Introduction
Colorectal cancer (CRC) is the third most common
cancer and the second leading cause of cancer-associated
mortalities worldwide (1). The
incidence rate of CRC in China has been nearly three-fold lower
than that in Europe (2,3); however, its incidence has increased
rapidly in recent years (4,5). CRC is more frequent in patients ranged
40–70 years old; however, an increasing number of patients are
diagnosed with CRC under 40 years of age (6). Currently, the underlying mechanism of
CRC carcinogenesis remains unclear. Due to improvement in early
detection and surgical treatment, the prognosis of patients with
CRC with localized tumors has been significantly enhanced (7). However, the prognosis for patients
with advanced tumors remains poor (8). Moreover, although clinical staging is
useful to some extent to predict CRC prognosis, patient outcomes
can vary significantly even for patients with similar clinical
features (9). Heterogeneity in
somatic or germline changes may substantially affect patient
prognosis.
Altered mRNA expression of genes involved in tumor
proliferation, autophagy and transcription has been reported to
play an important role in predicting the onset or survival outcome
of CRC (10–12). However, the number of studies
investigating mRNAs in order to predict the onset and prognosis of
CRC remains limited. A previous study reported that
cyclooxygenase-2 mRNA upregulation was associated with CRC
carcinogenesis using reverse transcription-quantitative PCR
(RT-qPCR) based on 60 CRC tumor tissues and normal tissues
(13). Another study reported that
increased expression of rabaptin-5-associated exchange factor mRNA
was associated with poor survival of CRC using RT-qPCR and survival
analysis based on 187 CRC tumor tissues (14). Wang et al (15) established a 31-gene expression
classifier to predict CRC recurrence using a gene expression
microarray based on 281 CRC samples. However, these studies
evaluated only a single clinical outcome (progression or
prognosis), and lacked laboratory-based validation experiments,
restricting the possible application of these reported mRNAs in
clinical practices. Therefore, it is imperative to identify and
validate key mRNAs associated with the carcinogenesis and prognosis
of CRC in order to further facilitate the development of new
targeted therapies.
Substantial developments in high-throughput
transcriptome sequencing and microarray technologies have provided
opportunities to identify novel mRNA biomarkers associated with the
tumorigenesis and prognosis of CRC. In the present study,
differential expression analysis was performed to explore critical
genes in CRC. Survival analysis was performed to evaluate the
prognostic value of TNNT2. Functional enrichment analysis
was employed to explore the potential biological processes involved
in CRC tumorigenesis and prognosis. Epidermal growth factor
receptor (EGFR) is a key factor for the ErbB signaling pathway
involved in tumor growth (16,17).
In addition, Fatty acid synthase (Fasn) is the key metabolic enzyme
that accounts for the glycerophospholipid metabolism pathway to
regulate the proliferation and migration in various tumors
(18,19). Therefore, EGFR and Fasn were
selected as a biomarker for the two respective signaling pathways.
RT-qPCR and western blotting were conducted to measure the mRNA and
protein expression levels of TNNT2 between CRC tumor and
normal cells. The protein expression of TNNT2 in CRC and
normal tissues was detected via immunohistochemistry.
In summary, the present study investigated the
expression of TNNT2 at the mRNA and protein level in CRC and
clarified the correlation between the TNNT2 expression and
clinicopathological parameters.
Materials and methods
Data sources
The data of CRC tumor and adjacent normal tissue
samples were obtained from The Cancer Genome Atlas (TCGA;
www.cancergenome.nih.gov) and the Gene
Expression Omnibus (GEO; https://www.ncbi.nlm.nih.gov/geo/; Access number:
GSE17537) databases. The TCGA-CRC dataset contained a total of 512
CRC samples, including 471 tumor samples and 41 adjacent normal
samples. The age of the samples is from 41 to 90 with the median
age of 68. Numbers of female and male patients is 212 and 235,
respectively. The GEO dataset contained 55 CRC tumor samples. The
age of those 55 patients is from 23 to 94 with the median age of
61. Numbers of female and male patients is 29 and 26,
respectively.
Differential expression analysis
Differential expression analysis was performed on
the TCGA-CRC dataset using edgeR package in R v. 3.5.3 software
(20). First, genes were excluded
with average counts <10. Then the samples were divided into
normal tissue group (N) and tumor tissue group (T) according to the
sample type. A false discovery rate (FDR) <0.05 and |log2 fold
change (FC)| >1 were set as the criteria for screening
differentially expressed genes.
Gene set enrichment analysis
(GSEA)
GSEA (version 2.2) was conducted for functional
enrichment analysis (21). The
selected gene set was Kyoto Encyclopedia of Genes and Genomes
(KEGG) pathway. P<0.05 was set as the threshold for screening
significantly enriched KEGG pathways.
Cell culture
The normal colorectal cell line FHC, colon cancer
cell line LoVo, CRC cell line SW620, and colon cancer cell line
SW1116 were purchased from BeNa Culture Collection. FHC, LoVo,
SW620 and SW1116 cells were cultured in DMEM (Gibco; Thermo Fisher
Scientific, Inc.), DMEM/F12 (Gibco; Thermo Fisher Scientific,
Inc.), DMEM/F-12K (Gibco; Thermo Fisher Scientific, Inc.) and
DMEM/L-15 (Gibco; Thermo Fisher Scientific, Inc.) containing 10%
fetal bovine serum (FBS; Hyclone; GE Healthcare Life Sciences) and
1% penicillin/streptomycin (Hyclone; GE Healthcare Life Sciences),
respectively. The cells were incubated at 37°C with 5%
CO2.
Overexpression of TNNT2
RNA was extracted from LoVo cells using Trizol
reagent (Thermo Fisher Scientific, Inc.). cDNA was synthesized by
TransScript® Two-Step RT-PCR SuperMix (TransGen
Biotech). ORF sequence of TNNT2 was amplified via RT-PCR
according to the manufacturer's instructions of
2×TransTaq® HiFi PCR SuperMix II (TransGen Biotech).
TNNT2 primer sequences were as follows: Forward,
5′-ATGTCTGACATAGAAGAGGTGGTGG-3′ and reverse,
5′-CTATTTCCAGCGCCCGGTGACTTTA-3′. PCR reaction condition was as
follows: 94°C 3 min, 1 cycle, 94°C 30 sec, 55°C 30 sec, 72°C 3 min,
35 cycles and 72°C 10 min, 1 cycle. Then PCR products were inserted
into the pCMV-Myc vector (Biovector Co., Ltd.) to construct the
expression vector pCMV-Myc-TNNT2. LoVo, SW620 and SW1116
cells were transfected with 16 µg/ml pCMV-Myc-TNNT2 using
Lipofectamine 2000 (Thermo Fisher Scientific, Inc.) for 48 h
according to the manufacturer's instructions.
