Introduction
Advanced treatments have effectively reduced the
deaths from myocardial infarction (MI), however the morbidity and
mortality of post-infarction ischemic heart failure (IHF) are
increasing and becoming a major threat to human health worldwide
(1–3). Adverse ventricular remodeling (AVR)
following MI is the pathological basis of IHF and is largely
ascribed to inflammatory responses (4–6).
Various immune cells, including T helper lymphocytes, regulatory T
cells (Tregs), monocytes and macrophages, participate in the
complicated process (7,8). Notably, Tregs, which are regarded to
be a subset of anti-inflammatory lymphocytes, act as a key player
in immune suppression and modulate the immune balance (9–11).
Recently, Tregs have shown to play an important role
in cardiovascular diseases such as dilated cardiomyopathy (12), hypertension (13), atherosclerosis (14), acute coronary syndrome (ACS)
(15) and chronic heart failure
(CHF) (9,16). Clinical studies report that a
reduced number and impaired function of Tregs are present in CHF
(9,10,17).
The underlying mechanism may be attributed to impaired thymic
output of nascent Tregs and increased cell apoptosis in periphery
(10). Following ischemic injury,
high sensitivity to FasL-induced apoptosis or IL-2 deprivation may
also contribute to the defect of Tregs in patients with CHF
(10). Tregs can improve cardiac
repair and attenuate AVR following MI by inhibiting inflammation
and cardiomyocytes damage through cell-to-cell contact and
inhibitory cytokines production, including IL-10 and TGF-β
(17). Additionally, a novel
effector molecule of Tregs, sFGL2, has attracted attention as an
immunoregulatory factor.
sFGL2 belongs to the fibrinogen-related proteins
superfamily, which is mainly secreted by Tregs (18,19).
It exhibits immune regulatory activity in autoimmune
glomerulonephritis (20), renal
allograft acute rejection (21) and
viral hepatitis (22). Recent
evidence has indicated that sFGL2 is able to suppress the immune
response by inhibiting dendritic cell maturation and T cell
proliferation (23). Downregulation
of sFGL2 inhibits differentiation and activity of
CD4+CD25+Foxp3+ Tregs (23). Based on the observation that sFGL2
may be involved in the modulation of inflammatory responses, it was
hypothesized that sFGL2 may play a role in IHF.
Our previous study observed that serum levels of
sFGL2 were markedly reduced in patients with ACS, in accordance
with significantly decreased frequencies of Tregs (24). Long-term coronary ischemia and
inflammatory activation can inevitably give rise to myocardial
damage in ACS patients. Since we had demonstrated an altered status
of sFGL2 in vascular events, it was hypothesized that sFGL2 would
be implicated in the development of cardiac dilatation and
dysfunction. Thus, the present study aimed to measure the serum
sFGL2 levels to explore their possible changes in patients with IHF
and to further assess the association between sFGL2 levels and
cardiac function.
Materials and methods
Subjects
To match the sample size of each group, 136 subjects
were enrolled from the Union Hospital of Huazhong University of
Science and Technology (Wuhan, China) between September 2017 and
December 2018 in the present prospective study (Table I). These subjects were divided into
a healthy control group (n=32) and a IHF group (n=104). In order to
investigate the relationship between serum sFGL2 levels and cardiac
function, the 104 patients with IHF were classified into subgroups
according to the New York Heart Association (NYHA) functional
classification (25) or left
ventricular ejection fraction (LVEF) (25). Based on NYHA classification, the
patient subgroups were NYHA I–II (n=57) and NYHA III–IV (n=47).
Additionally, according to LVEF, the patients with IHF were
subdivided into a heart failure with preserved ejection fraction
(HFpEF) group (LVEF ≥50%, n=37), heart failure with mid-range
ejection fraction (HFmrEF) group (LVEF 40–49%, n=32) and the heart
failure with reduced ejection fraction (HFrEF) group (LVEF <40%,
n=35). The study was approved by the Ethics Committee of Tongji
Medical College, Huazhong University of Science and Technology
(approval. no. IORG0003571) and written informed consent was
obtained from each participant. The present study conformed to the
Declaration of Helsinki principles.
 | Table I.Baseline characteristics of healthy
controls and patients with IHF. |
Table I.
Baseline characteristics of healthy
controls and patients with IHF.
|
Characteristics | Controls
(n=32) | IHF (n=104) | P-value |
|---|
| Age (years) | 65.0±9.5 | 65.88±10.3 | 0.666 |
| Sex
(male/female) | 23/9 | 86/18 | 0.180 |
| Echocardiography
data |
|
|
|
| LVEF
(%) | 65.3±4.5 | 45.8±13.3 | <0.0001 |
| LVEDD
(cm) | 4.5±0.4 | 5.8±0.5 | <0.0001 |
| NYHA
classification |
|
|
|
| I–II
(n) | – | 57 | – |
| III–IV
(n) | – | 47 | – |
| NT-proBNP
(pg/ml) | – |
2,875.27±1,263.30 | – |
| Risk factors |
|
|
|
|
Hypertension, n (%) | 17 (53.1) | 70 (67.3) | 0.144 |
|
Diabetes, n (%) | 8 (25.0) | 43 (41.3) | 0.095 |
|
Hyperlipidemia, n (%) | 18 (56.3) | 76 (73.1) | 0.072 |
|
Smoking, n (%) | 9 (28.1) | 46 (44.2) | 0.105 |
Inclusion criteria
CHF was diagnosed by clinical history, physical
examination, electrocardiography, chest X-ray, echocardiography and
N-terminal pro-brain natriuretic peptide (NT-proBNP). Patients with
CHF were eligible for IHF if they had a history of MI or prior
revascularization, or ≥50% stenosis in two or more major epicardial
coronary artery. For comparison, 32 healthy volunteers from a
routine health examination were enrolled as normal controls, who
had no symptoms or signs of IHF.
Exclusion criteria
Patients with the following diseases were excluded
from the study: Valvular heart disease, rheumatic heart disease,
idiopathic dilated cardiomyopathy, hypertrophic cardiomyopathy,
serious infection, virus hepatitis, autoimmunity disease, renal
failure and malignant tumors.
Blood samples
Peripheral blood samples were obtained from all
patients in a fasting state with clean venipuncture of an
antecubital vein. The first 4 ml were collected into a heparinized
tube and was used for flow cytometric analysis, while the
subsequent 2 ml were collected into a sterile tube without the
anticoagulation for ELISA. Peripheral blood mononuclear cells
(PBMCs) were isolated by Ficoll density gradient centrifugation
(400 × g, 4°C, 25 min) and then used for flow cytometric analysis.
Serum was collected following centrifugation and frozen at −80°C
until analysis.
Flow cytometric analysis of Tregs
PBMCs were washed two times and suspended with PBS
at a density of 1×107 cell/ml. 100 µl of the cell
suspension was transferred to 1 ml Eppendorf tube and then the
cells were incubated with anti-human CD4-FITC (1:50; cat. no.
11-0049-42; eBioscience; Thermo Fisher Scientific, Inc.) and
anti-human CD25-PE (1:50; cat. no. 12-0259-80; eBioscience; Thermo
Fisher Scientific, Inc.) at 4°C for 30 min. Following the surface
staining, the cells were washed once and resuspended in 1X
fixation/permeabilization buffer (500 µl) according to the
manufacturer's instructions (eBioscience; Thermo Fisher Scientific,
Inc.), followed by two washes in 1X permeabilization buffer for
Foxp3 intracellular staining. The cells were then stained with
anti-human Foxp3-APC (1:50; cat. no. 17-4776-42; eBioscience;
Thermo Fisher Scientific, Inc.) at 4°C for 30 min. Isotype controls
were given to insure correct compensation and antibody specificity.
