Introduction
According to statistics from the World Health
Organization, cardiovascular disease resulted in ~17,100,000 cases
of mortality in 2004, accounting for 29% of total global mortality
(1). This is projected to rise to
23,600,000 by 2030 (1). Cardiac
arrest (CA), which is a common cause of disability and mortality,
is an important threat to human health, and the annual global
incidence of CA is (36-128)/100,000 individuals (2).
In China, the incidence of CA is ~41.8/100,000 and
CA results in ~544,000 cases of mortality annually (3), which is the highest rate worldwide.
In addition, at present, only 1% of patients with CA occurring
outside a hospital environment survive (4). Therefore, CA is considered a major
issue that requires attention worldwide.
With the increasing public knowledge of
cardiopulmonary resuscitation (CPR), the continued improvement of
rescue technology, and improvements to emergency network
construction, the probability of a patient with CA occurring
outside a hospital environment to recover due to restoration of
spontaneous circulation (ROSC) is increasing (5). However, patients with CA who undergo
CPR outside a hospital environment may suffer ischemic-hypoxic
injury, particularly in the vulnerable regions of the hippocampus,
cortex, thalamus and cerebellum. Ischemia may occur even if ROSC is
achieved, and may result in necrosis and apoptosis of neurons,
thereby leading to neurological damage and disorders including
learning difficulties, anterograde amnesia, coma, a persistent
vegetative state or mortality (6–9). The
success or failure of brain recovery may be dependent on the
quality of life of patients. In addition, numerous researchers
advocate a change from CPR to cardiopulmonary cerebral
resuscitation (CPCR). However, how to conduct CPCR so as to reduce
or avoid neuronal damage and promote neurological recovery remains
to be elucidated.
Mesenchymal stem cells (MSCs) are bone
marrow-derived non-hematopoietic stem cells, which have been
successfully applied in various types of tissue repair, first
observed by Friedenstein et al in 1976 (10). MSCs have the potential for
multi-directional differentiation, and can self-renew and
differentiate into numerous types of cell depending on the
microenvironment, including osteoblasts, chondroblasts, adipocytes
and muscle cells (11,12).
Previous studies have focused on the application of
MSCs for the repair of nerve tissue in models of focal cerebral
ischemia; however, whole brain ischemic injury may occur following
CA (13,14). There have been few studies
regarding MSC transplantation for the treatment of global ischemia,
particularly as a result of CA; however, they may reduce brain
damage and improve neurological function (15–17).
A previous study investigated MSC transplantation into the brain
and demonstrated that MSCs were able to differentiate into
neuron-like cells (18). The MSCs
were administered to a rat model following CPR via vascular
pathways, using magnetic resonance imaging in vivo tracking
technology to observe the MSCs passing through the blood-brain
barrier. MSCs have been shown to undergo directional migration to
the hippo-campus and temporal cortex, regions that are particularly
vulnerable following global cerebral ischemia (19), and have been shown to reduce brain
tissue damage to these areas, which may promote functional recovery
(20).
In the present study, MSCs were labeled with
4′6-diamidino-2-phenyl-indole (DAPI) fluorescent dye and
transplanted into rats following CPR using one of three methods:
Stereotaxic infusion into the lateral ventricle (LV), infusion to
the internal carotid artery (A), and infusion to the femoral vein
(V). The migration and distribution of MSCs in the brain, and their
effects on brain cell damage and neurological recovery were
observed. Furthermore, the effects of various methods of MSC
transplantation on cerebral resuscitation of the rats following CA
were investigated, in order to screen the most effective migratory
pathway.
Materials and methods
Experimental animals
A total of 40 Sprague-Dawley (SD) rats (age, 4–5
weeks; weight, 100–150 and 300–400 g) were obtained from the
Laboratory Animal Center of Sun Yat-sen University (Guangdong,
China). Their housing conditions consisted of a 12 h light/dark
cycle, 40–70% humidity (20–24°C) and ad libitum access to
food and water. The study was approved by the Animal Ethics
Committee of Sun Yat-sen University.
Culture of MSCs
In the present study, the method of adherent cell
culture was adopted. SD rats were anesthetized using CO2
inhalation and sodium pentobarbital (45 g/l; 0.1 ml/100 g;
Sigma-Aldrich, St. Louis, MO, USA) intraperitoneal injection prior
to their sacrifice by cervical dislocation. Then, rats were placed
into 75% ethanol for ~5 min for disinfection. Subsequently, the
rats were removed from the ethanol under sterile conditions, and in
a laminar flow cabinet, lower limb muscles and soft tissue were
cut, and the femur and tibia from each side were removed and placed
in petri dishes.
The ends of the femur and tibia were cut and flushed
with fetal calf serum-free Dulbecco's modified Eagle's medium
(DMEM; Gibco; Thermo Fisher Scientific, Inc., Waltham, MA,
USA)/Ham's F12, the bone marrow cavity was repeatedly washed until
the entire bone marrow cavity was white.
The fluid used for flushing was placed into a
centrifuge tube and centrifuged at 600 × g for 5 min. The
supernatant was removed and thoroughly mixed with DMEM (8 ml for
each rat) following centrifugation. The mixture (4 ml) was placed
into 25-cm2 flasks and stored in three incubators at
37°C in an atmosphere containing 5% CO2 with saturated
humidity. After 24 h, half the media were changed, and after 48 h,
all of the media were changed, this was repeated every other day
throughout the experiment. The media were aspirated when the cells
had grown to 90% cell confluence (~6–7 days), and the flask was
rinsed once with phosphate-buffered saline (PBS). Trypsin (0.25%, 3
ml) containing 0.1 mmol/l EDTA was added to the culture flasks for
2 min. Trypsin digestion was observed under an inverted microscope
(T2000U; Nikon Corporation, Tokyo, Japan); when the MSCs were round
and separated, DMEM was added to terminate the digestion.
The media were removed and the flask was washed,
prior to centrifugation at 600 × g for 5 min. The supernatant was
removed and the cell pellet was resuspended in DMEM (1:2,
respectively). This process was repeated when the culture next
reached ~90% confluence (~2–3 days). Cells from passage 3 (P3) were
digested with 0.25% trypsin and washed three times with PBS.
Fluorescent-labeled antibodies against cluster of differentiation
(CD)44 (cat. no. 561860), CD34 (cat. no. 551387), CD45 (cat. no.
561087) and CD90 (cat. no. 553012) (all diluted 1:250; all
purchased from BD Pharmigen, San Diego, CA, USA) were added and
incubated at 4°C for 30 min. The unbound antibodies were removed by
washing with PBS, and the cells were fixed with 1% paraformaldehyde
(Sigma-Aldrich) for 15 min. Surface antigen expression of the MSCs
was detected by flow cytometry (BD FACSCalibur; BD Biosciences,
Franklin Lakes, NJ, USA).
In addition, MSCs from P3 were stained with 4 ml
DMEM supplemented with nuclear stain solution containing 50
μg/ml DAPI (Biomol GmbH, Hamburg, Germany) for 2 h at 37°C
in a humidified incubator containing 5% CO2. After
staining with DAPI, the MSCs were observed under a fluorescence
microscope (Nikon Eclipse TiU; Nikon Corporation). These cells were
then prepared for transplantation.
Grouping
Prior to the establishment of a CA resuscitation
model, rats were randomly divided into four groups, which were
subdivided into 3 and 7 day subgroups. Asphyxiation was used to
generate a CA resuscitation model. The groups (n=8) were as
follows: i) Control group, rats received CPR without MSC
transplantation; ii) LV group, MSC transplantation was performed
into the lateral ventricle with a stereotaxic instrument following
ROSC; iii) A group, MSC transplantation via the inner side of the
carotid artery following ROSC; and iv) V group, MSC transplantation
was performed via the side of the femoral vein following ROSC. In
each transplantation group, MSC transplantation was conducted with
~1×106 cells 1 h after ROSC.
