Introduction
Rheumatoid arthritis (RA) is a type of systemic
chronic inflammatory disorder, the prevalence of which varies
worldwide between 0.5 and 1% (1).
RA is an autoimmune disease that is characterized by synovial
inflammation, synovial hyperplasia, neovascularization, and
ultimately cartilage and bone damage (2,3). RA
has a multi-factorial etiology, which is associated with internal
and external factors (4,5), including predisposing genes (6), lifestyle choices (7), infectious agents (8), and occupational exposures (9). Although the molecular pathogenesis of
RA remains unclear, recent evidence has suggested that the cytokine
network has an important role in the pathogenesis of RA (10). Proinflammatory cytokines, such as
interleukin (IL)-6 and tumor necrosis factor (TNF)-α, have a major
role in inflammation. TNF-α is an important regulatory factor of
the inflammatory and immune response, which can strongly promote
inflammation, and is associated with various pathological changes
of RA (11). IL-6 is a pleiotropic
cytokine, which is plentifully expressed in rheumatoid synovium and
may contribute to joint damage (12). IL-8 is a chemokine of the immune
system, which serves as a chemical signal that attracts neutrophils
to the site of inflammation (13).
IL-10 is an anti-inflammatory cytokine, which suppresses TNF-α
production and the development of type II collagen-induced
arthritis (CIA) in rats (14).
Nuclear factor (NF)-κB, which is a pleiotropic transcription
factor, is inactive in quiescent cells; however, it can promote the
transcription of various genes and the release of several
cytokines, which may contribute to inflammation once activated. An
excessive inflammatory reaction can also damage target cells and
tissues.
At present, non-steroidal anti-inflammatory drugs,
slow-acting anti-rheumatic drugs, adrenocorticotropic hormone,
novel biological agents, and some Chinese drugs are used clinically
to treat RA. However, due to the lack of efficacy and undesirable
side effects associated with Western medical treatments, an
effective and safe therapeutic strategy for the treatment of RA is
still required.
Traditional Chinese medicine, or herbal medicine,
has an important role in the treatment of RA. Plant-derived natural
products dominate the traditional medical systems. Bauhinia
championii (Benth.) Benth. is a perennial liana, which belongs
to the Bauhinia Leguminosae family. It is widely used to
treat many diseases. It has a bitter, acerbic taste, and warm in
nature. In addition, it has the ability to expel wind and eliminate
dampness, promote blood circulation to relieve pain, invigorate the
spleen, and regulate qi (15). It
is mainly used to treat epigastric pain (16), RA (17), and acute and chronic pain of the
lumbar region and leg (18,19).
Experimental studies focusing on this herbal remedy are few,
particularly those regarding the mechanism of action underlying the
treatment of RA. Our previous study indicated that Bauhinia
championii (Benth.) Benth. is efficacious in inhibiting paw
swelling and inflammation in CIA rats (20).
At present, there are no reports identifying
cytokines as the target molecules of Bauhinia championii
(Benth.) Benth. in the treatment of RA. Therefore, the present
study aimed to evaluate the anti-inflammatory effects of
Bauhinia championii (Benth.) Benth. on the CIA rat model.
The present study observed paw edema and histological alterations
in the CIA rats. Furthermore, the effects of Bauhinia
championii (Benth.) Benth. on the production of serum TNF-α,
IL-8, IL-6 and IL-10, and the protein expression of NF-κB in
synovial tissue were investigated, in order to elucidate the
mechanism by which Bauhinia championii (Benth.) Benth.
exerts its effect on CIA.
Materials and methods
Plant material
Rattans of Bauhinia championii (Benth.)
Benth. were collected in the mountainous woods of Minhou (E119.22,
N25.88; Fuzhou, China) in April 2011. Bauhinia championii
(Benth.) Benth. was identified by Professor Lu Wei (Fujian
University of Traditional Chinese Medicine, Fuzhou, China). A
voucher specimen was deposited at the Pharmacy College, Fujian
University of Traditional Chinese Medicine. The samples were dried,
milled, passed through a stainless steel sieve, and stored until
use at 4°C. The same batch of samples was used throughout the
present study.
Animals
A total of 50 specific-pathogen-free Wistar male
rats, weighing 200±20 g, were offered by the Animal Care and Use
Committee, Fujian University of Traditional Chinese Medicine. The
rats were purchased from Shanghai SLAC Laboratory Animal Co. Ltd.
(Shanghai, China) [license no. SCX (hu) 2007-2005]. The rats were
housed in an environment containing 55±5% humidity, with an ambient
temperature (21–23°C), under a 12-h light/dark cycle with ad
libitum access to food and water. Animal welfare was taken into
consideration, in accordance with international ethical guidelines
and the National Institutes of Health Guide concerning the Care and
Use of Laboratory Animals (21).
The study was approved by the ethics committee of Fujian University
of Traditional Chinese Medicine.