All of the antibodies used for flow cytometry were from eBioscience
(Thermo Fisher Scientific, Inc.). Stained cells were analyzed on a
fluorescence-activated cell sorting (FACS) flow cytometer (FACS
Aria; BD Biosciences). All data were analyzed using FlowJo V7.6.1
(FlowJo LLC).
Proliferation and functional
suppression assays
PBMCs from controls (n=10) and patients with IHF
(n=10) were stained with anti-human CD4-FITC (1:50; cat. no.
11-0049-42; eBioscience; Thermo Fisher Scientific, Inc.) and
anti-human CD25-PE (1:50; cat. no. 12-0259-80; eBioscience; Thermo
Fisher Scientific, Inc.) at 4°C for 30 min. Following surface
staining, CD4+CD25− T cells (responder T
cells; Tresp) and CD4+CD25+ Tregs were
obtained by FACS sorting using a FACS Aria (BD Biosciences).
CD4+CD25− T cells were suspended with PBS at
a density of 2×106 cell/ml and labelled with 2 µM
carboxyfluorescein succinimidyl ester (CFSE; Thermo Fisher
Scientific, Inc.) at 37°C in 5% CO2 for 10 min while
rotating once at 5 min. Then CFSE-labelled Tresp cells
(1×105/well) from controls or IHF group were cultured
alone or co-cultured with CD4+CD25+ Tregs
from controls or IHF group at different ratio of 1:1, 2:1, 4:1 and
8:1 with stimulation of plate-bound anti-CD3 (10 µg/ml;
eBioscience; Thermo Fisher Scientific, Inc.) and soluble anti-CD28
(5 µg/ml; eBioscience; Thermo Fisher Scientific, Inc.). All cells
were incubated in complete RPMI 1640 supplemented with 10% fetal
bovine serum (Invitrogen; Thermo Fisher Scientific, Inc.) with a
final volume of 200 µl/well in 96-well plates (BD Biosciences) at
37°C and 5% CO2 for 4 days. Proliferation of Tresp cells
were analyzed by flow cytometry based on CFSE dilution of gated
CD4+ T cells. The percentages of CFSElow
cells cultured alone or co-cultured with Tregs in each group were
analyzed, and then the reduced proportions of these percentages in
co-culture system were calculated as follows: (A-B)/A, where A is
the percentage of CFSElow Tresp cells cultured alone and
B is the percentage of CFSElow Tresp cells co-cultured
with Tregs.
Detection of cytokines by ELISA
Serum levels of sFGL2 (cat. no. 436907; BioLegend,
Inc.) and cell culture supernatant levels of IFN-γ (cat. no.
430104; BioLegend, Inc.) and IL-17 (cat. no. 433914; BioLegend,
Inc.) were measured using ELISA kits according to the
manufacturer's instructions.
Statistical analysis
Continuous variables were expressed as mean ±
standard deviation in text and figures. Unpaired two-tailed
Student's t-test was performed to detect two group differences and
one-way analysis of variance (ANOVA) with Bonferroni's post-hoc
test for multiple comparisons. Categorical data were expressed as
frequencies and Chi-square test was performed for comparisons
between groups. Pearson's correlation coefficients were used to
establish associations between variables. Cut-off values for serum
sFGL2 levels predicting IHF were analyzed by receiver operating
characteristic (ROC) curve analysis. GraphPad Prism 5.0 (GraphPad
Software, Inc.) and SPSS 19.0 (IBM Corp.) software were used for
data analysis. P<0.05 was considered to indicate a statistically
significant difference.
Results
Basic clinical characteristics
The baseline characteristics of the 136 subjects are
presented in Table I. Groups
(Controls and IHF) were comparable with respect to age, gender and
incidence of hypertension, diabetes, hyperlipidemia and smoking.
Compared with controls, patients with IHF showed a lower LVEF and a
larger left ventricular end-diastolic dimension (LVEDD). Table SI shows the demographic and
clinical characteristics of controls and the NYHA I–II and NYHA
III–IV groups. Basic clinical characteristics of controls and the
HFpEF, HFmrEF and HFrEF groups are summarized in Table SII.
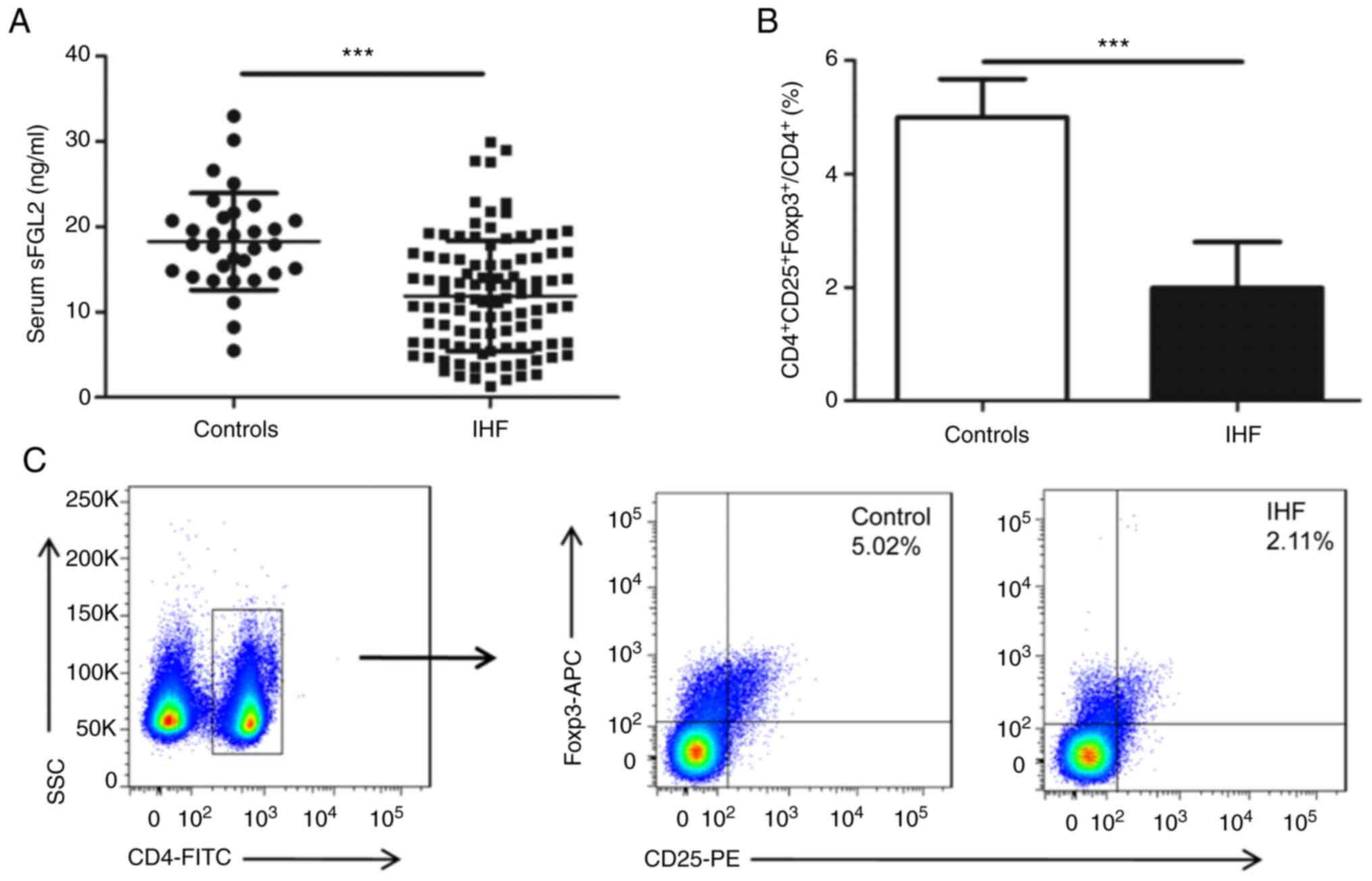
Serum sFGL2 levels and circulating
Tregs frequencies are decreased in patients with IHF
Serum sFGL2 levels and peripheral Tregs frequencies
were measured by ELISA and flow cytometry in patients with IHF,
respectively. As shown in Fig. 1A,
sFGL2 levels were noticeably reduced among patients with IHF
(11.90±6.48 ng/ml) compared with controls (18.27±5.69 ng/ml;
P<0.0001). The frequencies of
CD4+CD25+Foxp3+ Tregs were
significantly reduced in the IHF group (1.99±0.81%) compared with
controls (4.99±0.67%; P<0.0001; Fig.