Transplantation process
Healthy male SD rats (weight, 300–400 g) underwent
fasting for 24 h with ad libitum access to water prior to
development of the model. Prior to surgery, anesthesia was induced
by CO2 inhalation and sodium pentobarbital (45 g/l; 0.1
ml/100 g) intraperitoneal injection. Bilateral skin preparation was
performed on the chest, back and groin of the rats, which were
fixed on the operating table in the supine position. Tracheal
intubation was conducted using a medical ear, nose and throat
mirror and a focus light under direct vision. The tracheal tube was
fixed to the lower lip area following successful tracheal
intubation and attached to a CO2 concentration monitor
(Capstar-100; CWE, Inc., Ardmore, PA, USA), in order to
continuously monitor end-expiratory carbon dioxide
(ETCO2) levels. Following disinfection, the lower limb
was cut and the femoral artery was dissected and ligated with a
surgical suture, subsequent to blocking the ophthalmic artery blood
flow with tweezers. A cut was made above the femoral artery
ligation point with ophthalmic scissors, and a heparinzation
polyethylene pipe (Beckton Dickinson UK, Ltd., Oxford, UK) was
inserted into the cut and into the thoracic aorta along the femoral
artery (3–4 cm). Subsequently, the ductus arteriosus was fixed with
a suture and the arterial catheter was connected to a multichannel
analyzer (Spacelabs Healthcare, Snoqualmie, WA, USA) containing
pressure sensors for physiological parameters, for the continuous
monitoring of mean arterial pressure (MAP). A temperature sensor
was inserted into the anus of the rats at a depth of 3–4 cm for
continuous monitoring of temperature changes and a metal needle was
inserted subcutaneously in the upper limbs and the left lower limb
and connected to an electrocardiography (ECG) machine (Spacelabs
Healthcare) for continuous ECG monitoring.
Therapeutic agent-induced asphyxiation
and CA resuscitation procedures
Following surgery, the rats were allowed to fully
awaken and baseline physiological parameters were recorded. A
respiratory inhibitor, vecuronium (Zhejiang Xianju Pharmaceutical
Co., Ltd., Taizhou, China), was injected at a concentration of 1.0
mg/kg in the designated door of a T-branch pipe connected to the
arterial catheter. A total of 10 sec after injection, the rats
gradually stopped breathing. Subsequently, changes in blood
pressure were observed in the rats; reduced MAP to 20 mmHg in 4–5
min is considered a criterion for CA. The ventilator was opened and
adjusted, and the device parameters for chest compression were set
to ensure the pressing head was adjusted to the lower sternum of
the rat and the lower end was located on the top 2.5 cm of the
xiphoid. Following 5 min and 45 sec of CA, the endotracheal tube
was connected to the ventilator with oxygen ventilation, a tidal
volume of 0.6 ml/100 g and a respiratory rate of 100 beats/min.
Following 6 min of CA, the chest compressions were conducted using
a CPR device (developed independently by the Institute of
Cardiopulmonary Cerebral Resuscitation, Sun Yat-sen University)
with a pressing frequency of 200 times/min, a ratio of pressing to
ventilation of 2:1 and a compression depth of 1/3 of the
anteroposterior diameter. Following 2 min of compression, 0.1 ml
adrenaline was injected via the femoral artery with 0.1 ml saline
and heparin. Continuous chest compressions and ventilation were
conducted until the MAP was maintained at >60 mmHg for 5 min,
which is a criteria for ROSC. Pure oxygen aeration was conducted
for 15 min, followed by mechanical ventilation with 50% oxygen. If,
following 5 min of chest compressions, the rats failed to achieve
ROSC, the recovery was considered a failure and the rat was
excluded from the study. Following ROSC, the rats received
continuous mechanical ventilation for a further 30 min and
hemodynamic changes were continuously monitored.
Transplantation of MSCs following
recovery
DAPI-labeled MSCs were administered to the rats 1 h
after ROSC according to their groups via the lateral cerebral
ventricles using a stereotaxic instrument, via the internal carotid
artery, or by femoral vein injection. Subsequently, all catheters
were removed and 250 g/l (0.2 ml) cephalosporin VI (Beijing
Tsinghua Unisplendour Pharmaceutical Factory, Beijing, China) was
administered by intramuscular injection, and the rats were returned
to the animal cages. On the first day following ROSC, rats were
housed indoors individually, maintained at room temperature (~25°C)
and artificially fed every 6 h with 5% dextrose saline injection.
After 3 days the rats were allowed to return to the group cage.
Detailed records of survival following ROSC were
kept. At the end of the experiment, the rat mortality and time, and
survival rates were statistically analyzed.
Assessment of neurological function in
rats
The experimental rats were scored on days 1, 3 and 7
following ROSC using the Neurological Deficit Scores (NDS) as a
standard (21). NDS were used to
grade brain functions, such as awakening, cranial nerve reflex,
motor function and the simple act of reflection. Scores range from
0 to 80 points; a score of 0 represents brain death and a score of
80 represents normal brain function.
Pathological examination of the
hippocampus and temporal cortex
Normal, healthy, nerve cells were cut using a
microtome (Leica RM2235; Leica Biosystems, Wetzlar, Germany) and
sections (4 μM) were stained with hematoxylin and eosin
(H&E; Wuhan Boster Biotechnology, Ltd., Wuhan, China) and
observed under a microscope (T2000U; Nikon, Tokyo, Japan).
Blood specimen collection
Anesthesia was induced with CO2 and the
rats were then sacrificed using an intraperitoneal injected of
sodium pentobarbital (45 g/l; 0.1 ml/100 g). The rats were fixed on
an operating table, the abdominal wall was opened and the inferior
vena cava was separated. A syringe was used to take 5 ml blood
samples from the inferior vena cava, the blood samples were then
injected into a drying tube for 10 min, and centrifuged at 1,200 ×
g for 15 min. The supernatant was placed into a centrifuge tube and
maintained at −80°C to preserve the S100 calcium-binding protein B
(S100B) levels in the serum, which were uniformly analyzed at the
end of the experiment.
Detection of brain water content
After blood specimens were collected, the chest was
exposed and paraformaldehyde was injected from the internal carotid
artery to the brain, until the superior vena cava returned clear
paraformaldehyde. Following paraformaldehyde perfusion, the rats
were cervically dislocated, the skull was opened and the right side
of the brain was removed. The right side of the brain was removed
and the wet-weight was determined using an analytical balance. The
tissue was then dried in an oven at 105°C for 48 h and the dry
weight was measured. The water content of the brain was calculated
according to the Elliot formula: Wet weight - dry weight)/wet
weight × 100%. Determination of S100B protein in the sera was
conducted using an enzyme-linked immunosorbent assay (ELISA; Wuhan
Huamei Biotech Co., Ltd., Wuhan, China).
Statistical analysis
Statistical analyses were conducted using SPSS
version 20.0 for Mac (IBM SPSS, Armonk, NY, USA) and the data are
presented as the mean ± standard deviation. Groups were compared
using analysis of variance and the χ2 test. P<0.05
was considered to indicate a statistically significant
difference.
