|
1
|
McGlynn KA, Petrick JL and El-Serag HB:
Epidemiology of hepatocellular carcinoma. Hepatology. 73 (Suppl
1):S4–S13. 2021. View Article : Google Scholar
|
|
2
|
Fujiwara N, Friedman S, Goossens N and
Hoshida Y: Risk factors and prevention of hepatocellular carcinoma
in the era of precision medicine. J Hepatol. 68:526–549. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Villanueva A: Hepatocellular carcinoma. N
Engl J Med. 380:1450–1462. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Calderaro J, Ziol M, Paradis V and
Zucman-Rossi J: Molecular and histological correlations in liver
cancer. J Hepatol. 71:616–630. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Craig A, von Felden J, Garcia-Lezana T,
Sarcognato S and Villanueva A: Tumour evolution in hepatocellular
carcinoma. Nat Rev Gastroenterol Hepatol. 17:139–152. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sia D, Villanueva A, Friedman S and Llovet
J: Liver cancer cell of origin, molecular class, and effects on
patient prognosis. Gastroenterology. 152:745–761. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Yang JD, Hainaut P, Gores GJ, Amadou A,
Plymoth A and Roberts LR: A global view of hepatocellular
carcinoma: Trends, risk, prevention and management. Nat Rev
Gastroenterol Hepatol. 16:589–604. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Bruix J, Gores GJ and Mazzaferro V:
Hepatocellular carcinoma: Clinical frontiers and perspectives. Gut.
63:844–855. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Llovet J, Montal R, Sia D and Finn R:
Molecular therapies and precision medicine for hepatocellular
