Introduction
Kidney transplantation has been established as the
optimal renal replacement therapy for end-stage renal diseases,
which surpasses dialysis treatment for the quality and quantity of
life, as well as cost-effectiveness (1); however, rejection episodes and
infection remain the major obstacles associated with kidney
transplantation. Based on the increasing application of
non-invasive monitoring technologies, the diagnosis of renal
insufficiency during the early stages post-transplantation has
progressed considerably in past decades; however, specific
biomarkers for the noninvasive diagnosis/prognosis of acute
rejection (AR), particularly antibody-mediated rejection (ABMR),
are yet to be identified.
Chemokine (C-X-C motif) ligand 13 (CXCL13),
otherwise known as B cell-attracting chemokine 1, is a small
cytokine belonging to the CXC chemokine superfamily (2). As its name suggests, CXCL13 is
selectively chemotactic for circulating B cells by interacting with
chemokine receptor (CXCR)5 (3,4), a
7-transmembrane G-protein-coupled receptor expressed on the surface
of mature B cells and a subset of memory cells (5,6). The
gene for CXCL13 is located on human chromosome 4 in a cluster with
other CXC chemokines (7),
including interleukin-8 and interferon-inducible protein 10.
Recent studies suggest that the ligation of CXCR5
with CXCL13 may lead to an aberrant aggregation of B cells, which
has been confirmed in rheumatoid arthritis, gastric lymphoma, and
central nervous system lymphoma (8–11).
Additionally, a notable colocalization of CXCL13 expression with
CXCR5 and cluster of differentiation 20-positive B lymphocytes has
also been detected in renal allografts undergoing rejection
(12,13). In addition, our previous study
revealed that CXCL13 expression levels are highly upregulated in
the peripheral blood mononuclear cells of patients with AR
(14).
The particular interaction between CXCL13 and B
lymphocytes, as well as the significance of B cell infiltration in
transplant rejection, may be detected noninvasively as an
intragraft signature by measuring the levels of CXCL13 in urine
samples. Furthermore, such an investigation may contribute to the
monitoring of immune kinetics. To test this hypothesis, the urinary
protein expression levels of CXCL13 were measured following renal
transplantation in a total of 146 renal allograft recipients. The
present study examined whether urinary CXCL13 may effectively
identify AR, in particular ABMR. Secondly, whether the early
elevation of urinary CXCL13 expression levels may serve as an
indication of graft function was investigated.
Materials and methods
Study population and sample
collection
The present study retrospectively reviewed 146
patients (aged 22–69 years old; 97 males and 49 females) who
received a single kidney transplantation from donors who had
succumbed to mortality between June 2006 and December 2009 at the
Kidney Disease Center, the First Affiliated Hospital of College of
Medicine of Zhejiang University (Hangzhou, China). Fresh
first-morning urine specimens were routinely collected from the
patients every 2 weeks during the first 2 months following
transplantation. In addition, urine samples were collected from
patients who had undergone transplantation and were scheduled for a
biopsy with a serum creatinine (Scr) concentration ≥25% above
baseline levels post-transplantation, and from patients who were to
undergo a protocol needle biopsy with stable renal function within
2–3 months post-transplantation. Furthermore, urine samples were
obtained from 36 patients with stable renal function and 21
patients with AR every day within the first week and at a one-week
interval up to the first month post-transplantation. According to
the mean urinary CXCL13/Cr levels (>2 pg/µmol Cr or <2
pg/µmol Cr) exhibited by patients within the first week
post-transplantation, patients were separated into two groups: High
CXCL13/Cr levels group (>2 pg/µmol Cr) and low CXCL13/Cr levels
(<2 pg/µmol Cr) group. For these 57 patients, renal function at
3, 6 and 12 month time intervals post-transplantation were
investigated. On the day of the biopsy, urinary samples were
collected prior to biopsy collection. Furthermore, 40 healthy
individuals were included as controls (aged 27–65 years old; 24
males and 16 females) that did not exhibit any signs of infection
or malignant tumors. On the first day of recruitment, one urine
sample was collected from each patient. All patients were assigned
to a diagnostic category based on an aggregate of all available
diagnostic data, including clinical and pathological manifestation
as determined by histological analysis (15).
Patients classified in the AR group exhibited
histological alterations following H&E and Periodic Acid-Schiff
(PAS) staining. Immunohistochemical analysis was performed using
the Cd4 stain. For H&E and PAS staining, renal tissues were
fixed in a 4% formaldehyde solution for 48 h at 24°C and then
embedded in paraffin. Sections (4 µm) were both stained using
H&E stain at 24°C for 2 h and PAS stain at 24°C for 3 h. For
IHC staining, paraffin embedded sections (4 µm), fixed in a 4%
formaldehyde solution for 48 h at 24°C, and subsequently incubated
for 30 min at 37°C with a polyclonal rabbit anti-human C4d antibody
(cat. no. BI-RC4D; 1:50; Biomedica, Inc., Vienna, Austria).
Following this, sections were blocked with 5% bovine serum albumin
(cat. no. A1933; Sigma-Aldrich; Merck KGaA, Darmstadt, Germany) at
24°C for 30 min. Following three washes with PBS, sections were
incubated for 30 min at 24°C with peroxidase AffiniPure goat
anti-rabbit secondary antibodies (cat. no. 111-035-003; 1:4,000;
Jackson ImmunoResearch Laboratories, Inc., West Grove, PA, USA).
Antibody detection was performed using a DAB Horseradish Peroxidase
Color Development Kit (cat. no. GA042329; Gene Tech Co., Ltd., Hong
Kong, China). Images of these stained sections were obtained using
a light microscope (magnification, ×200 and ×400). Classification
was performed using the Banff 97 criteria (16), while meeting the clinical criteria
associated with renal dysfunction (Scr elevation of ≥25% above
baseline within 6 months post-transplant); patients classified as
stable renal transplant manifested as normal allograft function and
no abnormal pathological findings (NO-AR) in the protocol biopsies
performed 2–3 months following transplantation. Primary grafts were
also received from deceased donors.
All patients provided written informed consent. All
procedures performed in studies involving human participants were
approved by the Ethics Committee of the First Affiliated Hospital
of College of Medicine of Zhejiang University (Hangzhou, China) and
with the 1964 Helsinki declaration and its later amendments or
comparable ethical standards (Reference number: 2017–390).
In the present study, immunosuppressive agents were
used as previously described (17,18).
All patients received a regimen of three immunosuppressive drugs at
the time of transplantation, comprising a calcineurin inhibitor
(tacrolimus), prednisone and azathioprine or mycophenolate mofetil.
Anti-rejection therapy following a clinical and biopsy-proven
diagnosis of AR constituted a 3-day course of intravenous
methylprednisolone (6–10 mg/kg per day, once a day). A lack of
response to steroid treatment (graft function exhibited no
improvement or worsened) was defined as steroid-resistant AR
(SRAR). Histology was classified according to the Banff 97
classification (16,19) and was performed by two experienced
renal pathologists in a blinded fashion.