Results
Isolation, cultivation and identification
of MSCs
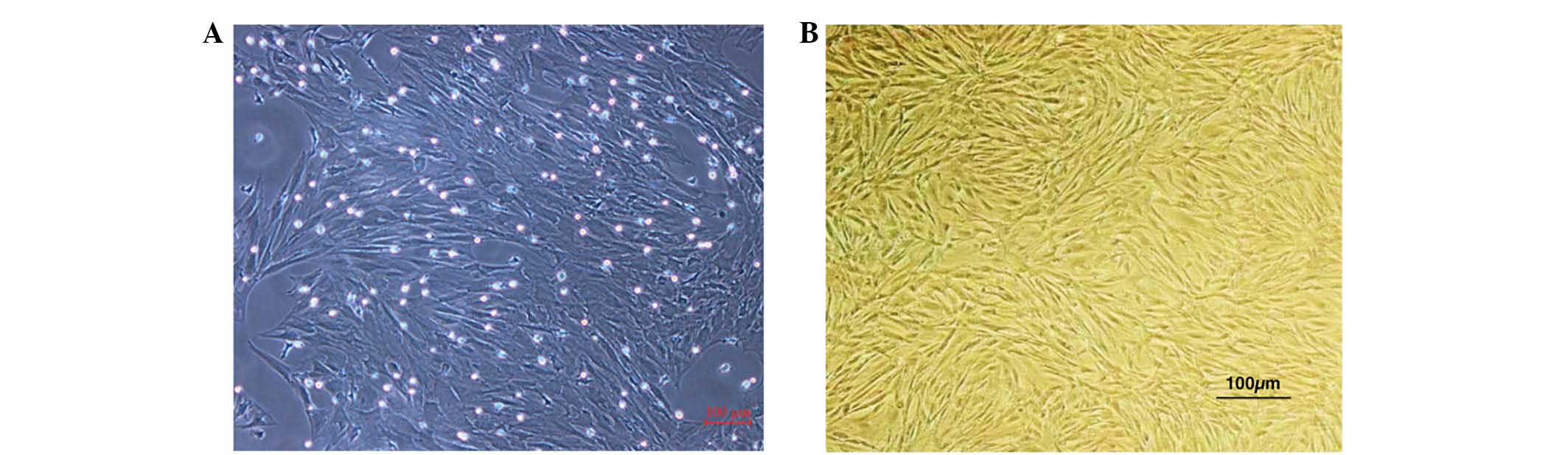
The P3 MSCs demonstrated uniform cell morphology as
presented in Fig. 1A and B.
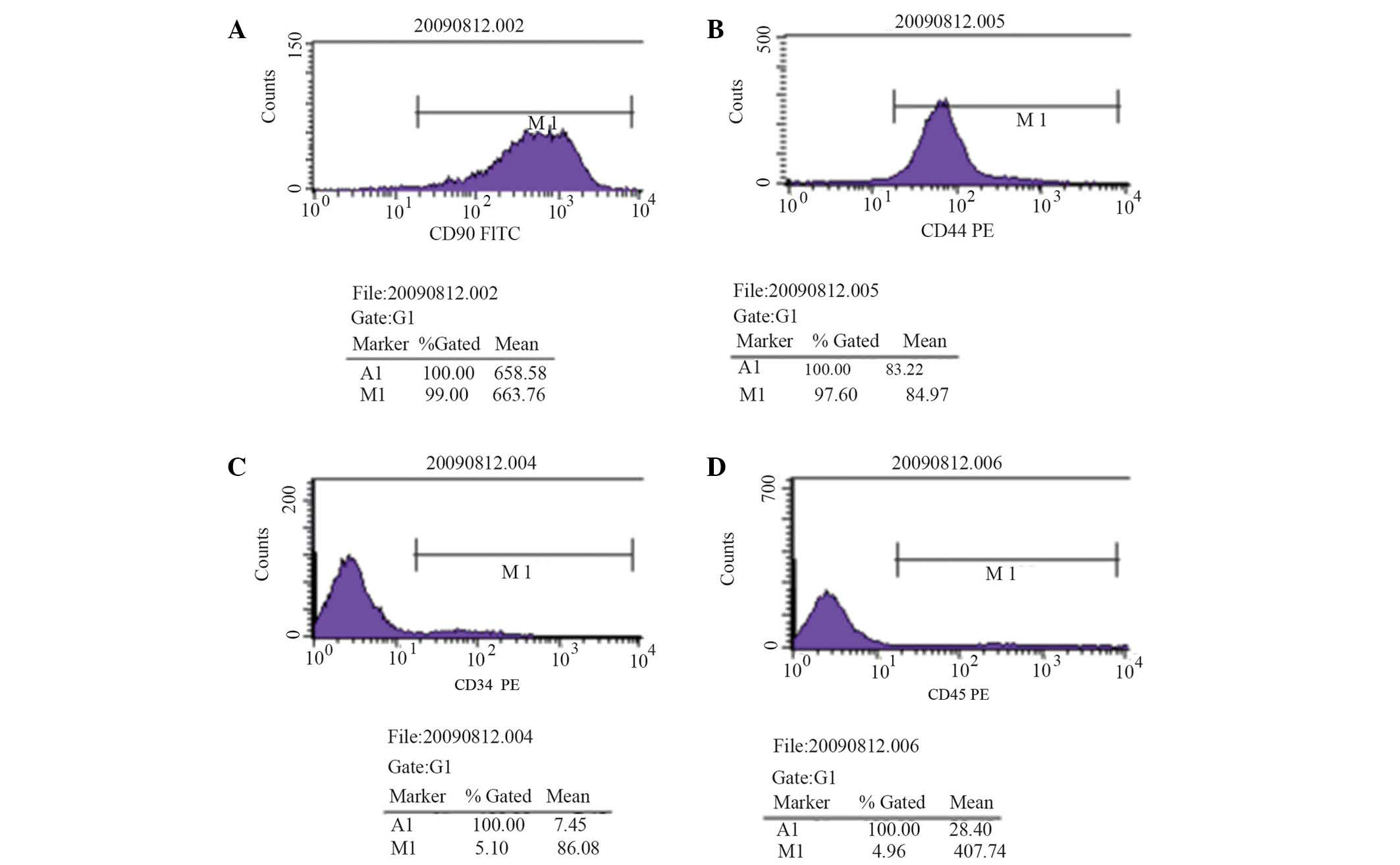
Stromal cell surface markers were detected by flow cytometry; CD90
expression was detected in 99.00% of cells and CD44 expression was
detected in 97.60% of cells (Fig. 2A
and B). Hematopoietic cell surface markers were also observed;
CD34 expression was detected in 5.10% of cells and CD45 expression
was detected in 4.96% of cells (Fig.
2C and D). These results indicate that MSCs obtained in the
present study were of a high purity following isolation, culture
and passage.
Observation of MSCs fluorescently labeled
with DAPI
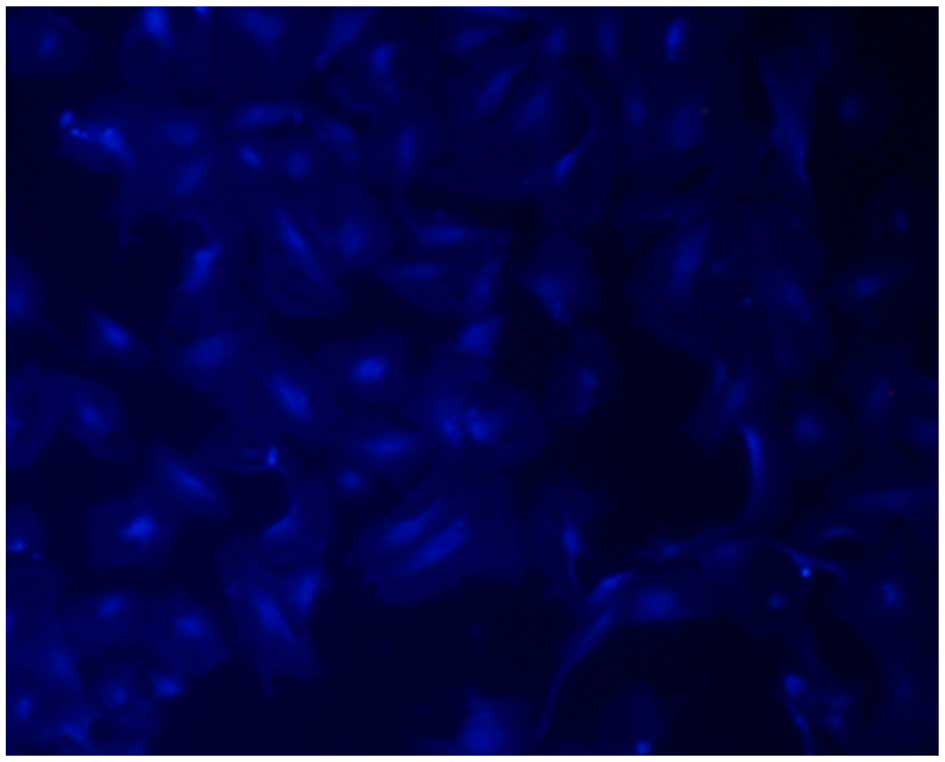
The transplanted MSCs were observed under a
fluorescence microscope, the results demonstrated that the rate of
DAPI staining was 99%, suggesting that DAPI may be used as a tracer
to label MSCs for in vivo transplantation (Fig. 3).
