As one of the most common causes of death, cancer is
a serious health problem globally and the mortality remains the
first in China and the second in the US (first in 21 states) and
other Western countries (1,2). There were 4,292,000 new cases with
2,814,000 deaths of cancers and the incidence and mortality of lung
cancer were the highest in China in 2015 (1). The common treatments for cancer
include surgery, radiation, chemotherapy, targeted therapy and
immunotherapy, while chemotherapy remains one of the most important
treatments (3,4). Numerous chemotherapeutic drugs have
been developed and used for the treatment of cancer, such as
paclitaxel, cisplatin, 5-fluorouraci, cyclophosphamide, irinotecan,
mitomycin C and doxorubicin (5–11).
However, the effectiveness of chemotherapy as monotherapy is
limited in cancer therapy due to low water solubility, lack of
convincing anticancer activity and therapeutic selectivity, and
drug resistance especially multiple drug resistance (MDR) (12–15).
Therefore, the combination of various chemotherapeutic drugs with
different mechanisms has become the standard clinical practice for
cancer treatment (16–24).
Paclitaxel is a natural plant alkaloid that is
isolated from the bark of the pacific yew tree and the active
ingredient was firstly isolated and named as Taxol by Wani and Wall
(25–27). Paclitaxel is a mitotic inhibitor for
targeting tubulin by stabilizing the microtubule polymer and
protecting it from disassembly to prevent the metaphase spindle
configuration of chromosomes. Thus, it caused abnormality of
mitotic spindle assembly, chromosome segregation, and cell
division, resulting in blocking the progression of mitosis and
prolonging activation of the mitotic checkpoint to trigger cell
apoptosis or blocking cell cycle arrest at G2/M without cell
division of treated cells (28–33).
Although paclitaxel is widely used for the treatment of various
cancers including cervical, breast, ovarian, brain, bladder,
prostate, liver and lung cancers, the application of paclitaxel in
clinic is significantly limited due to MDR (34–39).
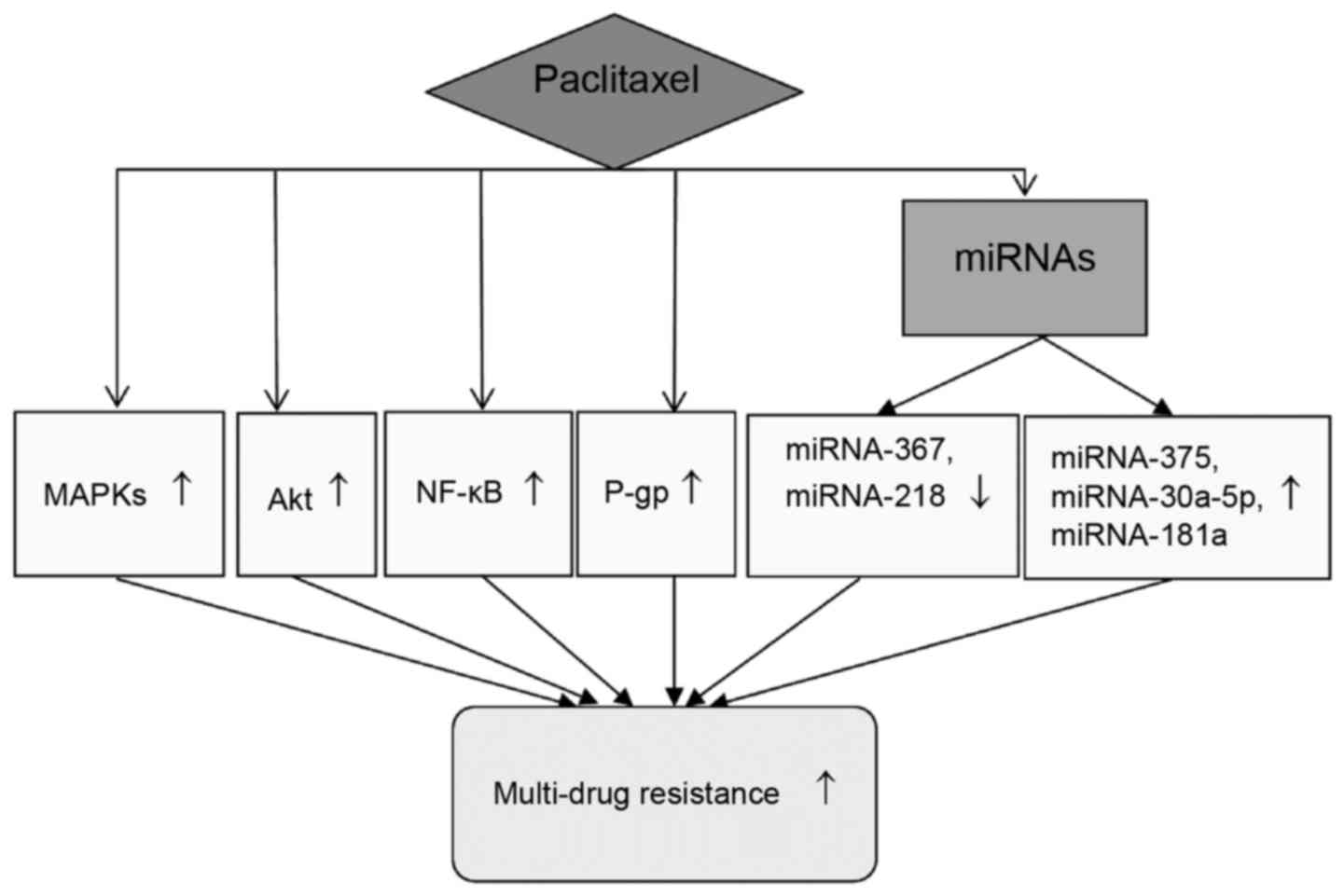
Many factors may be responsible for the MDR of paclitaxel and the
possible mechanisms are proposed in Fig. 1. The multidrug resistance gene 1
encodes the transporter P-glycoprotein (P-gp) leading to MDR
(40–46). The activation of protein kinase B
(Akt) and nuclear factor-κB (NF-κB) is the important cause for MDR
(47,48). The activation of mitogen-activated
protein kinases (MAPKs) is also responsible for MDR (49,50).
Therefore, in order to improve the therapeutic effect of
paclitaxel, it is necessary to reverse its MDR.
