|
1
|
Hochwald O, Jabr M, Osiovich H, Miller SP,
McNamara PJ and Lavoie PM: Preferential cephalic redistribution of
left ventricular cardiac output during therapeutic hypothermia for
perinatal hypoxic-ischemic encephalopathy. J Pediatr.
164:999–1004.e1. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Looney AM, Ahearne C, Boylan GB and Murray
DM: Glial Fibrillary acidic protein is not an early marker of
injury in perinatal asphyxia and Hypoxic-ischemic encephalopathy.
Front Neurol. 6:2642015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Khan RH, Islam MS, Haque SA, Hossain MA,
Islam MN, Khaleque MA, Chowdhury B and Chowdhury MA: Correlation
between grades of intraventricular hemorrhage and severity of
hypoxic ischemic encephalopathy in perinatal asphyxia. Mymensingh
Med J. 23:7–12. 2014.PubMed/NCBI
|
|
4
|
Tagin M, Abdel-Hady H, Rahman Ur S,
Azzopardi DV and Gunn AJ: Neuroprotection for perinatal hypoxic
ischemic encephalopathy in low-and Middle-income countries. J
Pediatr. 167:25–28. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Li H, Han W, Wang H, Ding F, Xiao L, Shi
R, Ai L and Huang Z: Tanshinone IIA inhibits Glutamate-induced
oxidative toxicity through prevention of mitochondrial dysfunction
and suppression of MAPK activation in SH-SY5Y human neuroblastoma
cells. Oxid Med Cell Longev. 2017:45174862017. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kim EO, Kang SE, Im CR, Lee JH, Ahn KS,