Fresh urinary samples were collected and centrifuged
for 10 min at 800 × g at 4°C, using a D-37520 Sorvall Legend RT
centrifuge (Heraeus Holding GmbH, Hanau, Germany). The supernatant
was frozen in 1 ml aliquots at −80°C. Urinary Cr and protein were
detected in all samples.
ELISA: Quantification of CXCL13 in
urine samples
The expression levels of CXCL13 were measured in
urinary samples using a commercial human CXCL13 ELISA kit,
according to the manufacturer's protocols (R&D Systems, Inc.,
Minneapolis, MN, USA, cat. no. DCX130). All samples were undiluted
and analyzed in duplicate.
Statistical analysis
To eliminate the influence of renal function on
urinary protein quantitation, all urinary CXCL13 levels were
normalized to urine creatinine (Cr) in the present study. Summary
statistics for normally distributed quantitative variables were
expressed as the mean ± standard deviation. For non-normally
distributed variables, we used the median and interquartile range
(IQR). Differences in the continuous variables were judged using a
Mann-Whitney U test or Kruskal-Wallis H test followed by Tukey's
post hoc test. A conventional receiver operating characteristic
(ROC) curve was conducted to determine the sensitivities and
specificities for patients with and without AR. Youden's index,
defined as sensitivity + specificity-1, was used to calculate the
diagnostic threshold. All statistical analyses were performed using
SPSS software package (version 23.0; IBM Corp., Armonk, NY, USA),
and a two-sided P<0.05 was considered to indicate a
statistically significant difference.
Results
Patients and baseline clinical and
biopsy characteristics
A total of 146 patients who had both biopsy results
and matched urine samples were analyzed in the present study,
including 49 patients with biopsy-proved AR. Among the 49 patients
with AR, 37 were diagnosed as acute cellular rejection (ACR),
exhibiting significant infiltration of interstitial mononuclear
cells, including >25% of parenchyma affected and moderate (>4
mononuclear cells/tubular cross section) to severe tubulitis
(>10 mononuclear cells/tubular cross section); and 12 were
diagnosed with ABMR, exhibiting microvascular inflammation or
arteritis and positive C4d staining results (data not shown).
Demographic information for the four histologically-defined groups
is summarized in Table I, and no
differences in the baseline characteristics were observed
(P>0.05). The remaining 97 biopsy specimens revealed NO-AR