Preparation of ethyl acetate
fractions
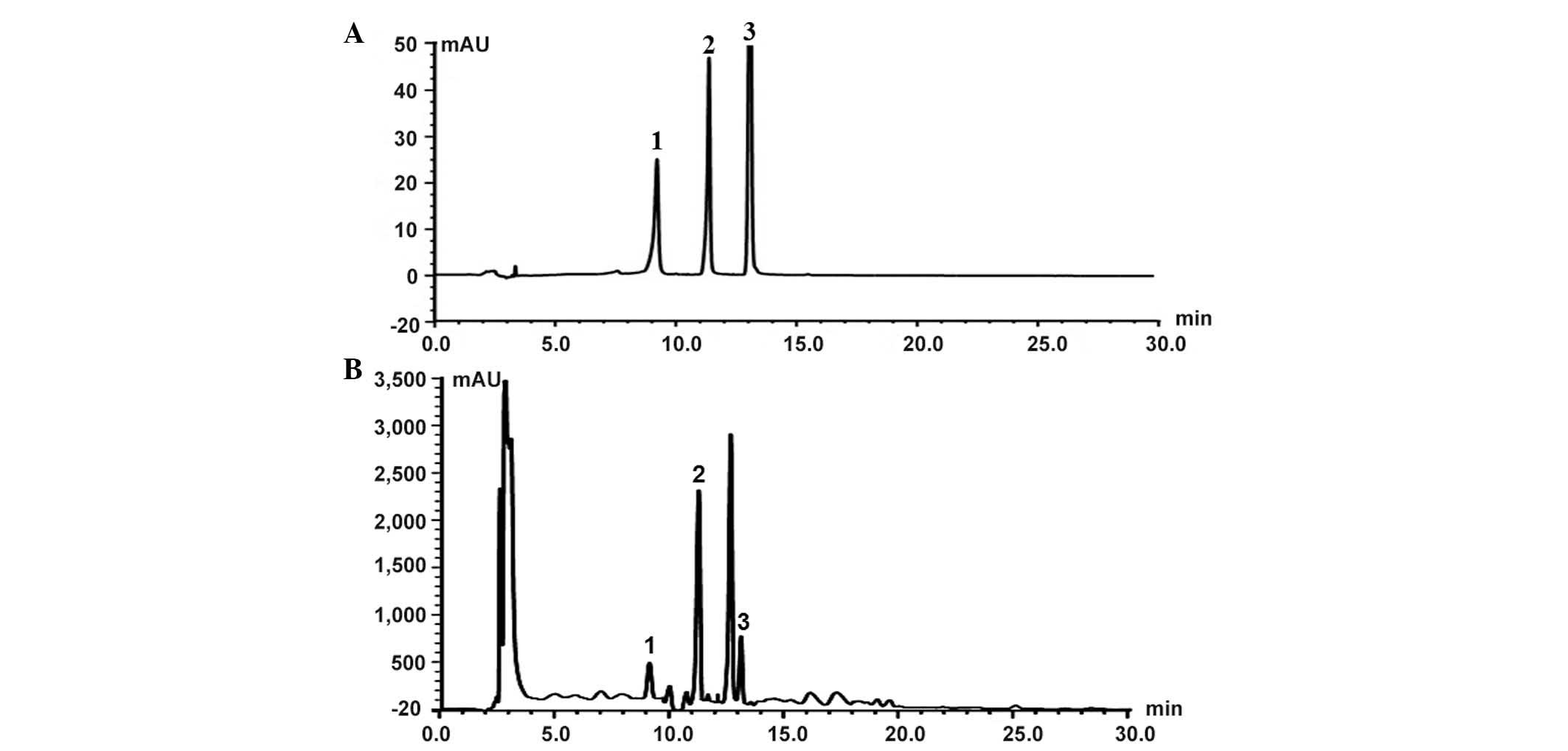
Extraction of ethyl acetate fractions was prepared
according to previously described methods (22). The prepared 1.0 g Bauhinia
championii (Benth.) Benth. extraction (BCBE) was dissolved in
acetonitrile, and was subjected to high-performance liquid
chromatography (HPLC) analysis in order to identify the major peaks
(Fig. 1). HPLC analysis was
performed on a Waters UPLC system (Waters, Ltd., Hertfordshire,
UK). Chromatographic separation was performed at 25°C on an
Diamonsil C18 (250×4.6 mm, 5 µm; Beijing Dikma Technology
Co., Ltd., Beijing, China). The mobile phases consisted of 0.1%
formic acid in (A) water and (B) acetonitrile with 0.1% formic acid
(both purchased from Sinopharm Chemical Reagent Co., Ltd.,
Shanghai, China). The gradient elution program was as follows: 0
Min at (A) 25 and (B) 75%, 15 min at (A) 45 and (B) 55%, and 40 min
at (A and B) 50%. The flow rate was maintained at 1 ml/min, and the
ample volume injected was 10 µl. The extracted fractions
were maintained at 4°C until subsequent use.
CIA model generation and BCBE
administration
The CIA model was generated according to a previous
study (22). A total of 50 Wistar
rats were randomly divided into five groups: Normal group, model
group, tripterygium glycosides tablet (TGT) group, BCBE low-dose
group and BCBE high-dose group (n=10/group). Firstly, 2 mg/ml
bovine type II collagen (Sigma-Aldrich, St. Louis, MO, USA) was
emulsified with an equal volume of complete Freund's adjuvant
(Sigma-Aldrich) to a final concentration of 0.1 mg/ml. Secondly, in
all groups apart from the normal group, the rats were injected with
0.2 mg collagen emulsion into the tail root via intradermal
injection. A secondary immunization test was performed 7 days later
with similar methods. Drugs were administered intragastrically once
a day from the first day after primary immunization. The normal
group and model group received 10 ml/kg 9.0 g/l sodium chloride
daily; the BCBE high-dose group received 0.5 g/kg BCBE daily; the
BCBE low-dose group received 0.125 g/kg BCBE daily; and the TGT
positive control group received 1 mg/kg TGT daily (Huangshi Feiyun
Pharmaceutical Co., Ltd., Huangshi, China). All animals were
treated continuously for 28 days.
Measurement of paw edema
Over the course of the experiment, paw volume was
measured using a YLS-7B plethysmometer (Yi Yan Technology
Development Co., Ltd., Jinan, China). Swelling was expressed as the
volume difference (ml) before and after modeling (23).
Determination of IL-6, IL-8, IL-10 and
TNF-α levels
The rats were sacrificed with urethane (1,500 mg/kg;
i.p.; Sinopharm Chemical Reagent Co., Ltd.) and blood samples were
collected. The blood samples were centrifuged at 1,500 × g for 20
min at 4°C in order to obtain the supernatant and serum.
Enzyme-linked immunosorbent assay kits were used to measure the
serum levels of IL-8 (ER-1578; Beijing Zhongshan Golden Bridge
Biotechnology Co., Ltd., Beijing, China), IL-6 (113897105), IL-10
(1388127105) (both purchased from Wuhan Boster Biological
Technology, Ltd., Wuhan, China) and TNF-α (AE90301Ra) (Shanghai
Lianshuo Biological Technology Co., Ltd., Shanghai, China),
according to the manufacturer's protocols.
Histopathological examination
Briefly, right ankles were obtained from the rats
and were fixed in 10% formalin solution for histopathological
examination. The samples were then decalcified in 12.5%
ethylenediaminetetraacetic acid (pH 7.0) for ~20 days, dehydrated
in ethanol, cleared with dimethyl benzene, and embedded in paraffin
blocks. The specimens were then serially cut into 5 µm
sections, and were stained with hematoxylin and eosin (HE; Beyotime
Institute of Biotechnology, Haimen, China) prior to observation
under a light microscope (DM4000B, Leica Microsystems, Wetzlar,
Germany).
