Cancer is one of the most dreaded diseases and is a
major threat to human life. Among different clinical disorders,
cancer is the second most common cause of death after
cardiovascular diseases (1).
Different approaches and strategies, such as chemotherapy,
radiotherapy, surgery, immunotherapy and small molecule-targeted
therapy, have been studied and applied to target and treat cancer
(2,3).
Chemotherapeutic drugs work by targeting
fast-growing and proliferating cells, leading to cell death and
shrinking of the tumors. The conventional cancer chemotherapy, ‘the
standard treatment’, is not always successful, even after 50–100
years of research and clinical experience, although cases of
lymphocytic leukemia and Hodgkin's lymphoma have been treated
successfully in this manner (1).
Conventional chemotherapy indiscriminately delivers the toxic
anticancer agent to tumors and normal tissues simultaneously
(4). Therefore, cancer-selective
drug delivery approaches are required to avoid undesirable systemic
side effects. One way of tackling these problems is to deliver
anticancer drugs selectively to the tumor site (5). One of the different approaches is
using gasotransmitters to selectively provide anticancer drugs to
the tumor site (6).
The three small, diffusible gaseous mediators nitric
oxide (NO), carbon monoxide (CO) and hydrogen sulfide
(H2S) serve multiple roles in normal physiology and the
pathogenesis of numerous diseases. Several studies have emphasized
the roles of NO, CO and H2S in cancer (7–10);
however, there are numerous puzzles and controversies. Some studies
have demonstrated that these mediators are pro-tumorigenic, while
others have reported that they have an antitumorigenic effect
(11–13). It is now recognized that these
three gases exhibit bell-shaped (also termed ‘biphasic’, ‘bimodal’
or ‘Janus-faced’) pharmacological characteristics in cancer
(6). An improved understanding of
the complicated pharmacological nature of these mediators has
far-reaching consequences. It also tackles some of the difficulties
of the field, enabling the development of novel therapeutic
techniques based on pharmacologically suppressing mediator
production (6). The present
review discusses the important roles of NO, CO and H2S
in tumor pathophysiology, addressing how different levels of these
gases can affect tumor growth, angiogenesis and survival.
Furthermore, it highlights the potential therapeutic value of the
gasotransmitters in cancer chemotherapy.
The use of chemicals to treat a disease is called
chemotherapy. This therapeutic model was conceptually born in the
early 20th century when the German physician Paul Ehrlich adopted
chemicals to treat infectious diseases (14,15). Ehrlich stepped into the field of
oncology with great ambition, trying to explore de novo
pharmacological bullets to shoot cancer cells (16). The net findings of all his
experiments were disappointing since none of the proposed drugs
worked on cancer cells (17).
Cancer chemotherapy remained indistinct for >30
years, and scientists continued to follow Ehlrich's fishing
strategy after his death. Certain researchers studied the effect of
mustard gas or its derivatives on bone marrow eradication; an idea
that was obtained from using the gases during the First World War
(18,19). Others, such as Sidney Farber, used
anti-folates, such as aminopterin and 6-mercaptopurine, to treat
childhood cancers (20). In 1950,
6-mercaptopurine was selected for a clinical trial investigating
the treatment of acute lymphatic leukemia in children. Despite the
promising initial results leading to cancer remission, all
investigated chemicals had significant adverse effects indicated by
quick relapse a few weeks after treatment (21). The chemotherapeutic drug screening
mission was continued. By 1964, ~215,000 chemicals, plant
derivatives and fermentation products were studied, and several
million mice were included in these studies (22). The challenges encountered in the
discovery and delivery of the proper anticancer chemotherapeutics
were developing a convenient model to reduce the vast repertoire of
chemicals into a considerable list that could have efficiency
against cancer, obtaining suitable funds to support the suggested
studies and treatment modalities, and admission to clinical
facilities to examine the impact of the selected substances.
Therefore, different organizations, funding agencies and research
centers were established to support scientists and oncologists
economically, in order to defeat cancer.
After all these chemotherapeutic screening failures,
scientists turned the view back, asking what makes cancer cells
switch their response to treatment from sensitive to resistant.
Scientists examined if it would be better to employ dual
chemotherapy rather than the conventional monotherapy approach
used, and this idea of using multiple chemical combinations
immediately appeared promising. Freireich et al (23) were the first scientists who
combined a four-drug regime (vincristine, amethopterin,
mercaptopurine and prednisone) to treat leukemia in children.
Despite full cancer remission for several months, they observed
severe brain metastasis and death, and thus, stopped this
chemotherapeutic regimen. The outcome of tetra-combinatorial
therapeutic approaches, including mechlorethamine, oncovin,
procarbazine and prednisone (MOPP), and mechlorethamine, oncovin,
methotrexate and prednisone, in treating Hodgkin's diseases was
surprising, as the complete remission rate increased to 80% in the
USA (24). Furthermore, ~60% of
patients with Hodgkin's treated with MOPP never relapsed (25). MOPP, ‘the miracle’, made the
concept of cancer curability possible. Indications from combination
chemotherapies in treating certain types of advanced hematological
malignancies motivated scientists to consider a similar therapeutic
regime for solid tumors; however, the primary method for treating
solid tumors was surgery (26).
By the early 1970s, the adjuvant chemotherapy approach was
introduced, where chemotherapy was used after surgery to target
microscopic tumors and reduce cancer recurrence (26). Bonadonna et al (27) introduced the first combinational
chemotherapeutic-postoperative approach, called cyclophosphamide,
methotrexate, fluorouracil-adjuvant therapy, to treat early-stage
breast cancer in women. The concept of combinational adjuvant
chemotherapy was popular in the USA. Fisher et al (28) examined L-phenylalanine mustard to
target breast cancer and other solid tumors, such as colorectal
cancer. Depending on the type and size of the tumor, an additional
approach, called neoadjuvant chemotherapy, is currently used. In
this approach, chemotherapy is applied before the surgery or the
primary therapy (29).