Yang WM, Um JY, Lee SG and Yun M: Tanshinone IIA induces TRAIL
sensitization of human lung cancer cells through selective ER
stress induction. Int J Oncol. 48:2205–2212. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mao C, Zhang Y, Zhang Y, Cao L, Shao H,
Wang L, Zhu L and Xu Z: The effect of tanshinone IIA on the
cardiovascular system in ovine fetus in utero. Am J Chin Med.
37:1031–1044. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Gao S, Liu Z, Li H, Little PJ, Liu P and
Xu S: Cardiovascular actions and therapeutic potential of
tanshinone IIA. Atherosclerosis. 220:3–10. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Shen JL, Chen YS, Lin JY, Tien YC, Peng
WH, Kuo CH, Tzang BS, Wang HL, Tsai FJ, Chou MC, et al: Neuron
regeneration and proliferation effects of Danshen and Tanshinone
IIA. Evid Based Complement Alternat Med. 2011:3789072011.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
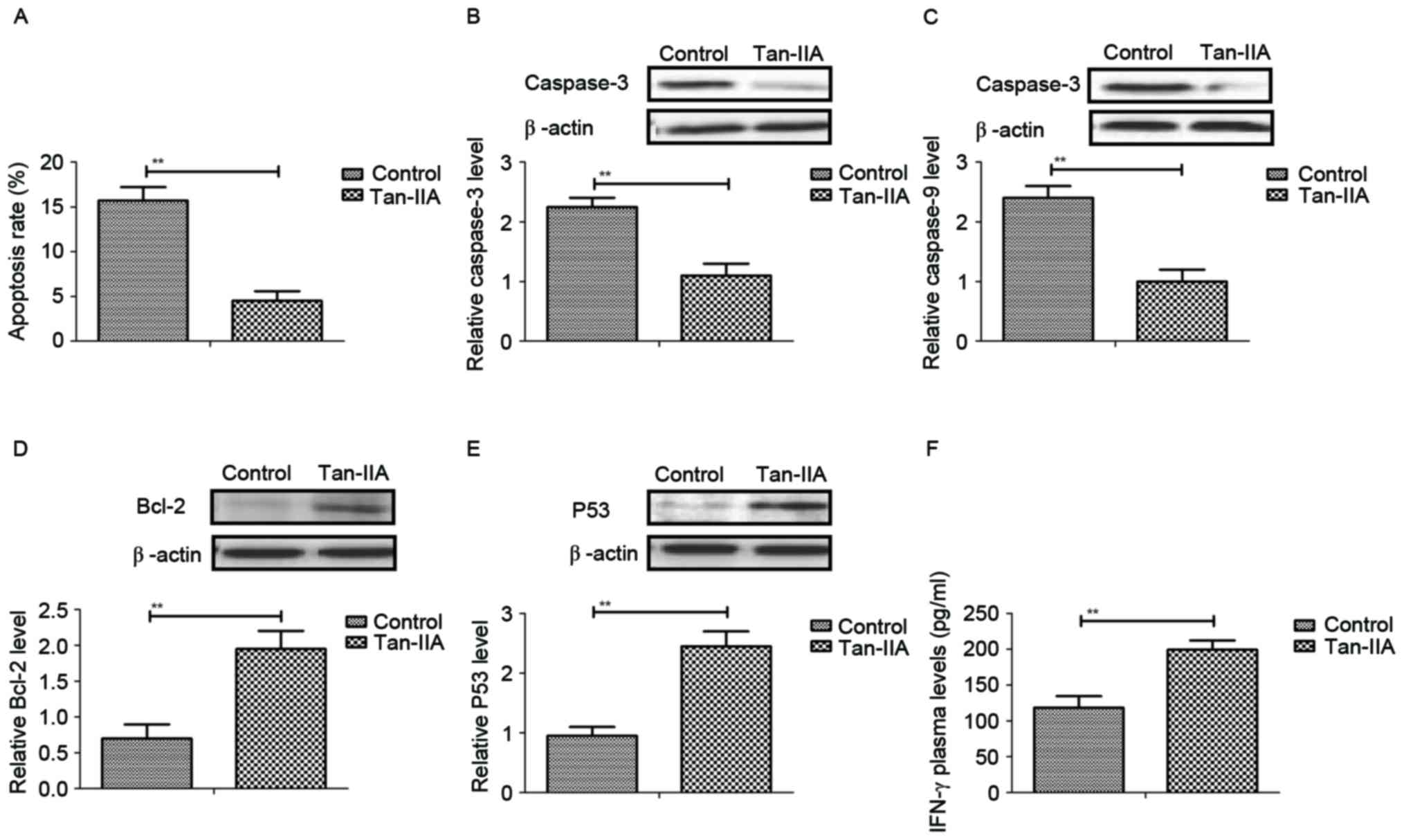
Hernandez-Jimenez M, Sacristan S, Morales
C, García-Villanueva M, García-Fernández E, Alcázar A, González VM
and Martín ME: Apoptosis-related proteins are potential markers of
neonatal hypoxic-ischemic encephalopathy (HIE) injury. Neurosci
Lett. 558:143–148. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Li SJ, Liu W, Wang JL, Zhang Y, Zhao DJ,
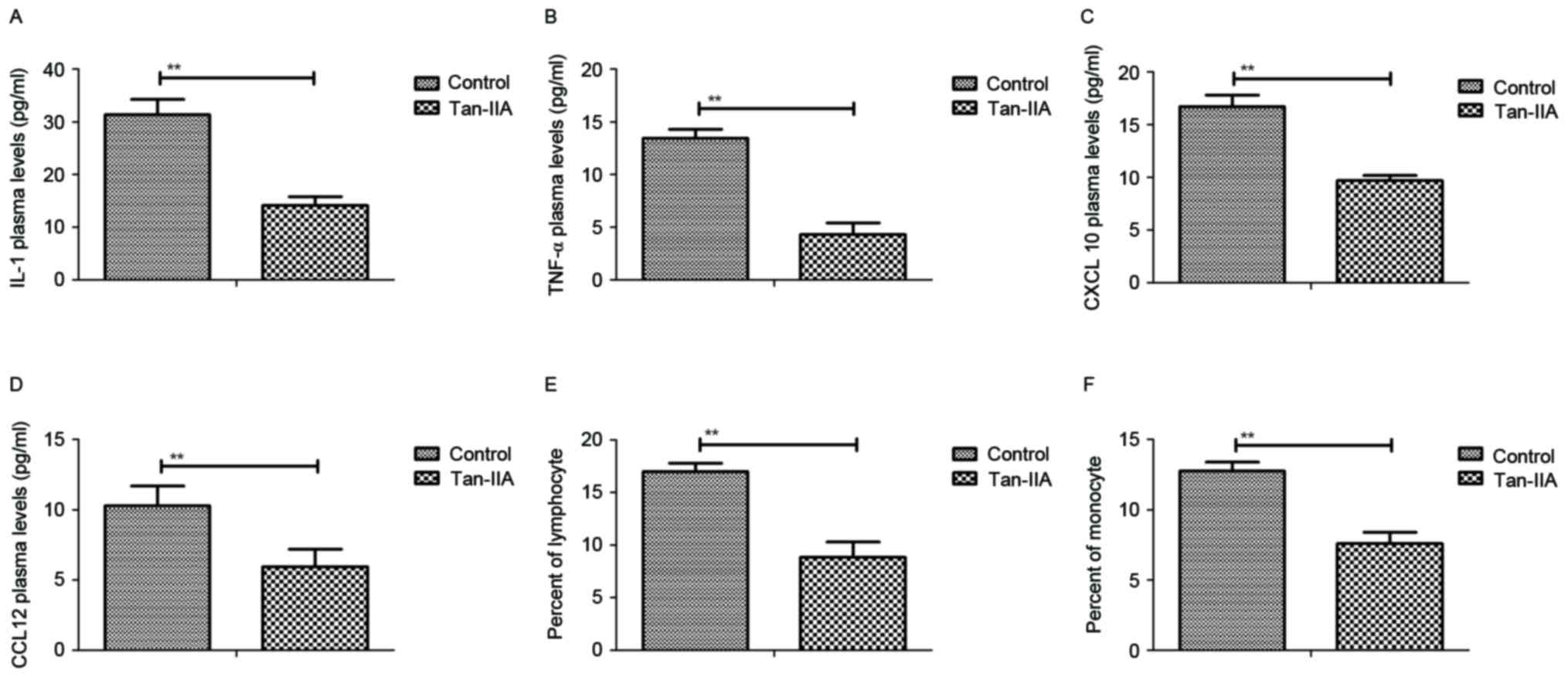
Wang TJ and Li YY: The role of TNF-α, IL-6, IL-10, and GDNF in
neuronal apoptosis in neonatal rat with hypoxic-ischemic