carcinoma. Nat Rev Clin Oncol. 15:599–616. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Chan LK and Ng IO: Joining the dots for
better liver cancer treatment. Nat Rev Gastroenterol Hepatol.
17:74–75. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
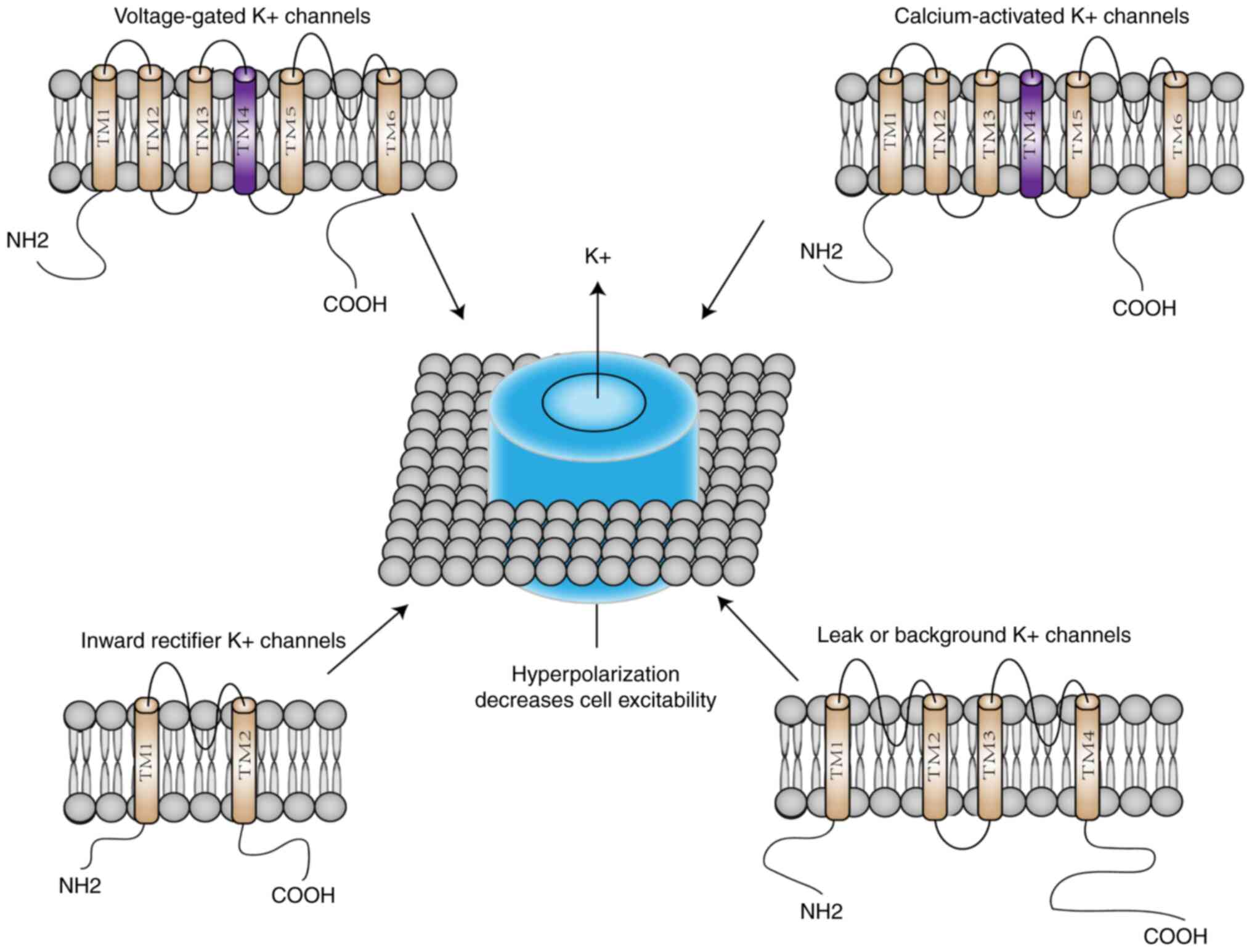
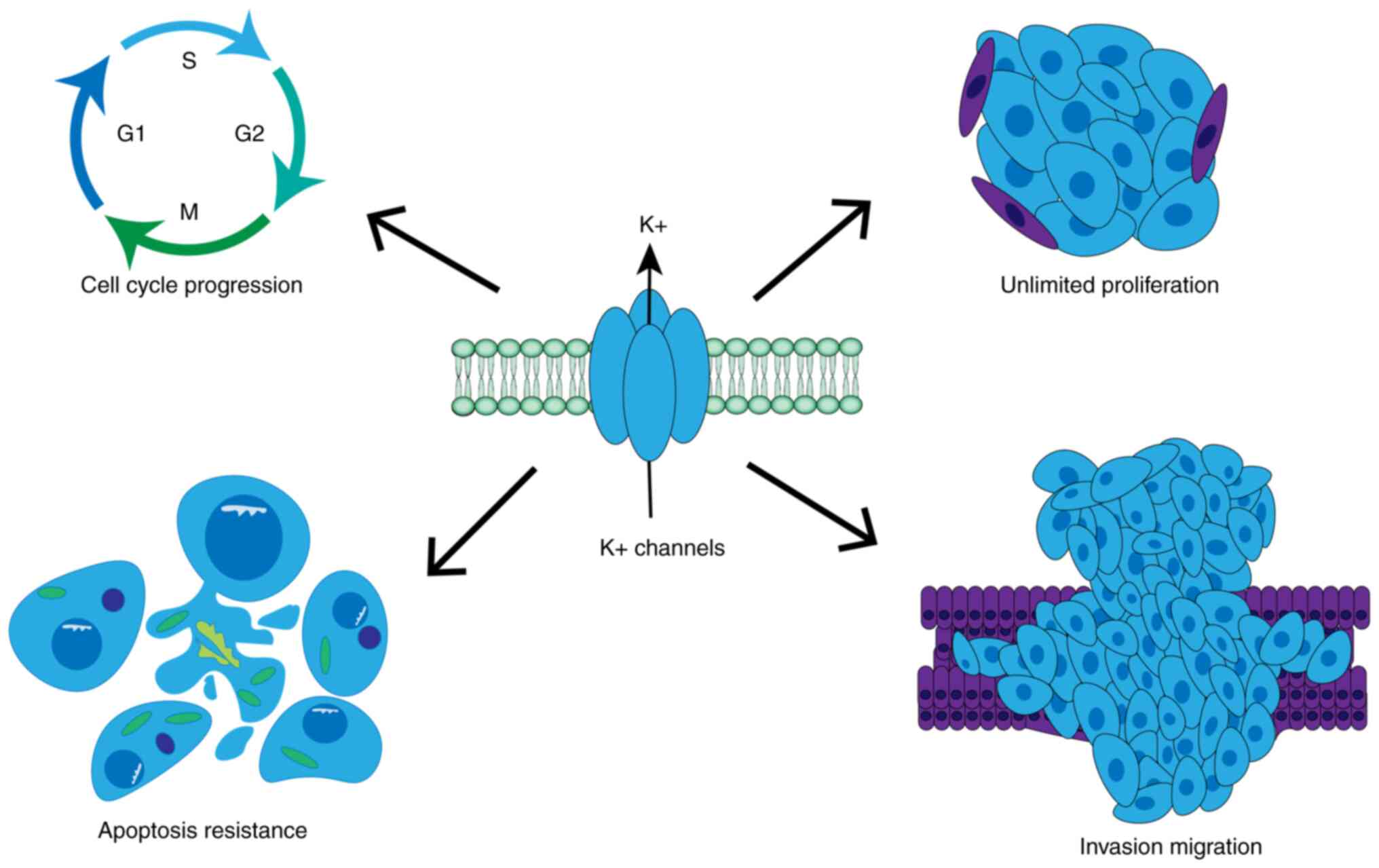
Kunzelmann K: Ion channels and cancer. J
Membr Biol. 205:159–173. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lang F, Föller M, Lang KS, Lang PA, Ritter
M, Gulbins E, Vereninov A and Huber SM: Ion channels in cell
proliferation and apoptotic cell death. J Membr Biol. 205:147–157.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Prevarskaya N, Skryma R and Shuba Y: Ion
channels in cancer: Are cancer hallmarks oncochannelopathies?
Physiol Rev. 98:559–621. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Prevarskaya N, Skryma R and Shuba Y: Ion
channels and the hallmarks of cancer. Trends Mol Med. 16:107–121.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Huang X and Jan LY: Targeting potassium
channels in cancer. J Cell Biol. 206:151–162. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Conti M: Targeting K+ channels for cancer
therapy. J Exp Ther Oncol. 4:161–166. 2004.PubMed/NCBI
|
|
17
|
Teisseyre A, Gąsiorowska J and Michalak K:
Voltage-gated potassium channels Kv1.3-potentially new molecular
target in cancer diagnostics and therapy. Adv Clin Exp Med.
24:517–524. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kale VP, Amin SG and Pandey MK: Targeting
ion channels for cancer therapy by repurposing the approved drugs.