Most, if not all, solid tumors acquire drug
resistance after a few cycles of chemotherapy, and thus, an
efficient chemotherapeutic approach has not been developed yet.
This is mainly due to dynamic phenotypic and genotypic changes in
cancer cells and their surrounding microenvironment. Despite the
common non-curative effect of chemotherapy, the disease
progression-free survival curves have been markedly improved
(30). Any effective therapeutic
approach requires systematic knowledge regarding the drug's
mechanism of action, primary pharmacologic metabolites, the
differences in pharmacokinetics and pharmacodynamics, and the
behavior of cancer cells and their crosstalk with the tumor
microenvironment (TME) (31).
This knowledge has markedly progressed during the last 20–30 years
upon the emergence of novel technical avenues in genomic and
proteomic analysis. As a result, novel treatment modalities, such
as immunotherapy and targeted therapy, have been introduced and
suggested to be applied either separately or in combination with
chemotherapy.
Chemotherapeutic drugs are clustered into subgroups
according to their structure and overall mechanisms of action. Each
subgroup is subdivided into several cytostatic drugs, which are
used to treat different types of cancer (32). Table SI lists the most prominent types
of drugs, their mechanism of action, the targeted cancer types and
the number of clinical trials for each drug.
In non-hematological malignancy, a tumor is a
disorganized, miscommunicated aberrant tissue, where tumor cells
are surrounded by stroma and they all interact unsystematically
within one unit. The stroma consists of cellular and non-cellular
compartments, and altogether they are referred to as the TME. The
TME is made up of different types of cells, such as
cancer-associated fibroblasts (CAFs), tumor-associated macrophages
(TAMs), different sub-types of anti- and pro-inflammatory immune
cells, adipocytes and tumor-associated vasculature (endothelial
cells and pericytes), and extracellular matrix (ECM) (33). These compartments interact with
each other and with tumor cells, initiating various biochemical and
cellular signals, which drive cancer cell proliferation, invasion
and the response to treatment (34). Chemotherapy eliminates and reduces
tumor growth primarily, whereas a small population of cancer cells
shift their survival machinery and do not respond to the treatment,
as they become more aggressive cells, which serve as the source of
relapse. The TME has the potential to drive the
anti-chemotherapeutic effect of cancer cells by interfering with
different survival mechanisms and cellular signaling pathways
(35). This is evident in
different types of cancer, such as breast and ovarian cancer, in
which enriched TME signatures associated with a treatment-resistant
phenotype are observed (34).
Among the different signatures, the hypoxic nature of the TME
decreases the proliferation rate and induces survival of cancer
cells, thus reducing their response to chemotherapy (36–38). The hypoxic TME triggers angiogenic
switch by inducing aberrant blood vessel formation in cancer, and
due to the leaky properties of cancer-associated vasculature, the
drugs that circulate in the blood will not be delivered efficiently
to the core of the tumor (39,40). Additionally, the pharmacokinetic
action of certain chemotherapeutic drugs depends on the
availability of free radicals. Therefore, the cytotoxic activity of
those drugs is reduced in the absence or presence of low oxygen
(O2) levels (40,41).
The architecture of the TME, characterized by its
phenotypic plasticity and heterogenic properties, is essential to
allow or prevent drug delivery to the tumor (42). The reorganization of the ECM due
to the interaction of cancer cells with CAFs and TAMs leads to drug
sequestration, preventing them from reaching the cancer cells
(34,43,44).
In the last decades, three gaseous molecules have
been identified as gasotransmitters: NO, CO and H2S.
These particular gases are similar to each other in their
production and function, but exert their functions in unique ways
in the human body (45). NO is
produced endogenously in endothelial cells from L-Arg by a family
of enzymes, called NO synthases (NOS), in the vasculature, which
modulates vascular tone by activating soluble guanylyl cyclase
(sGC) enzyme and producing cyclic GMP (46). Endogenous CO is produced by the
enzyme heme oxygenase (HO), which converts free heme to biliverdin
(47). CO has a vasorelaxant and
an antiproliferative action on vascular smooth muscles cells
(VSMCs), making it an important determinant of vascular tone in
several pathophysiological conditions (48). H2S is produced
endogenously in mammalian tissues from L-cysteine by
cystathionine-β-synthase (CBS), cystathionine γ-lyase and another
mitochondrial enzyme, 3-mercaptopyruvate sulfurtransferase
(49). It regulates vascular
diameter, and protects the endothelium from oxidative stress,
ischemia reperfusion injury and chronic inflammation by activating
several K+ channels in VSMCs (50,51). According to Wang et al
(52), other molecules, such as
sulfur dioxide, methane, hydrogen gas, ammonia and carbon dioxide,
are also considered to be potential gasotransmitter candidates,
despite the fact that they have not been adequately explored or do
not completely fit the diagnostic criteria for endogenous
gasotransmitters.
