Introduction
Anaplastic thyroid cancer (ATC) constitutes 1–2% of
all thyroid cancers and has a poor prognosis with a median survival
time of 6 months in 50% of patients and only a 1-year survival time
in 20% of patients (1). The
comprehensive treatment for ATC includes surgery and systematic
chemotherapy combined with radioiodine therapy; however, the
therapeutic outcomes are not promising owing to its rapid
proliferation and aggressive nature and the lack of
thyroid-specific role of iodine intake (2,3).
Systemic chemotherapies based on combining paclitaxel or docetaxel
with carboplatin or doxorubicin are adopted for patients with
metastases (2,4,5).
However, clinical data has revealed that serious adverse effects
and drug resistance hinder combination treatment, posing
difficulties in completing the course (5–7). A
lack of reliable treatment for ATC due to resistance to
chemotherapy leads to unlimited local growth and distal metastases
in patients with ATC (8).
All-trans-retinoic acid (ATRA) has been used to impel ATC
cell redifferentiation with increased iodine uptake and improved
radiosensitivity (9); however, the
results are not promising and even exhibit the opposite effects in
other ATC cell lines. Therefore, there is an urgent need to
identify novel and safe drugs or redifferentiation agents with
fewer side effects for ATC therapy.
Phytochemicals are effective in the management of
inflammation and cancer (10).
Dietary phytochemicals are potential modulators of immunological
status and possess various pharmacological properties including
anticancer, antioxidant, and anti-inflammatory effects (11). The therapeutic efficacy of
phytochemicals shows promise in the management of several cancers
(12). However, certain studies on
the use of phytochemicals to treat ATC have exhibited some special
features, which are presented in detail below. For example, ATRA
induced redifferentiation in ATC cells (SW1736) and inhibited cell
growth (9) but was ineffective in
THJ-11T, THJ-16T, and THJ-21T cells (13). However, resveratrol reversed ATRA
resistance in THJ-11T cells that were resistant to treatment only
with resveratrol. These findings suggest that phytochemicals not
only show promising antitumor effects in ATC cells but also exhibit
the possibility to induce ATC cell redifferentiation in
vivo. Further preclinical or clinical studies focusing on the
treatment of ATC may face challenges of drug resistance.
Phytochemicals may serve as prospective adjuvants to prevent drug
resistance in ATC.
In the present review, some of the natural
phytochemicals used to treat ATC were summarized and similar
anticancer effects of other phytochemicals were listed. The
references are mainly derived from searching internet databases
such as Google Scholar, PubMed, and ScienceDirect. The search was
restricted to studies published in English and those conducted on
humans. Only articles and reviews were selected and symposium or
conference papers were excluded. The present review focused on
agents obtained from plants that exhibit a potential role in the
treatment of ATC. Compounds obtained from other organisms were
excluded.
Phytochemicals effective in ATC cells
Aloperine
Aloperine is a quinolizidine alkaloid extracted from
Sophora alopecuroides L., commonly used to treat infections,
rheumatism, heart disorders, and gastrointestinal diseases
(14). To date, the anticancer
effects of aloperine include inhibition of cell growth, induction
of apoptosis, activation of reactive oxygen species (ROS), and
modulation of autophagy in several cancers, such as breast,
prostate, ovarian, and thyroid cancer (15–18).
Aloperine was revealed to inhibit the proliferation of ATC cells
(8505C and KMH-2) and tumorigenesis in vivo. It also
promoted caspase-dependent apoptosis in 8505C and KMH-2 cells by
intrinsic or extrinsic pathways (19). Moreover, aloperine promoted the
activation of autophagy in KMH-2 ATC cells by suppressing the
activation of the Akt/mammalian target of rapamycin (mTOR) pathway.
The cytotoxic effect of aloperine in KMH-2 ATC cells resulted from
aloperine-mediated autophagy (18).
Apigenin (APG)
APG is a flavone widely found in fruit, vegetables,
and seasoning herbs, such as artichoke, onions, and dried chamomile
flowers (20). APG exerts
anticancer effects by altering cell viability, migration and
invasion potential, dendrite morphology, G2/M phase arrest, and
apoptosis by inactivation of the extracellular signal-regulated
protein kinase (ERK) and the Akt/mTOR signaling pathway (21). In 1999, it was reported that APG
exerted anticancer effects on ATC cells (ARO) that lack
antiestrogen binding sites or estrogen receptors (22). APG also induced apoptosis in ATC
cells (FRO) by increasing c-Myc levels and phosphorylation of both
p38 and p53. c-Myc may act as a core regulator in the progression
of APG-induced apoptosis of ATC cells (23). In addition, APG exerted
growth-inhibition effects in ATC cells (ARO), inhibited both
autophosphorylation of epidermal growth factor receptor (EGFR)
tyrosine and phosphorylation of its downstream effector
mitogen-activated protein kinase (MAPK) and decreased c-Myc
phosphorylation (24). PLX4032 is
a BRAFV600E inhibitor that can enhance the effects of APG in ATC
cells (8505C and FRO) harboring BRAFV600E (25). The outcomes of using APG and
PLX4032 include the decreasing of cell viability, increasing the
dead cell percentage, promoting the expression of cleaved poly-ADP
ribose polymerase (PARP)-1 and cleaved caspase-3 protein, and
decreasing phosphorylated (p)-ERK expression. However, treatment
with APG and PLX4032 failed to alter the protein levels of p-ERK in
FRO cells. Additionally, treatment with APG and tumor necrosis
factor (TNF)-related apoptosis-inducing ligand (TRAIL) decreased
the viability of ATC cells (8505C and CAL-62) and Bcl-2 protein
levels, and increased the protein levels of cleaved PARP and
p-ERK1/2. Suppression of Akt signaling enhanced the effects of APG
and TRAIL treatment by modulation of Bcl-2 family protein levels in
8505C and CAL-62 cells (26).
Artemisinin (ART)
ART is a sesquiterpene isolated from Artemisia
annua L. It is known as qinghao (a herb with a long history of
use in China), and as a sesquiterpene with a unique peroxide
structure, ART exhibits excellent activity against malaria
(27). ART and its derivatives are
potential candidates that have been demonstrated to increase the
apoptosis and autophagy of cancer cells, promote cell cycle arrest,
suppress the invasion and migration of cancer cells, and induce
ferroptosis in cancer cells (28).
It was revealed that ART could suppress cell growth, induce arrest
in the G2/M phase, and increase cyclin D1 in BHT-101 ATC cells but
not in CAL-62 ATC cells. Using RNA-seq, it was determined that
ART-resistant CAL-62 cells were associated to the abnormal
activation of WNT signaling. Lastly, the issue of ART resistance
was overcome by co-treating cells with ART and pyrvinium pamoate,
which is a WNT signaling inhibitor (29).
Baicalein
Baicalein is a flavone extracted from Scutellaria
(S.) baicalensis Georgi or S. lateriflora L. It has
several anticancer properties including the inhibition of cell
proliferation, invasiveness, migration, and EMT progression; and an
increase in apoptosis and autophagy (30–32).
Some studies have demonstrated that treatment with baicalein (50 or
100 µM) and docetaxel (10 nM) can significantly enhance the
anticancer effects of docetaxel by the suppression of proliferation
and induction of apoptosis, and by significantly inhibiting the
expression of transforming growth factor (TGF)-β1, vascular
endothelial growth factor (VEGF), caspase-3, Bax, E-cadherin,
N-cadherin, and mTOR. Moreover, baicalein and docetaxel
significantly reduced Bcl-2 expression and the phosphorylation of
ERK and Akt in 8505C ATC cells (33). Furthermore, baicalein treatment
inhibited the proliferation of FRO ATC cells and induced apoptosis
with increased DNA fragmentation. Baicalein at concentrations of 50
and 100 µM was demonstrated to decrease the expression of Bax,
PARP, cytochrome c, cleaved caspase-3, and Cox-2, and
increase Bcl-2 expression. Baicalein exerted anticancer effects in
FRO ATC cells mainly by promoting the phosphorylation of ERK, p38,
MAPK, and Akt (34). Additionally,
baicalein decreased cell viability and the number of cell colonies,
and increased cell apoptosis, cell cycle arrest, and autophagy in
FRO ATC cells. It significantly increased the expression of
Beclin-1, Atg5, p62, Atg12, caspase-3, and caspase-8. Furthermore,
it significantly decreased the ratios of caspase-3 and caspase-8,
p-ERK/ERK, and p-Akt/Akt, suggesting its potential in suppressing
ERK and phosphatidylinositol 3-kinase/protein kinase B (PI3K/Akt)
signaling (32).
Chrysin
Chrysin is a phytochemical widely present in
Matricaria chamomilla L., Oroxylum Indicum (L.) Kurz,
Passiflora edulis Sims, and P. caerulea L. It is also
found in honey, passion fruit, and mushrooms (35,36).
