Introduction
Primary Sjögren's syndrome (pSS) is a systemic
autoimmune disease characterized by the infiltration of periductal
lymph cells in the lacrimal and salivary gland tissues (1). Abnormal activation of T and B cells
is vital for the progression of pSS. T cell stimulative and
differentiative activities require two signals. The first signal
being T cell receptor recognition of the major histocompatibility
complex on antigen-presenting cells (APCs) (2); the second signal is a co-stimulatory
signal mediated by auxiliary biomolecules on APCs (3–6).
Costimulatory molecule has importance in treatment of autoimmune
disease, since manipulating co-stimulatory signals may offer a way
to reinforce or halt immune responses. B7/CD28/CTLA4 pathway has
the ability to both positively and negatively regulate immune
responses. The CD28/CTLA4/B7 pathway signaling pathway is the most
explored T cell co-stimulatory pathway and is pivotal for T cell
stimulation and tolerance (7).
Inducible T cell co-stimulator (ICOS) is a component
of the CD28 superfamily, which is predominantly expressed on the
surface of stimulated T cells (8,9).
ICOS supports CD4+ T follicular helper (Tfh) cell
differentiation and function during the germinal center (GC)
response (10–13). As such, the absence of ICOS or
ICOS ligand in humans and mice induces serious abnormalities
(14–18). It is known that ICOS is
predominantly expressed on both follicular and regulatory
follicular T helper cells (Tfh and Tfr cells) which regulate
antagonistically the quantity and quality of humoral immunity
(19,20). The expression of ICOS lead to
dysfunction of T-cell in SLE patients (21) Researcher first focused on T cells
and evaluated the key activation molecules, HLA-DR, and
costimulatory molecules such as ICOS on CD3+ T cells (22). The ICOS expression in SLE was
correlated to the anti-DNA antibodies. Enhanced expression of
ICOS-expressing CD3+ T cells may suggest that the systemic lupus
erythematosus (SLE) patients are at a more severe inflammatory
status (22). Previous studies
have reported increased ICOS protein and mRNA expression levels in
the peripheral blood of patients with pSS (23,24). The present study found that the
expression of ICOS was shown to affect saliva weight and aquaporin
5 (AQP5) expression; however, the specific downstream signal
transduction constituents involved remain unknown.
Previous studies indicate that ICOS is pivotal for
stimulating the PI3K/Akt/mTOR signaling pathway (25,26), which is also found to be
associated with inflammatory activation (27). Sicca symptoms, including dry eyes
and mouth, are characteristic features of pSS. AQP5 affects saliva
secretion; it is distributed in the salivary gland tissues and
functions as a water channel in the secretory glands (28). The expression mechanism of
co-stimulatory molecules and their receptors in pSS is still
unclear, and further research is needed. It was hypothesized that
the expression level and equilibrium of ICOS, as well as relevant
expression of AQP5, may markedly affect the sicca symptoms
identified in pSS. Thus, the present study aimed to explore whether
ICOS affected AQP5 expression by promoting salivary gland
inflammation and to offer a prospective candidate for pSS
diagnosis.
Materials and methods
Dataset access and information
The Gene Expression Omnibus (GEO; http://www.ncbi.nlm.nih.gov/gds) datasets
GSE40611 and GSE84844 were used. These datasets came from the
GPL570 (HG-U133_Plus_2) Affymetrix Human Genome U133 Plus 2.0 Array
and were analyzed by R packages (http://www.R-project.org/). GSE40611 comprises 17
healthy salivary gland samples and 18 pSS salivary gland samples;
GSE84844 contains 30 normal whole blood samples and 30 pSS whole
blood. The Perl command ‘strawberry-perl-5.32.1.1-64bit’
(strawberryperl.com/releases.html) was used to transform the
genetic probe IDs in the matrix files into the genetic symbols in
the dataset files to acquire a matrix file of formal symbols. All
datasets were normalized using the limma R package (version 4.1.0
for Windows, R Core Team, Vienna, Austria http://www.R-project.org/) (29). The genetic expression information
was log2 transformed.
Dataset analyses
The Perl (strawberry-perl-5.32.1.1-64bit) command is
used to convert the genetic probe IDs in the matrix document to the
genetic symbols of the platform to obtain the matrix document
containing the official symbols (https://strawberryperl.com/releases.html strawberry
perl.com project).
The pSS expression datasets were standardized by
impute R package and limma R package (R for Windows 4.1.0 Setup and
http://www.rstudio.com). Differentially expressed
genes (DEGs) between patients and healthy individuals were
identified by volcano plot (−https://www.rstudio.com) using the limma R package.
All P-value (false discovery rate) <0.05) and |log2 (FC)|
>0.75 were considered to indicate a statistically significant
difference by comparing pSS with healthy controls using the limma R
package.
Functional enrichment analyses
Gene Ontology (GO) and Kyoto Encyclopedia of Genes
and Genomes (KEGG) analyses were completed based on the GEO
database (30–32). The outcomes of the R analyses were
submitted to determine the putative underlying roles of the
selected genes. False discovery rate <0.05 and P<0.05 were
considered to indicate a statistically significant difference.
Protein-protein interaction (PPI)
network establishment
The identified DEGs were uploaded to the Search Tool
for the Retrieval of Interacting Genes/Proteins (STRING) database
(https://string-db.org) (33). The interaction score was set to
0.8. The hub genes were identified and Cytoscape
(Cytoscape_3_8_2_windows_64bit; http://cytoscape.org/download.html) was used to plot
the network diagram; nodal points denoted a gene or protein
(34); the number of edges
between nodal points denoted the molecular interplay.
Patients
A total of 95 patients with pSS and 68 healthy
individuals admitted to Affiliated Hospital of Nantong University
between September 2017 and September 2018 who met the inclusion
criteria (as described below) were selected by the random number
table method. The patients with pSS were diagnosed according to the
2016 American-European Consensus Group SS categorization standards
(35). Salivary gland biopsy
samples were harvested, and the pathological status of 95 pSS
patients was evaluated to determine the pathological findings.
Donors bearing inflammatory diseases, cancer or contagious diseases
were excluded from the study. The study was approved by the ethical
board of Affiliated Hospital of Nantong University (Jiangsu, China;
approval no. 2017-K003). All patients were >18 years old and
provided written informed consent. Features of healthy individuals
and pSS patients are given in Table
I.
 | Table I.Clinicopathological characteristics
of healthy control individuals and patients with pSS. |
Table I.
Clinicopathological characteristics
of healthy control individuals and patients with pSS.
| Clinicopathological
characteristic | Patients with
pSS | Healthy control
patients | P-value |
|---|
| Cases, n | 95 | 68 |
|
| Sex, Female | 95 (100%) | 68 (100%) |
|
| Age,
yearsa | 48.82±1.33 | 47.31±1.425 | 0.4472 |
| Disease duration
(years)a | 1.54±0.221 | 0 | NA |
| ESSDAIc | 4 (0–7) | 0 (0–2) | <0.001 |
| Number of
cariesc | 4 (1–8) | 0 | NA |
| Autoantibody
positivity: |
|
|
|
|
Anti-SSA and/or
anti-SSBb | 95 (100) | 0 (0) | NA |
|
Rheumatoid factorb |
|
| <0.001 |
|
≤20 | 31 (33%) | 68 (100%) |
|
|
≥20 | 64 (67%) | 0 (0%) |
|
Inclusion and exclusion criteria of
patients with pSS
The inclusion criteria were as follows: Diagnosis of
pSS, >18 years old, no known cognitive defects and of Chinese
nationality. The exclusion criteria included: Secondary Sjögren's
syndrome, physiopsychological problems (psychiatric disorders) that
may affect the results, pulmonary injury not associated with pSS
(such as lung infections, asthmatic disease, persistent obstructive
lung illness, lung tuberculosis, bronchodilation and pulmonary
carcinoma), interstitial lung disease induced by organic matter or
pneumoconiosis, long-term utilization of medicines causing lung
fibrosis, and persistent cardiac, hepatic or renal function
disorders.
Disease activity
Disease activity was assessed by the European League
Against Rheumatism Sjögren's Syndrome Disease Activity Index
(ESSDAI) (36). The ESSDAI
includes measures systematic activity and 12 domains. Each domain
is divided into 3–4 levels (0, no activity; 1, low activity; 2,
moderate activity; 3, high activity). According to the ESSDAI, low
activity, <5; moderate activity, 5–13; and high activity, >13
(37).
