Introduction
Acute lung injury (ALI) is a lung disease
characterised by severe inflammation of endothelial and epithelial
cells of the lung (1). Hypoxemia,
pulmonary edema and widespread capillary leakage are usually
observed in patients with ALI (2).
This is caused by inflammation-related stimuli, primarily sepsis
and pneumonia, which lead to leukocyte migration and overproduction
of pro-inflammatory mediators, including interleukin (IL)-6, IL-8
and tumour necrosis factor-α (TNF-α) (3). ALI is a fatal disease that can cause
persistent respiratory failure and multiorgan dysfunction, and
patients with ALI may be dependent on mechanical ventilation
(4–6). Although intensive care has been
greatly improved, the mortality rate caused by ALI is between 40
and 70%, and ~200,000 individuals are affected by the condition in
America every year. Thus, novel drugs and therapies are required
for the treatment of ALI.
Toll-like receptor 4 (TLR4) is the ligand of
lipopolysaccharide (LPS), which is one of the pathogen-associated
molecular pattern recognition molecules (7,8).
TLR4 recognises pathogen-associated proteins, such as LPS, and
activates the nuclear factor κ-light-chain-enhancer of activated B
cells (NF-κB) signalling pathway, leading to the secretion of
inflammatory cytokines and chemokines (9). In chronic diseases, NF-κB is known to
be activated; this efficiently initiates and accelerates the
inflammatory response and induces the immune response (10–12).
Although it is well established that TLR4 affects downstream NF-κB
activation, the effect of triptolide on TLR4-NF-κB signalling has
yet to be elucidated.
Triptolide is a diterpenoid epoxide extracted from
the perennial plant Tripterygium wilfordii Hook F, which is
known in Chinese as ‘lei gong teng’ (13,14),
and has been used for the therapy of arthritic ailments in
Traditional Chinese Medicine for numerous years. T.
wilfordii contains >100 bioactive compounds and triptolide
is one of the major biologically active components. In vivo
and in vitro experiments have demonstrated that triptolide
has a role in numerous immune disorders, including multiple
sclerosis, colitis, lupus nephritis and transplant rejection
(6,15,16).
The anti-inflammatory activity of triptolide not only activates
immune cells, such as T cells and monocytes, but also resident
tissue cells (17,18). In the present study, the
anti-inflammatory effects of triptolide were investigated, and the
mechanisms underlying the action of triptolide in ALI were
explored. This may provide effective treatments for ALI, which may
ultimately aid the clinical therapy for patients with ALI.
Materials and methods
Animals and reagents
Six- to eight-week-old male BALB/c mice were
obtained from the Laboratory Animal Center of Shihezi University
(Shihezi, China) and housed in specific pathogen-free conditions.
All procedures were in accordance with the Declaration of Helsinki
of the World Medical Association. The protocols were also approved
by the Institutional Animal Care and Use Committee of the Shihezi
University School of Medicine. Triptolide was purchased from
Shanghai DND Pharm-Technology Co., Inc. (Shanghai, China). The
purity of triptolide was ≥98%, and the triptolide was dissolved in
dimethyl sulphoxide (DMSO). Dulbecco’s modified Eagle’s medium and
fetal bovine serum were provided by Gibco-BRL (Carlsbad, CA, USA).
Penicillin, streptomycin and LPS were purchased from Sigma (St.
Louis, MO, USA). Antibodies against TLR4, phosphorylated-nuclear
factor of κ light polypeptide gene enhancer in B cells inhibitor-α
(p-IκB-α) and phosphorylated-NF-κB (p65) were purchased from Santa
Cruz Biotechnology, Inc. (Santa Cruz, CA, USA), and antibodies
against β-actin were purchased from TransGenic Biotechnology
(Beijing, China). Monocyte chemotactic protein (MCP)-1 was
purchased from Thermo Fisher Scientific, Inc. (Rockford, IL,
USA).
Cytokine determination
For the ALI model, mice were fasted overnight but
allowed water ad libitum. Mice were anaesthetised with
intraperitoneal pentobarbital (50 mg/kg), and a dose of 1 mg/kg LPS
was instilled intratracheally to induce ALI. The bronchoalveolar
lavage fluid (BALF) was harvested as previously described (19) and the concentrations of
inflammatory cytokines (TNF-α, IL-1β, IL-6 and IL-8) were
determined using ELISA kits (Neobioscience, Beijing, China) in
accordance with the manufacturer’s instructions, using a Benchmark
Microplate Reader (Bio-Rad, Hercules, CA, USA). All of the samples
were analysed for cytokine levels in duplicate.
Grouping of mice
The mice were randomly divided into six groups, with
each group containing >10 mice. The negative control and
triptolide groups were administered an intravenous injection of
corresponding concentrations of DMSO or triptolide, respectively,
and after 30 min they were intratracheally treated with
phosphate-buffered saline. The LPS group was treated with an
intravenous injection of vehicle DMSO and, after 30 min, received
an intratracheal injection of LPS (1 mg/kg). The LPS + triptolide
groups were administered an intravenous injection of triptolide (1,
10 and 50 μg/kg) and, after 30 min, received an intratracheal
injection of LPS (1 mg/kg). Twelve hours after LPS administration,
all animals were sacrificed.