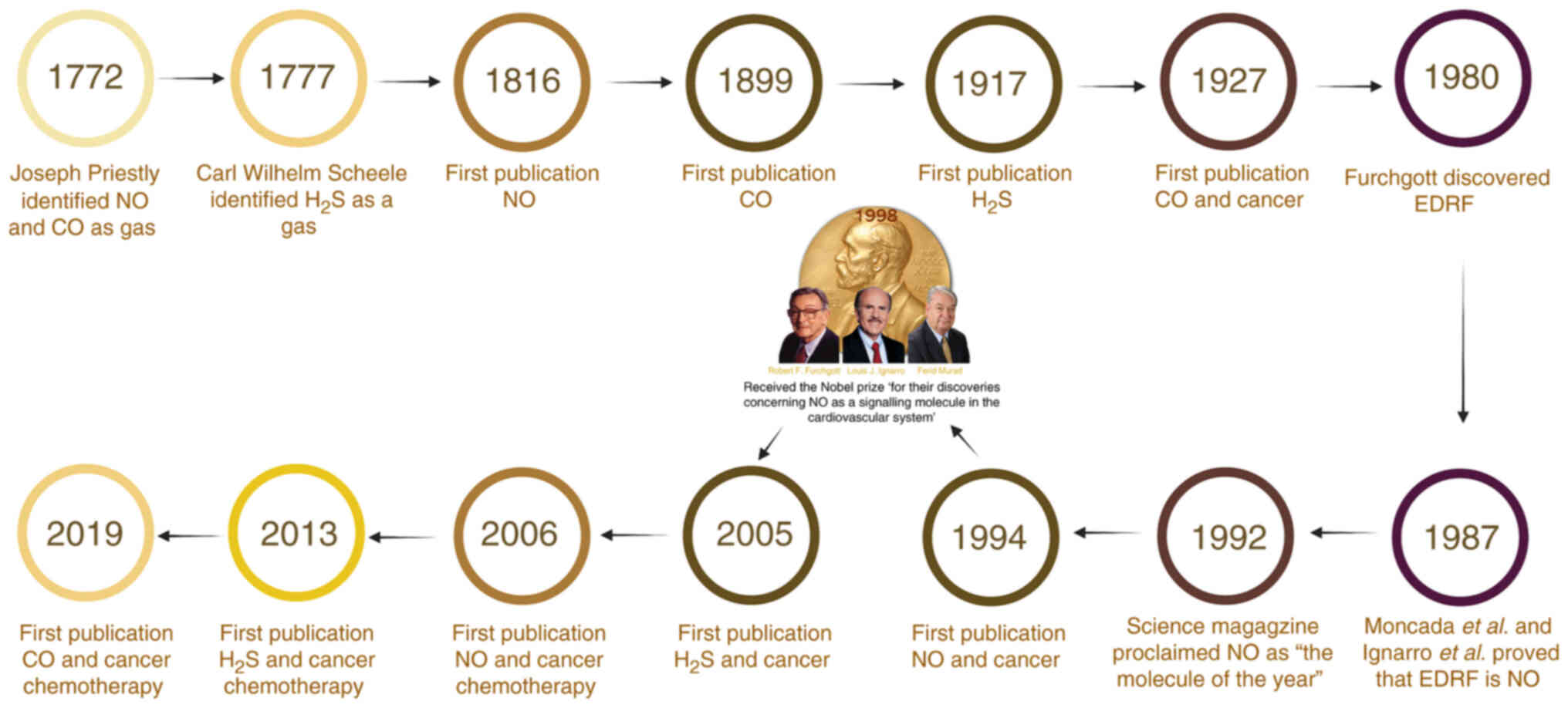
NO was discovered in 1772 by Joseph Priestley as a
clear, colorless gas with a half-life of 6–10 sec (53). In 1979, Gruetter et al
(54) found that adding NO in a
mixture with nitrogen or argon gases into an organ bath vessel
containing isolated pre-contracted strips of a bovine coronary
artery induces vascular smooth muscle relaxation. In 1980,
Furchgott and Zawadzki (55)
revealed that endothelial cells produce endothelium-derived
relaxing factor (EDRF) in response to stimulation by acetylcholine
in vessels with intact endothelium. After 7 years and in two
unrelated studies, both Ignarro et al (56,57) and Palmer et al (56,57) demonstrated that EDRF is NO.
Moncada et al (58)
demonstrated that NO is synthesized from the amino acid L-arginine.
Earlier, Murad et al (59)
reported that nitro vasodilators, such as nitroglycerin (GTN) and
sodium nitroprusside, induce vascular tissue relaxation, stimulate
sGC expression and increase cGMP levels in tissues. All these
studies contributed to the establishment of a signaling molecule in
the cardiovascular system. In 1992, the cover of Science magazine
proclaimed NO as the molecule of the year (60). Furthermore, 6 years later, Pfizer,
Inc. introduced Viagra, a drug that inhibits phosphodiesterase-5
via the NO-cGMP signaling cascade, which revolutionized the
management of erectile dysfunction (61). In the same year, the importance of
the NO discovery was acknowledged by awarding the Nobel Prize in
Physiology and Medicine to Furchgott, Ignarro and Murad (62).
Few discoveries have had the type of impact on
biology that NO has had since it was discovered (63). The first scientific article
described NO in 1816 (64), while
in 1994, Thomsen, et al (48,65) were the first to report a link
between NO and cancer action. In 1993, there were >1,000 new
publications on the biology of NO. At the end of the 20th century,
the rate of NO publications approached a plateau at ~6,000 papers
per year, spanning almost every area of biomedicine (63). The number of published articles in
PubMed (pubmed.ncbi.nlm.nih.gov/) reached 58,848 by the end of
2020.
In the late 1200s, a poisonous gas produced by the
incomplete combustion of wood similar to CO was described by the
Spanish alchemist Arnold of Villanova (66). Between 1772 and 1799, an English
chemist, Joseph Priestley, recognized and characterized CO
(53). The first scientific
article described CO in 1899 (67), and subsequently, the ‘first paper
linking CO to cancer was published in 1927 (68). Between 1920 and 1960, Roughton
performed several kinetic studies on CO and hemoglobin (69–71). In 1944, he revealed that CO bound
to hemoglobin changed the oxyhemoglobin dissociation curve, and
demonstrated that CO was produced in the body during the metabolism
of the hemoglobin molecule (72).
Subsequently, Tenhunen et al (73) described and characterized HO as
the enzyme responsible for breaking down heme in the body,
demonstrating that heme catalysis resulted in the subsequent
release of CO and free iron as by-products.
