Introduction
Acne occurs in all areas of the body with high
concentrations of pilosebaceous glands, but occurs on the face,
back and chest in particular. Inflammatory acne lesions may result
in permanent scars, the severity of which may depend on delays in
treating acne patients. The prevalence and severity of acne
scarring in the population has not been well studied, although the
available literature usually shows that it is correlated with the
severity of acne (1). A study of
2,133 volunteers aged 18–70 from the general population showed that
almost 1% of people had acne scars, although only 1 in 7 of these
individuals were considered to have ‘disfiguring scars’ (1). Severe scarring caused by acne is
associated with substantial physical and psychological distress,
particularly in adolescents. There are many treatments for acne or
acne scars, particularly fractional laser therapy. Fractional laser
therapy has been shown to be an effective treatment method for acne
or acne scars; however, it is associated with a long period of
erythema and edema (5–10 days), which may hinder patients’ daily
lives.
Autologous platelet-rich plasma (PRP) is the plasma
portion of autologously sourced blood with an iatrogenically high
platelet concentration, which is extensively used to promote soft
and hard tissue healing and to significantly reduce wound-healing
time (2–4). At sites of tissue damage, platelets
are the first cells to arrive and play an important role in
mediating tissue repair through the release of growth factors
(GFs), such as PDGF, TGF-β, EGF, VEGF, IGF and FGF, from their
α-granules (5,6). These factors are known to regulate
cell migration, attachment, proliferation and differentiation, and
to promote extracellular matrix accumulation via binding to
specific cell surface receptors (7). Adding autologous thrombin and calcium
ions triggers the activation process. Once platelets are activated,
secretion of GFs begins within 10 min and 95% of all factors are
secreted within 1 h (8).
Furthermore, PRP is easily obtained from autogenous whole blood by
two centrifuging steps. At present, PRP is extensively used for
bone cartilage tissue regeneration, soft tissue healing wound
healing, and cosmetic and maxillo-facial surgery, and the effects
in the clinic are positive (2,9,10).
The 2,940-nm erbium fractional laser has
photothermal and mechanical effects (11). It removes the abnormal tissue and
rough epidermal through tissue vaporization. It induces collagen
regeneration and remodeling in the dermal layer while epidermal
stem cells located in the hair follicle and surrounding residual
skin island proliferate, until the wound is healed (12). The objective of our study was to
evaluate whether the combination of autologous PRP and 2,940-nm
erbium fractional laser therapy increases the treatment effect for
facial acne or acne scars and reduces the adverse effects.
Materials and methods
Participants
In total, 22 participants with moderate to severe
facial acne or acne scars (including 16 patients who suffered from
facial acne scars and 6 patients who suffered from acne scars with
concomitant acne) were enrolled in this study. The mean participant
age was 28 (range, 19–39 years), and the sample included 17 females
and 5 males. The study reported on the skin type of the subjects
using the Fitzpatrick skin type classification and subjects had
either skin type III or IV. Participants were excluded if they
reported a history of keloid scar formation, any active
inflammation, oral isotretinoin use within the preceding 6 months,
diabetes, collagen vascular disease, or ablative or nonablative
laser skin resurfacing within the preceding 12 months, or if they
were pregnant or lactating.
This study was conducted in accordance with the
Declaration of Helsinki and with approval from the Ethics Committee
of Guangzhou General Hospital of Guangzhou Military Command.
Written informed consent was obtained from all participants.
PRP preparation
PRP were obtained using a two-stage centrifuging
process. Whole blood samples (10 ml) were drawn from the
participant’s medial cubital vein and collected in a sterile tube
containing 1 ml anticoagulant. Four tubes were collected per
participant. After measuring the blood platelet concentration, the
tubes were centrifuged at 1500 revolutions per minute (rpm) for 10
min in a centrifugal apparatus. The first spin separated
platelet-poor plasma (PPP) from red blood cells (RBCs) and PRP. The
PPP, PRP and a few RBCs were aspirated into a new tube, mixed,
platelet concentration was detected again, and in the second spin,
the tubes were centrifuged at 3000 rpm for 20 min. The upper
section consisted of PPP and the PRP collected at the bottom of the
tube. Then, 6–10 ml PPP and PRP were aspirated, mixed and platelet
concentration was detected again to guarantee that the platelet
concentration in the PRP ranged from 700,000,000–1,000,000,000
platelets per ml. Prior to treatment calcium gluconate was added at
a ratio of 1:9 (calcium gluconate/plasma) to activate
platelets.