encephalopathy. Eur Rev Med Pharmacol Sci. 18:905–909.
2014.PubMed/NCBI
|
|
12
|
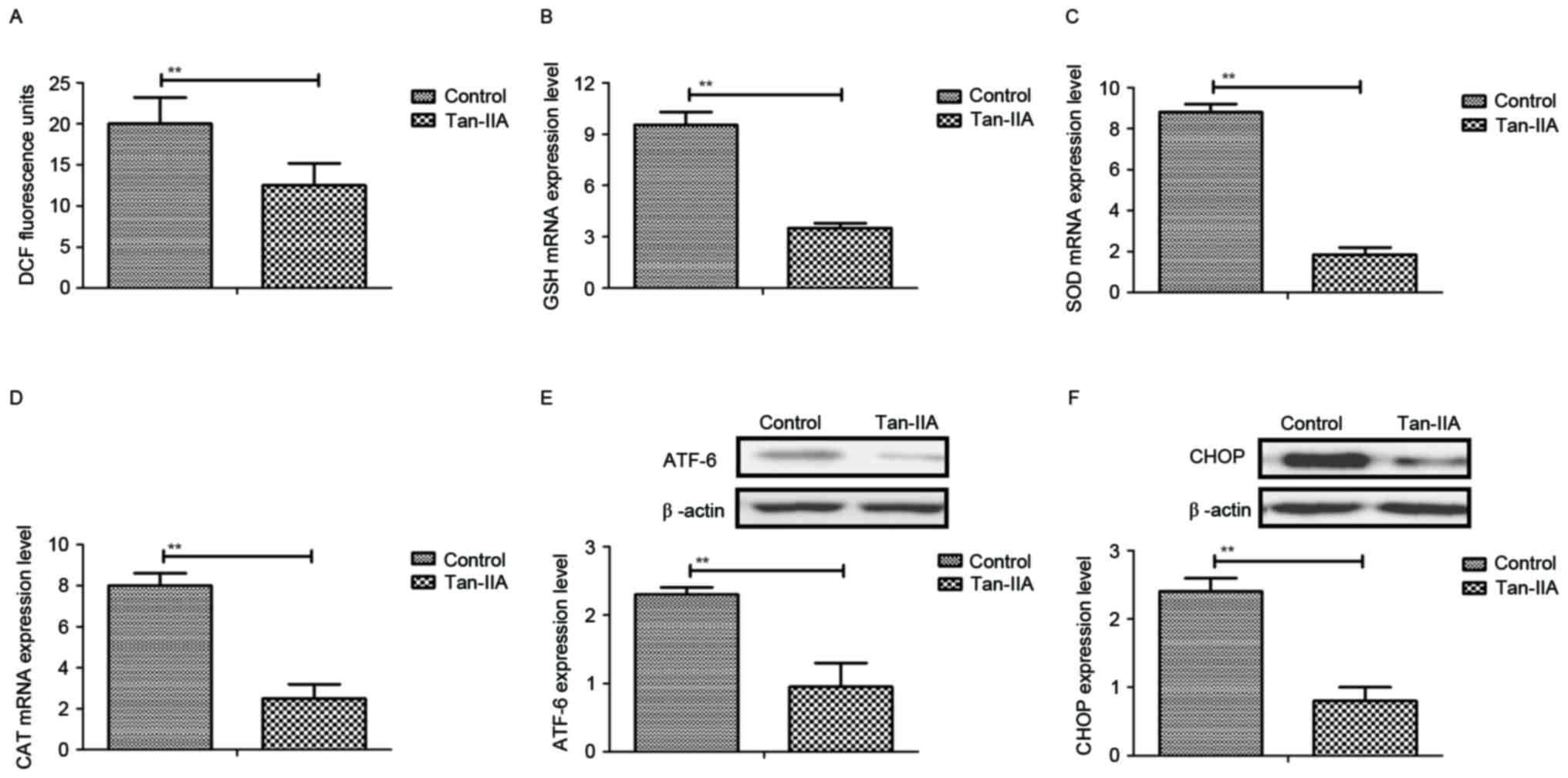
Liu L, Liu C, Lu Y and Jiang Y: ER stress
related factor ATF6 and caspase-12 trigger apoptosis in neonatal
hypoxic-ischemic encephalopathy. Int J Clin Exp Pathol.
8:6960–6966. 2015.PubMed/NCBI
|
|
13
|
Johnson CT, Burd I, Raghunathan R,
Northington FJ and Graham EM: Perinatal inflammation/infection and
its association with correction of metabolic acidosis in
hypoxic-ischemic encephalopathy. J Perinatol. 36:448–452. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Chapados I and Cheung PY: Not all models
are created equal: Animal models to study hypoxic-ischemic
encephalopathy of the newborn. Commentary on Gelfand SL et
al: A new model of oxidative stress in rat pups (Neonatology
2008;94:293-299). Neonatology. 94:300–303. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Cikla U, Chanana V, Kintner DB, Udho E,
Eickhoff J, Sun W, Marquez S, Covert L, Otles A, Shapiro RA, et al:
ERα signaling is required for TrkB-mediated hippocampal
neuroprotection in female neonatal mice after hypoxic ischemic
encephalopathy(1,2,3). eNeuro. 3:pii2016. View Article : Google Scholar
|
|
16
|
Can MM, Tanboğa IH, Türkyilmaz E, Karabay
CY, Akgun T, Koca F, Tokgoz HC, Keles N, Ozkan A, Bezgin T, et al:
The risk of false results in the assessment of platelet function in
the absence of antiplatelet medication: Comparison of the PFA-100,