NO is a small biomolecule that exerts different
effects on tumor growth and invasion. It is a pleiotropic regulator
and serves essential roles in various intercellular or
intracellular processes, including vasodilatation,
neurotransmission and macrophage-mediated immunity (7). Vascular endothelial cells can
synthesize NO from L-arginine, and this biosynthetic pathway has
been thoroughly documented in numerous other cell types, including
nervous and immune cells (80,81). It can display a cytotoxic property
at higher concentrations as generated by activated macrophages and
endothelial cells (7). A total of
three different isoforms of the NOS family synthases have been
identified: Endothelial NOS (eNOS), neuronal NOS (nNOS) and
inducible NOS (iNOS). The gene symbol nomenclatures are NOS1 for
nNOS, NOS2 for iNOS and NOS3 for eNOS (7). However, the role of NO in cancer
biology, particularly in breast cancer, only started to be
elucidated in 1994 (82). It has
been detected that NOS expression is increased in various types of
cancer, such as breast, cervical, brain, laryngeal, and head and
neck cancer (83) (Table I). NO exhibits a pro- or
antitumorigenic effect (84). NO
appears to enhance tumor growth and cell proliferation at
measurable concentrations in different clinical samples from
different cancer types (85).
In contrast to conventional signaling molecules that
act by binding to specific receptor molecules, NO exerts its
biological actions via a wide range of chemical reactions (86). The NO concentration and minor
differences in the composition of the intracellular and
extracellular environment determine the exact reactions attained.
Under normal physiological conditions, cells produce small but
significant amounts of NO, contributing to the regulation of
anti-inflammatory effects and its antioxidant properties (83). However, in tissues with a high NO
output, iNOS is activated, and nitration (addition of
NO2), nitrosation (addition of NO+) and
oxidation will be dominant (87).
The interaction of NO with O2 or superoxide
(O2−) results in the formation of reactive
nitrogen species (RNS). The RNS, dinitrogen trioxide
(N2O3) and peroxynitrite (ONOO), can induce
two types of chemical stresses: Nitrosative and oxidative (88). N2O3
effectively nitrosates various biological targets to yield
potentially carcinogenic nitrosamines and nitrosothiol derivatives,
and N-nitrosation may have essential implications in the known
association between chronic inflammation and malignant
transformation (88).
O2− and NO may rapidly interact to produce
the potent cytotoxic oxidants ONOO− and its conjugated
acid, peroxynitrous acid. In natural solutions, ONOO is a powerful
oxidant, oxidizing thiols or thioethers, nitrating tyrosine
residues, nitrating and oxidizing guanosine, degrading
carbohydrates, initiating lipid peroxidation, and cleaving DNA,
which has important implications in cancer (83).
The effects of NO in a multistage model of cancer
have been reported previously, it can drive angiogenesis,
apoptosis, the cell cycle, invasion and the metastatic process
(83,85). NO also serves a role in cellular
transformation, the onset of neoplastic lesion formation, and the
monitoring of invasion and colonization throughout metastasis
(89). Therefore, understanding
its role in promoting TME elements is crucial as it will reduce the
ambiguity, and aid the development of NO-based cancer therapeutics,
which will be effective in the prevention and treatment of a range
of human cancer types.
The TME is characterized by hypoxia and acidity.
Small pH drops (−0.6 U) favor the production of bioactive NO from
nitrite, as evidenced by a higher degree of cyclic guanosine
3′,5′-monophosphate-dependent vasorelaxation in arterioles. A small
dose of nitrite may make tumors more sensitive to radiation,
resulting in a considerable growth delay and improved survival in
mice (90). Therefore, low pH has
been revealed to be an ideal setting for tumor-selective NO
generation in response to nitrite systemic injection (90). The generation of NO by iNOS
inhibits C-X-C motif chemokine ligand 10 expression in melanoma
cells, resulting in a protumorigenic TME (91). Furthermore, eNOS upregulation in
the TME reduced both the frequency and size of tumor implants in a
surgical model of pancreatic cancer liver metastasis (92) and the influence of NO on tumor
cell protease expression since tumor cell anoikis and invasion are
both regulated by myofibroblast-derived matrix. Within tumor cells,
eNOS-dependent downregulation of the matrix protease cathepsin B
was detected, and cathepsin B silencing reduced tumor cell
invasiveness in a manner comparable to eNOS upregulation.
Therefore, an NO gradient within the TME influences tumor
progression through orchestrated molecular interactions between
tumor cells and stroma.
The role of NO in the complex interactions between
the TME and the immune response is a good example of how
complicated the molecular and cellular mechanisms determining the
involvement of NO in cancer biology are. Although the activities of
NO in the TME are varied and context-dependent, the evidence
suggests that NO is an immunosuppressive mediator (93). By targeting tumors in a cell
nonautonomous manner, S-nitroso glutathione (GSNO), a NO donor,
reduced the tumor burden in a mouse model of castration-resistant
prostate cancer (CRPC). Both the abundance of anti-inflammatory M2
macrophages and protein kinase R-like endoplasmic reticulum kinase
expression were decreased by GSNO, indicating that NO influences
TAM activity. GSNO also reduced IL-34, indicating that TAM
differentiation was suppressed. This demonstrates the importance of
NO in CRPC tumor inhibition via the TME (94).
One of the important characteristics of cancer
cells is the acidic microenvironment (reduced intracellular pH) due
to accumulation of lactic acid that results from a high rate of
glycolysis. H2S donors trigger the activation of
cellular transporters, such as glutamine transporter-1 (GLT-1) and
ATP-binding cassette transporter A1, which directly regulates the
aerobic glycolysis, which is a metabolic indicator of cancer
(116). Nevertheless, activation
of GLT-1 has both a promoting and an inhibiting effect depending on
the cancer cell type, and thus, further studies are required to
clarify the consequent responses (8).
It has been demonstrated that most cancer cells
exhibit increased uptake of glucose and high lactate production,
known as the Warburg effect, due to glycolysis that causes the
acidic TME, which enhances tumor progression (117). Previous studies have
demonstrated that continuous exposure of cancer cells to a low
concentration of H2S results in inhibition of cancer
progression. This anticancer effect is mainly due to an increase in
metabolic lactic acid production by H2S and diminishes
the pH regulatory system, which consequently leads to intense
intracellular acidification and eventually drives cancer cell death
(107,118).