Chrysin has been demonstrated to inhibit the growth of cancer cells
through the induction of apoptosis, cell cycle arrest, suppression
of angiogenesis, and inhibition of invasion and metastasis, without
causing toxicity or undesirable side effects to normal cells both
in vivo and in vitro. Chrysin exerts these effects by
selectively modulating multiple cell signaling pathways related to
inflammation, proliferation, angiogenesis, invasion and metastasis,
and survival of cancer cells (37). Chrysin exerted anticancer effects
in ATC cells (HTH7 and KAT18) such as inhibition of cell growth,
alteration of protein levels, and increasing the ratio of Bax to
Bcl-2 expression (38). Changes in
protein levels included a decrease in the expression of cyclin D1,
Mcl-1, and XIAP, and a significant increase in the expression of
cleaved caspase-3 and cleaved PARP. In addition, chrysin was
revealed as a potential Notch activator in ATC cells (HTh7 and
KAT18) (39). Chrysin treatment
resulted in cell growth inhibition and increased the protein and
mRNA expression of Notch 1 and hairy/enhancer of split 1 (Hes1).
The proliferation-inhibition effect of chrysin in ATC cells was due
to apoptosis resulting from Notch1 activation and an increase in
cleaved PARP protein in vivo. Moreover, chrysin suppressed
the growth of ATC xenografts and delayed the calculated median time
to tumor progression in vivo (39).
Curcumin
Curcumin is a polyphenol obtained from the rhizomes
of Curcuma longa. It is one of the most promising naturally
occurring compounds used to treat cancers, including breast, lung,
gastric, colorectal, pancreatic, and hepatic cancers (40). Curcumin intervention was
demonstrated to result in a decrease in cell viability, suppression
of aggressiveness, and an increase in apoptosis in the ATC cell
lines SW1736 and 8505C. It also decreased the mRNA expression of
PAX8, TTF1, TTF2, and TPO in SW1736 cells while decreasing the
miRNA expression of hsa-miR-221, hsa-miR-222, hsa-miR-21, and
hsa-miR-146b in both SW1736 and 8505C (41). Curcumin was revealed to
significantly reduce the oxidative stress index in ATC cells
(CAL-62) accumulating in the G0/1 phase, and also suppress spheroid
formation and cellular motility in Matrigel (42). Moreover, curcumin increased the
therapeutic efficacy of drugs used to treat ATC. Curcumin combined
with docetaxel decreased the viability of ATC cells and induced
apoptosis. It improved the anticancer effect of docetaxel in ATC
cells by inhibiting p65 activation and COX2 expression and
decreasing the threshold of cell apoptosis by docetaxel (43). Thus, the role of curcumin as an
adjuvant in ATC chemotherapy should be further explored.
Deguelin
Deguelin is one of the four natural rotenoids
obtained from the bark, roots, and leaves of plants from the
Leguminosae family. It is an NADH:ubiquinone oxidoreductase
(complex I) inhibitor (44,45).
Low doses of deguelin have been demonstrated to result in cell
cycle arrest, induction of tumor apoptosis, and suppression of
angiogenesis and metastasis. Its anticancer effects are related to
the protein levels of PI3K, MAPK, Akt, mTOR, NF-κB, caspase-3/8/9,
matrix metalloproteinase (MMP)-2, and MMP-9 (45). Deguelin enhanced superoxide
dismutase (SOD) activity and effectively induced apoptosis (similar
to docetaxel) in CAL-62 ATC cells. It has been shown to play
similar roles as that of curcumin, such as blocking spheroid
formation and cellular motility in Matrigel and cell cycle arrest
(42).
Epigallocatechin-3-gallate (EGCG)
EGCG is one of the most abundant ingredients in
green tea that has been widely studied as a phytochemical and
nutraceutical (46). EGCG has been
demonstrated to induce ROS generation and upregulate AMPK. Through
the increase in liver kinase B1 (LKB1) and
Ca2+/calmodulin-dependent protein kinase kinase (CaMKK),
it caused a decrease in mTOR expression, which finally led to
anticancer effects (47). A
previous study revealed that EGCG inhibited the proliferation,
viability, cell cycle progression, migration, and invasion of ARO
ATC cells, and induced apoptosis in ARO cells by reducing the
protein levels of H-RAS, p-RAF, p-MEK1/2, p-EGFR, and p-ERK1/2.
In vivo, EGCG inhibited the growth of ARO cell carcinoma
xenografts by increasing apoptosis and blocking angiogenesis
(48). Furthermore, EGCG
significantly inhibited epithelial-mesenchymal transition (EMT),
invasion, and migration in 8505C ATC cells by regulating the
TGF-β/Smad signaling pathways in vivo. The regulatory
mechanism of TGF-β/Smad signaling pathways includes E-cadherin
reduction and vimentin induction, and the inhibition of Smad2/3
phosphorylation and Smad4 translocation (49).
Evodiamine (EVO)
EVO is an important alkaloid isolated from the fruit
of Tetradium ruticarpum (A.Juss.) T.G. Hartley, and is one
of the most important components of the Chinese herb ‘Wu-Zhu-Yu’
(50). EVO has been revealed to
exert its anticancer effects by inhibiting cell growth, invasion,
and metastasis, and inducing apoptosis in cancer cells in colon
cancer, lung cancer, hepatocellular carcinoma, and melanoma
(51). Mechanisms of the
anticancer effects of EVO in ARO ATC cells include the inhibition
of cell proliferation, increase in DNA fragmentation, induction of
apoptosis, and G2/M phase arrest. Moreover, EVO was demonstrated to
change the protein levels and activity in ARO ATC cells, which
included increasing the levels of cdc25C, cyclin B1, and cdc2-p161;
decreasing the level of cdc2-p15; and promoting caspase-3/8/9
activation and PARP cleavage (52). Results from a proteomic strategy
indicated that the anticancer effects of EVO in ARO ATC cells were
due to the differentially expressed proteins involved in
transcription control, signal transduction/calcium regulation,
protein folding, and lipid metabolism (53). Furthermore, EVO was shown to
decrease cell viability and the protein levels of Bcl-2 and p-Akt,
and increase cytotoxicity and the percentage of apoptotic cells in
SW1736 ATC cells. EVO exhibited synergistic effects when used with
other anticancer agents such as wortmannin, TGF-β, and PXD101 (a
histone deacetylase inhibitor). Co-treatment with EVO and
wortmannin decreased cell viability and the levels of p-Akt and
Bcl-2, and promoted cytotoxicity. Additionally, following treatment
with TGF-β, EVO decreased variations in morphology, growth, and
migration by increasing p21 and p53, and decreasing the protein
levels of β-catenin, N-cadherin, vimentin, p-Akt, and MMP-2/9
(54). A previous study
demonstrated that co-treatment of SW1736 ATC cells with EVO and
PXD101 decreased cell viability, the percentage of viable cells,
and Bcl-2 expression, while increasing cytotoxicity, the percentage
of apoptotic cells, and the expression of γH2AX, acetyl histone H3,
and cleaved PARP. Moreover, EVO increased PXD101 cytotoxicity, ROS
production, the expression of γH2AX and cleaved PARP, and the
Bcl-2/Bax ratio (55). Different
ATC cell lines (SW1736 and KAT4B) have different sensitivities to
EVO (56). Previous research
revealed that EVO treatment induced a higher apoptotic percentage
in SW1736 cells than in KAT4B cells (56). Mechanistic studies demonstrated
that the activation of p53 and its downstream proteins, the
blockage of MMP, and an increase in intracellular peroxide
production leads to EVO-induced G2/M arrest and apoptosis in SW1736
cells. However, in KAT4B cells, EVO induced only a few apoptotic
events and only cell accumulation in the G2/M phase. Notably, the
alkylation of EVO at position 14 may be crucial in inducing
apoptosis in SW1736 cells (56).
Indirubin
Indirubin is a bis-indole alkaloid and the
main active constituent of Danggui Longhui Wan, a Chinese
traditional medicine used to treat chronic myeloid leukemia
treatment (57). It has been
reported that indirubin and its derivatives compete with ATP
binding and suppress cyclin-dependent kinases (CDKs), resulting in
apoptosis and G2/M arrest in cancer cells (58). A previous has shown that
7-bromoindirubin-3′-oxime (7BIO; an indirubin derivative) can impel
DNA fragmentation and lactate dehydrogenase liberation in ATC cells
(BHT-101, SW1736, HTh7, and C643). However, 7BIO failed to promote
caspase activation in these ATC cell lines and increased cleaved
PARP fragments only in C643 cells. Moreover, all ATC cell lines
except for C643 exhibited a significant increase in the proportion
of cells in the G1 phase after treatment with 7BIO. Notably,
caspase suppression did not affect the viability of cells after
incubation with 7BIO. The authors of the study suggest that 7BIO
may be a potential candidate to treat ATC treatment; however, the
mechanisms of 7BIO in exerting an effect in different ATC cells
require further research (59).
Isoflavones [genistein (Gen) and
daidzein]
Gen is an isoflavone that is abundantly present in
legumes, lupine, coffee, soybeans, fava bean, and kudzu. Gen exerts
its antitumor effects through cell growth inhibition, alteration of
the cell cycle, apoptosis induction, angiogenesis suppression,
invasion and metastasis suppression, and modulation of epigenetic
changes (60). The anticancer
effect of Gen in ATC cells (UCLA RO-81-A-1) has been shown as early
as 1999 (22). The concurrent
treatment of Gen and photodynamic therapy (PDT) mediated by
photofrin revealed promising antitumor effects in SUN-80 ATC cells.