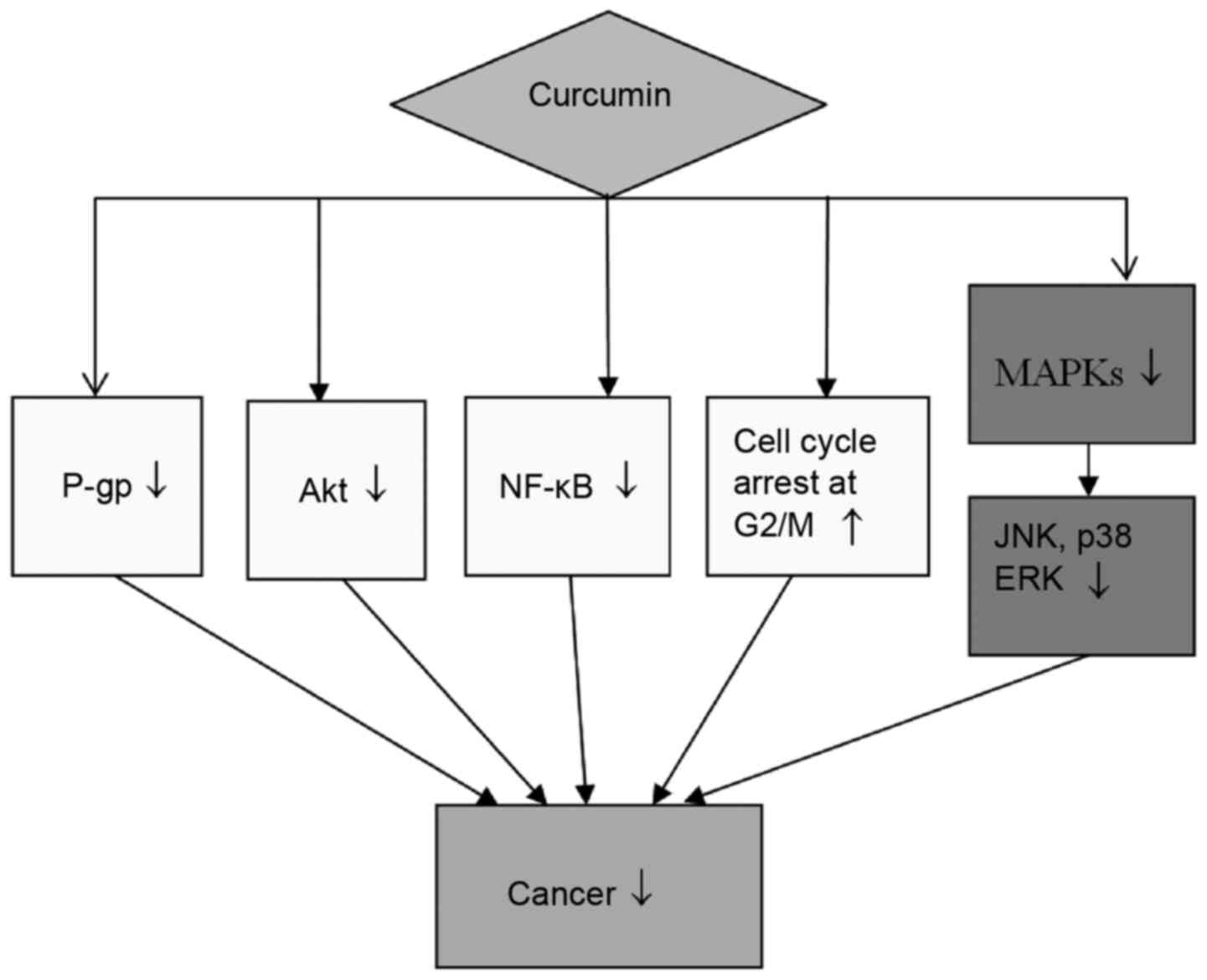
Curcumin is an effective monomer component extracted
from the roots of Zingiberaceae. It shows many biological functions
such as antioxidant, anti-inflammation and especially antitumor
(51–55). Many previous studies showed that
curcumin inhibited cancer cell growth and reversed MDR through
various mechanisms including antiproliferation, induction of
apoptosis and blocking cell cycle arrest at G2/M of cancer cells
(56,57) as shown in Fig. 2. NF-κB is a nuclear protein and a
transcription factor; it is in activated status in a variety of
cancers (58). NF-κB plays a key
role in the aspects of cell proliferation, differentiation,
survival, metastasis, and apoptosis. Curcumin inhibits the
activation of NF-κB and NF-κB regulated Akt (59–61).
Curcumin reduces the expression levels of c-Jun N-terminal kinase
(JNK), MAPK p38 and extracellular signal-regulated kinase (ERK)
(62,63). Curcumin blocks cell cycle arrest at
G2/M of cancer cells (64–67). Curcumin also inhibits the expression
of P-gp, therefore, it may not only become a promising anticancer
drug but also an excellent agent for MDR reversal (68–71).
Based on the mechanisms of anticancer action of
curcumin, it is rational and valuable to use the combination of
paclitaxel and curcumin for synergistic anticancer activity and
reversing MDR of paclitaxel (Table
I). Numerous previous studies showed that the combination of
paclitaxel and curcumin reversed the MDR of paclitaxel and
inhibited cancer cell growth more effectively than paclitaxel
alone. This review focuses on the combination of paclitaxel and
curcumin in cancer therapy for different types of cancers.
Cervical cancer is the second most common cancer in
female reproductive system and almost 500,000 new cases are
diagnosed in women worldwide every year (72). It ranked both the fourth-most common
cause of cancer and the fourth-most common cause of death from
cancer in women worldwide (73).
The commonly used chemotherapeutic drugs for the treatment of
cervical cancer include cisplatin, paclitaxel, fluorouracil,
gemcitabine, ifosfamide and mitomycin C. Recent studies indicated
that the combination of paclitaxel and curcumin was quite effective
for the treatment of cervical cancer in preclinical settings
(74–78). Studies have demonstrated that
curcumin sensitized paclitaxel-induced apoptosis via enhancing the
expression of p53, activation of caspase-3, −7, −8 and −9, cleavage
of poly(ADP-ribose) polymerase (PARP) and release of cytochrome c
by western blot analysis (74,77).
Therefore, the combination of paclitaxel and curcumin may have
synergistic anticancer effect and be a promising regimen for the
treatment of cervical cancer.
MDR significantly affects the antitumor activity of
paclitaxel against cervical cancer, while reversal of MDR improves
its anticancer effect. A study by Bava et al showed that
paclitaxel could activate NF-κB and Akt leading to the development
of MDR of paclitaxel, whereas curcumin was able to reverse MDR of
paclitaxel via the inhibition of NF-κB (the inhibition of
phosphorylation of IKBa and the reduction of p65-NF-κB subunit) and
Akt (74). Cyclooxygenase-2 (COX-2)
and cyclin D1 are the most important gene products regulated by
NF-κB and Akt. Another study by the same group noted that
paclitaxel activated the expression levels of COX-2 and cyclin D1,
while curcumin downregulated the expression levels of COX-2 and
cyclin D1 (75). The combination of
paclitaxel and curcumin could inhibit anti-apoptotic proteins
including cellular inhibitor of apoptosis 1 (cIAP1), X-linked
inhibitor of apoptosis protein (XIAP) and survivin through the
inhibition of NF-κB and Akt (76,77).
The study also showed that the combination of paclitaxel and
curcumin reversed the MDR of paclitaxel by inhibiting JNK, p38 MAPK
and ERK (76). Punfa et al
reported that the encapsulation of curcumin in
polylactic-co-glycolic acid nanoparticles could target P-gp and
reduce its expression and the combination of paclitaxel and
curcumin reversed the MDR of paclitaxel by targeting P-gp in
cervical cancer cells (78).