Within the TME, there are key proteins and enzymes,
such as matrix metalloproteinase, adhesive enzymes (E-cadherin) and
integrins, which serve an essential role in the migration and
metastasis of cancer cells (119,120). Tumor cells that enter the stroma
within the TME after detaching from the main tumor move into the
blood vessels and ultimately reach the other organs in the body
(121). H2S donors
have been used in different studies and have been demonstrated to
successfully prevent migration and invasion by decreasing proteins
and enzymes involved in migration and invasion in different cancer
types (8,122,123). For example, it has been reported
that treatment of hepatocellular carcinoma cells with 600–1,000 µM
sodium hydrosulfide (NaHS), which is an H2S donor,
efficiently reduces migration and invasion in a
concentration-dependent manner via modulation of the EGFR/ERK/MMP-2
and PTEN/AKT signaling pathways (124). Similarly, NaHS treatment
prevents migratory activity in thyroid cancer cells by deactivating
the PI3K/AKT/mTOR and MAPK signaling pathways (125). Furthermore, NaHS reduces the
MMP-2 protein levels in gastric cancer (126). Additionally, H2S
serves a role in a different stage of cancer development and is
involved in modulation of the TME, which regulates the rate of
cancer progression and the effectiveness of therapy (106).
CO is best recognized for being a toxic gas
produced by the burning of fossil fuels. On the one hand, CO
poisoning is associated with high mortality rates, and thus, it
attracts a lot of attention (127). On the other hand, CO has been
conclusively demonstrated to be a gasotransmitter with
physiological activities in mammals (128,129). CO is now accepted as a potential
therapeutic agent along with its physiological roles and has
entered multiple clinical trials (130,131). CO is produced in all cells by
HO-1 and HO-2 (132). Each
possesses strong cytoprotective functions for the cell, evidenced
by the fact that the absence of either, particularly the
stress-response isoform HO-1, is detrimental to the cell and
organism (133,134). The inducible HO isoform (HO-1)
can be upregulated in response to various stimuli, including heme,
oxidative stress, ultraviolet irradiation, heat shock, hypoxia and
NO (135). The constitutive HO
isoform (HO-2) is expressed in several tissues, including the
brain, kidney, liver and spleen (6). Low CO concentrations also activate
KATP channels and influence various intracellular kinase
pathways, including the PI3K-AKT and p38 MAPK signaling pathways