Biochim Biophys Acta. 1848:2747–2755. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kuang Q, Purhonen P and Hebert H:
Structure of potassium channels. Cell Mol Life Sci. 72:3677–3693.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Bates E: Ion channels in development and
cancer. Annu Rev Cell Dev Biol. 31:231–247. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Comes N, Serrano-Albarrás A, Capera J,
Serrano-Novillo C, Condom E, Ramón Y Cajal S, Ferreres JC and
Felipe A: Involvement of potassium channels in the progression of
cancer to a more malignant phenotype. Biochim Biophys Acta.
1848:2477–2492. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Zúñiga L, Cayo A, Gonzalez W, Vilos C and
Zúñiga R: Potassium channels as a target for cancer therapy:
Current perspectives. Onco Targets Ther. 15:783–797. 2022.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Taylor MD, Northcott PA, Korshunov A,
Remke M, Cho YJ, Clifford SC, Eberhart CG, Parsons DW, Rutkowski S,
Gajjar A, et al: Molecular subgroups of medulloblastoma: The
current consensus. Acta Neuropathol. 123:465–472. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Comes N, Bielanska J, Vallejo-Gracia A,
Serrano-Albarrás A, Marruecos L, Gómez D, Soler C, Condom E, Ramón
Y Cajal S, Hernández-Losa J, et al: The voltage-dependent K(+)
channels Kv1.3 and Kv1.5 in human cancer. Front Physiol. 4:2832013.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Pillozzi S, Masselli M, De Lorenzo E,
Accordi B, Cilia E, Crociani O, Amedei A, Veltroni M, D'Amico M,
Basso G, et al: Chemotherapy resistance in acute lymphoblastic
leukemia requires hERG1 channels and is overcome by hERG1 blockers.
