LEDs. For the absorption spectrum of
PpIX, there is a maximum peak at 410 nm and smaller peaks near 510,
545, 580 and 630 nm. Therefore, we used blue (peak wavelength, 456
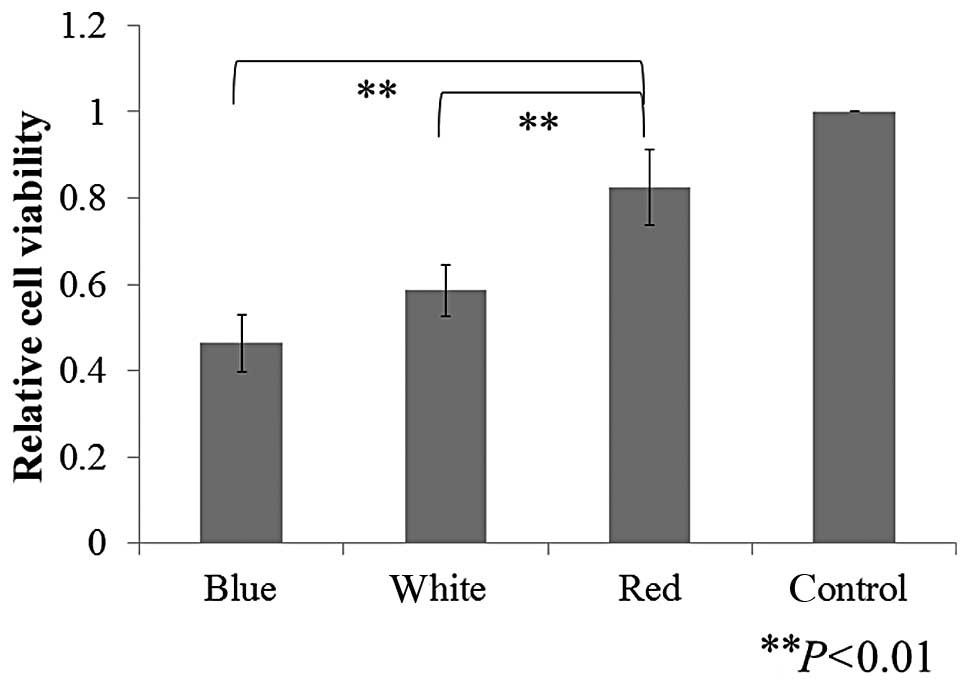
nm), white and red (635 nm) LEDs. Cell viability was significantly
lower in the treatment groups compared to the control group
(Fig. 3). The blue and white LEDs
showed greater antitumor effects compared to the red LEDs (Fig. 3). This result indicates that blue
and white LEDs are potential light sources for ALA-PDT in human
colon cancer cells.
Antitumor effect of ALA-PDT using LEDs in
a CRC-bearing mouse model
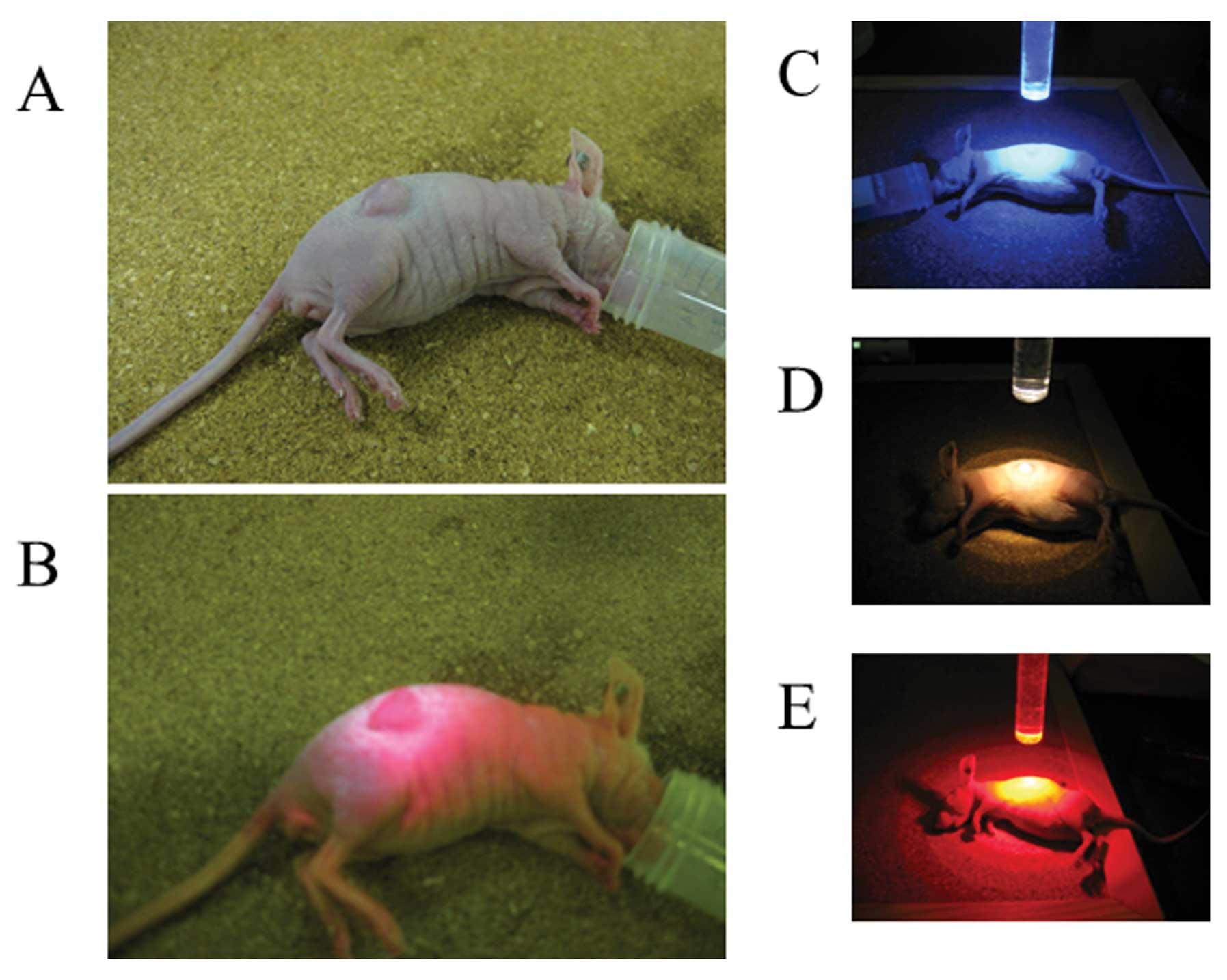
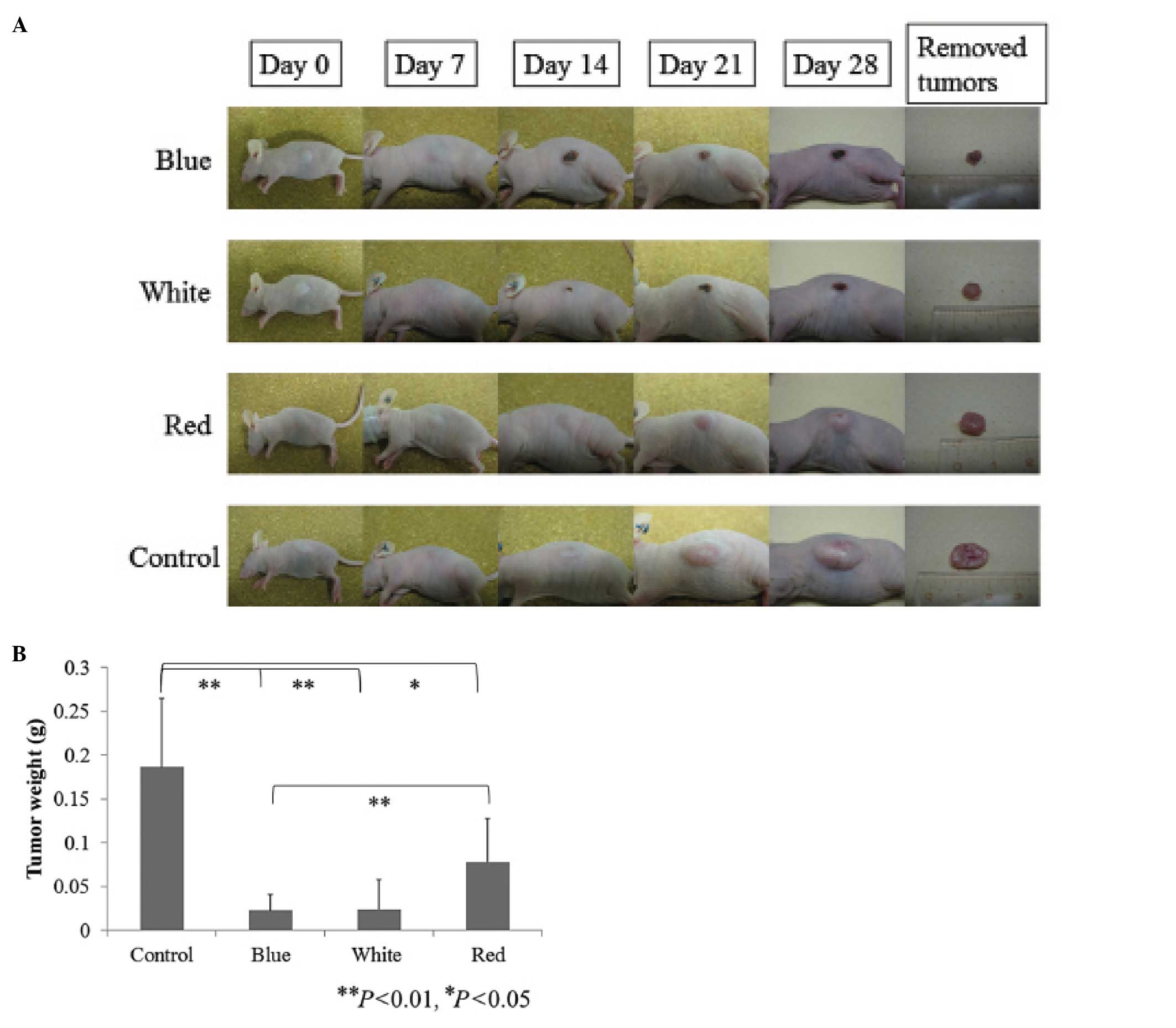
Fig. 4 shows the
experimental procedure of ALA-PDT using LEDs in a CRC-bearing mouse
model. Five hours subsequent to 5-ALA administration, tumors were
detected as red fluorescence using ALA-PDD (Fig. 4B). Tumor growth was clearly
suppressed in the treatment groups (Fig. 5A). Tumor weights were significantly