Treatment
Prior to treatment, all treatment areas were gently
cleansed using a mild cleanser, and a topical anesthetic cream was
applied for 30 min. The entire face of each participant was then
treated with an erbium fractional laser. Treatment parameters:
wavelength, 2,940 nm; pulse duration, 300–600 μsec; pulse energy,
600–1200 mJ (selected according to acne scar level); microbeam
diameter, 2–7 mm; and penetration depth, 18–24 μm. Concurrent
forced-air cooling was used for the whole process. The end-point of
the laser treatment was moderate erythema or punctiform errhysis
(for severe acne scars). Following the treatment of the
participants with autologous PRP, PRP mixed with calcium gluconate
was coated onto each therapeutic area (thickness ~0.5 mm).
Participants were then instructed to compress their faces with
gauze for 15–20 min while remaining supine before being allowed to
go home, and were instructed to avoid sun exposure. One or two
months after the initial treatment, all participants underwent one
additional treatment session with the same treatment.
Measurements
Photographic documentation was performed using
identical camera settings and lighting and the same positioning
with the same camera. After the first treatment session,
participants were evaluated for adverse events at 7 days, 1, 2 and
3 months. Erythema and edema were graded on a 5-point scale (0,
none; 1, trace; 2, mild; 3, moderate; 4, severe). Two
dermatologists who were blinded to subject treatment group
evaluated the serial photographs in a randomized fashion (before
and after treatment, without labeling) to determine whether
discernible clinical improvement had occurred. Evaluators used a
quartile grading scale of 0 (no change, 0%), 1 (mild improvement,
0–25%), 2 (moderate improvement, 25–50%), 3 (marked improvement,
50–75%), and 4 (excellent improvement, 75–100%). In addition, each
participant was asked to rate his/her overall satisfaction with the
treatment 4 weeks after it was completed using a quartile grading
system (0 unsatisfied, 1 slightly satisfied, 2 satisfied or 3 very
satisfied). Patients were also asked to report on any side-effects
of the treatment, including bleeding, oozing, post-treatment
dyschromia, crust and duration of erythema.
Results
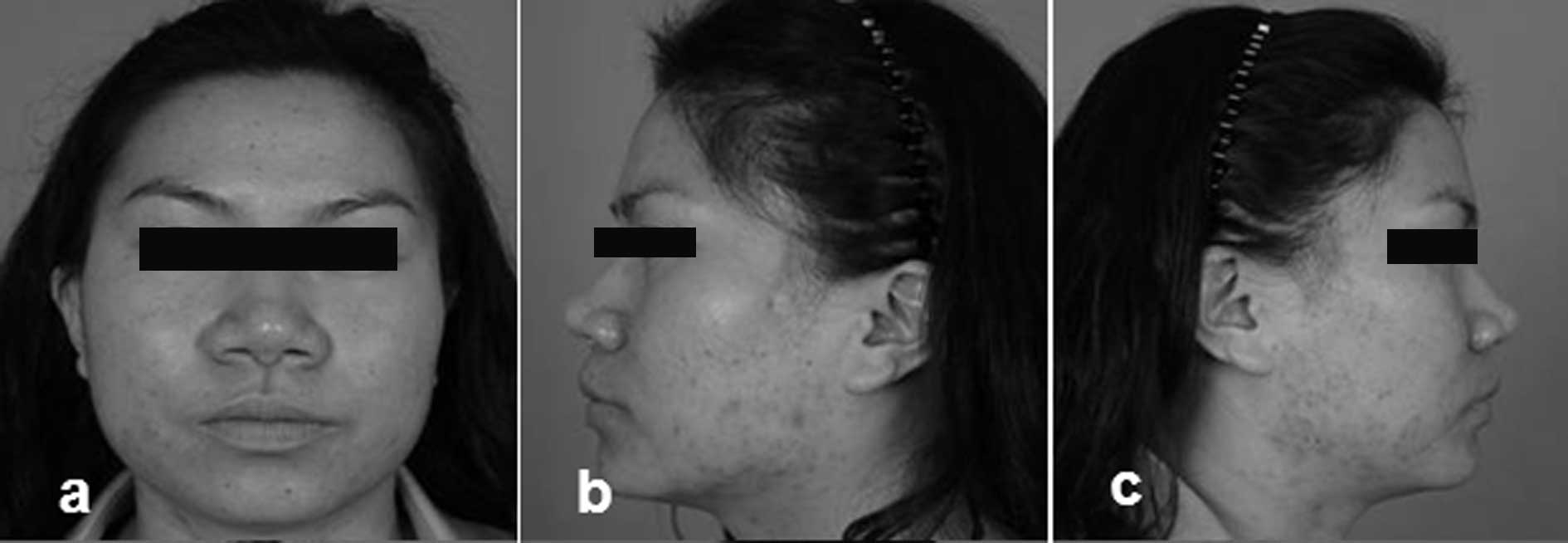
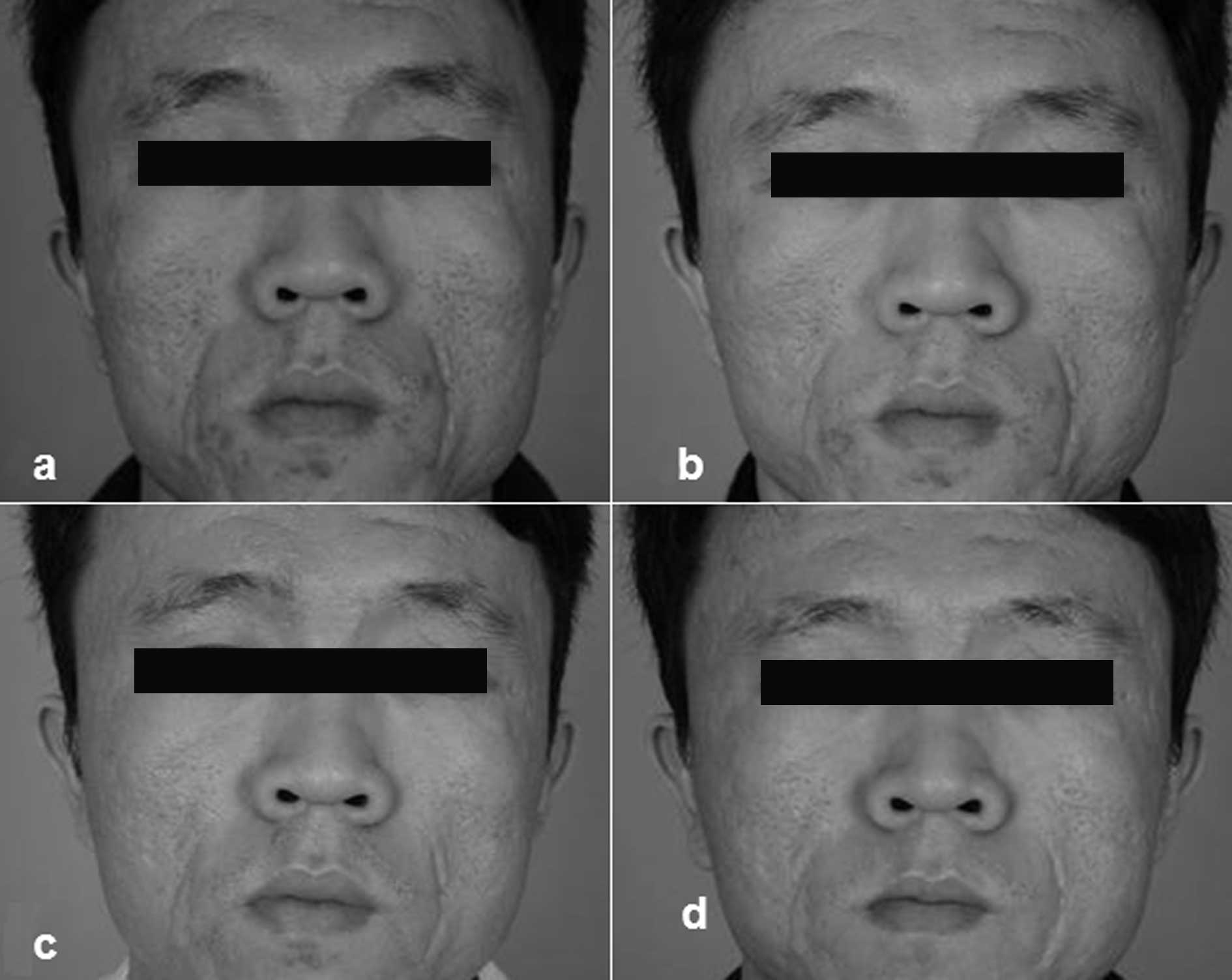
All 22 participants completed the study, and were
followed up for 1–3 months. The serial photographs were evaluated
prior to and following treatment (Figs. 1–4).