Blood. 117:902–914. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Hemmerlein B, Weseloh RM, Mello de Queiroz
F, Knötgen H, Sánchez A, Rubio ME, Martin S, Schliephacke T, Jenke
M, Heinz-Joachim-Radzun, et al: Overexpression of Eag1 potassium
channels in clinical tumours. Mol Cancer. 5:412006. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Pardo LA and Stühmer W: The roles of K(+)
channels in cancer. Nat Rev Cancer. 14:39–48. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Bachmann M, Li W, Edwards MJ, Ahmad SA,
Patel S, Szabo I and Gulbins E: Voltage-gated potassium channels as
regulators of cell death. Front Cell Dev Biol. 8:6118532020.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Shen Z, Yang Q and You Q: Researches
toward potassium channels on tumor progressions. Curr Top Med Chem.
9:322–329. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Wang Z: Roles of K+ channels in regulating
tumour cell proliferation and apoptosis. Pflugers Arch.
448:274–286. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ben-Moshe S and Itzkovitz S: Spatial
heterogeneity in the mammalian liver. Nat Rev Gastroenterol
Hepatol. 16:395–410. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Liu J, Lv XW, Zhang L, Wang H, Li J and Wu
B: Review on biological characteristics of Kv1.3 and its role in
liver diseases. Front Pharmacol. 12:6525082021. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Sevelsted Møller L, Fialla AD, Schierwagen
R, Biagini M, Liedtke C, Laleman W, Klein S, Reul W, Koch Hansen L,
Rabjerg M, et al: The calcium-activated potassium channel KCa3.1 is
an important modulator of hepatic injury. Sci Rep. 6:287702016.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kondo R, Deguchi A, Kawata N, Suzuki Y and
Yamamura H: Involvement of TREK1 channels in the proliferation of
human hepatic stellate LX-2 cells. J Pharmacol Sci. 148:286–294.
2022. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Xia Z, Huang X, Chen K, Wang H, Xiao J, He
K, Huang R, Duan X, Liu H, Zhang J and Xiang G: Proapoptotic role
of potassium ions in liver cells. Biomed Res Int. 2016:17291352016.
View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Craig A and Villanueva A: Liver capsule:
Molecular-based signatures in hepatocellular carcinoma. Hepatology.
63:20182016. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Ghatta S, Nimmagadda D, Xu X and O'Rourke
ST: Large-conductance, calcium-activated potassium channels:
Structural and functional implications. Pharmacol Ther.
110:103–116. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Marty A: Ca-dependent K channels with
large unitary conductance in chromaffin cell membranes. Nature.
291:497–500. 1981. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Knaus HG, Schwarzer C, Koch RO, Eberhart
A, Kaczorowski GJ, Glossmann H, Wunder F, Pongs O, Garcia ML and
Sperk G: Distribution of high-conductance Ca(2+)-activated K+
channels in rat brain: Targeting to axons and nerve terminals. J
Neurosci. 16:955–963. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
He Y, Lin Y and He F, Shao L, Ma W and He
F: Role for calcium-activated potassium channels (BK) in migration
control of human hepatocellular carcinoma cells. J Cell Mol Med.
25:9685–9696. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Wulff H and Castle N: Therapeutic
potential of KCa3.1 blockers: Recent advances and promising trends.