Quantitative polymerase chain reaction
(qPCR) analysis of mRNA expression
Total RNA was extracted using a RNApure kit (BioTeke
Corp., Beijing, China) and reverse transcribed using murine
leukaemia virus-reverse transcriptase (Invitrogen Life
Technologies, Carlsbad, CA, USA). The quality of the mRNA was
analysed using denaturing agarose gel electrophoresis containing
1.5% formaldehyde. Each cDNA sample was made in triplicate. PCR
amplifications were performed using an Applied Biosystems 7500
Real-Time PCR system (Applied Biosystems™, Foster City, CA, USA).
PCR was performed under the following thermal cycling conditions:
40 cycles of 10 sec at 95°C and 1 min at 60°C using SYBR-Green.
Primers for macrophage inflammatory protein (MIP)-1α, MIP-1β,
chemokine (C-C motif) ligand 5 (RANTES), interferon γ-induced
protein-10 (IP-10), MCP-1 and β-actin were as follows: MIP-1α,
5′-TGTTTGCTGCCAAGTAGCCACATC-3′ and 5′-AACAGTGTGACCAACTGGGAGGGA-3′;
MIP-1β, 5′-AAACCTAACCCCGAGCAACA-3′ and 5′-CCATTGGTGCTGAGAACCCT-3′;
RANTES, 5′-TCGTGCCCACGTCAAGGAGTATTT-3′ and
5′-ACTAGAGCAAGCGATGACAGGGAA-3′; IP-10, 5′-GGTCTGAGTGGGACTCAAGG-3′
and 5′-TCTTTTTCATCGTGGCAATG-3′; MCP-1, 5′-TGCATCTGCCCTAAGGTCTTC-3′
and 5′-AAGTGCTTGAGGTGGTTGTGG-3′; β-actin,
5′-AGAGGGAAATCGTGCGTGAC-3′ and 5′-CAATAGTGATGACCTGGCCGT-3′.
Myeloperoxidase (MPO) assays
Tissue samples from different groups of mice were
subjected to four freeze-thaw cycles and centrifuged at 12,000 × g
for 10 min at 4°C. The supernatant was assayed for MPO activity
using ELISA kits of MPO (R&D Systems Inc. Minneapolis, MN, USA)
in accordance with the manufacturer’s instructions.
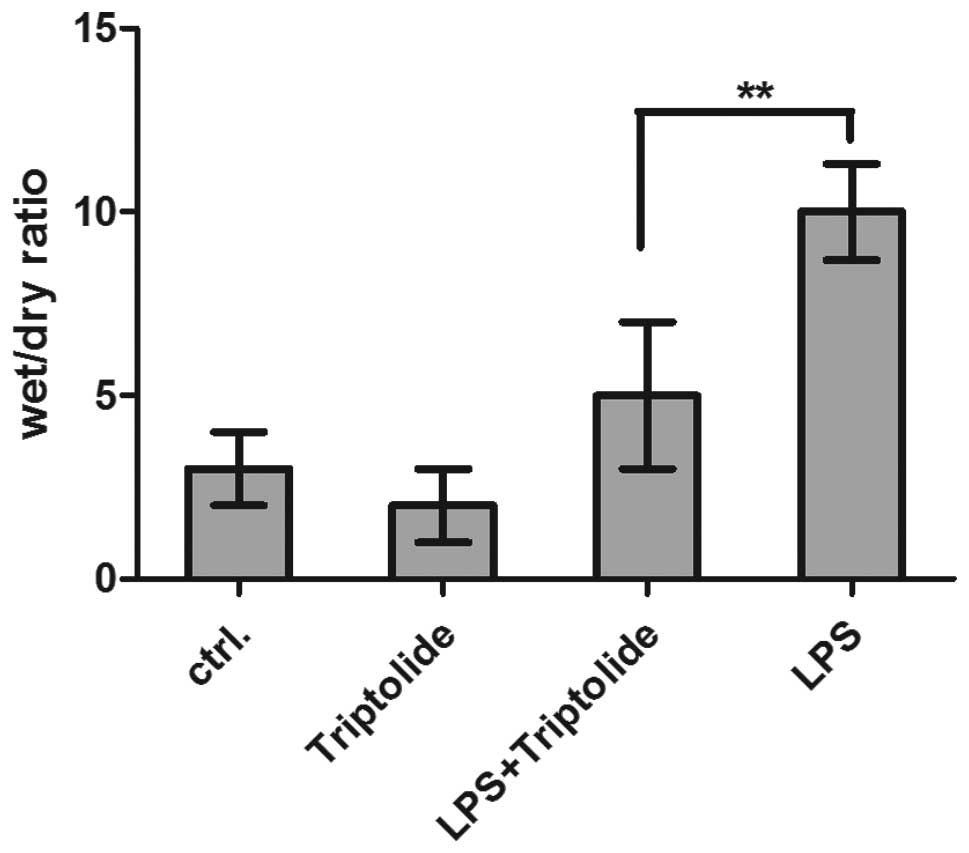
Lung wet/dry weight ratio
The wet/dry weight ratio is an indicator of lung
edema. The ratios were calculated by dividing the wet weight by the
dry weight. The middle lobe of the right lung was excised and the
wet weight was recorded, and the lung was then placed in an
incubator at 80°C for 24 h to obtain the dry weight.