multiplate electrical impedance aggregometry and verify now assays.
Thromb Res. 125:e132–e137. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Livak KJ and Schmittgen TD: Analysis of
relative gene expression data using real-time. quantitative PCR and
the 2(-Delta Delta C(T)) method. Methods. 25:402–408. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hashiguchi A, Yano S, Nitta K, Ide W,
Hashimoto I, Kamada H and Kuratsu J: Hemisplenial-accompanied by
internal border-zone infarction: Clinical relevance of the splenium
of the corpus callosum as a border-zone area between anterior and
posterior cerebral arteries. J Neurol Neurosurg Psychiatry.
81:704–706. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Bechet S, Hill F, Gilheaney Ó and Walshe
M: Diagnostic accuracy of the modified Evan's blue dye test in
detecting aspiration in patients with tracheostomy: A systematic
review of the evidence. Dysphagia. 31:721–729. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Farahat FM, Rohlman DS, Storzbach D,
Ammerman T and Anger WK: Measures of short-term test-retest
reliability of computerized neurobehavioral tests. Neurotoxicology.
24:513–521. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Sant'Anna G, Laptook AR, Shankaran S, Bara
R, McDonald SA, Higgins RD, Tyson JE, Ehrenkranz RA, Das A,
Goldberg RN, et al: Phenobarbital and temperature profile during
hypothermia for hypoxic-ischemic encephalopathy. J Child Neurol.