Erythema evaluation
All participants recorded the duration of erythema.
The mean duration of erythema was 1.86±0.87 days. In total, 95% of
the erythema was moderate, only 1 patient who accepted laser
grinding at a high pulse energy manifested severe erythema and 77%
of the erythema lasted <2 days.
Evaluation by dermatologists
On the quartile grading scale, the clinical
improvement at 4 weeks after the first treatment was 2.77±0.39,
corresponding to moderate improvement. A total of 68% of
participants demonstrated excellent or marked improvement after the
first treatment, while 90.9% demonstrated excellent or marked
improvement after the third time. No patient was reported to show
no improvement.
Self-evaluation
All participants showed satisfactory changes.
According to the quartile grading scale, the self-evaluation was
3.3±0.36, and 91% of patients described themselves as ‘satisfied’
or ‘very satisfied’ with their overall improvement, and 45% wanted
to receive further treatment.
Side-effects
Overall, the treatment was well tolerated. The
patients felt apparent burning pain during the whole procedure and
some experienced punctiform errhysis. Notably, after PRP was coated
onto the face, the burning pain disappeared instead of tautness.
Subsequently, at days 4 or 5 the epidermis of some patients
desquamated, some formed a scab and the scab desquamated in 1 week.
There were no participants with pigmentation.
Discussion
Acne has a prevalence of >90% among adolescents
and persists into adulthood in ~12–14% of cases with psychological
and social implications of high gravity (13). Types of acne scars include keloid,
hypertrophic and atrophic scars (14). Atrophic acne scarring is by far the
most common form, particularly on the face. A descriptive,
universally acceptable classification system of atrophic acne scars
includes three scar types: icepick, boxcar and rolling (15). Atrophic facial acne scarring is a
widely prevalent condition that may negatively impact on a
patient’s quality of life (16).
Acne scarring is common but difficult to treat. Treatments for acne
scars include drugs, chemical peels, dermabrasion/microdermabrasion
punch techniques, dermal grafting, needling, silicone gel combined
therapy, intralesional steroid therapy, cryotherapy and pulsed dye
laser surgery surgical ablation dermabrasion (16–19).
Erbium fractional laser therapy is an effective treatment for
facial acne scars. The 2,940-nm erbium fractional laser has the
shortest duration of erythema, compared with other fractional
lasers, which usually last for 3 days (17), and always resolves within 2 weeks.
Moreover, there is a high probability of hyperpigmentation which
usually lasts for ~1 month, and in rare cases up to 6 months; scar
improvement is in the range of 26–83%; and the procedure may be
relatively uncomfortable. Fractional laser skin resurfacing may
cause adverse reactions such as erythema, acne, milia, infection,
scarring and pigmentation (20).
The complications of incomplete scar removal, poor intraoperative
visualization, scar worsening, tissue fibrosis and permanent
pigmentary alteration have limited the clinical utility of the
treatment.
Autologous PRP is the plasma portion of autologously
sourced blood with an iatrogenically high platelet concentration.
At sites of tissue damage, platelets are the first cells to arrive
and are important in mediating tissue repair through the release of
growth factors from their α-granules. Platelet-derived factors may
influence cellular growth, morphogenesis and differentiation and
may be used therapeutically to accelerate the natural healing
process (21). Studies have
consistently shown that PRP concentrates are an abundant source of
GFs; moreover, the proportion of these GFs approaches the human
physiological ratio, therefore PRP concentrates are more effective
than any single GF. PRP has wound-healing properties, affecting
keratinocytes, endothelial cells, erythrocytes, fibroblasts and
collagen. Hence, PRP may improve the quality of
re-epithelialization and healing. Another study observed a greater
proliferation of stem cells when the skin was treated with PRP
activated with calcium and thrombin than with nonactivated PRP. To
date, PRP has been confirmed to be useful for cosmetic and plastic
surgery (22,23).