Pulmonary histopathology
The lobe of the left lung was harvested 12 h after
LPS administration and fixed with an intratracheal instillation of
1 ml buffered formalin (10%, pH 7.2). The following procedures were
performed as previously described (20,21).
The lobe was further fixed in 10% neutral buffered formalin for 24
h at 4°C. The tissues were embedded in paraffin and cut into 5-μm
sections. Hematoxylin and eosin staining was performed following
the standard protocol.
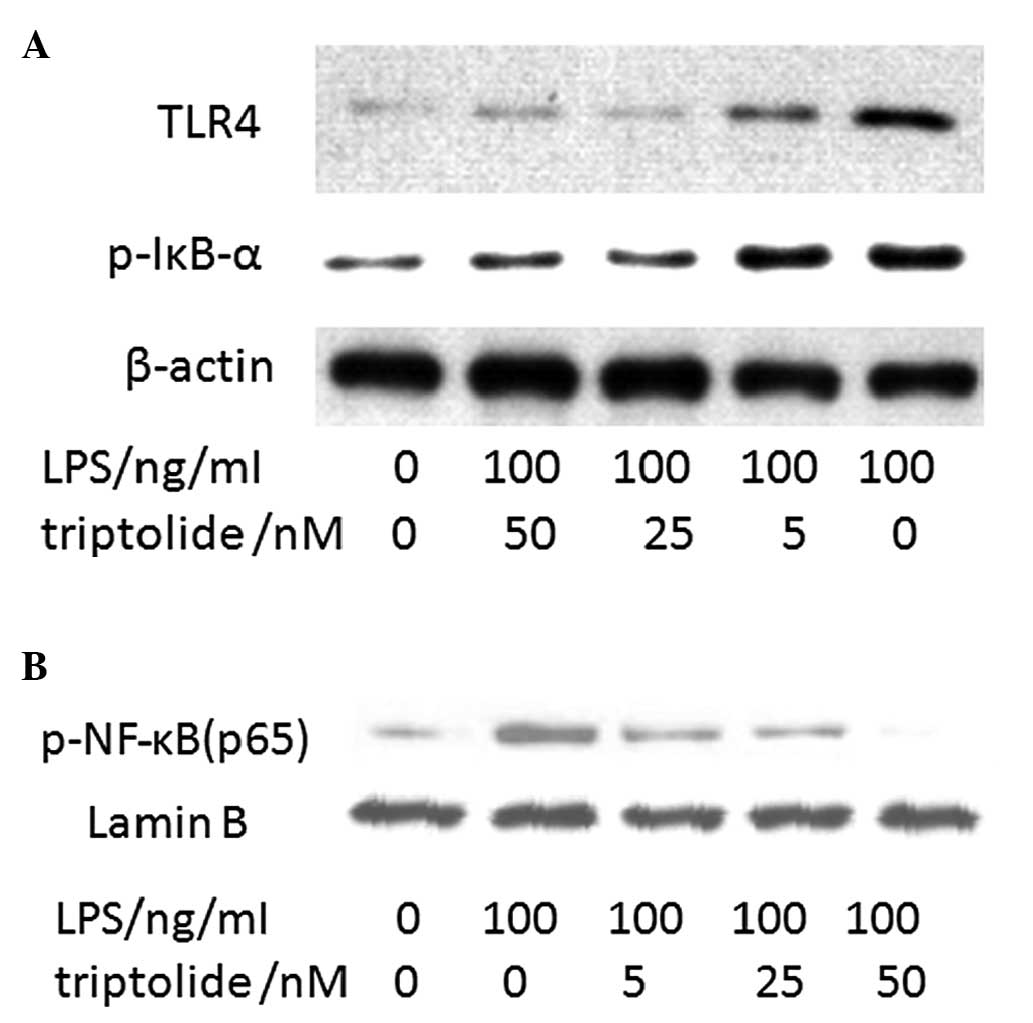
Western blot analysis
Western blot assay was performed according to the
methods of Lewis et al (22) and Vallejo-Illarramendi et al
(23). Briefly, A549 cells were
seeded into 48-well plates. After 6 h, the adherent cells were
treated with 100 ng/ml LPS along with various concentrations of
triptolide for 1 h. The total cell lysates were prepared. The
expression levels of TLR4, p-IκB-α, p-NF-κB (p65) was detected and
β-actin and lamin B were used as controls. Briefly, the steps
included gel electrophoresis, transfer, blocking, incubation with
primary antibody and secondary antibody, colorimetric detection.
Antibodies against TLR4, p-IκB-α and p-NF-κB (p65) were purchased
from Santa Cruz Biotechnology, Inc. and antibodies against β-actin
were purchased from TransGenic Biotechnology (Beijing, China). The
secondary antibodies of goat anti-mouse IgG and goat anti-rabbit
antibody were obtained from Santa Cruz Biotechnology, Inc.
Statistical analysis
Data were entered into a database and analysed using
SPSS statistical software (SPSS, Inc., Chicago, IL, USA). Data are
expressed as the mean ± standard deviation or the standard error of
the mean. Analysis of variance was used to determine statistically
significant differences between groups, followed by the Student’s
t-test. P<0.05 was considered to indicate a statistically
significant difference.