Monitoring of recovering rats
Physiological parameters were monitored in each
group prior to and 5, 10, 20 and 30 min following ROSC. As
presented in Tables I and II, there were no significant differences
between the MAP, heart rate and ETCO2 of rats in each
group at the end of the surgical procedure or after ROSC.
 | Table IComparison of baseline MAP, HR and
ETCO2 levels in each group (mean ± standard
deviation). |
Table I
Comparison of baseline MAP, HR and
ETCO2 levels in each group (mean ± standard
deviation).
| Group | MAP (mmHg) | HR (bpm) | ETCO2
(mmHg) |
|---|
| Control (n=8) | 133.63±11.19 | 383.50±15.03 | 35.34±4.32 |
| V (n=8) | 129.13±8.43 | 389.25±19.61 | 39.01±6.70 |
| A (n=8) | 133.25±9.49 | 400.38±16.55 | 38.85±5.68 |
| LV (n=8) | 122.75±9.94 | 388.87±25.40 | 37.51±6.42 |
| F-value | 2.121 | 1.051 | 0.674 |
| P-value | 0.120 | 0.386 | 0.575 |
 | Table IIComparison of MAP, HR and
ETCO2 levels in each group at various time-points
following ROSC (mean ± standard deviation). |
Table II
Comparison of MAP, HR and
ETCO2 levels in each group at various time-points
following ROSC (mean ± standard deviation).
| Parameter | Time (ROSC) | Group Con
(n=8) | Group V (n=8) | Group A (n=8) | Group LV (n=8) | F-value | P-value |
|---|
| MAP (mmHg) | 5 min | 113.63±19.09 | 119.13±26.64 | 136.38±15.73 | 127.00±12.03 | 2.136 | 0.118 |
| 10 min | 134.13±21.86 | 122.20±15.12 | 140.45±13.52 | 135.33±20.32 | 1.465 | 0.246 |
| 20 min | 107.58±23.09 | 101.08±15.56 | 111.92±14.27 | 110.96±13.18 | 0.667 | 0.580 |
| 30 min | 103.75±10.36 | 98.63±9.04 | 102.50±7.39 | 101.81±10.39 | 0.340 | 0.797 |
| HR (bpm) | 5 min | 308.13±25.72 | 295.38±19.84 | 312.13±31.48 | 307.50±23.35 | 0.646 | 0.592 |
| 10 min | 322.75±44.44 | 313.75±30.70 | 316.75±28.47 | 310.38±26.95 | 0.205 | 0.892 |
| 20 min | 285.89±36.42 | 285.25±44.56 | 306.00±14.98 | 308.38±27.69 | 1.167 | 0.340 |
| 30 min | 289.00±35.96 | 293.50±31.38 | 303.63±11.09 | 304.63±20.82 | 0.304 | 0.822 |
| ETCO2
(mmHg) | 5 min | 50.98±12.40 | 53.11±6.70 | 60.46±7.33 | 56.49±10.19 | 1.542 | 0.225 |
| 10 min | 50.61±8.42 | 52.51±8.42 | 57.78±8.45 | 55.94±7.97 | 1.215 | 0.323 |
| 20 min | 56.99±5.25 | 59.11±7.32 | 60.15±8.94 | 51.83±8.67 | 1.854 | 0.160 |
| 30 min | 49.38±5.59 | 52.38±5.57 | 57.78±6.13 | 53.00±7.65 | 2.441 | 0.085 |
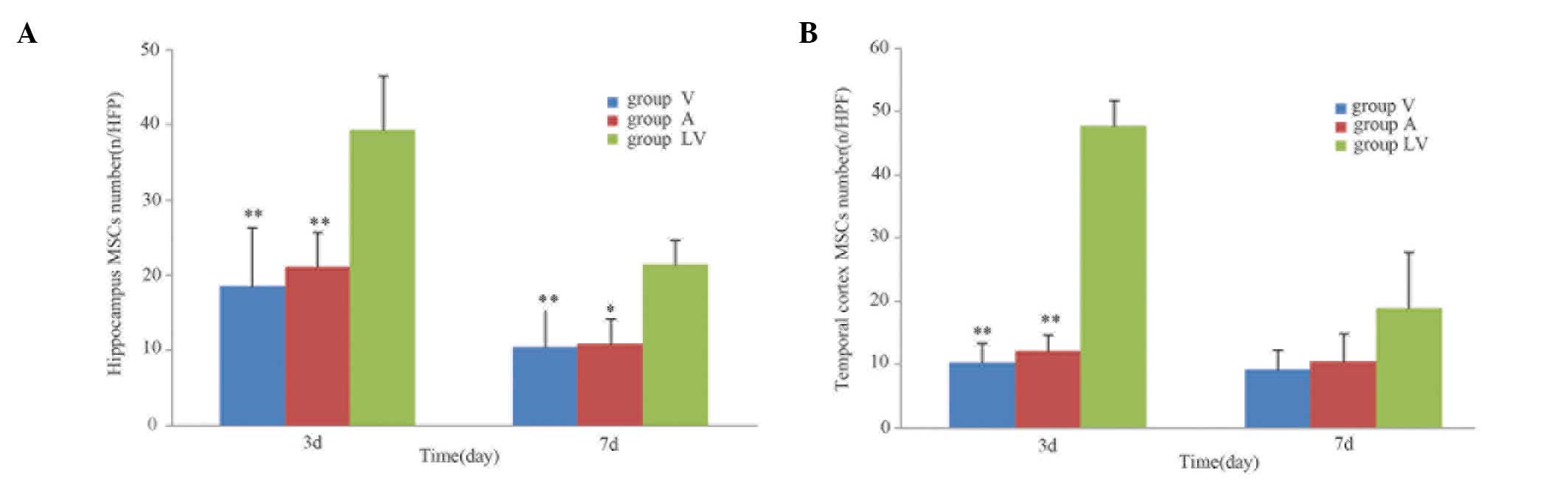
Distribution and migration of
transplanted MSCs
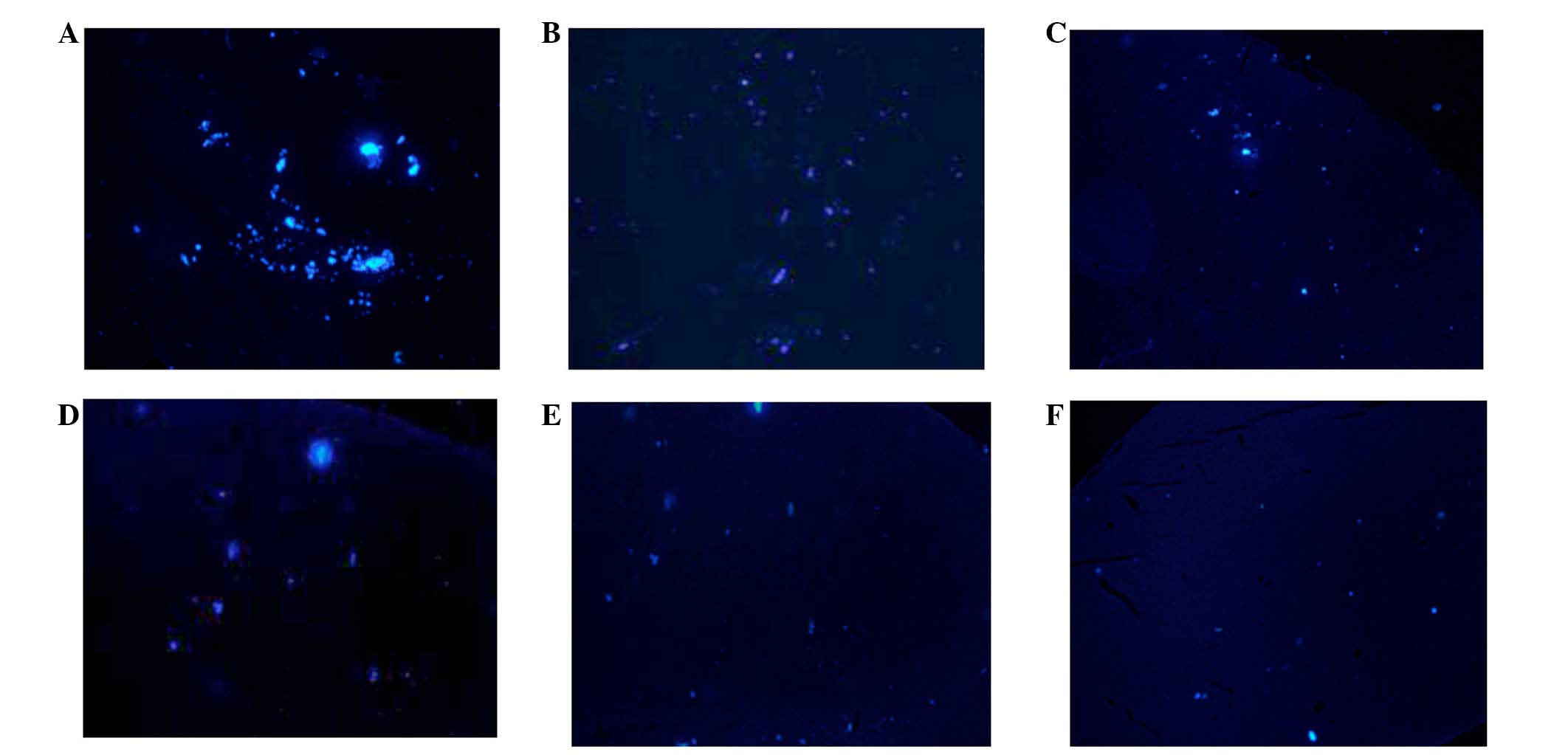
Following transplantation of MSCs, the blue
fluorescent-labeled cells were observed in the brain on day 3
post-ROSC. The MSCs were predominantly distributed in the
hippocampus and temporal cortex, which is consistent with global
cerebral ischemia. On day 3 following ROSC, the number of MSCs in
the LV group was significantly greater, as compared with the A and
V groups (P<0.01). There was no significant difference between
the A and V groups (P>0.05). On day 7 following ROSC, a greater
number of MSCs in the LV group were observed in the hippocampal
region, as compared with in the A and V groups (P<0.05);
however, there was no difference in the number of MSCs in the
temporal cortex regions between the various transplant groups
(P>0.05; Figs. 4 and 5).