Expert Rev Clin Pharmacol. 3:385–396. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Todesca LM, Maskri S, Brömmel K, Thale I,
Wünsch B, Koch O and Schwab A: Targeting Kca3.1 channels
in cancer. Cell Physiol Biochem. 55:131–144. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Song P, Du Y, Song W, Chen H, Xuan Z, Zhao
L, Chen J, Chen J, Guo D, Jin C, et al: KCa3.1 as an effective
target for inhibition of growth and progression of intrahepatic
cholangiocarcinoma. J Cancer. 8:1568–1578. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Fan J, Tian R, Yang X, Wang H, Shi Y, Fan
X, Zhang J, Chen Y, Zhang K, Chen Z and Li L: KCNN4 promotes the
stemness potentials of liver cancer stem cells by enhancing glucose
metabolism. Int J Mol Sci. 23:69582022. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Du Y, Song W, Chen J, Chen H, Xuan Z, Zhao
L, Chen J, Jin C, Zhou M, Tuo B, et al: The potassium channel
KCa3.1 promotes cell proliferation by activating SKP2 and
metastasis through the EMT pathway in hepatocellular carcinoma. Int
J Cancer. 145:503–516. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Li QT, Feng YM, Ke ZH, Qiu MJ, He XX, Wang
MM, Li YN, Xu J, Shi LL and Xiong ZF: KCNN4 promotes invasion and
metastasis through the MAPK/ERK pathway in hepatocellular
carcinoma. J Investig Med. 68:68–74. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Ranjan A, Iyer SV, Ward C, Link T, Diaz
FJ, Dhar A, Tawfik OW, Weinman SA, Azuma Y, Izumi T and Iwakuma T:
MTBP inhibits the Erk1/2-Elk-1 signaling in hepatocellular
carcinoma. Oncotarget. 9:21429–21443. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Rodríguez-Rasgado J, Acuña-Macías I and
Camacho J: Eag1 channels as potential cancer biomarkers. Sensors
(Basel). 12:5986–5995. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Chávez-López MG, Zúñiga-García V,
Pérez-Carreón JI, Avalos-Fuentes A, Escobar Y and Camacho J: Eag1
channels as potential early-stage biomarkers of hepatocellular
carcinoma. Biologics. 10:139–148. 2016.PubMed/NCBI
|
|
50
|
Chen J, Xuan Z, Song W, Han W, Chen H, Du
Y, Xie H, Zhao Y, Zheng S and Song P: EAG1 enhances hepatocellular
carcinoma proliferation by modulating SKP2 and metastasis through
pseudopod formation. Oncogene. 40:163–176. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Lotshaw D: Biophysical, pharmacological,
and functional characteristics of cloned and native mammalian
two-pore domain K+ channels. Cell Biochem Biophys. 47:209–256.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Kheradpezhouh E, Ma L, Morphett A, Barritt
GJ and Rychkov GY: TRPM2 channels mediate acetaminophen-induced
liver damage. Proc Natl Acad Sci USA. 111:3176–3181. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Li WC, Xiong ZY, Huang PZ, Liao YJ, Li QX,
Yao ZC, Liao YD, Xu SL, Zhou H, Wang QL, et al: KCNK levels are
prognostic and diagnostic markers for hepatocellular carcinoma.
Aging (Albany NY). 11:8169–8182. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Innamaa A, Jackson L, Asher V, van
Schalkwyk G, Warren A, Keightley A, Hay D, Bali A, Sowter H and
Khan R: Expression and effects of modulation of the K2P potassium
channels TREK-1 (KCNK2) and TREK-2 (KCNK10) in the normal human
ovary and epithelial ovarian cancer. Clin Transl Oncol. 15:910–918.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
He Y, Hu H, Wang Y, Yuan H, Lu Z, Wu P,
Liu D, Tian L, Yin J, Jiang K and Miao Y: ALKBH5 inhibits
pancreatic cancer motility by decreasing long non-coding RNA
KCNK15-AS1 methylation. Cell Physiol Biochem. 48:838–846. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Alvarez-Baron C, Jonsson P, Thomas C,
Dryer S and Williams C: The two-pore domain potassium channel
KCNK5: Induction by estrogen receptor alpha and role in
proliferation of breast cancer cells. Mol Endocrinol. 25:1326–1336.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Kim CJ, Cho YG, Jeong SW, Kim YS, Kim SY,
Nam SW, Lee SH, Yoo NJ, Lee JY and Park WS: Altered expression of
KCNK9 in colorectal cancers. APMIS. 112:588–594. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Peroz D, Rodriguez N, Choveau F, Baró I,
Mérot J and Loussouarn G: Kv7.1 (KCNQ1) properties and
channelopathies. J Physiol. 586:1785–1789. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
White BD, Chien AJ and Dawson DW:
Dysregulation of Wnt/β-catenin signaling in gastrointestinal
cancers. Gastroenterology. 142:219–232. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Fan H, Zhang M and Liu W: Hypermethylated
KCNQ1 acts as a tumor suppressor in hepatocellular carcinoma.