Results
Triptolide improves the pulmonary
histopathological status of mice with ALI
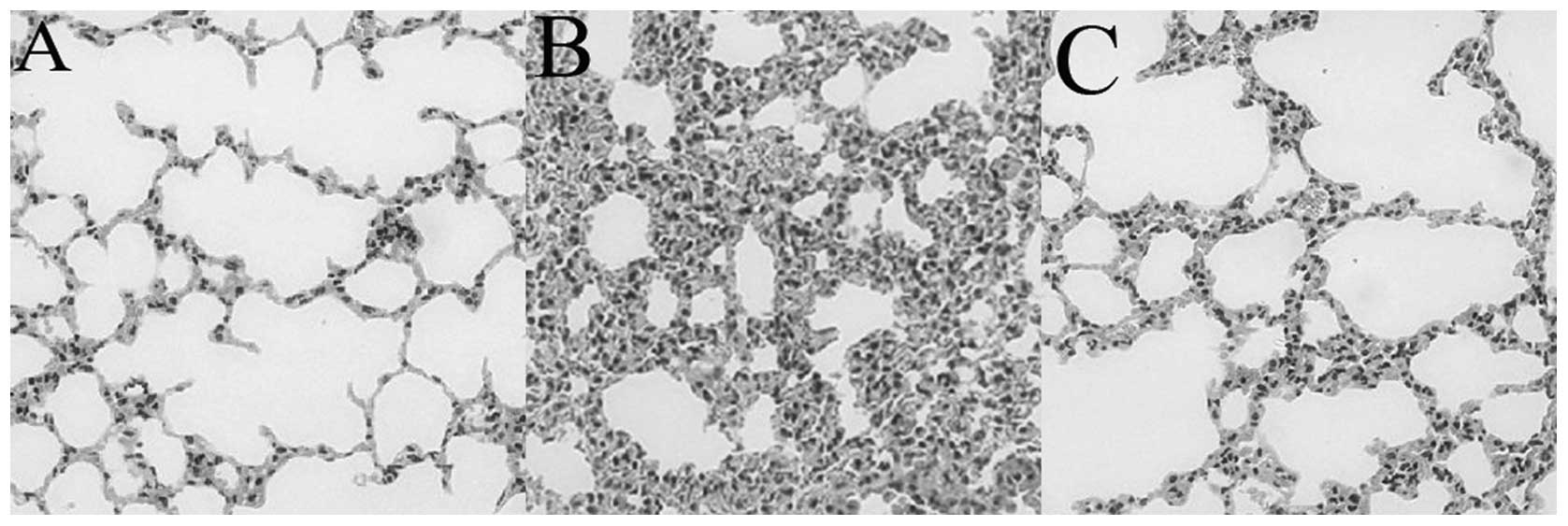
The pulmonary histopathological alterations of the
mice are shown in Fig. 1. In the
LPS group, the lung tissues stained with hematoxylin and eosin
exhibited widespread alveolar wall thickness, alveolar collapse and
notable inflammatory cell infiltration (Fig. 1B). However, lungs from the control
and triptolide groups exhibited normal structures (Fig. 1A and C). These results indicate
that triptolide improves the histopathological status of lungs in
LPS-treated mice and inhibits the infiltration of the inflammatory
cells into lung tissue.
Triptolide inhibits the expression of
chemokines in the lung tissues of mice with ALI
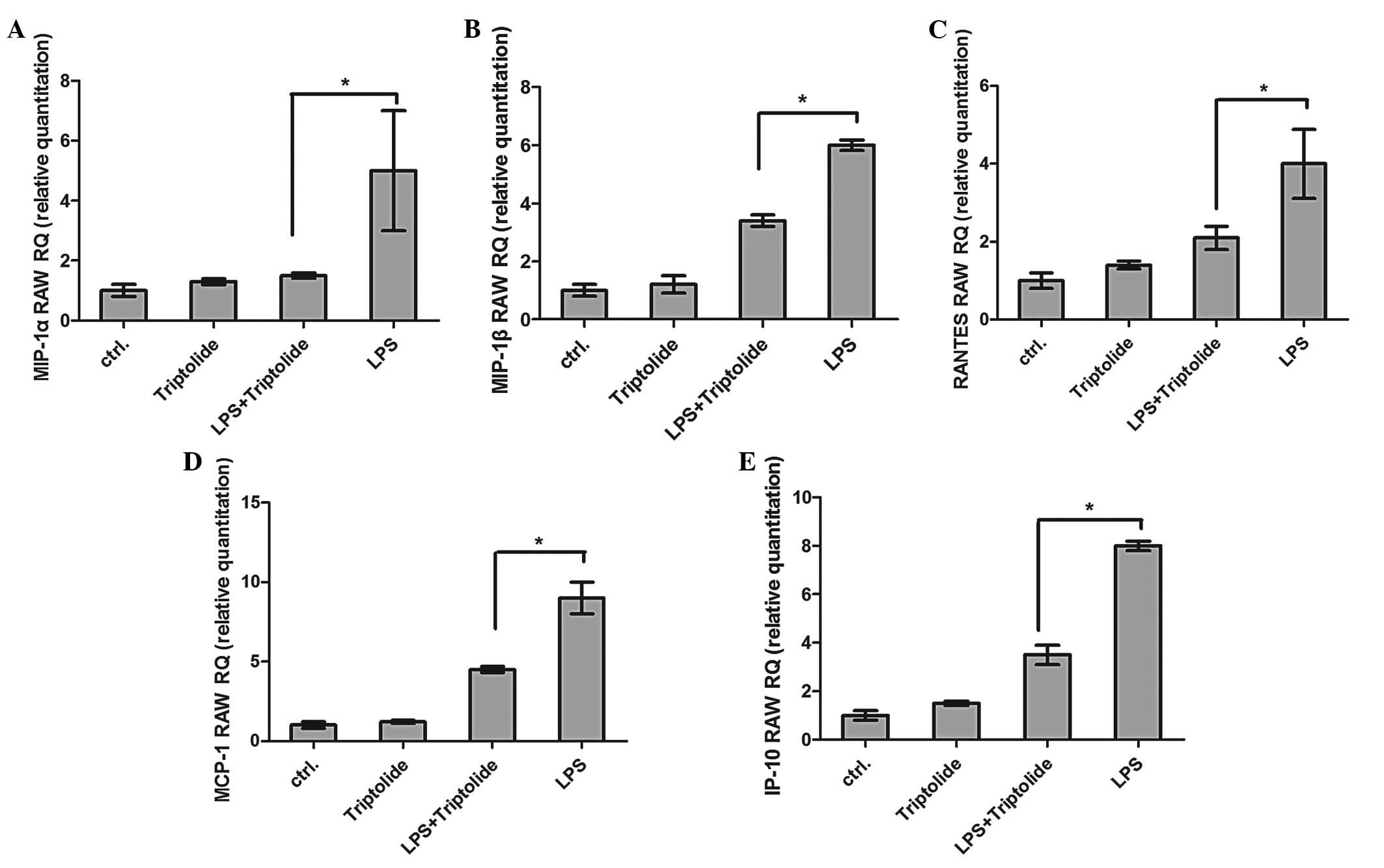
Following LPS administration, the expression of the
