General context
Evolution of COVID-19 outbreak in
Italy and the patient characteristics
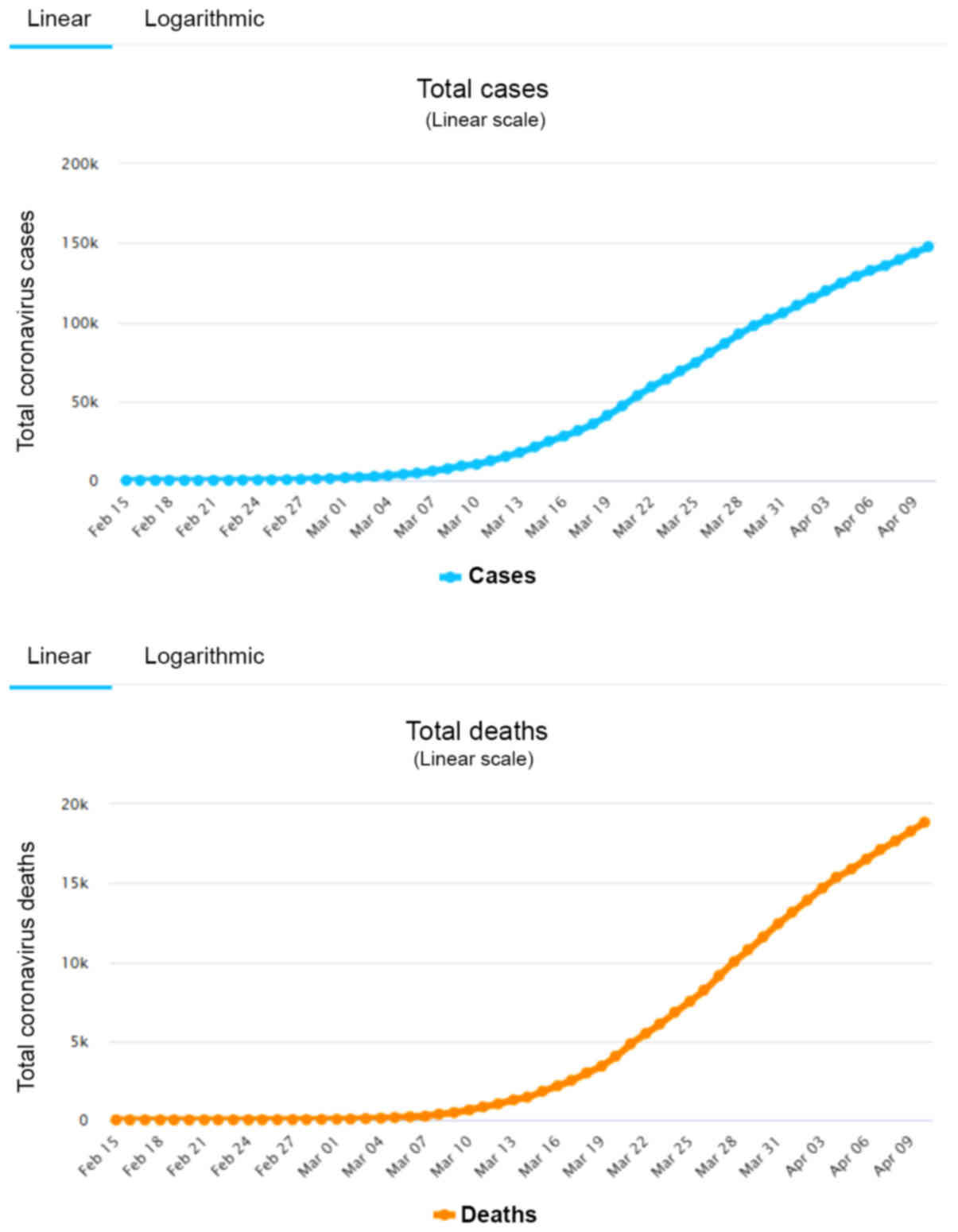
After the beginning of the COVID-19 outbreak in
China, when information of its characteristics began arriving in
Europe, the Italian Ministry of Health established a task-force
group for the coordination of all COVID-19 related issues on 22
January. On 31 January, Italy declared a public health emergency
(1). The first cases of positive
infections attributed to COVID-19 were confirmed by the Superior
Health Institute (Istituto Superiore di Sanità, ISS) on 30 January,
referring to two Chinese tourists already hospitalised from 29
January, in Rome. The first indigenous case, an Italian man aged 38
years, was confirmed positive 3 weeks later, on 21 February in
Codogno (named as patient ‘one’) (1). How patient one was infected remains
unknown, though there are some indications that COVID-19 might have
come to Italy from Germany towards the end of January. In the next
two days, 36 new cases appeared, none of which had contact with the
first patient or anyone with the COVID-19 infection. This was the
beginning of one of the largest and most uncontrolled groups of
patients with COVID-19 in the world, which rapidly triggered
intra-community transmission in Italy. Until 24 February (3 days
later), where the official graphs of disease incidence start, 221
positive cases and 7 deaths were recorded in Italy. From 24
February until 3 March, the number of Italians whose infections
were attributed to SARS-CoV-2 increased 10-fold (2,263 positives
and 79 deaths). Four weeks later (30 March), there were a total of
75,528 positive cases and 11,591 deaths (ca. 150 times increase) in
Italy. The hospitals and medical personnel in Northern Italy became
overwhelmed by the tens of thousands of victims (in just a few
weeks) whose infections were attributed to SARS-CoV-2. On April 10,
there was a total of 147,577 positive cases and 18,849 deaths
(Fig. 1) (2,3). An
analysis of the sub-set of patients whose deaths were attributed to
COVID-19 (4) was performed with a
sample of 1,453 deaths. This analysis showed that 96.5% of people
who died were suffering from one or more pre-existing medical
conditions, such as hypertension (69.9%), diabetes mellitus
(31.8%), and ischemic cardiomyopathy (28.0%) (5). Deaths were associated with one, two
or three co-existing comorbidities in 14.8, 20.7 and 61.0% of
cases, respectively. It is apparent that the existence of
comorbidities is associated with the average age of 78-years of
those who died (median 80, range 5–100, IQR 73–85). Deaths of those
less than 50 years of age were 1.2% of the cases. The average age
of infected people is currently 62 years (32.9% women and 67.1%
men), but this reflects most probably the average age of people
receiving medical assistance who were consequently tested. Among
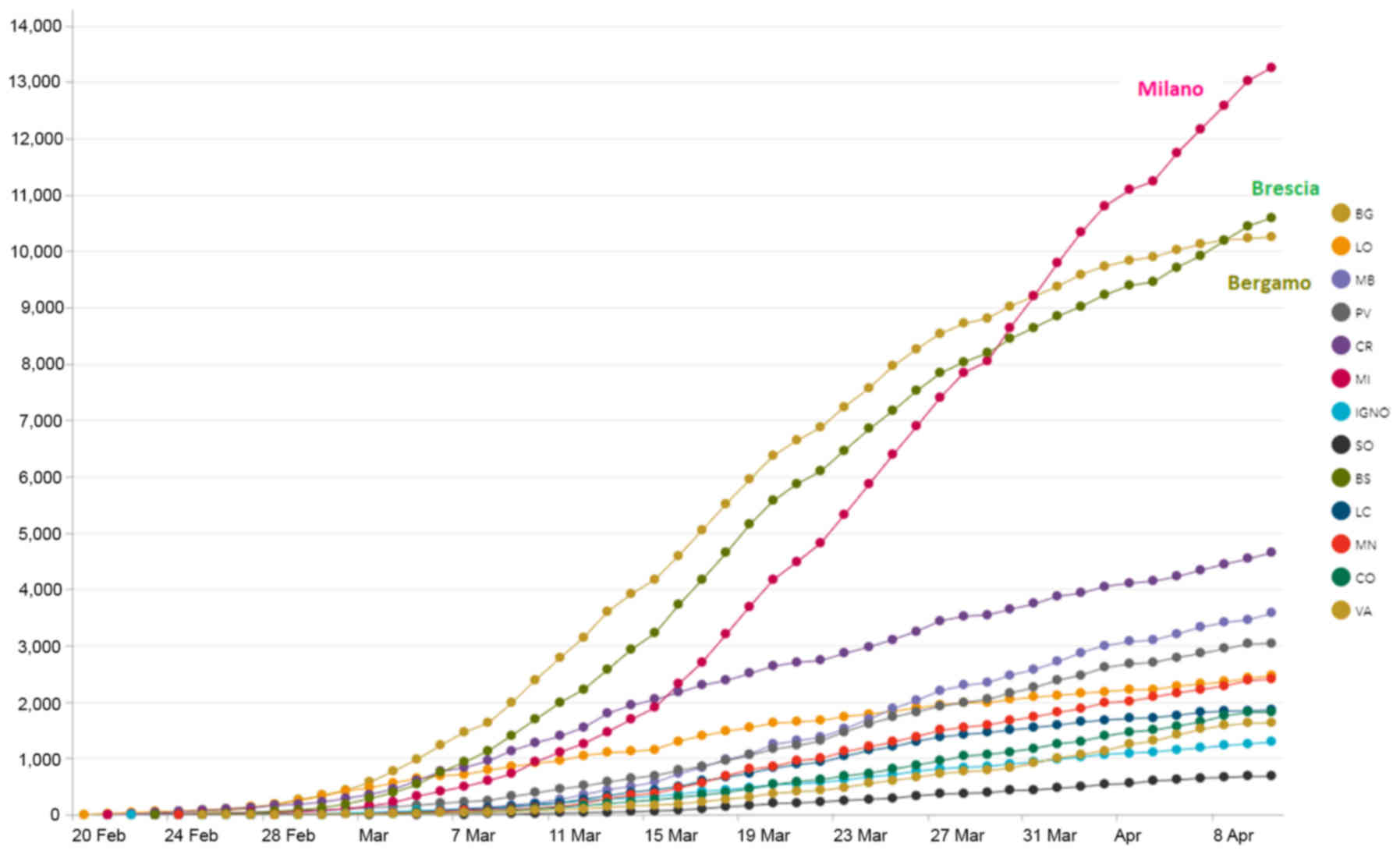
all cases in Italy, 70.2% those who tested positive, and 79.4% of
those who died came from the four Northern Italy regions (Lombardi,
Emilia Romagna, Veneto and Piemonte) where the outbreak started
(Table I and Fig. 2).
 | Table I.COVID-19 outbreak in Northern Italy
up to 10 April 2020. |
Table I.