1B and C).
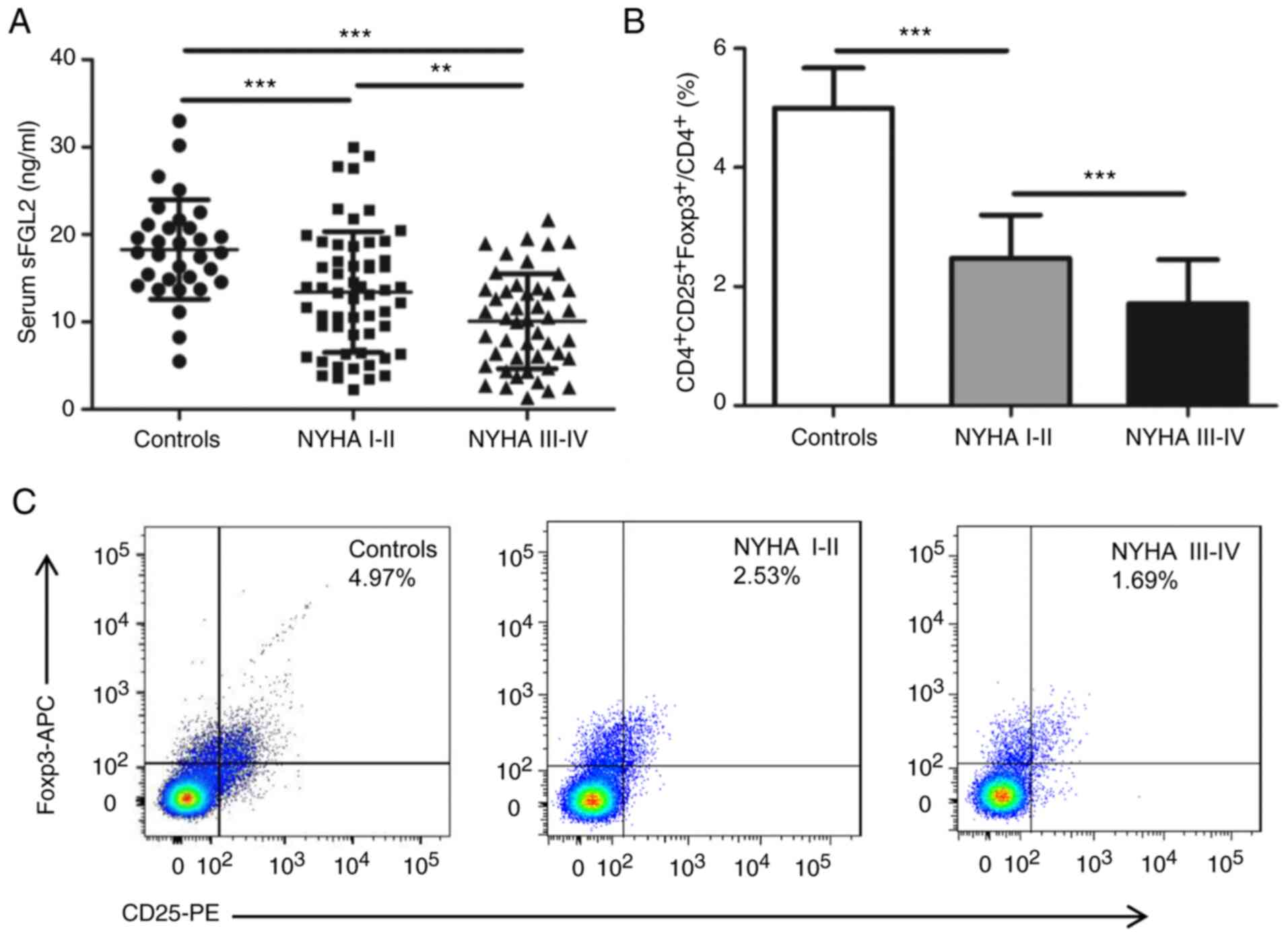
Serum sFGL2 levels and circulating
Tregs frequencies are decreased with the deterioration of cardiac
function in IHF
To investigate the relationship between sFGL2
levels, circulating Tregs frequencies and cardiac function in IHF,
the patients were stratified into subgroups based on NYHA
classification. As shown in Fig.
2A, sFGL2 levels were markedly reduced in the NYHA I–II group
(13.40±6.92 ng/ml, P<0.001) and the NYHA III–IV group
(10.08±5.44 ng/ml, P<0.001) compared with controls (17.73±4.56
ng/ml) and sFGL2 levels in the NYHA III–IV group were even lower
than those in the NYHA I–II group (P<0.01). Similarly, the
frequencies of CD4+CD25+Foxp3+
Tregs were markedly decreased in the NYHA I–II group (2.48±0.72%,
P<0.001) and the NYHA III–IV group (1.72±0.73%, P<0.001)
compared with controls (4.85±0.51%), while Tregs frequencies in the
NYHA III–IV group were further decreased from those in the NYHA
I–II group (P<0.001; Fig. 2B and
C).