MDR of paclitaxel significantly limits its
therapeutic effect and clinical application. Royt et al
demonstrated that the combination of paclitaxel and curcumin
significantly improved the anticancer effect by reversing MDR of
paclitaxel via inhibition of NF-κB (84). Inhibition of phosphorylation of IKBa
contributed to the inhibition of NF-κB and paclitaxel induced the
phosphorylation of IKBa to activate NF-κB (85). However, curcumin inhibited the
phosphorylation of IKBa to inhibit the activation of NF-κB
(86). Paclitaxel activated the
gene products of matrix metalloprotein-9 (MMP-9), COX-2, C-myc and
cyclin D1, while curcumin inhibited their activation through
inhibition of NF-κB and Akt (85,86).
Wang et al developed a multifunctional anti-cancer
nanomedicine loaded with magnetic nanoparticles (MNPs), paclitaxel
and curcumin and showed that the nanoparticles reduced the
expression of P-gp and increased paclitaxel accumulation in breast
cancer MCF-7/ADR cells, thereby, enhancing the therapeutic efficacy
of paclitaxel against breast cancer cells and the effect was due to
reversing MDR of paclitaxel through inhibition of P-gp by curcumin
(87).
Ovarian cancer is one of the most common cancers in
the female reproductive system and the fifth most common cause of
cancer deaths in women worldwide; its incidence has been increasing
recently (2). Paclitaxel has been
used for the treatment of ovarian cancer for many years. Numerous
studies have shown that the combination of paclitaxel and curcumin
was more effective than paclitaxel alone for the treatment of
ovarian cancer preclinically (82,88–93).
The expression of potassium channel TREK-1 was increased in ovarian
cancer cells and the inhibitors of potassium channels could inhibit
the cell growth and proliferation of ovarian cancer cells. A study
by Innamaa et al showed that curcumin inhibited ovarian
cancer cell proliferation via inhibition of TREK-1 and enhanced the
anticancer effect of paclitaxel against ovarian cancer (89). Deng et al reported that the
combination of paclitaxel and curcumin blocked cell cycle arrest at
G2/M and showed synergistic anticancer effect against human ovarian
cancer cells HO-8910 (90).
MDR of paclitaxel is developed mainly due to the
activation of NF-κB and Akt, which are the mediators of cell
survival, proliferation and metastasis. The activation of matrix
metalloprotein-2 (MMP-2), MMP-9, survivin, human telomerase reverse
transcriptase (hTERT), vascular endothelial growth factor (VEGF),
and basic fibroblast growth factor (b-FGF) also results in MDR of
paclitaxel. MDR is a major problem for paclitaxel in the treatment
of brain cancer. Curcumin could inhibit the expression levels of
NF-κB, Akt, MMP-2, MMP-9, survivin, hTERT, VEGF, and b-FGF,
therefore, the combination of paclitaxel and curcumin could enhance
the anticancer effect of paclitaxel for the treatment of brain
cancer by reversing MDR of paclitaxel (95). A study by Manju et al also
showed that the multifunctional magnetic nanoparticles (MNPs)
loaded with paclitaxel and curcumin showed stronger anticancer
effect than the combination of paclitaxel and curcumin freely by
targeting and reducing P-gp for the treatment of brain cancer
(96).
Bladder cancer is the most common cancer in the
urinary system and the ninth most common cancer worldwide (72). The common chemotherapeutic drugs for
the treatment of bladder cancer include cisplatin, carboplatin,
gemcitabine, paclitaxel, docetaxel, doxorubicin, fluorouracil,
methotrexate, vinblastine, ifosfamide, and pemetrexed. Kamat et
al demonstrated that the combination of paclitaxel and curcumin
blocked cell cycle arrest at G2/M in human bladder cancer cells and
showed synergistic therapeutic effect against bladder cancer
(98).
Prostate cancer is the most common cause of cancer
and the second-most common cause of death from cancer among men
worldwide (2,72). Numerous studies have showed that the
combination of paclitaxel and curcumin were more effective than
paclitaxel alone against prostate cancer through various mechanisms
(99–101). Proliferation cell nuclear antigen
(PCNA) and MMP-2 are both involved in cell proliferation and
invasion of prostate cancer cells. Zhao et al have showed
that the combination of paclitaxel and curcumin significantly
decreased the quantities and expression levels of PCNA and MMP-2 in
prostate cancer cells compared to paclitaxel alone (99). Tumor cell immigration from one organ
to another contributes to tumor metastasis. Paclitaxel or curcumin
alone could reduce the immigration of cancer cells and the
combination of paclitaxel and curcumin exhibited synergistic
antimetastasis effect in prostate cancer via inhibition of cell
immigration (100). The results
from the studies of Huang et al indicated that the
expression of Bcl-2 was inhibited and the expression of Bax was
enhanced when prostate cancer cells were treated with the
combination of paclitaxel and curcumin (101). The study by Thomas et al
also showed that the combination of paclitaxel and curcumin could
effectively inhibit the growth of prostate cancer cells by
activating the expression levels of p21 and p53 to influence cell
apoptosis (102).
Liver cancer is one of the most common cancers and
the second (in the USA) or third (worldwide) most common cause of
deaths from cancer (2,73,104).
China has the highest rates of incidence and mortality of liver
cancer in the world (105). The
chemotherapeutic drugs such as 5-fluorouracil, doxorubicin, and
cisplatin have been used for the treatment of liver cancer for many
years. However, the effects of treatment are unsatisfactory because
of MDR and other factors, resulting in the average survival time of
only between 6 and 20 months (106). In general, liver cancer cells are
highly resistant to paclitaxel (106). However, the studies by Zhou et
al showed that curcumin significantly enhanced the sensitivity
of liver cancer Hep3B cells to paclitaxel and the combination of
paclitaxel and curcumin may provide a superior therapeutic index
for the treatment of liver cancer (107).
Lin28 is an RNA-binding protein that inhibits the
process of pre-let-7 miRNAs to reduce tumorigenesis (108). Zhou et al found that the
expression of Lin28 was directly activated by NF-κB and associated
with the resistance of paclitaxel to liver cancer cells (107). Curcumin could down-regulate the
expression of Lin28 and NF-κB activation induced by paclitaxel to
enhance the sensitivity of liver cancer cells to paclitaxel.
Therefore, the combination of paclitaxel and curcumin showed
synergistic effects on cell growth inhibition and apoptotic
induction against liver cancer cells by reversing MDR of
paclitaxel.
Lung cancer is the most common cancer and most
common cause of death from cancer worldwide (2,73). The
mortality of lung cancer has declined and survival rate has
increased in the United Kingdom and the United States (109). However, the incidence and
mortality of lung cancer are still increase in the developing
countries, therefore, substantial efforts are needed to decrease
the mortality of lung cancer. The studies by Boztas et al,
found that the combination of paclitaxel and curcumin
synergistically improved paclitaxel induced apoptosis in lung
cancer H1299 cells, and enhanced the cell growth inhibition for a
low IC50 values for the combination compared to
paclitaxel or curcumin alone (82).
Therefore, the combination of paclitaxel and curcumin may be an
excellent choice for the treatment of lung cancer due to the
synergistic anticancer effect. Muthoosamy et al developed a
drug delivery system loaded with paclitaxel and curcumin by
functionalizing reduced graphene oxide with an amphiphilic polymer
PF-127 via hydrophobic assembly. Cell proliferation assay showed
highly potent synergistic effect with the combination to inhibit
the cell growth of lung cancer cells A549 with IC50
~13.24 µg/ml (110). The possible
mechanism may be associated with increased reactive oxygen species,
mitochondrial membrane potential depletion and cell apoptosis
(110).