RT-qPCR
Total RNA of FHC, LoVo, SW620 and SW1116 cells was
extracted using Trizol (Invitrogen; Thermo Fisher Scientific,
Inc.). The purity and concentration of RNA were determined via
NanoDrop ND-2000 spectrophotometer (NanoDrop Technologies; Thermo
Fisher Scientific, Inc.). Then the RNA was reverse transcribed into
cDNA using TransScript® Two-Step RT-PCR SuperMix
(TransGen Biotech) according to the manufacturer's instructions.
RT-qPCR was performed according to the manufacturer's instructions
of the SYBR Premix Ex Taq kit (Roche Diagnostics), with GAPDH used
as the internal reference. The thermocycling conditions were as
follows: Step 1, 95°C for 5 min; step 2, 95°C for 30 sec; step 3,
58–65°C for 30 sec; step 4, 72°C for 30 sec; step 5, repeat from
step 2 for 34 cycles; step 6, 72°C for 10 min. The relative
expression of TNNT2 was calculated using the
2−ΔΔCq method. The primer sequences of RT-qPCR are
listed in Table I.
 | Table I.Primer sequences for reverse
transcription-quantitative PCR. |
Table I.
Primer sequences for reverse
transcription-quantitative PCR.
| Gene | Primer sequence
(5′→3′) |
|---|
| TNNT2 | F:
TTCACCAAAGATCTGCTCCTCGCT |
|
| R:
TTATTACTGGTGTGGAGTGGGTGTGG |
| EGFR | F:
TCCCTCAGCCACCCATATGTAC |
|
| R:
GTCTCGGGCCATTTTGGAGAATTC |
| Fasn | F:
ATGCGGGACAGAGCAACTACGG |
|
| R:
CAGCCTTCTCAGCCAGCACAAA |
| GAPDH | F:
GGTGAAGGTCGGTGTGAACG |
|
| R:
CTCGCTCCTGGAAGATGGTG |
Western blotting
The cells were lysed using RIPA solution and then
total proteins were extracted. The proteins were quantified using
bovine serum albumin (BSA; Boster Biological Technology Co., Ltd).
The protein samples were electrophoresed on 10% SDS-PAGE and
transferred onto PVDF membranes. After blocking with 1X Blotto
(Thermo Fisher Scientific, Inc.) for 2 h at room temperature, the
membranes were incubated with anti-Cardiac Troponin T antibody
(cat. no. ab91605; 1:1,000; Abcam) and anti-GAPDH antibody (cat.
no. ab8245; 1:1,000; Abcam) at 4°C overnight. After washing with
TBST three times at room temperature, the membranes were incubated
with horseradish peroxidase (HRP)-labeled goat anti-rabbit IgG as
the secondary antibody (cat. no. ab6728; 1:1,000; Abcam) for 1.5 h
at room temperature. The proteins were visualized using Western
Lightning™ Chemiluminescence reagent (PerkinElmer, Inc.), and
densitometric analysis was conducted using LabWorks™ 4.6 (UVP,
LLC). GAPDH was used as the internal control.
Immunohistochemistry
The CRC and normal tissues were fixed using 4%
paraformaldehyde at 4°C overnight, embedded with paraffin, and
sliced into 3–5 µm sections, followed by dewaxing. After antigen
retrieval by microwave, the sections were blocked with 10% normal
goat serum (Beijing Solarbio Science & Technology Co., Ltd.)
and incubated at room temperature for 20 min. Then the primary
antibody rabbit anti-cardiac troponin T (cat. no. ab91605; Abcam)
were added for an incubation at 4°C overnight. The biotin-labeled
IgG (cat. no. Sp-9001; 1: 1,000; OriGene Technologies, Inc.) was
used as secondary antibody for 30 min at room temperature. After
development in DAB and counterstaining with hematoxylin for 5 min
at room temperature, the sections were sealed with resinene. Five
fields were randomly selected and imaged under an optical
microscope (BX51T-PHD-J11, Olympus Corporation). The images were
analyzed using Image-Pro Plus (Media Cybernetics, Inc.).
Statistical analysis
Cox regression analysis was performed by using
survival and survminer packages in R software (22). Clinical factors, including age, sex,
TNM staging system [American Joint Committee on Cancer (AJCC)
(23) and the International Union
Against Cancer (UICC) (24)] and
gene expression levels, were adjusted in the Cox regression model.
P<0.1 was set as the threshold to screen factors significantly
associated with CRC survival. Kaplan-Meier analysis was performed
by stratifying CRC patients according to median TNNT2
expression. Data were presented as the mean ± SEM, n=3. The
significance was assessed via one-way ANOVA (with Tukey's post hoc
analysis). Statistical analysis was performed using GraphPad Prism
Version 5.0 software (GraphPad Software, Inc.).