Measurement of physiological parameters
in experimental rats
Mortality rate
One rat in the control group survived only 1 day
following ROSC; however, there were no mortalities in the
experimental groups.
Weight
The weight of the rats declined in each group
following ROSC; however, differences in weight between days 3 and
7, and prior to the experiment were not statistically significant
(P>0.05; Table III).
 | Table IIIComparison of weight following
recovery at various time-points among the groups (mean ± standard
deviation). |
Table III
Comparison of weight following
recovery at various time-points among the groups (mean ± standard
deviation).
| Time | Group Con | Group V | Group A | Group LV | F-value | P-value |
|---|
| Prior to
recovery | 364.87±19.67 | 348.78±20.65 | 348.50±23.88 | 351.87±22.99 | 0.87 | 0.47 |
| ROSC 3 days | 321.37±21.66 | 308.65±19.64 | 310.78±26.41 | 308.13±27.00 | 0.47 | 0.70 |
| ROSC 7 days | 277.00±10.12 | 273.75±11.78 | 287.00±10.93 | 285.75±19.07 | 0.72 | 0.57 |
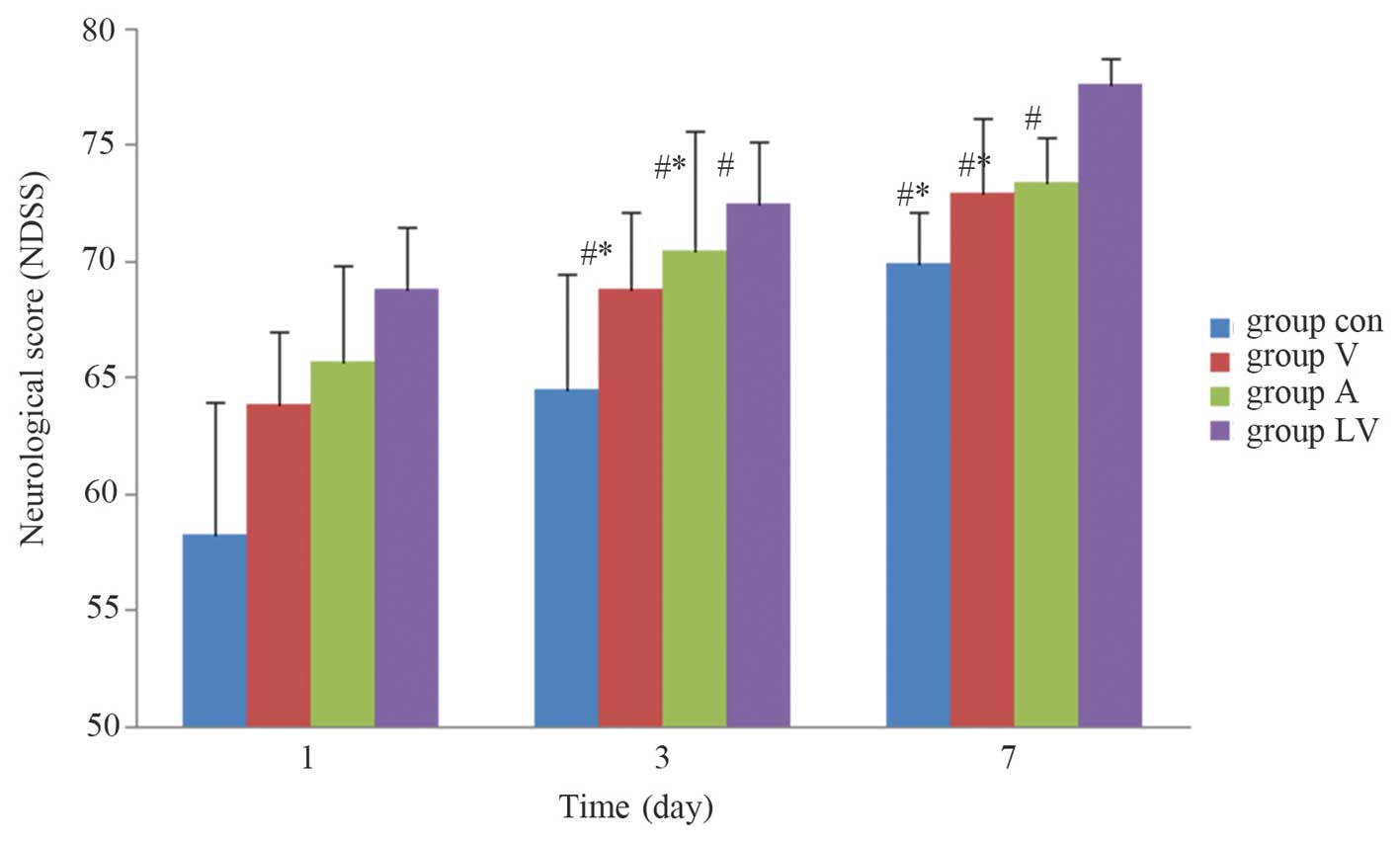
NDSS
Neurological scores of the rats were not
statistically different among the groups 1 day after ROSC
(P>0.05). However, 3 and 7 days after ROSC, the NDSS were
significantly higher in the MSC transplantation groups, as compared
with those in the control group (P<0.05), and were significantly
higher in the LV group than in the A and V groups (P<0.05).
There was no significant difference between the A and V groups
(P>0.05; Fig. 6).