Biochem Biophys Res Commun. 503:3100–3107. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Li C, Miao R, Zhang J, Qu K and Liu C:
Long non-coding RNA KCNQ1OT1 mediates the growth of hepatocellular
carcinoma by functioning as a competing endogenous RNA of miR-504.
Int J Oncol. 52:1603–1612. 2018.PubMed/NCBI
|
|
62
|
Wan J, Huang M, Zhao H, Wang C, Zhao X,
Jiang X, Bian S, He Y and Gao Y: A novel tetranucleotide repeat
polymorphism within KCNQ1OT1 confers risk for hepatocellular
carcinoma. DNA Cell Biol. 32:628–634. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Zhong W, Dai Q and Huang Q: Effect of
lncRNA KCNQ1OT1 on autophagy and drug resistance of hepatocellular
carcinoma cells by targeting miR-338-3p. Cell Mol Biol
(Noisy-le-grand). 66:191–196. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Jiang M, Cui BW, Wu YL, Zhang Y, Shang Y,
Liu J, Yang HX, Qiao CY, Zhan ZY, Ye H, et al: P2X7R orchestrates
the progression of murine hepatic fibrosis by making a feedback
loop from macrophage to hepatic stellate cells. Toxicol Lett.
333:22–32. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Yang G, Zhou L, Xu Q, Meng F, Wan Y, Meng
X, Wang L and Zhang L: LncRNA KCNQ1OT1 inhibits the
radiosensitivity and promotes the tumorigenesis of hepatocellular
carcinoma via the miR-146a-5p/ACER3 axis. Cell Cycle. 19:2519–2529.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Zhang J, Zhao X, Ma X, Yuan Z and Hu M:
KCNQ1OT1 contributes to sorafenib resistance and programmed
death-ligand-1-mediated immune escape via sponging miR-506 in
hepatocellular carcinoma cells. Int J Mol Med. 46:1794–1804.
2020.PubMed/NCBI
|
|
67
|
Xie Z and Askari A: Na(+)/K(+)-ATPase as a
signal transducer. Eur J Biochem. 269:2434–2439. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Rajasekaran SA, Palmer LG, Quan K, Harper
JF, Ball WJ Jr, Bander NH, Peralta Soler A and Rajasekaran AK:
Na,K-ATPase beta-subunit is required for epithelial polarization,
suppression of invasion, and cell motility. Mol Biol Cell.
12:279–295. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Zhuang L, Xu L, Wang P, Jiang Y, Yong P,
Zhang C, Zhang H, Meng Z and Yang P: Na+/K+-ATPase α1 subunit, a
novel therapeutic target for hepatocellular carcinoma. Oncotarget.
6:28183–28193. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Xu ZW, Wang FM, Gao MJ, Chen XY, Hu WL and
Xu RC: Targeting the Na(+)/K(+)-ATPase alpha1 subunit of hepatoma
HepG2 cell line to induce apoptosis and cell cycle arresting. Biol
Pharm Bull. 33:743–751. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Udoh US, Banerjee M, Rajan PK, Sanabria
JD, Smith G, Schade M, Sanabria JA, Nakafuku Y, Sodhi K, Pierre SV,
et al: Tumor-suppressor role of the α1-Na/K-ATPase signalosome in
NASH related hepatocellular carcinoma. Int J Mol Sci. 23:73592022.