patients (n=58) in the protocol biopsy, and dysfunction with no
rejection (DNR, n=39), including acute tubular necrosis (ATN; n=10)
and chronic allograft nephropathy (CAN; n=29) in the indication
biopsy.
 | Table I.Baseline characteristics of transplant
recipients, grouped according to histological results. |
Table I.
Baseline characteristics of transplant
recipients, grouped according to histological results.
| Variables | AR (n=49) | ATN (n=10) | CAN (n=29) | NO-AR (n=58) |
|---|
| Mean age (mean ±
standard deviation) | 36.9±9.6 | 37.3±5.8 | 45.8±9.5 | 39.8±10.1 |
| Age range | 25-59 | 27-49 | 23-69 | 22-57 |
| Gender, n (%) |
|
|
|
|
| Male | 34 (69.4%) | 7 (70.0%) | 20 (68.9%) | 36 (62.1%) |
|
Female | 15 (30.6%) | 3 (30.0%) | 9 (31.1%) | 22 (37.9%) |
| Cause of ESRD, n
(%) |
|
|
|
|
|
Glomerulonephritis | 38 (77.6%) | 8 (80.0%) | 24 (82.7%) | 44 (75.9%) |
|
Hypertension | 2 (4.1%) | 0 | 1 (3.4%) | 2 (3.4%) |
|
Obstructive uropathy | 1 (2.1%) | 0 | 0 | 1 (1.7%) |
|
Diabetes | 4 (8.1%) | 1 (10.0%) | 2 (6.9%) | 4 (6.8%) |
|
Others | 4 (8.1%) | 1 (10.0%) | 2 (7.0%) | 7 (12.1%) |
| Dialysis time (mean ±
standard deviation) | 6.5±4.1 | 5.3±2.8 | 6.3±4.7 | 6.9±7.1 |
| HLA mismatch (mean ±
standard deviation) | 3.6±1.3 | 3.5±1.2 | 3.9±1.5 | 3.2±1.3 |
| Cold ischemia (mean ±
standard deviation) | 8.3±1.9 | 8.6±2.0 | 8.5±2.1 | 8.1±1.6 |
| Panel reactive
antibody, n (%) |
|
|
|
|
|
<10% | 44 (89.8%) | 9 (90.0%) | 26 (89.7%) | (93.1%) |
|
>10% | 5 (10.2%) | 1 (10.0%) | 3 (10.3%) | 4 (6.9%) |
Urinary CXCL13/Cr is a diagnostic
biomarker of acute renal allograft rejection
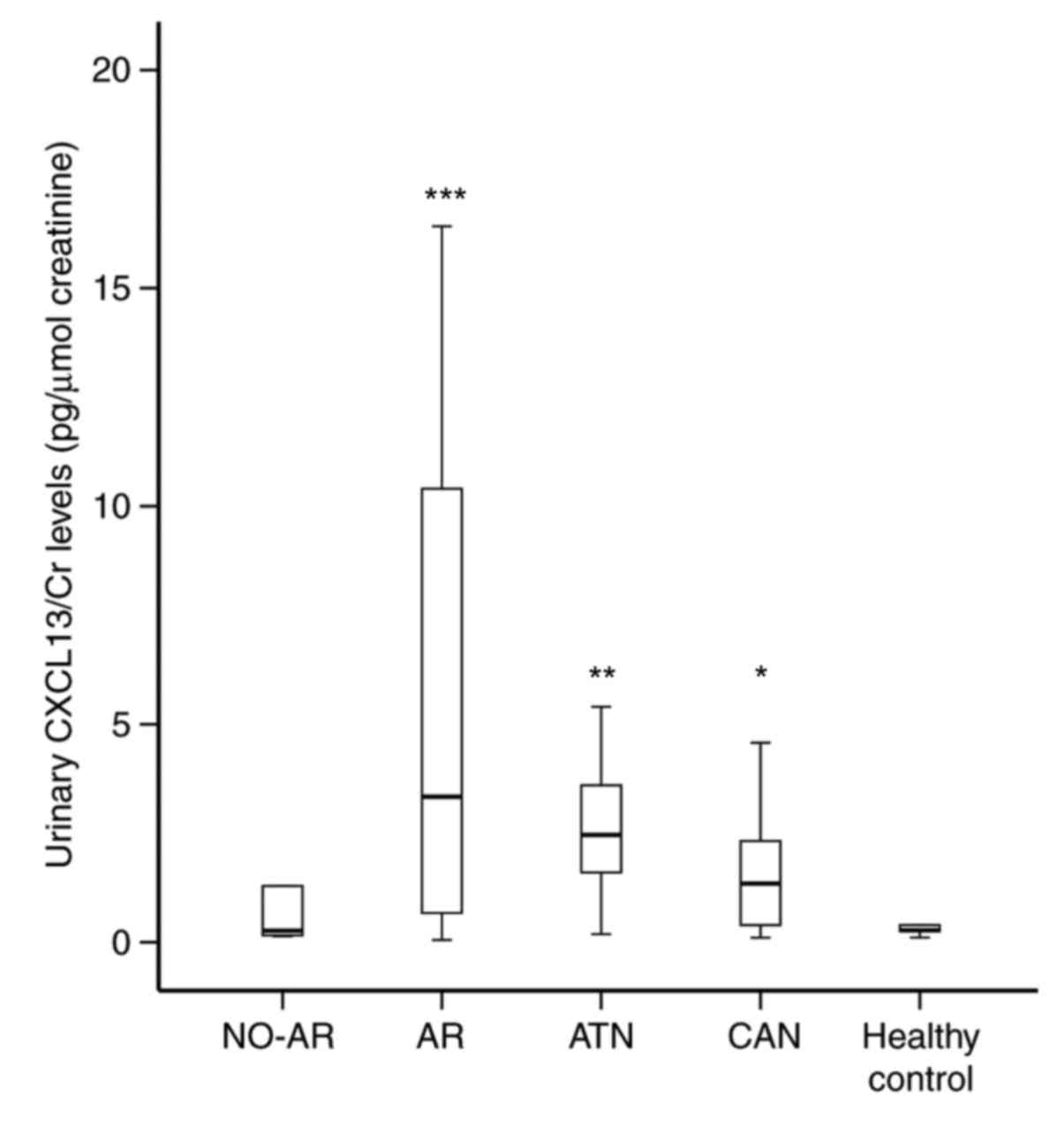
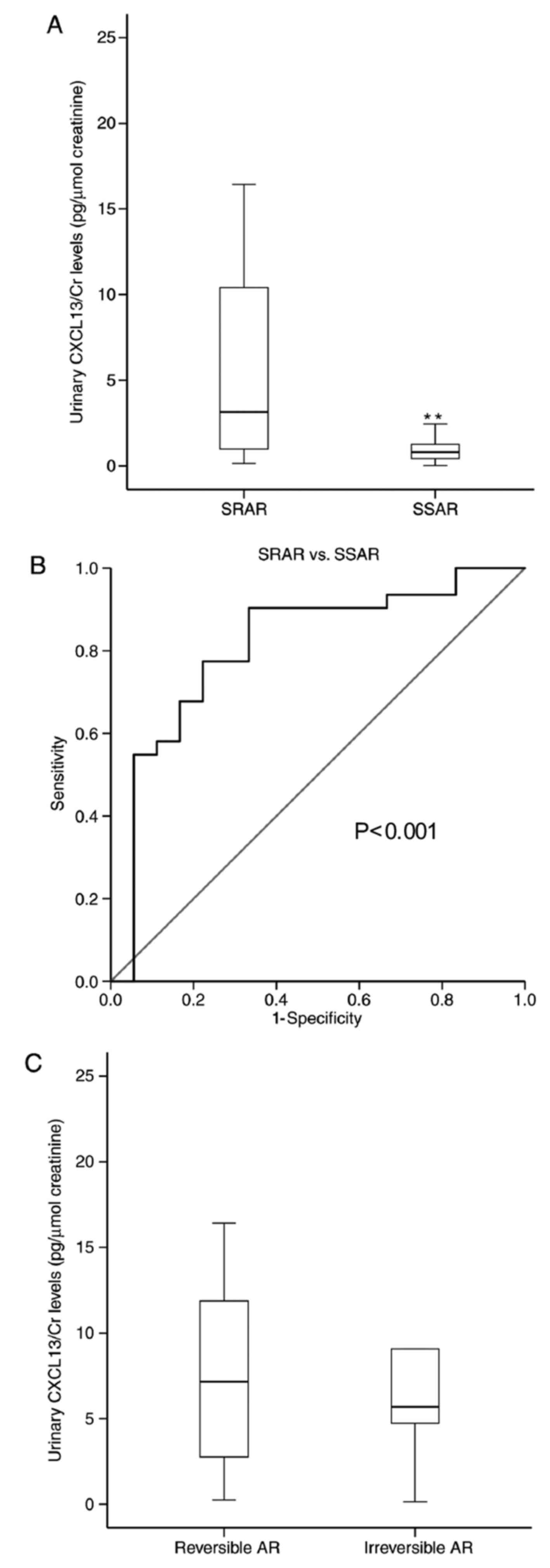
As presented in Fig.
1, the CXCL13/Cr urinary levels were significantly different
between the diagnostic groups (P<0.0001). Urinary CXCL13/Cr was
notably low in NO-AR (median: 0.244; IQR, 0.164–0.562 pg/µmol Cr)
and healthy control subjects (median: 0.275; IQR, 0.165–0.409
pg/µmol Cr) (P=0.772). Conversely, the levels of CXCL13/Cr in the
urine were differentially elevated in patients with ATN (median:
2.46; IQR, 1.370–3.775 pg/µmol Cr; P<0.001), CAN (median: 0.706;
IQR, 0.278–2.309 pg/µmol Cr) (P=0.01), and AR in particular
(median: 2.438; IQR, 0.802–8.261 pg/µmol Cr); P<0.0001) compared
with patients with NO-AR. It is important to note that the urinary
CXCL13/Cr levels in patients with AR were significantly higher than
that of patients with DNR (ATN + CAN; P=0.034).