Paclitaxel has been widely used for the treatment of
various cancers including cervical, breast, ovarian, brain,
prostate, liver and lung cancers. However, MDR greatly limits the
anticancer efficacy and clinical application of paclitaxel. As we
discussed in this review that curcumin alone or in combination with
chemotherapeutic drugs may alter the signaling pathways and
molecular interactions which regulate MDR. Numerous cell and animal
studies have showed that the combination of paclitaxel and curcumin
exhibited synergistic anticancer effect and reverse MDR of
paclitaxel in various cancers therapy. Therefore, it is speculated
that the combination of paclitaxel and curcumin may be an ideal
strategy in clinical practice for cancer treatment. However, owing
to the low water solubility of curcumin and paclitaxel, the
combination of paclitaxel and curcumin may not be suitable to be
administered as an intravenous infusion. Moreover, the formulation
suitable for parenteral administration of the original product
Taxol has to contain additional surfactants such as Cremophor EL
that may cause acute hypersensitivity reactions and peripheral
neuropathy. Therefore, the dosage for easy dissolution and
absorption is the most serious challenge in clinical practice.
The prospect of the combination of paclitaxel and
curcumin in clinical application for cancer therapy appears to be
promising but also challenging. Therefore, the feasibility and
effectiveness of the combination should be further evaluated in
clinical studies. To our knowledge, there is no report of the
combination of paclitaxel and curcumin in clinical setting for
cancer treatment from the literature up to date. However,
paclitaxel has been widely used for the treatment of patients with
different cancers. Clinical trials of curcumin alone or in
combination with other anticancer drugs have been reported and the
safety and tolerability of curcumin in patients have been
well-established in clinical studies (112–116). Dhillon et al reported a
phase II trial of curcumin in patients with advanced pancreatic
cancer (112). The results showed
that oral administration of 8 g curcumin to the patients daily is
well tolerated and has biological activity in some patients with
pancreatic cancer (112). The
combination of curcumin and gemcitabine in patients with advanced
pancreatic cancer has also been reported (113). In addition, a randomized control
trial has been conducted for the combination of curcumin with
standard care FOLFOX (oxaliplatin + fluorouracil + folinic acid)
chemotherapy in patients with inoperable colorectal cancer
(114). Noteworthy, there are
studies on the combination of docetaxel (a taxane derivative with
similar chemical structure of paclitaxel) and curcumin in patients
with advanced and metastatic breast cancer or castration-resistant
prostate cancer (115,116). The results indicate that some
improvements were observed for biological and clinical responses in
most breast cancer patients and a high response rate, good
tolerability and patient acceptance were achieved in prostate
cancer patients. Furthermore, the low bioavailability of curcumin
could be markedly improved via the use of structural analogues or
special formulations such as highly bioavailable curcumin
(Theracurmin) and/or liposomal curcumin (117,118). In addition, paclitaxel and
curcumin could be encapsulated in biodegradable nanoparticles to
avoid acute hypersensitivity reactions and peripheral neuropathy
from Cremophor EL.
This study was financially supported by the National
Natural Science Foundation of China (81341124,81101678), Science
and Technology Support Project of Sichuan Province (2017JQ0013),
Sichuan Provincial Human Resource and Social Security Department
(2016–183), the Joint Fund of Sichuan Province, Luzhou City and
Southwest Medical University (14JC0134, 14ZC0026, 14ZC0066), the
Joint Fund of Luzhou City and Southwest Medical University
(2013LZLY-K80, 2015LZCYD-S09 (4/8).
|
1
|
Chen W, Zheng R, Baade PD, Zhang S, Zeng
H, Bray F, Jemal A, Yu XQ and He J: Cancer statistics in China,
2015. CA Cancer J Clin. 66:115–132. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Siegel RL, Miller KD and Jemal A: Cancer
statistics, 2016. CA Cancer J Clin. 66:7–30. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Szekeres T and Novotny L: New targets and
drugs in cancer chemotherapy. Med Princ Pract. 11:117–125. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Wu ES, Oduyebo T, Cobb LP, Cholakian D,
Kong X, Fader AN, Levinson KL, Tanner EJ III, Stone RL, Piotrowski
A, et al: Lymphopenia and its association with survival in patients
with locally advanced cervical cancer. Gynecol Oncol. 140:76–82.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sideris S, Aoun F, Zanaty M, Martinez NC,
Latifyan S, Awada A and Gil T: Efficacy of weekly paclitaxel
treatment as a single agent chemotherapy following first-line
cisplatin treatment in urothelial bladder cancer. Mol Clin Oncol.
4:1063–1067. 2016.PubMed/NCBI
|
|
6
|
Dilruba S and Kalayda GV: Platinum-based
drugs: Past, present and future. Cancer Chemother Pharmacol.
77:1103–1124. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Pan X, Zhang X, Sun H, Zhang J, Yan M and
Zhang H: Autophagy inhibition promotes 5-fluorouraci-induced
apoptosis by stimulating ROS formation in human non-small cell lung
cancer A549 cells. PLoS One. 8:e566792013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Emadi A, Jones RJ and Brodsky RA:
Cyclophosphamide and cancer: Golden anniversary. Nat Rev Clin
Oncol. 6:638–647. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Vanhoefer U, Harstrick A, Achterrath W,
Cao S, Seeber S and Rustum YM: Irinotecan in the treatment of
colorectal cancer: Clinical overview. J Clin Oncol. 19:1501–1518.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Xu T, Qin L, Zhu Z, Wang X, Liu Y, Fan Y,
Zhong S, Wang X, Zhang X, Xia L, et al: MicroRNA-31 functions as a
tumor suppressor and increases sensitivity to mitomycin-C in
urothelial bladder cancer by targeting integrin α5. Oncotarget.
7:27445–27457. 2016.PubMed/NCBI
|
|
11
|
Bae YJ, Yoon YI, Yoon TJ and Lee HJ:
Ultrasound-guided delivery of siRNA and a chemotherapeutic drug by
using microbubble complexes: In vitro and in vivo evaluations in a
prostate cancer model. Korean J Radiol. 17:497–508. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Zhou Q, Ye M, Lu Y, Zhang H, Chen Q, Huang
S and Su S: Curcumin improves the tumoricidal effect of mitomycin C
by suppressing ABCG2 expression in stem cell-like breast cancer
cells. PLoS One. 10:e01366942015. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wei Z, Liang L, Junsong L, Rui C, Shuai C,
Guanglin Q, Shicai H, Zexing W, Jin W, Xiangming C, et al: The
impact of insulin on chemotherapeutic sensitivity to 5-fluorouracil
in gastric cancer cell lines SGC7901, MKN45 and MKN28. J Exp Clin
Cancer Res. 34:642015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Talekar M, Ouyang Q, Goldberg MS and Amiji
MM: Cosilencing of PKM-2 and MDR-1 sensitizes multidrug-resistant
ovarian cancer cells to paclitaxel in a murine model of ovarian
cancer. Mol Cancer Ther. 14:1521–1531. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kenicer J, Spears M, Lyttle N, Taylor KJ,
Liao L, Cunningham CA, Lambros M, MacKay A, Yao C, Reis-Filho J, et
al: Molecular characterisation of isogenic taxane resistant cell
lines identify novel drivers of drug resistance. BMC Cancer.