Western blot analysis
Synovial tissues were obtained from the hind paws
after stripping away the skin, muscle, fatty tissues, bone and
tendons. Subsequently, the synovial tissues were immediately frozen
in liquid nitrogen and stored at −80°C. Randomly, synovial tissues
from three rats per group were adequately homogenized using
non-denaturing lysis buffer (Beyotime Institute of Biotechnology),
and were centrifuged at 12,000 × g for 15 min at 4°C. The protein
concentration in the supernatants was then determined using a BCA
Protein Assay Kit (Beyotime Institute of Biotechnology). The
supernatants were denatured in protein loading buffer, and protein
samples (30 µg) were separated by 12% sodium dodecyl
sulfate-polyacrylamide gel electrophoresis and were transferred to
polyvinylidene difluoride membranes (EMD Millipore, Billerica, MA,
USA). Non-specific binding was blocked for 3 h with 5% skim milk in
Tris-buffered saline containing 0.1% Tween. Membranes were
incubated with rabbit NF-κB p65 (cat. no. 8242) and β-actin (cat.
no. 4967) primary antibodies (1:1,000 dilution; Cell Signaling
Technology, Danvers, MA, USA) overnight at 4°C, and were then
incubated with an appropriate horseradish peroxidase-conjugated
secondary antibody (1:500 dilution; cat. no. C-0029; Beijing
Biosynthesis Biotechnology Co., Ltd., Beijing, China) for 2 h at
room temperature. Subsequently, the membranes were washed and were
visualized using enhanced chemiluminescence western detection
reagents (Beyotime Institute of Biotechnology).
Immunohistochemical analysis
Paraffin-embedded sections (5 µm) were used
for immunohistochemical analysis, according to the manufacturer's
protocol. Briefly, paraffin sections were deparaffinized,
rehydrated, submerged in 3% hydrogen peroxide (Sinopharm Chemical
Reagent Co., Ltd, Shanghai, China), washed with phosphate buffered
saline and blocked with goat serum (Beijing Zongshan Golden Bridge
Biotechnology Co., Ltd.). Then, the samples were incubated with
rabbit polyclonal anti-TNF-α (1:500; bs 0078R), rabbit polyclonal
anti IL-6 (1:500 dilution; bs6309R) and rabbit polyclonal anti IL-8
(1:500 dilution; bs0780R) (both purchased from Beijing Biosynthesis
Biotechnology Co., Ltd.) overnight at 4°C. Sections were then
incubated with a biotinylated secondary antibody (polyclonal goat
anti-rabbit IgG streptavidin antibody; 1:500 dilution; ZB-5301;
Beijing Zhongshan Golden Bridge Biotechnology Co., Ltd.) at 37°C
for 2 h. The sections were then developed with diaminobenzidine and
counterstained with hematoxylin and eosin (both purchased from
Beyotime Institute of Biotechnology). The primary antibody was
omitted in the negative control. Microscopic images were acquired
using a Leica microscope (DM4000B; Leica Microsystems) and five
high power fields (magnification, ×400) were randomly selected in
each slide. The average proportion of positive cells in each field
were counted using Image Pro Plus (version 6.0; Media Cybernetics,
Inc., Rockville, MD, USA). Immunohistochemical score was used to
evaluate the slices (24,25).
RNA extraction and reverse
transcription-polymerase chain reaction (RT-PCR) analysis
Total RNA was extracted from the synovial tissues
using TRIzol® (Invitrogen; Thermo Fisher Scientific,
Inc., Waltham, MA, USA). Total RNA (2 µg) was reverse
transcribed to cDNA using a RevertAid First Strand cDNA Synthesis
Kit (Thermo Fisher Scientific, Inc.). The reaction mixture
contained 1 µl Oligo(dT)18 Primer, 5X Reaction Buffer, 1
µl Ribolock RNase Inhibitor (20 U/µl), 2 µl
dNTP (10 mM), 1 µl RevertAid M-MuLV Reverse Transcriptase
(200 U/µl) and 20 µl nuclease-free water. The
obtained cDNA was used to determine the mRNA expression levels of
IL-6, IL-8, TNF-α and NF-κB by PCR using Taq DNA polymerase
(Thermo Fisher Scientific, Inc.). The PCR reaction volume was 20
µl, containing 10 µl DreamTaq Green PCR Master Mix
(2X), 0.4 µl forward primer (1 µM), 0.4 µl
reverse primer (1 µM), 1 µl template DNA (1
µg) and 8.2 µl nuclease-free water. The PCR was
conducted under the following conditions using a thermal cycler
(C1000 Touch; Bio-Rad Laboratories, Inc., Hercules, CA, USA):
Initial denaturation at 95°C for 3 min, annealing at 95°C for 30
sec and extension at 72°C for 45 sec. The annealing temperatures
and number of amplification cycles were 50°C and 38 cycles for
IL-6, 57°C and 35 cycles for IL-8, 58°C and 35 cycles for TNF-α,
60°C and 35 cycles for NF-κB, and 55°C and 35 cycles for GAPDH.
Primers were purchased Shanghai Sangon Biological Engineering Co.,
Ltd. (Shanghai, China), from and the sequences were as follows:
IL-6, forward 5′-GACAAAGCCAGAGTCCTTCA-3′, reverse
5′-ACTAGGTTTGCCGAGTAGAC-3′; IL-8, forward
5′-GACTGTTGTGGCCCTGGAG-3′, reverse 5′-CCGTCAAGCTCTGGATGTTCT-3′;
TNF-α, forward 5′-CTCCCAGGTTCTCTTCAAGG-3′, reverse
5′-TGGAAGACTCCTCCCAGGTA-3′; NF-κB, forward
5′-GCGCATCCAGACCAACAATAAC-3′, and reverse
5′-GCCGAAGCTGCATGGACACT-3′; and GAPDH, forward
5′-ACTGGCATTGTGATGGACTC-3′, and reverse 5′-CAGCACTGTGTTGGCATAGA-3′.
Glyceraldehyde 3-phosphate dehydrogenase was used as an internal
control. All processes were performed on the basis of
manufacturer's protocol. Finally, the PCR products were analyzed by
gel electrophoresis (1.5% agarose), the agarose gels were stained
using GoldView (Beyotime Institute of Biotechnology) and DNA bands
were examined using a Gel Documentation system (Gel Doc 2000;
Bio-Rad Laboratories, Inc.).
Statistical analysis
Data are presented as the mean ± standard deviation.