Results
TNNT2 is upregulated in CRC samples
compared with paracancerous samples
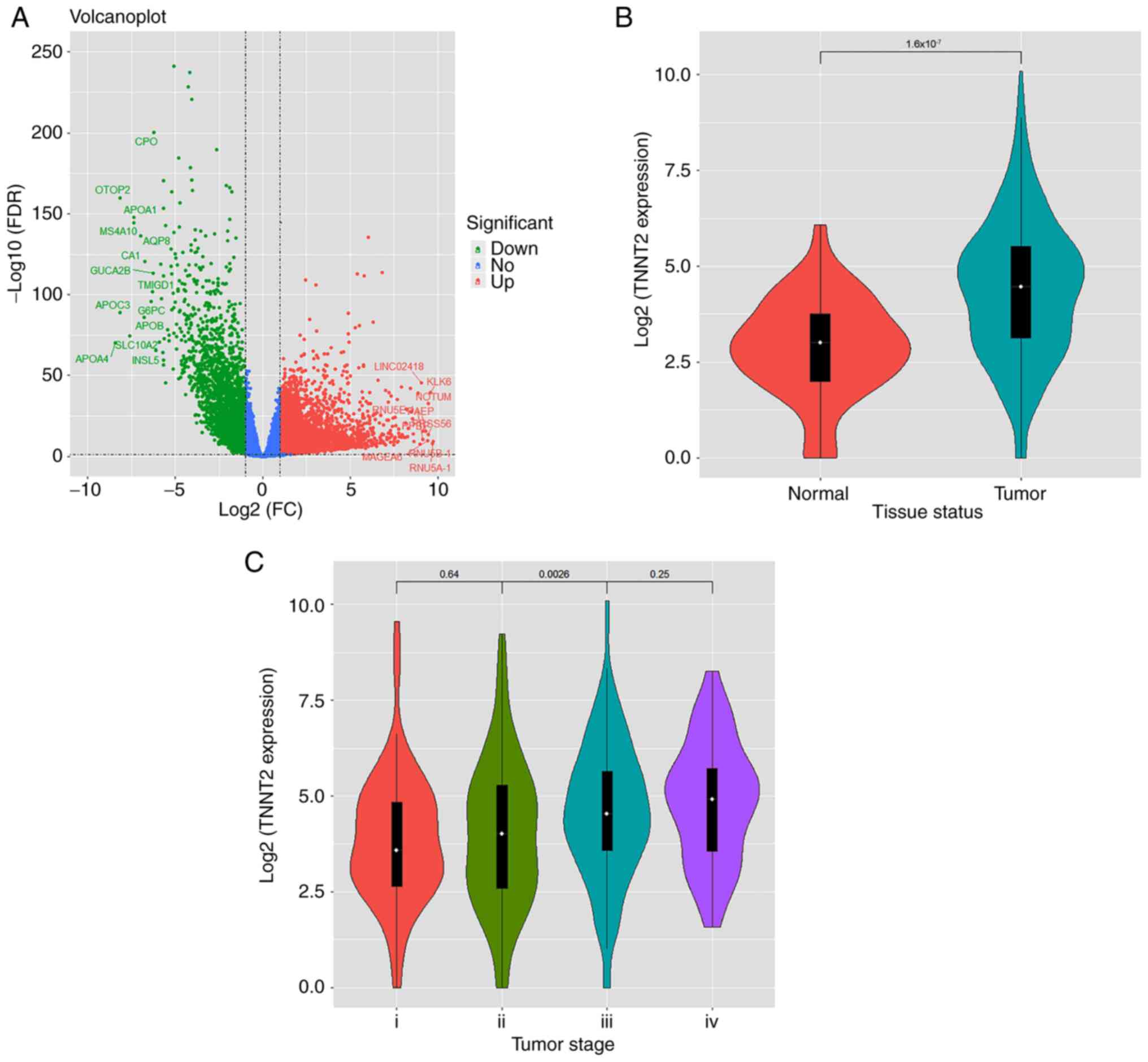
A total of 2,703 downregulated genes and 4,001
upregulated genes between CRC tumor samples and paracancerous
samples were identified. The volcano blot is presented in Fig. 1A. Analysis of these differentially
expressed genes revealed that TNNT2 was significantly
upregulated in CRC tumor samples vs. adjacent normal samples, as
indicated by Fig. 1B
(P=1.6×10−7). Furthermore, there was a positive
association between TNNT2 gene expression with the stages of
patients with CRC, especially between stage II and stage III, as
indicated in Fig. 1C (P=0.0026). As
the association between TNNT2 and CRC has not been
investigated in previous studies, TNNT2 was selected as the
key candidate gene, and the association of TNNT2 with the
progression and prognosis of CRC was investigated.
Elevated TNNT2 is associated with poor
prognosis in CRC
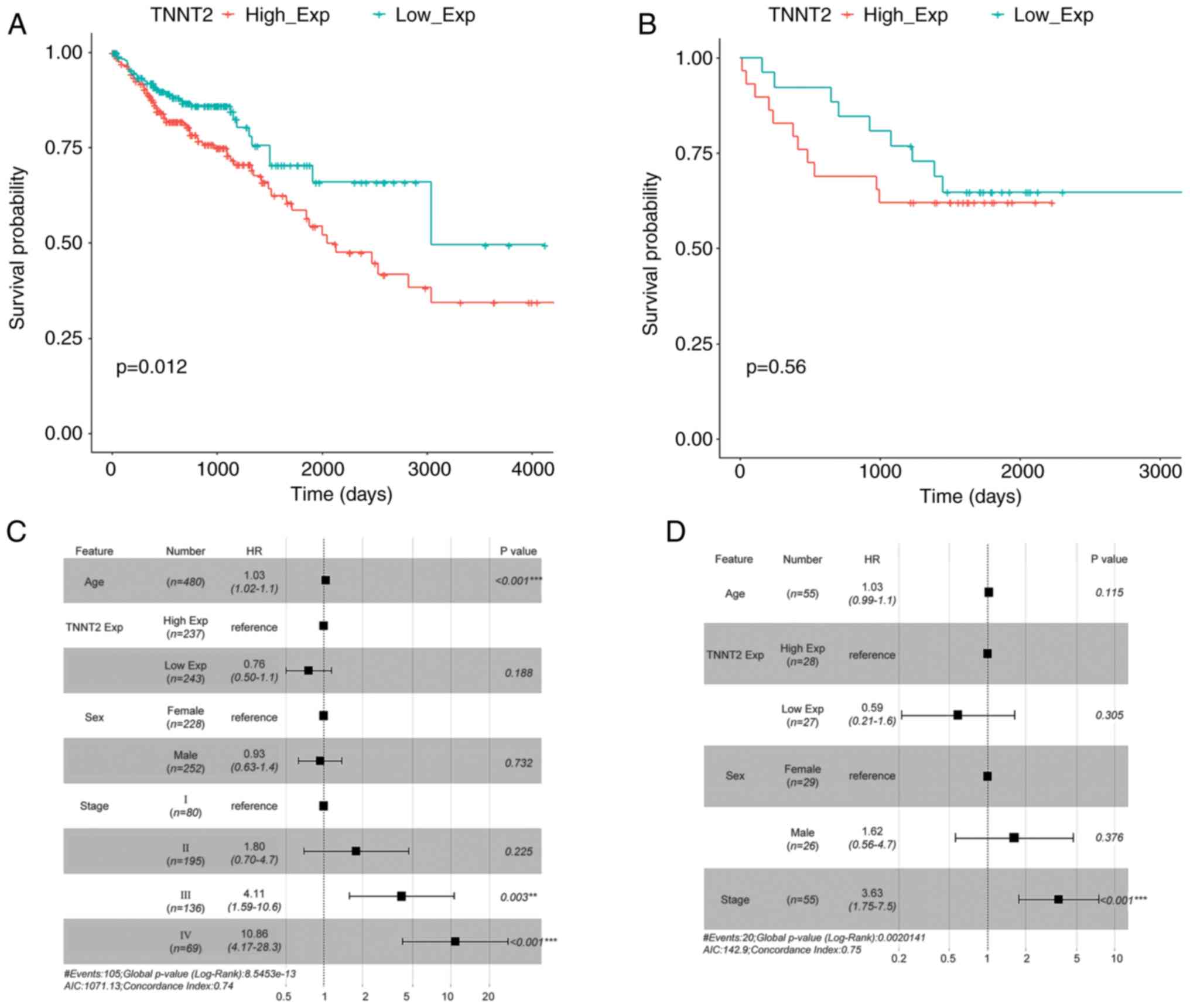
CRC samples were divided into a high- and
low-expression group according to the median level of TNNT2
expression which was 4.82 (log2-based) according to the survival
package. The survival curve was plotted using survminer package
(Fig. 2A). It was revealed that the
expression level of TNNT2 had a significant effect on
survival outcome (P=0.012). Moreover, a Cox regression model was
constructed adjusting for age, sex, staging and TNNT2
expression level (high or low) (Fig.