27:451–457. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Shankaran S: Hypoxic-ischemic
encephalopathy and novel strategies for neuroprotection. Clin
Perinatol. 39:919–929. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Peliowski-Davidovich A: Hypothermia for
newborns with hypoxic ischemic encephalopathy. Paediat Child
Health. 17:41–43. 2012. View Article : Google Scholar
|
|
24
|
Barks JD, Liu YQ, Shangguan Y, Li J, Pfau
J and Silverstein FS: Impact of indolent inflammation on neonatal
hypoxic-ischemic brain injury in mice. Int J Dev Neurosci.
26:57–65. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Girard S, Sebire H, Brochu ME, Briota S,
Sarret P and Sébire G: Postnatal administration of IL-1Ra exerts
neuroprotective effects following perinatal inflammation and/or
hypoxic-ischemic injuries. Brain Behav Immun. 26:1331–1339. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Aly H, Khashaba MT, El-Ayouty M, El-Sayed
O and Hasanein BM: IL-1beta, IL-6 and TNF-alpha and outcomes of
neonatal hypoxic ischemic encephalopathy. Brain Dev. 28:178–182.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Gotsch F, Romero R, Friel L, Kusanovic JP,
Espinoza J, Erez O, Than NG, Mittal P, Edwin S, Yoon BH, et al:
CXCL10/IP-10: A missing link between inflammation and
anti-angiogenesis in preeclampsia? J Matern Fetal Neonatal Med.
20:777–792. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Tomita K, Freeman BL, Bronk SF, LeBrasseur
NK, White TA, Hirsova P and Ibrahim SH: CXCL10-mediates macrophage,
but not other innate immune cells-associated inflammation in murine
nonalcoholic steatohepatitis. Sci Rep. 6:287862016. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Kurian GA, Rajagopal R, Vedantham S and
Rajesh M: The role of oxidative stress in myocardial ischemia and
reperfusion injury and remodeling: Revisited. Oxid Med Cell Longev.
2016:16564502016. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Perrone S, Szabo M, Bellieni CV, Longini
M, Bangó M, Kelen D, Treszl A, Negro S, Tataranno ML and Buonocore
G: Whole body hypothermia and oxidative stress in babies with
hypoxic-ischemic brain injury. Pediatr Neurol. 43:236–240. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ten VS, Yao J, Ratner V, Sosunov S, Fraser
DA, Botto M, Sivasankar B, Morgan BP, Silverstein S, Stark R, et
al: Complement component c1q mediates mitochondria-driven oxidative
stress in neonatal hypoxic-ischemic brain injury. J Neurosci.
30:2077–2087. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Demarest TG, Schuh RA, Waddell J, McKenna
MC and Fiskum G: Sex-dependent mitochondrial respiratory impairment
and oxidative stress in a rat model of neonatal hypoxic-ischemic
encephalopathy. J Neurochem. 137:714–729. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Wang Y, Tu L, Li Y, Chen D and Wang S:
Notoginsenoside R1 protects against neonatal cerebral
Hypoxic-ischemic injury through estrogen Receptor-dependent
activation of endoplasmic reticulum stress pathways. J Pharmacol
Exp Ther. 357:591–605. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Kong D, Zhu J, Liu Q, Jiang Y, Xu L, Luo
N, Zhao Z, Zhai Q, Zhang H, Zhu M and Liu X: Mesenchymal stem cells
protect neurons against hypoxic-ischemic injury via inhibiting
parthanatos, necroptosis, and apoptosis, but not autophagy. Cell
Mol Neurobiol. 37:303–313. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Yan SZ, Wang XL, Wang HY, Dong P and Zhao
YS: Effects of umbilical cord blood mononuclear cells
transplantation via lateral ventricle on the neural apoptosis and
the expression of Bax and Bcl-2 proteins in neonatal rats with
hypoxic-ischemic brain damage. Zhongguo Dang Dai Er Ke Za Zhi.