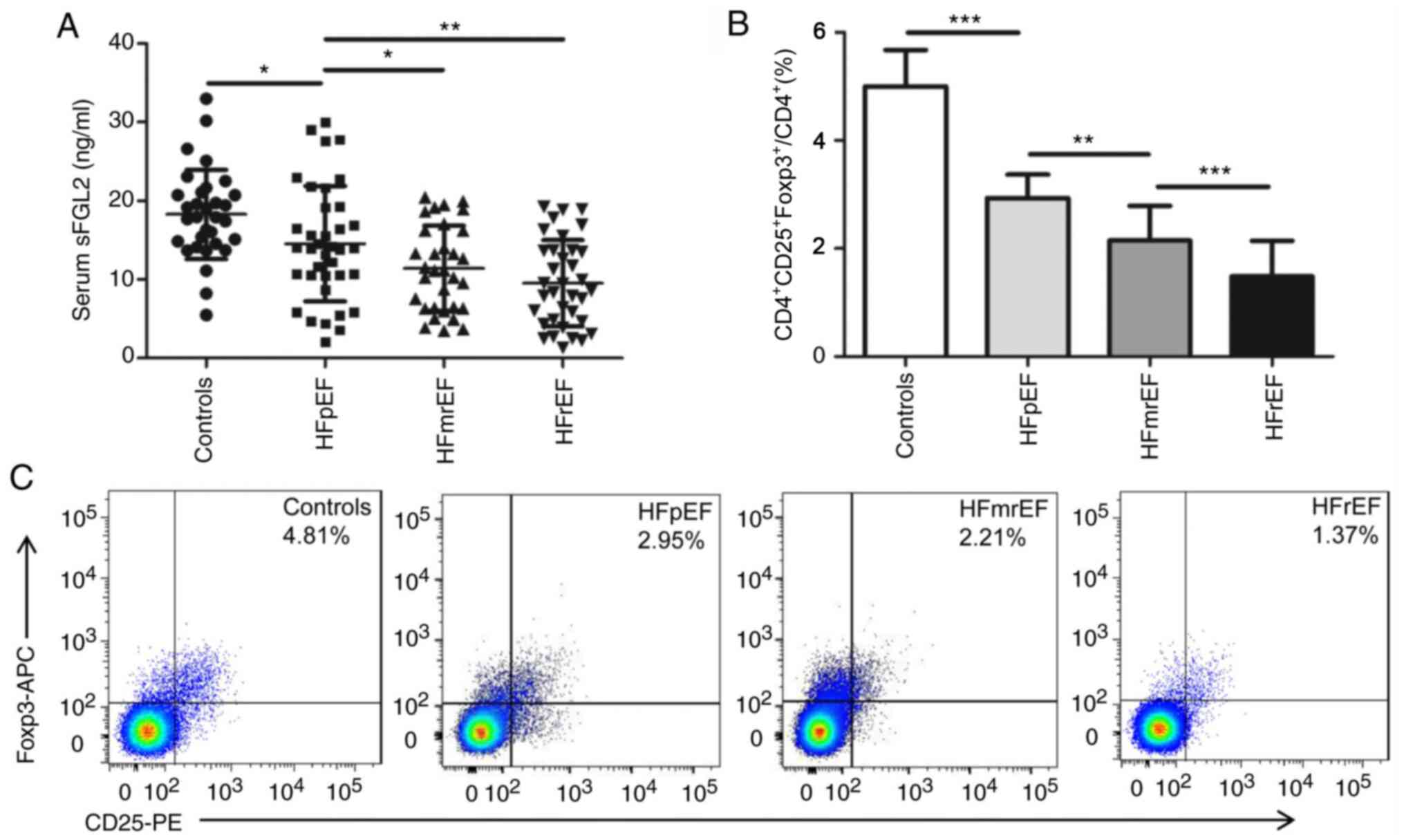
The above results implied that the reduction of
sFGL2 and Tregs was intimately associated with cardiac function. To
verify this, serum sFGL2 levels in patients with IHF with
preserved, mid-range and reduced LVEF were analyzed. Fig. 3A shows that sFGL2 levels were
prominently higher in the control group (19.18±4.24 ng/ml) than in
the HFpEF group (14.55±7.33 ng/ml, P<0.05), the HFmrEF group
(11.43±5.41 ng/ml, P<0.001) and the HFrEF group (9.53±5.48
ng/ml, P<0.001). Lower sFGL2 levels were observed in the HFmrEF
group (P<0.05) and the HFrEF group (P<0.01) compared with the
HFpEF group. However, no significant difference in sFGL2 levels
were observed between the HFmrEF and HFrEF groups. Analogously,
that the percentages of circulating
CD4+CD25+Foxp3+ Tregs were
significantly reduced in the three patient groups compared with
controls. Furthermore, in conformity to the downward trend of sFGL2
levels, the HFpEF group had significantly high Tregs frequencies,
followed by the HFmrEF group and the HFrEF group (Fig. 3B and C).
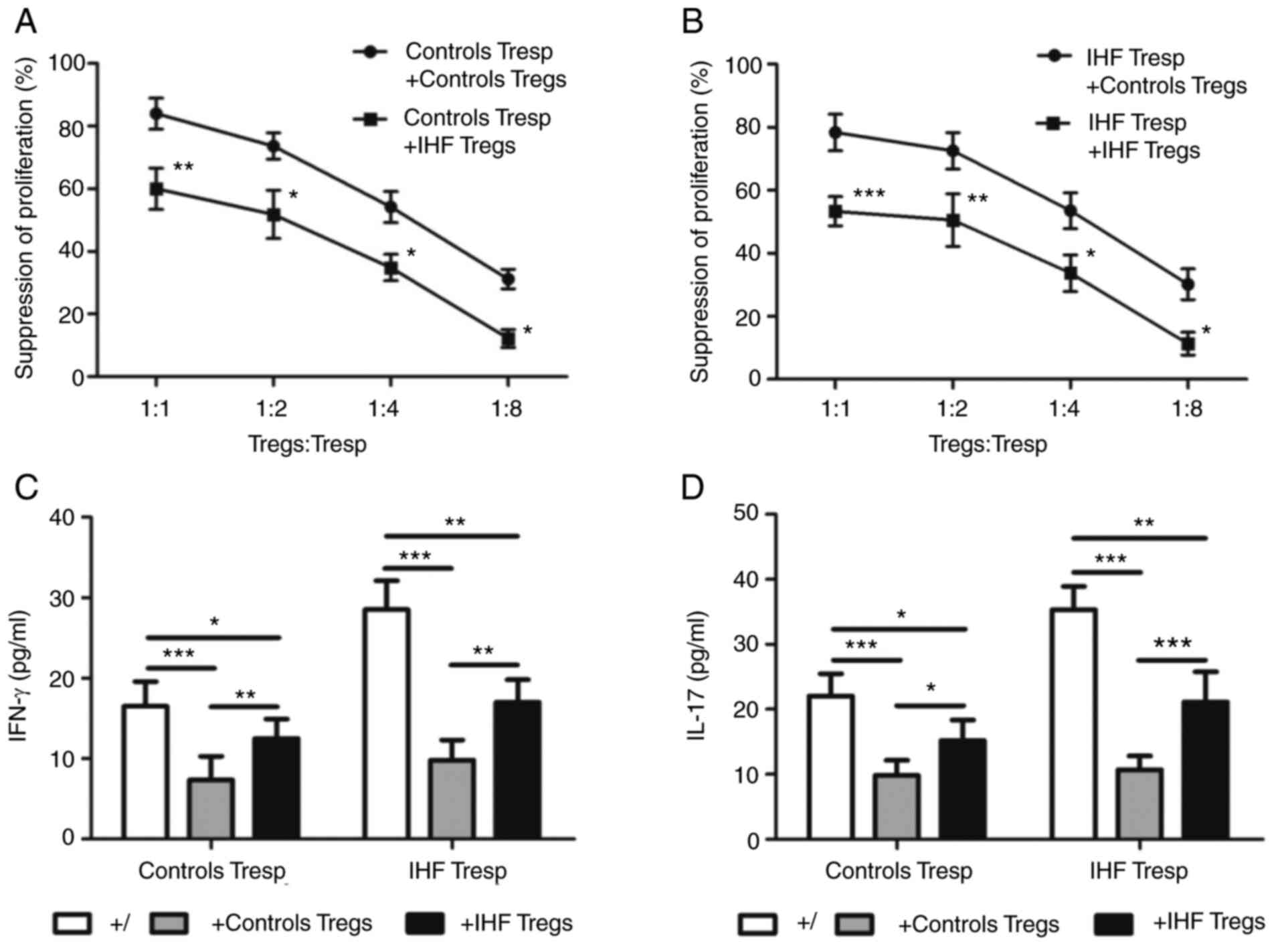
Tregs from patients with IHF present
compromised suppressive function
Quantitative analysis of the suppressive function of
Tregs was performed by co-culturing CD4+CD25+
Tregs and CFSE-labelled CD4+CD25− Tresp cells
in different ratios (1:1, 1:2, 1:4 and 1:8) stimulated by
anti-CD3/28. As seen in Fig. 4A and
B, CD4+CD25+ Tregs from the control and
IHF groups were both able to suppress the proliferation of
CD4+CD25− Tresp cells from each group.
However, compared with controls, Tregs from patients with IHF
exhibited impaired ability to suppress proliferation of Tresp cells
from the two groups. In addition, the suppressive ability of Tregs
was closely related to the ratio of Tregs to Tresp cells.