2C). It was revealed that compared with the high-TNNT2
expression group, the low-expression group exhibited a more
favorable survival outcome. Additionally, patients with CRC with
higher stages had a higher risk of mortality.
Validation of the prognostic effect of
TNNT2 in a GEO cohort
The same method was utilized for the survival
analysis to verify the association of TNNT2 expression with
survival in GEO dataset GSE17537. The survival curve suggested that
different expression levels of TNNT2 had an effect on
survival in patients with CRC, but the difference was not
statistically significant (P=0.56). The Cox regression analysis
indicated that the TNNT2 low expression group had a lower
risk of mortality compared with the high expression group, and
patients at higher stages had a higher risk of mortality (Fig. 2B and D).
Significantly enriched pathways in CRC
samples with high TNNT2 expression
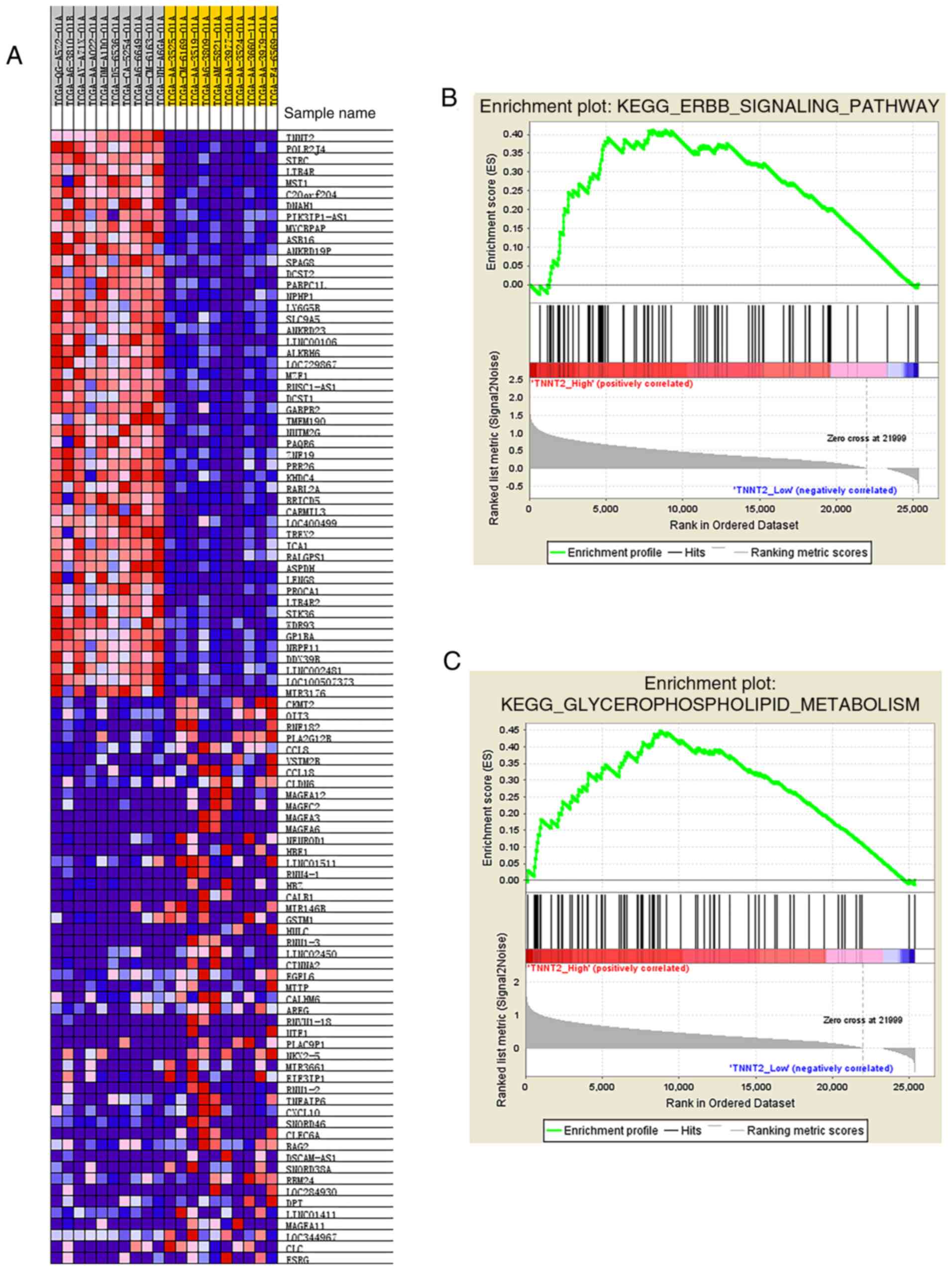
According to the median expression level of
TNNT2, CRC samples were stratified into high and low
expression groups, and then differential expression analysis was
performed. A total of 784 differentially expressed genes were
identified, of which 163 genes were downregulated and 621 genes
were upregulated. The top 100 differentially expressed genes within
down- and upregulated gene sets were selected, respectively. A
heatmap was constructed comprising the 200 selected genes in 10 CRC
samples with the highest and lowest TNNT2 expression,
respectively (Fig. 3A). According
to the functional enrichment analysis, the ‘ErbB signaling pathway’
and ‘glycerophospholipid metabolism pathway’ were significantly
activated in the high TNNT2 expression group (Fig. 3B).