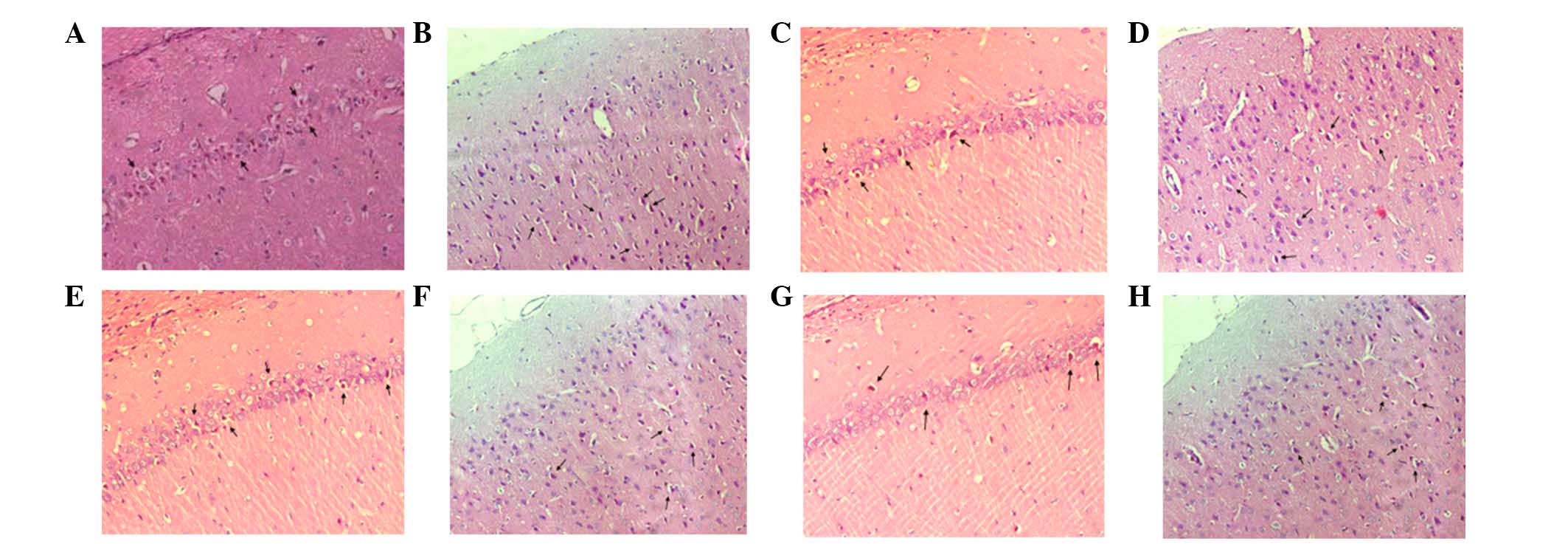
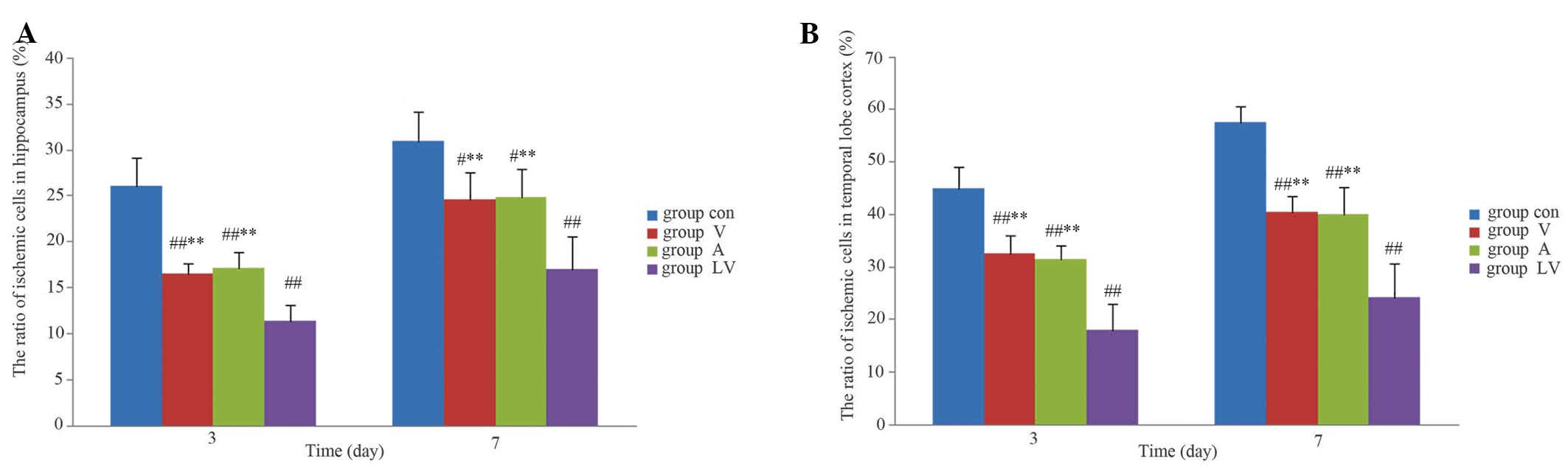
Pathological examination of the
hippocampus and temporal cortex with HE staining
Following staining of the normal, healthy, nerve
cells with HE they were observed under a microscope; nuclei were
stained lightly, no vacuoles were observed, and axons visibly
extended to the surrounding cells. However, rats with global
cerebral ischemia following CPR exhibited nerve cell damage visible
in regions of the hippocampus and the temporal cortex. The damage
was demonstrated predominantly by nuclear condensation, and
vacuolar alterations around the nucleus, which was were called
eosinophilic-like changes (Fig.
7). The number of cells exhibiting these changes were
significantly lower in the hippocampus and temporal cortex of the
MSC transplantation groups, as compared with in the control group
(P<0.01). In addition, nerve damage was significantly reduced in
the LV group, as compared with in the A and V groups (P<0.01);
however, there was no significant difference between the A and V
groups (P>0.05; Fig. 8).
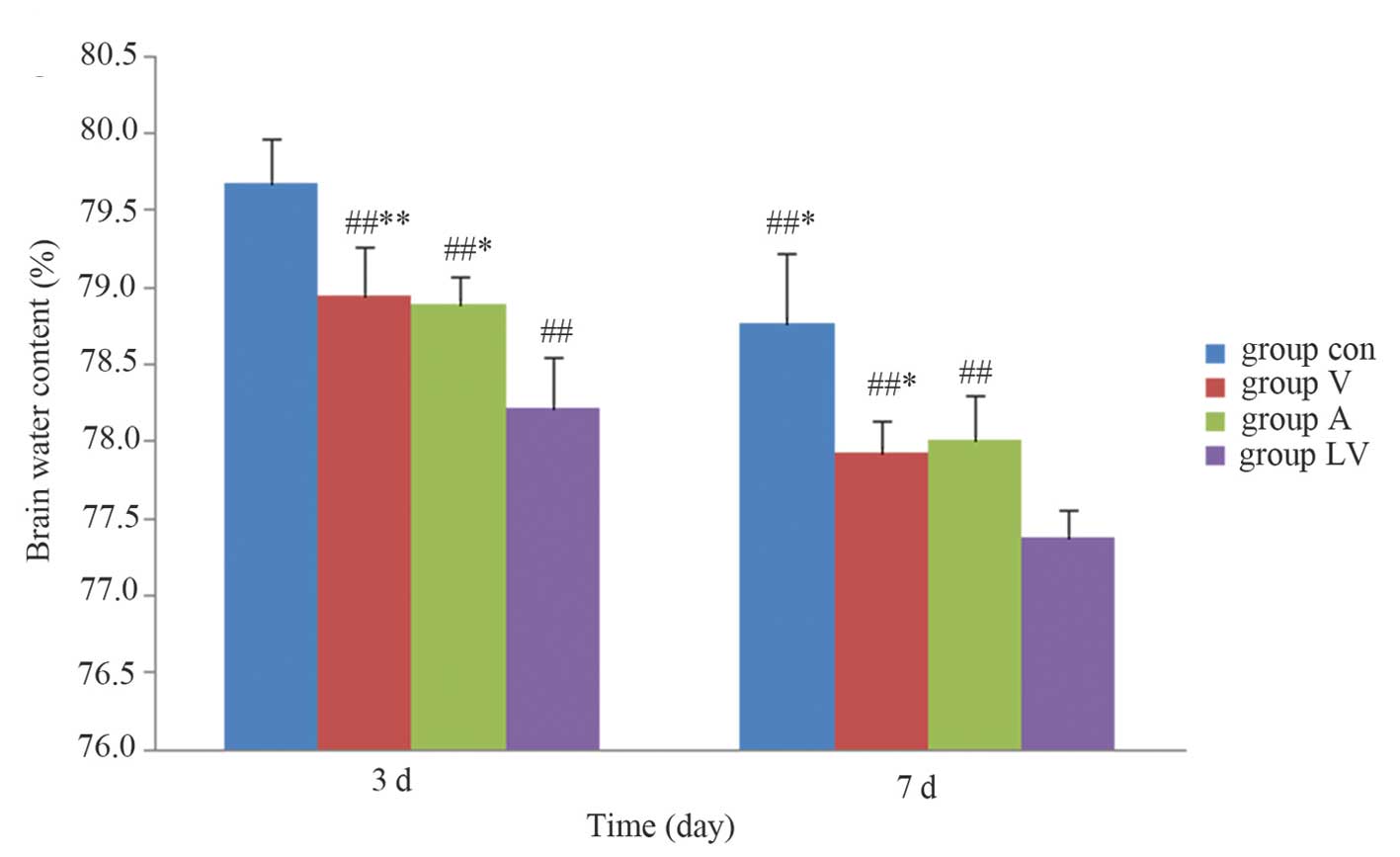
Detection of brain water content
The brain water content was significantly lower in
the MSC groups than in the control group 3 and 7 days after ROSC
(P<0.01). The content was significantly lower in the LV group
than in group A (P<0.05) and group V (P<0.01) on day 3
following ROSC. In addition, brain water content was significantly
lower in the LV group, as compared with in the A and V groups
(P<0.05) 7 days following ROSC; however, there were no
significant differences between groups A and V at either time
(P>0.05; Fig. 9).