COVID-19 outbreak in Northern Italy
up to 10 April 2020.
|
| Absolute
figures | % | % of total |
|---|
|
|
|
|
|
|---|
|
| Positive cases | Tests | Deaths | Pos/tests | Deaths/pos | Positive cases | Tests | Deaths |
|---|
| Lombardi |
56,048 | 186,325 | 10,238 | 30.1 | 18.3 | 38.0 | 20.5 | 54.3 |
| Emilia Romagna |
19,128 |
85,884 |
2,397 | 22.3 | 12.5 | 13.0 |
9.5 | 12.7 |
| Veneto |
13,421 | 180,700 |
793 |
7.4 |
5.9 |
9.1 | 19.9 |
4.2 |
| Piemonte |
15,012 |
57,457 |
1,532 | 26.1 | 10.2 | 10.2 |
6.3 |
8.1 |
| Total | 147,577 | 906,864 | 18,849 | | | 70.2 | 56.3 | 79.4 |
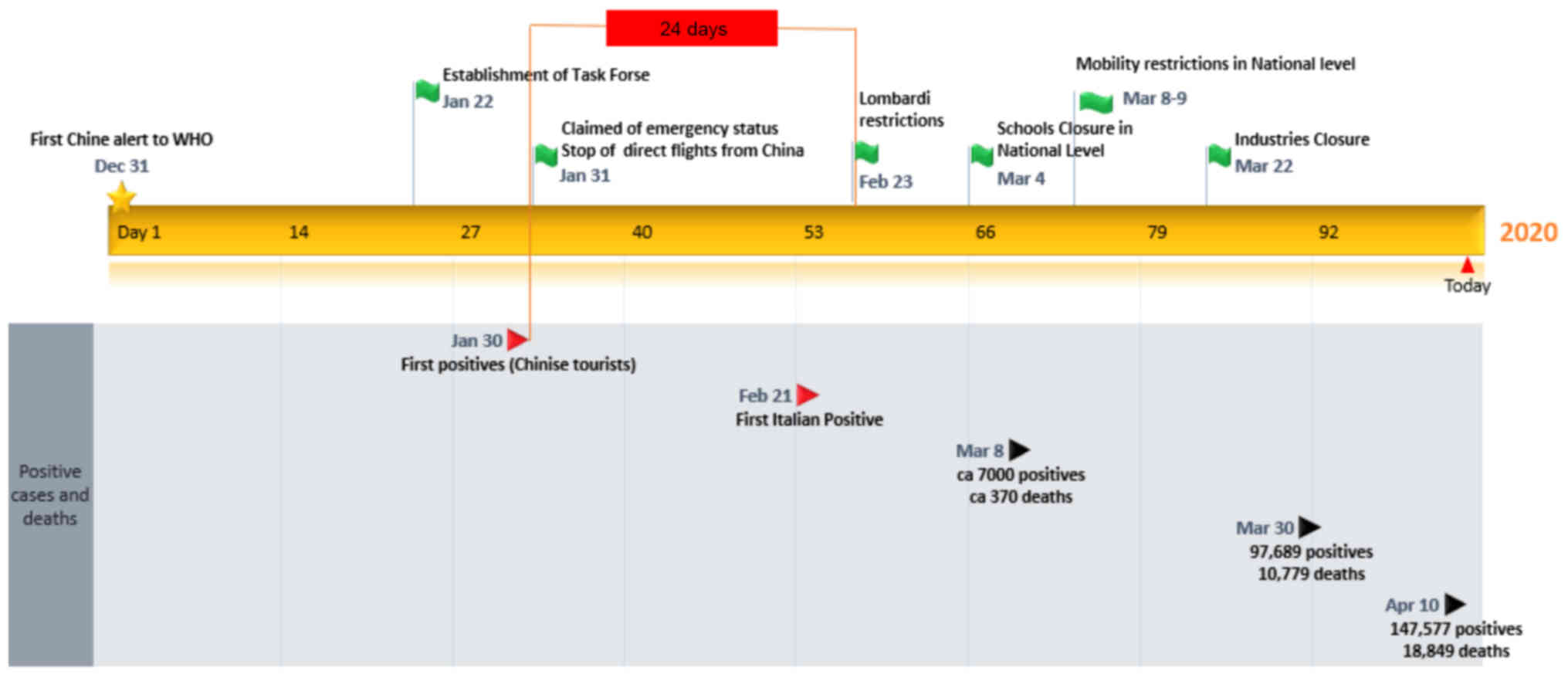
The measures
As shown in the timeline in Fig. 3, the first measures taken against
the COVID-19 pandemic announced on 30 January was with the closure
of direct flights from China. Measures in Lombardi started at
February (6), after the first
positive case of an Italian person in Codogno on 21 February,
locking down specific areas. On 4 March, school closure was
announced at the national level, and a series of mobility
restriction measures started to be applied.
On March 8, following ca. 7,000 positive cases and
ca. 370 deaths recorded, restriction of movement from the Northern
Italy infected areas to the rest of Italy was announced. This
announcement created an immediate wave of people leaving the
infected areas and moving to the rest of Italy leading to a new
restriction one day later, forbidding the mobility among provinces
in all of Italy. On March 22, when deaths had increased to ca. 800
deaths per day, closure of all industries not related to food,
medicines and strategic needs was ordered. For the general
population, mobility was allowed only for serious reasons, such as
specific family needs (e.g., support of elderly family members),
critical employment (e.g., medical doctors, nurses, supermarket
employees), shopping from supermarkets and purchase of medicines,
as well as taking out domestic dogs. A decline in the rate of
increase of new cases were recorded, thus leading the Director of
the Superior Health Institute, Silvio Brusaferro, to state on April
10 that ‘The contagion curve signals a situation in decline but we
must not let down our guard’ (8).
The most recent reduction of admittance of COVID-19 cases to the
emergency department of the aforementioned Northern Italy regions
appears to support this evaluation.
The patient ‘zero’ discussion
The first confirmed COVID-19 patients in Italy were
a couple of Chinese tourists (husband and wife 67 and 66 years old,
respectively). The couple entered Italy on 23 January from the
airport of Milan-Malpensa, passing from Verona and Parma where they
rented a car and drove to Rome. In Rome, they manifested symptoms,
and were confirmed as COVID-19 positives on 30 January. A
phylogenetic analysis indicated that the two persons were infected
in China, probably around 19 January, before their entrance to
Italy (9). These patients were not
characterized as patients ‘zero’ or ‘one’.
Twenty-two days later, on 21 February, an Italian
man was confirmed positive and named as patient ‘one’. The trace
analysis of the so-called patient ‘one’ gave indications that
COVID-19 might have come to Italy from Germany about the end of
January. Up to now, the patient ‘zero’ that infected this patient
(assuming the infection came from another human), is officially
unknown.
Beyond the officially named cases above, there are
articles in journals mentioning that an elderly patient with
COVID-19-related symptoms, entered a hospital in Piacenza (Emilia
Romagna) on January. Later, he was identified positive and
eventually died. Another elderly man entered another hospital in
the same area on February 17, and was also confirmed positive later
(10).
As expected, a thorough discussion in Italian and
global journals describes the possibility that a considerable
number of infected Chinese people entered Italy. The Guardian
mentioned in an article of 25 March cases of prejudice against
Chinese people in Italy, that ca. 310,000 Chinese people are living
in Italy, being the 3rd largest foreign community, with more than
half of them settled in Northern Italy, and ca. 30,000 living and
working in Prato (Tuscany), the center of Italian textile industry
(11). Though the current
consensus in the West is that COVID-19 entered Italy from China, it
does not appear that the workers of Prato are the original carriers
of the virus, as the initial outbreak of infection was not observed
in Prato.
In a mathematical model developed by researchers in
Shanghai, it was calculated that 34 unobserved infected people
travelling out of China in the very beginning of the epidemic would
have been enough to create what we see today (12). Given the fact that commercial
collaboration between China and the rest of the world is strong, it
is apparent that during January thousands of people (Chinese and
Europeans) travelled from China to Europe. Obviously, some of them
were already infected, and most probably, their numbers were higher
than 34. Considering that Lombardi has 3 very busy international
airports (Malpena, Linate, and Bergamo), has strong commerce, and
has a great number of international events organized constantly in
the area, it is safe to assume that a number of infected people,
directly from China but also through other countries (as the case
of the so-called Italian patient ‘one’), entered Italy in that
period. Consequently, it is very probable that it was not only one
patient ‘zero’ but many.