TNNT2 overexpression upregulates the
ErbB signaling and glycerophospholipid metabolism pathways in CRC
cell lines
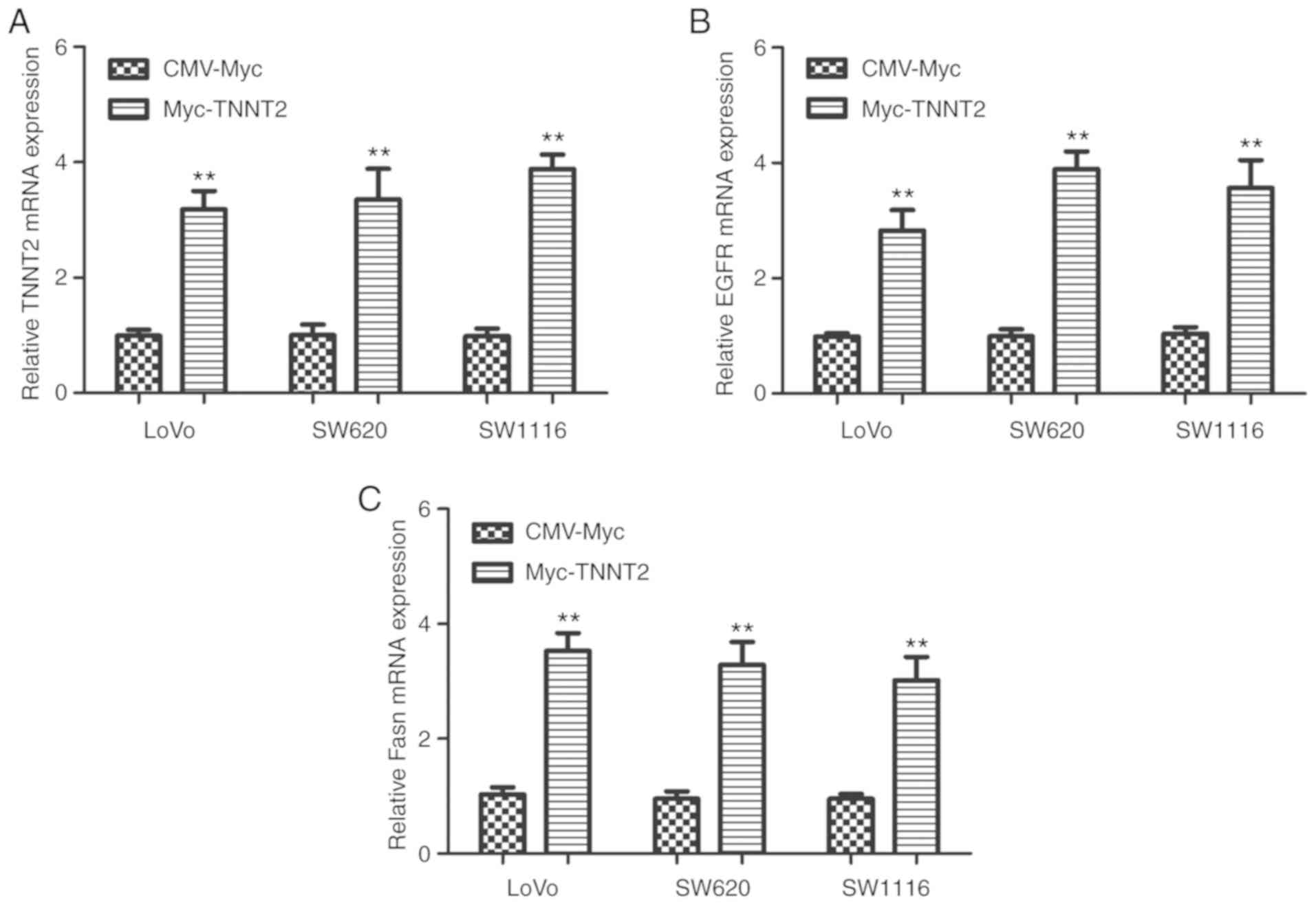
In order to further confirm the effect of
TNNT2 on the ErbB signaling pathway and glycerophospholipid
metabolism pathway, RT-PCR were carried out in CRC cell lines
transfected with the expression vector pCMV-Myc-TNNT2. As
indicated in Fig. 4A, TNNT2
expression was significantly increased in LoVo, SW620 and SW1116
cells following transfection with pCMV-Myc-TNNT2.
Additionally, the expression of EGFR and Fasn were
significantly increased (Fig. 4B and
C). This result demonstrated that high TNNT2 expression
upregulates the ErbB signaling and glycerophospholipid metabolism
pathway in CRC cell lines, which was consistent with the present
bioinformatics analysis.
Validation of elevated TNNT2