View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Tang S, Yang X, Zhou C, Mei Y, Ye J, Zhang
X, Feng G, Zhang W, Zhang X and Fan W: Sodium pump Na + /K + ATPase
subunit α1-targeted positron emission tomography imaging of
hepatocellular carcinoma in mouse models. Mol Imaging Biol.
24:384–393. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Garty H and Karlish SJD: Role of FXYD
proteins in ion transport. Annu Rev Physiol. 68:431–459. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Gao Q, Chen X, Duan H, Wang Z, Feng J,
Yang D, Song L, Zhou N and Yan X: FXYD6: A novel therapeutic target
toward hepatocellular carcinoma. Protein Cell. 5:532–543. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Feske S, Wulff H and Skolnik EY: Ion
channels in innate and adaptive immunity. Annu Rev Immunol.
33:291–353. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Teisseyre A, Palko-Labuz A, Sroda-Pomianek
K and Michalak K: Voltage-gated potassium channel Kv1.3 as a target
in therapy of cancer. Front Oncol. 9:9332019. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Zúñiga-García V, Chávez-López Mde G,
Quintanar-Jurado V, Gabiño-López NB, Hernández-Gallegos E,
Soriano-Rosas J, Pérez-Carreón JI and Camacho J: Differential
expression of ion channels and transporters during hepatocellular
carcinoma development. Dig Dis Sci. 60:2373–2383. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Prosdocimi E, Checchetto V and Leanza L:
Targeting the mitochondrial potassium channel Kv1.3 to kill cancer
cells: Drugs, strategies, and new perspectives. SLAS Discov.
24:882–892. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Na W, Ma B, Shi S, Chen Y, Zhang H, Zhan Y
and An H: Procyanidin B1, a novel and specific inhibitor of Kv10.1
channel, suppresses the evolution of hepatoma. Biochem Pharmacol.
178:1140892020. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Zhao W, Bai B, Hong Z, Zhang X and Zhou B:
Berbamine (BBM), a natural STAT3 inhibitor, synergistically
enhances the antigrowth and proapoptotic effects of sorafenib on
hepatocellular carcinoma cells. ACS Omega. 5:24838–24847. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Zhou Q, Kwan HY, Chan HC, Jiang JL, Tam SC
and Yao X: Blockage of voltage-gated K+ channels inhibits adhesion
and proliferation of hepatocarcinoma cells. Int J Mol Med.
11:261–266. 2003.PubMed/NCBI
|
|
82
|
Rosa P, Catacuzzeno L, Sforna L, Mangino
G, Carlomagno S, Mincione G, Petrozza V, Ragona G, Franciolini F
and Calogero A: BK channels blockage inhibits hypoxia-induced
migration and chemoresistance to cisplatin in human glioblastoma
cells. J Cell Physiol. 233:6866–6877. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Wang X, Chen Y, Zhang Y, Guo S, Mo L, An H
and Zhan Y: Eag1 voltage-dependent potassium channels: Structure,
electrophysiological characteristics, and function in cancer. J
Membr Biol. 250:123–132. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
García-Quiroz J and Camacho J: Astemizole:
An old anti-histamine as a new promising anti-cancer drug.