Though direct flight from China to Italy were
blocked on 31 January, infected people were already in Italy as
proven by the entrance of the infected Chinese tourists already
from 23 January. In addition, elimination of direct flights from
China, though a first measure, cannot prevent the entrance of
infected people from China though transit flights and infected
people from other countries.
In conclusion, the number, origin, and identity of
patients ‘zero’ in Italy and other countries will probably remain
unknown. What we do know is that asymptomatic patients and patients
with mild symptoms remained unidentified, greatly contributing in
the spread of the infection.
Demographics and health
Demographics
Population density
Italy has a population density of 192
persons/km2, which is lower than that of other European
countries such as Germany (233 persons/km2) and Belgium
(337 persons/km2), but higher than Spain (92
persons/km2) and France (104 persons/km2)
(13). Wuhan in China, where the
COVID-19 pandemic presumably started, has an urban population of
8,896,900 persons in an area of 1,528 km2 (density 5,823
persons/km2) (14)
(Table II). Considering the
sub-provincial and prefecture population and area, the density is
estimated at ca. 1,200 persons/km2 (15). Codogno, the city in Lombardy where
the Italian outbreak started, has a population density of 790
persons/km2 while Milan has a density of 7,700
persons/km2. As Italy and Spain have higher number of
cases per million habitants (16)
though lower population density, it is clear that this parameter
should be considered per area of frequent mobility of the majority
of the population (e.g., city level) rather than in country level.
In any case, the population density as a factor for the outbreak in
Northern Italy should be evaluated together with other factors that
will be discussed below.
 | Table II.Population density of various
countries and cities of interest. |
Table II.
Population density of various
countries and cities of interest.
| Country/city | Population density
(persons/km2) | Positive cases per
million habitants |
|---|
| Country |
|
Belgium |
337 | 2,049 |
|
France |
104 | 1,240 |
|
Germany |
223 | 1,366 |
|
Italy |
192 | 2,307 |
|
Spain | 92 | 3,172 |
| City |
|
Milan | 7,700 | 4,231 |
|
Wuhan | 5,823 | 5,000 (ca.) |
| Lodi
(province of Codogno) | 1,109 | 2,472 |
|
Codogno |
790 |
187,946a |
Age-distribution
According to Eurostat (17) in 2019, the average age of the
population in Italy was 46.7 years, the highest in Europe (EU-28
average 43.1), seven years older than the average age in China and
slightly above that in South Korea. Italy has the lowest share of
persons of age 0–14 (13.4%) and the highest share of persons above
65 years (22.6%) in the EU. Germany, Portugal and Greece are in the
2nd, 3rd, and 4th places of aged population, after Italy (17) without considerable differences. Up
to now, the data regarding the infection and death curves in
Germany where the first case was reported around the same time as
in Italy, are quite different than the curves in Italy. In Germany,
during the first month, 66 cases and 0 deaths were observed vs.
1,049 cases and 29 deaths in Italy while during the second month
Germany had 52.547 cases and 389 deaths vs. 75.528 and 11.591
deaths in Italy. Thus, it is unclear whether the higher age of
Italian population might at least partially explain the very high
figures of related spread and deaths in Italy. Other factors might
also play a role, such as differences in number of tests made,
differences in testing for SARS-CoV-2 infection at the population
levels and strategy of testing (e.g., only seriously ill
individuals), and different coding of causes of death. The
aforementioned factors may well explain the surprisingly large
difference in spread and case-fatality rates reported across
different countries, including Italy, Spain, Germany and China.
Health state
There are various parameters that are related to the
health state of a country's population such as smoking habits,
sport activities and level of happiness.
Smoking
Smoking increases the expression of the gene for the
conversion enzyme of angiotensin 2 (ECA2), the binding receptor for
SARS-CoV-2, which explains the increased susceptibility to
infection of smokers. Smoking is the leading cause of chronic
obstructive pulmonary disease, and an independent risk factor for
severe evolution of COVID-19. However, a smoking ban law is in
place in Italy since 2005, smoking rate for 2019 was 22% (9.8% in
the ages 65+) with only 14% in Northern Italy (18). The smoking rate for Germany for
2019 was ca. 21.6% with Bavaria and Baden-Württemberg which have
the most COVID-19 cases have the lowest smoking rates in Germany
(20.6 and 21.3%, respectively) (19). Though there is no doubt that
smoking increases susceptibility to COVID-19 symptoms' severity,
there is no reason to believe that it is a key parameter for
Northern Italy outbreak in comparison with other countries.
Physical activity, obesity and population health
index (PHI)
In Italy, more than 60% of persons aged 50–69 years
and 65+ declare middle or high level of physical activity; Northern
Italy has higher scores than the average (20,21).
Italy has the lowest percentage of overweight population in EU-28,
and the second lowest percentage of obesity (22). In ages 65+, 43 and 14% of the
Italian population is considered overweight (BMI 25–29.9) and obese
(BMI >30), respectively (23),
with Northern Italy having lower values. Regarding various PHI,
Italy together with Sweden have the highest values of Lifestyle and
Health Behaviors Index and a low PHI regarding deaths due to
diseases of respiratory system (24). In a ranking of the Healthiest
Countries 2020 by the Bloomberg Healthier Country Index (25), Italy and Spain had the highest
scores in Europe, considering various factors such as Health risks
(tobacco use, high blood pressure, obesity), healthy diet, outdoor
activities, life expectancy, and causes of death. As indicated from
the above information, the only element related to the COVID-19
extreme outbreak is related to deaths due to respiratory diseases
in the Italian population.
Patient comorbidities
Until 9 April, 83.2% of deaths in Italy were in
patients over 70 years while the infection median age is 62 (vs. 80
for deceased) (4). According to
statistical models, the majority of elderly will probably require
intensive care, putting pressure on the Italian health care system.
Based on existing data, it can be concluded that the deaths caused
by COVID-19 occur mainly among the elderly. This clearly means that
countries will have to take aggressive protection measures for the
protection of the elderly to remain below the critical number of
cases that exceeds the capabilities of their health systems.
However, Japan, an older nation than Italy (the average age of the
Japanese is 47.3 years), had only 59 officially registered deaths
on 31 March. So clearly, age, though important, is not the only
factor involved.
What is highly related to age is the existence of
comorbidities that increase the risk of mortality from COVID-19
infection. Recent statistics on increased mortality in Italy are
based on defining COVID-19 deaths as deaths in patients
hospitalised for SARS-CoV-2 and with a positive PCR test,
independent of pre-existing diseases that could have caused death.
This method was selected because no clear criteria for defining
COVID-19 deaths are available. Choosing to define COVID-19 death in
this way may lead to some level of overestimation of the fatality
rate. On the other hand, deaths at home are not subject of testing
for COVID-19 and consequently a number of COVID-19 related deaths
might not be registered. In any case, ISS reported that ‘Acute
Respiratory Distress syndrome was observed in the majority of
patients (96.7% of cases), followed by acute renal failure (23.5%).
Superinfection was observed in 11% and acute cardiac injury in 9.8%
of cases’. In an ideal situation, a global agreement in the way
COVID-19 deaths are registered should be established to allow for
global monitoring and clear comparisons among countries. This is
the only secure way to learn from each other and allow countries of
the world to follow best practices in managing such pandemics in
the future.
The Italian Public Health Institute (ISS) published
on 26 March 2020 an assessment in a sample of 710 hospitalized
patients who died, according to which only 2.1% of the cases had no
comorbidities. Whereas, 97.9% of the cases had one, two or three
and more pre-existing comorbidities in the 21.3, 25.9 and 50.7% of
the cases, respectively (26). The
most common pre-existing chronic pathologies (diagnosed before
contacting the infection) in deceased patients in Italy were:
hypertension − 73.0%, old diabetes − 31.3%, ischemic heart disease
− 27.8%, atrial fibrillation − 23.7%, chronic renal failure −
22.2%, active cancer in the last 5 years − 17.3%, chronic
obstructive pulmonary disease (COPD) − 16.7% (26). The existence of pre-existing
comorbidities does not mean that COVID-19 infection did not
contribute to the death of patients, but it does show that the
number of deaths in Italy and elsewhere is increasing as a large
proportion of patients had other underlying diseases.
Hypertension
An essential risk factor is antihypertensive
treatment with angiotensin converting enzyme inhibitors (ACE-i).
According to recent data, before hospitalization, 36% of Italian
patients deceased with COVID-19, underwent ACE-i therapy while 16%
was treated with angiotensin receptor blockers (ARBs). It is
unclear at this time whether there is a direct link between severe
progression and/or death and treatment with ACE-i and/or ARBs or it
is just a coincidence caused by old age and high blood pressure
itself (27).
In the case of COVID-19, an important element is the
molecule that acts as a receptor for the virus: the angiotensin
converting enzyme (ACE2) (28). It
is found on the surface of cells lining the airways and lungs,
facilitating the entry of the virus into the body (29). At the same time, ACE2 is a target
of the antihypertensive therapeutic class of ACE-i. Given the high
prevalence of hypertension among severe cases of COVID-19, it has
been hypothesized that hypertensive patients taking these
treatments have an increased risk of COVID-19 infection due to the
high level of the enzyme to which the virus binds (30).