Healthy individuals' inclusion
criteria
The inclusion criteria were as follows: >18 years
old, no known cognitive defects, not known any disease and of
Chinese nationality.
Saliva collection
Patients were not allowed to stimulate the salivary
flow. Patients were asked to hold the tongue against the roof of
the mouth (the palate) until there was adequate saliva. Salivary
samples were pooled and harvested in specimen cups for 300 sec.
Between 9:00 and 12:00 a.m., salivary sample harvesting was
completed to decrease the impact of circadian fluctuation. The
salivary specimens were centrifuged at 4,500 × g for 5 min at 4°C
and the debris and cells were discarded (38). After centrifugation, the weight of
the saliva was measured. Specimens were stored at −80°C until
subsequent analyses.
Blood collection
Blood from 95 pSS patient and 68 controls was
collected at 9–12 a.m. The patients did not have strenuous exercise
and fasting state. Peripheral blood (5 ml) was collected from each
patient and controls in the Rheumatic Immunology Department. Blood
samples were centrifuged at 978 × g for 1 min at 4°C. The uppermost
transparent liquid is extracted and stored at −80°C. All patients
and controls signed informed consent.
ELlSA
A human ICOS ELISA kit (XG-K3005; Suzhou Bright
Scistar Biotechnology Company Ltd.) was utilized to quantify the
ICOS content in saliva and in blood. A human TNF-α ELISA kit (cat.
no. DTA00D; R&D Systems, Inc.) was used to measure the levels
of TNF-α, according to the manufacturer's instructions. 100 µl
blood and 100 µl saliva from 95 pSS patients and 68 controls were
incubated in 96-well plates at 37°C for 60 min. Subsequently, the
absorbance was measured in a microplate reading device at 450 nm.
All experiments were performed in triplicate.
Immunofluorescence analyses
Salivary gland samples were fixed in 4%
paraformaldehyde at 4°C for 180 min, followed by incubation at 4°C
for 12 h in 30% sucrose. Next, the specimens were placed in optimal
cutting temperature compound and sectioned into 5-µm slices. The
salivary gland samples were blocked with 0.1% BSA (cat. no. A8010;
Beijing Solarbio Science & Technology Co., Ltd.) at 37°C for 60
min and then incubated with antibodies against ICOS (cat. no.
ab175401; Abcam; 1:100) at 4°C for 12 h. Subsequently, the sections
were incubated with goat anti-rabbit IgG antibody (H+L; cat. no.
BA-5000-1.5; Vector Laboratories, Inc.; 1:1,000) for 30 min at room
temperature. Staining was developed with red fluorescent dyes (cat.
no. FP1494001KT; PerkinElmer, Inc.; 1:3,000) for 10 min at room
temperature and DAPI (cat. no. C0065; Beijing Solarbio Science
& Technology Co., Ltd.) for 5 min at room temperature. After
all incubation steps, the samples were washed with PBS for 5 min.
An Olympus BX53 fluorescence microscope (Olympus Corporation) was
used to detect the fluorescence expression of samples. Images were
analyzed using Cellsens Standard version 1.9 software (Olympus
Corporation).
Western blot analysis
Salivary gland tissues were lysed in RIPA lysis
buffer (Beyotime Institute of Biotechnology) containing PMSF
(Beyotime Institute of Biotechnology). Protein concentrations were
determined by BCA assay (Beyotime Institute of Biotechnology). A
total of 5 µg protein samples were separated by 10% SDS-PAGE and
then transferred to PVDF membranes (Beyotime Institute of
Biotechnology). The membranes were blocked with 5% BSA (cat. no.
SW3015; Beijing Solarbio Science & Technology Co., Ltd) for 1 h
at room temperature and then incubated with the following primary
antibodies at 4°C for 12 h: anti-ICOS (cat. no. ab224644; Abcam;
1:1,000), anti-AQP5 (cat. no. ab191061; Abcam; 1:1,000),
anti-phosphorylated (p)-PI3K (cat. no. ab278545; Abcam; 1:1,000),
anti-p-AKT (cat. no. ab8933; Abcam; 1;1000), anti-p-mTOR (cat. no.
ab109268; Abcam; 1:1,000), PI3K (cat. no. ab32089; Abcam, 1:1,000),
AKT (cat. no. ab8805; Abcam; 1:1,000), mTOR (cat. no. ab134903;
Abcam; 1:1,000), anti-Bcl-2 (cat. no. ab59348; Abcam; 1:1,000) and
anti-TNF-α (cat. no. ab183218; Abcam; 1:1,000). GAPDH (cat. no.
ab8245, Abcam, 1:1000) was used as an internal control for
normalization. Rabbit anti-mouse or goat anti-rabbit IgG H&L at
37°C for 60 min (cat. nos. ab6728 and ab6721, respectively; Abcam,
1:5,000). Proteins were visualized using an Enhanced ECL
Chemiluminescence Detection kit (cat. no. E411-03; Vazyme Biotech
Co., Ltd.). Densitometric analysis was conducted using Image Lab
System version 6.1 (Bio-Rad Laboratories, Inc.). The assays were
repeated at least times.
Statistical analysis
An independent samples t-test was conducted to
determine differences between two groups. χ2 test was
used to assess differences in proportion. SPSS 19.0 software (IBM
Corp.) was used for statistical analysis. All experiments were
performed in triplicate. Shapiro-Wilk test was utilized to assess
the normal distribution of the data. Spearman correlation analysis
to determine relationships between variables. Comparisons were made
using one-way ANOVA followed by Tukey's honestly significant
difference post hoc test. Data are expressed as mean ± SEM.