Treatment using this combination led to antitumor effects including
cell growth inhibition, mitochondrial membrane depolarization,
apoptosis induction, promotion of ROS production, and alterations
in the protein levels of caspase-3/8/9/12, cytochrome c, and
other apoptosis-related proteins (61). In addition, it has been reported
that Gen suppresses cell viability and promotes apoptosis in ATC
cells (SW1736 and 8505C). Additionally, Gen was demonstrated to
increase the expression of genes related to the
thyroid-differentiated phenotype, such as TG, sodium-iodine
symporter (NIS), TPO, TSHR, and TTF2 in both SW1736 and 8505C
cells. Notably, Gen reduced colony formation only in 8505C cells
but not in SW1736 cells (41).
Moreover, co-treatment with thymoquinone and Gen suggests promising
anticancer effects in ATC cells. Co-treatment using thymoquinone
and Gen is detailed in a subsequent section.
Myricetin
Numerous studies have confirmed the potent
anticancer effects of myricetin on cancers such as those of the
breast, liver, ovary, colon, and thyroid (62–66).
Myricetin has been demonstrated to decrease the growth of ATC cells
(SNU-80 HATC) and induce a significant increase in DNA condensation
and the proportion of cells in the sub-G1 phase (66). Myricetin was shown to induce ATC
cell death by an increase in the activation of caspase cascades and
the Bax:Bcl-2 ratio (66).
Myricetin was also revealed to alter the mitochondrial membrane
potential and increase the release of apoptosis-inducing factor
(AIF) from mitochondria to the cytosol (66).
Quercetin
Quercetin is a natural flavonoid that is abundant in
the daily diet. Several in vivo and in vitro studies
have revealed that quercetin exerts anticancer effects by
inhibiting cell proliferation, affecting cell cycle progression,
promoting apoptosis, inhibiting angiogenesis and metastasis, and
even affecting autophagy (67).
Quercetin has been shown to suppress the growth of ATC cells (FRO
and ARO) and reduce CD97 expression (68). CD97 is a dedifferentiation marker
relevant to cancer progression and metastasis. It was decreased by
certain redifferentiating agents such as ATRA in CD97-positive
human follicular thyroid carcinoma (FTC-133) cells (69). Quercetin has been demonstrated to
increase or induce NIS in FRO cells, but it failed to increase NIS
expression in ARO cells (68).
Resveratrol. Resveratrol
(trans−3,5,4¢-trihydroxystilbene) was first isolated from
the roots of Veratrum album (white hellebore) and
Polygonum cuspidatum (Japanese knotweed) and is abundantly
present in grapes, berries, and peanuts (70). Resveratrol exhibits potential in
the treatment of cancers, such as those of the head and neck,
thyroid, breast, lung, stomach, colon, kidney, cervix, bladder,
ovary, and skin in humans (71).
Resveratrol treatment was demonstrated to suppress the growth of
ATC cells (HTh7 and 8505C) by apoptosis induction and S-phase cell
cycle arrest. It also increased Notch1 protein expression and
activated the Notch1 pathway and upregulated the protein levels of
thyroid-specific genes, such as Pax8, NIS, TTF1, and TTF2 (72). A previous study by the authors
revealed that resveratrol decreased the total ATC cell count
(THJ-16T and THJ-21T) by decreasing cyclin D1 expression,
increasing the apoptotic cell fractions, and activation of
caspase-3. Resveratrol was not able to suppress the growth of
THJ-11T ATC cells; however, it promoted ATRA sensitivity in THJ-11T
ATC cells by suppressing peroxisome proliferator-activated
receptor-β/δ and increasing cellular retinoic acid receptor-β and
cellular retinoic acid-binding protein (CRABP)2. In addition, the
efficacy of resveratrol in increasing thyroglobulin and E-cadherin
levels was manifested by the appearance of membranous E-cadherin in
THJ-11T ATC cells (13). Liu et
al researched the ability of resveratrol in improving ATRA
sensitivity in THJ-11T ATC cells. Resveratrol abolished CRABP2
methylation through demethylation of three CpG methylation sites on
the promoter of CRABP2 and due to its suppressive effect on DNA
methyltransferase (DNMT1 and DNMT3A) protein levels (73). Wu et al explored the
association between the activation of STAT3 signaling and the
antitumor effect of resveratrol in ATC cells (THJ-11T, THJ-16T, and
THJ-21T). In this study it was revealed that resveratrol suppressed
LIF and STAT3 expression and inhibited p-STAT3 nuclear
translocation in THJ-16T and THJ-21T cells but not in THJ-11T
cells, indicating LIF upregulation and more frequent p-STAT3
nuclear translocation. A STAT3 inhibitor, AG490, which
significantly prevents p-STAT3 nuclear translocation, reversed the
resveratrol toleration of THJ-11T cells (74). Another study by Zheng et al
demonstrated that the molecular mechanisms of the anticancer
effects of resveratrol are associated to resveratrol-induced
oxidative damage due to increased ROS and oxidative stress-induced
mitochondrial swelling. Compared with untreated THJ-11T cells,
resveratrol-treated THJ-16T cells exhibited a marked increase in
ROS generation, a decrease in catalase (CAT) and SOD2 levels,
stronger activation of caspase-9/caspase-3, and more impaired
mitochondrial function. In addition, co-treatment with antioxidants
such as N-acetylcysteine attenuated the antitumor effects of
resveratrol in THJ-16T cells (75). Xiong et al explored the
redifferentiating effect of resveratrol in THJ-16T and THJ-21T ATC
cells and determined that resveratrol increased phosphatase and
tensin homolog (PTEN) levels, resulting in distinct NIS and PTEN
nuclear co-translocation in THJ-16T and THJ-21T ATC cells. However,
NIS did not appear on the ATC cell membrane (76). In addition, resveratrol in
different delivery systems has also exhibited potential in treating
ATC. Resveratrol sustained-release targeting nanoparticles
successfully suppressed ATC cell growth in vivo. Resveratrol
overcame the side effects and secondary drug resistance of
docetaxel/doxorubicin in treating ATC xenograft models (77).
Thymoquinone (TQ)
TQ (2-isopropyl-5-methyl-1,4-benzoquinone) is a
bioactive substance isolated from Nigella sativa seeds
(78). TQ exerts anticancer
effects on several types of cancers, such as skin cancer,
glioblastoma, breast cancer, pancreatic cancer, colorectal
carcinoma, bladder cancer, and cervical squamous carcinoma
(79). The combined intervention
of TQ and Gen has been demonstrated to suppress cell survival,
angiogenesis, telomerase activation, and increase pro-apoptotic
protein expression in ATC cells (CAL-62 and ACC 448). The
anticancer effects of the combination of TQ and Gen were attributed
to a reduction of NF-κB, VEGF, and human telomerase reverse
transcriptase (hTERT) and suppression of p21 and PTEN. Moreover,
co-treatment with TQ and Gen was more effective in ATC cells than
in FTC cells (80).
Triptolide (TPL)
TPL is a diterpenoid trioxide isolated from a
perennial vine-like Chinese herb Tripterygium wilfordii
Hook. f. (81). TPL inhibits
cancer cell growth and shows promising antitumor effects in cancers
such as prostate cancer, ovarian cancer, breast cancer,
neuroblastoma, lung cancer, acute myeloid leukemia, and multiple
gastrointestinal cancers in preclinical studies (82). Previous research revealed the
anticancer effects of TPL in ATC cells (TA-K), including the
inhibition of cell growth and induction of apoptosis by suppression
of the NF-κB pathway but not the p53 signaling pathway (83). Inhibition of the transcriptional
activation of NF-κB by TPL in TA-K cells was due to the blocking
between the p65 subunit and CREB-binding protein (CBP)/p300 in the
early stages and a decrease in p65 expression in the later stage.
In addition, TPL decreased the protein levels of proliferation,
angiogenesis, and invasion targets such as cyclin D1, VEGF, and
urokinase-type plasminogen activator in ATC cells (TA-K and 8505C)
(84). A previous study revealed
that TPL has an angiogenesis-suppressive effect in both TK-A cells
and human umbilical vein endothelial cells; these findings were
also reported in vivo studies (85). Furthermore, TPL may be considered
an adjuvant in the treatment of 8505C ATC cells. When used as an
adjuvant, BIIB021, a novel heat shock protein 90 inhibitor,
exhibited improved anticancer effects in decreasing cell viability
and dead cell percentage and increasing cytotoxicity compared with
BIIB021 treatment alone. Co-treatment with BIIB021 and TPL
increased cytotoxicity in 8505C ATC cells through activation of DNA
damage response, suppression of the NF-κB and PI3K/Akt/mTOR
pathways, and a decrease in surviving (86).
Discussion
Phytochemicals have five broad unique aspects and
limitations. First, some phytochemicals promote the activation of
ROS in ATC cells. The anticancer effects of phytochemicals in ATC
cells, including cell growth inhibition, suppression of
angiogenesis, and autophagy modulation, promotion of apoptosis cell
cycle arrest, and ROS activation are presented in Table I. Phytochemicals are generally
considered to have the ability to reduce ROS activity in other
cancers (87–89). It is unusual for phytochemicals to
have the capacity to increase the activation of ROS in ATC cells.
Second, unlike other anticancer agents, phytochemicals exert
therapeutic effects on numerous cancers and are associated only
with a few side effects (90).