The European Society of Cardiology (ESC) recommended
continuing antihypertensive treatment with these drugs and
emphasized the lack of evidence to support the adverse effect
(31). High ACE2 levels (also due
to anti-hypertensive drug therapy) might even be beneficial, and
not adverse, given the competition for the same receptor between
ACE2 and viral spike protein for the same ACE2 reception (this is
the rationale for a trial initiated currently with ACE2 as basis
for two nationwide studies investigating this issue in Italy)
(32).
Diabetes mellitus
Diabetes increases the risk of severe evolution of
COVID-19, under conditions of glycemic imbalance, and even
pulmonary bacterial over-infection. COVID-19 increases the risk of
diabetic complications, including diabetic ketoacidosis, an acute
complication, with a severe prognosis. The mechanism by which
diabetes complicates the evolution of COVID-19 is not known exactly
(33).
Studies on other infections that overlap with
diabetes describe hyperglycemia as a promoter of immunosuppression.
In addition, diabetes is associated with cardiovascular and kidney
disease and older age, and all of these factors contribute to the
severe evolution of infections. The interaction between diabetes
and the virus is complex, and it is not clear whether hyperglycemia
contributes to SARS-CoV-2 virulence, or whether it alters
carbohydrate metabolism. In addition, the metabolic imbalances
caused by diabetes are multiple and lead to a pro-inflammatory and
pro-oxidative status in the body, which decreases resistance to the
virus. ACE-i, is also used commonly for diabetes patients to
prevent diabetic micro- and macro-vascular complications, which can
affect the cardiovascular and renal systems. However, as we
mentioned above there is no evidence to suggest that ACE-i
treatment was discontinued in diabetes during the COVID-19 epidemic
(34).
Though the correlation between the death probability
of COVID-19 patients and existence of comorbidities is apparent,
there is no reason to believe that this is a phenomenon specific
for Northern Italy. The comorbidities mentioned above are usually
found in the elderly all over the word.
Cancers
Cancer patients are more susceptible to infection
than the general population due to the immunosuppression produced
by the cancer itself but also by the antineoplastic treatments.
Among the groups of patients most at risk of severe infections are
those with haematological disorders (leukemia, lymphoma),
leukopenia caused by neoplasia and treatment (chronic decrease in
the number of leukocytes), low level of immunoglobulins (as in
multiple myeloma), chronic immunosuppression by treatments such as
corticosteroids or monoclonal antibodies, allogeneic stem cell
transplantation or other cell therapies (35).
The pulmonary impairment induced by major
cytokine-mediated inflammation underlies severe events in patients
with COVID-19. However, the immune system is affected in cancer by
overexpression of immunosuppressive cytokines, decreased
proinflammatory signals, impaired dendritic cell maturation and
increased immunosuppressive leukocyte count (36).
The evolution of COVID-19 in cancer patients has
been highlighted in a recent study showing the increased risk of
hospitalization, severe evolution and death for oncological
patients, as well as shorter duration until the occurrence of
severe events (37). The study
analyzed 1,590 patients. Of these, 18 (1%) had a history of cancer
- a proportion higher than the incidence of cancer in the Chinese
population (0.29%, according to 2005 estimates). Lung cancer was
the most common form in infected patients (28%). Of the 18
oncological patients, 16 had received treatment, of which 4 had
been treated by chemotherapy or surgery in the previous month. They
were at even greater risk of severe events (3 of the 4 patients),
compared to those who had been treated long ago (6 of the 14
patients). Compared with the rest of the group, cancer patients
were older (63.1 vs. 48.7 years, mean age), more were smokers (22
vs. 7%), had more severe respiratory manifestations (47 vs. 23%)
and had a more severe CT scan (94 vs. 71%).
Genetic polymorphisms and susceptibility to
COVID-19 in Italy
Genetic predisposition can be a key point related to
regional/territorial and ethnic differences on COVID −19 incidence
and severity of the disease. Research in the topic of polymorphism
related to COVID-19 susceptibility is at the beginning. Still, many
studies have been focused mainly on genes such as ACE2 and TMPRSS2
that modulate the expression of angiotensin I, converting enzyme 2
(ACE2) receptor and transmembrane protease serine 2 (TMPRSS2). ACE2
is the receptor used by the S protein of COVID-19 to bind to and to
facilitate the attachment to target cells, while TMPRSS2 is
implicated in the fusion between viral and cellular membranes by
cleaves protein S at the S2 and S1/S2 sites (37–39).
Down expression of ACE2 receptors determined by ACE2 polymorphism
could decrease the possibility that the virus enters in the
organism and have a protective effect. In contrast, the higher
expression is associated with higher susceptibility and worst
evolution (12). Asselta et
al (40), tried to explain the
high incidence, severity and sex differences in COVID-19 infection
in Italy by investigating the polymorphism of ACE2 and TMPRSS2
genes. However, no difference in ACE2 genes was found that could
explained the sex differences or higher susceptibility and
mortality in the Italian population. Regarding the genetic
variation in TMPRSS2, 3 variants were observed, one exonic variant
(p.Val60Met) and 2 haplotypes that are more frequent in Italian
population compared to the East Asian population that also
determines an increased susceptibility to influenza (40). Further studies should be done in
order to validate this hypothesis that can help the physicians to
identify risk population and apply personalized preventive and
therapeutic strategies.
For the purpose of our analysis, the existing data
are very limited to allow to consider this factor as a key
contributor for the outbreak, thought this remains a
possibility.
Societal customs and epidemic-specific
attitudes
Societal customs
Indoor social life
In Northern Italy, mainly due to the climate but
also as habit, there is a preference to in-door gathering social
activities instead of out-door (out-door shifts in bars and
restaurants are less common than in other countries). The COVID-19
outbreak in Northern Italy started at the end of January -
beginning of February 2020, when meteorological conditions restrict
social activities to indoors, favoring a high rate of viral and
bacterial transmission/contamination. Furthermore, it should be
noted that elderly people in Northern Italy are very social, and
they are used to indoor activities such as dancing and gaming
places, probably more frequently than in Southern Italy and other
countries. It is also frequent to visit emerging care units for
very simple medical cases, a factor that probably contributed
further to the observed high rate of contamination.
Family habits
Another important factor that probably contributed
significantly to the high rate of contamination is family habits.
According to Eurostat data of 2018, in Italy the mean age that
young people (which can host the virus without symptoms) leave the
parental household is 30.1 years [4th position after Croatia,
Malta, and Slovakia (41)]. The
EU-28 average is 26.0 years while in Germany, France, Spain, and
Greece the average is 23.7, 23.7, 29.5 and 29.3 years, respectively
(41). In addition, extended
families in Italy as well as in the rest of Mediterranean countries
are very close with frequent physical contact between them, putting
the elderly in Northern Italy at risk. This intergenerational mix
may have played an important role in the high infection rate.
However, data has shown that other countries with similar family
habits, like Greece, avoided such high spread of infection,
indicating that more factors likely play a role.
Epidemic-specific attitudes
Privacy
Searching for other attitudes that might have played
a role in the high infection rate in Northern Italy, we came to the
following two possible factors. The first factor is related to the
level of interpersonal open communication. People in many countries
usually avoid speaking and revealing personal information including
health issues. In the case of COVID-19 epidemic avoidance to share
with friends and colleagues that symptoms appeared, prevents other
persons from being alerted, isolate themselves and to ask for
medical consultation and/or care in time. However, the level of
contribution of this factor in Northern Italy outbreak is difficult
to estimate objectively, and it cannot be considered as unique to
this case.
Inter-species transmission
A second factor is related to the fact that most of
the families in Northern Italy have dogs. Taking-out the dogs is
permitted and exempted from the mobility restrictions. The case of
inter-species transmission between humans and dogs is not yet
scientifically examined but based on a recent study we performed
there are no reasons to believe that this transmission possibility
does not exist (42). However, in
the absence of adequate experimental studies also this factor
cannot be considered at present; yet it remains as a
possibility.