χ2 test was used to assess the differences in
proportion. Median (interquartile range), analyzed by the
Mann-Whitney U test. P<0.05 was considered to indicate a
statistically significant difference.
Results
Identification of DEGs in patients
with pSS
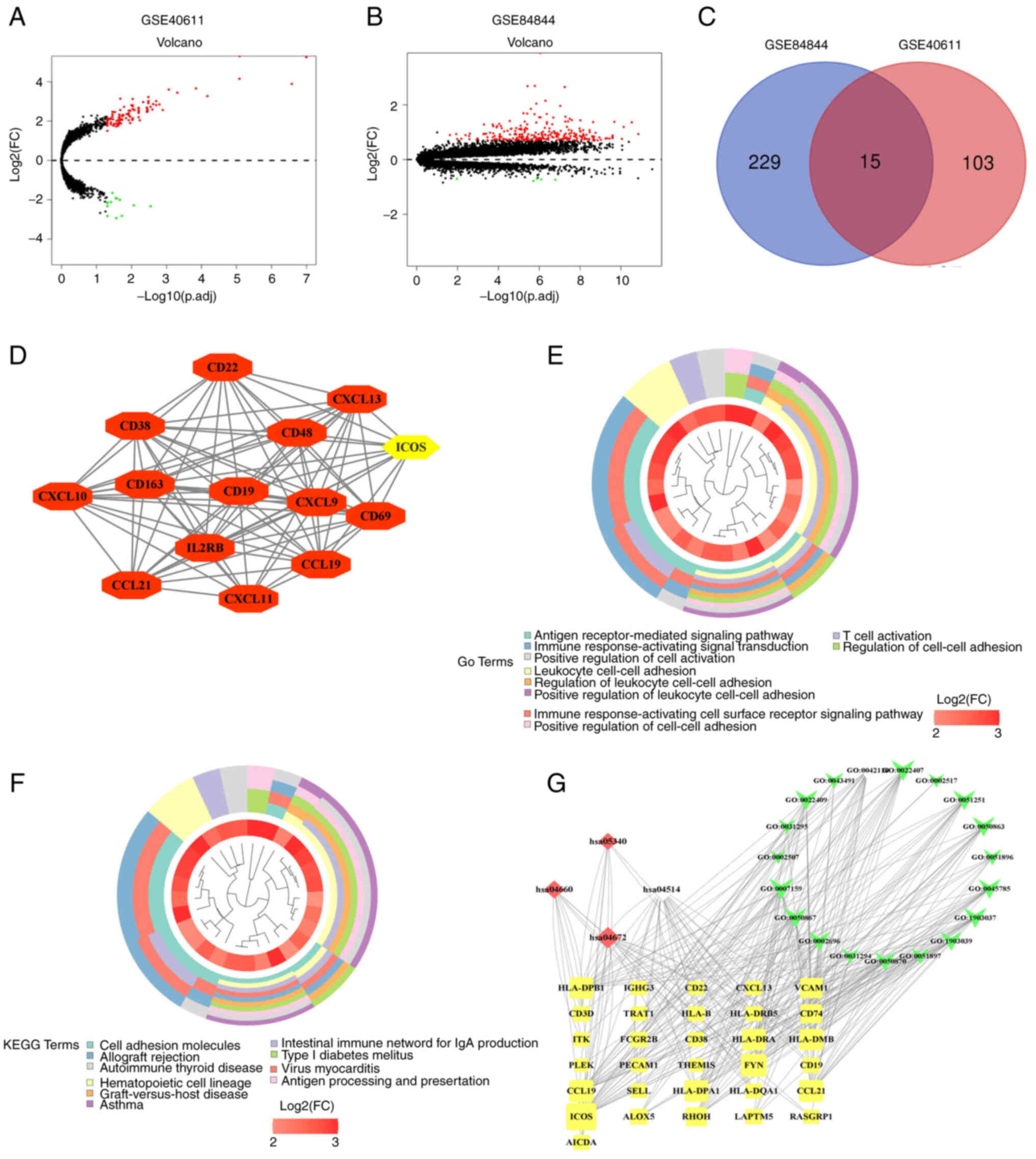
GSE40611 genetic expression matrix and corresponding
annotated files were acquired from GEO database. The dataset, which
included 17 healthy salivary gland and 18 pSS salivary gland was
analyzed using the GPL570 Affymetrix Human Genome U133 Plus 2.0
Array. A total of 118 DEGs genes were identified as consistently
differentially expressed in pSS, and these are represented using
volcano plots (Fig. 1A). Among
these, 13 were downregulated and 105 were upregulated. GSE84844
genetic expression matrix and corresponding annotated files were
acquired from GEO database. GSE84844 microarray included 30 healthy
blood and 30 pSS blood was analyzed using the GPL570 Affymetrix
Human Genome U133 Plus 2.0 Array. Similarly, DEGs were identified
using volcano plots of the Differentially expressed mRNAs were
analyzed in whole blood (GSE84844) (Fig. 1B). Here, a total of 244 genes were
identified that were consistently differentially expressed in pSS
compared with the control group data. Among these, 5 were
downregulated and 239 were upregulated. The GSE40611 and GSE84844
data were merged to establish an intersection of DEGs and 15
overlapping DEGs were found (Fig.
1C), including CXCL10, OAS3, MX1, MS4A1, GZMA, ICOS, CENPK,
TCL1A, EVI2A, IFI44L, IFIT1, CD69, FAM26F, CKS2 and TRAT1. Among
these, 0 were downregulated and 15 were upregulated.
The STRING database was used for PPI network
analysis of these DEGs, and Cytoscape software was utilized to
visualize the outcomes of the GSE40611 database (Fig. 1D). In the PPI analyses, the
association between nodal points was analyzed to determine the
interactions between the proteins encoded by DEGs in patients with
pSS. According to the PPI results, 14 immune-related genes were
found, including CD22, CD38, CXCL10, CD163, CXCL13, CD48, CD19,
IL2RB, CCL21, CXCL9, ICOS, CD69, CCL19, CXCL11. Based on the PPI
results and 15 overlapping DEGs, co-expressed genes CXCL10, CD69
and ICOS were identified. A previous study reported that the
expression of ICOS is associated with EULAR primary Sjögren's
syndrome disease activity (ESSDAI) score and gradation of focus
scoring, indicating that ICOS may be associated with the severity
of pSS (23). A modification
based on focus score (FS) calculation was proposed in 1974
(39) and further work
established FS ≥1 (i.e., ≥1 focus per 4 mm2) for use in
classification criteria (40–44). Therefore, ICOS was identified as a
core gene for further research.
The 105 upregulated genes were uploaded for GO term
and KEGG pathway enrichment analyses. In the GO analysis, the
biological process (BP) term in which ICOS participated in were
selected (Fig. 1E). The results
revealed that ‘leukocyte cell-cell adhesion’ (GO:0007159;
P=2.20×10−10) was the most significant for BP, followed
by ‘T cell activation’ (GO:0042110; P=1.19×10−9),
‘regulation of leukocyte cell-cell adhesion’ (GO:1903037;
P=4.75×10−9), ‘positive regulation of cell-cell
adhesion’ (GO:0022409; P=5.03×10−9), ‘positive
regulation of leukocyte cell-cell adhesion’ (GO:1903039;
P=7.89×10−9), ‘regulation of cell-cell adhesion’
(GO:0022407; P=2.21×10−8), ‘positive regulation of T
cell activation’ (GO:0050870; P=3.05×10−8), ‘regulation
of T cell activation’ (GO:0050863; P=3.77×10−8),
‘positive regulation of cell activation’ (GO:0050867;
P=7.69×10−8) and ‘positive regulation of lymphocyte
activation’ (GO:0051251; P=1.02×10−7).
In addition, KEGG analysis revealed that ‘cell
adhesion molecules’ (hsa04514; P=3.25×10−9), ‘intestinal
immune network for IgA production’ (hsa04672;
P=6.00×10−9), ‘primary immunodeficiency’ (hsa05340;
P=0.000280497) and ‘T cell receptor signaling pathway’ (hsa04660;
P=0.001814358) were shown. (Fig.
1F).
Biological annotation of the DEGs in patients with
pSS identified from the integrated analysis of the microarray data
was performed using Cytoscape. BP functional enrichment GO terms
(GO:0007159 leukocyte cell-cell adhesion; GO:0042110 T cell
activation; GO:1903037 regulation of leukocyte cell-cell adhesion;
GO:0022409 positive regulation of cell-cell adhesion; GO:1903039
positive regulation of leukocyte cell-cell adhesion; GO:0022407
regulation of cell-cell adhesion; GO:0050870 positive regulation of
T cell activation; GO:0050863 regulation of T cell activation;
GO:0050867 positive regulation of cell activation; GO:0051251
positive regulation of lymphocyte activation), KEGG pathways
(hsa04514 cell adhesion molecules; hsa04672 intestinal immune
network for IgA production; hsa05340 primary immunodeficiency;
hsa04660 T cell receptor signaling pathway) and DEGs (HLA-DPB1,
IGHG3, CD22, CXCL13, VCAM1, CD3D, TRAT1, HLA-B, HLA-DRB5, CD74,
ITK, FCGR2B, CD38, HLA-DRA, HLA-DMB, PLEK, PECAM1, THEMIS, FYN,
CD19, CCL19, SELL, HLA-DPA1, HLA-DQA1, CCL21, ICOS, ALQX5, RHOH,
LAPTM5, RASGRP1, AICDA.) with P<0.05 involving ICOS
participation were obtained (Fig.
1G).