(128). CO exerts adverse
biological effects at higher concentrations, which, in vivo,
are mainly attributed to the binding of CO to hemoglobin. The
resulting carboxyhemoglobin reduces the O2-carrying
capacity of the blood and leads to tissue hypoxia. In vitro,
CO inhibits mitochondrial electron transport by irreversibly
inhibiting cytochrome c oxidase (128).
Cellular and animal pharmacological experiments
suggest numerous therapeutic indications where HO-1 or CO
administration imparts benefits in treating conditions such as
sepsis, bacterial infection, cancer, inflammation, circadian clock
regulation, stroke, erectile dysfunction and heart attack (131). Some of the best-characterized
physiological effects of CO include anti-inflammatory,
antiproliferative, anti-apoptotic and anticoagulative responses. By
contrast, at higher concentrations, CO becomes cytotoxic (136). In contrast to NO, the
cytoprotective and cytotoxic effects of CO are intimately
intertwined. For example, a low level of CO-mediated inhibition of
mitochondrial activity, followed by a slight increase in
intracellular reactive O2 species production, is
important in CO-mediated cytoprotective signaling events (137,138). In a way, the cytoprotective
effects of CO resemble the protective effects of pharmacological
preconditioning. A short, relatively mild insult triggers a
secondary cytoprotective phenotype via activation of the
prototypical antioxidant response element NRF2-related factor.
Thus, a protective cellular phenotype is maintained in the cell for
a long time after CO has already been cleared from the biological
system (6).
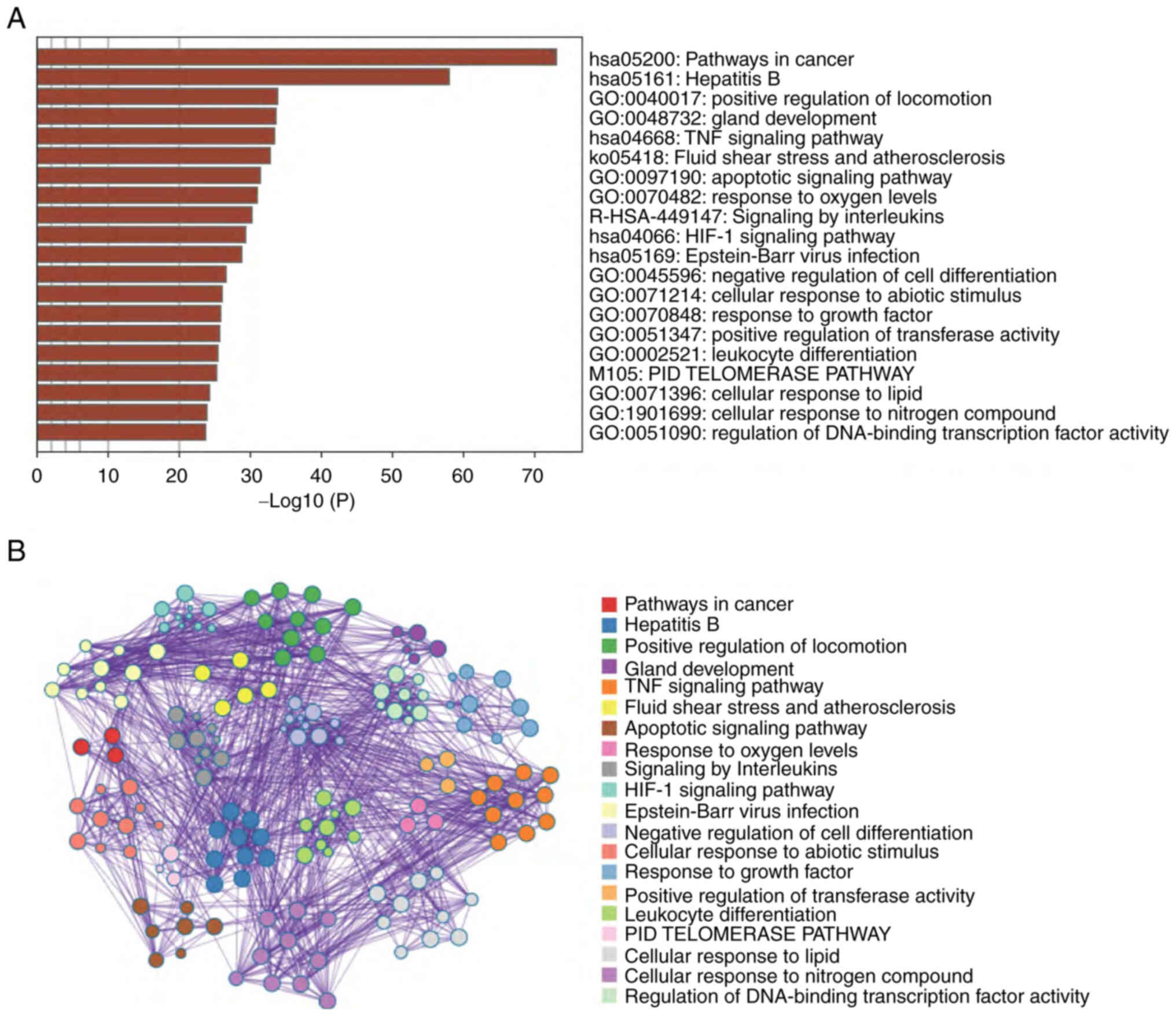
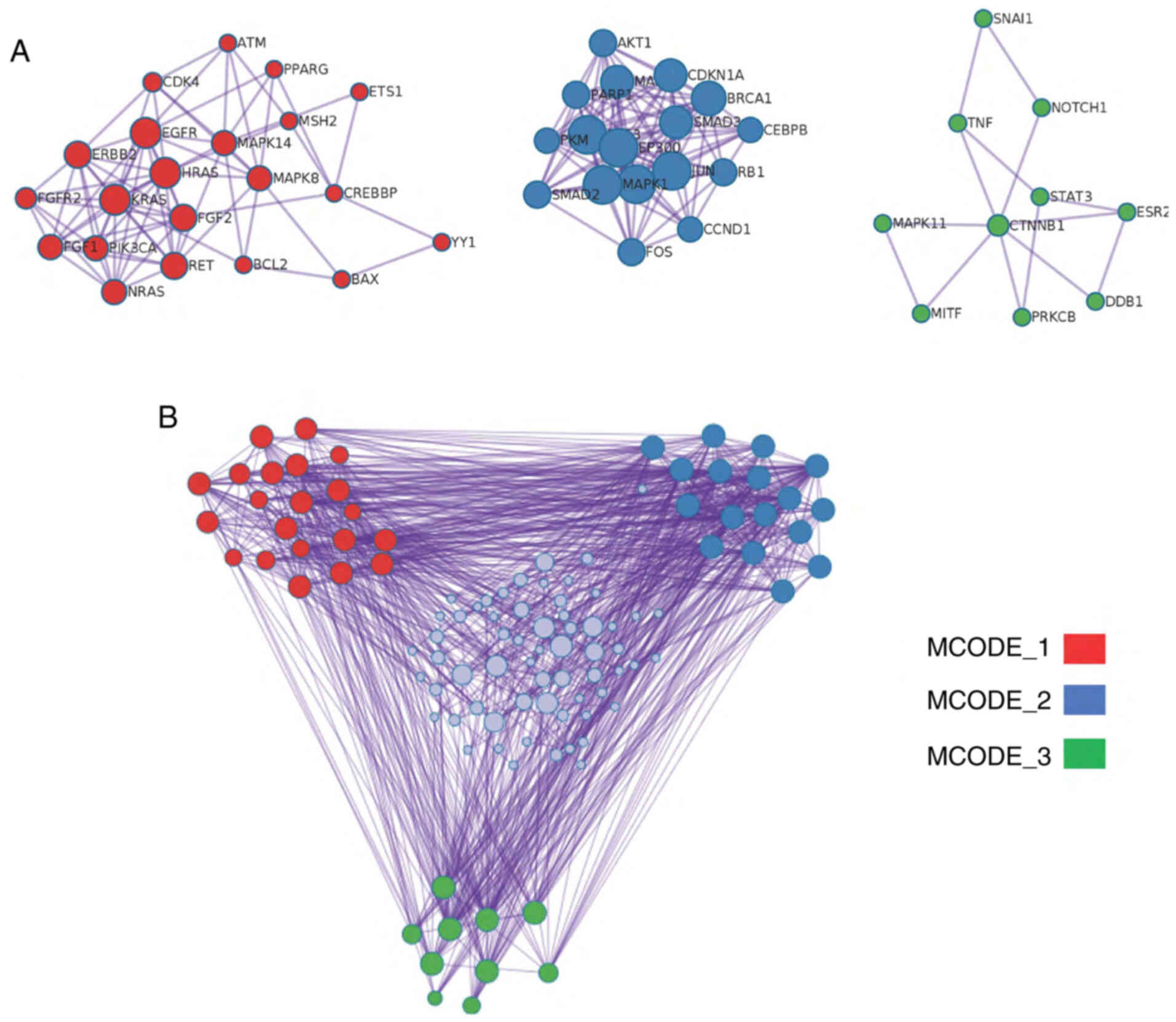
To highlight the significance of gasotransmitter
signaling cascades in tumor growth and the chemotherapeutic
response, network analysis approaches were utilized to identify the
gasotransmitter-tumor signaling signature. Utilizing the PubMed
(https://pubmed.ncbi.nlm.nih.gov/) and
Web of Science (https://clarivate.com/webofsciencegroup/solutions/web-of-science/)
databases, ~127 candidates (genes and proteins) were identified,
which were significantly related to the gasotransmitters and
tumorigenesis simultaneously. Using the selected list of
candidates, the present network analyses were applied using the
Enrich R (https://maayanlab.cloud/Enrichr/) and Metascape
(https://metascape.org/gp/index.html#/main/step1)
databases to identify all possible genes, proteins and pathways
that may represent tumor-gasotransmitters interrelated signaling.