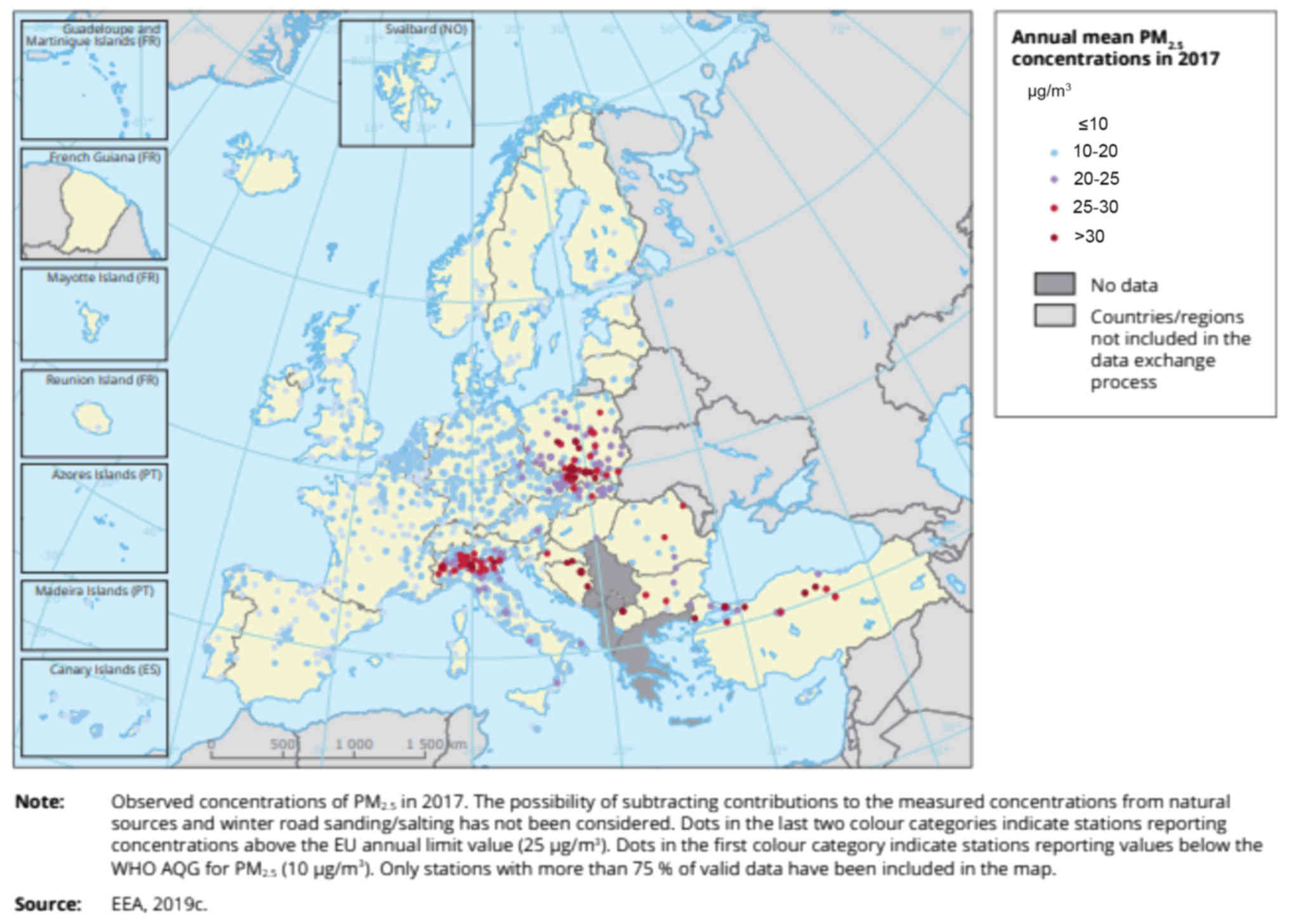
Environmental factors
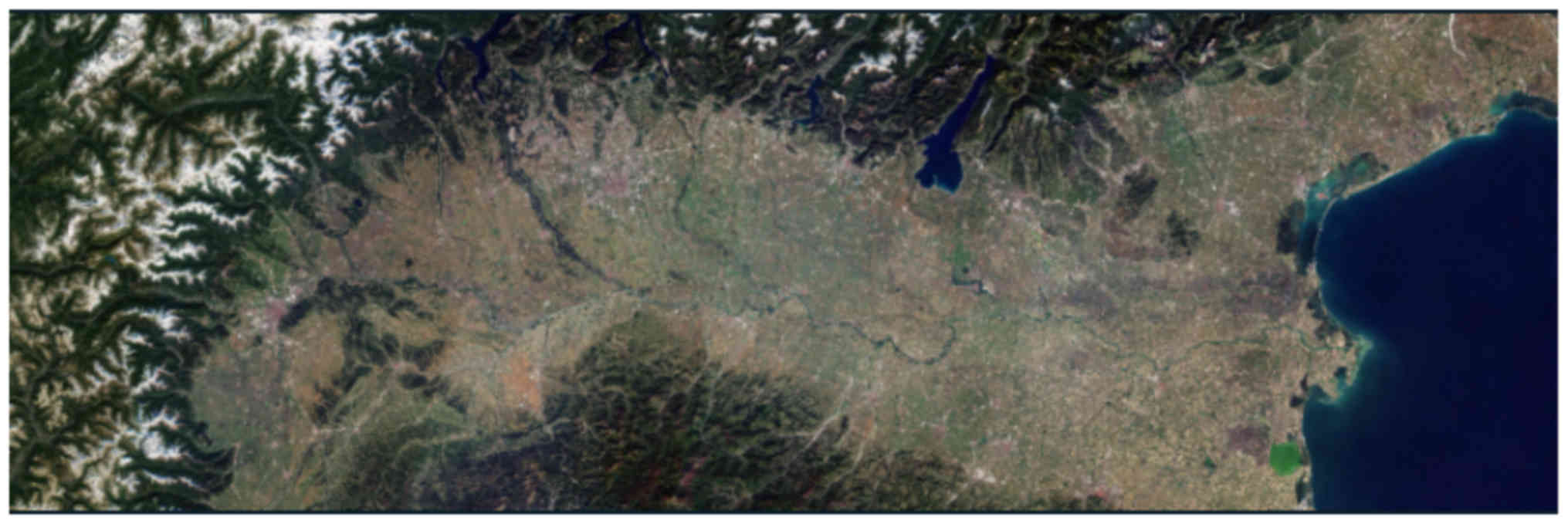
Po valley in Northern Italy is the area between the
Alps and the Appennines and it includes the regions of Lombardia,
Emilia Romagna, Piemonte, Veneto, Friuli Venezia Giulia (and all
‘red’ zones of Codogno, Lodi, Cremona, Padua, Bergamo, and Brescia)
(Fig. 3) (43). Po valley is the industrial center
and the most densely populated area of Italy. Due to the large
number of industries as well as the climate of this area (high
humidity, plain, very low wind intensity), Po valley has a very
poor air quality, characterized by high concentrations of fine
particles, nitrogen dioxide, and ozone) (Figs. 4–6; Table
III) (44,45).
 | Table III.Percentage of Italian urban
population exposed to concentrations above EU standards for
selected pollutants such as BaP, NO2, O3,
PM10 and PM2.5 for the years 2012–2017 (45). |
Table III.
Percentage of Italian urban
population exposed to concentrations above EU standards for
selected pollutants such as BaP, NO2, O3,
PM10 and PM2.5 for the years 2012–2017 (45).
|
|
| 2013 | 2014 | 2015 | 2016 | 2017 |
|---|
| BaP | Annual mean |
2.8 |
1.5 |
7.8 |
5.7 |
6.6 |
| NO2 | Annual mean | 27.5 | 15.7 | 27.9 | 23.2 | 23.8 |
| O3 | Percentile
93.15 | 52.0 | 25.6 | 72.5 | 45.4 | 62.9 |
| PM10 | Percentile
90.41 | 64.9 | 48.9 | 64.9 | 42.5 | 44.2 |
| PM2.5 | Annual mean | 72.0 | 27.0 | 78.3 | 59.2 | 75.0 |
As indicated by European Environment Agency (EEA)
the worst cases in Europe regarding the risk accumulation due to
exceedance of EU limits and exposure of the urban population to all
three pollutants simultaneously (PM, O3, and
NO2), refer to 2.0 million inhabitants in the Po valley
and 0.5 million inhabitants in Greece (44).
Poor air quality is associated with chronic lung
disease and decreased lifespan. PM can deteriorate lung and
cardiovascular diseases and has been shown to decrease life
expectancy. NO2 can affect the lung, the liver, and the
blood, increase the effects of already existing lung diseases as
well as to increase the susceptibility to respiratory infections.
Inhalation of O3 leads to decrease of the inhaled oxygen
having as secondary effect overload of the heart (46). For this reason, it further
increases the risk for people with respiratory and/or heart
diseases.
Based on data above we believe that as high air
pollution in Northern Italy is an area specific factor and highly
related with possible compromise of the health of respiratory
system of the population, it could be an important contributing
factor in the COVID-19 extreme outbreak.
Finally, any lifestyle, iatrogenic, biotoxic, or
environmental/occupational factor, or especially combinations of
such factors, that have been shown in the biomedical literature to
adversely impact the immune system cannot be ruled out as
contributing to increased incidence of viral infections.
Identifying any such potential contributing factors, and
attributing them to any particular region or country, requires a
separate and major study.
Administrative issues
Administrative organisation of Italy,
bias, and bureaucracy
Italy is organized in 20 regions that have a great
level of autonomy including different health systems. This autonomy
gave the power to the various regions to decide the way to confront
COVID-19 pandemic, taking different measures and applying different
in-house made protocols. This stand also for municipalities inside
the regions. This autonomy resulted in valuable time being lost
until a more harmonised strategy could be applied.
In the beginning of the outbreak, and though a
centralized taskforce was in place from the 22 January, a
significant number of politicians and scientists seemed to
underestimate the risk, producing controversary and some misleading
claims. As an example, though at 23 February the President of
Lombardi Region announced the first restrictive measures (6), on 27 February, a campaign was
launched by the Milan Mayor, with the logo ‘Milan don't stop’
(‘Milano non si ferma’), promoting mobility, aiming to protect
people from being afraid, and based on the belief that the
possibility of a serious outbreak was an exaggeration.
Though, information from China was already available
and many scientists globally warned about the risk of a great
outbreak, this knowledge was not used efficiently, resulting in the
fast spread of COVID-19 in the population. The fact that Milan and
Bergamo areas have three international airports and a great number
of visitors from all over the world, for business and tourism, the
effect of this international influx of people was probably
underestimated.
After the beginning of the spread, authorities
failed to inform the citizens promptly. Communication on events
where positive cases where identified were not announced publicly
or they were announced only at community level. Consequently, a
large number of citizens initially took no measures to restrict
contact with infected persons. Decision-making for weeks was not
based on a prevention logic, but rather following the already
existing cases. Restriction of mobility among areas in all Italy
was decided after closure of universities and the transfer of
students from Northern Italy to the whole territory.