lower in the treatment groups compared to the control group
(Fig. 5B). In the blue and white
LED groups, the tumor inhibition rates were approximately 88% to
those of the control group (Fig.
5B). Similar to the in vitro study, the antitumor
effects of ALA-PDT using blue or white LEDs varied significantly
from those with red LEDs (Fig. 5B).
These results indicate that ALA-PDT using LEDs, particularly blue
or white, is a potentially effective treatment modality for human
colon cancer cells.
Discussion
In this study, ALA-PDT using 3 types of LEDs
demonstrated significant antitumor effects in vitro and
in vivo. ALA-PDT using blue or white LEDs was more effective
compared to the conventional red LEDs. These results suggest that
ALA-PDT using LEDs, particularly blue or white, is a potential
novel treatment modality for human CRC cells.
In general, lasers are used as light sources in
ALA-PDT. Over the past decade, the efficacy of LEDs for ALA-PDT has
been reported (7,9,22). In
this study, we demonstrated the efficacy of LEDs as a light source
for ALA-PDT in human colon cancer cells. Since LEDs have several
advantages, such as being smaller, easier to use, and more
cost-effective compared to lasers, they may soon be widely used as
a novel light source for ALA-PDT in human colon cancer cells.
In the majority of cases where ALA-PDT is used for
the treatment of various types of cancer, a laser emitting 630 nm
is usually used (17–19,23).
However, the most effective wavelength for ALA-PDT in human CRC
cells has not yet been fully evaluated. Our in vivo study
suggests that ALA-PDT using blue or white LEDs may be more suitable
for the treatment of CRC cells compared to conventional red LEDs.
The optimal wavelength for PDT should be chosen using an
appropriate action spectrum. For PpIX, the Soret band (400–500 nm)
is 20–30-fold larger compared to the absorption band at 630–635 nm
(4). Therefore, blue light sources
have been developed for this treatment. However, the absorption of
hemoglobin and melanin, the main absorbers in human tissue,
decreases with increasing wavelengths (24,25).
