Introduction
Endometriosis (EMS), a chronic inflammatory disease
among women of reproductive age (age, 15–49 years old), is defined
as the presence of endometrial-like tissues outside the uterus
(1). The theory of retrograde
menstruation suggests that shed endometrial fragments may pass back
into the peritoneal cavity via the fallopian tubes, initiating the
formation of endometriotic lesions (2).
In the human endometrium, apoptosis is particularly
important due to the dynamic cycles of shedding and proliferation
(3); ectopic endometrial cells
have been reported to exhibit abnormal proliferative and apoptotic
regulation in response to appropriate stimuli (4). At present, the reduced susceptibility
of endometriotic epithelial and stromal cells to apoptosis has been
considered to contribute to the pathogenesis of EMS (5). Apoptosis in the eutopic endometrium
of women with EMS and endometriotic lesions was observed to be
lower than that of the the normal endometrium of women without EMS
(5).
It has been well reported that EMS is a
hormone-responsive disease associated with increased estrogen
production and resistance against the progesterone-based response
(6,7). Increased expression levels of
estrogen receptors (ER) α and β have been observed in ectopic
tissue compared with in normal and eutopic endometrium (8). In addition, increased estrogen
availability in EMS was reported to lead to notable protein kinase
activation and apoptosis inhibition (9).
Thymic stromal lymphopoietin (TSLP) is produced by
stromal cells, epithelial cells, fibroblasts, basophils,
keratinocytes and other cells types (10,11).
TSLP was reported to stimulate the growth and activation of B
cells; however, analysis has demonstrated that TSLP affects the
hematopoietic and non-hematopoietic cell lineages (12); endometrial stromal cells (ESCs) can
synthesize and secrete TSLP (13).
Additionally, interleukin (IL)-1β was reported to increase the
expression of TSLP mRNA and secretion within ESCs, which can be
promoted by IL-4 (13). Our
previous study revealed that estrogen can increase the production
of TSLP in ESCs in a dose-dependent manner, and that ESC-derived
and exogenous TSLP can activate the secretion of ESC-associated
growth-promoting cytokines (monocyte chemotactic protein-1 and
IL-8) and promote the viability and proliferation of ESCs (14).
The mechanism underlying the inhibition of apoptosis
mediated by estrogen in EMS is not completely clear; whether
estrogen regulates the apoptosis of ESCs by modulating the
expression of TSLP requires further investigation. Therefore, the
present study aimed to investigate the effects of the estrogen-TSLP
axis on the inhibition of EMS-associated apoptosis.
Materials and methods
Tissues
To study how estrogen regulates the apoptosis of
ESCs in EMS, we collected ectopic endometrium from subjects with
EMS and obtained ectopic ESCs from hyperoestrogenic environment
rather than normal ESCs from women without EMS. They may have
distinctive characteristics. Participants were women attending the
Obstetrics and Gynecology Hospital of Fudan University between May
and December 2017. Ectopic endometrial tissues were obtained from
fertile women (age, 21–46 years old) with ovarian (n=25) and pelvic
(n=5) EMS. Clinical suspicion of endometriosis was based upon
patient symptoms including dysmenorrhea, deep dyspareunia, chronic
pelvic pain, infertility and cyclical alterations in bowel and
urinary habits occurring only during menstruation. After physical
examination, patients were subjected to transvaginal ultrasound or
MRI. According to the suspicion of the presence of deep
infiltrating lesions or if the patient had persistent pain or
infertility, a surgical laparoscopic procedure was indicated.
During laparoscopy, biopsies from ectopic lesions were obtained
from each patient. Based on histopathology and medical records,
patients with endometrioma (OMA), superficial peritoneal
endometriosis (SPE), and deep infiltrating endometriosis (DIE) were
included, however, adenomyosis or pelvic inflammatory disease (PID)
related infertility were excluded. All samples were obtained in the
proliferative phase of the endometrial cycle, which were confirmed
histologically according to established criteria (15,16).
None of the women had received hormonal medication in the 3 months
prior to surgery. The collection of tissue samples was conducted
following the obtainment of informed consent from patients and was
in accordance with the requirements of the Research Ethics
Committee of the Hospital of Obstetrics and Gynecology, Fudan
University (Shanghai, China).
Culture of ESCs
The ectopic lesion tissues were collected under
sterile conditions and were transported to our laboratory
(Laboratory for Reproductive Immunology, Hospital of Obstetrics and
Gynecology, Fudan University Shanghai Medical College) on ice in
Dulbecco's modified Eagle's medium (DMEM)/F-12 (HyClone; GE
Healthcare Life Sciences, Logan, UT, USA). All tissues were minced
into 2 mm pieces and then digested with 20% collagenase type IV
(0.1%; Sigma-Aldrich; Merck KGaA, Darmstadt, Germany) for 40 min at
37°C with constant agitation. The tissue pieces were filtered via
sterile gauze pads (pore diameter sizes: 100, 200 and 400 mesh) to
remove cellular debris and separate the ESCs from epithelial cells.
The filtrate was then centrifuged at 150 × g at 4°C for 8 min and
washed with PBS. Following removal of the supernatant, the cells
were resuspended in DMEM/F-12 containing 10% fetal bovine serum
(FBS; Sigma-Aldrich; Merck KGaA), plated in culture flasks and
incubated in a humidified incubator with 5% CO2 at 37°C.
The culture medium was replaced every 2–3 days. These methods
supplied >95% Vimentin-positive (Vimentin+)
cytokeratin-negative (cytokeratin−) ESCs as demonstrated
previously (17).
ELISA
ESCs were seeded at 1×105 cells/well in
24-well plates and treated with various concentrations of 17-β
estradiol (E2; 10−9M, 10−8M or
10−7 M; Sigma-Aldrich; Merck KGaA) in phenol red-free
DMEM (HyClone; GE Healthcare Life Sciences) containing 10%
dextran-coated charcoal-treated FBS (Sigma-Aldrich; Merck KGaA),
and incubated for 48 h with 5% CO2 at 37°C. The controls
were treated with 0.1% dimethyl sulfoxide (DMSO; Sigma-Aldrich;
Merck KGaA). After 48 h of culture, the culture supernatant was
harvested via centrifugation at 150 × g at 4°C for 8 min to remove
cellular debris, and stored at −80°C. Then an ELISA (cat. no.