One-way analysis of variance and the Student-Newman-Keuls post-hoc
test were used to determine significant differences between the
groups. SPSS software (version 16.0; SPSS, Inc., Chicago, IL, USA)
was used to perform statistical analysis. P<0.05 was considered
to indicate a statistically significant difference.
Results
Effects of BCBE on paw edema
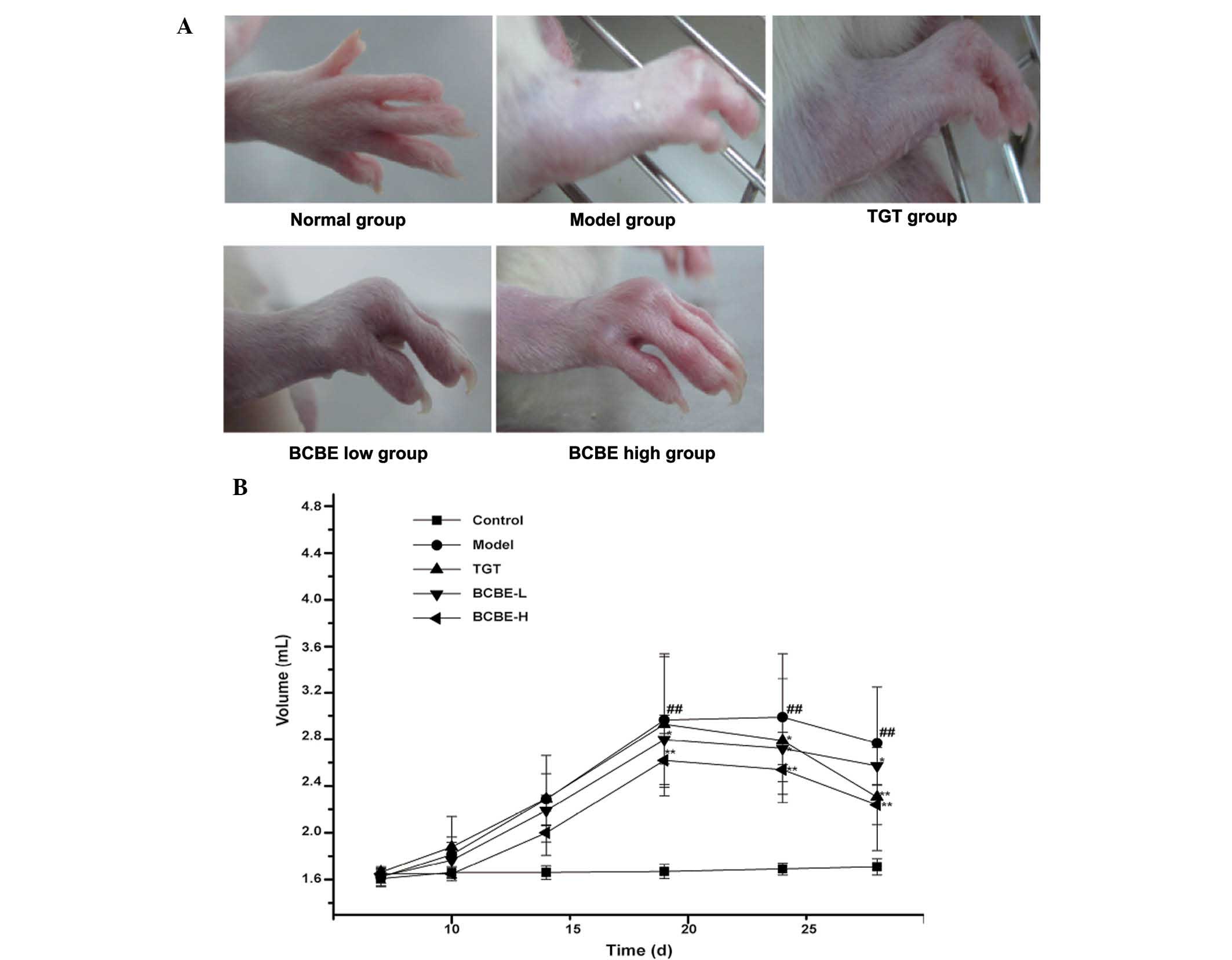
The general condition of the rats was monitored
during treatment. The onset time of paw edema for the majority of
rats was day 3 after the second immunization. Post-treatment, red
swelling in the right hind paw was markedly ameliorated in the
BCBE-treated groups (Fig. 2A). As
shown in Fig. 2B, paw edema was
observed between days 1 and 28. Paw edema increased in severity
over time, and paw swelling volume reached its maximum on day 18.
However, paw edema in the BCBE groups increased more slowly
compared with the model group, and was significantly decreased
after day 18 (P<0.05). With therapeutic action, the paw swelling
volume was gradually reduced over time. Furthermore, the
edema-reducing effects of BCBE appeared earlier than those of
TGT.
Effects of BCBE on serum cytokine levels
in CIA rats
As shown in Table
I, the serum levels of IL-6, IL-8 and TNF-α were significantly
increased in the model group compared with in the normal group
(P<0.01), thus suggesting that the model group exhibited a
marked inflammatory response. However, the cytokine levels were
decreased in the TGT and BCBE groups. Furthermore, the levels of
IL-6, IL-8 and TNF-α differed between the high-dose and model
groups (P<0.01). These results suggest that BCBE may reduce the
levels of proinflammatory cytokines, in order to dose-dependently
relieve CIA-associated inflammation and gradually alleviate joint
damage. Conversely, the levels of the chemotactic cytokine IL-10
were markedly reduced in the model group, and were increased in the
TGT and BCBE groups.
 | Table ISerum levels of IL-6, IL-8, IL-10 and
TNF-α in a rat model of type II collagen-induced arthritis in
response to BCBE. |
Table I
Serum levels of IL-6, IL-8, IL-10 and
TNF-α in a rat model of type II collagen-induced arthritis in
response to BCBE.