14:762–772. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Martín AJ, Alfonso PG, Rupérez AB and
Jiménez MM: Nab-paclitaxel plus gemcitabine as first-line
palliative chemotherapy in a patient with metastatic pancreatic
cancer with Eastern Cooperative Oncology Group performance status
of 2. Oncol Lett. 12:727–730. 2016.PubMed/NCBI
|
|
17
|
Ebara S, Kobayashi Y, Sasaki K, Araki M,
Sugimoto M, Wada K, Fujio K, Takamoto A, Watanabe T, Yanai H, et
al: A case of metastatic urachal cancer including a neuroendocrine
component treated with gemcitabine, cisplatin and paclitaxel
combination chemotherapy. Acta Med Okayama. 70:223–227.
2016.PubMed/NCBI
|
|
18
|
Kalaghchi B, Abdi R, Amouzegar-Hashemi F,
Esmati E and Alikhasi A: Concurrent chemoradiation with weekly
paclitaxel and cisplatin for locally advanced cervical cancer.
Asian Pac J Cancer Prev. 17:287–291. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yilmaz A, Alp E, Onen HI and Menevse S:
Reduced BCL2 and CCND1 mRNA expression in human cervical cancer
HeLa cells treated with a combination of everolimus and paclitaxel.
Contemp Oncol (Pozn). 20:28–32. 2016.PubMed/NCBI
|
|
20
|
Trendowski M, Christen TD, Acquafondata C
and Fondy TP: Effects of cytochalasin congeners,
microtubule-directed agents, and doxorubicin alone or in
combination against human ovarian carcinoma cell lines in vitro.
BMC Cancer. 15:632–645. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
van der Noll R, Marchetti S, Steeghs N,
Beijnen JH, Mergui-Roelvink MW, Harms E, Rehorst H, Sonke GS and
Schellens JH: Long-term safety and anti-tumour activity of olaparib
monotherapy after combination with carboplatin and paclitaxel in
patients with advanced breast, ovarian or fallopian tube cancer. Br
J Cancer. 113:396–402. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Huang L, Chen S, Yang W, Xu B, Huang T,
Yang H, Zheng H, Wang Y, Song E, Zhang J, et al: Efficacy and
safety analysis of trastuzumab and paclitaxel based regimen plus
carboplatin or epirubicin as neoadjuvant therapy for clinical stage
II–III, HER2-positive breast cancer patients: A phase 2,
open-label, multicenter, randomized trial. Oncotarget.
6:18683–18692. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Xiao B, Si X, Han MK, Viennois E, Zhang M
and Merlin D: Co-delivery of camptothecin and curcumin by cationic
polymeric nanoparticles for synergistic colon cancer combination
chemotherapy. J Mater Chem B Mater Biol Med. 3:7724–7733. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Tsuda N, Watari H and Ushijima K:
Chemotherapy and molecular targeting therapy for recurrent cervical
cancer. Chin J Cancer Res. 28:241–253. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Schwab CL, English DP, Roque DM and Santin
AD: Taxanes: Their impact on gynecologic malignancy. Anticancer
Drugs. 25:522–535. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wani MC and Horwitz SB: Nature as a
remarkable chemist: A personal story of the discovery and
development of Taxol. Anticancer Drugs. 25:482–487. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Weaver BA: How Taxol/paclitaxel kills
cancer cells. Mol Biol Cell. 25:2677–2681. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zhang D, Yang R, Wang S and Dong Z:
Paclitaxel: New uses for an old drug. Drug Des Devel Ther.
8:279–284. 2014.PubMed/NCBI
|
|
29
|
Takashima S, Kiyoto S, Takahashi M, Hara
F, Aogi K, Ohsumi S, Mukai R and Fujita Y: Clinical experience with
nanoparticle albumin-bound paclitaxel, a novel taxane anticancer
agent, and management of adverse events in females with breast
cancer. Oncol Lett. 9:1822–1826. 2015.PubMed/NCBI
|
|
30
|
Chen NC, Chyau CC, Lee YJ, Tseng HC and
Chou FP: Promotion of mitotic catastrophe via activation of PTEN by
paclitaxel with supplement of mulberry water extract in bladder
cancer cells. Sci Rep. 6:204172016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Zhong ZF, Tan W, Wang SP, Qiang WA and
Wang YT: Anti-proliferative activity and cell cycle arrest induced
by evodiamine on paclitaxel-sensitive and -resistant human ovarian
cancer cells. Sci Rep. 5:164152015. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Liu K, Cang S, Ma Y and Chiao JW:
Synergistic effect of paclitaxel and epigenetic agent phenethyl
isothiocyanate on growth inhibition, cell cycle arrest and
apoptosis in breast cancer cells. Cancer Cell Int. 13:102013.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Takatori E, Shoji T, Kumagai S, Sawai T,
Kurose A and Sugiyama T: Are platinum agents, paclitaxel and
irinotecan effective for clear cell carcinoma of the ovary? DNA
damage detected with γH2AX induced by anticancer agents. J Ovarian
Res. 5:162012. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Harisa GI, Ibrahim MF, Alanazi F and
Shazly GA: Engineering erythrocytes as a novel carrier for the
targeted delivery of the anticancer drug paclitaxel. Saudi Pharm J.
22:223–230. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Wu ZH, Lu MK, Hu LY and Li X: Praziquantel
synergistically enhances paclitaxel efficacy to inhibit cancer cell
growth. PLoS One. 7:e517212012. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Li CM, Lu Y, Chen J, Costello TA,
Narayanan R, Dalton MN, Snyder LM, Ahn S, Li W, Miller DD, et al:
Orally bioavailable tubulin antagonists for paclitaxel-refractory
cancer. Pharm Res. 29:3053–3063. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Oostendorp RL, Buckle T, Lambert G,
Garrigue JS, Beijnen JH, Schellens JH and van Tellingen O:
Paclitaxel in self-micro emulsifying formulations: Oral
bioavailability study in mice. Invest New Drugs. 29:768–776. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Borst P and Schinkel AH: P-glycoprotein
ABCB1: A major player in drug handling by mammals. J Clin Invest.
123:4131–4133. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Sui H, Fan ZZ and Li Q: Signal
transduction pathways and transcriptional mechanisms of
ABCB1/Pgp-mediated multiple drug resistance in human cancer cells.
J Int Med Res. 40:426–435. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Kim H, Park GS, Lee JE and Kim JH: A
leukotriene B4 receptor-2 is associated with paclitaxel resistance
in MCF-7/DOX breast cancer cells. Br J Cancer. 109:351–359. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Ran X, Yang J, Liu C, Zhou P, Xiao L and
Zhang K: MiR-218 inhibits HMGB1-mediated autophagy in endometrial
carcinoma cells during chemotherapy. Int J Clin Exp Pathol.