As shown in Fig. 2A and B, the
most relevant enriched pathways in the present analysis were ones
related to cancer, which in turn, justifies the relevance and
accuracy of the selected candidate list and highlights the
significance of gasotransmitter signaling cascades in tumor
development and growth. Additionally, different essential cellular
signaling pathways were significantly enriched, such as the
‘positive regulation of locomotion’, ‘TNF signaling pathway’,
‘apoptotic signaling pathway’ and ‘HIF-1 signaling pathway’. These
pathways serve an essential role in driving the fate of cancer
cells and their response to different treatment modalities
(139). Therefore, it is
reasonably relevant to investigate the crosstalk between
gasotransmitters and tumor cells.
The present review investigated links between the
current candidate list and a drug signature database containing
annotations regarding drug induction or inhibition of gene
expression. As shown in Table
SII, the present candidate list was significantly enriched and
associated with different anticancer or cancer-related drugs. The
odds ratio ranking method is simply the odds ratio; however, the
combined score is the odds ratio multiplied by the negative natural
log of the P-value derived from Fisher's exact test and the Enrichr
z-score (combined score=log(p)*z). Overall, this suggested that
gasotransmitters serve essential roles in drug response signaling
by cancer cells. Therefore, well-designed mechanistic studies are
required to elucidate such roles and open novel avenues for drug
discovery and cancer treatment modalities.
Following the crucial discovery of gasotransmitters
as fundamental biological molecules, their physiological
significance has become a debated topic in recent decades.
Utilizing gasotransmitters as therapeutic aids is justified by
their roles in carcinogenesis, including enhancement of apoptotic
stimuli, inhibition of metastasis and inhibition of angiogenesis.
Therefore, using them alone or in combination with cytotoxic agents
is an essential research platform for researchers and clinicians in
cancer therapy (6,140–142).
Platinum compounds have been investigated
extensively, and several studies have demonstrated that tumor cells
are sensitized to cisplatin compounds by NO donors (143,144). In vitro, combination of
cisplatin with natural NO gas or the NO donors diethylamine NONOate
(DEA NONOate) or 1-propanamine,
3-(2-hydroxy-2-nitroso-1-propylhydrazino) NONOate increased the
killing efficacy of cisplatin by 50–1,000 times compared with
cisplatin alone, and the effect lasted for a number of hours
(145). Furthermore, the
combination treatment of cisplatin and diethylenetriamine NONOate
reverses resistance and induces apoptosis in prostate cancer cell
lines (146) and metastatic
human colon carcinoma cell lines (147). NO-producing aspirin compounds
that can emit NO for several hours have also been investigated. For
example, in a clonogenic assay, nitroaspirin exhibited
dose-dependent cytotoxicity and greatly boosted cisplatin
cytotoxicity in both resistant and susceptible cells (148).
Carmustine is a chemotherapeutic drug that is
combined with a NO source (the donor drug DEA NONOate), and the
combination of chlorotoxin-NO, carmustine, or temozolomide enhances
glioma cell death. Two variables that contributed to the enhanced
cytotoxic activity of these cells were the production of active
levels of the cytoprotective enzyme O6-methylguanine-DNA
methyltransferase activity and altered p53 activity (149).
In the same year, Shami, Saavedra, Wang, Bonifant,
Diwan, Singh, Gu, Fox, Buzard, Citro, Waterhouse, Davies, Ji and
Keefer (150) created
glutathione/glutathione S-transferase-activated nitric oxide
(JS-K), a selective targeted NO donor that was active in
vitro and in vivo against human HL60 leukemia cells,
following its reaction with glutathione to produce NO in
vivo. JS-K acts as a chemosensitizer for doxorubicin-induced
cytotoxicity in renal (151),
prostate (152) and bladder
cancer cells (153).
NF-κB and NOS activation make HT29 human colon
cancer cells more sensitive to doxorubicin cytotoxicity (154). Simvastatin increases NF-κB
activity and NO production, while also increasing doxorubicin
intracellular accumulation and cytotoxicity (154). The enhanced intracellular
accumulation of doxorubicin is caused by tyrosine nitration in
P-glycoprotein and multidrug resistance protein 1 by NO (155). In mice with triple-negative
breast cancer, NO-releasing nanoparticles in combination with
doxorubicin or a doxorubicin nanoparticle carrier decreased cell
survival, caused apoptosis, elevated doxorubicin intracellularly,
compromised lysosomal membrane integrity and suppressed tumor
growth (156). Subsequently, an
S class nanocarrier of NO (Nano-NO) was developed, and successfully
targeted NO to hepatocellular cancer (157). Nano-NO has improved the
administration and efficacy of chemotherapy. Additionally,
combining nanomaterials with NO donors, as shown by Housein et
al (78) and others (158), has improved the method of NO
delivery. The aforementioned Nano-NO make tumor cells more
susceptible to chemotherapy.