DTSLP0; R&D Systems Europe, Ltd., Abingdon, UK) was conducted
according to the manufacturer's protocol to determine the
expression of TSLP in the supernatant of the samples.
Treatment of ESCs
ESCs were cultured in 24-well plates at
1×105 cells/well and treated with various concentrations
of recombinant human TSLP (rhTSLP; 1, 10 or 100 ng/ml; cat. no.
1938-TS, R&D Systems Europe, Ltd.) for 48 h; the control group
was treated with 0.1% PBS. ESCs in TSLP-treated group or control
group were cultured in DMEM/F-12 containing 10% fetal bovine serum
(FBS; Sigma-Aldrich; Merck KGaA) and incubated in a humidified
incubator with 5% CO2 at 37°C for 48 h.
In addition, ESCs under the same culture conditions
were treated with E2 (10−7 M) alone,
anti-human TSLP neutralizing antibody (αTSLP; 0.25 µg/ml; cat. no.
AF1398, R&D Systems Europe, Ltd.) alone or E2 and
αTSLP for 48 h at 37°C with 5% CO2. The concentration of
E2 was 10−7 for a better stimulation of TSLP
secretion of ESCs (Fig. 1). The
controls were treated with 0.1% DMSO for 48 h at 37°C with 5%
CO2. The ESC groups were employed for apoptosis analysis
and flow cytometry (FCM) as described below.
Apoptosis analysis
Apoptotic cell death was detected via Annexin
V-fluorescein isothiocyanate (FITC)/propidium iodide (PI) staining
using the apoptosis kit (Annexin V FITC Apop Dtec kit, BD
Biosciences, Franklin Lakes, NJ, USA). ESCs (1×105
cells) from the various cultures were trypsinized using 0.25%
Trypsin (1×, Phenol Red; no EDTA; Gibco, Grand Island, New York,
NY, USA) for 3 min at 37°C with 5% CO2 and collected,
washed and resuspended in 300 µl binding buffer included in the
apoptosis kit, followed by incubation with 5 µl Annexin V-FITC and
2.5 µl PI at room temperature for 15 min in the dark. Then, 200 µl
binding buffer was added and the cell samples were analyzed with a
Beckman CyAn flow cytometer (Beckman Coulter, Inc., Brea, CA, USA)
using Becton Dickinson CellQuest software (version 7.1; Becton
Dickinson). Annexin V+ PI− cells were in the
early stage of apoptosis and Annexin V+ PI+
cells were late apoptotic cells. The percentage of the early
apoptotic cells was determined as the apoptosis rate. The
experiments were performed in triplicate.
FCM
The ESCs (1×105 cells) in the various
treatment groups were centrifuged immediately at 150 × g at 4°C for
8 min. The expression of B- cell lymphoma 2 (Bcl-2), Fas and Fas
ligand (FasL) was analyzed by FCM. These ESCs were fixed use 0.5 ml
Fixation Buffer (Biolegend, Inc., San Diego, CA, USA) in the dark
for 20 min at room temperature. For permeabilization, we resuspend
fixed cells in diluted Intracellular Staining Permeabilization Wash
Buffer (Biolegend, Inc., San Diego, CA, USA) and centrifuged at 350
× g for 5–10 min, and repeated the process twice at room
temperature. Staining was performed with Brilliant Violet™
421-conjugated anti-human Bcl-2 (cat. no. 658709),
allophycocyanin-conjugated anti-human Fas (cat. no. 305611) and
phycoerythrin-conjugated anti-human FasL (cat. no. 306406)
antibodies (5 µl separately, all antibodies were obtained from
Biolegend, Inc., San Diego, CA, USA) at room temperature for 30 min
in the dark. In addition, isotypic IgG antibodies (5 µl
separately), including Brilliant Violet™ 421 anti-mouse IgG1
antibody (cat. no. 406615), APC anti-mouse IgG1 antibody (cat. no.
406609) and PE anti-mouse IgG1 antibody (cat. no. 406607) were used
as controls. Subsequently, the cells were washed twice and
resuspended in PBS for FCM analysis. Samples were analyzed with a
Beckman Cyan flow cytometer (Beckman Coulter, Inc.) using CellQuest
software (version 7.1; Beckman Coulter, Inc.). The experiments were
performed in triplicate and repeated three times.
Statistical analysis
All data were analyzed via one-way analysis of
variance, followed by a Tukey post-hoc test for the comparison of
multiple groups using SPSS software, version 11.5 (SPSS, Inc.,
Chicago, IL, USA). Each experiment was conducted three times and
results are presented as the mean ± standard error. P<0.05 was
considered to indicate a statistically significant difference.
Results
Estrogen promotes TSLP secretion of
ESCs
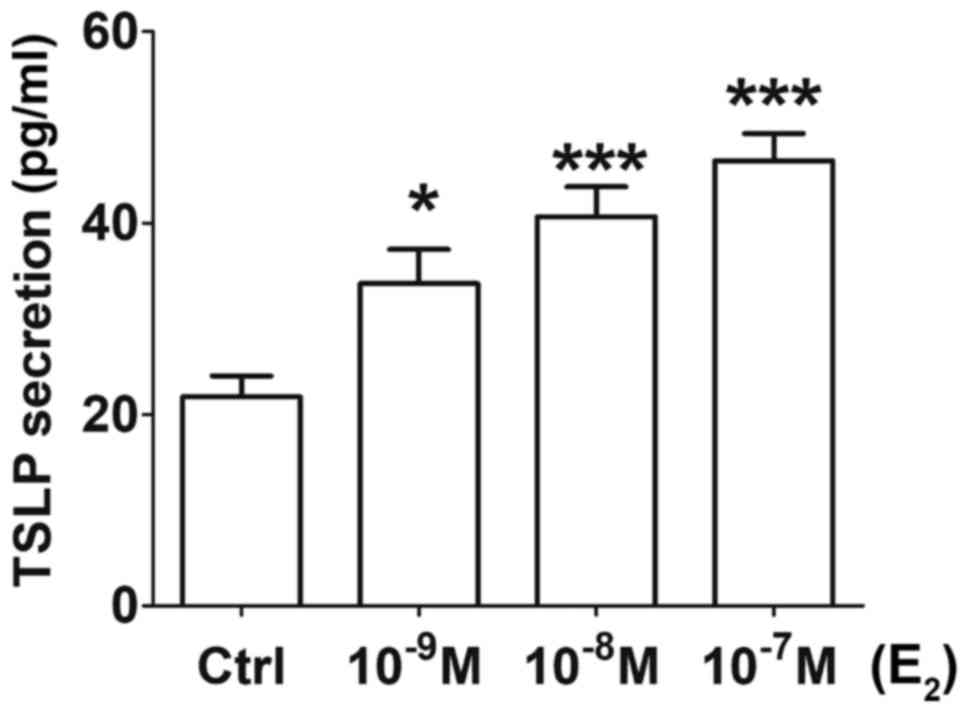
Following 48 h of incubation, the concentration of
TSLP in the ESC culture supernatant was significantly higher with
increased concentrations of E2 (10−9,
10−8 or 10−7 M) (Fig. 1) compared with in the control
group. ESCs obtained from the ectopic lesions from patients with
EMS exhibited basal secretion levels of TSLP as >20 pg/ml TSLP
was detected in the control group (treated with 0.1% DMSO), which
was consistent with previous studies (13,14).