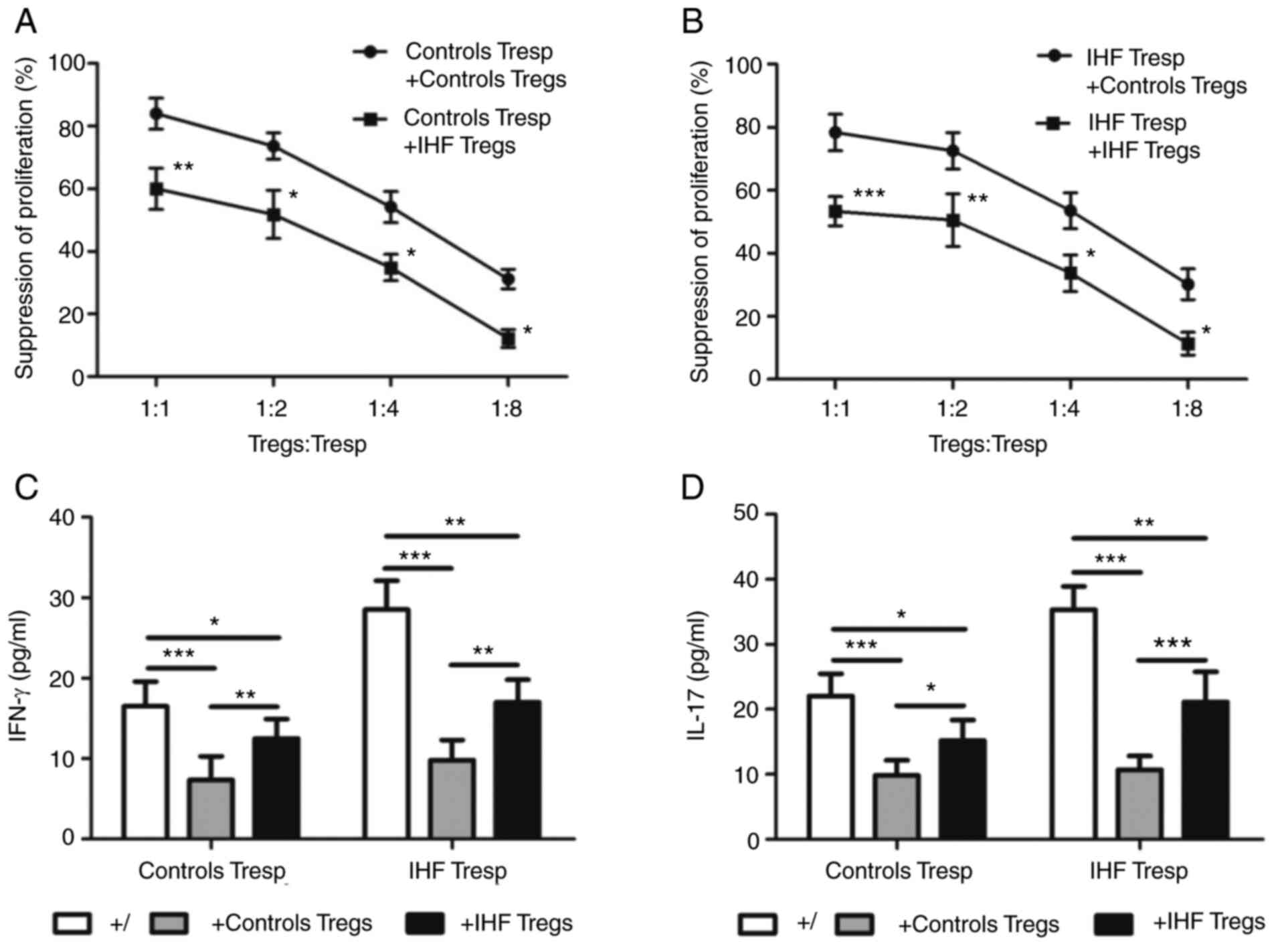 | Figure 4.Tregs from patients with IHF present
compromised suppressive function. CD4+CD25+
Tregs and CFSE-labelled CD4+CD25− T (Tresp)
cells were co-cultured at different ratio of 1:1, 1:2, 1:4 and 1:8
for proliferation and suppression assay. Then, four days later,
supernatants from the co-cultured T cells at a 1:1 ratio were
assayed for IFN-γ and IL-17 by ELISA. (A) Co-cultured with Tresp
cells from controls, Tregs from patients with IHF showed reduced
suppressive function compared with controls. (B) Co-cultured with
Tresp cells from patients with IHF, Tregs from patients with IHF
showed reduced suppressive function compared with controls. Tregs
from patients with IHF were less effective in suppressing (C) IFN-γ
and (D) IL-17 secretion compared with controls. *P<0.05,
**P<0.01, ***P<0.001. Tregs, regulatory T Cells; IHF,
ischemic heart failure; Tresp, responder T cells. |
Over-expressed pro-inflammatory cytokines such as
IFN-γ and IL-17 participate in immune imbalance in the progress of
IHF (9). Thus, the IFN-γ and IL-17
levels in the supernatants of the co-culture system were next
assessed to investigate whether Tregs were effective to suppress
IFN-γ and IL-17 production by Tresp cells. Regardless of
co-cultured with Tresp cells from controls or patients with IHF,
Tregs from patients with IHF were significantly worse at
suppressing IFN-γ and IL-17 secretion compared with controls
(Fig. 4C and D).
Correlations of serum sFGL2 levels and
circulating Tregs frequencies with the indexes of cardiac
function
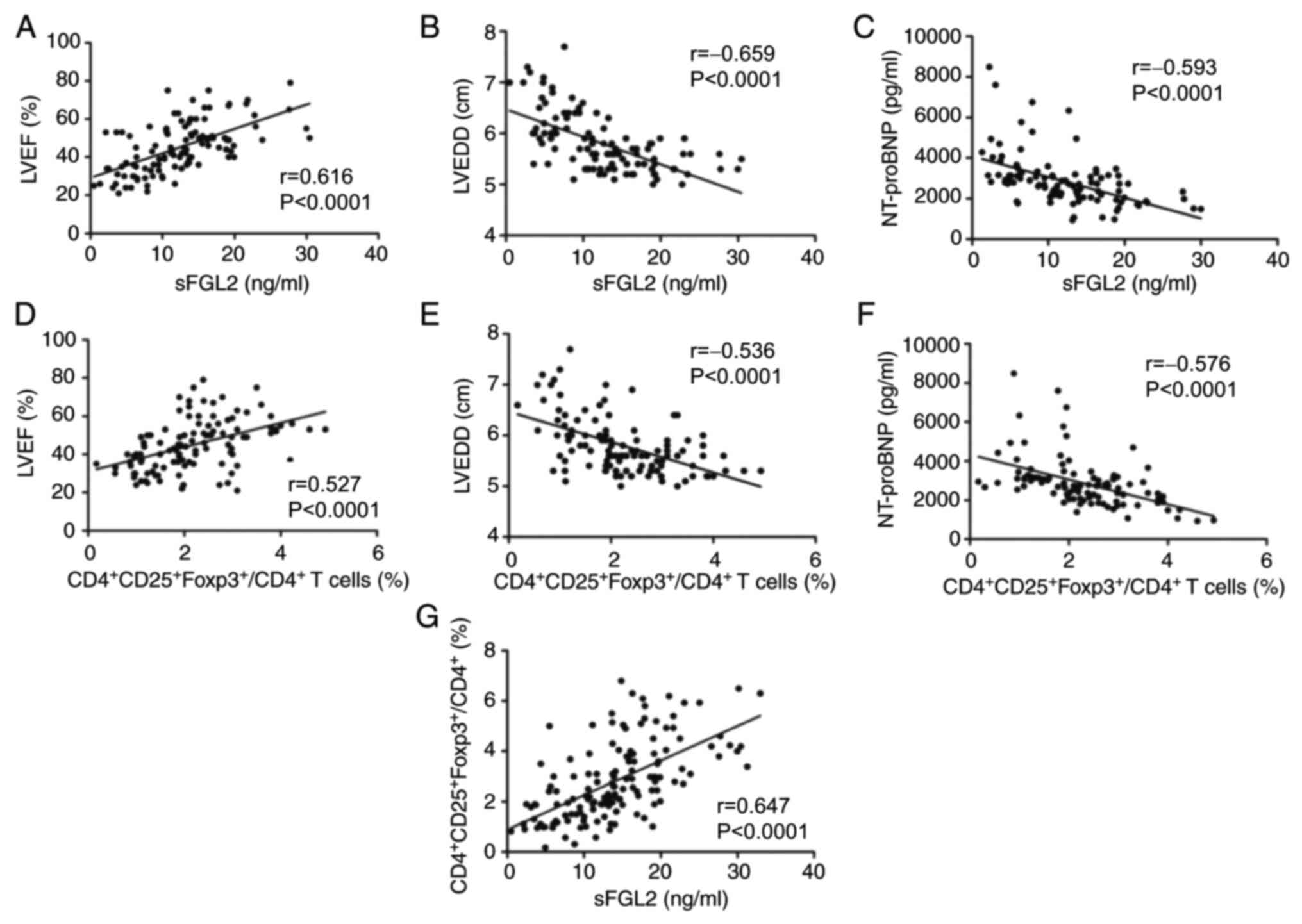
The correlations of serum sFGL2 levels and
circulating Tregs frequencies with the indexes of cardiac function
in patients with IHF was next analyzed. As shown in Fig. 5A-F, both sFGL2 levels and
CD4+CD25+Foxp3+ Tregs frequencies
were positively correlated with LVEF (r=0.616, P<0.0001 and
r=0.527, P<0.0001, respectively), whereas they were negatively
correlated with LVEDD (r=−0.659, P<0.0001 and r=−0.536,
P<0.0001, respectively) and NT-proBNP (r=−0.593, P<0.0001 and
r=−0.576, P<0.0001, respectively) in patients with IHF.