Features of healthy individuals and
patients with pSS
To verify the role of ICOS, saliva, salivary gland
and whole blood were collected from 95 patients with pSS and 68
healthy individuals. There was no statistically significant
difference in the age (P=0.4472). In order to avoid gender
differences, all female patients were selected as both the pSS
patients and the healthy individuals. Compared with that of healthy
individuals, the positive rate of anti-Sjogren's syndrome A
antibody (anti-SSA) and/or anti-Sjogren's syndrome B antibody
(anti-SSB) was higher. The number of caries diagnosed by two
dentists and the amount of dental caries in patients with pSS was
greater. In addition, compared with that of healthy individuals,
the ESSDAI and rheumatoid factor was higher in pSS patients
(Table I)
ICOS expression in salivary glands,
whole blood and saliva of healthy individuals and patients with
pSS
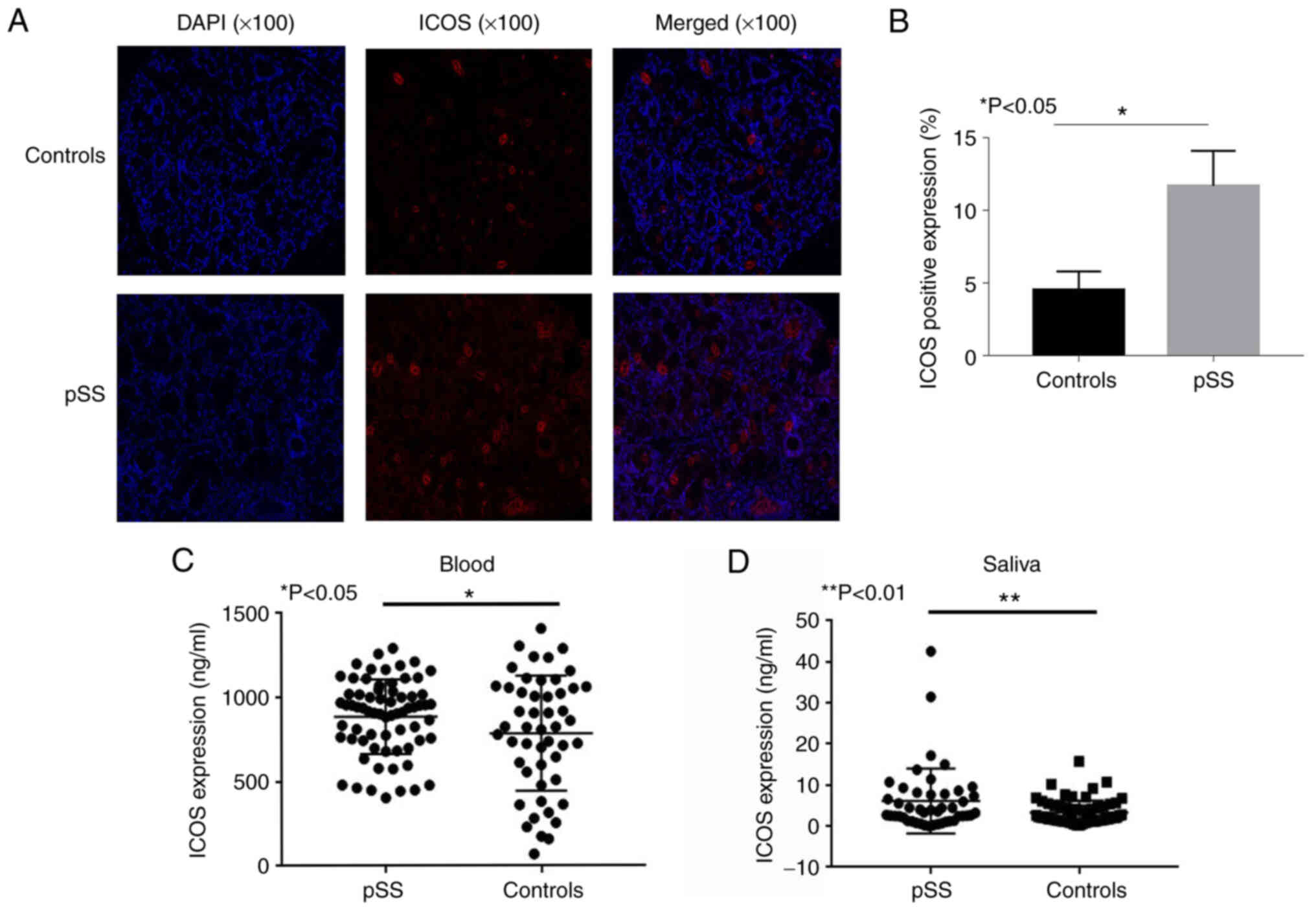
Immunofluorescence analysis of salivary gland
samples from patients with pSS revealed that these samples
displayed a higher expression level of ICOS compared with that of
controls (Fig. 2A and B). The
positive ratio of ICOS in the salivary gland tissues of controls
and pSS patients was 3.76 and 14.4%, respectively (P<0.05).
Compared with that of healthy individuals, the levels of ICOS in
peripheral blood (P<0.05; Fig.
2C) and salivary samples (P<0.01; Fig. 2D) were increased in patients with
pSS, as determined by ELISA.
ICOS expression affects the expression
of AQP5
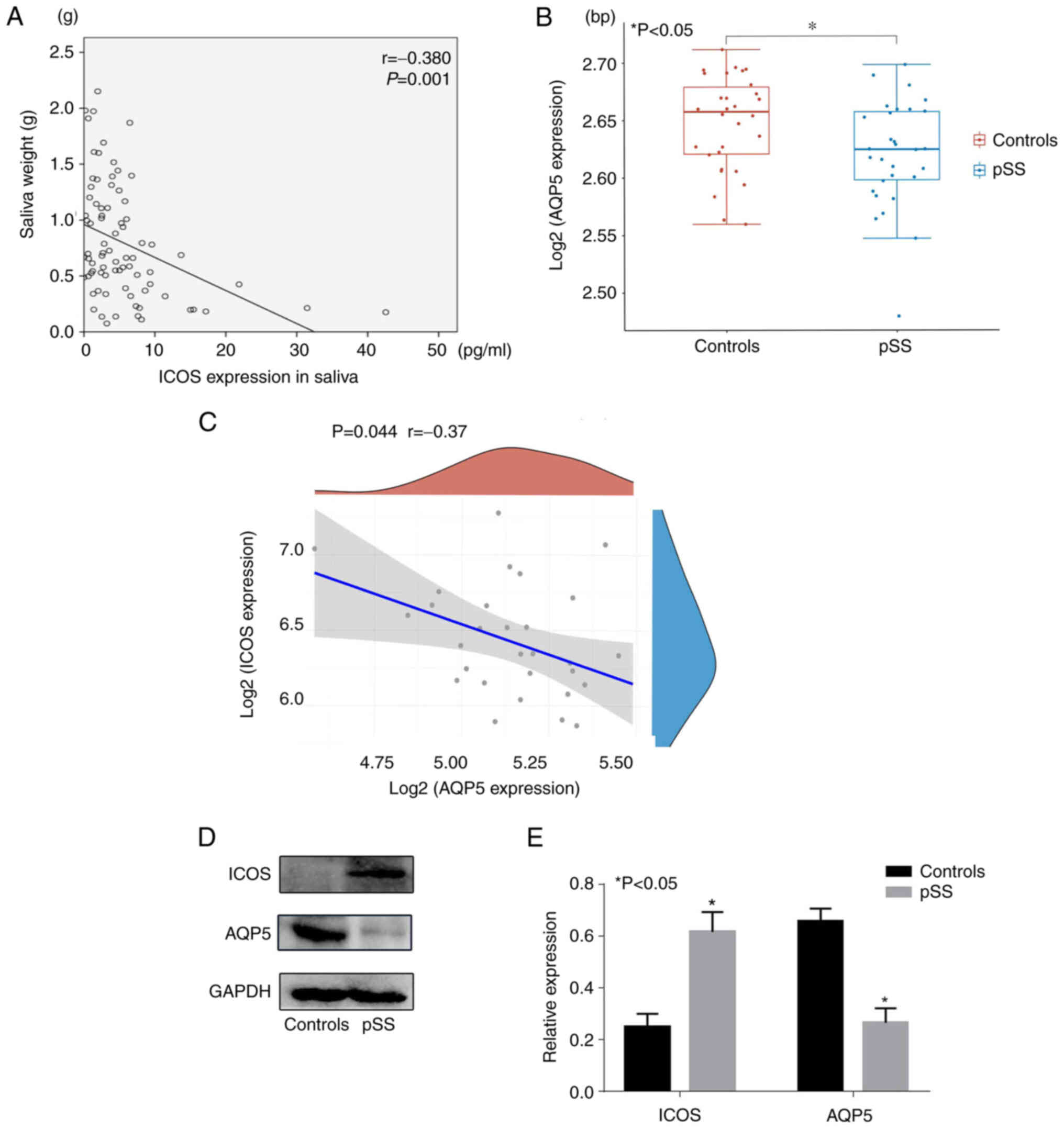
Saliva was collected from patients with pSS and
controls. Salivary weight was negatively associated with the
expression of ICOS in patients with pSS (r=−0.380; P=0.001;
Fig. 3A). The GSE84844 dataset
comprises 30 normal and 30 pSS whole blood samples. Compared with
those in healthy individuals, the levels of AQP5 in salivary gland
tissues were lower in patients with pSS (P<0.05; Fig. 3B) in GSE84844. According to the
data, AQP5 was negatively correlated with the expression of ICOS in
patients with pSS (r=−0.37; P=0.044 Fig. 3C). The salivary gland tissues of
95 patients and 68 healthy individuals were harvested and used for
western blot analysis. The results demonstrated that the expression
of AQP5 in patients with pSS was significantly lower compared with
that in healthy individuals (P<0.05; Fig. 3D and E), whereas the expression of
ICOS in patients with pSS was significantly higher compared with
that in healthy individuals (P<0.05). Based on these results, it
was hypothesized that the expression of ICOS may affect the
expression of AQP5 and thus the secretion of saliva.