18:862–866. 2016.(In Chinese). PubMed/NCBI
|
|
36
|
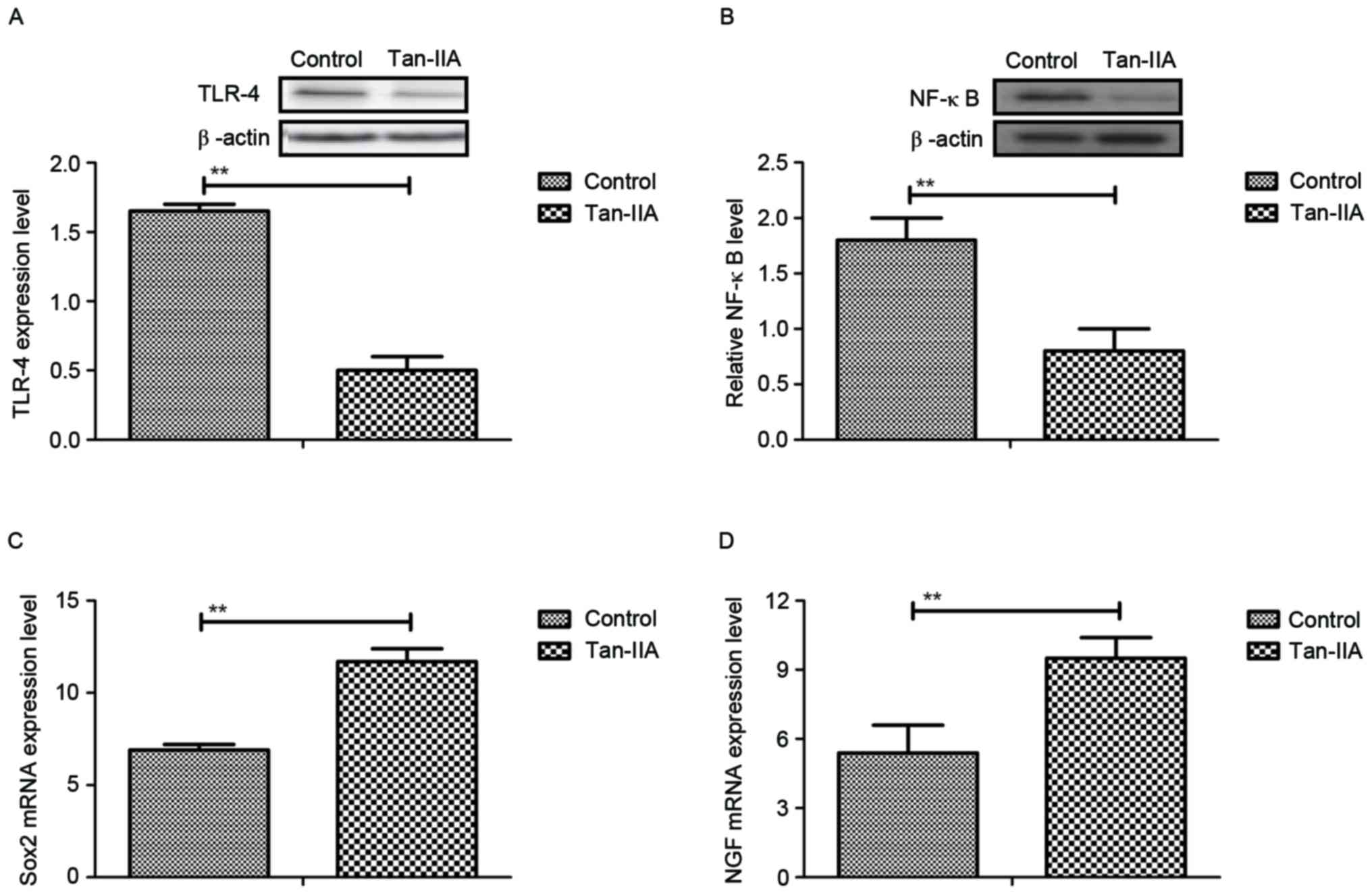
Liang ZQ, Li YL, Zhao XL, Han R, Wang XX,
Wang Y, Chase TN, Bennett MC and Qin ZH: NF-kappaB contributes to
6-hydroxydopamine-induced apoptosis of nigral dopaminergic neurons
through p53. Brain Res. 1145:190–203. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Kairisalo M, Korhonen L, Sepp M, Pruunsild
P, Kukkonen JP, Kivinen J, Timmusk T, Blomgren K and Lindholm D:
NF-kappaB-dependent regulation of brain-derived neurotrophic factor
in hippocampal neurons by X-linked inhibitor of apoptosis protein.
Eur J Neurosci. 30:958–966. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Ulbrich F, Lerach T, Biermann J, Kaufmann
KB, Lagreze WA, Buerkle H, Loop T and Goebel U: Argon mediates
protection by interleukin-8 suppression via a TLR2/TLR4/STAT3/NF-κB
pathway in a model of apoptosis in neuroblastoma cells in vitro and
following ischemia-reperfusion injury in rat retina in vivo. J
Neurochem. 138:859–873. 2016. View Article : Google Scholar : PubMed/NCBI
|