8:6617–6626. 2015.PubMed/NCBI
|
|
42
|
Yang X, Iyer AK, Singh A, Choy E, Hornicek
FJ, Amiji MM and Duan Z: MDR1 siRNA loaded hyaluronic acid-based
CD44 targeted nanoparticle systems circumvent paclitaxel resistance
in ovarian cancer. Sci Rep. 5:85092015. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Yang X, Iyer AK, Singh A, Milane L, Choy
E, Hornicek FJ, Amiji MM and Duan Z: Cluster of differentiation 44
targeted hyaluronic acid based nanoparticles for MDR1 siRNA
delivery to overcome drug resistance in ovarian cancer. Pharm Res.
32:2097–2109. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Mao K, Liu F, Liu X, Khuri FR, Marcus AI,
Li M and Zhou W: Re-expression of LKB1 in LKB1-mutant EKVX cells
leads to resistance to paclitaxel through the up-regulation of MDR1
expression. Lung Cancer. 88:131–138. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Chen SY, Hu SS, Dong Q, Cai JX, Zhang WP,
Sun JY, Wang TT, Xie J, He HR, Xing JF, et al: Establishment of
paclitaxel-resistant breast cancer cell line and nude mice models,
and underlying multidrug resistance mechanisms in vitro and in
vivo. Asian Pac J Cancer Prev. 14:6135–6140. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Januchowski R, Wojtowicz K,
Sujka-Kordowska P, Andrzejewska M and Zabel M: MDR gene expression
analysis of six drug-resistant ovarian cancer cell lines. BioMed
Res Int. 2013:2417632013. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Wu G, Qin XQ, Guo JJ, Li TY and Chen JH:
AKT/ERK activation is associated with gastric cancer cell
resistance to paclitaxel. Int J Clin Exp Pathol. 7:1449–1458.
2014.PubMed/NCBI
|
|
48
|
Jeong JY, Kim KS, Moon JS, Song JA, Choi
SH, Kim KI, Kim TH and An HJ: Targeted inhibition of phosphatidyl
inositol-3-kinase p110β, but not p110α, enhances apoptosis and
sensitivity to paclitaxel in chemoresistant ovarian cancers.
Apoptosis. 18:509–520. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Liu Z, Zhu G, Getzenberg RH and Veltri RW:
The upregulation of PI3K/Akt and MAP kinase pathways is associated
with resistance of microtubule-targeting drugs in prostate cancer.
J Cell Biochem. 116:1341–1349. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Mei M, Xie D, Zhang Y, Jin J, You F, Li Y,
Dai J and Chen X: A new
2α,5α,10β,14β-tetraacetoxy-4(20),11-taxadiene (SIA) derivative
overcomes paclitaxel resistance by inhibiting MAPK signaling and
increasing paclitaxel accumulation in breast cancer cells. PLoS
One. 9:e1043172014. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Zhou M, Fan C and Tian N: Effects of
curcumin on the gene expression profile of L-02 cells. Biomed Rep.
3:519–526. 2015.PubMed/NCBI
|
|
52
|
Zhang Y, Liang D, Dong L, Ge X, Xu F, Chen
W, Dai Y, Li H, Zou P, Yang S, et al: Anti-inflammatory effects of
novel curcumin analogs in experimental acute lung injury. Respir
Res. 16:432015. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Fan Z, Yao J, Li Y, Hu X, Shao H and Tian
X: Anti-inflammatory and antioxidant effects of curcumin on acute
lung injury in a rodent model of intestinal ischemia reperfusion by
inhibiting the pathway of NF-κB. Int J Clin Exp Pathol.
8:3451–3459. 2015.PubMed/NCBI
|
|
54
|
Ferreira VH, Nazli A, Dizzell SE, Mueller
K and Kaushic C: The anti-inflammatory activity of curcumin
protects the genital mucosal epithelial barrier from disruption and
blocks replication of HIV-1 and HSV-2. PLoS One. 10:e01249032015.
View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Robles-Escajeda E, Das U, Ortega NM, Parra
K, Francia G, Dimmock JR, Varela-Ramirez A and Aguilera RJ: A novel
curcumin-like dienone induces apoptosis in triple-negative breast
cancer cells. Cell Oncol (Dordr). 39:265–277. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Park W, Amin AR, Chen ZG and Shin DM: New
perspectives of curcumin in cancer prevention. Cancer Prev Res
(Phila). 6:387–400. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Zhou H, Beevers CS and Huang S: The
targets of curcumin. Curr Drug Targets. 12:332–347. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Philip M, Rowley DA and Schreiber H:
Inflammation as a tumor promoter in cancer induction. Semin Cancer
Biol. 14:433–439. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Cao F, Liu T, Xu Y, Xu D and Feng S:
Curcumin inhibits cell proliferation and promotes apoptosis in
human osteoclastoma cell through MMP-9, NF-κB and JNK signaling
pathways. Int J Clin Exp Pathol. 8:6037–6045. 2015.PubMed/NCBI
|
|
60
|
Bansal SS, Goel M, Aqil F, Vadhanam MV and
Gupta RC: Advanced drug delivery systems of curcumin for cancer
chemoprevention. Cancer Prev Res (Phila). 4:1158–1171. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Guan F, Ding Y, Zhang Y, Zhou Y, Li M and
Wang C: Curcumin suppresses proliferation and migration of
MDA-MB-231 breast cancer cells through autophagy-dependent Akt
degradation. PLoS One. 11:e01465532016. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Collett GP and Campbell FC: Curcumin
induces c-jun N-terminal kinase-dependent apoptosis in HCT116 human
colon cancer cells. Carcinogenesis. 25:2183–2189. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Li X, Lu Y, Jin Y, Son JK, Lee SH and
Chang HW: Curcumin inhibits the activation of immunoglobulin
e-mediated mast cells and passive systemic anaphylaxis in mice by
reducing serum eicosanoid and histamine levels. Biomol Ther
(Seoul). 22:27–34. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Liu D and Chen Z: The effect of curcumin
on breast cancer cells. J Breast Cancer. 16:133–137. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Astuti PD, Utami E, Nugrahani AW and
Sudjadi S: Genistein abrogates G2 arrest induced by curcumin in p53
deficient T47D cells. Daru. 20:822012. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Cheng C, Jiao JT, Qian Y, Guo XY, Huang J,
Dai MC, Zhang L, Ding XP, Zong D and Shao JF: Curcumin induces G2/M
arrest and triggers apoptosis via FoxO1 signaling in U87 human
glioma cells. Mol Med Rep. 13:3763–3770. 2016.PubMed/NCBI
|
|
67
|
Eom DW, Lee JH, Kim YJ, Hwang GS, Kim SN,
Kwak JH, Cheon GJ, Kim KH, Jang HJ, Ham J, et al: Synergistic
effect of curcumin on epigallocatechin gallate-induced anticancer
action in PC3 prostate cancer cells. BMB Rep. 48:461–466. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Xiao J, Chu Y, Hu K, Wan J, Huang Y, Jiang
C, Liang G and Li X: Synthesis and biological analysis of a new
curcumin analogue for enhanced anti-tumor activity in HepG 2 cells.
Oncol Rep. 23:1435–1441. 2010.PubMed/NCBI
|
|
69
|
Zhang Y, Jiang X, Peng K, Chen C, Fu L,
Wang Z, Feng J, Liu Z, Zhang H, Liang G, et al: Discovery and
evaluation of novel anti-inflammatory derivatives of natural
bioactive curcumin. Drug Des Devel Ther. 8:2161–2171.