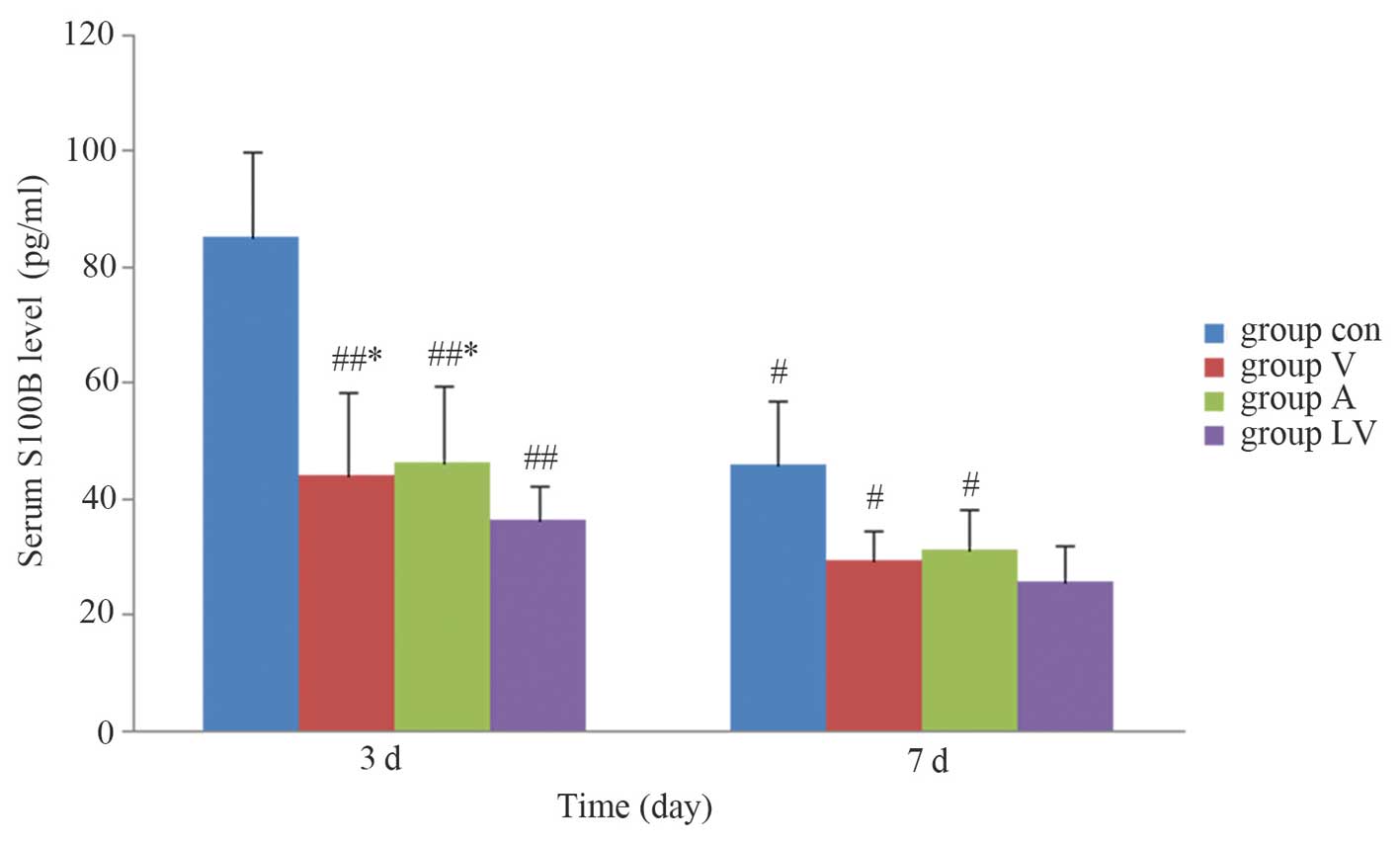
Detection of serum S100B levels by
ELISA
Serum S100B levels were significantly increased in
each group after ROSC. Serum S100B levels were significantly lower
in each of the MSC transplantation groups, as compared with in the
control group 3 and 7 days after ROSC (P<0.05), serum S100B
levels were significantly lower in the LV group than in groups A
and V 3 days after ROSC (P<0.05); however, there was no
significant difference between groups A and V (P>0.05). S100B
levels had decreased in each group 7 days after ROSC; however,
there were no significant differences amongst the LV, A and V
groups (P>0.05; Fig. 10).
Discussion
Global cerebral ischemia is a serious complication
following CA, which directly affects patient prognosis following
CPR. MSC transplantation is a novel therapeutic strategy used to
treat ischemic injury, which has been used in the treatment of
cerebral infarction and other nervous system diseases to
therapeutic benefit (11). At
present, very few studies have focused on MSC transplantation
therapy for CA-induced global cerebral ischemia; however, previous
studies have indicated that MSC transplantation may reduce brain
damage and improve neurological function (12,22,23).
In the present study, DAPI-positive MSCs were predominantly
observed in the regions of serious ischemic injury and in areas
surrounding the hippocampus and temporal cortex 3 and 7 days after
transplantation. In each MSC transplantation group, other parts of
the brain exhibited no staining, indicating that the MSCs undergo
regional distribution; these results are consistent with those of a
previous in vitro study (24).
Pathological examination demonstrated that the
number of damaged neurons in ischemic areas of the brain was
significantly increased following CPR. Cell damage was
predominantly pyknotic, and changes to the distribution of dye
around the nucleus were detected after HE staining. The proportion
of injured neurons in the hippocampus and temporal cortex was lower
in the MSC transplantation groups, as compared with in the control
group, thus suggesting that MSC transplantation may improve global
ischemic injury and further promote recovery. The present study
also demonstrated that brain water content was lower in the MSC
transplantation groups than in the control group 3 and 7 days
post-transplantation with MSCs, thus indicating that MSCs may also
exert a therapeutic effect on brain edema.
The results of the present study demonstrated that
the NDSS of rats in the MSC transplantation groups were higher than
in the control group 3 and 7 days after ROSC, and the NDSS were
close to normal levels by day 7.