| Group | IL-6 (pg/ml) | IL-8 (ng/ml) | IL-10 (pg/ml) | TNF-α (ng/ml) |
|---|
| Normal | 65.958±2.582 | 0.131±0.015 | 49.403±1.744 | 0.284±0.042a |
| Model |
160.854±3.221b | 0.296±0.013b |
35.792±2.681b | 1.079±0.087b |
| TGT |
86.281±3.677a | 0.232±0.035c |
40.854±1.461a | 0.646±0.038a |
| BCBE low |
97.513±3.355a | 0.262±0.041 | 38.001±1.783 | 0.897±0.074c |
| BCBE high |
81.363±3.468a | 0.186±0.050a |
39.412±1.988a | 0.469±0.091a |
Effects of BCBE on histopathological
alterations
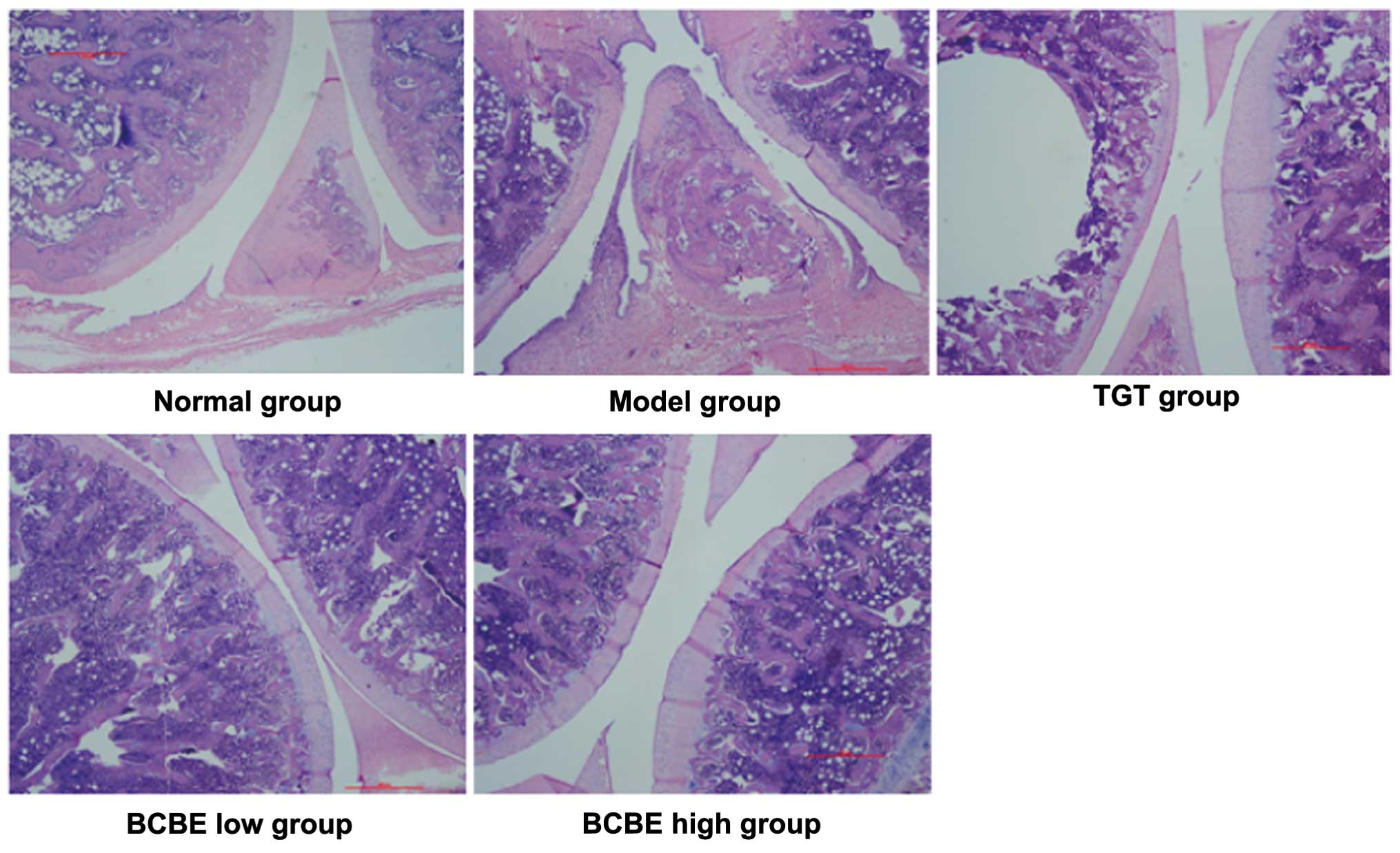
As shown in Fig. 3,
representative pathological sections from CIA rat joints were
stained with HE. Rats in the normal group exhibited a normal
histological architecture. Conversely, the model group exhibited
markedly abnormal histological architecture, including significant
synovial cell proliferation with a disorganized arrangement,
hyperplasia, inflammation, and extensive erosive changes to
cartilage and bone. The BCBE-treated rats exhibited a nearly normal
histological architecture compared with the model group. In the
BCBE low-dose group, synovial tissue displayed moderate hyperplasia
and infiltration of inflammatory cells, with pannus formation and
some cartilage damage. In the BCBE high-dose group, only mild
synovial proliferation was observed, cell morphology was normal, a
small number of inflammatory cells had infiltrated, no typical
pannus had formed, and the cartilage surface was smooth with no
obvious damage and no obvious bone erosion.