2014.PubMed/NCBI
|
|
70
|
Zhang Y, Zhao C, He W, Wang Z, Fang Q,
Xiao B, Liu Z, Liang G and Yang S: Discovery and evaluation of
asymmetrical monocarbonyl analogs of curcumin as anti-inflammatory
agents. Drug Des Devel Ther. 8:373–382. 2014.PubMed/NCBI
|
|
71
|
Olivera A, Moore TW, Hu F, Brown AP, Sun
A, Liotta DC, Snyder JP, Yoon Y, Shim H, Marcus AI, et al:
Inhibition of the NF-κB signaling pathway by the curcumin analog,
3,5-Bis(2-pyridinylmethylidene)-4-piperidone (EF31):
Anti-inflammatory and anti-cancer properties. Int Immunopharmacol.
12:368–377. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Torre LA, Bray F, Siegel RL, Ferlay J,
Lortet-Tieulent J and Jemal A: Global cancer statistics, 2012. CA
Cancer J Clin. 65:87–108. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Balanda M, Quiero A, Vergara N, Espinoza
G, Martín HS, Rojas G and Ramírez E: Prevalence of human
papillomavirus infection among women presenting for cervical cancer
screening in Chile, 2014–2015. Med Microbiol Immunol (Berl).
205:585–594. 2016. View Article : Google Scholar
|
|
74
|
Bava SV, Puliappadamba VT, Deepti A, Nair
A, Karunagaran D and Anto RJ: Sensitization of taxol-induced
apoptosis by curcumin involves down-regulation of nuclear
factor-kappaB and the serine/threonine kinase Akt and is
independent of tubulin polymerization. J Biol Chem. 280:6301–6308.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Bava SV, Sreekanth CN, Thulasidasan AKT,
Anto NP, Cheriyan VT, Puliyappadamba VT, Menon SG, Ravichandran SD
and Anto RJ: Akt is upstream and MAPKs are downstream of NF-κB in
paclitaxel-induced survival signaling events, which are
down-regulated by curcumin contributing to their synergism. Int J
Biochem Cell Biol. 43:331–341. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Sreekanth CN, Bava SV, Sreekumar E and
Anto RJ: Molecular evidences for the chemosensitizing efficacy of
liposomal curcumin in paclitaxel chemotherapy in mouse models of
cervical cancer. Oncogene. 30:3139–3152. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Dang YP, Yuan XY, Tian R, Li DG and Liu W:
Curcumin improves the paclitaxel-induced apoptosis of HPV-positive
human cervical cancer cells via the NF-κB-p53-caspase-3 pathway.
Exp Ther Med. 9:1470–1476. 2015.PubMed/NCBI
|
|
78
|
Punfa W, Suzuki S, Pitchakarn P, Yodkeeree
S, Naiki T, Takahashi S and Limtrakul P: Curcumin-loaded PLGA
nanoparticles conjugated with anti-P-glycoprotein antibody to
overcome multidrug resistance. Asian Pac J Cancer Prev.
15:9249–9258. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Faião-Flores F, Suarez JAQ, Pardi PC and
Maria DA: DM-1, sodium
4-(5-(4-hydroxy-3-methoxyphenyl)-3-oxo-penta-1,4-dienyl)-2-methoxy-phenolate:
A curcumin analog with a synergic effect in combination with
paclitaxel in breast cancer treatment. Tumour Biol. 33:775–785.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Banerjee M, Singh P and Panda D: Curcumin
suppresses the dynamic instability of microtubules, activates the
mitotic checkpoint and induces apoptosis in MCF-7 cells. FEBS J.
277:3437–3448. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Zhan Y, Chen Y, Liu R, Zhang H and Zhang
Y: Potentiation of paclitaxel activity by curcumin in human breast
cancer cell by modulating apoptosis and inhibiting EGFR signaling.
Arch Pharm Res. 37:1086–1095. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Boztas AO, Karakuzu O, Galante G, Ugur Z,
Kocabas F, Altuntas CZ and Yazaydin AO: Synergistic interaction of
paclitaxel and curcumin with cyclodextrin polymer complexation in
human cancer cells. Mol Pharm. 10:2676–2683. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Thadakapally R, Aafreen A, Aukunuru J,
Habibuddin M and Jogala S: Preparation and characterization of
PEG-albumin-curcumin nanoparticles intended to treat breast cancer.
Indian J Pharm Sci. 78:65–72. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Royt M, Mukherjee S, Sarkar R and Biswas
J: Curcumin sensitizes chemotherapeutic drugs via modulation of
PKC, telomerase, NF-kappaB and HDAC in breast cancer. Ther Deliv.
2:1275–1293. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Aggarwal BB, Shishodia S, Takada Y,
Banerjee S, Newman RA, Bueso-Ramos CE and Price JE: Curcumin
suppresses the paclitaxel-induced nuclear factor-kappaB pathway in
breast cancer cells and inhibits lung metastasis of human breast
cancer in nude mice. Clin Cancer Res. 11:7490–7498. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Kang HJ, Lee SH, Price JE and Kim LS:
Curcumin suppresses the paclitaxel-induced nuclear factor-kappaB in
breast cancer cells and potentiates the growth inhibitory effect of
paclitaxel in a breast cancer nude mice model. Breast J.
15:223–229. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Wang J, Wang F, Li F, Zhang W, Shen Y,
Zhou D and Guo S: A multifunctional poly(curcumin) nanomedicine for
dual-modal targeted delivery, intracellular responsive release,
dual-drug treatment and imaging of multidrug resistant cancer
cells. J Mater Chem B Mater Biol Med. 4:2954–2962. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Ganta S, Devalapally H and Amiji M:
Curcumin enhances oral bioavailability and anti-tumor therapeutic
efficacy of paclitaxel upon administration in nanoemulsion
formulation. J Pharm Sci. 99:4630–4641. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Innamaa A, Jackson L, Asher V, van
Schalkwyk G, Warren A, Keightley A, Hay D, Bali A, Sowter H and
Khan R: Expression and effects of modulation of the K2P potassium
channels TREK-1 (KCNK2) and TREK-2 (KCNK10) in the normal human
ovary and epithelial ovarian cancer. Clin Transl Oncol. 15:910–918.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Deng S, Xu J, Li R and Zhou Q: Inhibitory
effect of curcumin-loaded solid lipid nanoparticles combined with
paclitaxel on human ovarian cancer cell line HO-8910. China
Pharmacy. 24:1756–1759. 2013.http://en.cnki.com.cn/Article_en/CJFDTOTAL-ZGYA201319013.htm
|
|
91
|
Abouzeid AH, Patel NR, Sarisozen C and
Torchilin VP: Transferrin-targeted polymeric micelles co-loaded
with curcumin and paclitaxel: Efficient killing of
paclitaxel-resistant cancer cells. Pharm Res. 31:1938–1945. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Liu Z, Zhu YY, Li ZY and Ning SQ:
Evaluation of the efficacy of paclitaxel with curcumin combination
in ovarian cancer cells. Oncol Lett. 12:3944–3948. 2016.PubMed/NCBI
|
|
93
|
Kar R, Sharma C, Sen S, Jain SK, Gupta SD
and Singh N: Response of primary culture of human ovarian cancer
cells to chemotherapy: In vitro individualized therapy. J Cancer
Res Ther. 12:1050–1055. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Galia A, Calogero AE, Condorelli R,
Fraggetta F, La Corte A, Ridolfo F, Bosco P, Castiglione R and
Salemi M: PARP-1 protein expression in glioblastoma multiforme. Eur
J Histochem. 56:e92012. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Hossain M, Banik NL and Ray SK:
Synergistic anti-cancer mechanisms of curcumin and paclitaxel for
growth inhibition of human brain tumor stem cells and LN18 and
U138MG cells. Neurochem Int. 61:1102–1113. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Manju S, Sharma CP and Sreenivasan K:
Targeted coadministration of sparingly soluble paclitaxel and
curcumin into cancer cells by surface engineered magnetic
nanoparticles. J Mater Chem. 21:15708–15717. 2011. View Article : Google Scholar
|
|
97
|
Cui Y, Zhang M, Zeng F, Jin H, Xu Q and
Huang Y: Dual-targeting magnetic PLGA Nanoparticles for codelivery
of paclitaxel and curcumin for brain tumor therapy. ACS Appl Mater
Interfaces. 8:32159–32169. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Kamat AM, Sethi G and Aggarwal BB:
Curcumin potentiates the apoptotic effects of chemotherapeutic
agents and cytokines through down-regulation of nuclear
factor-kappaB and nuclear factor-kappaB-regulated gene products in
IFN-alpha-sensitive and IFN-alpha-resistant human bladder cancer
cells. Mol Cancer Ther. 6:1022–1030. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Zhao H, Yu X, Qi R, Shang F and Su Z:
Inhibitory effects of curcumin in combination with paclitaxel on
prostate cancer xenografted model. Xiandai Shengwu Yixue Jinzhan.