Treatment with 10−9 M E2 resulted in a
significant increase of TSLP secretion (P<0.05); upon
administration of 10−8 and 10−7 M
E2, the concentration of TSLP in the supernatant was
increased by ~2-fold compared with in the control (P<0.001)
(Fig. 1). The results suggested
that estrogen promoted TSLP secretion of ESCs in a dose-dependent
manner.
TSLP inhibits the apoptosis of
ESCs
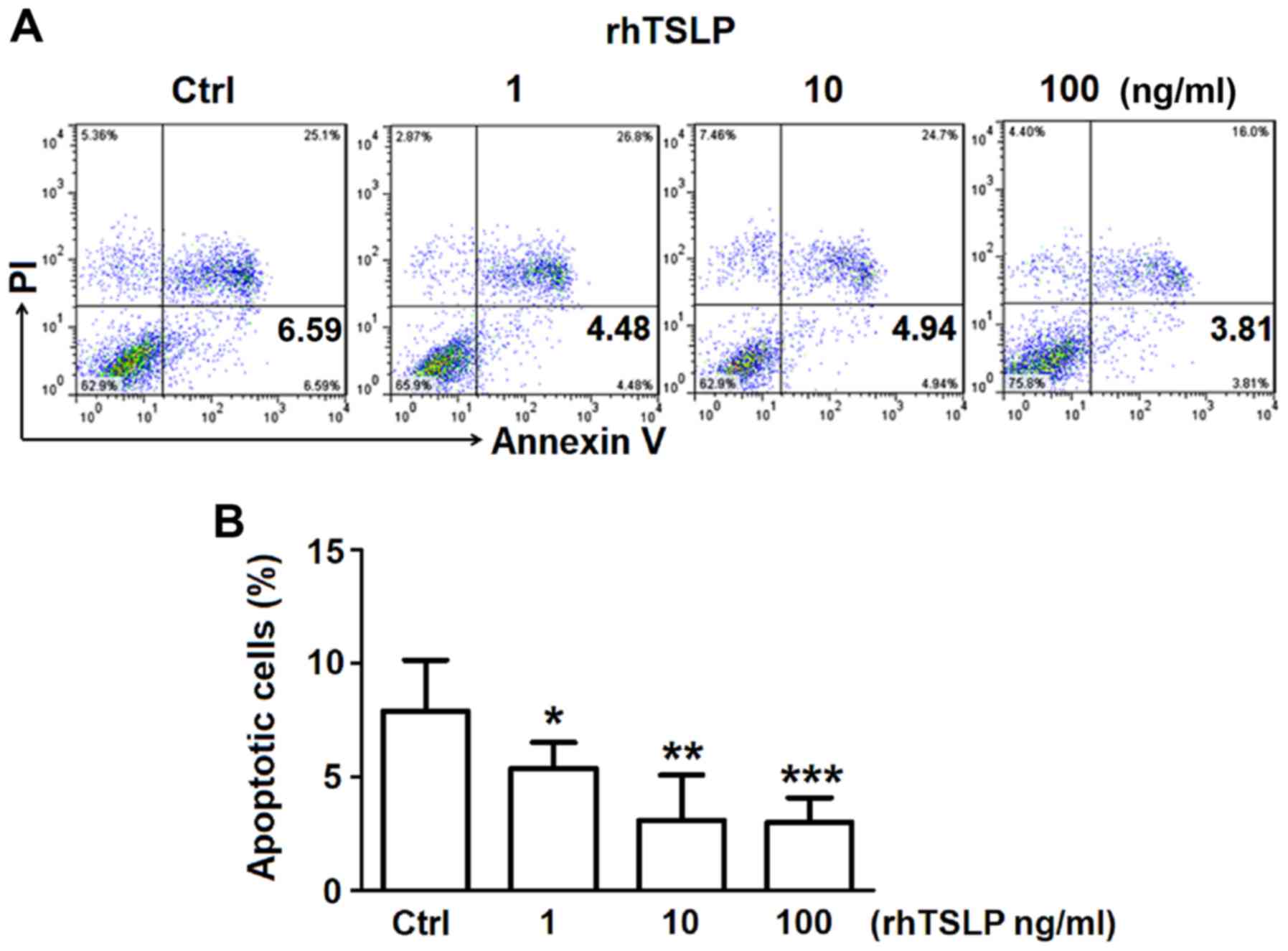
In order to investigate the how TSLP affects the
apoptosis of ESCs, increasing concentrations of rhTSLP was applied
to ESCs in vitro obtained from the ectopic lesions of
patients with EMS. After 48 h following treatment, ESCs were
obtained for FCM analysis to detect the rate of apoptosis. The
administration of rhTSLP resulted in decreases in the number of
apoptotic ESCs (Fig. 2A). Analysis
of the early apoptotic rate demonstrated that 1 ng/ml rhTSLP
significantly reduced the early apoptotic rate (P<0.05);
however, highly significant reductions in apoptosis were reported
in response to 10 and 100 ng/ml (rhTSLP (P<0.01; P<0.001)
(Fig. 2B). These results suggested
that exogenous TSLP could inhibit the apoptosis of ESCs in
vitro.