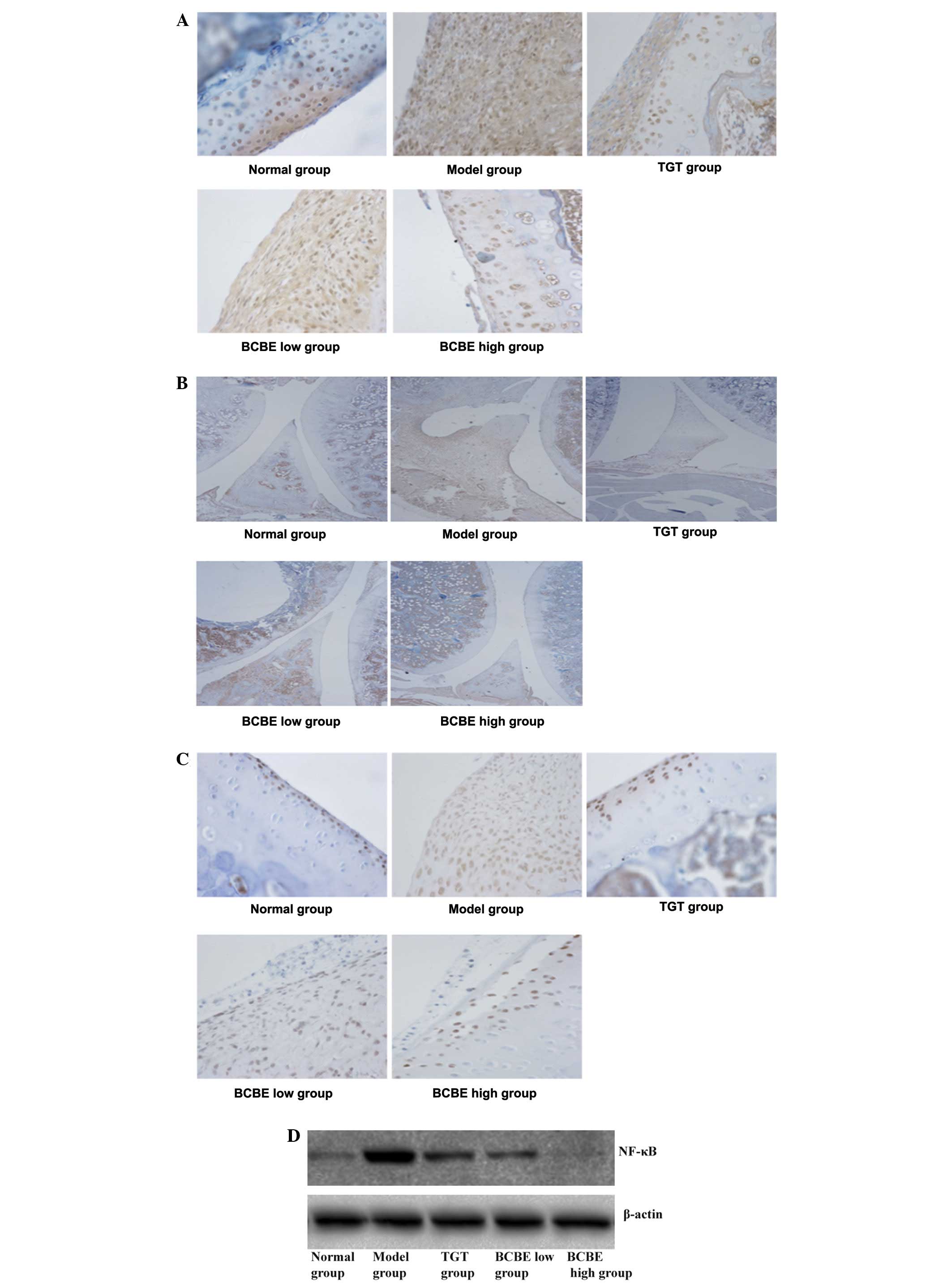
Effects of BCBE on the expression levels
of IL-6, IL-8, TNF-α and NF-κB
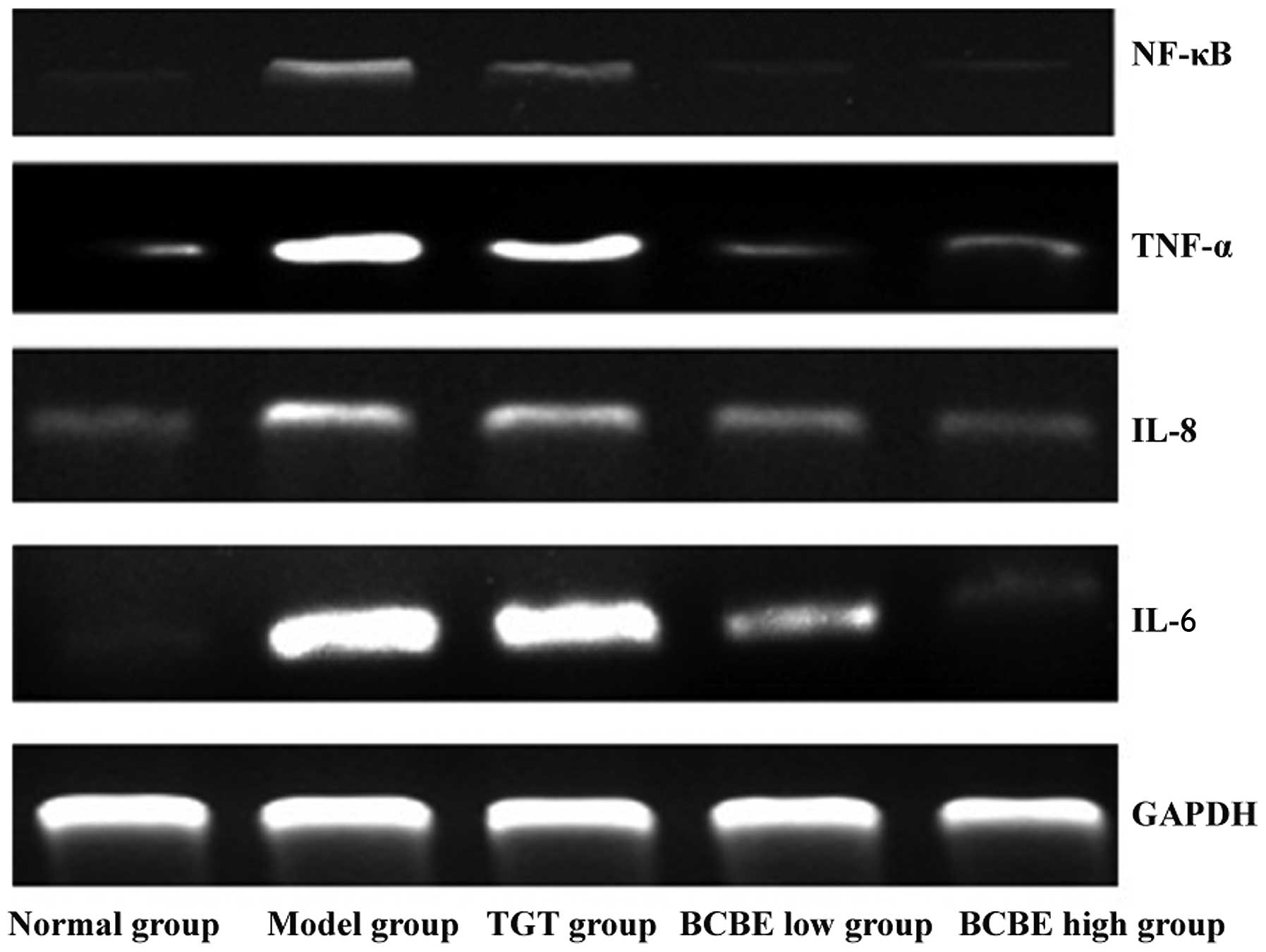
The mRNA expression levels of IL-6, IL-8, TNF-α and
NF-κB are presented in Fig. 4. In
the model group, the mRNA expression levels of IL-6, IL-8, TNF-α
and NF-κB were increased compared with those in the normal group;
however, the expression levels were reduced following treatment
with TGT and different doses of BCBE. Results from
immunohistochemistry and western blotting indicated that the
patterns of IL-6, IL-8, TNF-α and NF-κB protein expression were
similar to their respective mRNA expression patterns (Fig. 5A–D).