10:823–827. 2010.(In Chinese).
|
|
100
|
Wand D, Qi R, Zhao H and Yu X: Effects of
curcumin combined with paclitaxel on the invasion and senescence of
human prostatic carcinoma PC3 cells. Xiandai Shengwu Yixue Jinzhan.
12:6239–6241. 2012.(In Chinese).
|
|
101
|
Huang YT, Huang DM, Chueh SC, Teng CM and
Guh JH: Alisol B acetate, a triterpene from Alismatis rhizoma,
induces Bax nuclear translocation and apoptosis in human
hormone-resistant prostate cancer PC-3 cells. Cancer Lett.
231:270–278. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Thomas SL, Zhong D, Zhou W, Malik S,
Liotta D, Snyder JP, Hamel E and Giannakakou P: EF24, a novel
curcumin analog, disrupts the microtubule cytoskeleton and inhibits
HIF-1. Cell Cycle. 7:2409–2417. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Mathur A, Abd Elmageed ZY, Liu X,
Kostochka ML, Zhang H, Abdel-Mageed AB and Mondal D: Subverting
ER-stress towards apoptosis by nelfinavir and curcumin coexposure
augments docetaxel efficacy in castration resistant prostate cancer
cells. PLoS One. 9:e1031092014. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Yang JD and Roberts LR: Hepatocellular
carcinoma: A global view. Nat Rev Gastroenterol Hepatol. 7:448–458.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Wei KR, Yu X, Zheng RS, Peng XB, Zhang SW,
Ji MF, Liang ZH, Ou ZX and Chen WQ: Incidence and mortality of
liver cancer in China, 2010. Chin J Cancer. 33:388–394.
2014.PubMed/NCBI
|
|
106
|
Byam J, Renz J and Millis JM: Liver
transplantation for hepatocellular carcinoma. Hepatobiliary Surg
Nutr. 2:22–30. 2013.PubMed/NCBI
|
|
107
|
Zhou M, Li Z, Han Z and Tian N:
Paclitaxel-sensitization enhanced by curcumin involves
down-regulation of nuclear factor-κB and Lin28 in Hep3B cells. J
Recept Signal Transduct Res. 35:618–625. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
O'Day E, Le MTN, Imai S, Tan SM, Kirchner
R, Arthanari H, Hofmann O, Wagner G and Lieberman J: An RNA-binding
protein, Lin28, recognizes and remodels g-quartets in the microRNAs
(miRNAs) and mRNAs it regulates. J Biol Chem. 290:17909–17922.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Dubey AK, Gupta U and Jain S: Epidemiology
of lung cancer and approaches for its prediction: A systematic
review and analysis. Chin J Cancer. 35:71–83. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Muthoosamy K, Abubakar IB, Bai RG, Loh HS
and Manickam S: Exceedingly higher co-loading of curcumin and
paclitaxel onto polymer-functionalized reduced graphene oxide for
highly potent synergistic anticancer treatment. Sci Rep.
6:328082016. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Su GM, Davey MW and Davey RA: Induction of
broad drug resistance in small cell lung cancer cells and its
reversal by paclitaxel. Int J Cancer. 76:702–708. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Dhillon N, Aggarwal BB, Newman RA, Wolff
RA, Kunnumakkara AB, Abbruzzese JL, Ng CS, Badmaev V and Kurzrock
R: Phase II trial of curcumin in patients with advanced pancreatic
cancer. Clin Cancer Res. 14:4491–4499. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Epelbaum R, Schaffer M, Vizel B, Badmaev V
and Bar-Sela G: Curcumin and gemcitabine in patients with advanced
pancreatic cancer. Nutr Cancer. 62:1137–1141. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Irving GR, Iwuji CO, Morgan B, Berry DP,
Steward WP, Thomas A, Brown K and Howells LM: Combining curcumin
(C3-complex, Sabinsa) with standard care FOLFOX chemotherapy in
patients with inoperable colorectal cancer (CUFOX): Study protocol
for a randomised control trial. Trials. 16:1102015. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Bayet-Robert M, Kwiatkowski F, Leheurteur
M, Gachon F, Planchat E, Abrial C, Mouret-Reynier MA, Durando X,
Barthomeuf C and Chollet P: Phase I dose escalation trial of
docetaxel plus curcumin in patients with advanced and metastatic
breast cancer. Cancer Biol Ther. 9:8–14. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Mahammedi H, Planchat E, Pouget M, Durando
X, Curé H, Guy L, Van-Praagh I, Savareux L, Atger M, Bayet-Robert
M, et al: The new combination docetaxel, prednisone and curcumin in
patients with castration-resistant prostate cancer: A pilot phase
II study. Oncology. 90:69–78. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Kanai M, Otsuka Y, Otsuka K, Sato M,
Nishimura T, Mori Y, Kawaguchi M, Hatano E, Kodama Y, Matsumoto S,
et al: A phase I study investigating the safety and
pharmacokinetics of highly bioavailable curcumin (Theracurmin) in
cancer patients. Cancer Chemother Pharmacol. 71:1521–1530. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Storka A, Vcelar B, Klickovic U, Gouya G,
Weisshaar S, Aschauer S, Bolger G, Helson L and Wolzt M: Safety,
tolerability and pharmacokinetics of liposomal curcumin in healthy
humans. Int J Clin Pharmacol Ther. 53:54–65. 2015. View Article : Google Scholar : PubMed/NCBI
|