chemokines MIP-1α, MIP-1β, RANTES, MCP-1 and IP-10, detected using
qPCR, in lung tissue samples was markedly increased (Fig. 2). However, pretreatment with
triptolide significantly reduced the LPS-induced expression of
MIP-1α, MIP-1β, RANTES, MCP-1 and IP-10 (P<0.05). No significant
differences were observed in the expression of chemokines between
the LPS + triptolide and control groups (Fig. 2).
Triptolide inhibits inflammatory
cytokines in the BALF of mice with ALI
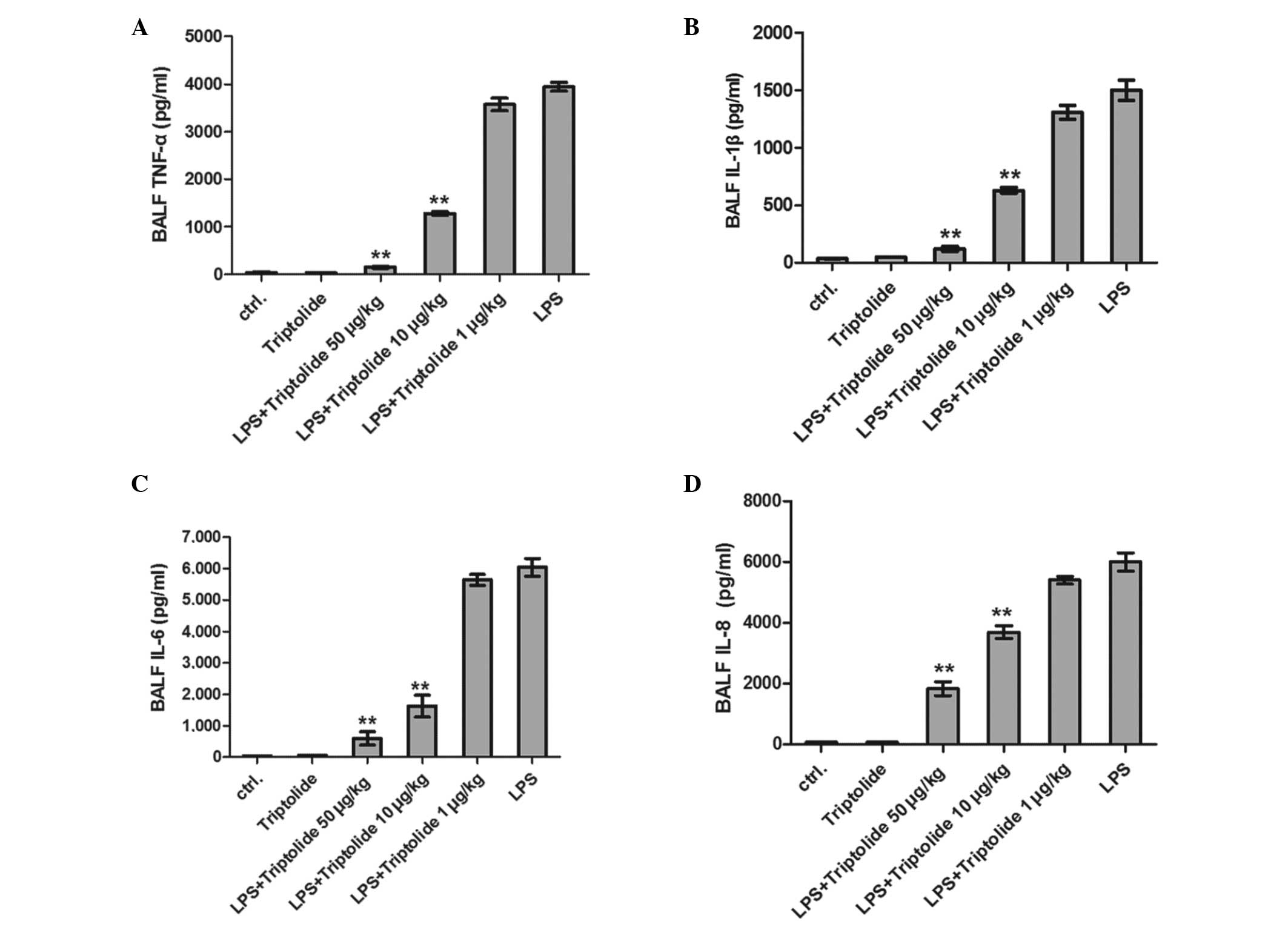
In order to elucidate the effect of triptolide on
the mice with ALI, the mice were pretreated with different
concentrations of triptolide and challenged with LPS. The
concentrations of TNF-α, IL-1β, IL-6 and IL-8 in the BALF were then
detected after 8 h. It was found that the concentrations of the