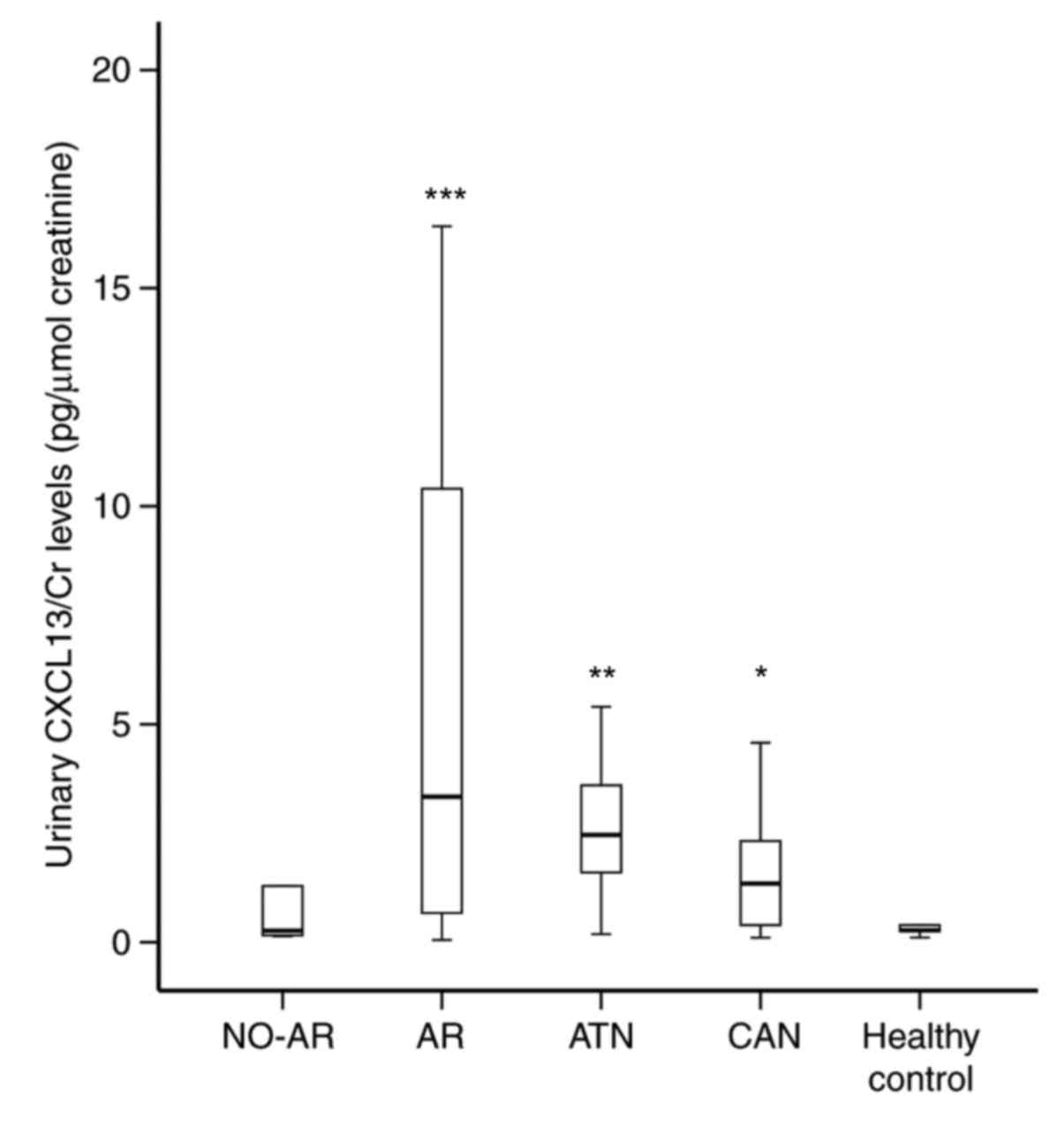 | Figure 1.Median concentration of urinary
CXCL13/Cr in patients with AR, ATN, CAN, NO-AR, and healthy
controls. Among the five groups, there was a significant
statistical difference in the CXCL13/Cr levels in the urine. The
graph shows that urinary CXCL13/Cr levels were significantly
elevated in patients with CAN (n=29), ATN (n=10), and AR (n=49),
compared with in NO-AR patients (n=58), *P<0.01, **P<0.001,
and ***P<0.0001, respectively. ATN, acute tubular necrosis; AR,
acute rejection; CAN, chronic allograft nephropathy; Cr,
creatinine; CXCL13, C-X-C motif chemokine 13; NO-AR, patients with
stable renal function. |
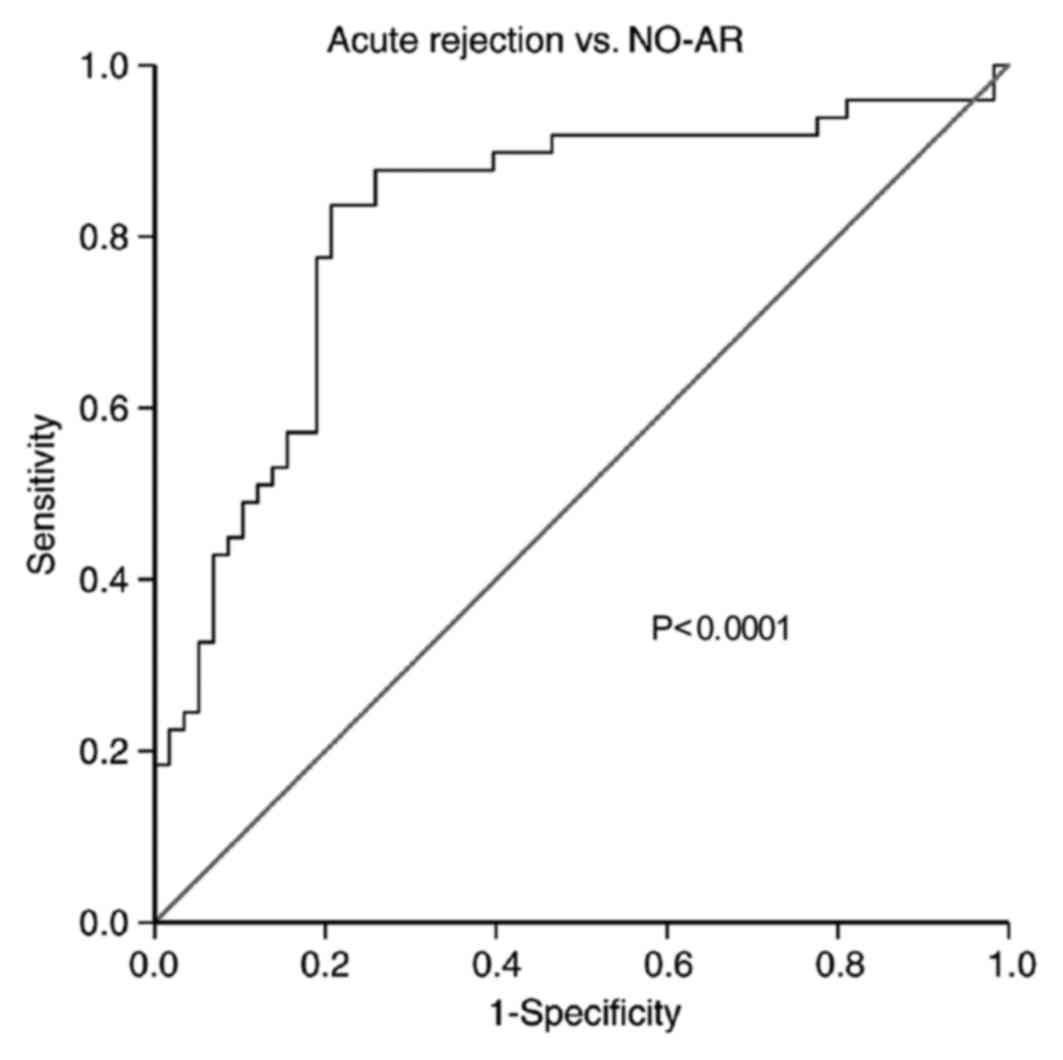
A ROC curve analysis for CXCL13/Cr was conducted to
assess its performance in the diagnosis of AR (Fig. 2), compared with the diagnosis of
NO-AR. The results revealed that CXCL13/Cr yielded a good
diagnostic power, with an area under the curve (AUC) of 0.818 [95%
confidence interval (CI): 0.732–0.903]. At the cut point for
optimizing the diagnostic effect, the sensitivity and the
specificity reached 84 and 79%, respectively. In addition, the
analysis was repeated while distinguishing AR from the DNR
diagnosis, which yielded an AUC of 0.632 (95% CI: 0.516–0.748;
P=0.034).