In addition, the penetration depth of light into tissue increases
with increasing wavelength, up to at least 800 nm (4). Light within the Soret band (410 nm)
leads to the highest level of cell inactivation, up to
approximately 2 mm from the surface in human skin and muscle
tissues; at depths exceeding 2 mm, 635 nm light may be optimal
(4,26). Therefore, we expected the blue LED
to be less effective compared to the red LED in our in vivo
study. However, we showed that ALA-PDT using blue LEDs yielded the
greatest antitumor effects in vitro and in vivo.
These results may mainly be due to the tumor specificity and higher
absorption of PpIX in the blue band compared to that in the red
band (Fig. 1). Another reason is
that the blue LED may have photo-degraded PpIX as well as its
photoproduct, photo-protoporphyrin (Ppp). Ppp has 2 absorption
peaks at approximately 440 and 670 nm (27). Based on these absorption peaks, the
combination of 2 wavelengths, 635 and 670 nm, or a broad spectral
region covering the 2 peaks may be more effective compared to using
a single wavelength (4). A previous
report has demonstrated the efficacy of combining these 2
wavelengths in ALA-PDT (27).
However, for Ppp, the blue band (at approximately 450 nm) is
markedly larger compared to the absorption band at 670 nm (27). Therefore, irradiation by the blue
LED (at approximately 450 nm) may effectively induce the
photo-degradation of PpIX as well as that of Ppp, resulting in
additional PDT effects. Consequently, ALA-PDT using blue LED had
the most antitumor effect in our study. Notwithstanding, ALA-PDT
using the white LED with a broad spectrum, demonstrated high
efficacy, similar to the blue LED. This result may mainly be due to
the broad spectrum that covers the peaks of PpIX and Ppp.
CRC is the third most common cancer and the fourth
most common cause of cancer-related mortality worldwide. The most
common curative therapy for colon cancer is surgical resection. The
reported incidence of recurrent disease after primary curative
resection ranges from 5 to 50% (28–30).
Peritoneal carcinomatosis (PC) is common and is the second most
frequent cause of mortality in CRC patients (31,32).
For CRC patients with PC, the mean and median overall survivals
have been reported to be 6.9 and 5.2 months, respectively (31). During the past decade, the
development of a new concept involving cytoreductive surgery and
hyperthermic intraperitoneal chemotherapy (HIPEC) has produced
promising results (32). However,
these procedures are so invasive that the rate of major morbidity
and mortality is extremely high (32,33).
Therefore, novel and non-invasive treatments for patients with PC
are required. ALA-PDT using LEDs may have the potential to become a
novel treatment for CRC patients with PC, since ALA-PDT is
non-invasive and has the potential to be used in repeated
treatments and in combination with other modalities.
The preferential accumulation of ALA-induced
porphyrins in tumor cells provides the possibility of
photo-detection by PpIX fluorescence (4,5,34).
This procedure may be performed by means of fiber optic monitoring
systems or fluorescence imaging systems after topical, local
internal or systemic administration of ALA. A certain study
demonstrated strong red fluorescence induced by ALA in urothelial
carcinoma using fluorescence cystoscopy (34). Moreover, laparoscopy equipped with a
fluorescence imaging system is used for PDD in urology (35,36).
In gastrointestinal tumors, a certain study showed that
laparoscopic fluorescence diagnosis using ALA administration may
increase the sensitivity and specificity of diagnostic staging
laparoscopy in rats with induced peritoneal dissemination (37). Over the past decade,
laparoscopic-assisted colectomy (LAC) has been performed as
standard surgery for CRC patients. Therefore, in the future,
ALA-PDT and PDD using fluorescence laparoscopy may prove to be
effective diagnostic and treatment modalities for CRC patients with
PC.
Our study has inherent limitations since we used
subcutaneous xenograft, not PC models and only one cell line,
HT-29. Thus, additional studies are required to confirm whether or
not ALA-PDT using LEDs is efficacious in other cell lines and in
mice with PC.
In conclusion, we demonstrate that ALA-PDT using
LEDs induces tumor cell death in the HT-29 CRC cell line in
vitro and in vivo. Our findings provide insight into a
novel treatment modality for CRC patients.
References
|
1
|
Nitsche U, Maak M, Schuster T, et al:
Prediction of prognosis is not improved by the seventh and latest
edition of the TNM classification for colorectal cancer in a
single-center collective. Ann Surg. 254:793–801. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mulsow J, Merkel S, Agaimy A and
Hohenberger W: Outcomes following surgery for colorectal cancer
with synchronous peritoneal metastases. Br J Surg. 98:1785–1791.