cytokines were significantly decreased in mice pretreated with
triptolide in a dose-dependent manner (Fig. 3).
Triptolide efficiently decreases the MPO
activity in lung tissues of mice injured by LPS
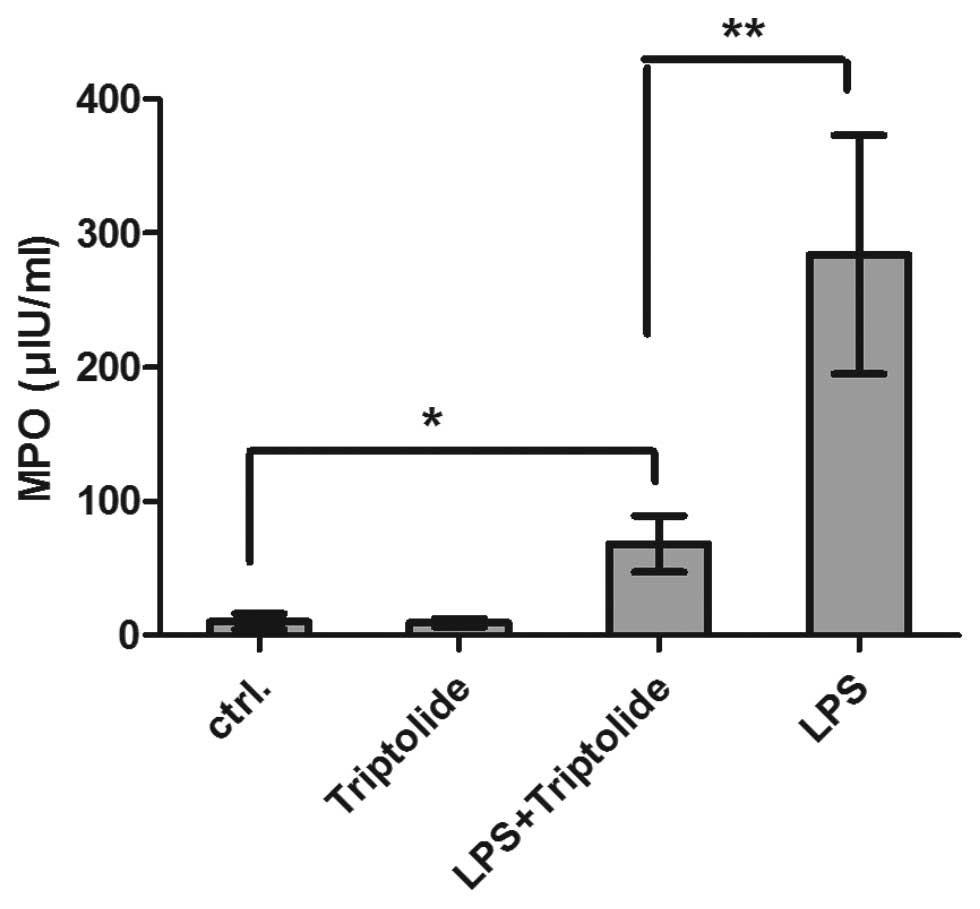
The MPO activity in lung tissues was significantly
increased following treatment with LPS compared with the control
tissues (Fig. 4). However,
triptolide pretreatment markedly decreased the MPO activity
compared with the LPS group (P<0.01).
Triptolide inhibits the lung edema of
mice with ALI
Compared with the negative control group, the lung
wet/dry weight ratios were significantly increased in the LPS group
(Fig. 5); however, the wet/dry
weight ratios of the lungs were significantly reduced by triptolide
administration (P<0.01, LPS + triptolide versus LPS groups).