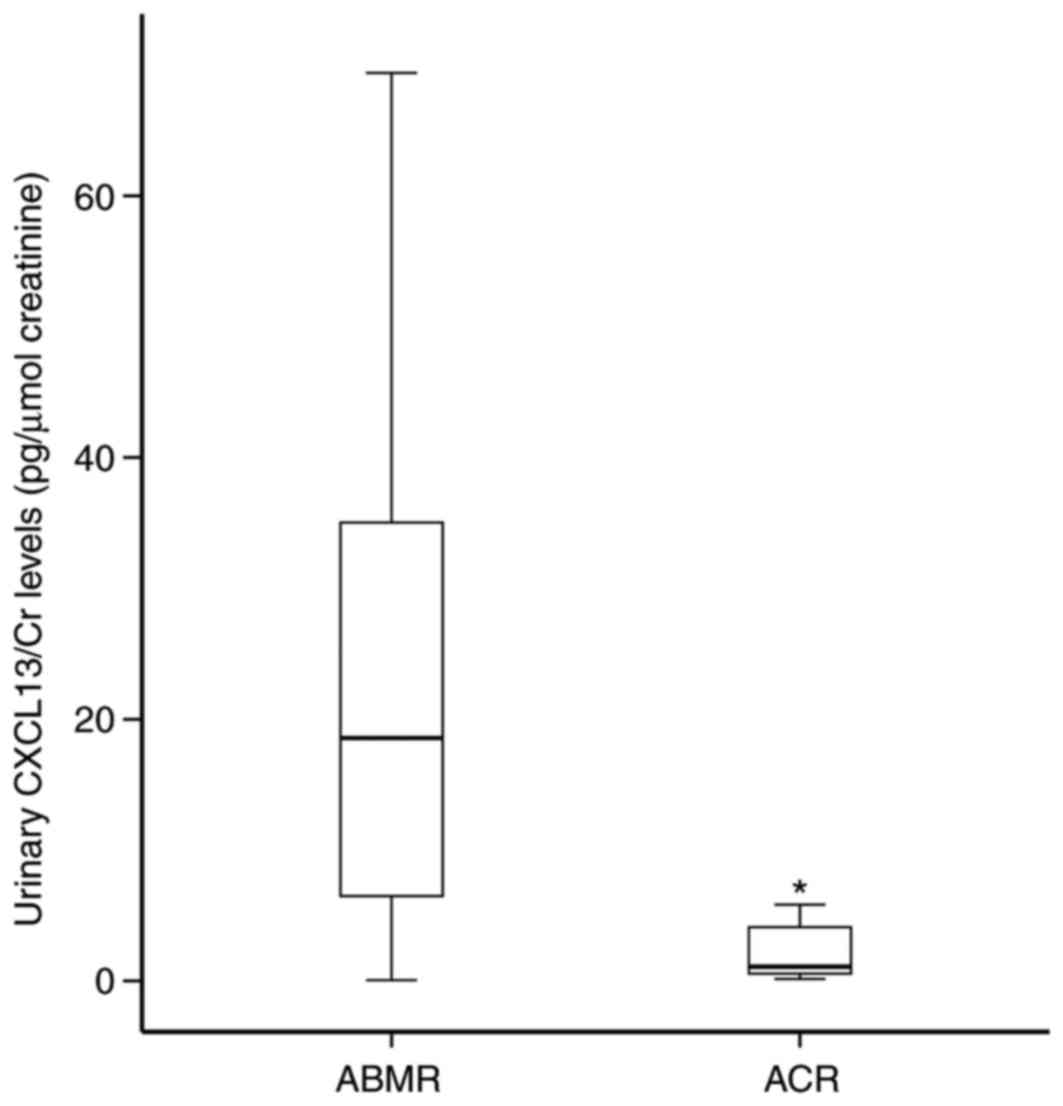
Urinary CXCL13/Cr level identifies
ABMR
Among the 49 patients with AR, 37 were diagnosed as
ACR and 12 were ABMR according to the antibody-mediated rejection
criteria. As expected, the levels of urinary CXCL13/Cr in the
patients with ABMR (median: 18.559; IQR: 5.206–35.281 pg/µmol Cr)
were significantly higher than those with ACR (median: 1.237; IQR:
0.686–4.425 pg/µmol Cr) (Fig.
3).
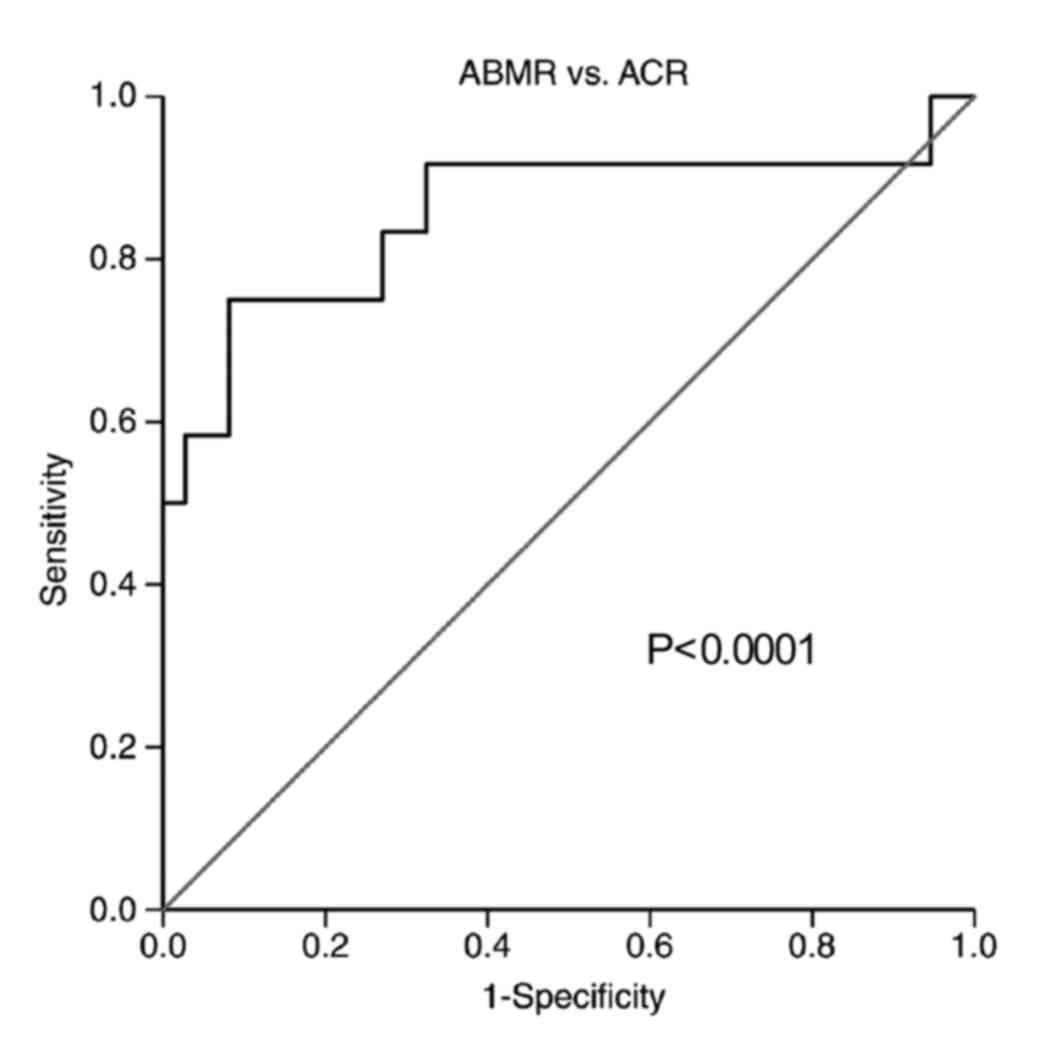
A ROC curve was performed to determine the
discriminatory capacity of CXCL13/Cr levels for ABMR. The results
indicated that urinary CXCL13/Cr effectively distinguished ABMR
from ACR with an AUC of 0.856 (95% CI: 0.701–1.0; Fig. 4).