expression in CRC cell lines and tissues
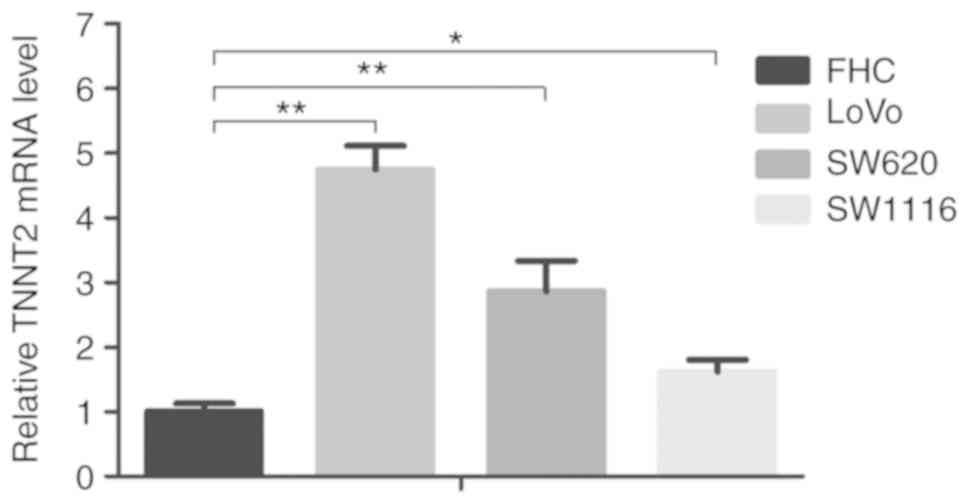
The mRNA and protein expression levels of
TNNT2 were detected in normal colorectal cell line FHC,
colon cancer cell line LoVo, CRC cell line SW620 and colon cancer
cell line SW1116. The result revealed that compared with the normal
colorectal cells, the mRNA expression level of TNNT2 was
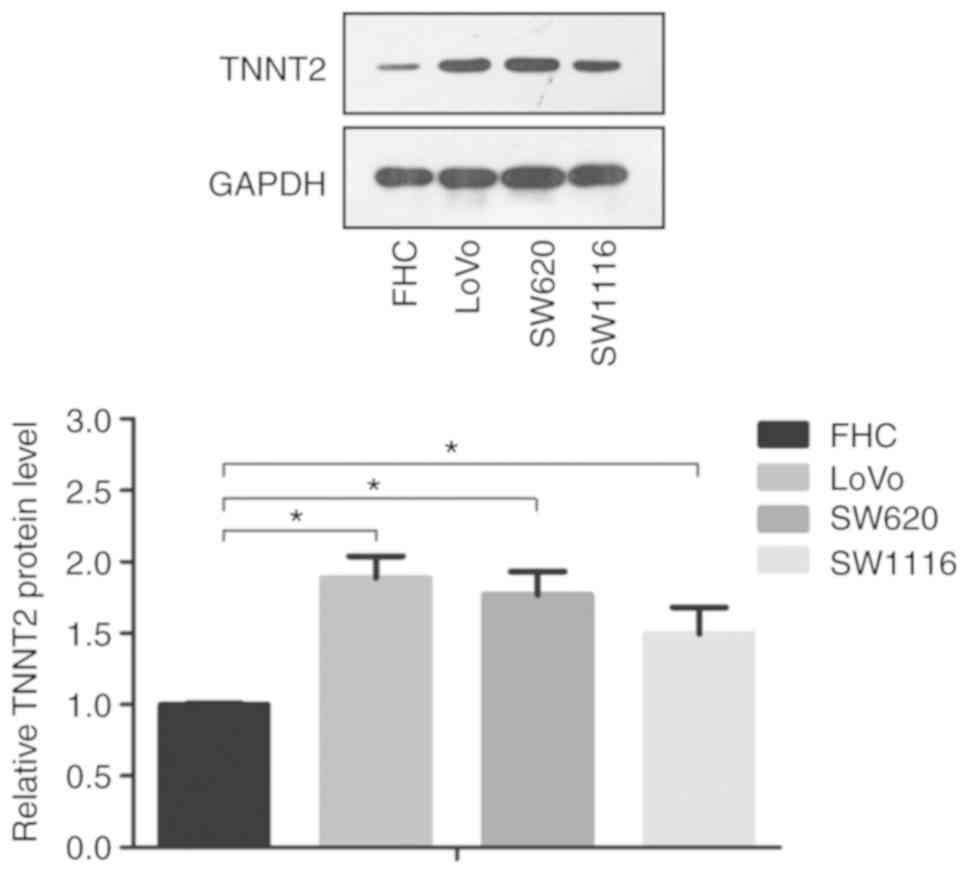
significantly increased in the CRC cells (P<0.05; Fig. 5). Moreover, the protein expression
level of TNNT2 in CRC cells was higher compared with in
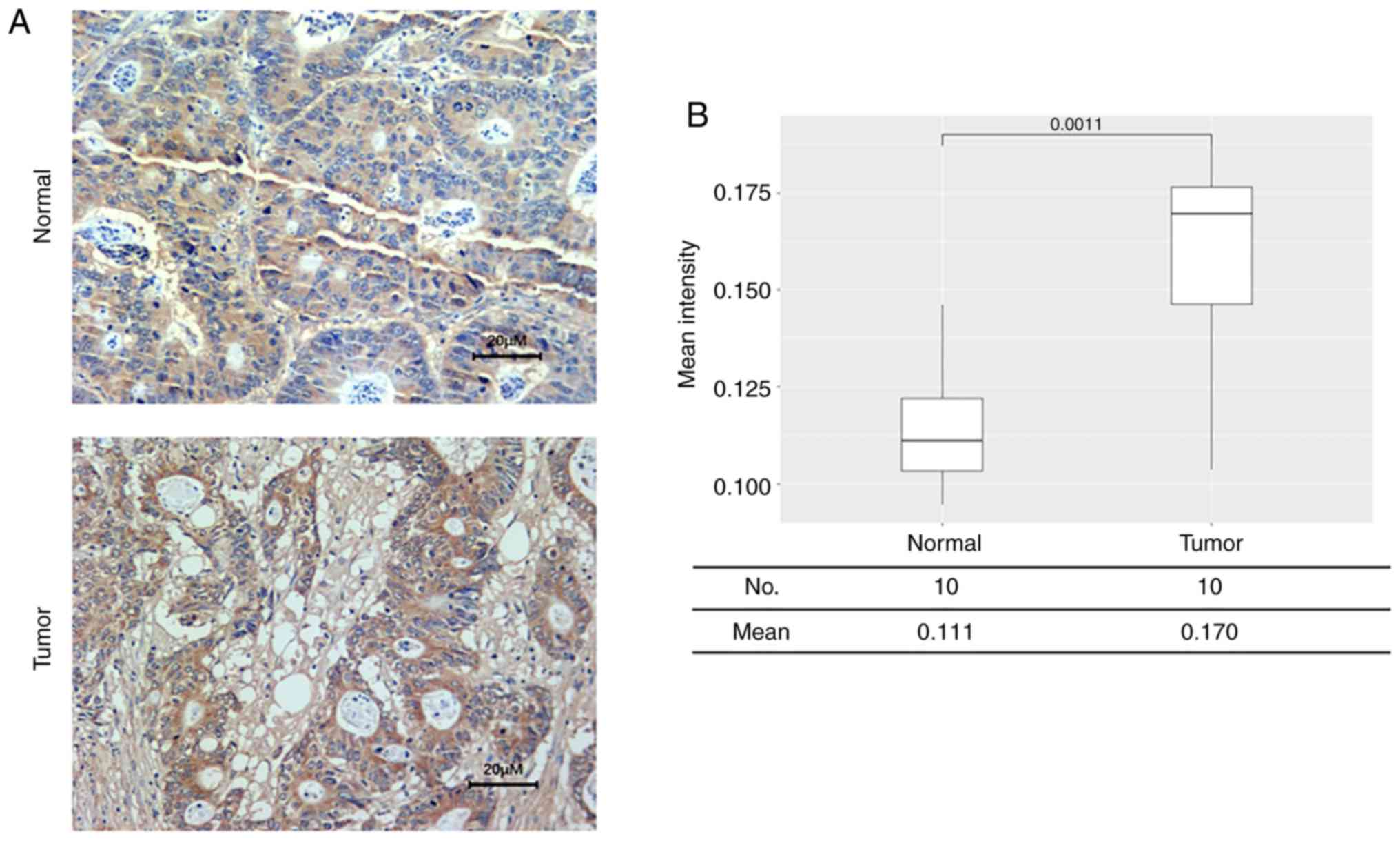
normal colorectal cells (P<0.05; Fig. 6). Immunohistochemistry was performed
to detect the protein expression of TNNT2 in CRC and normal
tissues. The result indicated increased protein expression level of
TNNT2 in CRC tissues in comparison to that in normal tissues
(P<0.05; Fig. 7).