Third, phytochemicals exhibit promise as adjuvants in enhancing the
sensitivities of other anticancer agents such as PLX4032, TRAIL,
docetaxel, TGF-β, wortmannin, PXD101, ATRA, and BIIB021 (25,26,43,54,55,73,86).
However, the varying sensitivities of different ATC cell lines
often restrict phytochemical use (13,59,68).
Moreover, drug resistance exhibited by ATC cells continues to pose
a serious challenge. Fourth, the active metabolites of
phytochemicals cannot always reach the target tissue at therapeutic
concentrations. Furthermore, urinary excretion, short elimination
half-life, and water solubility decrease the bioavailability of
phytochemicals (91). Some
research groups have improved the bioavailability of phytochemicals
(92), thereby increasing the
possibility of their use as biomedicine. Fifth, clinical trials are
seldom conducted on phytochemicals; therefore, data on their
efficacy in treating patients with ATC are lacking. The majority of
references presented in this review are studies on the anticancer
effects of phytochemicals in ATC cells. In animal models, daidzein,
evodiamine, and resveratrol have been demonstrated to be effective
as anticancer or chemopreventive agents (93,94).
Only a few studies have reported that curcumin decreases the
genotoxicity of 131I therapy in patients with
differentiated thyroid cancer (DTC) (95). A supplement containing spirulina,
curcumin, and Boswellia has been shown to reduce the size of
thyroid nodules in euthyroid patients with benign thyroid nodules
(96).
 | Table I.Anticancer effects of different
phytochemicals in ATC cells. |
Table I.
Anticancer effects of different
phytochemicals in ATC cells.
| Phytochemicals | Cell growth
inhibition | Apoptosis
induction | Cell cycle
arrest | Angiogenesis
suppression | Autophagy
modulation | ROS activation |
|---|
| Aloperine | √ | √ | 0 | 0 | √ | 0 |
| Apigenin | √ | √ | 0 | 0 | 0 | 0 |
| Artemisinin | √ | 0 | √ | 0 | 0 | 0 |
| Baicalein | √ | √ | √ | 0 | √ | 0 |
| Chrysin | √ | √ | 0 | 0 | 0 | 0 |
| Curcumin | √ | √ | √ | 0 | 0 | 0 |
| Deguelin | √ | √ | √ | √ | 0 | 0 |
|
Epigallocatechin-3-gallate | √ | √ | √ | √ | 0 |
|
| Evodiamine | √ | √ | √ | 0 | 0 | √ |
| Indirubin | √ | √ | √ | 0 | 0 | 0 |
| Isoflavones
(genistein and daidzein) | √ | √ | 0 | 0 | 0 | √ |
| Myricetin | √ | √ | √ | 0 | 0 | 0 |
| Quercetin | √ | √ | √ | √ | √ | 0 |
| Resveratrol | √ | √ | √ | 0 | 0 | √ |
| Thymoquinone | √ | √ | 0 | √ | 0 | 0 |
| Triptolide | √ | √ | 0 | √ | 0 | 0 |
There are five types of thyroid cancer including
ATC, medullary thyroid carcinoma DTC, poorly differentiated thyroid
carcinoma, and Hurthle cell thyroid carcinoma (97). ATC is one of the most aggressive
human carcinomas, which arises from the follicular cells in the
thyroid gland. Although both ATC and DTC originate from thyroid
follicular cells, their clinical and biological features vary
considerably. The primary differences are shown in Table II. i) Incidence: ATC only accounts
for <1% of the total cases of thyroid tumors (98), whereas DTC accounts for >95% of
cases (99). ii) Gender ratio: DTC
patients have a female:male ratio of 3:1 (100), whereas this ratio in ATC is 1.5:2
(101). iii) Mortality: Although
the incidence of ATC is quite low (3.6% of all cases of thyroid
cancer in different areas) (102), deaths due to ATC account for
14–39% of all deaths due to thyroid cancer. The average survival
time of patients with ATC was 5–6 months (101). iv) Migration and invasiveness:
ATC is more prone to aggressive local disease and distant
metastasis than DTC. Approximately 97% of patients with ATC present
with a rapidly enlarging thyroid mass (103). Almost 50% of patients with ATC
were found to have distant metastasis at diagnosis. Metastasis also
occurred in approximately 25% of patients during their disease
course (104). Metastases mainly
involve the cervical lymph nodes in patients with DTC. v)
Biological features: ATC cells lose some biological features such
as iodine-uptake capacity and TSH dependence, which are
characteristic features of normal follicular cells (101). These features are still present
in DTC, and radioiodine ablation and TSH suppression are necessary
components of DTC treatment (98).
vi) Sensitivity to chemotherapy drugs: ATC is resistant to numerous
first-line anticancer drugs such as sorafenib and lenvatinib used
in a clinical setting to treat DTC (98,105).
 | Table II.Differences between ATC and DTC. |
Table II.
Differences between ATC and DTC.
| Type of cancer | Incidence (of total
cases) | Sex ratio
(F:M) | Lethality rate | Migration and
invasiveness | Thyroid-specific
features | Sensitivity to
chemotherapy drugs |
|---|
| DTC | >95% |
3:1 | Normal | Normal | Partly | Normal |
| ATC | <1% | 1.5:2 | High | Easily
appearing | None | Poor |
The anticancer effects of phytochemicals in DTC and
ATC differ. In DTC cells, resveratrol treatment led to cell growth
suppression, induction of apoptosis, cell cycle arrest, and
redifferentiation (68,106). Treatment with resveratrol (1–10
µM), was demonstrated to increase the activation of MAPK and the
protein levels of nuclear p53 protein, c-Fos, c-Jun, and p21 in DTC
cells (107). Moreover,
resveratrol enhanced the activation of Notch1, which is considered
a regulator of thyroid-specific gene expression (99) and the cause of autophagic flux in
DTC cells (108,109). However, this effect of
resveratrol was not observed in ATC cells. For example, resveratrol
promoted the apoptosis of ATC cells but did not increase MAPK
activation and p53 expression. Resveratrol also increased the
activation of Notch1 signaling and the protein expression of
thyroid-specific genes. Unfortunately, the location of important
thyroid-specific proteins, such as NIS, differs from that in normal
thyroid cells and is accompanied by a loss of function (72,76).
Quercetin was revealed to impel NIS protein expression and decrease
CD97 protein levels, a de-differentiation marker, in DTC cells
(68). However, while quercetin
decreased CD expression in both FRO and ARO ATC cells, it only
induced NIS protein expression in FRO ATC cells (68). These studies suggest that ATC, but
not DTC, may have unique drug-resistance mechanisms. Therefore,
effective drugs and therapies are urgently required for
undifferentiated thyroid cancer.
The mechanisms of drug resistance in ATC are poorly
understood. Some studies have hypothesized and found evidence for
the following aspects: i) STAT3 activation: Wu et al
reported that activation of STAT3 signaling is associated with the
resistance of ATC cells to resveratrol (74). Wang et al established the
connection between STAT3 and ATC resistance to BRAF inhibition
(110). ii) Drug- efflux pumps:
Abbasifarid et al suggested that ATP-binding cassette (ABC)
transporters ABCC1, ABCG2, and ABCB1 are the key determinants of
the resistance of ATC to chemotherapy (8). ABC transporters efflux anticancer
drugs and play a role in the development of drug resistance in
cancer cells (111). In addition,
signal transduction pathways such as PI3K/Akt (112), MAPK (113) and Notch (114) not only regulate the expression of
ABCC1, ABCG2, and ABCB1 but also participate in the development of
drug resistance. iii) Energy metabolism: Ma and Cheng demonstrated
that metabolic reprogramming in ATC cells confers upon them a
capacity of resistance to doxorubicin. Targeting 6-phosphogluconate
dehydrogenase overcame this drug resistance (115). A previous study by one of the
authors determined that PDH activity plays a role in the transient
resistance of ATC to artemisinin (116).
Phytochemicals such as resveratrol affect the
phosphorylation and nuclear translocation of STAT3 (74). Furthermore, they regulate some
signaling pathways that participate in drug resistance in ATC. For
example, aloperine, APG and baicalein were demonstrated to suppress
Akt activation in ATC cells (19,26,32).
Baicalein inhibited MAPK phosphorylation (34) and chysin increased Notch1
expression. Cancer is a metabolic disease with a special metabolic
profile in tumor cells (117).
Tumor cells depend on increased aerobic glycolysis by mitochondrial
oxidative phosphorylation to provide energy for their rapid growth,
invasion, and drug resistance. There are three major interferences
in tumor therapy, namely, dynamic cancer ecosystems, profitable
temporal and spatial diversity of environmental conditions, and
heritable cell phenotypes (118).
The evolution phenomenon known as competitive release explains how
drug-resistant cells attain a better opportunity to rapidly
proliferate by eliminating the drug-sensitive cells (118). It reveals that traditional
anticancer therapy to kill the majority of tumor cells as a
strategy to treat metastatic cancer is unreasonable from the point
of evolution. However, some alternative strategies have focused on
evolution-based methods that yield more benefits in the long-term
control compared with traditional therapy by only eliminating tumor
cells. Treatment with phytochemicals can alter several signaling
cascades and the modulation of the metabolic properties of cancer
cells (119). However, they also
influence the mitochondrial membrane potential and regulate the
mitochondrial metabolic pathways (120). For example, resveratrol not only
exerts its antitumor effects on ATC cells alone but can also
reverse drug resistance in these cells. Treatment of
resveratrol-sensitive ATC cells with resveratrol alone, leads to
changes in the morphological characteristics of mitochondria and an
increase in ROS production (75).