Thus, triptolide inhibits lung edema in mice with ALI.
Triptolide inhibits the NF-κB pathway in
the A549 lung cell line
In order to elucidate the mechanism underlying the
anti-inflammatory effects of triptolide, the A549 cell line was
used as a cell model. Following LPS administration, it was observed
using western blot analysis that the expression levels of TLR4,
p-IκB-α and p-NF-κB p65 were significantly increased. However, 3 h
after triptolide pretreatment, the LPS-induced expression of
p-IκB-α and p-NF-κB p65 was significantly suppressed (Fig. 6).
Discussion
ALI is a type of diffuse alveolar injury and is a
complex clinical syndrome that is initiated by injury to the lung
(24,25). In the present study, the effect of
triptolide was investigated using a murine model of LPS-induced
ALI. The activation and recruitment of neutrophils are considered
to have an important role in the progression of ALI. IL-8 is a
potent chemokine that attracts neutrophils to the inflammatory
sites. In the present study it was demonstrated that, in the ALI
model, chemokine levels, including those of IL-8, IP-10, MIP-1α,
MIP-1β and RANTES, were significantly increased in the BALF, and
this was accompanied by the gathering of neutrophils, macrophages
and monocytes to the inflammatory sites, which accelerated the
progression of ALI. However, pretreatment with triptolide
effectively inhibited the production of chemokines and, therefore,
relieved the progression of ALI.
The local production of cytokines (TNF-α, IL-1 and
IL-6) by lung tissues in response to infectious or inflammatory
stimuli may also attract immune cells, such as neutrophils,
dendritic cells and monocytes, to the inflammatory sites (26,27),
leading to pulmonary injury. The cytokines also activate
granulocytes, which cause acute neutrophilic inflammation and
attract natural killer cells, monocytes and a variety of other
immune cells (28,29).
MPO, a major constituent of neutrophil cytoplasmic
granules, and its activity in lung tissue are direct indicators of
neutrophil sequestration in lung tissues (30). In the present study, the results
demonstrated that MPO activity increased markedly in lung tissues
following LPS treatment. Notably, pretreatment with triptolide
significantly decreased the MPO activity. This finding was
consistent with the results from the histopathological analysis,
which demonstrated that pretreatment with triptolide markedly
attenuated the neutrophil infiltration in lungs and maintained the
normal structure and function of the lungs in murine models. It was
also observed that there was a significant reduction in the
pulmonary edema of the lungs following pretreatment with
triptolide, as well as a reduction in the wet/dry ratios of lung
tissues.
The mechanism underlying the anti-inflammatory
activity of triptolide was also investigated in the present study.
It was indicated that triptolide may play a key role in the
TLR4-NF-κB signalling pathway by inhibiting the expression of TLR4,
decreasing the phosphorylation and degradation of IκB and
inhibiting the consequent activation of NF-κB (p65) to decrease the
production of cytokines and alleviate the progression of ALI. Thus,
the results from this study provide an insight for the development
of triptolide-based therapies for the treatment of ALI.
Furthermore, the findings may help to elucidate the mechanism and
targets of triptolide in cells in anti-inflammatory responses.
References
|
1
|
Chang CH, Kao CH, Chio CC, Lin CH, Lin MT
and Chang CP: Attenuating heatstroke-induced acute lung
inflammation, edema, and injury in rats by exercise
preconditioning. J Trauma Acute Care Surg. 74:1052–1059. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sharma S, Smith A, Kumar S, et al:
Mechanisms of nitric oxide synthase uncoupling in endotoxin-induced
acute lung injury: role of asymmetric dimethylarginine. Vascul
Pharmacol. 52:182–190. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Fu PK, Yang CY, Tsai TH and Hsieh CL:
Moutan cortex radicis improves lipopolysaccharide-induced acute
lung injury in rats through anti-inflammation. Phytomedicine.
19:1206–1215. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Pati S, Gerber MH, Menge TD, et al: Bone
marrow derived mesenchymal stem cells inhibit inflammation and
preserve vascular endothelial integrity in the lungs after
hemorrhagic shock. PLoS One. 6:e251712011. View Article : Google Scholar
|
|
5
|
Goodman RB, Pugin J, Lee JS and Matthay
MA: Cytokine-mediated inflammation in acute lung injury. Cytokine
Growth Factor Rev. 14:523–535. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wen HL, Liang ZS, Zhang R and Yang K:
Anti-inflammatory effects of triptolide improve left ventricular
function in a rat model of diabetic cardiomyopathy. Cardiovasc
Diabetol. 12:502013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Seki H, Tasaka S, Fukunaga K, et al:
Effect of Toll-like receptor 4 inhibitor on LPS-induced lung
injury. Inflamm Res. 59:837–845. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jeyaseelan S, Chu HW, Young SK, Freeman MW
and Worthen GS: Distinct roles of pattern recognition receptors
CD14 and Toll-like receptor 4 in acute lung injury. Infect Immun.
73:1754–1763. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kennedy M, Phelps D and Ingenito E:
Mechanisms of surfactant dysfunction in early acute lung injury.