TSLP increases the number of
Bcl-2+ ESCs
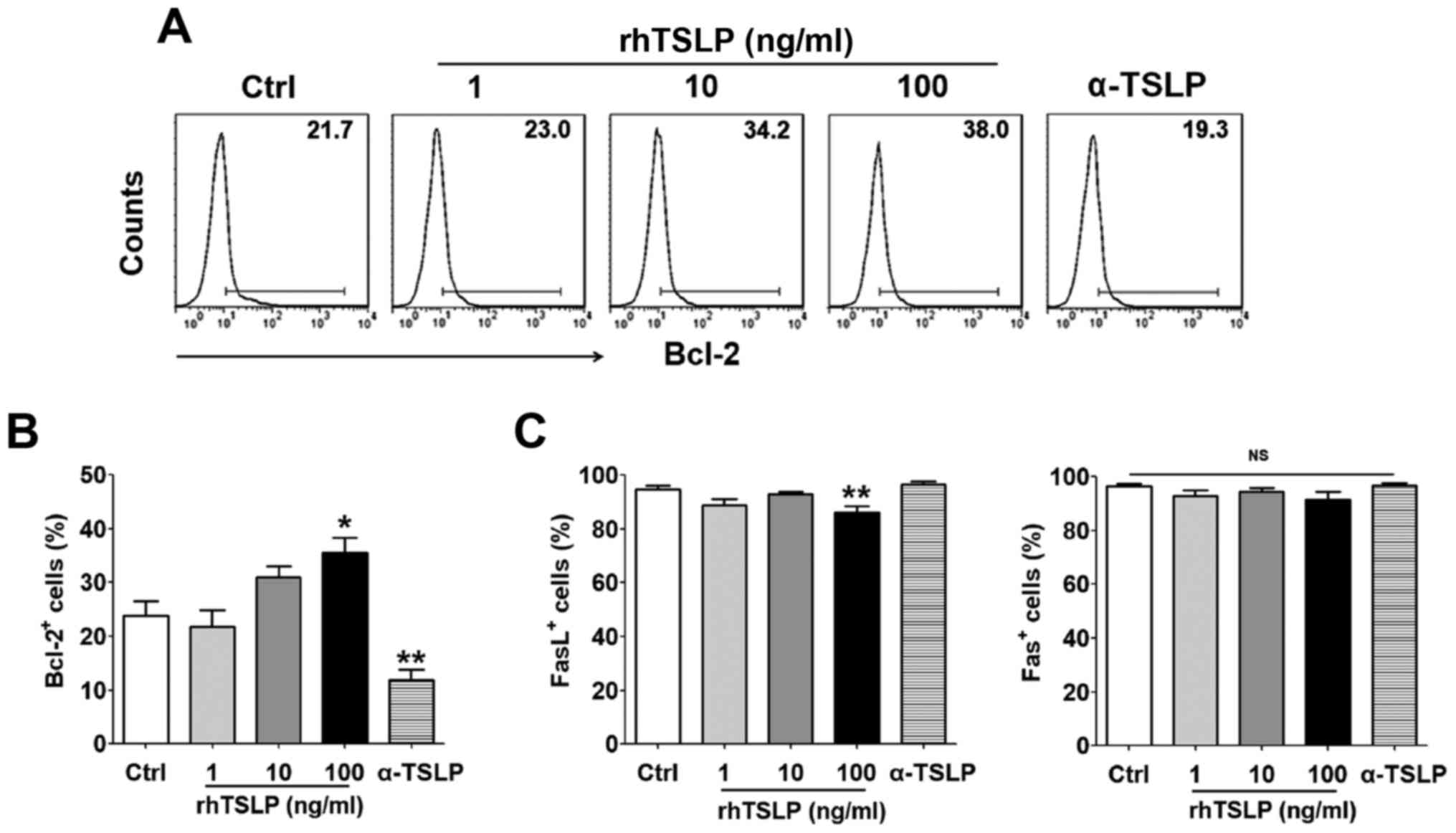
Following the treatment ESCs with rhTSLP for 48 h,
cells expressing the antiapoptotic protein Bcl-2, and two
apoptosis-associated markers, Fas and FasL were detected by FCM. As
the concentration of TSLP increased, the proportion of
Bcl-2+ ESCs also increased (Fig. 3A); a significant difference was
observed in response to treatment of the highest concentration (100
ng/ml) of rhTSLP compared with the control group (P<0.05)
(Fig. 3B). On the contrary, the
number of Bcl-2+ ESCs was significantly reduced when
αTSLP was applied to neutralize TSLP in the culture system compared
with in the control (P<0.01). The 100 ng/ml rhTSLP treatment
group exhibited a significantly decreased number of
FasL+ ESCs (P<0.01); however, no significance was
observed in Fas+ ESCs between these groups (Fig. 3C). Additionally, applying αTSLP did
not exhibit notable effects on the number of Fas+ and
FasL+ ESCs (Fig. 3C).
These results indicated that TSLP might inhibit ESC apoptosis
probably by promoting Bcl-2 expression in ESCs rather than via the
Fas/FasL pathway.