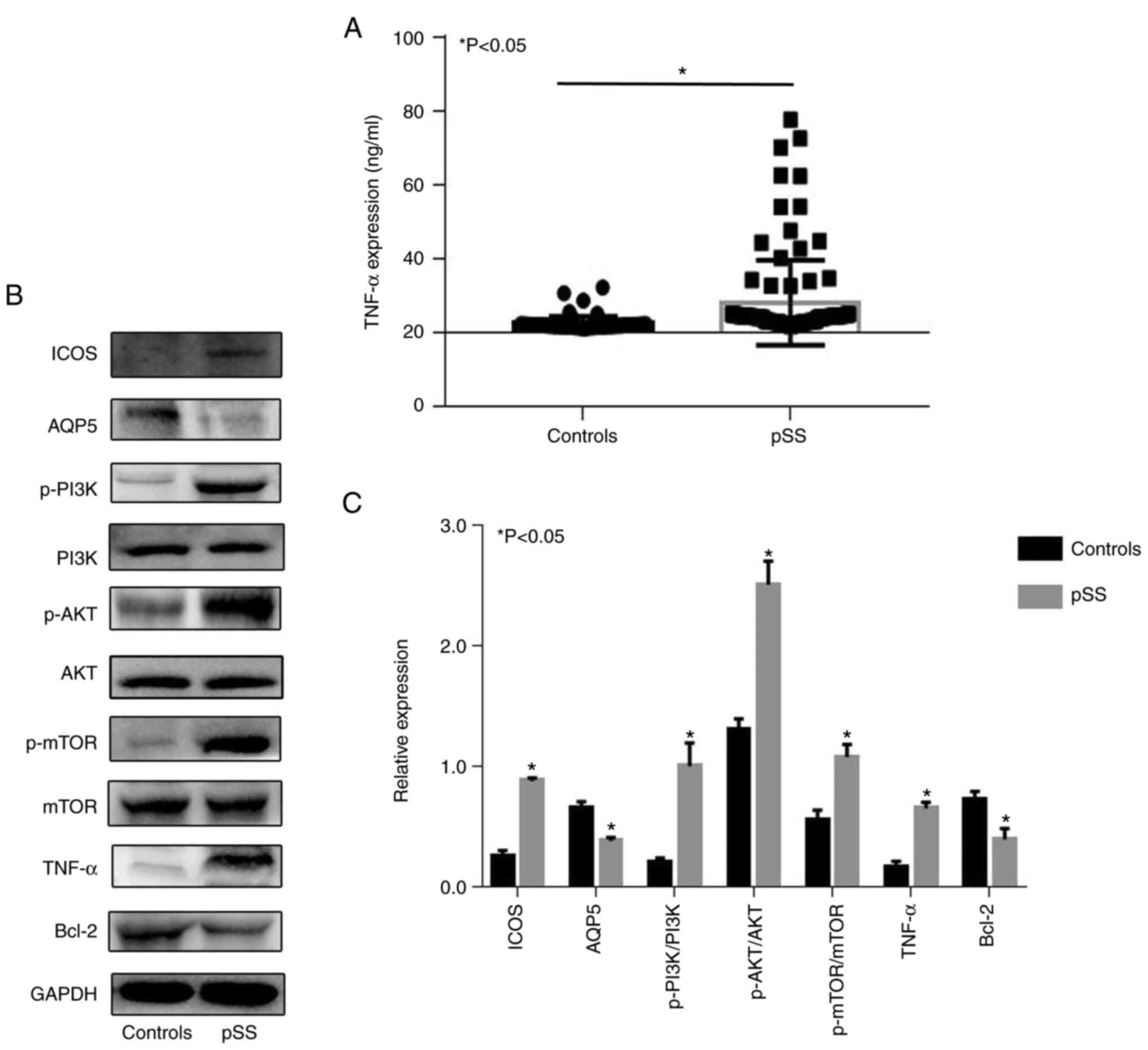
Relative protein expression in pSS
patients
A previous study reported that ICOS signaling can
affect the expression of inflammatory cytokine through the
PI3K-Akt-mTOR pathway. ICOS signaling appears to be critical for Ab
production, but its role in the maintenance phase may involve
inflammatory cytokines such as TNF-α (44). To investigate a putative
association between the PI3K/AKT/mTOR signaling pathway and the
expression of relative protein in pSS patients the expressions of
ICOS, AQP5, p-PI3K, p-AKT, p-mTOR, TNF-α and Bcl-2 were determined.
Compared with those of healthy individuals, the levels of TNF-α in
serum were elevated in patients with pSS, as determined by ELISA
(P<0.05; Fig. 4A). Western
blotting analysis showed that p-PI3K/PI3k, p-AKT/AKT, p-mTOR/mTOR
ratios, as well as TNF-α protein expression level were
significantly increased, whereas the expression of Bcl-2 and AQP5
were significantly decreased in patients with pSS (all P<0.05;
Fig. 4B and C).
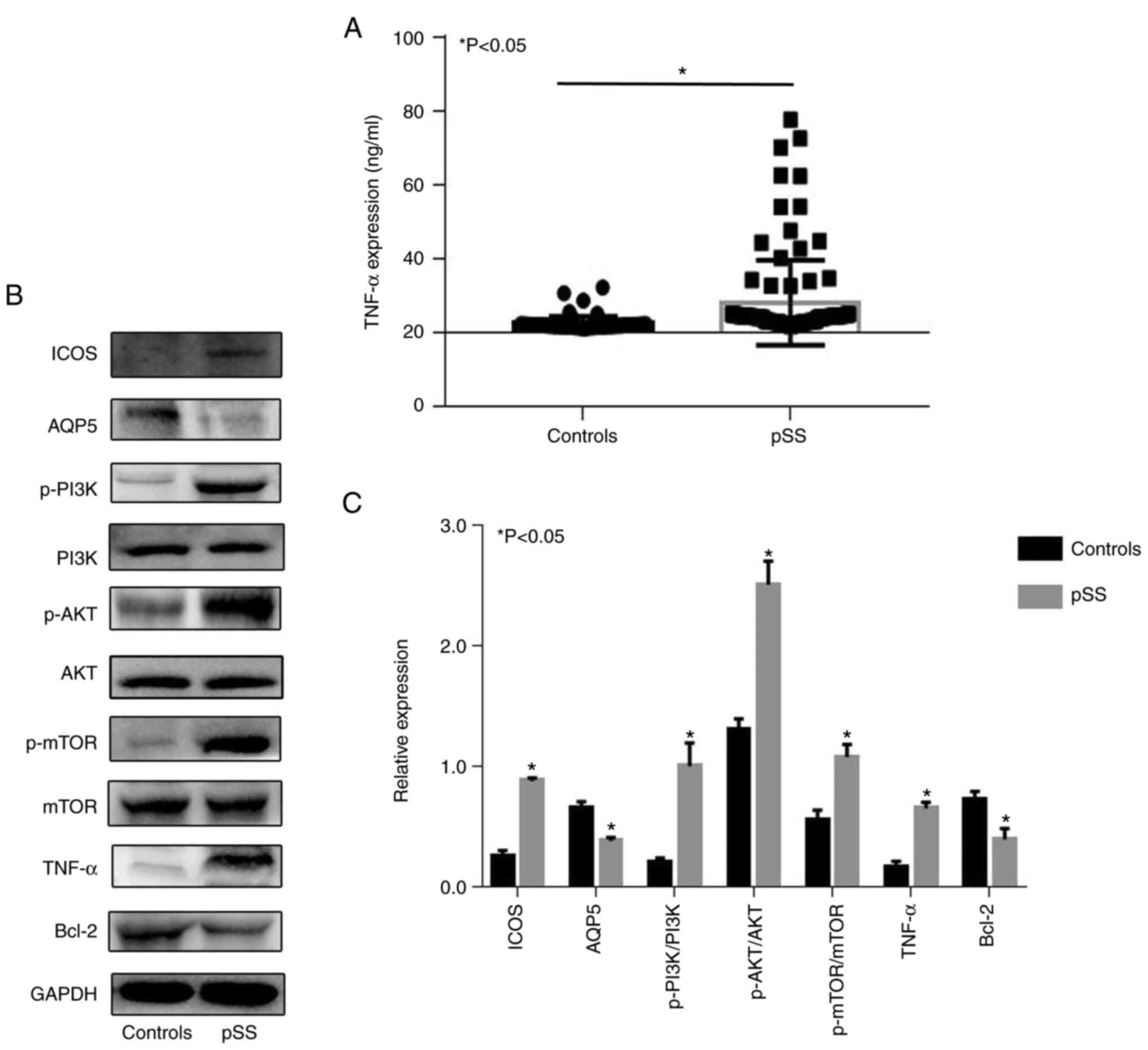 | Figure 4.Relative protein expression in pSS
patients. (A) Expression of TNF-α in the serum of patients with pSS
and controls. (B and C) The protein expression levels of ICOS,
AQP5, PI3K, p-PI3K, AKT, p-AKT, mTOR, p-mTOR, TNF-α and Bcl-2 in
patients with pSS and the control group were evaluated by western
blotting. GAPDH served as a positive control.