Another key factor that prevents stopping the
COVID-19 spread on-time is related to the extreme bureaucracy and
the lack of flexibility in decision making. Public administration
and public officers' culture demands following strictly procedures
even in the case that are not fit-for-purpose and not
result-oriented, minimizing the capacity to operate with
flexibility and under extreme conditions where procedures are not
in place. Serious delays still exist in communicating test results,
end of quarantine certificates, etc.
The collapse of the health system
The Italian health system in the affected areas has
been overwhelmed by the massive increase in the number of patients
with the new coronavirus and is currently struggling to cope. The
lesson learned in the devastated Northern of Italy is that the
infection spread should be controlled before the healthcare system
reaches the saturation point. Saturation of the health system leads
to a tremendous increase of deaths and undermines the efficacy of
the medical staff performance. One of the worst fears of the
Italian government is that as the virus starts to spread to the
south of the country, much poorer and much less equipped, if the
experience of Northern Italy is repeated in the south.
The latest data show that medical personnel make up
ca. 9% of the total cases of COVID-19 in Italy, much higher than
the percentage claimed in China. The high rate of infections among
healthcare professionals is an important problem because those
infected must be isolated and cannot work for at least 14 days,
further weakening the already exhausted workforce. The
vulnerability of the medical personnel is related to their daily
contact with infected patients (patients with an important viral
load) as well as asymptomatic. Also, due to the characteristic
demand in the medical sector, which in some cases implies the lack
of a healthy lifestyle, sleep deprivation and chronic fatigue, the
susceptibility to viral infection is increased. Not infrequently,
those in the medical field come to have the most severe forms of
infection. The high proportion of healthcare professionals with
COVID-19 in Italy is a strong warning to the world: protecting
healthcare personnel should be number one priority.
Though Northern Italy has a good health system, it
was found unprepared to deal with the pandemic. Personal protection
equipment was not fully available for the medical staff and there
was no effort to prohibit citizens to take out of market a huge
number of masks without need. Lack of hand sanitizers for the
general population were sold out already from day 1.
Testing strategy
While the original thought of Italian authorities
was to test both symptomatic and asymptomatic, on February 25,
Italy changed its rt-PCR testing strategy for suspected cases of
SARS-CoV-2 infection. The Ministry of Health then issued
recommendation to prioritize testing for patients with clinical
symptoms, suspected of COVID-19 and requiring hospitalization.
Testing was limited to those with mild symptoms. Asymptomatic cases
even after contact with positive cases were not tested. This
testing strategy probably led to a high proportion of positive
results vs tests performed (21.5%, 97,689 positive cases out of
454,030 tested until 30 March) and an apparent increase in
fatality. This is because, in the absence of testing patients with
milder forms of disease and asymptomatic, the real denominator
(real number of positive cases) remains unknown and certainly
higher than the one reported.
South Korea had the necessary kits and equipment to
perform over 10,000 tests a day. Testing started early on a large
scale, setting a world record. By mid-March, South Korea conducted
over 230,000 free tests, including through the drive-through
system. This led to the identification of a large number of people
with mild or borderline symptoms. This may be one of the reasons
why South Korea has a much lower claimed fatality rate compared to
Italy (1.0 vs. 7.2% - on March 17). Mass testing was one of the
reasons for the successful model in controlling the spread of
infection. In Germany, a leader in the UE in terms of health
infrastructure, a similar pattern was followed as in South Korea,
including asymptomatic persons. With an extensive network of
laboratories at regional level that allows mass testing, the system
can perform approximately 12,000 tests per day.
It is clear as mentioned before that comparison of
fatality rate between countries is meaningful only when the same
testing strategy and the same approach on considering deaths as
COVID-19 deaths, is applied. It is apparent that full testing from
the very beginning allows to form the best strategy to prevent
spread of infection and to estimate better the real fatality. In
the absence of such possibility (due to no testing availability or
financial reasons), restriction of citizens mobility is necessary
to minimises the spread. Wide testing as measure to decrease spread
when the infection curves are in maximum and restriction measures
are in place are of low value. However, such strategy can still
give a better idea of the real ‘picture’ and it might be deemed
necessary when re-opening will be considered. In this case, the
kind of test, its accuracy and sensitivity, and data regarding the
degree of immunity that can be developed after contamination,
should be considered.
Discussion
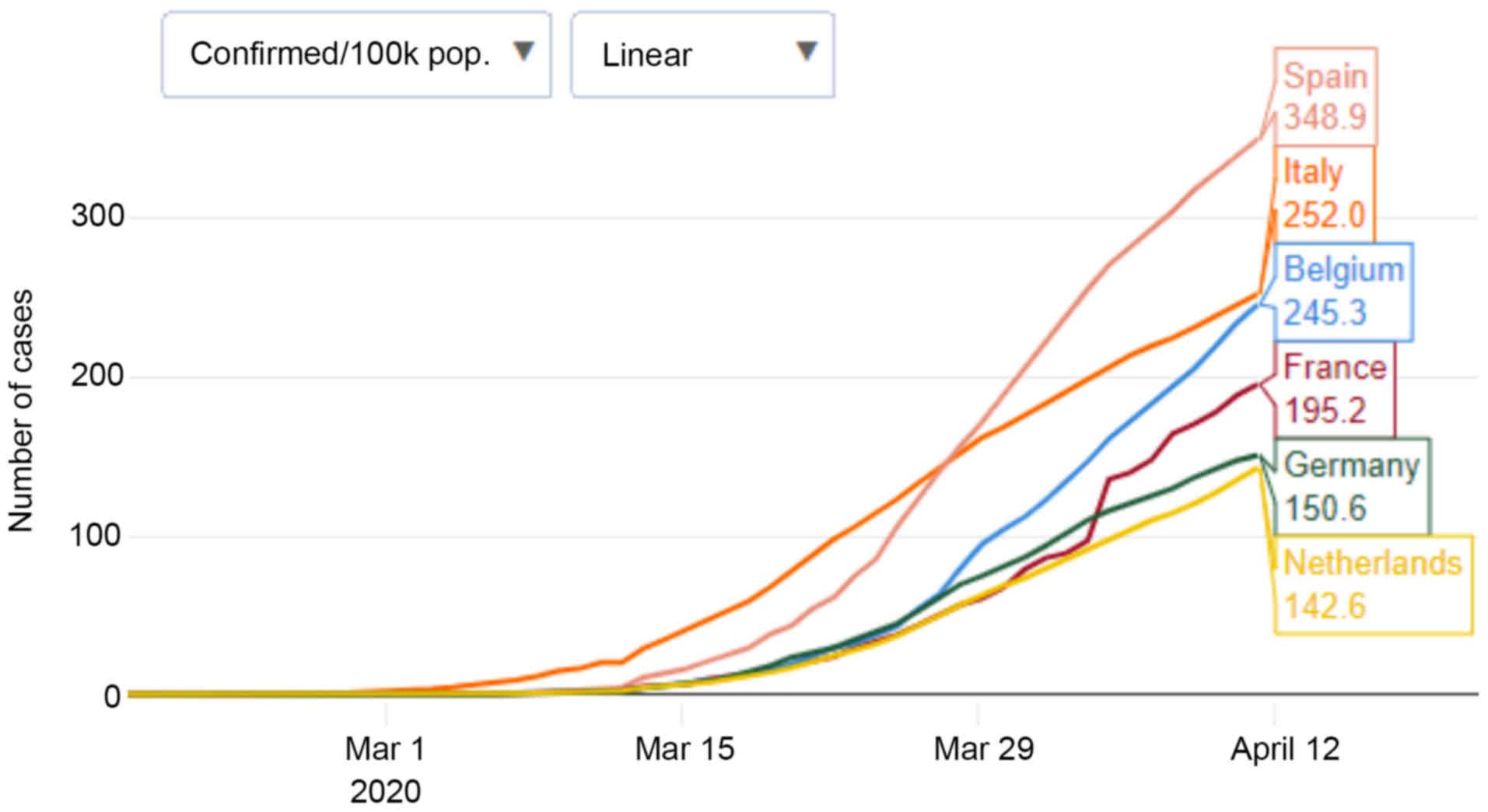
As shown in Fig. 7,
global epidemiological data indicate that the epidemic evolution in
each country follows different curves, with different infection
rates, different figures regarding the number of positive cases,
the presumed percentage of infected population and the number of
related deaths. The reason for these differences is clearly
multiparametric and is related to the factors analysed above, and
possibly others. The evaluation of which factor is more specific
for Northern Italy and which might contribute the most is quite
complex and with high uncertainty. For this evaluation, we compared
the relevance of these factors for four different cases; Northern
Italy, Germany (central Europe, high positives, low deaths), and
Greece (south Europe, low positives, low deaths) using a scale of
relevance from 1 to 3+ (Table
IV). Greece up to 10 April had 2,011 positive cases (ca. 20 per
100,000 people) and 90 deaths (47).
 | Table IV.Comparison of factors relevance among
Northern Italy, Germany, and Greece. |
Table IV.