Estrogen increases the number of
Bcl-2+ ESCs by inducing the secretion of TSLP
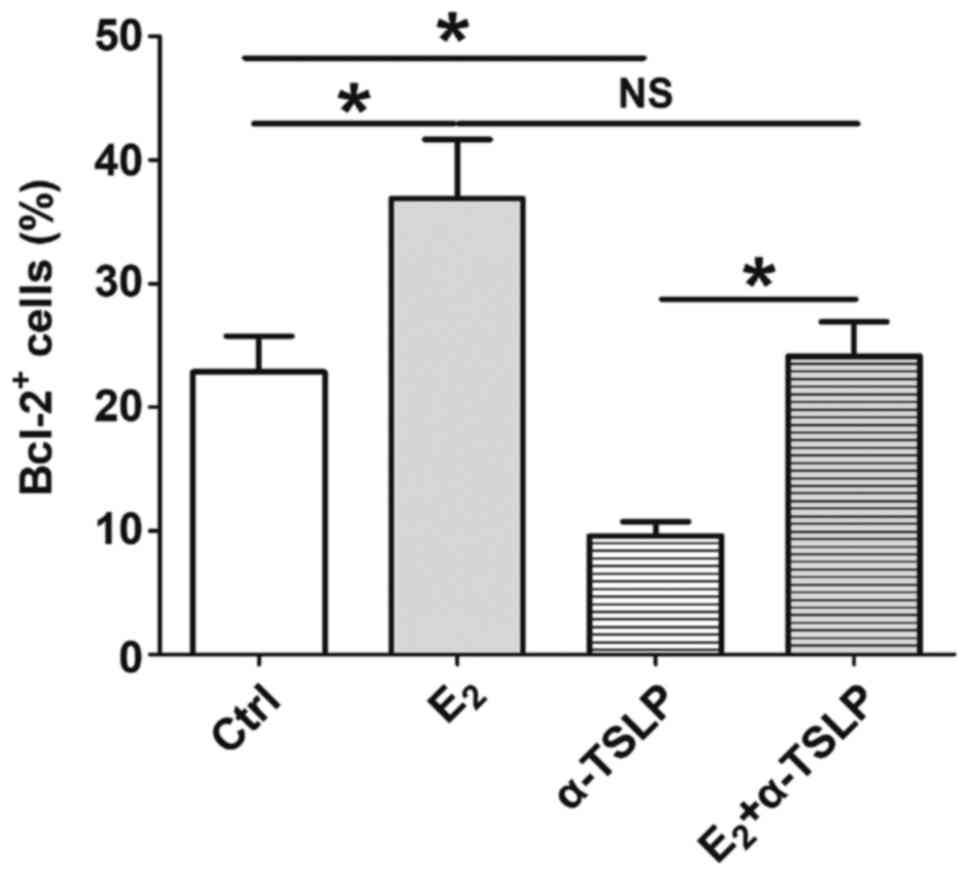
Following treatment with E2
(10−7 M) and/or αTSLP for 48 h, ESCs were obtained for
FCM analysis to detect the expression of Bcl-2. As presented in
Fig. 4, E2 induced a
significant increase in the number of Bcl-2+ ESCs
compared with in the control (P<0.05). This effect was notably
inhibited when ESCs were incubated with αTSLP within the
E2 treatment system; however, no significant difference
was reported compared with in the control and E2
treatment groups. As aforementioned, applying αTSLP to the ESC
culture system significantly suppressed the number of
Bcl-2+ ESC (Fig. 3B);
however, in the presence of E2, the inhibitory effects
of αTSLP were significantly reversed (P<0.05) (Fig. 4). The results suggested that
estrogen could promote TSLP secretion in ESCs, resulting in an
increase of Bcl-2 expression and inhibition of ESC apoptosis.
Estrogen-TSLP suppresses the apoptosis
of ESCs
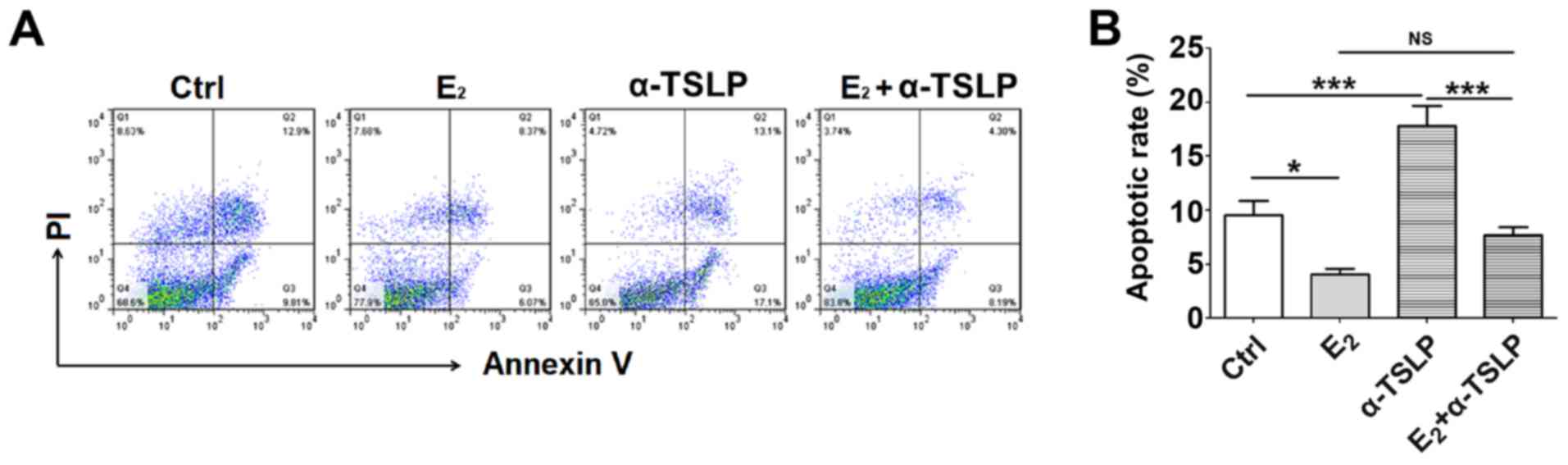
To investigate the effect of estrogen and TSLP on
the early apoptotic rate of ESCs, cells treated with E2
and/or αTSLP were obtained for FCM analysis (Fig. 5A). Treatment with exogenous
E2 led to a significant decrease in the apoptotic rate
of ESCs (P<0.05) and neutralized TSLP resulted in a
significantly increased apoptotic rate compared with in the control
(P<0.001) (Fig. 5B). In the
E2 and αTSLP combined treatment group, the apoptotic
rate was significantly reduced compared with in the αTSLP group
(P<0.001) (Fig. 5B), but
notably increased compared with in the E2 group. This
suggested that the respective antiapoptotic and proapoptotic
effects of E2 and αTSLP were reduced when combined.
Discussion
Accumulating studies have reported the importance of
eutopic endometrium dysfunction in the pathogenesis of EMS
(14,18–21).
According to the implantation theory, intrinsic factors of the
eutopic endometrium in women with EMS, including aberrantly
produced cytokines, growth factors and specific cancer-associated
molecules, may be transported to the endometriotic implants and
contribute to abnormal cell survival in ectopic tissues (14,18,19).