These results indicate that resveratrol suppresses ATC cell growth
and drug resistance through an impaired effect on mitochondria. In
a previous study by one of the authors, it was determined that
treatment with ART significantly changed mitochondrial protein
levels including the downregulation of COX7A2 and COX2 and the
upregulation of YEM1L1, ALAS1, COX14, and OAT after 48 h of
treatment. CAL-62 cells showed a transient and reversible
resistance to ART (only at 48 h), which was correlated to the
time-dependent changes in PDK1, HIF1a, and PDHA levels (117). These results suggest that
improved mitochondrial function may strongly be associated to drug
resistance in ATC cells. The inhibitory effect of phytochemicals of
ATC cells is important in overcoming drug resistance. The findings
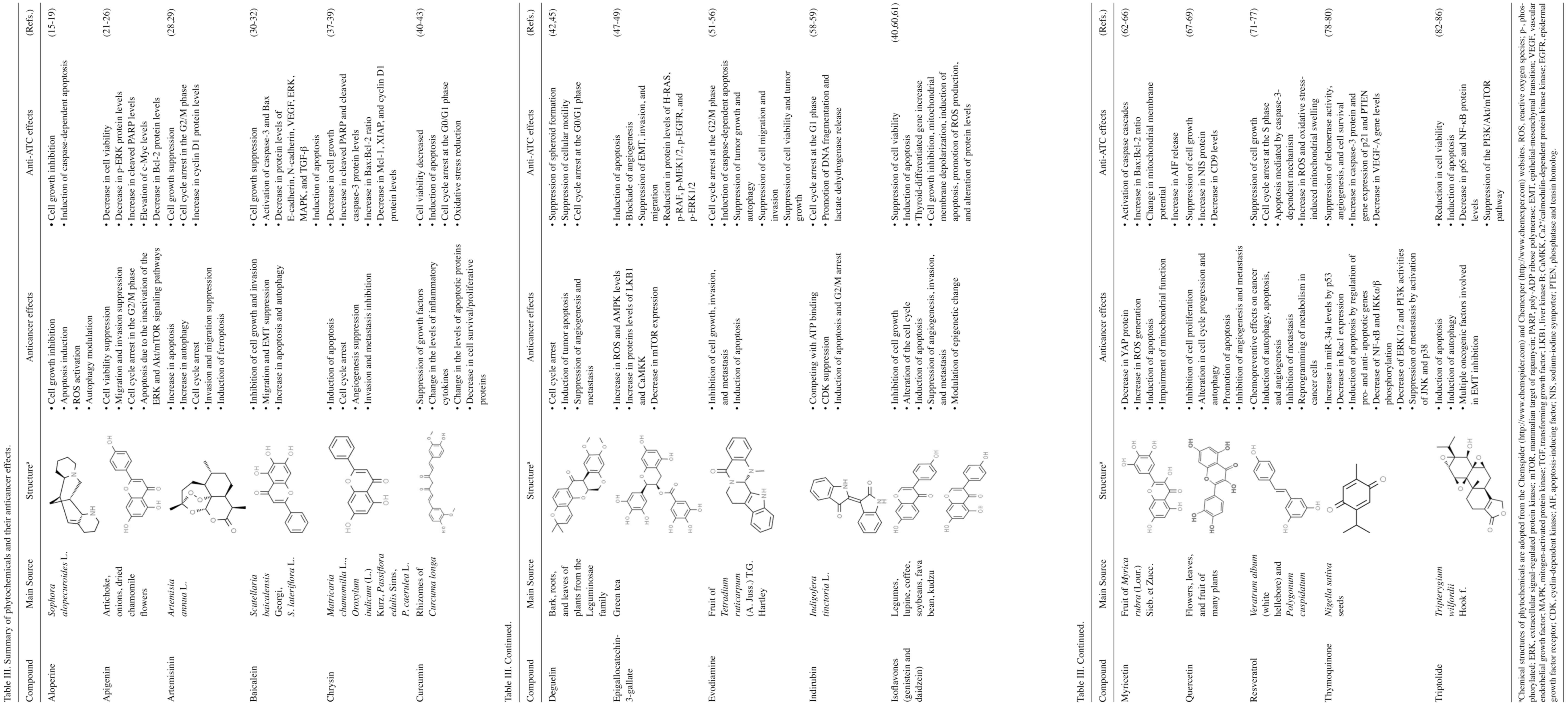
of the present review (Table III)
may improve the utility of phytochemicals as adjuvants in the
therapy of ATC, help prevent drug resistance, and provide a novel
perspective for further research on ATC therapy.
Acknowledgements
We are thankful for the generous support of Shandong
Provincial Natural Science Foundation.
Funding
This review was financially supported by the Shandong Provincial
Natural Science Foundation, China (grant no. ZR2020QC075).
Availability of data and materials
Not applicable.
Authors' contributions
JZ and YL contributed to the conception of the
present review. All authors (YL, JZ, HZ and ZD) contributed to the
resources, data curation, and writing of the manuscript as well as
the literature review analysis. ZD and YL reviewed and edited the
manuscript. Data authentication is not applicable. All authors read
and approved the final version of the manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
References
|
1
|
O'Neill JP and Shaha AR: Anaplastic
thyroid cancer. Oral Oncol. 49:702–706. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Saini S, Tulla K, Maker AV, Burman KD and
Prabhakar BS: Therapeutic advances in anaplastic thyroid cancer: A
current perspective. Mol Cancer. 17:1542018. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Tesselaar MH, Crezee T, Schuurmans I,
Gerrits D, Nagarajah J, Boerman OC, van Engen-van Grunsven I, Smit
JWA, Netea-Maier RT and Plantinga TS: Digitalislike compounds
restore hNIS expression and iodide uptake capacity in anaplastic
thyroid cancer. J Nucl Med. 59:780–786. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Haugen BR, Sawka AM, Alexander EK, Bible
KC, Caturegli P, Doherty GM, Mandel SJ, Morris JC, Nassar A, Pacini
F, et al: American thyroid association guidelines on the management
of thyroid nodules and differentiated thyroid cancer task force
review and recommendation on the proposed renaming of encapsulated
follicular variant papillary thyroid carcinoma without invasion to
noninvasive follicular thyroid neoplasm with papillary-like nuclear
features. Thyroid. 27:481–483. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Haddad RI, Nasr C, Bischoff L, Busaidy NL,
Byrd D, Callender G, Dickson P, Duh QY, Ehya H, Goldner W, et al:
NCCN guidelines insights: Thyroid carcinoma, version 2.2018. J Natl
Compr Cancer Netw. 16:1429–1440. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Zheng X, Cui D, Xu S, Brabant G and
Derwahl M: Doxorubicin fails to eradicate cancer stem cells derived
from anaplastic thyroid carcinoma cells: Characterization of
resistant cells. Int J Oncol. 37:307–315. 2010.PubMed/NCBI
|
|
7
|
Xu Y, Han YF, Ye B, Zhang YL, Dong JD, Zhu
SJ and Chen J: MiR-27b-3p is involved in doxorubicin resistance of
human anaplastic thyroid cancer cells via targeting peroxisome
proliferator-activated receptor gamma. Basic Clin Pharmacol
Toxicol. 123:670–677. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Abbasifarid E, Sajjadi-Jazi SM, Beheshtian
M, Samimi H, Larijani B and Haghpanah V: The role of ATP-binding
cassette transporters in the chemoresistance of anaplastic thyroid
cancer: A systematic review. Endocrinology. 160:2015–2023. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lan L, Basourakos S, Cui D, Zuo X, Deng W,
Huo L, Chen H, Zhang G, Deng L, Shi B and Luo Y: ATRA increases
iodine uptake and inhibits the proliferation and invasiveness of
human anaplastic thyroid carcinoma SW1736 cells: Involvement of
β-catenin phosphorylation inhibition. Oncol Lett. 14:7733–7738.
2017.PubMed/NCBI
|
|
10
|
Avila-Carrasco L, Majano P, Sánchez-Toméro
JA, Selgas R, López-Cabrera M, Aguilera A and Mateo GG: Natural
plants compounds as modulators of epithelial-to-mesenchymal
transition. Front Pharmacol. 10:7152019. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Chen CY, Kao CL and Liu CM: The cancer
prevention, anti-inflammatory and anti-oxidation of bioactive
phytochemicals targeting the TLR4 signaling pathway. Int J Mol Sci.