Discussion
It is well-known that CIA is similar to human RA
with regards to clinical manifestations, serological parameters,
and immunological and pathological alterations. In the present
study, CIA was established as an experimental animal model of RA.
The general condition of the rats was monitored and paw edema was
observed, suggesting the model was successful, since arthritis is
characterized by paw redness and paw edema. In addition, according
to histopathological analysis of the ankle joint, anomalous
hyperplasia of synovial membranes, collagen fiber deposition, large
numbers of inflammatory cells, and cartilage and bone erosion were
detected in the model group. These phenomena were also described in
previous studies (26,27), and were attenuated following
treatment with BCBE. Therefore, BCBE may relieve paw edema and
alleviate synovial membrane hyperplasia, thus indicating that BCBE
may possess certain anti-inflammatory effects.
TNF-α is an important inflammatory mediator that can
stimulate the secretion of numerous other inflammatory cytokines.
It has been reported that the main pathological features of RA are
closely associated with immunomodulatory cytokines, including
proinflammatory cytokines (TNF-α, IL-6 and IL-8) and
anti-inflammatory cytokines (IL-10) in serum (28,29).
Previous studies have demonstrated that TNF-α overproduction is
associated with the progression of RA, thus suggesting that it may
be used as a parameter for the evaluation of disease-modifying
anti-rheumatic drugs (30,31). The present study indicated that the
levels of proinflammatory cytokines (TNF-α, IL-6 and IL-8) were
substantially increased in the model group, whereas IL-10 was
decreased. Furthermore, the treatment groups exhibited marked
suppression of TNF-α, IL-6 and IL-8 expression, whereas IL-10
expression was increased. These results suggested that BCBE was
effective at suppressing the development of proinflammatory
cytokines, but increased the expression of IL-10. Therefore, BCBE
may be considered a potential therapeutic or preventive candidate
for the treatment of acute inflammation in RA.
NF-κB is a pleiotropic transcription factor and a
pivotal regulator of RA-associated inflammation. It is inactive in
quiescent cells, but once activated, it can promote the
transcription of several genes and release cytokines that
contribute to inflammation. NF-κB is essential for triggering and
amplifying the cytokine network (32). It has previously been reported that
the NF-κB signaling pathway may result in downregulation of the
expression of various anti-apoptotic and cytokine genes (33). In addition, NF-κB has been
demonstrated to regulate the expression of TNF-α and IL-6 (34). As determined by western blot
analysis, NF-κB was significantly inhibited in the synovial tissue
by BCBE. In conclusion, the anti-inflammatory effects of BCBE may
be associated with the inhibition of NF-κB, TNF-α, IL-6 and IL-8,
and the induction of IL-10; however, further evidence is
required.
Acknowledgments
The present study was performed in the State Key
Laboratory of Chinese Pharmacies of Fujian Provincial Department of
Science and Technology, Collaborative Innovation Center for
Rehabilitation Technology and Traditional Chinese Medicine
Rehabilitation Research Center of the State Administration of
Traditional Chinese Medicine. The present study was financially
supported by the National Natural Science Foundation of China
(grant no. 81370096), Fujian Province Science-Technology Plan
Projects (grant no. 2010Y2004) and the 2014 National College
Students' Innovative Entrepreneurial Training Plan Project (grant
no. 201410393008).
Abbreviations:
|
RA
|
rheumatoid arthritis
|
|
CIA
|
collagen-induced arthritis
|
|
BCBE
|
Bauhinia championii (Benth.)
Benth. extraction
|
|
TGT
|
tripterygium glycosides tablet
|
|
IL
|
interleukin
|
|
TNF-α
|
tumor necrosis factor-α
|
|
NF-κB
|
nuclear factor-κB
|
|
RT-PCR
|
reverse transcription-polymerase chain
reaction
|
|
HE
|
hematoxylin and eosin
|
References
|
1
|
Brenner M, Meng HC, Yarlett NC, Joe B,
Griffiths MM, Remmers EF, Wilder RL and Gulko PS: The non-MHC
quantitative trait locus Cia5 contains three major arthritis genes
that differentially regulate disease severity, pannus formation,
and joint damage in collagen- and pristane-induced arthritis. J
Immunol. 174:7894–7903. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ono Y, Inoue M, Mizukami H and Ogihara Y:
Suppressive effect of Kanzo-bushi-to, a Kampo medicine, on
collagen-induced arthritis. Biol Pharm Bull. 27:1406–1413. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Helliwell P, Woodburn J, Redmond A, Turner
D and Davys H: Current concepts in rheumatoid arthritis. The Foot
and Ankle in Rheumatoid Arthritis: A Comprehensive Guide. Elsevier
Health Sciences; Edinburgh: pp. 1–16. 2007
|
|
4
|
Kochi Y, Suzuki A, Yamada R and Yamamoto
K: Genetics of rheumatoid arthritis: Underlying evidence of ethnic
differences. J Autoimmun. 32:158–162. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Symmons DP: Environmental factors and the
outcome of rheumatoid arthritis. Best Pract Res Clin Rheumatol.
17:717–727. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Huizinga TW: Genetics in rheumatoid
arthritis. Best Pract Res Clin Rheumatol. 17:703–716. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kallberg H, Padyukov L, Plenge RM,
Ronnelid J, Gregersen PK, van der Helm-van Mil AH, Toes RE,
Huizinga TW, Klareskog L and Alfredsson L; Epidemiological
Investigation of Rheumatoid Arthritis study group. Gene-gene and
gene-environment interactions involving HLA-DRB1, PTPN22, and
smoking in two subsets of rheumatoid arthritis. Am J Hum Genet.