Discussion
In the present study, the potential mRNA signatures
associated with CRC risk were explored using datasets from publicly
available databases. Differential expression analysis in TCGA
cohort indicated that TNNT2 was significantly upregulated in
CRC samples and may be associated with the onset of CRC. Survival
analysis was performed to investigate the potential of TNNT2
as a prognostic biomarker. The carcinogenic and prognostic value of
TNNT2 was further replicated in an external validation
dataset, GSE17537. Furthermore, laboratory work was also conducted
to confirm the increased mRNA and protein expressions of
TNNT2 in CRC cell lines. The RT-qPCR and western blot
analyses revealed that TNNT2 mRNA and protein expressions
were significantly elevated in CRC cell lines compared with normal
colorectal cell lines, which further validated the present
analysis.
TNNT2 encodes the tropomyosin-binding subunit
of the troponin complex, which controls muscle contraction in
response to differential concentrations of intracellular calcium
ions (25,26). Several studies have reported the
association between abnormal TNNT2 mRNA splicing and dilated
cardiomyopathy risk (27,28). Typically, altered mRNA splicing
generates different transcripts, which are then translated into
protein isoforms and influence diverse biological processes
(29). However, abnormal mRNA
splicing may result in significant changes to protein structure and
function, thus resulting in tumorigenesis (30). Lokody and Isabel (31) reported that aberrant mRNA splicing
promotes the growth of colon tumors via upregulation of PRPF6, a
driver of colon carcinogenesis. According to genome-wide profiling
of alternative splicing events, Zong et al (32) identified 13 genes with differential
mRNA splicing patterns, which may predict colorectal cancer
prognosis. The present study demonstrated that TNNT2 was
differentially expressed between CRC tumor and adjacent normal
tissues, based on both bioinformatics analysis and experimental
strategies. Normal colon tissue is composed of smooth muscle.
TNNT2 is expressed at a low level in normal colon tissue,
which is consistent with the present results (33). Therefore, it was speculated that
TNNT2 may not serve a physiological role in normal colon
tissue. A significant difference in TNNT2 mRNA expression
between different tumor stages was also identified. Thus, it was
hypothesized that the altered mRNA and protein expression levels of
TNNT2 in CRC cells may be induced by abnormal TNNT2
mRNA splicing, which may result in colorectal carcinogenesis.
According to the current functional enrichment
analysis, the ‘ErbB signaling pathway’ was significantly activated
in the high TNNT2 expression group. Upregulation, or
mutation of several members of the ErbB pathway including EGFR,
ErbB2 and ErbB3, have been identified in numerous cancer types
(34). By modulating extracellular
matrix components, ErbB recepters serve a notable role in tumor
proliferation and metastasis (35).
Upregulation of EGFR, a member of the ErbB family, is associated
with the onset and prognosis of colorectal cancer, via activating
multiple pathways, such as the MAPK and PI3K pathways (36). The current finding that
differentially expressed genes in the high TNNT2 expression
group were enriched in the ErbB signaling pathway was in accordance
with previous studies and suggested that elevated TNNT2
expression might influence CRC tumorigenesis and prognosis through
regulating the ErbB signaling pathway. In addition, the current
study identified that the glycerophospholipid metabolism pathway
was also activated in CRC samples with high TNNT2
expression. Based on global lipid omics analysis, Hung et al
(37) reported that diverse
glycerophospholipid levels were associated with chromosome
instability in gastric cancer. Several studies have reported an
association between alteration of lipid metabolism and the risk of
colorectal cancer (38,39). The results of the present study were
consistent with previous studies and suggested that high expression
of TNNT2 may affect CRC tumorigenesis via regulation of
glycerophospholipid metabolism.
In conclusion, the present study revealed that
elevated TNNT2 expression is associated with the
tumorigenesis and prognosis of CRC, which may facilitate the
identification of novel biomarkers and the development of targeted
therapeutic strategies.
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the present
study are available from the corresponding author on reasonable
request.
Authors' contributions
LJ and LF contributed to the design of the study,
wrote the manuscript and analyzed the data. ZZ, SS and RD revised
the manuscript and contributed to the design of the study. ZW, YZ
and ZR acquired, analyzed and interpreted the data. YL made
substantial contributions to the conception and design of the
present study and revised the manuscript. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
Written informed consent was obtained from all
participants and the present study was approved by the Ethics
Committee of Fourth Hospital of Hebei Medical University
(Shijiazhuang, China; approval no. 2019MEC107).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
Bray F, Ferlay J, Soerjomataram I, Siegel
RL, Torre LA and Jemal A: Global cancer statistics 2018: GLOBOCAN
estimates of incidence and mortality worldwide for 36 cancers in
185 countries. CA Cancer J Clin. 68:394–424. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Douaiher J, Ravipati A, Grams B, Chowdhury
S, Alatise O and Are C: Colorectal cancer-global burden, trends,
and geographical variations. J Surg Oncol. 115:619–630. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Favoriti P, Carbone G, Greco M, Pirozzi F,
Pirozzi RE and Corcione F: Worldwide burden of colorectal cancer: A
review. Updates Surg. 68:7–11. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chen W, Zheng R, Baade PD, Zhang S, Zeng
H, Bray F, Jemal A, Yu XQ and He J: Cancer statistics in China,
2015. CA Cancer J Clin. 66:115–132. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zheng R, Zeng H, Zhang S, Chen T and Chen
W: National estimates of cancer prevalence in China, 2011. Cancer
Lett. 370:33–38. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Karanikas M and Esebidis A: Increasing
incidence of colon cancer in patients <50 years old: A new
entity? Ann Transl Med. 4:1642016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zhang X, Shao S, Gao Y, Zhang M and Lu Y:
Meta-analysis of relationship between extranodal tumor deposits and
prognosis in patients with colorectal cancer. Zhonghua Wei Chang
Wai Ke Za Zhi. 19:334–338. 2016.(In Chinese). PubMed/NCBI
|
|
8
|
Brenner H, Kloor M and Pox CP: Colorectal
cancer. Lancet. 383:1490–1502. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yusup A, Wang HJ, Rahmutula A, Sayim P,
Zhao ZL and Zhang GQ: Clinical features and prognosis in colorectal
cancer patients with different ethnicities in Northwest China.
World J Gastroenterol. 41:7183–7188. 2013. View Article : Google Scholar
|
|
10
|
Ren Q and Jin B: The clinical value and
biological function of PTTG1 in colorectal cancer. Biomed
Pharmacother. 89:108–115. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gil J, Ramsey D, Szmida E, Leszczynski P,
Pawlowski P, Bebenek M and Sasiadek MM: TheBAXgene as a candidate
for negative autophagy-related genes regulator on mRNA levels in
colorectal cancer. Med Oncol. 34:162017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Mansour MA and Senga T: HOXD8 exerts a
tumor-suppressing role in colorectal cancer as an apoptotic
inducer. Int J Biochem Cell Biol. 88:1–13. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Roelofs HM, Te Morsche RH, van Heumen BW,
Nagengast FM and Peters WH: Over-expression of COX-2 mRNA in
colorectal cancer. BMC Gastroenterology. 14:12014. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Zhang JS, Yang LQ, Du BR and Gao H: Higher
RABEX-5 mRNA predicts unfavourable survival in patients with
colorectal cancer. Eur Rev Med Pharmacol Sci. 21:2372–2376.