In the eutopic endometrium of women with EMS, the physiological
increase in the apoptotic rate in the late secretory phase was not
observed, indicating that the imbalance of apoptosis and
proliferation may contribute to the implanting of the eutopic
endometrium and the survival of the ectopic endometrium (22). In the present study, the apoptosis
of eutopic endometrium in the presence of a specific estrogen at
high concentrations was investigated to determine the essential
role of eutopic endometrium in the occurrence and development of
EMS.
Estrogen induces the development of the ectopic
endometrium and induce alterations in estrogen signaling (23). The expression levels of ERα and ERβ
of the ectopic endometrial tissues differ to that of eutopic
tissues, which possess markedly higher expression levels of ERβ
(23,24). Via the exogenous addition of
estrogen to the ectopic ESC culture system, estrogen was reported
to suppress the apoptosis of ESCs, which was associated with
promotion of Bcl-2 expression in the present study. As the gene of
a typical apoptosis-associated molecule, Bcl-2 may be considered as
a novel proto-oncogene that inhibits cell death by regulating
mitochondrial membrane function (25). Upregulated Bcl-2 protein expression
has been observed in ESCs of ovarian EMS compared with eutopic ESCs
from women with and without EMS (26).
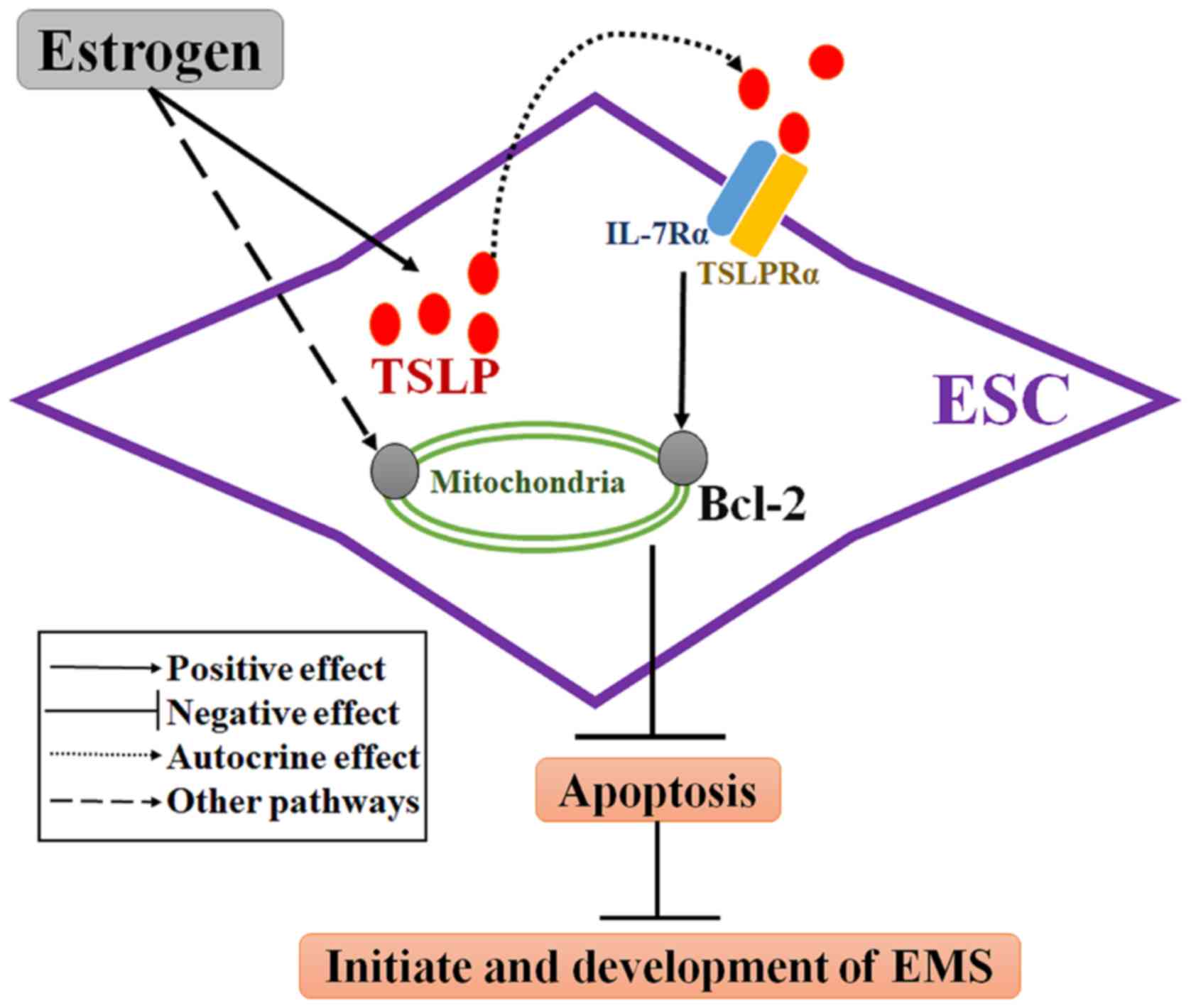
TSLP is a cytokine with structural and functional
similarities to members of the hematopoietin family (10). The functional and high affinity
TSLP receptor (TSLPR) complex is a heterodimer of TSLPRα and IL-7
receptor-α (27,28). TSLP has previously been reported as
a contributory factor to a variety of cancers, including pancreatic
and breast cancers, which have been associated with Th2-related
chronic inflammation (29,30). Consistent with previous studies
(13,14), the present study demonstrated that
ESCs from patients with EMS possess basal TSLP secretion levels in
the absence of estrogen. The limitation for the present study is
the lack of analysis of TSLP secretion by ESCs from the control
without EMS. Here, it was demonstrated that TSLP secretion was
promoted in a dose-dependent manner in response to estrogen
treatment. Additionally, TSLP was reported to the affect the
mitochondria-dependent intrinsic apoptosis pathway (31). It has been demonstrated that TSLP
promotes lymphocyte survival, which was accompanied with increased
Bcl-2 expression (32,33). In ESCs, rhTSLP was observed to
decrease the apoptotic rate and promote Bcl-2 expression within
ESCs in the present study. Inhibition of TSLP via a TSLP
neutralizing antibody revealed that the apoptotic rate of ESCs
increased and the number of Bcl-2+ ESCs decreased;
however, that of Fas/FasL+ ESCs were notably unaltered
in the present study. This suggested that endogenous TSLP may
regulate ESC apoptosis in an autocrine manner associated with
Bcl-2, but not Fas/FasL (Fig. 6).