*P<0.05. AQP5, aquaporin 5; ICOS, inducible T cell
co-stimulator; p-, phosphorylated; pSS, primary Sjogren's
syndrome. |
Discussion
pSS is a systemic autoimmune disease characterized
by periductal lymphocyte infiltration in the lacrimal and salivary
glands, resulting in low tear and saliva secretion, dry mouth and
eyes, early tooth loss (45,46), atypical and/or serious dental
caries (47–51), onset of oral moniliasis, atrophic
oral mucous damage and tongue lobulation (52). Complications, such as variations
in sense of taste, dysphagia (53,54), inability to eat or speak,
sensation of burning and persistent fatigue (54), may decrease the quality of life of
patients. However, the cellular and body fluid causal links
involved in the etiopathogenesis of pSS remain to be
elucidated.
It has been demonstrated that ICOS is important in
T-cell-driven multiorgan inflammatory events in autoimmunity
illnesses (55). A previous study
reported that ICOS signaling can affect the expression of
inflammatory cytokine through the PI3K-Akt-mTOR pathway. ICOS
signaling appears to be critical for Ab production, but its role in
the maintenance phase may involve inflammatory cytokines such as
TNF-a. A previous study also reported that the expression of ICOS
is markedly associated with ESSDAI score and gradation of focus
scoring, indicating that ICOS may be associated with the severity
of pSS (23). However, the
mechanism by which the expression of ICOS affects the secretion of
saliva has not been studied to date. The present study compared pSS
salivary tissue expression dataset (GSE40611) and whole blood
expression dataset (GSE84844) from GEO. In addition, saliva,
salivary gland tissues and whole blood were collected from 95
patients with pSS and 68 healthy individuals. The positive ratio of
ICOS in the salivary gland tissues of controls and pSS patients was
3.76 and 14.4%, respectively. Compared with that of healthy
individuals, the levels of ICOS in peripheral blood and salivary
samples were increased in patients with pSS, as determined by
ELISA. As with blood, saliva is a complex fluid containing a
variety of enzymes, hormones, antibodies, antimicrobial
constituents, and growth factors (56). Saliva and tears drain the main
targets of autoimmune response, which in the case of pSS are the
salivary and lacrimal glands (57). Saliva has been used as a
prospective biofluid for identifying specific markers for pSS with
underlying functions and clinical impact (58,59). In the present study, in the saliva
of patients with pSS, a negative correlation was detected between
the expression of ICOS and the salivary weight.
AQPs are membrane proteins that mediate water
movement across the lipid bilayer in response to an osmotic
gradient (60). AQPs have been
identified in nearly every living organism (61). A previous study revealed that
disordered salivary secretion was partially due to the aberrant
distributional status of AQP5 in human salivary gland epithelial
cells (62). AQP5 is affected
leading to the reduction of salivary secretion by apoptotic
biomolecules and inflammatory cell factors (62). However, the association of
cellular factors with pSS remains elusive in terms of
immunopathogenesis. To verify the expression of AQP5, salivary
gland tissues were collected from normal and pSS patients. Compared
with those in healthy individuals, the levels of AQP5 in salivary
gland tissues were lower in patients with pSS. The GSE84844 dataset
showed AQP5 was negatively correlated with the expression of ICOS
in patients with pSS. The salivary gland tissues of 95 patients and
68 healthy individuals were harvested and used for western blot
analysis. The results demonstrated that the expression of AQP5 in
patients with pSS was significantly lower compared with that in
healthy individuals whereas the expression of ICOS in patients with
pSS was significantly higher compared with that in healthy
individuals. The effect of ICOS on AQP5 expression is unclear.
In the present study, the salivary weight was
negatively correlated with the expression of ICOS in patients with
pSS. Compared with that of healthy individuals, the expression of
ICOS was elevated in patients with pSS in whole blood and salivary
gland tissue. A previous study revealed that ICOS/PI3K signal
transduction was pivotal for the production of Tfh cells (25). Similar defects in antibody
generation are detected in immunized mice lacking ICOS or
selectively dysregulated ICOS/PI3K signal transduction (44).
A previous study reported that ICOS signaling can
affect the expression of inflammatory cytokine through the
PI3K-Akt-mTOR pathway (26).
Another study indicated that ICOS increased the expression of TNF-α
(44). The high expression of
TNF-α is vital for the development of collagen-induced arthritis
(CIA) in human rheumatoid arthritis (63,64). Increased circulation of IL-6 and
TNF-α in patients with pSS has also been reported (65–70). The expression of TNF-α can caused
epithelial cell impairment such as salivary gland epithelial cells
in pSS (71). A previous study
revealed that the overexpression of TNF-α in murine models
decreases the expression of Bcl-2 and induces the downstream
caspase cascade, causing inherent inflammatory pathway stimulation
(72) In the present study, the
expression of TNF-α in the serum of patients with pSS was greater
compared with that in healthy individuals. Compared with healthy
individuals, the expression of ICOS, TNF-α, p-PI3K, p-AKT and
p-mTOR was increased, whereas the expression of Bcl-2 and AQP5 was
reduced in patients with pSS. It was hypothesized that ICOS may
lead to salivary gland inflammatory responses and may affect saliva
secretion. In summary, ICOS may serve a role in salivary gland
inflammatory events, which may be an underlying causal link for the
reduction in saliva secretion exhibited by patients with pSS.
However, owing to the rarity of pSS disease and the
limited research time, the sample size of the present study was
small. In the future, the sample size should be increased to
validate the conclusions of the present study. It is a matter for
regret that no mature cell model or animal model has been found to
detect the expression of AQP5 by overexpression or knockout of
ICOS. In the future, once there is a mature cell model or animal
model, the verification of relevant experiments will be
performed.
Acknowledgements
Not applicable.
Funding
The present study was supported by The National Natural Science
Foundation of China (grant no. 81801610).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
JJ and ZX conceived and designed the experiments;
PL, YJ and RZ performed the experiments; PL, YJ and RZ analyzed the
data, provided reagents/materials/analysis tools and wrote the
manuscript. ZX and JJ confirm the authenticity of all the raw data.
All authors read and approved the final version of manuscript.
Ethics approval and consent to
participate
Written informed consent for the use of saliva,
whole blood samples and salivary gland tissues was obtained from
all patients. The present study was approved by the ethics
committee of the Affiliated Hospital of Nantong University
(Nantong, China; approval no. 2017-K003).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Manoussakis MN and Moutsopoulos HM:
Sjögren's syndrome: Autoimmune epithelitis. Baillieres Best Pract
Res Clin Rheumatol. 14:73–95. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Norcross MA: A synaptic basis for
T-lymphocyte activation. Ann Immunol (Paris). 135D:113–134.
1984.PubMed/NCBI
|
|
3
|
Janeway CA Jr and Bottomly K: Signals and
signs for lymphocyte responses. Cell. 76:275–285. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Jenkins MK: The ups and downs of T cell
costimulation. Immunity. 1:443–446. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Li X, Yu D, Yu N, Wang X, Li X, Harris DCH
and Wang Y: B7-H4 deficiency in salivary gland of patients with
primary Sjögren's syndrome impairs the regulatory effect on T
cells. Int J Rheum Dis. 20:474–480. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Mozaffarian N, Wiedeman AE and Stevens AM:
Active systemic lupus erythematosus is associated with failure of
antigen-presenting cells to express programmed death ligand-1.