Levels of urinary CXCL13/Cr are
associated with the response to anti-rejection treatment and
prognosis
The present study analyzed the association between
CXCL13/Cr levels in the urine specimens obtained prior to biopsy
with the response to anti-rejection therapy. As aforementioned, the
AR recipients received anti-rejection treatment with high-dose
methylprednisolone. There were 18 patients who demonstrated a
positive response to anti-rejection treatment, and Cr declined to
baseline levels following anti-rejection therapy
(steroid-sensitive). Conversely, 31 recipients showed a poor
response to anti-rejection treatment, in whom Cr did not recover to
baseline levels and were maintained above 200 µmol/l following
anti-rejection therapy (steroid-resistant). Additionally, 6
patients lost renal function and returned to dialysis after 3
months. Compared with patients with steroid-sensitive AR, urinary
CXCL13/Cr levels were significantly higher in patients with SRAR
(median: 5.55; IQR: 1.508–11.874; P<0.001), as presented in
Fig. 5. Therefore, urinary
CXCL13/Cr may also be used to detect steroid-resistant rejection
among patients with AR. An ROC analysis was performed, which
revealed that the CXCL13/Cr levels in the urine may be a moderately
good predictor of a poor response to anti-rejection treatment, with
an AUC of 0.810 (95% CI: 0.676–0.945). Based on the ROC curve
(Fig. 5), a CXCL13/Cr value of 0.9
was associated with 90% sensitivity and 67% specificity for
detecting a patient with steroid-resistant rejection; however, no
significant discrepancy was observed between the recipients with
allograft dysfunction and reversible acute rejection (P=0.259).
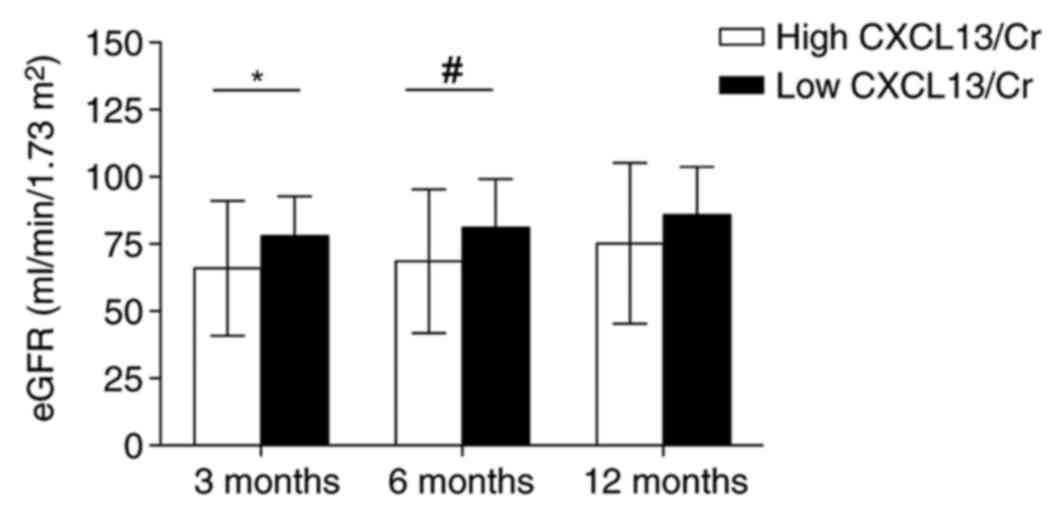
Post-transplantation urinary CXCL13/Cr
levels are associated with restricted graft outcome
Urine samples were obtained from 36 patients with
stable renal function and 21 patients with AR every day within the
first week and at a one-week interval up to the first month
post-transplantation. These samples were additionally used to
investigate whether elevated CXCL13/Cr levels in the urine within
the first month post-transplantation were predictive of graft
function after 3, 6 and 12 months. The 57 patients were divided
into two groups according to the individual mean urinary CXCL13/Cr
levels within the first month post-transplantation; 2 pg/µmol Cr
was defined as the cutoff value. With an exception of 12 months,
the 3 and 6-month estimated glomerular filtration rates were
significantly lower in patients with high CXCL13/Cr levels (>2
pg/µmol Cr) compared with in patients with low CXCL13/Cr levels
(<2 pg/µmol Cr; Fig. 6). In
addition, whether elevated levels of urinary CXCL13/Cr during the
first month post-transplantation were associated with poor graft
function independent of AR was investigated in the present study.
Urinary CXCL13/Cr levels of the patients in the group without any
signs of clinical rejection were analyzed separately. The results
of the analysis indicated that there was no significant difference
in the graft function between patients with high urinary CXCL13/Cr
and the other patients throughout the entire first year (data not
shown).
Discussion
The accurate and timely detection of transplant
rejection and effective therapy are essential for the long-term
survival of kidney transplant patients. Measurement of Scr
following kidney transplantation is one of the most widely used
methods of monitoring renal allograft function; however, the
elevation of Scr is a relatively late event of intragraft injury
(20).
Some publications have revealed that distinct
alterations occur in the levels of certain proteins in the urine
obtained from transplant patients during AR, which are notably
pronounced compared with alterations in Scr. For example, Hu et
al (21) reported that CXCL9
and CXCL10 are associated with acute renal injury, by screening
urine samples for 23 types of chemokines and cytokines. Matz et
al (20) further demonstrated
that CXCL-10 expression in the urine may be used to identify
patients with ongoing AR episodes several days prior to a biopsy
based on increasing Scr levels. In addition, data from a
multicenter observational Clinical Trials in Organ Transplantation
Protocol-01 (CTOT-01) (22)
revealed that CXCL9 protein levels possess a strong predictive
value for noninvasively diagnosing T cell-mediated rejection
(TCMR). In addition, Ho et al (23) recently reported that elevated
urinary matrix metalloproteinase-7 may be used to detect underlying
renal allograft inflammation and injury, which may improve the
overall diagnostic performance of urinary CXCL10 for distinguishing
normal histology from subclinical and clinical injury.