Therefore, these results indicate that endogenous and exogenous
TSLP may inhibit ESC apoptosis by upregulating the expression of
Bcl-2.
In the present study, E2 inhibited the
apoptosis of ESCs mainly by upregulating the anti-apoptosis protein
Bcl-2. When TSLP was neutralized in the presence of estrogen,
upregulated Bcl-2 and the reduced apoptotic rate induced by
estrogen were partly reversed; however, αTSLP did not fully promote
the antiapoptotic and pro-Bcl-2 effects of estrogen. This suggested
that TSLP secretion may be one of the mechanisms underlying
estrogen-inhibited ESC apoptosis. Other signaling pathways may
affect ESC apoptosis; however, further investigation is required.
The antiapoptotic effects of estrogen are conducted via numerous
pathways involving nuclear and extranuclear ER signaling (9). For instance, the activation of
extranuclear kinases by the estrogen-ER complex was reported to
lead to a rapid non-genomic signaling cascade, resulting in
apoptosis inhibition (9).
In conclusion, the present study revealed a novel
estrogen-dependent mechanism underlying the suppression of ESCs
apoptosis associated with TSLP secretion and Bcl-2 regulation. In
addition, endogenous and estrogen-induced production of endometrial
TSLP may promote the initiate and development of EMS via apoptosis
inhibition. From the present study, estrogen-TSLP axis may be a new
therapeutic target for EMS. This study provides evidence that
blocking this pathway may promote ESC apoptosis in treating EMS,
but this needs to be investigated further.
Acknowledgements
Not applicable.
Funding
The present study was supported by the Major
Research Program of National Natural Science Foundation of China
(NSFC; grant nos. 91542108, 81471513, 31671200, 31600735 and
81601354), the Shanghai Rising-Star Program (grant no.
16QA1400800), the Development Fund of Shanghai Talents (grant no.
201557), the Innovation-oriented Science and Technology Grant from
NPFPC Key Laboratory of Reproduction Regulation (grant no.
CX2017-2), the Program for Zhuoxue of Fudan University, the Natural
Science Foundation of Jiangsu Province (grant no. BK20160128), and
the Fundamental Research Funds for the Central Universities (grant
no. 021414380180).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
H-LY and K-KC conducted all experiments and prepared
the figures and the manuscript. JM, W-JZ and L-BL conducted flow
cytometry analysis. LY, YM, M-YW, S-YH and Z-ZL collected the
samples and performed cell isolation. J-FY collected the clinical
information and analyzed the data. D-JL assisted in the study
design and critically revised the manuscript for important
intellectual content. M-QL designed the study, supervised the
project and edited the manuscript. All the authors were involved in
writing the manuscript.
Ethics approval and consent to
participate
The present study was approved by the Research
Ethics Committee in Hospital of Obstetrics and Gynecology, Fudan
University. Written informed consent was obtained from all patients
prior to enrollment within the study.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
EMS
|
endometriosis
|
|
ESCs
|
endometrial stromal cells
|
|
TSLP
|
thymic stromal lymphopoietin
|
|
Bcl-2
|
B-cell lymphoma
|
|
rhTSLP
|
recombinant human TSLP
|
|
αTSLP
|
anti-human TSLP neutralizing
antibody
|
|
TSLPR
|
TSLP receptor
|
|
E2
|
17-β estradiol
|
|
ER
|
estrogen receptor
|
|
IL
|
interleukin
|
|
ELISA
|
enzyme linked immunosorbent assay
|
|
FCM
|
flow cytometry
|
|
DMEM/F12
|
Dulbecco's modified Eagle's
medium/F12
|
|
FBS
|
fetal bovine serum
|
|
PI
|
propidium iodide
|
References
|
1
|
Kennedy S, Bergqvist A, Chapron C,
D'Hooghe T, Dunselman G, Greb R, Hummelshoj L, Prentice A and
Saridogan E; ESHRE Special Interest Group for Endometriosis and
Endometrium Guideline Development Group, : ESHRE guideline for the
diagnosis and treatment of endometriosis. Hum Reprod. 20:2698–2704.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Sampson JA: Metastatic or embolic
endometriosis, due to the menstrual dissemination of endometrial
tissue into the venous circulation. Am J Pathol. 3:93–110.
1927.PubMed/NCBI
|
|
3
|
Harada T, Kaponis A, Iwabe T, Taniguchi F,
Makrydimas G, Sofikitis N, Paschopoulos M, Paraskevaidis E and
Terakawa N: Apoptosis in human endometrium and endometriosis. Hum
Reprod Update. 10:29–38. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Dufournet C, Uzan C, Fauvet R, Cortez A,
Siffroi JP and Daraï E: Expression of apoptosis-related proteins in
peritoneal, ovarian and colorectal endometriosis. J Reprod Immunol.
70:151–162. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nasu K, Nishida M, Kawano Y, Tsuno A, Abe
W, Yuge A, Takai N and Narahara H: Aberrant expression of
apoptosis-related molecules in endometriosis: A possible mechanism
underlying the pathogenesis of endometriosis. Reprod Sci.
18:206–218. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rizner TL: Estrogen metabolism and action
in endometriosis. Mol Cell Endocrinol. 307:8–18. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Patel BG, Rudnicki M, Yu J, Shu Y and
Taylor RN: Progesterone resistance in endometriosis: Origins,
consequences and interventions. Acta Obstet Gynecol Scand.
96:623–632. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Pellegrini C, Gori I, Achtari C, Hornung
D, Chardonnens E, Wunder D, Fiche M and Canny GO: The expression of
estrogen receptors as well as GREB1, c-MYC, and cyclin D1,
estrogen-regulated genes implicated in proliferation, is increased
in peritoneal endometriosis. Fertil Steril. 98:1200–1208. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Reis FM, Petraglia F and Taylor RN:
Endometriosis: Hormone regulation and clinical consequences of
chemotaxis and apoptosis. Hum Reprod Update. 19:406–418. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rochman Y and Leonard WJ: Thymic stromal
lymphopoietin: A new cytokine in asthma. Curr Opin Pharmacol.