Kim et al used intradermal radiofrequency
combined with autologous PRP in the treatment of striae distensae;
it was administered to the participants once every 4 weeks. The
application of PRP not only accelerated recovery and reduced
adverse events such as erythema or edema, but also enhanced
localized collagen neogenesis and redistribution. All the
participants showed satisfactory changes (24). Lee et al conducted a
split-face trial that treated acne scars with PRP following
ablative CO2 fractional resurfacing. Fourteen Korean
participants with acne scars were included in this study. They
received one session of ablative CO2 fractional
resurfacing, and then facial halves were randomly assigned to
receive treatment with autologous PRP injections on one side
(experimental side) and normal saline injections on the other side
(control side). Erythema edema on the experimental side improved
faster than on the control side, and overall degree of clinical
improvement was significantly better on the experimental side than
on the control side (25).
All participants showed satisfactory changes in our
study. According to the quartile grading scale, the self-evaluation
was 3.3±0.36 and 91% of patients described themselves as
‘satisfied’ or ‘very satisfied’ with their overall improvement, and
45% of participants wanted to receive the next treatment. On the
quartile grading scale, the clinical improvement at 4 weeks after
the first treatment was 2.77±0.39, corresponding to moderate
improvement. A total of 68% of participants demonstrated excellent
or marked improvement after the first treatment, while 90.9%
demonstrated excellent or marked improvement after the third
treatment. No patient was reported to show no improvement. The
total duration of erythema lasted 1.86±0.87 days on average. A
total of 95% of the erythema was moderate, only one patient who
accepted laser grinding at a high pulse energy manifested with
severe erythema and 77% of the erythema lasted <2 days. All
participants showed satisfactory changes, and no participants had
pigmentation. Certain studies have demonstrated that PRP may also
contain a small number of leukocytes that synthesize interleukins
as part of a non-specific immune response (26). A previous study of PRP has
demonstrated antimicrobial activity against Escherichia
coli, Staphylococcus aureus, including
methicillin-resistant Staphylococcus aureus, Candida
albicans and Cryptococcus neoformans. In this study all
the infected acne was cured, and in addition, after ablative erbium
fractional resurfacing, no wounds were infected (27).
A combination of erbium fractional laser therapy and
autologous PRP may have synergistic benefits on effectiveness and
cause fewer adverse events. In our study, we did not compare the
effects of erbium fractional laser therapy or autologous PRP alone
with those of the erbium fractional laser and autologous PRP
combination in the treatment of mild and moderate inflammatory acne
and acne scars. PRP may be effective for controlling inflammation
and promoting healing by inhibiting P. acnes and
accelerating re-epithelialization and collagen remodeling. Further
controlled studies are required to address such comparisons.
Additionally, the optimization of treatment protocols and
confirmation of the efficacy of treatment should be established by
clinical trials involving larger numbers of patients.
Acknowledgements
This study was supported by the National Basic
Science and Development Program of China (973 Program,
2012CB518105), the Major National Science and Technology Programs
(2011ZXJ09104-07C), the National Nature and Science Foundation of
China (no. 81171812), the Guangdong Provincial Science and
Technology Projects (nos. 2009B080701092 and 2011B061300073), and
the Guangzhou City Science and Technology Project (10C36091671 and
2012J4100044).
References
|
1
|
Fabbrocini G, Annunziata MC, D’Arco V, et
al: Acne scars: pathogenesis, classification and treatment.
Dermatol Res Pract. 893080:2010.PubMed/NCBI
|
|
2
|
Alsousou J, Ali A, Willett K and Harrison
P: The role of platelet-rich plasma in tissue regeneration.
Platelets. May 30–2012.(Epub ahead of print).
|
|
3
|
Lacci KM and Dardik A: Platelet-rich
plasma: support for its use in wound healing. Yale J Biol Med.
83:1–9. 2010.PubMed/NCBI
|
|
4
|
Arora NS, Ramanayake T, Ren YF and Romanos
GE: Platelet-rich plasma: a literature review. Implant Dent.
18:303–310. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Boswell SG, Cole BJ, Sundman EA, Karas V
and Fortier LA: Platelet-rich plasma: a milieu of bioactive
factors. Arthroscopy. 28:429–439. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Dhillon RS, Schwarz EM and Maloney MD:
Platelet-rich plasma therapy - future or trend? Arthritis Res Ther.