Furthermore, it was found that sFGL2 levels were significantly and
positively correlated with the frequencies of
CD4+CD25+Foxp3+ Tregs (r=0.647,
P<0.0001, Fig. 5G).
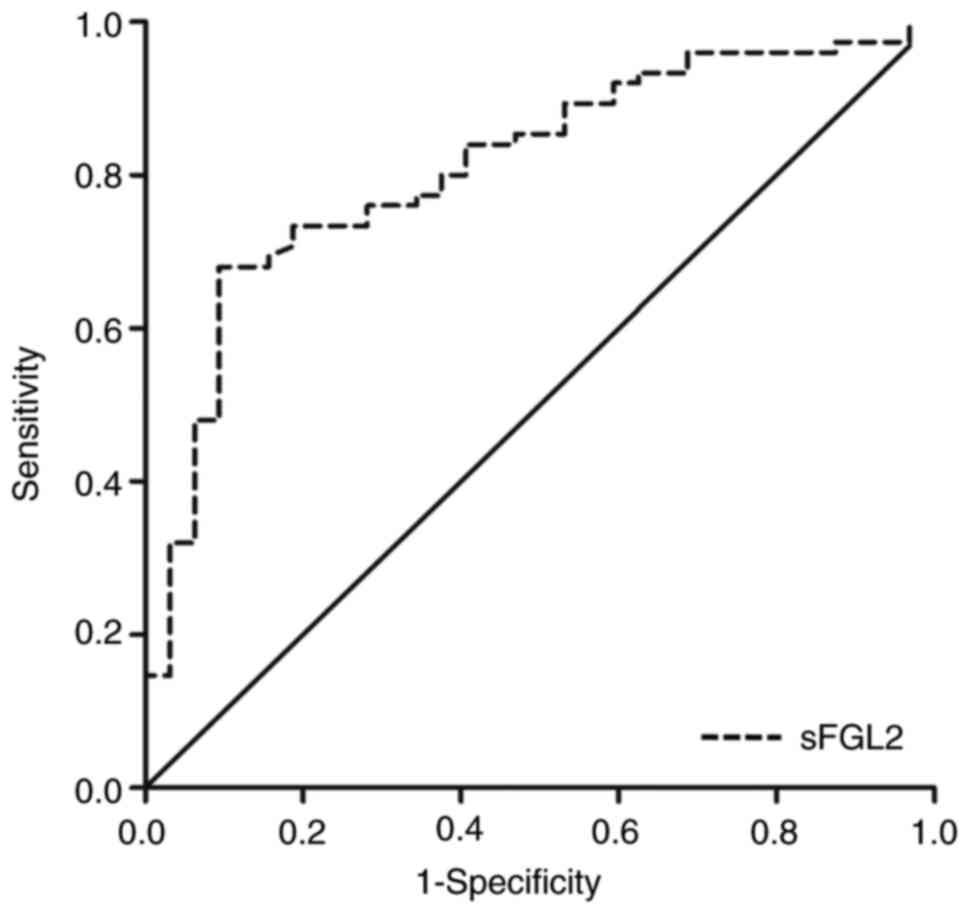
Diagnosis efficacy of serum sFGL2 for
IHF
As shown in Fig. 6,
ROC curve analysis was performed in controls and patients with IHF
to assess the diagnosis efficacy of serum sFGL2 in IHF. The area
under the curve (AUC) was 0.811 (95% confidence
interval=0.724-0.897, P<0.0001). The cut-off value for sFGL2 was
13.57 ng/ml, with a sensitivity of 68.0% and a specificity of
90.6%.
Discussion
The present study proved for the first time, to the
best of the authors' knowledge, that serum sFGL2 levels were
markedly decreased in patients with IHF, synchronically accompanied
by a pronounced reduction of circulating
CD4+CD25+Foxp3+ Tregs frequencies
and compromised Tregs suppressive function. In patients with IHF,
sFGL2 levels and Tregs frequencies were decreased with the
deterioration of cardiac function. In addition, a positive
correlation was observed between serum sFGL2 levels and LVEF and a
significant inverse correlation between serum sFGL2 levels and
LVEDD and NT-proBNP. Moreover, sFGL2 levels were significantly and
positively correlated with the frequencies of
CD4+CD25+Foxp3+ Tregs.
In this research, all patients enrolled had IHF and
had had a long course of the disease. Prior to developing heart
failure, some of them had severe coronary stenosis and/or
myocardial infarction and received revascularization. Existing
myocardial damage and inflammation eventually lead to heart failure
(3). By the time the specimens were
collected for the present study, the patients had received
revascularization long ago. The previous revascularization did not
alter or modify the cardiovascular markers, such as LVEF and
LVEDD.
With more emerging evidence, imbalance between pro-
and anti-inflammatory responses has been associated with the
pathophysiologic process of IHF (4,5,8).
Following MI injury, cell debris, reactive oxygen species and
proteases are generated immediately and attract inflammatory cells
such as neutrophils, macrophages and T cells to the infarcted
heart. These immune cells secrete large amounts of proinflammatory
cytokines and chemokines and mediate cardiac injury (8,16).
CD4+CD25+Foxp3+ Treg cells are
actively engaged in the control of a variety of physiological and
pathological immune responses (11,26).
Previous studies have shown that Tregs are increased in murines
undergoing experimental MI and recruited to the infarcted
myocardium to prevent excessive matrix degradation, limit
postinfarction inflammation and ameliorate cardiac remodeling
(27–29). As suggested by these studies, the
cardioprotective effects of Tregs may be involved in the
rebalancing of the immune system and protection against myocardial
fibrosis and AVR leading to heart failure. The role can be achieved
by suppressing T cell proliferation and modulating
monocyte/macrophage differentiation through direct interaction with
target cells and inhibitory cytokines production such as IL-10 and
TGF-β (30,31). Alternatively, clinical studies have
reported that the frequency and function of circulating Tregs were
impaired in patients with CHF and showed a significant inverse
correlation with cardiac function (9,32).