8:249–254. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Liu YJ, Soumelis V, Watanabe N, Ito T,
Wang YH, Malefyt Rde W, Omori M, Zhou B and Ziegler SF: TSLP: An
epithelial cell cytokine that regulates T cell differentiation by
conditioning dendritic cell maturation. Annu Rev Immunol.
25:193–219. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhang Y and Jin LP: Effects of TSLP on
obstetrical and gynecological diseases. Am J Reprod Immunol.
77:2017. View Article : Google Scholar
|
|
13
|
Urata Y, Osuga Y, Izumi G, Takamura M,
Koga K, Nagai M, Harada M, Hirata T, Hirota Y, Yoshino O and
Taketani Y: Interleukin-1β stimulates the secretion of thymic
stromal lymphopoietin (TSLP) from endometrioma stromal cells:
Possible involvement of TSLP in endometriosis. Hum Reprod.
27:3028–3035. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chang KK, Liu LB, Li H, Mei J, Shao J, Xie
F, Li MQ and Li DJ: TSLP induced by estrogen stimulates secretion
of MCP-1 and IL-8 and growth of human endometrial stromal cells
through JNK and NF-kappaB signal pathways. Int J Clin Exp Pathol.
7:1889–1899. 2014.PubMed/NCBI
|
|
15
|
Hayata T, Matsu T, Kawano Y, Matsui N and
Miyakawa I: Scanning electron microscopy of endometriotic lesions
in the pelvic peritoneum and the histogenesis of endometriosis. Int
J Gynaecol Obstet. 39:311–319. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Moen MH and Halvorsen TB: Histologic
confirmation of endometriosis in different peritoneal lesions. Acta
Obstet Gynecol Scand. 71:337–342. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Chang KK, Liu LB, Jin LP, Zhang B, Mei J,
Li H, Wei CY, Zhou WJ, Zhu XY, Shao J, et al: IL-27 triggers IL-10
production in Th17 cells via a c-Maf/RORγt/Blimp-1 signal to
promote the progression of endometriosis. Cell Death Dis.
8:e26662017. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yu JJ, Sun HT, Zhang ZF, Shi RX, Liu LB,
Shang WQ, Wei CY, Chang KK, Shao J, Wang MY and Li MQ: IL15
promotes growth and invasion of endometrial stromal cells and
inhibits killing activity of NK cells in endometriosis.
Reproduction. 152:151–160. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Carvalho L, Podgaec S, Bellodi-Privato M,
Falcone T and Abrão MS: Role of eutopic endometrium in pelvic
endometriosis. J Minim Invasive Gynecol. 18:419–427. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Mei J, Zhu XY, Jin LP, Duan ZL, Li DJ and
Li MQ: Estrogen promotes the survival of human secretory phase
endometrial stromal cells via CXCL12/CXCR4 up-regulation-mediated
autophagy inhibition. Hum Reprod. 30:1677–1689. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhang L, Liu Y, Xu Y, Wu H, Wei Z and Cao
Y: The expression of the autophagy gene beclin-1 mRNA and protein
in ectopic and eutopic endometrium of patients with endometriosis.
Int J Fertil Steril. 8:429–436. 2015.PubMed/NCBI
|
|
22
|
Szymanowski K: Apoptosis pattern in human
endometrium in women with pelvic endometriosis. Eur J Obstet
Gynecol Reprod Biol. 132:107–110. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Bulun SE, Monsavais D, Pavone ME, Dyson M,
Xue Q, Attar E, Tokunaga H and Su EJ: Role of estrogen receptor-β
in endometriosis. Semin Reprod Med. 30:39–45. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bukulmez O, Hardy DB, Carr BR, Word RA and
Mendelson CR: Inflammatory status influences aromatase and steroid
receptor expression in endometriosis. Endocrinology. 149:1190–1204.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Leibowitz B and Yu J: Mitochondrial
signaling in cell death via the Bcl-2 family. Cancer Biol Ther.
9:417–422. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Nishida M, Nasu K, Ueda T, Fukuda J, Takai
N and Miyakawa I: Endometriotic cells are resistant to
interferon-gamma-induced cell growth inhibition and apoptosis: A
possible mechanism involved in the pathogenesis of endometriosis.
Mol Hum Reprod. 11:29–34. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Park LS, Martin U, Garka K, Gliniak B, Di
Santo JP, Muller W, Largaespada DA, Copeland NG, Jenkins NA, Farr
AG, et al: Cloning of the murine thymic stromal lymphopoietin
(TSLP) receptor: Formation of a functional heteromeric complex
requires interleukin 7 receptor. J Exp Med. 192:659–670. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zhong J and Pandey A: Site-directed
mutagenesis reveals a unique requirement for tyrosine residues in
IL-7Rα and TSLPR cytoplasmic domains in TSLP-dependent cell
proliferation. BMC Immunol. 11:52010. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
De Monte L, Reni M, Tassi E, Clavenna D,
Papa I, Recalde H, Braga M, Di Carlo V, Doglioni C and Protti MP:
Intratumor T helper type 2 cell infiltrate correlates with
cancer-associated fibroblast thymic stromal lymphopoietin
production and reduced survival in pancreatic cancer. J Exp Med.
208:469–478. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Pedroza-Gonzalez A, Xu K, Wu TC, Aspord C,
Tindle S, Marches F, Gallegos M, Burton EC, Savino D, Hori T, et
al: Thymic stromal lymphopoietin fosters human breast tumor growth
by promoting type 2 inflammation. J Exp Med. 208:479–490. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ly JD, Grubb DR and Lawen A: The
mitochondrial membrane potential (deltapsi(m)) in apoptosis; an
update. Apoptosis. 8:115–128. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Pu HH, Duan J, Wang Y, Fan DX, Li DJ and
Jin LP: Thymic stromal lymphopoietin promotes the proliferation of
human trophoblasts via phosphorylated STAT3-mediated c-Myc
upregulation. Placenta. 33:387–391. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Kitajima M, Lee HC, Nakayama T and Ziegler
SF: TSLP enhances the function of helper type 2 cells. Eur J
Immunol. 41:1862–1871. 2011. View Article : Google Scholar : PubMed/NCBI
|