2011. View
Article : Google Scholar : PubMed/NCBI
|
|
3
|
Dougherty TJ, Gomer CJ, Henderson BW, et
al: Photodynamic therapy. J Natl Cancer Inst. 90:889–905. 1998.
View Article : Google Scholar
|
|
4
|
Peng Q, Warloe T, Berg K, et al:
5-Aminolevulinic acid-based photodynamic therapy. Clinical research
and future challenges. Cancer. 79:2282–2308. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Ishizuka M, Abe F, Sano Y, et al: Novel
development of 5-aminolevurinic acid (ALA) in cancer diagnoses and
therapy. Int Immunopharmacol. 11:358–365. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Murayama Y, Harada Y, Imaizumi K, et al:
Precise detection of lymph node metastases in mouse rectal cancer
by using 5-aminolevulinic acid. Int J Cancer. 125:2256–2263. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Juzeniene A, Juzenas P, Ma LW, Iani V and
Moan J: Effectiveness of different light sources for
5-aminolevulinic acid photodynamic therapy. Lasers Med Sci.
19:139–149. 2004.PubMed/NCBI
|
|
8
|
Brancaleon L and Moseley H: Laser and
non-laser light sources for photodynamic therapy. Lasers Med Sci.
17:173–186. 2002.PubMed/NCBI
|
|
9
|
Tsai JC, Chiang CP, Chen HM, et al:
Photodynamic therapy of oral dysplasia with topical
5-aminolevulinic acid and light-emitting diode array. Lasers Surg
Med. 34:18–24. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ickowicz Schwartz D, Gozlan Y, Greenbaum
L, Babushkina T, Katcoff DJ and Malik Z: Differentiation-dependent
photodynamic therapy regulated by porphobilinogen deaminase in B16
melanoma. Br J Cancer. 90:1833–1841. 2004.PubMed/NCBI
|
|
11
|
Maier A, Tomaselli F, Matzi V, Rehak P,
Pinter H and Smolle-Juttner FM: Photosensitization with
hematoporphyrin derivative compared to 5-aminolaevulinic acid for
photodynamic therapy of esophageal carcinoma. Ann Thorac Surg.
72:1136–1140. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Redondo P, Marquina M, Pretel M, Aguado L
and Iglesias ME: Methyl-ALA-induced fluorescence in photodynamic
diagnosis of basal cell carcinoma prior to Mohs micrographic
surgery. Arch Dermatol. 144:115–117. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Amo T, Kawanishi N, Uchida M, et al:
Mechanism of cell death by 5-aminolevulinic acid-based photodynamic
action and its enhancement by ferrochelatase inhibitors in human
histiocytic lymphoma cell line U937. Cell Biochem Funct.
27:503–515. 2009. View
Article : Google Scholar : PubMed/NCBI
|
|
14
|
Inoue H, Kajimoto Y, Shibata MA, et al:
Massive apoptotic cell death of human glioma cells via a
mitochondrial pathway following 5-aminolevulinic acid-mediated
photodynamic therapy. J Neurooncol. 83:223–231. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kim CH, Chung CW, Choi KH, et al: Effect
of 5-aminolevulinic acid-based photodynamic therapy via reactive
oxygen species in human cholangiocarcinoma cells. Int J Nanomed.
6:1357–1363. 2011.PubMed/NCBI
|
|
16
|
Wakui M, Yokoyama Y, Wang H, Shigeto T,
Futagami M and Mizunuma H: Efficacy of a methyl ester of
5-aminolevulinic acid in photodynamic therapy for ovarian cancers.
J Cancer Res Clin Oncol. 136:1143–1150. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Morton CA, McKenna KE and Rhodes LE:
Guidelines for topical photodynamic therapy: update. Br J Dermatol.
159:1245–1266. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Braathen LR, Szeimies RM, Basset-Seguin N,
et al: Guidelines on the use of photodynamic therapy for
nonmelanoma skin cancer: an international consensus. International
Society for Photodynamic Therapy in Dermatology, 2005. J Am Acad
Dermatol. 56:125–143. 2007.PubMed/NCBI
|
|
19
|
Apalla Z, Sotiriou E, Chovarda E, Lefaki
I, Devliotou-Panagiotidou D and Ioannides D: Skin cancer:
preventive photodynamic therapy in patients with face and scalp
cancerization. A randomized placebo-controlled study. Br J
Dermatol. 162:171–175. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Messmann H, Geisler M, Gross U, et al:
Influence of a haematoporphyrin derivative on the protoporphyrin IX
synthesis and photodynamic effect after 5-aminolaevulinic acid
sensitization in human colon carcinoma cells. Br J Cancer.