14:2192012. View
Article : Google Scholar : PubMed/NCBI
|
|
7
|
Tran KT, Griffith L and Wells A:
Extracellular matrix signaling through growth factor receptors
during wound healing. Wound Repair Regen. 12:262–268. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Crovetti G, Martinelli G, Issi M, et al:
Platelet gel for healing cutaneous chronic wounds. Transfus Apher
Sci. 30:145–151. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Cervelli V, Nicoli F, Spallone D, et al:
Treatment of traumatic scars using fat grafts mixed with
platelet-rich plasma, and resurfacing of skin with the 1540 nm
nonablative laser. Clin Exp Dermatol. 37:55–61. 2012.PubMed/NCBI
|
|
10
|
Sammartino G, Celentano L, Tia M, et al:
The usefulness of 111indium-oxine autologous platelet
gel graft imaging to evaluate osteoinduction in patients undergoing
surgery of jaw bone defects. Int J Immunopathol Pharmacol.
21:393–399. 2008.
|
|
11
|
Hosokawa Y, Kaji T, Shukunami C, et al:
Nondestructive micro-patterning of proteinous occlusion bodies in
water by femtosecond laser-induced mechanical force. Biomed
Microdevices. 9:105–111. 2007. View Article : Google Scholar
|
|
12
|
Reddy KK, Brauer JA and Geronemus RG:
Evidence for fractional laser treatment in the improvement of
cutaneous scars. J Am Acad Dermatol. 66:1005–1006. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Stathakis V, Kilkenny M and Marks R:
Descriptive epidemiology of acne vulgaris in the community.
Australas J Dermatol. 38:115–123. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Goodman G: Post acne scarring: a review. J
Cosmet Laser Ther. 5:77–95. 2003. View Article : Google Scholar
|
|
15
|
Jansen T and Podda M: Therapy of acne
scars. J Dtsch Dermatol Ges. 8(Suppl 1): S81–S88. 2010.(In
German).
|
|
16
|
O’Daniel TG: Multimodal management of
atrophic acne scarring in the aging face. Aesthetic Plast Surg.
35:1143–1150. 2011.PubMed/NCBI
|
|
17
|
Haider A and Shaw JC: Treatment of acne
vulgaris. JAMA. 292:726–735. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kwok T and Rao J: Laser management of acne
scarring. Skin Therapy Lett. 17:4–6. 2012.
|
|
19
|
Ong MW and Bashir SJ: Fractional laser
resurfacing for acne scars: a review. Br J Dermatol. 166:1160–1169.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Basta-Juzbašić A: Current therapeutic
approach to acne scars. Acta Dermatovenerol Croat. 18:171–175.
2010.PubMed/NCBI
|
|
21
|
Gao F, Wang JX and Han Y: Research advance
on application of platelet-rich plasma in wound repair – review.
Zhongguo Shi Yan Xue Ye Xue Za Zhi. 17:840–843. 2009.(In
Chinese).
|
|
22
|
Redler LH, Thompson SA, Hsu SH, Ahmad CS
and Levine WN: Platelet-rich plasma therapy: a systematic
literature review and evidence for clinical use. Phys Sportsmed.
39:42–51. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Cervelli V, Palla L, Pascali M, De Angelis
B, Curcio BC and Gentile P: Autologous platelet-rich plasma mixed
with purified fat graft in aesthetic plastic surgery. Aesthetic
Plast Surg. 33:716–721. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Kim IS, Park KY, Kim BJ, Kim MN, Kim CW
and Kim SE: Efficacy of intradermal radiofrequency combined with
autologous platelet-rich plasma in striae distensae: a pilot study.
Int J Dermatol. 51:1253–1258. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Lee JW, Kim BJ, Kim MN and Mun SK: The
efficacy of autologous platelet rich plasma combined with ablative
carbon dioxide fractional resurfacing for acne scars: a
simultaneous split-face trial. Dermatol Surg. 37:931–938. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Bielecki T, Dohan Ehrenfest DM, Everts PA
and Wiczkowski A: The role of leukocytes from L-PRP/L-PRF in wound
healing and immune defense: new perspectives. Curr Pharm
Biotechnol. 13:1153–1162. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Burnouf T, Chou ML, Wu YW, Su CY and Lee
LW: Antimicrobial activity of platelet (PLT)-poor plasma, PLT-rich
plasma, PLT gel, and solvent/detergent-treated PLT lysate
biomaterials against wound bacteria. Transfusion. 53:138–146. 2013.
View Article : Google Scholar : PubMed/NCBI
|