Consistent with the recent analogous researches, the present study
found that circulating Tregs frequencies were decreased in patients
with IHF, positively correlated with LVEF and negatively correlated
with LVEDD and NT-proBNP. Notably, the suppressive capacity of
Tregs on Tresp cells proliferation and pro-inflammatory cytokines
secretion was impaired in patients with IHF. This implied that the
homeostatic control of Tregs is disordered in IHF, while defective
Tregs are also correlated with the severity of disease. Given the
above, it is possible that impaired Tregs may be associated with
the immune imbalance and responsible for the uncontrolled
inflammatory response in IHF, which subsequently lead to myocardial
damage and deterioration of cardiac function.
sFGL2 is highly expressed in Tregs both at mRNA and
protein levels and it contributes to their suppressive activity
(20,23). A study on heart transplantation
documented that CD4+ T cells in fgl2 transgenic mice
exert reduced proliferative activity to alloantigen, anti-CD3 and
anti-CD28 stimulation compared with CD4+ T cells in
wild-type mice or fgl2 gene knockout mice (33). Simultaneously, the frequencies of
splenic Tregs in fgl2 transgenic mice were considerably increased
and immunosuppressive activity of Tregs in fgl2 transgenic mice was
enhanced in response to ConA stimulation (33). By contrast, sFGL2 deficiency due to
gene knockout or antibody blockade can significantly block Treg
suppressive function thus leading to immune dysregulation and
autoimmune glomerulonephritis (20). However the importance of traditional
cytokines released by Tregs such as IL-10 and TGF-β remains
controversial. Monoclonal antibodies against IL-10 or TGF-β fail to
inhibit Tregs activity and Tregs obtained from TGF-β-deficient mice
exhibit normal suppressive function (34,35).
Moreover, TGF-β and IL-10 do not decrease in patients with CHF
(10). Therefore, sFGL2 should not
only serve as an essential downstream effector of Tregs accounting
for suppressive effects other than the traditional
anti-inflammatory factors, but it should also increase the
frequency and immunosuppressive function of Tregs. Based upon the
data of the present study, sFGL2 levels were significantly
decreased in the serum of patients with IHF and positively
correlated with the frequencies of
CD4+CD25+Foxp3+ Tregs. This may be
explained by impaired Tregs that exhibit a deficient capacity to
secrete sFGL2 and subsequently by insufficient sFGL2 that
downregulates Tregs differentiation and suppressive function, thus
forming a vicious circle. sFGL2 has been demonstrated to bind
specifically to FcgRIIB and FcgRIII receptors expressed on the
surface of macrophages, dendritic cells and lymphocytes to achieve
immunosuppression (22,23). Accordingly, the notable reduction of
sFGL2 levels, accompanied by decreased Tregs frequencies and
compromised suppressive function, might serve a role in the
progression of IHF.
In fgl2 knockout mice, FGL2 deficiency leads to
significant early postnatal lethality due to acute congestive
cardiac failure, indicating that FGL2 has an important role in
normal cardiac function throughout embryonic and early postnatal
development (36). The data of the
present study showed that serum levels of sFGL2 were positively
correlated with LVEF and were negatively correlated with LVEDD and
NT-proBNP, suggesting that sFGL2 was related to the severity of
cardiac dilation and dysfunction.
Nevertheless, there are some potential limitations
to the present study. It did not calculate the mean fluorescence
intensity (MFI) as this study was carried out over a long time
span. The samples were collected and tested them in several batches
and different batches may present different MFI. In addition, the
flow cytometric labeling of Tregs showed high specificity and
prominent expression. Thus, the present study only analyzed the
proportion of Tregs. If the MFI had been assessed, the present
study would have been more rigorous. It also remains uncertain how
sFGL2 and Tregs modulate the immune balance in the progression of
IHF, resulting in alterations of cardiac function and structure. To
solve this problem, the authors of the present study are performing
an animal experiment to study the functional roles of sFGL2 and
Tregs in wound healing post-MI in a mouse model of permanent left
coronary artery ligation. The effects and mechanisms of sFGL2 and
Tregs on activation and proliferation of T cells and
differentiation of monocytes and macrophages are being investigated
using an experimental MI model of sfgl2 knockout and transgenic
mice. Further studies are needed to elucidate whether sFGL2 and
Tregs could have clinical applications in the treatment of heart
failure.
Taken together, the present study corroborated that
serum sFGL2 levels are decreased in IHF and correlated with cardiac
function, suggesting that the reduction of serum sFGL2 levels is
associated with IHF progression. As a novel downstream effector of
Tregs, sFGL2 could be a potential indicator for predicting disease
severity as well as a therapeutic target for IHF, all of which
should be confirmed by further studies.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
The present study was supported by the National
Natural Science Foundation of China (grant. nos. 81270267 and
81901429).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YY and SH contributed equally to this study. YY, KL
and ZW conceived and designed the study. YY and SH completed the
experiments. YY and SH collected blood samples. HL and CF
participated in data analysis. YY, KL and ZW wrote the manuscript.
All authors confirm the authenticity of all the raw data. All
authors read and approved the final version of the manuscript.
Ethics approval and consent to
participate
The present study was approved by the Ethics
Committee of Tongji Medical College, Huazhong University of Science
and Technology (approval. no. IORG0003571) and written informed
consent was obtained from each participant. This investigation
conformed to the Declaration of Helsinki principles.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Gerber Y, Weston SA, Enriquez-Sarano M,
Berardi C, Chamberlain AM, Manemann SM, Jiang R, Dunlay SM and
Roger VL: Mortality associated with heart failure after myocardial
infarction: A contemporary community perspective. Circ Heart Fail.
9:e0024602016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Barsheshet A, Moss AJ, Eldar M, Huang DT,
Hall WJ, Klein HU, McNitt S, Steinberg JS, Wilber DJ, Zareba W and
Goldenberg I: Time-Dependent benefit of preventive cardiac
resynchronization therapy after myocardial infarction. Eur Heart J.
32:1614–1621. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Briceno N, Schuster A, Lumley M and Perera
D: Ischaemic cardiomyopathy: Pathophysiology, assessment and the
role of revascularisation. Heart. 102:397–406. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Tang TT, Zhu YC, Dong NG, Zhang S, Cai J,
Zhang LX, Han Y, Xia N, Nie SF, Zhang M, et al: Pathologic T-cell
response in ischaemic failing hearts elucidated by T-cell receptor
sequencing and phenotypic characterization. Eur Heart J.