19:27292018. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Asadi-Samani M, Kooti W, Aslani E and
Shirzad H: A systematic review of Iran's medicinal plants with
anticancer effects. J Evid Based Complement Altern Med. 21:143–153.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Li YT, Tian XT, Wu ML, Zheng X, Kong QY,
Cheng XX, Zhu GW, Liu J and Li H: Resveratrol suppresses the growth
and enhances retinoic acid sensitivity of anaplastic thyroid cancer
cells. Int J Mol Sci. 19:10302018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Wang R, Deng X, Gao Q, Wu X, Han L, Gao X,
Zhao S, Chen W, Zhou R, Li Z and Bai C: Sophora alopecuroides L: An
ethnopharmacological, phytochemical, and pharmacological review. J
Ethnopharmacol. 248:1121722020. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tian D, Li Y, Li X and Tian Z: Aloperine
inhibits proliferation, migration and invasion and induces
apoptosis by blocking the Ras signaling pathway in human breast
cancer cells. Mol Med Rep. 18:3699–3710. 2018.PubMed/NCBI
|
|
16
|
Ling Z, Guan H, You Z, Wang C, Hu L, Zhang
L, Wang Y, Chen S, Xu B and Chen M: Aloperine executes antitumor
effects through the induction of apoptosis and cell cycle arrest in
prostate cancer in vitro and in vivo. Onco Targets Ther.
11:2735–2743. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Qiu M, Liu J, Su Y, Liu J, Wu C and Zhao
B: Aloperine induces apoptosis by a reactive oxygen species
activation mechanism in human ovarian cancer cells. Protein Pept
Lett. 27:860–869. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Yu HI, Shen HC, Chen SH, Lim YP, Chuang
HH, Tai TS, Kung FP, Lu CH, Hou CY, Lee YR, et al: Autophagy
modulation in human thyroid cancer cells following aloperine
treatment. Int J Mol Sci. 20:53152019. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Lee YR, Chen SH, Lin CY, Chao WY, Lim YP,
Yu HI and Lu CH: In vitro antitumor activity of aloperine on human
thyroid cancer cells through caspase-dependent apoptosis. Int J Mol
Sci. 19:3122018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Sharma A, Ghani A, Sak K, Tuli HS, Sharma
AK, Setzer WN, Sharma S and Das AK: Probing into therapeutic
anti-cancer potential of apigenin: Recent trends and future
directions. Recent Pat Inflamm Allergy Drug Discov. 13:124–133.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Zhao G, Han X, Cheng W, Ni J, Zhang Y, Lin
J and Song Z: Apigenin inhibits proliferation and invasion, and
induces apoptosis and cell cycle arrest in human melanoma cells.
Oncol Rep. 37:2277–2285. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Yin F, Giuliano AE and Van Herle AJ:
Growth inhibitory effects of flavonoids in human thyroid cancer
cell lines. Thyroid. 9:369–376. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Kim SH, Kang JG, Kim CS, Ihm SH, Choi MG,
Yoo HJ and Lee SJ: Apigenin induces c-Myc-mediated apoptosis in FRO
anaplastic thyroid carcinoma cells. Mol Cell Endocrinol.
369:130–139. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Yin F, Giuliano AE and Van Herle AJ:
Signal pathways involved in apigenin inhibition of growth and
induction of apoptosis of human anaplastic thyroid cancer cells
(ARO). Anticancer Res. 19:4297–4303. 1999.PubMed/NCBI
|
|
25
|
Kim SH, Kang JG, Kim CS, Ihm SH, Choi MG,
Yoo HJ and Lee SJ: Akt inhibition enhances the cytotoxic effect of
apigenin in combination with PLX4032 in anaplastic thyroid
carcinoma cells harboring BRAFV600E. J Endocrinol Invest.
36:1099–1104. 2013.PubMed/NCBI
|
|
26
|
Kim SH, Kang JG, Kim CS, Ihm SH, Choi MG,
Yoo HJ and Lee SJ: Suppression of AKT potentiates synergistic
cytotoxicity of apigenin with trail in anaplastic thyroid carcinoma
cells. Anticancer Res. 35:6529–6537. 2015.PubMed/NCBI
|
|
27
|
Ma N, Zhang Z, Liao F, Jiang T and Tu Y:
The birth of artemisinin. Pharmacol Ther. 216:1076582020.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Zhu S, Yu Q, Huo C, Li Y, He L, Ran B,
Chen J, Li Y and Liu W: Ferroptosis: A novel mechanism of
artemisinin and its derivatives in cancer therapy. Curr Med Chem.
28:329–345. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Li Y: Pyrvinium pamoate can overcome
artemisinin's resistance in anaplastic thyroid cancer. BMC
Complement Med Ther. 21:1562021. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Zeng Q, Zhang Y, Zhang W and Guo Q:
Baicalein suppresses the proliferation and invasiveness of
colorectal cancer cells by inhibiting snail-induced
epithelial-mesenchymal transition. Mol Med Rep. 21:2544–2552.
2020.PubMed/NCBI
|
|
31
|
Yu G, Chen L, Hu Y, Yuan Z, Luo Y and
Xiong Y: Antitumor effects of baicalein and its mechanism via TGFβ
pathway in cervical cancer hela cells. Evid Based Complement Altern
Med. 2021:55271902021.PubMed/NCBI
|
|
32
|
Yan W, Ma X, Zhao X and Zhang S: Baicalein
induces apoptosis and autophagy of breast cancer cells via
inhibiting PI3K/AKT pathway in vivo and vitro. Drug Des Devel Ther.
12:3961–3972. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Park CH, Han SE, Nam-Goong IS, Kim YI and
Kim ES: Combined effects of baicalein and docetaxel on apoptosis in
8505c anaplastic thyroid cancer cells via downregulation of the ERK
and Akt/mTOR pathways. Endocrinol Metab (Seoul). 33:121–132. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Han SE, Park CH, Nam-Goong IS, Kim YI and
Kim ES: Anticancer effects of baicalein in FRO thyroid cancer cells
through the up-regulation of ERK/p38 MAPK and Akt pathway. In Vivo.
33:375–382. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Naz S, Imran M, Rauf A, Orhan IE, Shariati
MA, Iahtisham-Ul-Haq, IqraYasmin, Shahbaz M, Qaisrani TB, Shah ZA,
et al: Chrysin: Pharmacological and therapeutic properties. Life
Sci. 235:1167972019. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Jung J: Emerging utilization of chrysin
using nanoscale modification. J Nanomater. 2016:e28940892016.
View Article : Google Scholar
|
|
37
|
Kasala ER, Bodduluru LN, Madana RM, Athira
KV, Gogoi R and Barua CC: Chemopreventive and therapeutic potential
of chrysin in cancer: Mechanistic perspectives. Toxicol Lett.
233:214–225. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Phan T, Yu XM, Kunnimalaiyaan M and Chen
H: Antiproliferative effect of chrysin on anaplastic thyroid
cancer. J Surg Res. 170:84–88. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Yu XM, Phan T, Patel PN, Jaskula-Sztul R
and Chen H: Chrysin activates notch1 signaling and suppresses tumor
growth of anaplastic thyroid carcinoma in vitro and in vivo.
Cancer. 119:774–781. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Giordano A and Tommonaro G: Curcumin and
cancer. Nutrients. 11:23762019. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Allegri L, Rosignolo F, Mio C, Filetti S,
Baldan F and Damante G: Effects of nutraceuticals on anaplastic
thyroid cancer cells. J Cancer Res Clin Oncol. 144:285–294. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Kocdor MA, Cengiz H, Ates H and Kocdor H:
Inhibition of cancer stem-like phenotype by curcumin and deguelin
in CAL-62 anaplastic thyroid cancer cells. Anticancer Agents Med
Chem. 19:1887–1898. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Hong JM, Park CS, Nam-Goong IS, Kim YS,
Lee JC, Han MW, Choi JI, Kim YI and Kim ES: Curcumin enhances
docetaxel-induced apoptosis of 8505C anaplastic thyroid carcinoma
cells. Endocrinol Metab (Seoul). 29:54–61. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Boyd J and Han A: Deguelin and its role in
chronic diseases. Adv Exp Med Biol. 929:363–375. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Tuli HS, Mittal S, Loka M, Aggarwal V,
Aggarwal D, Masurkar A, Kaur G, Varol M, Sak K, Kumar M, et al:
Deguelin targets multiple oncogenic signaling pathways to combat
human malignancies. Pharmacol Res. 166:1054872021. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Kim HS, Quon MJ and Kim JA: New insights
into the mechanisms of polyphenols beyond antioxidant properties;
lessons from the green tea polyphenol, epigallocatechin 3-gallate.
Redox Biol. 2:187–195. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Hayakawa S, Ohishi T, Miyoshi N, Oishi Y,
Nakamura Y and Isemura M: Anti-cancer effects of green tea
epigallocatchin–3-gallate and coffee chlorogenic acid. Molecules.
25:45532020. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Wu D, Liu Z, Li J, Zhang Q, Zhong P, Teng
T, Chen M, Xie Z, Ji A and Li Y: Epigallocatechin-3-gallate
inhibits the growth and increases the apoptosis of human thyroid
carcinoma cells through suppression of EGFR/RAS/RAF/MEK/ERK
signaling pathway. Cancer Cell Int. 19:432019. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Li T, Zhao N, Lu J, Zhu Q, Liu X, Hao F
and Jiao X: Epigallocatechin gallate (EGCG) suppresses
epithelial-mesenchymal transition (EMT) and invasion in anaplastic
thyroid carcinoma cells through blocking of TGF-β1/smad signaling
pathways. Bioengineered. 10:282–291. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Jiang ZB, Huang JM, Xie YJ, Zhang YZ,
Chang C, Lai HL, Wang W, Yao XJ, Fan XX, Wu QB, et al: Evodiamine
suppresses non-small cell lung cancer by elevating CD8+ T cells and
downregulating the MUC1-C/PD-L1 axis. J Exp Clin Cancer Res.