Anticancer Agents Med Chem. 11:307–314. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
de Guadalupe Chávez-López M, Pérez-Carreón
JI, Zuñiga-García V, Díaz-Chávez J, Herrera LA, Caro-Sánchez CH,
Acuña-Macías I, Gariglio P, Hernández-Gallegos E, Chiliquinga AJ
and Camacho J: Astemizole-based anticancer therapy for
hepatocellular carcinoma (HCC), and Eag1 channels as potential
early-stage markers of HCC. Tumour Biol. 36:6149–6158. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Roy AM, Baliga MS, Elmets CA and Katiyar
SK: Grape seed proanthocyanidins induce apoptosis through p53, Bax,
and caspase 3 pathways. Neoplasia. 7:24–36. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Mantena SK and Katiyar SK: Grape seed
proanthocyanidins inhibit UV-radiation-induced oxidative stress and
activation of MAPK and NF-kappaB signaling in human epidermal
keratinocytes. Free Radic Biol Med. 40:1603–1614. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Mohr CJ, Steudel FA, Gross D, Ruth P, Lo
WY, Hoppe R, Schroth W, Brauch H, Huber SM and Lukowski R:
Cancer-associated intermediate conductance
Ca2+-Activated K+ Channel KCa3.1. Cancers
(Basel). 11:1092019. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Catacuzzeno L, Fioretti B and Franciolini
F: Expression and role of the intermediate-conductance
calcium-activated potassium channel KCa3.1 in glioblastoma. J
Signal Transduct. 2012:4215642012. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Bulk E, Ay AS, Hammadi M, Ouadid-Ahidouch
H, Schelhaas S, Hascher A, Rohde C, Thoennissen NH, Wiewrodt R,
Schmidt E, et al: Epigenetic dysregulation of KCa 3.1 channels
induces poor prognosis in lung cancer. Int J Cancer. 137:1306–1317.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Toyama K, Wulff H, Chandy KG, Azam P,
Raman G, Saito T, Fujiwara Y, Mattson DL, Das S, Melvin JE, et al:
The intermediate-conductance calcium-activated potassium channel
KCa3.1 contributes to atherogenesis in mice and humans. J Clin
Invest. 118:3025–3037. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Freise C, Ruehl M, Seehofer D, Hoyer J and
Somasundaram R: The inhibitor of Ca(2+)-dependent K+ channels
TRAM-34 blocks growth of hepatocellular carcinoma cells via
downregulation of estrogen receptor alpha mRNA and nuclear
factor-kappaB. Invest New Drugs. 31:452–457. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Liu Y, Zhao L, Ma W, Cao X, Chen H, Feng
D, Liang J, Yin K and Jiang X: The blockage of KCa3.1 channel
inhibited proliferation, migration and promoted apoptosis of human
hepatocellular carcinoma cells. J Cancer. 6:643–651. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Freise C, Heldwein S, Erben U, Hoyer J,
Köhler R, Jöhrens K, Patsenker E, Ruehl M, Seehofer D, Stickel F
and Somasundaram R: K+-channel inhibition reduces portal perfusion
pressure in fibrotic rats and fibrosis associated characteristics
of hepatic stellate cells. Liver Int. 35:1244–1252. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Yang S, Yang S, Zhang H, Hua H, Kong Q,
Wang J and Jiang Y: Targeting Na+/K+-ATPase
by berbamine and ouabain synergizes with sorafenib to inhibit
hepatocellular carcinoma. Br J Pharmacol. 178:4389–4407. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Alevizopoulos K, Calogeropoulou T, Lang F
and Stournaras C: Na+/K+ ATPase inhibitors in cancer. Curr Drug
Targets. 15:988–1000. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Simpson CD, Mawji IA, Anyiwe K, Williams
MA, Wang X, Venugopal AL, Gronda M, Hurren R, Cheng S, Serra S, et
al: Inhibition of the sodium potassium adenosine triphosphatase
pump sensitizes cancer cells to anoikis and prevents distant tumor
formation. Cancer Res. 69:2739–2747. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Durlacher CT, Chow K, Chen XW, He ZX,
Zhang X, Yang T and Zhou SF: Targeting Na+/K+-translocating
adenosine triphosphatase in cancer treatment. Clin Exp Pharmacol
Physiol. 42:427–443. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Jiang W, Li G, Li W, Wang P, Xiu P, Jiang
X, Liu B, Sun X and Jiang H: Sodium orthovanadate overcomes
sorafenib resistance of hepatocellular carcinoma cells by
inhibiting Na+/K+-ATPase activity and
hypoxia-inducible pathways. Sci Rep. 8:97062018. View Article : Google Scholar : PubMed/NCBI
|