Rheumatology (Oxford). 47:1335–1341. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Greenfield EA, Nguyen KA and Kuchroo VK:
CD28/B7 costimulation: A review. Crit Rev Immunol. 18:389–418.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Hutloff A, Dittrich AM, Beier KC,
Eljaschewitsch B, Kraft R, Anagnostopoulos I and Kroczek RA: ICOS
is an inducible T-cell co-stimulator structurally and functionally
related to CD28. Nature. 397:263–266. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Sharpe AH and Freeman GJ: The B7-CD28
superfamily. Nat Rev Immunol. 2:116–126. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Crotty S: T follicular helper cell
differentiation, function, and roles in disease. Immunity.
41:529–542. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Suh WK: Life of T follicular helper cells.
Mol Cells. 38:195–201. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Liu D, Xu H, Shih C, Wan Z, Ma X, Ma W,
Luo D and Qi H: T-B-cell entanglement and ICOSL-driven feed-forward
regulation of germinal centre reaction. Nature. 517:214–218. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Xu H, Li X, Liu D, Li J, Zhang X, Chen X,
Hou S, Peng L, Xu C, Liu W, et al: Follicular T-helper cell
recruitment governed by bystander B cells and ICOS-driven motility.
Nature. 496:523–527. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Grimbacher B, Hutloff A, Schlesier M,
Glocker E, Warnatz K, Dräger R, Eibel H, Fischer B, Schäffer AA,
Mages HW, et al: Homozygous loss of ICOS is associated with
adult-onset common variable immunodeficiency. Nat Immunol.
4:261–268. 2003. View
Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tafuri A, Shahinian A, Bladt F, Yoshinaga
SK, Jordana M, Wakeham A, Boucher LM, Bouchard D, Chan VS, Duncan
G, et al: ICOS is essential for effective T-helper-cell responses.
Nature. 409:105–109. 2001. View
Article : Google Scholar : PubMed/NCBI
|
|
16
|
Dong C, Juedes AE, Temann UA, Shresta S,
Allison JP, Ruddle NH and Flavell RA: ICOS co-stimulatory receptor
is essential for T-cell activation and function. Nature.
409:97–101. 2001. View
Article : Google Scholar : PubMed/NCBI
|
|
17
|
Mak TW, Shahinian A, Yoshinaga SK, Wakeham
A, Boucher LM, Pintilie M, Duncan G, Gajewska BU, Gronski M,
Eriksson U, et al: Costimulation through the inducible costimulator
ligand is essential for both T helper and B cell functions in T
cell-dependent B cell responses. Nat Immunol. 4:765–772. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
McAdam AJ, Greenwald RJ, Levin MA,
Chernova T, Malenkovich N, Ling V, Freeman GJ and Sharpe AH: ICOS
is critical for CD40-mediated antibody class switching. Nature.
409:102–105. 2001. View
Article : Google Scholar : PubMed/NCBI
|
|
19
|
Li DY and Xiong XZ: ICOS+
Tregs: A functional subset of tregs in immune diseases. Front
Immunol. 11:21042020. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Zhu Y, Zou L and Liu YC: T follicular
helper cells, T follicular regulatory cells and autoimmunity. Int
Immunol. 28:173–179. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gang C, Jiahui Y, Huaizhou W, Qing C,
Dongbao Z and Qian S: Defects of mitogen-activated protein kinase
in ICOS signaling pathway lead to CD4(+) and CD8(+) T-cell
dysfunction in patients with active SLE. Cell Immunol. 258:83–89.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zhou H, Li B, Li J, Wu T, Jin X, Yuan R,
Shi P, Zhou Y, Li L and Yu F: Dysregulated T cell activation and
aberrant cytokine expression profile in systemic lupus
erythematosus. Mediators Inflamm. 2019:84509472019. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Luo J, Liao X, Zhang L, Xu X, Ying S, Yu
M, Zhu L, Lin S and Wang X: Transcriptome sequencing reveals
potential roles of ICOS in primary Sjögren's syndrome. Front Cell
Dev Biol. 8:5924902020. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
García-Espinoza JA, Muñoz-Valle JF,
García-Chagollán M, Hernández-Bello J, Palafox-Sánchez CA,
López-Villalobos EF, Sánchez-Zuno GA, Martínez-Bonilla GE,
Cerpa-Cruz S, Carrillo-Ballesteros FJ and Oregon-Romero E: ICOS
gene polymorphisms (IVS1 + 173 T/C and c. 1624 C/T) in Primary
Sjögren's syndrome patients: Analysis of ICOS expression. Curr
Issues Mol Biol. 44:764–776. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Gigoux M, Shang J, Pak Y, Xu M, Choe J,
Mak TW and Suh WK: Inducible costimulator promotes helper T-cell
differentiation through phosphoinositide 3-kinase. Proc Natl Acad
Sci USA. 106:20371–20376. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Gigoux M, Lovato A, Leconte J, Leung J,
Sonenberg N and Suh WK: Inducible costimulator facilitates
T-dependent B cell activation by augmenting IL-4 translation. Mol
Immunol. 59:46–54. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Bonifazi P, D'Angelo C, Zagarella S,
Zelante T, Bozza S, De Luca A, Giovannini G, Moretti S, Iannitti
RG, Fallarino F, et al: Intranasally delivered siRNA targeting
PI3K/Akt/mTOR inflammatory pathways protects from aspergillosis.
Mucosal Immunol. 3:193–205. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
King LS and Agre P: Pathophysiology of the
aquaporin water channels. Annu Rev Physiol. 58:619–648. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Farzan N, Vijverberg SJ, Arets HG,
Raaijmakers JA and Maitland-van der Zee AH: Pharmacogenomics of
inhaled corticosteroids and leukotriene modifiers: A systematic
review. Clin Exp Allergy. 47:271–293. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Ashburner M, Ball CA, Blake JA, Botstein
D, Butler H, Cherry JM, Davis AP, Dolinski K, Dwight SS, Eppig JT,
et al: Gene ontology: Tool for the unification of biology. The Gene
Ontology Consortium. Nat Genet. 25:25–29. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Kanehisa M, Goto S, Sato Y, Furumichi M
and Tanabe M: KEGG for integration and interpretation of
large-scale molecular data sets. Nucleic Acids Res. 40:(Database
issue). D109–D114. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Huang DW, Sherman BT, Tan Q, Kir J, Liu D,
Bryant D, Guo Y, Stephens R, Baseler MW, Lane HC and Lempicki RA:
DAVID Bioinformatics Resources: Expanded annotation database and
novel algorithms to better extract biology from large gene lists.
Nucleic Acids Res. 35:(Web Server issue). W169–W175. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Szklarczyk D, Gable AL, Lyon D, Junge A,
Wyder S, Huerta-Cepas J, Simonovic M, Doncheva NT, Morris JH, Bork
P, et al: STRING v11: Protein-protein association networks with
increased coverage, supporting functional discovery in genome-wide
experimental datasets. Nucleic Acids Res. 47((D1)): D607–D613.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Doncheva NT, Morris JH, Gorodkin J and
Jensen LJ: Cytoscape StringApp: Network analysis and visualization
of proteomics data. J Proteome Res. 18:623–632. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Vitali C, Bombardieri S, Jonsson R,
Moutsopoulos HM, Alexander EL, Carsons SE, Daniels TE, Fox PC, Fox
RI, Kassan SS, et al: Classification criteria for Sjögren's
syndrome: A revised version of the European criteria proposed by
the American-European Consensus Group. Ann Rheum Dis. 61:554–558.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Nocturne G: Sjögren's syndrome update:
Clinical and therapeutic aspects. Rev Med Interne. 40:433–439.
2019.(In French). View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Rosas J, Sánchez-Piedra C,
Fernández-Castro M, Andreu JL, Martínez-Taboada V and Olivé A;
SJÖGRENSER Group and part of the Spanish Society of Rheumatology
Systemic Autoimmune Diseases Study Group (EASSER), : ESSDAI
activity index of the SJÖGRENSER cohort: Analysis and comparison
with other European cohorts. Rheumatol Int. 39:991–999. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Chen X, Aqrawi LA, Utheim TP, Tashbayev B,
Utheim ØA, Reppe S, Hove LH, Herlofson BB, Singh PB, Palm Ø, et al:
Elevated cytokine levels in tears and saliva of patients with
primary Sjögren's syndrome correlate with clinical ocular and oral
manifestations. Sci Rep. 9:73192019. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Greenspan JS, Daniels TE, Talal N and
Sylvester RA: The histopathology of Sjögren's syndrome in labial
salivary gland biopsies. Oral Surg Oral Med Oral Pathol.