39:2492020. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Luo C, Ai J, Ren E, Li J, Feng C, Li X and
Luo X: Research progress on evodiamine, a bioactive alkaloid of
Evodiae fructus: Focus on its anti-cancer activity and
bioavailability (Review). Exp Ther Med. 22:13272021. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Chen MC, Yu CH, Wang SW, Pu HF, Kan SF,
Lin LC, Chi CW, Ho LLT, Lee CH and Wang PS: Anti-proliferative
effects of evodiamine on human thyroid cancer cell line ARO. J Cell
Biochem. 110:1495–1503. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Yu HI, Chou HC, Su YC, Lin LH, Lu CH,
Chuang HH, Tsai YT, Liao EC, Wei YS, Yang YT, et al: Proteomic
analysis of evodiamine-induced cytotoxicity in thyroid cancer
cells. J Pharm Biomed Anal. 160:344–350. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Kim SH, Kang JG, Kim CS, Ihm SH, Choi MG
and Lee SJ: Evodiamine suppresses survival, proliferation,
migration and epithelial-mesenchymal transition of thyroid
carcinoma cells. Anticancer Res. 38:6339–6352. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Kim SH, Kang JG, Kim CS, Ihm SH, Choi MG
and Lee SJ: Evodiamine in combination with histone deacetylase
inhibitors has synergistic cytotoxicity in thyroid carcinoma cells.
Endocrine. 65:110–120. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Chien CC, Wu MS, Chou SW, Jargalsaikhan G
and Chen YC: Roles of reactive oxygen species, mitochondrial
membrane potential, and p53 in evodiamine-induced apoptosis and
G2/M arrest of human anaplastic thyroid carcinoma cells. Chin Med.
16:1342021. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Xiao Z, Hao Y, Liu B and Qian L: Indirubin
and meisoindigo in the treatment of chronic myelogenous leukemia in
China. Leuk Lymphoma. 43:1763–1768. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Hoessel R, Leclerc S, Endicott JA, Nobel
ME, Lawrie A, Tunnah P, Leost M, Damiens E, Marie D, Marko D, et
al: Indirubin, the active constituent of a Chinese antileukaemia
medicine, inhibits cyclin-dependent kinases. Nat Cell Biol.
1:60–67. 1999. View
Article : Google Scholar : PubMed/NCBI
|
|
59
|
Broecker-Preuss M, Becher-Boveleth N, Gall
S, Rehmann K, Schenke S and Mann K: Induction of atypical cell
death in thyroid carcinoma cells by the indirubin derivative
7-bromoindirubin-3′-oxime (7BIO). Cancer Cell Int. 15:972015.
View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Mukund V, Mukund D, Sharma V, Mannarapu M
and Alam A: Genistein: Its role in metabolic diseases and cancer.
Crit Rev Oncol Hematol. 119:13–22. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Ahn JC, Biswas R and Chung PS: Combination
with genistein enhances the efficacy of photodynamic therapy
against human anaplastic thyroid cancer cells. Lasers Surg Med.
44:840–849. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Li M, Chen J, Yu X, Xu S, Li D, Zheng Q
and Yin Y: Myricetin suppresses the propagation of hepatocellular
carcinoma via down-regulating expression of YAP. Cells. 8:3582019.
View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Knickle A, Fernando W, Greenshields AL,
Rupasinghe HPV and Hoskin DW: Myricetin-induced apoptosis of
triple-negative breast cancer cells is mediated by the
iron-dependent generation of reactive oxygen species from hydrogen
peroxide. Food Chem Toxicol. 118:154–167. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Xu Y, Xie Q, Wu S, Yi D, Yu Y, Liu S, Li S
and Li Z: Myricetin induces apoptosis via endoplasmic reticulum
stress and DNA double-strand breaks in human ovarian cancer cells.
Mol Med Rep. 13:2094–2100. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Ma L, Cao X, Wang H, Lu K, Wang Y, Tu C,
Dai Y, Meng Y, Li Y, Yu P, et al: Discovery of Myricetin as a
potent inhibitor of human flap endonuclease 1, which potentially
can be used as sensitizing agent against HT-29 human colon cancer
cells. J Agric Food Chem. 67:1656–1665. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Jo S, Ha TK, Han SH, Kim ME, Jung I, Lee
HW, Bae SK and Lee JS: Myricetin induces apoptosis of human
anaplastic thyroid cancer cells via mitochondria dysfunction.
Anticancer Res. 37:1705–1710. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Tang SM, Deng XT, Zhou J, Li QP, Ge XX and
Miao L: Pharmacological basis and new insights of quercetin action
in respect to its anti-cancer effects. Biomed Pharmacother.
121:1096042020. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Kang HJ, Youn YK, Hong MK and Kim LS:
Antiproliferation and redifferentiation in thyroid cancer cell
lines by polyphenol phytochemicals. J Korean Med Sci. 26:893–899.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Hoang-Vu C, Bull K, Schwarz I, Krause G,
Schmutzler C, Aust G, Köhrle J and Dralle H: Regulation of CD97
protein in thyroid carcinoma. J Clin Endocrinol Metab.
84:1104–1109. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Ren B, Kwah MXY, Liu C, Ma Z, Shanmugam
MK, Ding L, Xiang X, Ho PCL, Wang L, Ong PS and Goh BC: Resveratrol
for cancer therapy: Challenges and future perspectives. Cancer
Lett. 515:63–72. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Rauf A, Imran M, Butt MS, Nadeem M, Peters
DG and Mubarak MS: Resveratrol as an anti-cancer agent: A review.
Crit Rev Food Sci Nutr. 58:1428–1447. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Yu XM, Jaskula-Sztul R, Ahmed K, Harrison
AD, Kunnimalaiyaan M and Chen H: Resveratrol induces
differentiation markers expression in anaplastic thyroid carcinoma
via activation of notch1 signaling and suppresses cell growth. Mol
Cancer Ther. 12:1276–1287. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Liu X, Li H, Wu ML, Wu J, Sun Y, Zhang KL
and Liu J: Resveratrol reverses retinoic acid resistance of
anaplastic thyroid cancer cells via demethylating CRABP2 gene.
Front Endocrinol (Lausanne). 10:7342019. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Wu J, Li YT, Tian XT, Liu YS, Wu ML, Li PN
and Liu J: STAT3 signaling statuses determine the fate of
resveratrol-treated anaplastic thyroid cancer cells. Cancer Biomark
Sect Dis Markers. 27:461–469. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Zheng X, Jia B, Tian XT, Song X, Wu ML,
Kong QY, Li H and Liu J: Correlation of reactive oxygen species
levels with resveratrol sensitivities of anaplastic thyroid cancer
cells. Oxid Med Cell Longev. 2018:62354172018. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Xiong L, Nie JH, Lin XM, Wu JB, Chen Z, Xu
B and Liu J: Biological implications of PTEN upregulation and
altered sodium/iodide symporter intracellular distribution in
resveratrol-suppressed anaplastic thyroid cancer cells. J Cancer.
11:6883–6891. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Xiong L, Lin XM, Nie JH, Ye HS and Liu J:
Resveratrol and its nanoparticle suppress
doxorubicin/docetaxel-resistant anaplastic thyroid cancer cells in
vitro and in vivo. Nanotheranostics. 5:143–154. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Imran M, Rauf A, Khan IA, Shahbaz M,
Qaisrani TB, Fatmawati S, Abu-Izneid T, Imran A, Rahman KU and
Gondal TA: Thymoquinone: A novel strategy to combat cancer: A
review. Biomed Pharmacother Biomedecine Pharmacother. 106:390–402.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Zhang M, Du H, Wang L, Yue Y, Zhang P,
Huang Z, Lv W, Ma J, Shao Q, Ma M, et al: Thymoquinone suppresses
invasion and metastasis in bladder cancer cells by reversing EMT
through the Wnt/β-catenin signaling pathway. Chem Biol Interact.
320:1090222020. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Ozturk SA, Alp E, Saglam ASY, Konac E and
Menevse ES: The effects of thymoquinone and genistein treatment on
telomerase activity, apoptosis, angiogenesis, and survival in
thyroid cancer cell lines. J Cancer Res Ther. 14:328–334.
2018.PubMed/NCBI
|
|
81
|
Kupchan SM, Court WA, Dailey RG Jr,
Gilmore CJ and Bryan RF: Triptolide and tripdiolide, novel
antileukemic diterpenoid triepoxides from Tripterygium wilfordii. J
Am Chem Soc. 94:7194–7195. 1972. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Noel P, Von Hoff DD, Saluja AK, Velagapudi
M, Borazanci E and Han H: Triptolide and its derivatives as cancer
therapies. Trends Pharmacol Sci. 40:327–341. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Zhu W, Hu H, Qiu P and Yan G: Triptolide
induces apoptosis in human anaplastic thyroid carcinoma cells by a
p53-independent but NF-kappaB-related mechanism. Oncol Rep.