2017.PubMed/NCBI
|
|
15
|
Wang L, Shen X, Wang Z, Xiao X, Wei P,
Wang Q, Ren F, Wang Y, Liu Z, Sheng W, et al: A molecular signature
for the prediction of recurrence in colorectal cancer. Mol Cancer.
14:222015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Yarden Y and Pines G: The ERBB network: At
last, cancer therapy meets systems biology. Nat Rev Cancer.
12:553–563. 2012. View
Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hynes NE and Lane HA: ERBB receptors and
cance: The complexity of targeted inhibitors. Nat Rev Cancer.
5:341–354. 2005. View
Article : Google Scholar : PubMed/NCBI
|
|
18
|
Wang H, Xi Q and Wu G: Fatty acid synthase
regulates invasion and metastasis of colorectal cancer via Wnt
signaling pathway. Cancer Med. 5:1599–1606. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Li N, Bu X, Tian X, Wu P, Yang L and Huang
P: Fatty acid synthase regulates proliferation and migration of
colorectal cancer cells Via HER2-PI3K/Akt signaling pathway. Nutr
Cancer. 64:864–870. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Nikolayeva O and Robinson MD: edgeR for
Differential RNA-seq and ChIP-seq Analysis: An application to stem
cell biology. Methods Mol Biol. 1150:45–79. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Subramanian A, Tamayo P, Mootha VK,
Mukherjee S, Ebert BL, Gillette MA, Paulovich A, Pomeroy SL, Golub
TR, Lander ES and Mesirov JP: Gene set enrichment analysis: A
knowledge-based approach for interpreting genome-wide expression
profiles. Proc Natl Acad Sci USA. 102:15545–15550. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Gazzoni GF, Fraga MB, Ferrari ADL, Soliz
PDC, Borges AP, Bartholomay E, Kalil CAA, Giaretta V and Rohde LEP:
Predictors of total mortality and echocardiographic response for
cardiac resynchronization therapy: A cohort study. Arq Bras
Cardiol. 109:569–578. 2017.(In English, Portuguese). PubMed/NCBI
|
|
23
|
Kang JS, Lee S, Son D, Han Y, Lee KB, Kim
JR, Kwon W, Kim SW and Jang JY: Prognostic predictability of the
new American Joint Committee on Cancer 8th staging system for
distal bile duct cancer: Limited usefulness compared with the 7th
staging system. J Hepatobiliary Pancreat Sci. 25:124–130. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Liu L, Shi M, Wang Z, Lu H, Li C, Tao Y,
Chen X and Zhao J: A molecular and staging model predicts survival
in patients with resected non-small cell lung cancer. BMC Cancer.
18:9662018. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ohtsuki I and Morimoto S: Troponin:
Regulatory function and disorders. Biochem Biophys Res Commun.
369:62–73. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wei B and Jin JP: TNNT1, TNNT2, and
TNNT3: Isoform genes, regulation, and structure-function
relationships. Gene. 582:1–13. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Van Spaendonck-Zwarts KY, Van Rijsingen
IA, Van den Berg MP, Lekanne Deprez RH, Post JG, van Mil AM,
Asselbergs FW, Christiaans I, van Langen IM, Wilde AA, et al:
Genetic analysis in 418 index patients with idiopathic dilated
cardiomyopathy: Overview of 10 years' experience. Eur J Heart Fail.
15:628–636. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Kong SW, Hu YW, Ho JW, Ikeda S, Polster S,
John R, Hall JL, Bisping E, Pieske B, dos Remedios CG and Pu WT:
Heart failure-associated changes in RNA splicing of sarcomere
genes. Circ Cardiovasc Genet. 3:138–146. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kozlovski I, Siegfried Z, Amar-Schwartz A
and Karni R: The role of RNA alternative splicing in regulating
cancer metabolism. Human Genet. 136:1113–1127. 2017. View Article : Google Scholar
|
|
30
|
Munkley J, Livermore K, Rajan P and
Elliott DJ: RNA splicing and splicing regulator changes in prostate
cancer pathology. Hum Genet. 136:1143–1154. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Lokody I: Alternative splicing: Aberrant
splicing promotes colon tumour growth. Nat Rev Cancer. 14:382–383.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Zong Z, Li H, Yi C, Ying H, Zhu Z and Wang
H: Genome-wide profiling of prognostic alternative splicing
signature in colorectal cancer. Front Oncol. 8:5372018. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Adams JE III, Bodor GS, Dávila-Román VG,
Delmez JA, Apple FS, Ladenson JH and Jaffe AS: Cardiac troponin I.
A marker with high specificity for cardiac injury. Circulation.
88:101–106. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
De Luca A, Carotenuto A, Rachiglio A,
Gallo M, Maiello MR, Aldinucci D, Pinto A and Normanno N: The role
of the EGFR signaling in tumor microenvironment. J Cell Physiol.
214:559–567. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Mallini P, Lennard T, Kirby J and Meeson
A: Epithelial-to-mesenchymal transition: What is the impact on
breast cancer stem cells and drug resistance. Cancer Treat Rev.
40:341–348. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Spano JP, Fagard R, Soria JC, Rixe O,
Khayat D and Milano G: Epidermal growth factor receptor signaling
in colorectal cancer: Preclinical data and therapeutic
perspectives. Ann Oncol. 16:189–194. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Hung CY, Yeh TS, Tsai CK, Wu RC, Lai YC,
Chiang MH, Lu KY, Lin CN, Cheng ML and Lin G: Glycerophospholipids
pathways and chromosomal instability in gastric cancer: Global
lipidomics analysis. World J Gastrointest Oncol. 11:181–194. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Mika A, Kobiela J, Czumaj A, Chmielewski
M, Stepnowski P and Sledzinski T: Hyper-elongation in colorectal
cancer tissue-cerotic acid is a potential novel serum metabolic
marker of colorectal malignancies. Cell Physiol Biochem.
41:722–730. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Mirnezami R, Spagou K, Vorkas PA, Lewis
MR, Kinross J, Want E, Shion H, Goldin RD, Darzi A, Takats Z, et
al: Chemical mapping of the colorectal cancer microenvironment via
MALDI imaging mass spectrometry (MALDI-MSI) reveals novel
cancer-associated field effects. Mol Oncol. 8:39–49. 2014.
View Article : Google Scholar : PubMed/NCBI
|