37:217–229. 1974. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Vitali C, Moutsopoulos HM and Bombardieri
S: The European Community Study Group on diagnostic criteria for
Sjögren's syndrome. Sensitivity and specificity of tests for ocular
and oral involvement in Sjögren's syndrome. Ann Rheum Dis.
53:637–647. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Vitali C, Bombardieri S, Moutsopoulos HM,
Balestrieri G, Bencivelli W, Bernstein RM, Bjerrum KB, Braga S,
Coll J, de Vita S, et al: Preliminary criteria for the
classification of Sjögren's syndrome. Results of a prospective
concerted action supported by the European Community. Arthritis
Rheum. 36:340–347. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Vitali C, Bombardieri S, Moutsopoulos HM,
Coll J, Gerli R, Hatron PY, Kater L, Konttinen YT, Manthorpe R,
Meyer O, et al: Assessment of the European classification criteria
for Sjögren's syndrome in a series of clinically defined cases:
Results of a prospective multicentre study. The European Study
Group on Diagnostic Criteria for Sjögren's Syndrome. Ann Rheum Dis.
55:116–121. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Daniels TE and Whitcher JP: Association of
patterns of labial salivary gland inflammation with
keratoconjunctivitis sicca. Analysis of 618 patients with suspected
Sjögren's syndrome. Arthritis Rheum. 37:869–877. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Panneton V, Bagherzadeh Yazdchi S, Witalis
M, Chang J and Suh WK: ICOS signaling controls induction and
maintenance of collagen-induced arthritis. J Immunol.
200:3067–3076. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Daniels TE, Silverman S Jr, Michalski JP,
Greenspan JS, Sylvester RA and Talal N: The oral component of
Sjögren's syndrome. Oral Surg Oral Med Oral Pathol. 39:875–885.
1975. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Baudet-Pommel M, Albuisson E, Kemeny JL,
Falvard F, Ristori JM, Fraysse MP and Sauvezie B: Early dental loss
in Sjögren's syndrome. Histologic correlates. European Community
Study Group on Diagnostic Criteria for Sjögren's Syndrome (EEC
COMAC). Oral Surg Oral Med Oral Pathol. 78:181–186. 1994.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Daniels TE and Fox PC: Salivary and oral
components of Sjögren's syndrome. Rheum Dis Clin North Am.
18:571–589. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Greenspan D: Xerostomia: Diagnosis and
management. Oncology (Williston Park). 10 (3 Suppl):S7–S11.
1996.
|
|
49
|
Lilly JP and Fotos PG: Sjögren's syndrome:
Diagnosis and management of oral complications. Gen Dent.
44:404–408; quiz. 419–420. 1996.PubMed/NCBI
|
|
50
|
Ravald N and List T: Caries and
periodontal conditions in patients with primary Sjögren's syndrome.
Swed Dent J. 22:97–103. 1998.PubMed/NCBI
|
|
51
|
Soto-Rojas AE, Villa AR, Sifuentes-Osornio
J, Alarcón-Segovia D and Kraus A: Oral manifestations in patients
with Sjögren's syndrome. J Rheumatol. 25:906–910. 1998.PubMed/NCBI
|
|
52
|
Hernandez YL and Daniels TE: Oral
candidiasis in Sjögren's syndrome: Prevalence, clinical
correlations, and treatment. Oral Surg Oral Med Oral Pathol.
68:324–329. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Rhodus NL, Colby S, Moller K and Bereuter
J: Quantitative assessment of dysphagia in patients with primary
and secondary Sjögren's syndrome. Oral Surg Oral Med Oral Pathol
Oral Radiol Endod. 79:305–310. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Pedersen AM, Reibel J and Nauntofte B:
Primary Sjögren's syndrome (pSS): Subjective symptoms and salivary
findings. J Oral Pathol Med. 28:303–311. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Odegard JM, DiPlacido LD, Greenwald L,
Kashgarian M, Kono DH, Dong C, Flavell RA and Craft J: ICOS
controls effector function but not trafficking receptor expression
of kidney-infiltrating effector T cells in murine lupus. J Immunol.
182:4076–4084. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Deepa T and Thirrunavukkarasu N: Saliva as
a potential diagnostic tool. Indian J Med Sci. 64:293–306. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Katsiougiannis S and Wong DT: The
Proteomics of Saliva in Sjögren's Syndrome. Rheum Dis Clin North
Am. 42:449–456. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Giusti L, Baldini C, Bazzichi L,
Bombardieri S and Lucacchini A: Proteomic diagnosis of Sjögren's
syndrome. Expert Rev Proteomics. 4:757–767. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Hu S, Wang J, Meijer J, Ieong S, Xie Y, Yu
T, Zhou H, Henry S, Vissink A, Pijpe J, et al: Salivary proteomic
and genomic biomarkers for primary Sjögren's syndrome. Arthritis
Rheum. 56:3588–3600. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Verkman AS: Aquaporins at a glance. J Cell
Sci. 124((Pt 13)): 2107–2112. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Hoffert JD, Chou CL and Knepper MA:
Aquaporin-2 in the ‘-omics’ era. J Biol Chem. 284:14683–14687.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Yoshimura S, Nakamura H, Horai Y, Nakajima
H, Shiraishi H, Hayashi T, Takahashi T and Kawakami A: Abnormal
distribution of AQP5 in labial salivary glands is associated with
poor saliva secretion in patients with Sjögren's syndrome including
neuromyelitis optica complicated patients. Mod Rheumatol.
26:384–390. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Brennan FM and McInnes IB: Evidence that
cytokines play a role in rheumatoid arthritis. J Clin Invest.
118:3537–3545. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Williams RO, Feldmann M and Maini RN:
Anti-tumor necrosis factor ameliorates joint disease in murine
collagen-induced arthritis. Proc Natl Acad Sci USA. 89:9784–9788.
1992. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Liu C, Guan Z, Zhao L, Song Y and Wang H:
Elevated level of circulating
CD4+Helios+FoxP3+ cells in primary
Sjogren's syndrome patients. Mod Rheumatol. 27:630–637. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Szodoray P, Papp G, Horvath IF, Barath S,
Sipka S, Nakken B and Zeher M: Cells with regulatory function of
the innate and adaptive immune system in primary Sjögren's
syndrome. Clin Exp Immunol. 157:343–349. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Roescher N, Tak PP and Illei GG: Cytokines
in Sjogren's syndrome: Potential therapeutic targets. Ann Rheum
Dis. 69:945–948. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Baturone R, Soto MJ, Márquez M, Macías I,
de Oca MM, Medina F, Chozas N, García-Pérez S and Girón-González
JA: Health-related quality of life in patients with primary
Sjögren's syndrome: Relationship with serum levels of
proinflammatory cytokines. Scand J Rheumatol. 38:386–389. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Szodoray P, Alex P, Brun JG, Centola M and
Jonsson R: Circulating cytokines in primary Sjögren's syndrome
determined by a multiplex cytokine array system. Scand J Immunol.
59:592–599. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Garcíc-Carrasco M, Font J, Filella X,
Cervera R, Ramos-Casals M, Sisó A, Aymamí A, Ballesta AM and
Ingelmo M: Circulating levels of Th1/Th2 cytokines in patients with
primary Sjögren's syndrome: Correlation with clinical and
immunological features. Clin Exp Rheumatol. 19:411–415.
2001.PubMed/NCBI
|
|
71
|
Fox RI, Kang HI, Ando D, Abrams J and Pisa
E: Cytokine mRNA expression in salivary gland biopsies of Sjögren's
syndrome. J Immunol. 152:5532–5539. 1994.PubMed/NCBI
|
|
72
|
Xu H, Li J, Zhao Y and Liu D: TNFα-induced
downregulation of microRNA-186 contributes to apoptosis in rat
primary cardiomyocytes. Immunobiology. 222:778–784. 2017.
View Article : Google Scholar : PubMed/NCBI
|