22:1397–1401. 2009.PubMed/NCBI
|
|
84
|
Zhu W, Ou Y, Li Y, Xiao R, Shu M, Zhou Y,
Xie J, He S, Qiu P and Yan G: A small-molecule triptolide
suppresses angiogenesis and invasion of human anaplastic thyroid
carcinoma cells via down-regulation of the nuclear factor-kappa B
pathway. Mol Pharmacol. 75:812–819. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Zhu W, He S, Li Y, Qiu P, Shu M, Ou Y,
Zhou Y, Leng T, Xie J, Zheng X, et al: Anti-angiogenic activity of
triptolide in anaplastic thyroid carcinoma is mediated by targeting
vascular endothelial and tumor cells. Vascul Pharmacol. 52:46–54.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Kim SH, Kang JG, Kim CS, Ihm SH, Choi MG,
Yoo HJ and Lee SJ: Synergistic cytotoxicity of BIIB021 with
triptolide through suppression of PI3K/Akt/mTOR and NF-κB signal
pathways in thyroid carcinoma cells. Biomed Pharmacother. 83:22–32.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Chikara S, Nagaprashantha LD, Singhal J,
Horne D, Awasthi S and Singhal SS: Oxidative stress and dietary
phytochemicals: Role in cancer chemoprevention and treatment.
Cancer Lett. 413:122–134. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Ahmad SS, Waheed T, Rozeen S, Mahmood S
and Kamal MA: Therapeutic study of phytochemicals against cancer
and Alzheimer's disease management. Curr Drug Metab. 20:1006–1013.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Tendulkar S and Dodamani S:
Chemoresistance in ovarian cancer: Prospects for new drugs.
Anticancer Agents Med Chem. 21:668–678. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Shin HJ, Hwang KA and Choi KC: Antitumor
effect of various phytochemicals on diverse types of thyroid
cancers. Nutrients. 11:1252019. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Manach C, Williamson G, Morand C, Scalbert
A and Rémésy C: Bioavailability and bioefficacy of polyphenols in
humans. I. Review of 97 bioavailability studies. Am J Clin Nutr. 81
(1 Suppl):230S–242S. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Pannu N and Bhatnagar A: Resveratrol: From
enhanced biosynthesis and bioavailability to multitargeting chronic
diseases. Biomed Pharmacother. 109:2237–2251. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Somjen D, Grafi-Cohen M, Katzburg S,
Weisinger G, Izkhakov E, Nevo N, Sharon O, Kraiem Z, Kohen F and
Stern N: Anti-thyroid cancer properties of a novel isoflavone
derivative, 7-(O)-carboxymethyl daidzein conjugated to
N-t-Boc-hexylenediamine in vitro and in vivo. J Steroid Biochem Mol
Biol. 126:95–103. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Zheng X, Jia B, Song X, Kong QY, Wu ML,
Qiu ZW, Li H and Liu J: Preventive potential of resveratrol in
carcinogen-induced rat thyroid tumorigenesis. Nutrients.
10:2792018. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Jafarpour SM, Safaei M, Mohseni M,
Salimian M, Aliasgharzadeh A and Farhood B: The radioprotective
effects of curcumin and trehalose against genetic damage caused by
I-131. Indian J Nucl Med. 33:99–104. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Stancioiu F, Mihai D, Papadakis GZ,
Tsatsakis A, Spandidos DA and Badiu C: Treatment for benign thyroid
nodules with a combination of natural extracts. Mol Med Rep.
20:2332–2338. 2019.PubMed/NCBI
|
|
97
|
Chmielik E, Rusinek D, Oczko-Wojciechowska
M, Jarzab M, Krajewska J, Czarniecka A and Jarzab B: Heterogeneity
of thyroid cancer. Pathobiolgy. 85:117–129. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Cabanillas ME, McFadden DG and Durante C:
Thyroid cancer. Lancet. 388:2783–2795. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Howlader N, Noone AM, Krapcho M, Miller D,
Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS,
Feuer EJ and Cronin KA: SEER Cancer Statistics Review, 1975–2018.
National Cancer Institute; Bethesda, MD: 2018
|
|
100
|
La Vecchia C, Malvezzi M, Bosetti C,
Garavello W, Bertuccio P, Levi F and Negri E: Thyroid cancer
mortality and incidence: A global overview. Int J Cancer.
136:2187–2195. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Molinaro E, Romei C, Biagini A, Sabini E,
Agate L, Mazzeo S, Materazzi G, Sellari-Franceschini S, Ribechini
A, Torregrossa L, et al: Anaplastic thyroid carcinoma: From
clinicopathology to genetics and advanced therapies. Nat Rev
Endocrinol. 13:644–660. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Smallridge RC and Copland JA: Anaplastic
thyroid carcinoma: Pathogenesis and emerging therapies. Clin Oncol
(R Coll Radiol). 22:486–497. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Ain KB: Anaplastic thyroid carcinoma:
Behavior, biology, and therapeutic approaches. Thyroid. 8:715–726.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Glaser SM, Mandish SF, Gill BS,
Balasubramani GK, Clump DA and Beriwal S: Anaplastic thyroid
cancer: Prognostic factors, patterns of care, and overall survival.
Head Neck. 38 (Suppl 1):E2083–E2090. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Ferrari SM, Elia G, Ragusa F, Ruffilli I,
Motta CL, Paparo SR, Patrizio A, Vita R, Benvenga S, Materazzi G,
et al: Novel treatments for anaplastic thyroid carcinoma. Gland
Surg. 9 (Suppl 1):S28–S42. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Xu G, Chen J, Wang G, Xiao J, Zhang N,
Chen Y, Yu H, Wang G and Zhao Y: Resveratrol inhibits the
tumorigenesis of follicular thyroid cancer via ST6GAL2-regulated
activation of the hippo signaling pathway. Mol Ther Oncolytics.
16:124–133. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Shih A, Davis FB, Lin HY and Davis PJ:
Resveratrol induces apoptosis in thyroid cancer cell lines via a
MAPK- and p53-dependent mechanism. J Clin Endocrinol Metab.
87:1223–1232. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Ferretti E, Tosi E, Po A, Scipioni A,
Morisi R, Espinola MS, Russo D, Durante C, Schlumberger M,
Screpanti I, et al: Notch signaling is involved in expression of
thyrocyte differentiation markers and is down-regulated in thyroid
tumors. J Clin Endocrinol Metab. 93:4080–4087. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Davis RJ, Pinchot S, Jarjour S,
Kunnimalaiyaan M and Chen H: Resveratrol-induced notch activation
potentially mediates autophagy in human follicular thyroid cancer
cells. J Surg Res. 2:331–332. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Wang Y, Hu Z, Ma W, Niu Y, Su J, Zhang L
and Zhao P: Signal transducer and activator of transcription 3
inhibition alleviates resistance to BRAF inhibition in anaplastic
thyroid cancer. Invest New Drugs. 39:764–774. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Kartal-Yandim M, Adan-Gokbulut A and Baran
Y: Molecular mechanisms of drug resistance and its reversal in
cancer. Crit Rev Biotechnol. 36:716–726. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Pick A and Wiese M: Tyrosine kinase
inhibitors influence ABCG2 expression in EGFR-positive MDCK BCRP
cells via the PI3K/Akt signaling pathway. ChemMedChem. 7:650–662.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Hoffmann K, Shibo L, Xiao Z, Longerich T,
Büchler MW and Schemmer P: Correlation of gene expression of
ATP-binding cassette protein and tyrosine kinase signaling pathway
in patients with hepatocellular carcinoma. Anticancer Res.
31:3883–3890. 2011.PubMed/NCBI
|
|
114
|
Wang Z, Li Y, Ahmad A, Azmi AS, Banerjee
S, Kong D and Sarkar FH: Targeting notch signaling pathway to
overcome drug resistance for cancer therapy. Biochim Biophys Acta.
1806:258–267. 2010.PubMed/NCBI
|
|
115
|
Ma L and Cheng Q: Inhibiting
6-phosphogluconate dehydrogenase reverses doxorubicin resistance in
anaplastic thyroid cancer via inhibiting NADPH-dependent metabolic
reprogramming. Biochem Biophys Res Commun. 498:912–917. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Li Y: Inactivation of PDH can reduce
anaplastic thyroid cancer cells' sensitivity to artemisinin.
Anticancer Agents Med Chem. 22:1753–1760. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Warburg O: On the origin of cancer cells.
Science. 123:309–314. 1956. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Enriquez-Navas PM, Wojtkowiak JW and
Gatenby RA: Application of evolutionary principles to cancer
therapy. Cancer Res. 75:4675–4680. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Siddiqui FA, Prakasam G, Chattopadhyay S,
Rehman AU, Padder RA, Ansari MA, Irshad R, Mangalhara K, Bamezai
RNK, Husain M, et al: Curcumin decreases Warburg effect in cancer
cells by down-regulating pyruvate kinase M2 via mTOR-HIF1α
inhibition. Sci Rep. 8:83232018. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Gibellini L, Bianchini E, De Biasi S, Nasi
M, Cossarizza A and Pinti M: Natural compounds modulating
mitochondrial functions. Evid Based Complement Altern Med.
2015:5272092015. View Article : Google Scholar : PubMed/NCBI
|