Comparison of factors relevance among
Northern Italy, Germany, and Greece.
| Factor | Northern Italy | Germany | Greece |
|---|
| Population
densitya | ++ | ++ | ++ |
|
Age-distribution | +++ | +++ | +++ |
| Smoking | + | ++ | +++ |
| Physical activity
and Population health index | ++ | ++ | ++ |
| In-door social
life | ++ | ++ | + |
| Family habits | ++ | + | +++ |
| Environmental
factors | +++ | + | ++ |
| Administrative
organisation, bias, and bureaucracy | +++ | NA | – |
| The collapse of the
health system | +++ | – | – |
| Testing
strategy | ++ | NA | ++ |
Patient comorbidities were not evaluated as they are
highly related to the age distribution.
As discussed before, population density, age
distribution, and physical activity combined with the population
health index are factors with very similar figures among various
countries (Italy, German and Greece in our example) and though they
play a role in a pandemic cannot be considered specific for Italy.
Regarding smoking it appears that northern Italians smoke much less
than in other areas, where the COVID-19 curves have a better
evolution (e.g., Greece). In-door social life is also a
characteristic common in most of the central and north European
countries with better COVID-19 evolution and though it can be
considered as a contributing factor, this is not enough to explain
the differences. Family habits are mentioned in various analyses as
a key factor for the difference of epidemic evolution between Italy
and Germany. However, it is generally acceptable that Greece as
well as S. Italy have in overall even more strict family ties than
in Northern Italy. Though, the evolution of the epidemic is better
in these areas. The issue of pollution of Po valley is a point that
could be considered as specific for Northern Italy. But again,
given the fact that also Greece (mainly in the area of Athens) as
well as some areas of Germany also have high air contamination, it
remains questionable if this is the key factor for the observed
differences of the contagious curves. The exact details for the
testing strategies are not available and a comparison cannot be
done securely. However, data on April 11 have shown that Italy
tested slightly more individuals than Germany (16,708 vs. 15,730
per million persons), and many more than Netherlands (5,926) and
Greece (4,055) (49), where the evolution of the contagion is much
more benign in all aspects.
Based on our analysis the administrative
organisation issues, human bias, and bureaucracy in relevance to
the epidemic seems to be the key factors for the extreme outbreak
in Northern Italy. Human bias could be considered the first and
most important factor. In the fields of psychology and sociology
the effects of bias in cases of danger and crisis are well known.
As it is already shown in studies made particularly for the case of
COVID-19, people tend to be overoptimistic considering that the
issue is not related to them (50,51).
This optimism together with emotional reactions leading to ignore
important numeric information, prioritizing freedom over security,
the perception that the danger is too far (China) (51), and the socioeconomic issues related
to an epidemic are factors that delay a rapid and correct reaction
in the beginning of an epidemic. These elements together with the
administrative and bureaucratic issues already discussed led to a
considerable delay in taking efficient measures against the
pandemic in Northern Italy leading to an excessive spread in the
very first stage (ca. all February) which is still difficulty to
put under control. On the contrary, countries that managed to take
measures very fast and applied them using centralized
administration and IT tools managed to keep the spread under
control (e.g., Greece).
The collapse of the health system is clearly the key
factor for the increased number of deaths. When infection is spread
so rapidly and a great number of patients is accumulated at the
same time in the same area, the local health systems can easily
pass their capacity. Unfortunately, this happened not only in
Northern Italy but also in many other countries or areas, up to
now, including Spain, UK, New York, and others.
Conclusions and lesson learned
Different epidemic contributing factors were
discussed, addressing those specific for Northern Italy, and which
probably contributed the most in the specific case of extreme
outbreak. Though all factors have some contribution, we consider
that the key factors that allowed the high spread of infections,
were that of existing bias, administrative organisation, and
bureaucracy. The high number of deaths is related to the collapse
of the health system. Apparently, the high number of deaths is also
a secondary result of the increase in the number of positive
cases.
The lesson learned from the Northern Italy COVID-19
outbreak case is that preparedness against infectious outbreaks is
of key importance. The faster the better. Politicians and scientist
should be alerted and ready to deal with such a case having
beforehand established precise emergency protocols. Contact tracing
and a fast, high rate of testing are key to mitigating and,
ultimately, confining the disease; these measures will inform those
that have been infected and those that are actively infected,
respectively. Emergency protocols should cover all aspects of an
epidemic, including activation of emergency measures in the health
system, legislative transformations, clear communication lines,
risk communication issues, and existence/development of
fit-for-purpose IT tools. In addition, strategic/proactive
measures, which, if enacted rigorously, would end most of the
concern about viral exposure translating into viral infection, are
needed. Politicians and involved scientist should also be well
aware about the psychological dimension of the human reactions and
people trained in risk management and risk communication should be
involved. The research in the area of infections should be further
enhanced using the up to now knowledge and experience. Concluding,
it is now clear that in the absence of vaccine, of appropriate
medicines and of immediately available test (as for every new
virus), the only possible measure that can be taken in order to
avoid an outbreak is imposing mobility restrictions as fast is
possible. In the case of Greece, where such measures were imposed
very fast, no exponential increase of infection is observed up to
now. Italy used the same strategy with delay and an outbreak was
inevitable, but it seems that after 6 weeks the peak is reached.
Though the financial impact of the restriction strategy is
important, minimizing the magnitude and the duration of emergency
can allow for a fast re-opening.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
Not applicable.
Authors' contributions
Conceptualization AT, DC, MG, DS, AOD, and DAS;
validation, research, resources, data reviewing, and writing MG,
DS, OA, DP, DT, RK, VR; review and editing, MG, AOD, AT, MA and DC.
All authors read and approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
DAS is the Editor-in-Chief for the journal, but had
no personal involvement in the reviewing process, or any influence
in terms of adjudicating on the final decision, for this article.
The other authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
ISS
|
Istituto Superiore di Sanità
|
|
ACE-i
|
angiotensin converting enzyme
inhibitors
|
|
ARBs
|
angiotensin receptor blockers
|
|
ACE2
|
angiotensin converting enzyme 2
|
|
ESC
|
European Society of Cardiology
|
|
EEA
|
European Environment Agency
|
|
IQR
|
interquartile range
|
|
TMPRSS2
|
transmembrane protease serine 2
|
References
|
1
|
Remuzzi A and Remuzzi G: COVID-19 and
Italy: What next? Lancet. 395:1225–1228. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Wordometer, . Coronavirus Italy, 2020.
https://www.worldometers.info/coronavirus/country/italy/Updated
April 15. 2020.
|
|
3
|
Ministero della Salute, . COVID-19 -
Situazione in Italia. http://www.salute.gov.it/portale/nuovocoronavirus/dettaglioContenutiNuovoCoronavirus.jsp?area=nuovoCoronavirus&id=5351&lingua=italiano&menu=vuotoUpdated
April 14. 2020.
|
|
4
|
Istituto Superiore di Sanità, .
Sorveglianza Integrata COVID-19 in Italia, AGGIORNAMENTO 30 marzo
2020 (2020g). https://www.epicentro.iss.it/coronavirus/bollettino/Infografica_30marzo%20ITA.pdfFebruary
27–2020
|
|
5
|
Istituto Superiore di Sanità, .
Characteristics of COVID-19 patients dying in Italy. Report based
on available data on April 13th. 2020.https://www.epicentro.iss.it/en/coronavirus/bollettino/Report-COVID-2019_13_april_2020.pdf
|
|
6
|
Ministero Della Salute, . Misure urgenti
in materia di contenimento e gestione dell'emergenza epidemiologica
da COVID-19. Regione Lombardia (20A01273). Official Journal of the
Italian Government (Gazzetta Ufficiale). 2020.https://www.gazzettaufficiale.it/eli/id/2020/02/25/20A01273/sgFebruary
23–2020
|
|
7
|
Regione Lombardia, . Interactive map,
2020. http://lispa.maps.arcgis.com/apps/opsdashboard/index.html#/637ec3dc28ec4ea591cc5c724f127701Updated
April 14. 2020.
|
|
8
|
Ministero dellaSalute, . Brusaferro (Iss):
‘La curva del contagio segnala una situazione in decrescita ma non
deve farci abbassare la guardia’. http://www.salute.gov.it/portale/nuovocoronavirus/dettaglioNotizieNuovoCoronavirus.jsp?lingua=italiano&menu=notizie&p=dalministero&id=4444April
10–2020
|
|
9
|
Giovanetti M, Benvenuto D, Angeletti S and
Ciccozzi M: The first two cases of 2019-nCoV in Italy: Where they
come from? J Med Virol. 92:518–521. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
La Repubblica, . Coronavirus, un anziano
colpito a gennaio: il ‘paziente uno’ prima di Mattia. https://www.repubblica.it/cronaca/2020/03/30/news/coronavirus_paziente_uno-252673269/March
30–2020
|
|
11
|
The Guardian, . ‘As if we were the
disease’: coronavirus brings prejudice for Italy's Chinese workers.
https://www.theguardian.com/global-development/2020/mar/25/as-if-we-were-the-disease-coronavirus-brings-prejudice-for-italys-chinese-workersMarch
25–2020
|
|
12
|
Li W, Zhang C, Sui J, Kuhn JH, Moore MJ,
Luo S, Wong SK, Huang IC, Xu K, Vasilieva N, et al: Receptor and
viral determinants of SARS-coronavirus adaptation to human ACE2.