ABMR has gradually become a major problem and is now
considered to be the main cause of long-term allograft dysfunction
compared with TCMR (24); however,
few studies have succeeded in identifying specific biomarkers for
the diagnosis and noninvasive serial monitoring of ABMR. Thus, ABMR
is often underdiagnosed in clinical research and routine clinical
practice. It was reported in the CTOT-01 study (22) that only two ABMRs and four mixed
rejections were diagnosed among 150 indication biopsies.
Using quantitative polymerase chain reaction, we
previously reported that CXCL13 expression levels are significantly
elevated in the peripheral blood mononuclear cells of transplant
rejection patients, which are also associated with a poor response
to anti-rejection therapy (14).
Furthermore, an expression analysis of biopsy specimens indicated
that the intrarenal CXCL13 mRNA expression levels were 27-fold
higher in transplants with B-cell clusters, compared with in
rejecting allografts without B-cell aggregation. Collectively,
these results suggest a potential role for CXCL13 in AR,
particularly in ABMR (13).
The present study reported that transplant patients
with AR episodes exhibited significantly increased urinary CXCL13
protein expression compared with patients with stable renal
function, ATN, as well as CAN. It is important to note that the
CXCL13 expression levels of almost all healthy controls were near
the lowest threshold of detection. In addition, among patients with
AR, the severity was associated with the CXCL13 levels in the
urine, which may be explained by the existence of a positive
feedback mechanism between CXCL13 and its receptor, CXCR5 (25). Additionally, higher CXCL13 levels
in the urine of patients with ABMR were observed, compared with in
patients with ACR. Therefore, the present study conducted an ROC
curve to test the discriminatory power of CXCL13 for ABMR. The
results revealed that AUC reached up to 0.856, with a cut point of
8.26 pg/µmol creatinine. These findings were consistent with the
results of Steinmetz et al (13) and our previous study (14), which generated a convincing
conclusion that the detection of urinary CXCL13 levels may provide
a good basis for the clinical diagnosis of AR and more importantly,
distinguish it from other patterns of rejection.
The prognostic attributes of CXCL13 expression for
AR, particularly ABMR, were further analyzed by conducting kinetic
observations of CXCL13 protein levels in urinary specimens obtained
from a subset of transplant patients. The present study revealed
that the 3 and 6-month renal function of patients with high levels
of CXCL13/Cr post-transplantation was decreased compared with
patients exhibiting low CXCL13/Cr levels; however, no variations
were observed when analysis was limited to patients without AR.
These data revealed an association between enhanced CXCL13
expression in the urine during the first month and intragraft
immune activation, which may result in AR and subsequent
compromised graft function.
The possible origin of CXCL13 has been investigated
in previous studies. In murine secondary lymphoid organs, CXCL13 is
primarily produced by stromal cells resident in B cell follicles,
comprising follicular dendritic cells and marginal reticular cells
(26,27). Conversely, germinal-center
follicular helper T (Tfh) cells may be potent producers of CXCL13
in humans (28,29). The early induction of CXCL13 in the
graft may be the result of tissue injury and innate immune
activation leads to the infiltration of inflammatory cells (such as
Tfh cells), which initiates the secretion of various chemokines,
including CXCL13. The release of CXCL13 may further increase the
recruitment of activated leukocytes to the graft in a
self-sustaining positive feedback loop thereafter.
The primary strength of this assay is its
non-invasiveness, which provides the opportunity for frequent,
serial immune monitoring. Compared with blood biomarkers, urine
markers have several advantages, including the non-invasive nature
of sample collection and few interfering proteins. Thus, this assay
can be performed in clinical practice to instruct clinical
decision-making with respect to the requirement for a biopsy
(separating patients into those that should undergo an immediate
biopsy from those that may be followed-up and even taper their
immunosuppressive therapy). Furthermore, this test may be used to
predict patient responses to anti-rejection therapy.
The present study was associated with several
limitations: Firstly, the clinical-pathological classification of
all patients relied on an allograft histological examination, which
may have been subject to sampling error. Secondly, this was a
retrospective analysis and there was a lack of data on peritubular
capillaritis, and donor-specific antibody status, to regroup all
patients according to the updated Banff criteria (30). Thus, it is possible that mixed
rejection phenotypes may have contaminated the ACR groups; however,
the relatively small in the quantity of ABMR patients suggests that
if the ACR group was contaminated with mixed rejection, the
differences in urinary CXCL13 levels between ACR and ABMR patients
may have been underestimated in the present study. Finally, the
cohort size of the present study was small, and these results will
require validation in larger prospective cohorts.
In conclusion, in addition to confirming the
feasibility of using urinary CXCL13 protein levels for the
noninvasive diagnosis of AR, the results of the present study
demonstrated that urinary CXCL13/Cr levels were highly associated
with ABMR, which may serve to distinguish ABMR from ACR.
Furthermore, patients with heightened urinary CXCL13/Cr were
associated with a poor response to steroid treatment and restricted
short-term graft function. Finally, the present study suggested
that monitoring the expression of CXCL13 protein in the urine of
renal transplant recipients may have contributed to early
individualized rectifications of immunosuppressive therapy and
therefore, lowered the incidence of severe graft damage.
Acknowledgements
The authors would like to thank the pathologists
from the Kidney Disease Immunology Laboratory, the First Affiliated
Hospital of Zhejiang University (Hangzhou, China).
Funding
The present study was supported by grants from the
Medical and Health Technology Development Program in Zhejiang
(grant no. 2014KYA057) and the Foundation of Zhejiang Provincial
Natural Science Foundation of China (grant no. LQ16H050003).
Availability of data and materials
The original datasets used and/or analyzed during
the present study are available from the corresponding author on
reasonable request.
Authors' contribution
JC and DC designed the study. CW and WP performed
sample collection. ZJ and DC performed sample collection, and
acquired and analyzed the data. DC and ZJ contributed to the
writing and editing of the manuscript.
Ethics approval and consent to
participate
All procedures performed in studies involving human
participants were approved by the Ethics Committee of the First
Affiliated Hospital of College of Medicine of Zhejiang University
(Hangzhou, China). All patients provided written informed
consent.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Garcia GG, Harden P and Chapman J: World
Kidney Day Steering Committee 2012: The global role of kidney
transplantation. Lancet. 379:e36–e38. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Ezzat M, El-Gammasy T, Shaheen K and Shokr
E: Elevated production of serum B-cell-attracting chemokine-1
(BCA-1/CXCL13) is correlated with childhood-onset lupus disease
activity, severity, and renal involvement. Lupus. 20:845–854. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hu H, Aizenstein BD, Puchalski A, Burmania
JA, Hamawy MM and Knechtle SJ: Elevation of CXCR3-binding
chemokines in urine indicates acute renal-allograft dysfunction. Am
J Transplant. 4:432–437. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Velaga S, Herbrand H, Friedrichsen M,
Jiong T, Dorsch M, Hoffmann MW, Förster R and Pabst O: Chemokine
receptor CXCR5 supports solitary intestinal lymphoid tissue
formation, B cell homing, and induction of intestinal IgA
responses. J Immunol. 182:2610–2619. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Förster R, Mattis AE, Kremmer E, Wolf E,
Brem G and Lipp M: A putative chemokine receptor, BLR1, directs B
cell migration to defined lymphoid organs and specific anatomic
compartments of the spleen. Cell. 87:1037–1047. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Förster R, Emrich T, Kremmer E and Lipp M:
Expression of the G-protein-coupled receptor BLR1 defines mature,
recirculating B cells and a subset of T-helper memory cells. Blood.