80:867–875. 2007. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Mackenzie AR and Dawson J: Could
rheumatoid arthritis have an infectious aetiology? Drug Discovery
Today: Disease Mechanisms. 2:345–349. 2005. View Article : Google Scholar
|
|
9
|
De Roos AJ, Cooper GS, Alavanja MC and
Sandler DP: Rheumatoid arthritis among women in the Agricultural
Health Study: Risk associated with farming activities and
exposures. Ann Epidemiol. 15:762–770. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Davis JM III and Matteson EL: Cytokine
biomarkers and the promise of personalized therapy in rheumatoid
arthritis. Reumatol Clin. 5:143–146. 2009.In Spanish. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
van den Berg WB: Anti-cytokine therapy in
chronic destructive arthritis. Arthritis Res. 3:18–26. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Jazayeri JA, Carroll GJ and Vernallis AB:
Interleukin-6 subfamily cytokines and rheumatoid arthritis: Role of
antagonists. Int Immunopharmacol. 10:1–8. 2010. View Article : Google Scholar
|
|
13
|
Brennan FM, Zachariae CO, Chantry D,
Larsen CG, Turner M, Maini RN, Matsushima K and Feldmann M:
Detection of interleukin 8 biological activity in synovial fluids
from patients with rheumatoid arthritis and production of
interleukin 8 mRNA by isolated synovial cells. Eur JImmunol.
20:2141–2144. 1990. View Article : Google Scholar
|
|
14
|
Persson S, Mikulowska A, Narula S, O'Garra
A and Holmdahl R: Interleukin-10 suppresses the development of
collagen type II-induced arthritis and ameliorates sustained
arthritis in rats. Scand J Immunol. 44:607–614. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Jiangsu New Medical College: Dictionary of
Chinese Traditional Drugs. Shanghai Scientific and Technical
Publishers; Shanghai, China: pp. p431986
|
|
16
|
Guo CQ and Xiang RM: Treatment of acute or
chronic backleg pain by yangtiteng. Minzu Minjian Yiyao.
9:612001.In Chinese.
|
|
17
|
Wei HS and Qi ZY: Curative effect
observation of fumigation treatment arthralgia 58 cases. Zhongyi
Waizhi Zazhi. 7:41–42. 1998.In Chinese.
|
|
18
|
Xie GC and Xiao QQ: Chinese Illuminations
of Well-Triedrecipe of Herbs. Shantou University Press; Shantou,
China: pp. p1252000
|
|
19
|
Fang D, Luo JY, Su GX, Tao YP, Tan XY and
Tan DH: Selectional medications prescription of Zhuang folk
medicine. Guangxi Nationalities Publishing House; Guangxi, China:
pp. 6–77. 1985
|
|
20
|
Zheng H, Xu W, Li H, Chu K, Chen L and
Zhang Y: Effects of ethyl acetate extracts from Bauhinia championii
(Benth.) Benth. on rats with collagen-induced arthritis. Fu Jian
Zhong Yi Xue Yuan Xue Bao. 23:31–34. 2013.
|
|
21
|
Institute of Laboratory Animal Resources
(US); Committee on Care Use of Laboratory Animals National
Institutes of Health (US): Division of Research Resources: Guide
for the care and use of laboratory animals. 8th edition. National
Academies Press; Washington, DC: 2011
|
|
22
|
Courtenay JS, Dallman MJ, Dayan AD, Martin
A and Mosedale B: Immunization against heterologous type II
collagen induces arthritis in mice. Nature. 283:666–668. 1980.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Gao Q, Shan J, Di L, Jiang L and Xu H:
Therapeutic effects of daphnetin on adjuvant-induced arthritic
rats. J Ethnopharmacol. 120:259–263. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Chen Q and Wei W: Effects and mechanisms
of glucosides of chaenomeles speciosa on collagen-induced arthritis
in rats. Int Immunopharmacol. 3:593–608. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Brand DD, Kang AH and Rosloniec EF:
Immunopathogenesis of collagen arthritis. Springer Semin
Immunopathol. 25:3–18. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Keyszer G, Redlich A, Häupl T, Zacher J,
Sparmann M, Engethüm U, Gay S and Burmester GR: Differential
expression of cathepsins B and L compared with matrix
metalloproteinases and their respective inhibitors in rheumatoid
arthritis and osteoarthritis: A parallel investigation by
semiquantitative reverse transcriptase-polymerase chain reaction
and immunohistochemistry. Arthritis Rheum. 41:1378–1387. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Myers LK, Rosloniec EF, Cremer MA and Kang
AH: Collagen-induced arthritis, an animal control of autoimmunity.
Life Sci. 61:1861–1878. 1997. View Article : Google Scholar
|
|
28
|
Brennan FM, Chantry D, Jackson A, Maini R
and Feldmann M: Inhibitory effect of TNF alpha antibodies on
synovial cell interleukin-1 production in rheumatoid arthritis.
Lancet. 2:244–247. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Tanida S, Yoshitomi H, Nishitani K,
Ishikawa M, Kitaori T, Ito H and Nakamura T: CCL20 produced in the
cytokine network of rheumatoid arthritis recruits CCR6+
mononuclear cells and enhances the production of IL-6. Cytokine.
47:112–118. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
DiMartino M, Wolff C, High W, Stroup G,
Hoffman S, Laydon J, Lee JC, Bertolini D, Galloway WA, Crimmin MJ,
et al: Anti-arthritic activity of hydroxamic acid-based
pseudopeptide inhibitors of matrix metalloproteinases and TNF alpha
processing. Inflamm Res. 46:211–215. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Hisadome M, Fukuda T, Sumichika H, Hanano
T and Adachi K: A novel anti-rheumatic drug suppresses tumor
necrosis factor-alpha and augments interleukin-10 in adjuvant
arthritic rats. Eur J Pharmacol. 409:331–335. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Morel J and Berenbaum F: Signal
transduction pathways: New targets for treating rheumatoid
arthritis. Joint Bone Spine. 71:503–510. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Osorio Y, Fortéa J, Bukulmez H,
Petit-Teixeira E, Michou L, Pierlot C, Cailleau-Moindrault S,
Lemaire I, Lasbleiz S, Alibert O, Quillet P, et al: Dense
genome-wide linkage analysis of rheumatoid arthritis, including
covariates. Arthritis Rheum. 50:2757–2765. 2004. View Article : Google Scholar
|
|
34
|
Tu S, Hu Y, Zeng K, Zhang M, Lai X and
Weichen Z: Effects of triptolide on the expression and activity of
NF-kappaB in synovium of collagen induced arthritis rats. J
Huazhong Univ Sci Technolog Med Sci. 25:543–545. 2005. View Article : Google Scholar
|