S100B protein, which is predominantly distributed in
the glial and Schwann cells, is an injury-specific protein that
appears following damage to the central nervous system (25). Hypoxic-ischemia injury to the brain
may result in secondary damage to the blood-brain barrier,
resulting in the release of S100B protein from the damaged nerve
and glial cells into the blood circulation, thus causing increased
serum levels. Measuring the levels of S100B following CA assesses
the extent of brain damage, which is more sensitive for predicting
the recovery of neurological function (26,27).
Results from the present study demonstrated that the protein levels
of serum S100B in each group were significantly increased following
ROSC; however, they were significantly decreased in the MSC
transplantation groups, as compared with in the control group 3 and
7 days after ROSC.
In conclusion, MSCs may improve neurological
recovery following injury via the repair of ischemic brain tissue.
The present study indicated that MSC transplantation following CA
and CPR had therapeutic benefits on global cerebral ischemia
injury, and provides a basis for animal experiments regarding MSC
transplantation for the recovery of brain function in patients with
CA.
Acknowledgments
The present study was supported in part by a
research grant from the Guangdong Provincial Department of Science
and Technology of China (grant no. 2012B03180045).
References
|
1
|
Thom T, Haase N, Rosamond W, Howard VJ,
Rumsfeld J, Manolio T, Zheng ZJ, Flegal K, O'Donnell C, Kittner S,
et al: Heart disease and stroke statistics - 2006 update: A report
from the American Heart Association Statistics Committee and Stroke
Statistics Subcommittee. Circulation. 113:e85–e151. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Grounds MD, White JD, Rosenthal N and
Bogoyevitch MA: The role of stem cells in skeletal and cardiac
muscle repair. J Histochem Cytochem. 50:589–610. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Grove JE, Lutzko C, Priller J, Henegariu
O, Theise ND, Kohn DB and Krause DS: Marrow-derived cells as
vehicles for delivery of gene therapy to pulmonary epithelium. Am J
Respir Cell Mol Biol. 27:645–651. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Huang Zi-Tong: Improve the level of
cardiopulmonary resuscitation measures and countermeasures.
Zhonghuajizheny-ixuezazhi. 3:153–154. 2004.
|
|
5
|
Bindslev L, Haack-Sørensen M, Bisgaard K,
Kragh L, Mortensen S, Hesse B, Kjaer A and Kastrup J: Labelling of
human mesenchymal stem cells with indium-111 for SPECT imaging:
Effect on cell proliferation and differentiation. Eur J Nucl Med
Mol Imaging. 33:1171–1177. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wen M and Li SL: The studies of magnetic
resonance imaging for molecular imaging. Zhongguo Yixue Yingxiang
Jishu. 1:147–150. 2007.In Chinese.
|
|
7
|
Jing XH, Yang L, Duan XJ, Xie B, Chen W,
Li Z and Tan HB: In vivo MR imaging tracking of magnetic iron oxide
nanoparticle labeled, engineered, autologous bone marrow
mesenchymal stem cells following intra-articular injection. Joint
Bone Spine. 75:432–438. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Fang X, Tang W, Sun S, Huang L, Huang Z
and Weil MH: Mechanism by which activation of delta-opioid receptor
reduces the severity of postresuscitation myocardial dysfunction.
Crit Care Med. 34:2607–2612. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hickey RW, Kochanek PM, Ferimer H,
Alexander HL, Garman RH and Graham SH: Induced hyperthermia
exacerbates neurologic neuronal histologic damage after asphyxial
cardiac arrest in rats. Crit Care Med. 31:531–535. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Friedenstein AJ, Chailakhyan RK and
Gerasimov UV: Bone marrow osteogenic stem cells: In vitro
cultivation and transplantation in diffusion chambers. Cell Tissue
Kinet. 20:263–272. 1987.PubMed/NCBI
|
|
11
|
Joshi D and Behari M: Neuronal stem cells.
Neurol India. 51:323–328. 2003.PubMed/NCBI
|
|
12
|
Zheng W, Honmou O, Miyata K, Harada K,
Suzuki J, Liu H, Houkin K, Hamada H and Kocsis JD: Therapeutic
benefits of human mesenchymal stem cells derived from bone marrow
after global cerebral ischemia. Brain Res. 1310:8–16. 2010.
View Article : Google Scholar
|
|
13
|
Chen J, Li Y, Katakowski M, Chen X, Wang
L, Lu D, Lu M, Cautam SC and Chopp M: Intravenous bone marrow
stromal cell therapy reduces apoptosis and promotes endogenous cell
proliferation after stroke in female rat. J Neurosci Res.
73:778–786. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Li Y, Chopp M, Chen J, Wang L, Gautam SC,
Xu YX and Zhang Z: Intrastriatal transplantation of bone marrow
nonhe-matopoietic cells improves functional recovery after stroke
in adult mice. J Cereb Blood Flow Metab. 20:1311–1319. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Li N, Sarojini H, An J and Wang E:
Prosaposin in the secretome of marrow stroma-derived neural
progenitor cells protects neural cells from apoptotic death. J
Neurochem. 112:1527–1538. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Li Y, Chopp M, Chen J, Wang L, Gautam SC,
Xu YX and Zhang Z: Intrastriatal transplantation of bone marrow
nonhe-matopoietic cells improves functional recovery after stroke
in adult mice. J Cereb Blood Flow Metab. 20:1311–1319. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Tang WC and Sun SJ: Cardiopulmonary
resuscitation and emergency cardiovascular Beijing. Beijing Science
and Technology Press. 572–586. 2008.
|
|
18
|
Barbash IM, Chouraqui P, Baron J, Feinberg
MS, Etzion S, Tessone A, Miller L, Guetta E, Zipori D, Kedes LH, et
al: Systemic delivery of bone marrow-derived mesenchymal stem cells
to the infarcted myocardium: Feasibility, cell migration and body
distribution. Circulation. 108:863–868. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zhang W, Smith C, Howlett C and
Stanimirovic D: Inflammatory activation of human brain endothelial
cells by hypoxic astrocytes in vitro is mediated by IL-1beta. J
Cereb Blood Flow Metab. 20:967–978. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Schoch HJ, Fischer S and Marti HH:
Hypoxia-induced vascular endothelial growth factor expression
causes vascular leakage in the brain. Brain. 125:2549–2557. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Geocadin RG, Ghodadra R, Kimura T, Lei H,
Sherman DL, Hanley DF and Thakor NV: A novel quantitative EEG
injury measure of global cerebral isehemia. Clin Neurophysiol.
111:1779–1187. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Perasso L, Cogo CE, Giunti D, Gandolfo C,
Ruggeri P, Uccelli A and Balestrino M: Systemic administration of
mesenchymal stem cells increases neuron survival after global
cerebral ischemia in vivo (2VO). Neural Plast. 2010:5349252010.
|
|
23
|
Ohtaki H, Ylostalo JH, Foraker JE,
Robinson AP, Reger RL, Shioda S and Prockop DJ: Stem/progenitor
cells from bone marrow decrease neuronal death in global ischemia
by modulation of inflammatory/immune responses. Proc Natl Acad Sci
USA. 105:14638–14643. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Wang L, Li Y, Chen X, Chen J, Gautam SC,
Xu Y and Chopp M: MCP-1, MIP-1, IL-8 and ischemic cerebral tissue
enhance human bone marrow stromal cell migration in interface
culture. Hematology. 7:113–117. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Zimmer DB, Cornwall EH, Landar A and Song
W: The S100 protein family: History, function and expression. Brain
Res Bull. 37:417–429. 1995. View Article : Google Scholar
|
|
26
|
Wojtczak-Soska K and Lelonek M: S-100B
protein: An early prognostic marker after cardiac arrest. Cardiol
J. 17:532–536. 2010.PubMed/NCBI
|
|
27
|
Grubb NR, Simpson C, Sherwood RA, Abraha
HD, Cobbe SM, O'Carroll RE, Deary I and Fox KA: Prediction of
cognitive dysfunction after resuscitation from out-of-hospital
cardiac arrest using serum neuron-specific enolase and protein
S-100. Heart. 93:1268–1273. 2007. View Article : Google Scholar : PubMed/NCBI
|