84:830–840. 1994.PubMed/NCBI
|
|
7
|
Gunn MD, Ngo VN, Ansel KM, Ekland EH,
Cyster JG and Williams LT: A B-cell-homing chemokine made in
lymphoid follicles activates Burkitt's lymphoma receptor-1. Nature.
391:799–803. 1998. View
Article : Google Scholar : PubMed/NCBI
|
|
8
|
Smith JR, Braziel RM, Paoletti S, Lipp M,
Uguccioni M and Rosenbaum JT: Expression of B-cell-attracting
chemokine 1 (CXCL13) by malignant lymphocytes and vascular
endothelium in primary central nervous system lymphoma. Blood.
101:815–821. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Amft N, Curnow SJ, Scheel-Toellner D,
Devadas A, Oates J, Crocker J, Hamburger J, Ainsworth J, Mathews J,
Salmon M, et al: Ectopic expression of the B cell-attracting
chemokine BCA-1 (CXCL13) on endothelial cells and within lymphoid
follicles contributes to the establishment of germinal center-like
structures in Sjogren's syndrome. Arthritis Rheum. 44:2633–2641.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shi K, Hayashida K, Kaneko M, Hashimoto J,
Tomita T, Lipsky PE, Yoshikawa H and Ochi T: Lymphoid chemokine B
cell-attracting chemokine-1 (CXCL13) is expressed in germinal
center of ectopic lymphoid follicles within the synovium of chronic
arthritis patients. J Immunol. 166:650–655. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Mazzucchelli L, Blaser A, Kappeler A,
Schärli P, Laissue JA, Baggiolini M and Uguccioni M: BCA-1 is
highly expressed in Helicobacter pylori-induced mucosa-associated
lymphoid tissue and gastric lymphoma. J Clin Invest. 104:R49–R54.
1999. View
Article : Google Scholar : PubMed/NCBI
|
|
12
|
Steinmetz OM, Stahl RA and Panzer U:
Chemokines and B cells in renal inflammation and allograft
rejection. Front Biosci (Schol Ed). 1:13–22. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Steinmetz OM, Panzer U, Kneissler U,
Harendza S, Lipp M, Helmchen U and Stahl RA: BCA-1/CXCL13
expression is associated with CXCR5-positive B-cell cluster
formation in acute renal transplant rejection. Kidney Int.
67:1616–1621. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Mao Y, Wang M, Zhou Q, Jin J, Wang Y, Peng
W, Wu J, Shou Z and Chen J: CXCL10 and CXCL13 Expression were
highly up-regulated in peripheral blood mononuclear cells in acute
rejection and poor response to anti-rejection therapy. J Clin
Immunol. 31:414–418. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chen D, Peng W, Jiang H, Yang H, Wu J,
Wang H and Chen J: Noninvasive detection of acute renal allograft
rejection by measurement of soluble Tim-3 in urine. Mol Med Rep.
16:915–921. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Racusen LC, Solez K, Colvin RB, Bonsib SM,
Castro MC, Cavallo T, Croker BP, Demetris AJ, Drachenberg CB, Fogo
AB, et al: The Banff 97 working classification of renal allograft
pathology. Kidney Int. 55:713–723. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Peng W, Chen J, Jiang Y, Shou Z, Chen Y
and Wang H: Acute renal allograft rejection is associated with
increased levels of vascular endothelial growth factor in the
urine. Nephrology (Carlton, Vic.). 13:73–79. 2008.PubMed/NCBI
|
|
18
|
Wu JY, Chen JH, Wang YM, He Q and Wu DB:
Improved clinical outcomes in Chinese renal allograft recipients
receiving lower dose immunosuppressants. Transplantation.
78:713–718. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Racusen LC, Halloran PF and Solez K: Banff
2003 meeting report: New diagnostic insights and standards. Am J
Transplant. 4:1562–1566. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Matz M, Beyer J, Wunsch D, Mashreghi MF,
Seiler M, Pratschke J, Babel N, Volk HD, Reinke P and Kotsch K:
Early post-transplant urinary IP-10 expression after kidney
transplantation is predictive of short- and long-term graft
function. Kidney Int. 69:1683–1690. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hu H, Kwun J, Aizenstein BD and Knechtle
SJ: Noninvasive detection of acute and chronic injuries in human
renal transplant by elevation of multiple cytokines/chemokines in
urine. Transplantation. 87:1814–1820. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Hricik DE, Nickerson P, Formica RN, Poggio
ED, Rush D, Newell KA, Goebel J, Gibson IW, Fairchild RL, Riggs M,
et al: Multicenter validation of urinary CXCL9 as a
risk-stratifying biomarker for kidney transplant injury. Am J
Transplant. 13:2634–2644. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ho J, Rush DN, Krokhin O, et al: Elevated
urinary matrix metalloproteinase-7 detects underlying renal
allograft inflammation and injury. Transplantation. 100:648–654.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Rabant M, Amrouche L, Lebreton X, Aulagnon
F, Benon A, Sauvaget V, Bonifay R, Morin L, Scemla A, Delville M,
et al: Urinary C-X-C motif chemokine 10 independently improves the
noninvasive diagnosis of antibody-mediated kidney allograft
rejection. J Am Soc Nephrol. 26:2840–2851. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Jenh CH, Cox MA, Hipkin W, Lu T,
Pugliese-Sivo C, Gonsiorek W, Chou CC, Narula SK and Zavodny PJ:
Human B cell-attracting chemokine 1 (BCA-1; CXCL13) is an agonist
for the human CXCR3 receptor. Cytokine. 15:113–121. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kielczewski JL, Horai R, Jittayasothorn Y,
Chan CC and Caspi RR: Tertiary lymphoid tissue forms in retinas of
mice with spontaneous autoimmune uveitis and has consequences on
visual function. J Immunol. 196:1013–1025. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Crotty S: Follicular helper CD4 T cells
(TFH). Ann Rev Immunol. 29:621–663. 2011. View Article : Google Scholar
|
|
28
|
Kim CH, Lim HW, Kim JR, Rott L, Hillsamer
P and Butcher EC: Unique gene expression program of human germinal
center T helper cells. Blood. 104:1952–1960. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Rasheed AU, Rahn HP, Sallusto F, Lipp M
and Muller G: Follicular B helper T cell activity is confined to
CXCR5(hi)ICOS(hi) CD4 T cells and is independent of CD57
expression. Eur J Immunol. 36:1892–1903. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Haas M, Sis B, Racusen LC, Solez K, Glotz
D, Colvin RB, Castro MC, David DS, David-Neto E, Bagnasco SM, et
al: Banff 2013 meeting report: Inclusion of c4d-negative
antibody-mediated rejection and antibody-associated arterial
lesions. Am J Transpl. 14:272–283. 2014. View Article : Google Scholar
|