Exp Lung Res. 23:171–189. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ben DF, Yu XY, Ji GY, et al: TLR4 mediates
lung injury and inflammation in intestinal ischemia-reperfusion. J
Surg Res. 174:326–333. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Huang D, Fang F and Xu F:
Hyperoxia-induced up-regulation of Toll-like receptors expression
in alveolar epithelial cells. Zhongguo Wei Zhong Bing Ji Jiu Yi
Xue. 23:645–649. 2011.(In Chinese).
|
|
12
|
Zhong WT, Wu YC, Xie XX, et al: Phillyrin
attenuates LPS-induced pulmonary inflammation via suppression of
MAPK and NF-κB activation in acute lung injury mice. Fitoterapia.
90:132–139. 2013.PubMed/NCBI
|
|
13
|
Matta R, Wang X, Ge H, Ray W, Nelin LD and
Liu Y: Triptolide induces anti-inflammatory cellular responses. Am
J Transl Res. 1:267–282. 2009.PubMed/NCBI
|
|
14
|
Qiu D and Kao PN: Immunosuppressive and
anti-inflammatory mechanisms of triptolide, the principal active
diterpenoid from the Chinese medicinal herb Tripterygium
wilfordii Hook. f Drugs R D. 4:1–18. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hoyle GW, Hoyle CI, Chen J, Chang W,
Williams RW and Rando RJ: Identification of triptolide, a natural
diterpenoid compound, as an inhibitor of lung inflammation. Am J
Physiol Lung Cell Mol Physiol. 298:L830–L836. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lee HF, Lee TS and Kou YR:
Anti-inflammatory and neuroprotective effects of triptolide on
traumatic brain injury in rats. Respir Physiol Neurobiol. 182:1–8.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Klawitter M, Quero L, Klasen J, et al:
Triptolide exhibits anti-inflammatory, anti-catabolic as well as
anabolic effects and suppresses TLR expression and MAPK activity in
IL-1β treated human intervertebral disc cells. Eur Spine J.
21(Suppl 6): S850–S859. 2012.PubMed/NCBI
|
|
18
|
Mei Z, Li X, Wu Q, Hu S and Yang X: The
research on the anti-inflammatory activity and hepatotoxicity of
triptolide-loaded solid lipid nanoparticle. Pharmacol Res.
51:345–351. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Jeyaseelan S, Chu HW, Young SK and Worthen
GS: Transcriptional profiling of lipopolysaccharide-induced acute
lung injury. Infect Immun. 72:7247–7256. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Guo Z, Li Q, Han Y, Liang Y, Xu Z and Ren
T: Prevention of LPS-induced acute lung injury in mice by
progranulin. Mediators Inflamm. 2012:5407942012.PubMed/NCBI
|
|
21
|
Fujino N, Kubo H, Suzuki T, et al:
Administration of a specific inhibitor of neutrophil elastase
attenuates pulmonary fibrosis after acute lung injury in mice. Exp
Lung Res. 38:28–36. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Lewis CW, Taylor RG, Kubara PM, Marshall
K, Meijer L and Golsteyn RM: A western blot assay to measure cyclin
dependent kinase activity in cells or in vitro without the use of
radioisotopes. FEBS Lett. 587:3089–3095. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Vallejo-Illarramendi A, Marciano DK and
Reichardt LF: A novel method that improves sensitivity of protein
detection in PAGE and Western blot. Electrophoresis. 34:1148–1150.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lim YS, Chung MH, Park SH, et al: Acute
and repeated inhalation lung injury by 3-methoxybutyl chloroformate
in rats: CT-pathologic correlation. Eur J Radiol. 62:227–234. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Parsons PE, Eisner MD, Thompson BT, et al;
NHLBI Acute Respiratory Distress Syndrome Clinical Trials Network.
Lower tidal volume ventilation and plasma cytokine markers of
inflammation in patients with acute lung injury. Crit Care Med.
33:1–6; discussion 230–232. 2005.
|
|
26
|
Trevejo JM, Marino MW, Philpott N, et al:
TNF-alpha -dependent maturation of local dendritic cells is
critical for activating the adaptive immune response to virus
infection. Proc Natl Acad Sci USA. 98:12162–12167. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Ning J, Liu QF, Luo XD, Fan ZP and Zhang
Y: Effect and mechanism of acute graft versus host disease on early
diffuse murine lung injury following allogeneic stem cell
transplantation. Sci China C Life Sci. 52:1016–1022. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Wu Y, Wan T, Zhou X, et al: Hsp70-like
protein 1 fusion protein enhances induction of carcinoembryonic
antigen-specific CD8+ CTL response by dendritic cell
vaccine. Cancer Res. 65:4947–4954. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Zhang N, Wang Z, Tang X, et al: Type 1
T-cell responses in chlamydial lung infections are associated with
local MIP-1alpha response. Cell Mol Immunol. 7:355–360. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Peng XM, Xie JH, Shuai B, et al:
Inhalation of aerosolized perfluorocarbon combined with
tetramethylpyrazine ameliorates hemodynamics and pulmonary
histopathology in a porcine model of acute lung injury. Nan Fang Yi
Ke Da Xue Xue Bao. 31:1382–1386. 2011.(In Chinese).
|