76:878–883. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Brunner H, Hausmann F, Krieg RC, et al:
The effects of 5-aminolevulinic acid esters on protoporphyrin IX
production in human adenocarcinoma cell lines. Photochem Photobiol.
74:721–725. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Calin MA, Diaconeasa A, Savastru D and
Tautan M: Photosensitizers and light sources for photodynamic
therapy of the Bowen’s disease. Arch Dermatol Res. 303:145–151.
2011.
|
|
23
|
van den Boogert J, van Staveren HJ, de
Bruin RW, Eikelaar JH, Siersema PD and van Hillegersberg R:
Photodynamic therapy for esophageal lesions: selectivity depends on
wavelength, power, and light dose. Ann Thorac Surg. 68:1763–1769.
1999.
|
|
24
|
Prahl S: Optical Absorption of Hemoglobin.
The Oregon Medical Laser Center; 1991, http://omlc.ogi.edu/spectra/hemoglobin/.
|
|
25
|
Jacques SL: Melanosome absorption
coefficient. The Oregon Medical Laser Center; 1998, http://omlc.ogi.edu/spectra/melanin/mua.html.
|
|
26
|
Moan J, Iani V and Ma LW: Choice of the
proper wavelength for photochemotherapy. Proc SPIE. 45:1608–1610.
1996.
|
|
27
|
Ma L, Bagdonas S and Moan J: The
photosensitizing effect of the photoproduct of protoporphyrin IX. J
Photochem Photobiol B. 60:108–113. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Hellinger MD and Santiago CA: Reoperation
for recurrent colorectal cancer. Clin Colon Rectal Surg.
19:228–236. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Fuzun M, Terzi C, Sokmen S, Unek T and
Haciyanli M: Potentially curative resection for locoregional
recurrence of colorectal cancer. Surg Today. 34:907–912. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Baca B, Beart RW Jr and Etzioni DA:
Surveillance after colorectal cancer resection: a systematic
review. Dis Colon Rectum. 54:1036–1048. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Sadeghi B, Arvieux C, Glehen O, et al:
Peritoneal carcinomatosis from non-gynecologic malignancies:
results of the EVOCAPE 1 multicentric prospective study. Cancer.
88:358–363. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Verwaal VJ, van Ruth S, de Bree E, et al:
Randomized trial of cytoreduction and hyperthermic intraperitoneal
chemotherapy versus systemic chemotherapy and palliative surgery in
patients with peritoneal carcinomatosis of colorectal cancer. J
Clin Oncol. 21:3737–3743. 2003. View Article : Google Scholar
|
|
33
|
Benizri EI, Bernard JL, Rahili A,
Benchimol D and Bereder JM: Small bowel involvement is a prognostic
factor in colorectal carcinomatosis treated with complete
cytoreductive surgery plus hyperthermic intraperitoneal
chemotherapy. World J Surg Oncol. 10:562012. View Article : Google Scholar
|
|
34
|
Kriegmair M, Baumgartner R, Knuechel R, et
al: Fluorescence photodetection of neoplastic urothelial lesions
following intravesical instillation of 5-aminolevulinic acid.
Urology. 44:836–841. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Adam C, Salomon G, Walther S, et al:
Photodynamic diagnosis using 5-aminolevulinic acid for the
detection of positive surgical margins during radical prostatectomy
in patients with carcinoma of the prostate: a multicentre,
prospective, phase 2 trial of a diagnostic procedure. Eur Urol.
55:1281–1288. 2009. View Article : Google Scholar
|
|
36
|
Hoda MR and Popken G: Surgical outcomes of
fluorescence-guided laparoscopic partial nephrectomy using
5-aminolevulinic acid-induced protoporphyrin IX. J Surg Res.
154:220–225. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Gahlen J, Prosst RL, Pietschmann M, et al:
Laparoscopic fluorescence diagnosis for intraabdominal fluorescence
targeting of peritoneal carcinosis experimental studies. Ann Surg.
235:252–260. 2002. View Article : Google Scholar
|