EMBO J. 24:1634–1643. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
World Atlas, . European Countries By
Population Density, 2017. https://www.worldatlas.com/articles/european-countries-by-population-density.htmlUpdated
August 1. 2017.
|
|
14
|
Wikipedia Wuhan, . https://en.wikipedia.org/wiki/WuhanUpdated April
13. 2020.
|
|
15
|
World Population Review, . Wuhan
Population, 2020. https://worldpopulationreview.com/world-cities/wuhan-population/Updated
April 14. 2020.
|
|
16
|
Statista, . COVID-19 cases per million
inhabitants: A comparison. https://www.statista.com/chart/21176/COVID-19-infection-density-in-countries-most-total-cases/April
8–2020
|
|
17
|
Eurostat, . Population structure and
ageing. 2019.https://ec.europa.eu/eurostat/statistics-explained/index.php/Population_structure_and_ageing#Median_age_is_highest_in_ItalyUpdated
July 2020.
|
|
18
|
Istituto Superiore di Sanità, . CS
N°12/2019 - Giornata Mondiale Senza Tabacco: Fumano Ancora Due
Italiani Su Dieci, Al Sud La Percentuale Piu' Alta Di Fumatrici
(2020c). https://ufficiostampa.iss.it/?p=1840March
30–2019
|
|
19
|
Statista, . Smoking rates in Germany.
https://www.statista.com/chart/20011/share-of-the-population-who-smoked-in-german-federal-states/November
19–2019
|
|
20
|
Istituto Superiore di Sanità, . Politiche
di promozione dell'attività fisica il contrasto delle malattie
cardiovascolari (2020d). https://www.epicentro.iss.it/attivita_fisica/attivita-fisica-prevenzione-cardiovascolareFebruary
13–2020
|
|
21
|
Istituto Superiore di Sanità, . La
sorveglianza Passi d'Argento (2020e). https://www.epicentro.iss.it/passi-argento/dati/attivitaFebruary
28–2020
|
|
22
|
Eurostat, . Overweight and obesity - BMI
statistics, 2014. https://ec.europa.eu/eurostat/statistics-explained/index.php/Overweight_and_obesity_-_BMI_statistics
|
|
23
|
Istituto Superiore di Sanità, . La
sorveglianza Passi d'Argento (2020f). https://www.epicentro.iss.it/passi-argento/dati/obesita#datiFebruary
28–2019.
|
|
24
|
Costa C, Santana P, Dimitroulopoulou S,
Burstrom B, Borrell C, Schweikart J, Dzurova D, Zangarini N,
Katsouyanni K, Deboseree P, et al: Population Health Inequalities
Across and Within European Metropolitan Areas through the Lens of
the EURO-HEALTHY Population Health Index. Int J Environ Res Public
Health. 16:8362019. View Article : Google Scholar
|
|
25
|
Miller LJ and Lu W: Economics. These Are
the World's Healthiest Nations. Bloomberg. 2019.https://www.bloomberg.com/news/articles/2019-02-24/spain-tops-italy-as-world-s-healthiest-nation-while-u-s-slipsFebruary
24–2019
|
|
26
|
Istituto Superiore di Sanità, .
Characteristics of COVID-19 patients dying in Italy. Report based
on available data on March 26th. 2020.https://www.epicentro.iss.it/coronavirus/bollettino/Report-COVID-2019_26_marzo_eng.pdf
|
|
27
|
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu
Y, Zhang L, Fan G, Xu J, Gu X, et al: Clinical features of patients
infected with 2019 novel coronavirus in Wuhan, China. Lancet.
395:497–506. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Hoffmann M, Kleine-Weber H, Schroeder S,
Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH,
Nitsche A, et al: SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2
and is blocked by a clinically proven protease inhibitor. Cell. May
4–2020.(Epub ahead of print). View Article : Google Scholar
|
|
29
|
Docea AO, Tsatsakis A, Albulescu D,
Cristea O, Zlatian O, Vinceti M, Moschos SA, Tsoukalas D, Goumenou
M, Drakoulis N, et al: A new threat from an old enemy: Re-emergence
of coronavirus (Review). Int J Mol Med. 45:1631–1643.
2020.PubMed/NCBI
|
|
30
|
Shi S, Qin M, Shen B, Cai Y, Liu T, Yang
F, Gong W, Liu X, Liang J, Zhao Q, et al: Association of cardiac
injury with mortality in hospitalized patients with COVID-19 in
Wuhan, China. JAMA Cardiol. Mar 25–2020.(Epub ahead of print).
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
European Society of Cardiology, . Position
Statement of the ESC Council on Hypertension on ACE-Inhibitors and
Angiotensin Receptor Blockers. https://www.escardio.org/Councils/Council-on-Hypertension-(CHT)/News/position-statement-of-the-esc-council-on-hypertension-on-ace-inhibitors-and-angMarch
13–2020
|
|
32
|
American College of Cardiology, . COVID-19
Clinical Guidance. For the Cardiovascular Care Team. https://www.acc.org//~/media/Non-Clinical/Files-PDFs-Excel-MS-Word-etc/2020/02/S20028-ACC-Clinical-Bulletin-Coronavirus.pdfMarch
6–2020
|
|
33
|
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z,
Xiang J, Wang Y, Song B, Gu X, et al: Clinical course and risk
factors for mortality of adult inpatients with COVID-19 in Wuhan,
China: A retrospective cohort study. Lancet. 395:1054–1062. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Wu Z and McGoogan JM: Characteristics of
and important lessons from the Coronavirus disease 2019 (COVID-19)
outbreak in China, summary of a report of 72,314 cases from the
Chinese Center for disease control and prevention. JAMA.
323:1239–1242. 2020. View Article : Google Scholar
|
|
35
|
Xia Y, Jin R, Zhao J, Li W and Shen H:
Risk of COVID-19 for patients with cancer. Lancet Oncol.
21:e1802020. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Liang W, Guan W, Chen R, Wang W, Li J, Xu
K, Li C, Ai Q, Lu W, Liang H, et al: Cancer patients in SARS-CoV-2
infection: A nationwide analysis in China. Lancet Oncol.
21:335–337. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Kuba K, Imai Y, Rao S, Gao H, Guo F, Guan
B, Huan Y, Yang P, Zhang Y, Deng W, et al: A crucial role of
angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced
lung injury. Nat Med. 11:875–879. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Cheng Z, Zhou J, To KK, Chu H, Li C, Wang
D, Yang D, Zheng S, Hao K, Bossé Y, et al: Identification of
TMPRSS2 as a susceptibility gene for severe 2009 pandemic A(H1N1)
influenza and A(H7N9) influenza. J Infect Dis. 212:1214–1221. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Lu R, Zhao X, Li J, Niu P, Yang B, Wu H,
Wang W, Song H, Huang B, Zhu N, et al: Genomic characterization and
epidemiology of 2019 novel coronavirus: implications for virus
origins and receptor binding. Lancet. 395:565–574. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Asselta R, Paraboschi EM, Mantovani A and
Duga S: ACE2 and TMPRSS2 variants and expression as
candidates to sex and country differences in COVID-19 severity in
Italy. medRxiv. doi.org/10.1101/2020.03.30.20047878.
|
|
41
|
Eurostat, . Estimated average age of young
people leaving the parental household by sex. https://appsso.eurostat.ec.europa.eu/nui/show.do?dataset=yth_demo_030&lang=enUpdated
February 24. 2020.
|
|
42
|
Goumenou M, Spandidos DA and Tsatsakis A:
[Editorial] Possibility of transmission through dogs being a
contributing factor to the extreme Covid-19 outbreak in North
Italy. Mol Med Rep. 21:2293–2295. 2020.PubMed/NCBI
|
|
43
|
European Space Agency, . Po Valley, Italy.
https://www.esa.int/ESA_Multimedia/Images/2019/05/Po_Valley_ItalyMay
17–2019
|
|
44
|
European Environment Agency, . Air quality
in Europe - 2019 report. No 10/2019. https://www.eea.europa.eu/publications/air-quality-in-europe-2019June
24–2019
|
|
45
|
European Environment Agency, . Air
polution profile: Italy (2019b). https://www.eea.europa.eu/themes/air/country-fact-sheets/2019-country-fact-sheets/italy
|
|
46
|
Sarigiannis DA, Kermenidou M, Nikolaki S,
Zikopoulos D and Karakitsios SP: Mortality and morbidity attributed
to aerosol and gaseous emissions from biomass use for space
heating. Aerosol Air Qual Res. 15:2496–2507. 2015. View Article : Google Scholar
|
|
47
|
Greek Civil Protection, . Press Conference
for the COVID-19 evolution. https://www.civilprotection.gr/el/enimerosi-apo-ton-yfypoyrgo-politikis-prostasias-kai-diaheirisis-kriseon-niko-hardalia-kai-ton-14April
10–2020
|
|
48
|
Johns Hopkins University of Medicine, .
Coronavirous Resource Center, 2020. https://coronavirus.jhu.edu/data/cumulative-casesUpdated
April 14. 2020.
|
|
49
|
Wordometer, . Confirmed Cases and Deaths
by Country, Territory, or Conveyance. https://www.worldometers.info/coronavirus/#countriesUpdated
April 15. 2020.
|
|
50
|
Kuper-Smith B, Doppelhofer L, Oganian Y,
Rosenblau G and Korn C: Optimistic beliefs about the personal
impact of COVID-19. PsyArXiv. doi:10.31234/osf.io/epcyb.
|
|
51
|
Van Bavel JJ, Baicker K, Boggio P, Capraro
V, Cichocka A, Crockett M, Cikara M, Crum A, Douglas K, Druckman J,
et al: Using Social and Behavioural Science to Support COVID-19
Pandemic Response. PsyArXiv. doi.org/10.31234/osf.io/y38m9.
|