40:3924–3933. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Swirski FK and Nahrendorf M: Leukocyte
behavior in atherosclerosis, myocardial infarction, and heart
failure. Science. 339:161–166. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Wang Z, Huang S, Sheng Y, Peng X, Liu H,
Jin N, Cai J, Shu Y, Li T, Li P, et al: Topiramate modulates
post-infarction inflammation primarily by targeting monocytes or
macrophages. Cardiovasc Res. 113:475–487. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yan X, Anzai A, Katsumata Y, Matsuhashi T,
Ito K, Endo J, Yamamoto T, Takeshima A, Shinmura K, Shen W, et al:
Temporal dynamics of cardiac immune cell accumulation following
acute myocardial infarction. J Mol Cell Cardiol. 62:24–35. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Prabhu SD and Frangogiannis NG: The
biological basis for cardiac repair after myocardial infarction:
From inflammation to fibrosis. Circ Res. 119:91–112. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Tang TT, Ding YJ, Liao YH, Yu X, Xiao H,
Xie JJ, Yuan J, Zhou ZH, Liao MY, Yao R, et al: Defective
circulating CD4CD25+Foxp3+CD127(low) regulatory T-cells in patients
with chronic heart failure. Cell Physiol Biochem. 25:451–458. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tang TT, Zhu ZF, Wang J, Zhang WC, Tu X,
Xiao H, Du XL, Xia JH, Dong NG, Su W, et al: Impaired thymic export
and apoptosis contribute to regulatory T-cell defects in patients
with chronic heart failure. PLoS One. 6:e242722011. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Dominguez-Villar M and Hafler DA:
Regulatory T cells in autoimmune disease. Nat Immunol. 19:665–673.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhu ZF, Tang TT, Dong WY, Li YY, Xia N,
Zhang WC, Zhou SF, Yuan J, Liao MY, Li JJ, et al: Defective
circulating CD4+LAP+ regulatory T cells in patients with dilated
cardiomyopathy. J Leukoc Biol. 97:797–805. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chen XH, Ruan CC, Ge Q, Ma Y, Xu JZ, Zhang
ZB, Lin JR, Chen DR, Zhu DL and Gao PJ: Deficiency of complement
C3a and C5a receptors prevents angiotensin II-induced hypertension
via regulatory T cells. Circ Res. 122:970–983. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Meiler S, Smeets E, Winkels H, Shami A,
Pascutti MF, Nolte MA, Beckers L, Weber C, Gerdes N and Lutgens E:
Constitutive GITR activation reduces atherosclerosis by promoting
regulatory CD4+ T-cell responses-brief report. Arterioscler Thromb
Vasc Biol. 36:1748–1752. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Flego D, Severino A, Trotta F, Previtero
M, Ucci S, Zara C, Massaro G, Pedicino D, Biasucci LM, Liuzzo G and
Crea F: Increased PTPN22 expression and defective CREB activation
impair regulatory T-cell differentiation in non-ST-segment
elevation acute coronary syndromes. J Am Coll Cardiol.
65:1175–1186. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tang TT, Yuan J, Zhu ZF, Zhang WC, Xiao H,
Xia N, Yan XX, Nie SF, Liu J, Zhou SF, et al: Regulatory T cells
ameliorate cardiac remodeling after myocardial infarction. Basic
Res Cardiol. 107:2322012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Meng X, Yang J, Dong M, Zhang K, Tu E, Gao
Q, Chen W, Zhang C and Zhang Y: Regulatory T cells in
cardiovascular diseases. Nat Rev Cardiol. 13:167–179. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Long R, You Y, Li W, Jin N, Huang S, Li T,
Liu K and Wang Z: Sodium tanshinone IIA sulfonate ameliorates
experimental coronary no-reflow phenomenon through down-regulation
of FGL2. Life Sci. 142:8–18. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Li WZ, Wang J, Long R, Su GH, Bukhory DK,
Dai J, Jin N, Huang SY, Jia P, Li T, et al: Novel antibody against
a glutamic acid-rich human fibrinogen-like protein 2-derived
peptide near Ser91 inhibits hfgl2 prothrombinase activity. PLoS
One. 9:e945512014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Shalev I, Liu H, Koscik C, Bartczak A,
Javadi M, Wong KM, Maknojia A, He W, Liu MF, Diao J, et al:
Targeted deletion of fgl2 leads to impaired regulatory T cell
activity and development of autoimmune glomerulonephritis. J
Immunol. 180:249–260. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhao Z, Yang C, Wang L, Li L, Zhao T, Hu
L, Rong R, Xu M and Zhu T: The regulatory T cell effector soluble
fibrinogen-like protein 2 induces tubular epithelial cell apoptosis
in renal transplantation. Exp Biol Med (Maywood). 239:193–201.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Foerster K, Helmy A, Zhu Y, Khattar R,
Adeyi OA, Wong KM, Shalev I, Clark DA, Wong PY, Heathcote EJ, et
al: The novel immunoregulatory molecule FGL2: A potential biomarker
for severity of chronic hepatitis C virus infection. J Hepatol.
53:608–615. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Chan CW, Kay LS, Khadaroo RG, Chan MWC,
Lakatoo S, Young KJ, Zhang L, Gorczynski RM, Cattral M, Rotstein O
and Levy GA: Soluble fibrinogen-like protein 2/fibroleukin exhibits
immunosuppressive properties: Suppressing T cell proliferation and
inhibiting maturation of bone marrow-derived dendritic cells. J
Immunol. 170:4036–4044. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Liu K, Li T, Huang S, Long R, You Y, Liu J
and Wang Z: The reduced soluble fibrinogen-like protein 2 and
regulatory T cells in acute coronary syndrome. Exp Biol Med
(Maywood). 241:421–425. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ponikowski P, Voors AA, Anker SD, Bueno H,
Cleland John GF, Coats Andrew JS, Falk V, González-Juanatey JR,
Harjola VP, Jankowska EA, et al: 2016 ESC Guidelines for the
diagnosis and treatment of acute and chronic heart failure: The
task force for the diagnosis and treatment of acute and chronic
heart failure of the European Society of Cardiology (ESC).
Developed with the special contribution of the Heart Failure
Association (HFA) of the ESC. Eur J Heart Fail. 37:2129–2200. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Kasper IR, Apostolidis SA, Sharabi A and
Tsokos GC: Empowering regulatory T cells in autoimmunity. Trends
Mol Med. 22:784–797. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Sharir R, Semo J, Shimoni S, Ben-Mordechai
T, Landa-Rouben N, Maysel-Auslender S, Shaish A, Entin-Meer M,
Keren G and George J: Experimental myocardial infarction induces
altered regulatory T cell hemostasis, and adoptive transfer
attenuates subsequent remodeling. PLoS One. 9:e1136532014.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Saxena A, Dobaczewski M, Rai V, Haque Z,
Chen W, Li N and Frangogiannis NG: Regulatory T cells are recruited
in the infarcted mouse myocardium and may modulate fibroblast
phenotype and function. Am J Physiol Heart Circ Physiol.
307:H1233–H1242. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Ramjee V, Li D, Manderfield LJ, Liu F,
Engleka KA, Aghajanian H, Rodell CB, Lu W, Ho V, Wang T, et al:
Epicardial YAP/TAZ orchestrate an immunosuppressive response
following myocardial infarction. J Clin Invest. 127:899–911. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Lu L, Barbi J and Pan F: The regulation of
immune tolerance by FOXP3. Nat Rev Immunol. 17:703–717. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Weirather J, Hofmann UD, Beyersdorf N,
Ramos GC, Vogel B, Frey A, Ertl G, Kerkau T and Frantz S: Foxp3+
CD4+ T cells improve healing after myocardial infarction by
modulating monocyte/macrophage differentiation. Circ Res.
115:55–67. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Li N, Bian H, Zhang J, Li X, Ji X and
Zhang Y: The Th17/treg imbalance exists in patients with heart
failure with normal ejection fraction and heart failure with
reduced ejection fraction. Clin Chim Acta. 411:1963–1968. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Bartczak A, Chruscinski A, Mendicino M,
Liu H, Zhang J, He W, Amir AZ, Nguyen A, Khattar R, Sadozai H, et
al: Overexpression of fibrinogen-like protein 2 promotes tolerance
in a fully mismatched murine model of heart transplantation. Am J
Transplant. 16:1739–1750. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Tang Q, Boden EK, Henriksen KJ,
Bour-Jordan H, Bi M and Bluestone JA: Distinct roles of CTLA-4 and
TGF-beta in CD4+CD25+ regulatory T cell function. Eur J Immunol.
34:2996–3005. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Miyara M and Sakaguchi S: Natural
regulatory T cells: Mechanisms of suppression. Trends Mol Med.
13:108–116. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Mu J, Qu D, Bartczak A, Phillips MJ,
Manuel J, He W, Koscik C, Mendicino M, Zhang L, Clark DA, et al:
Fgl2 deficiency causes neonatal death and cardiac dysfunction
during embryonic and postnatal development in mice. Physiol
Genomics. 31:53–62. 2007. View Article : Google Scholar : PubMed/NCBI
|