GTN in combination with vinorelbine and cisplatin
increases the response in patients with lung cancer and reduces the
median time to tumor progression (159). Additionally, the combination
treatment of GTN and valproic acid results in the inhibition of
Bcl-2 as well as the expression of Bax and caspase-3 in human K562
cells (160). STAT3 is
associated with a number of the substituted NO-releasing
quinolone-1,2,4-triazole/oxime derivatives (161). In melanoma with the B-Raf V600E
mutation and vemurafenib-resistant melanoma, STAT3 inhibitors have
shown efficacy (161). Poly-S
nitrosylated human albumin alters colon cancer cell resistance to
bevacizumab (162). Furthermore,
the combination of bevacizumab with S-nitrosylated human albumin
exhibits antitumor effects both in vitro and in vivo
(163).
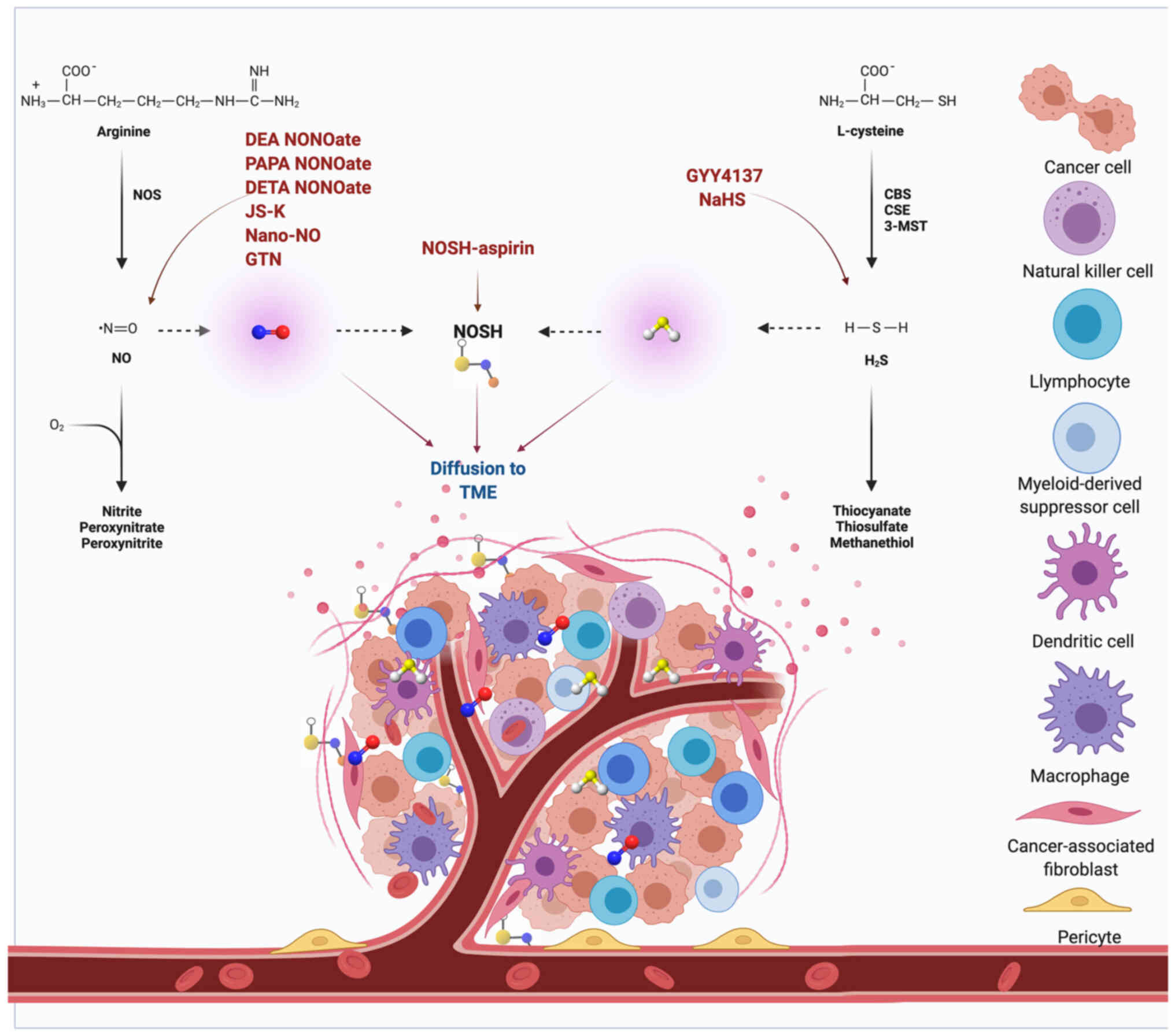
One must remember that the three gasotransmitters
do not work alone. Instead, they work together. This cooperation
occasionally occurs using overlapping signaling pathways (for
instance, both NO and CO stimulate the sGC pathway). NO directly
stimulates the sGC pathway, and H2S concurrently blocks
cGMP via inhibition of cGMP phosphodiesterase (166). One of the few studies of this
contest demonstrated the anticancer effect of a combined NO- and
H2S-donating compound, nitric oxide and hydrogen
sulfide-releasing hybrid-aspirin, both in vitro and in
vivo (6). The impact of NO
and H2S on the TME is displayed in Fig. 4, and several gasotransmitter-based
drugs targeting the TME are currently being investigated in
clinical studies (167–169). To further investigate and
understand the nature of these interactions, more comprehensive
studies are required, mainly in the context of cancer, which may be
utilized for therapeutic benefits in the future.
More than three decades of studies in the field of
the three gasotransmitters NO, CO and H2S have resulted
in the identification of several pathophysiological paradigms and
associated experimental therapeutic approaches that may be
ultimately suitable for clinical translation. In particular, the
initial perplexing observation that both gasotransmitter-synthesis
inhibitors and donors appear to have anticancer effects, which the
complex biology and bell-shaped pharmacology of NO, CO and
H2S can explain, should not be considered as a barrier
to translation into clinical settings. Their critical functions in
normal cells compared with cancer cells open avenues for
combinatorial treatment approaches together with chemotherapeutic
drugs, aiming for improved clinical significance.
Not applicable.
Funding: No funding was received.
Not applicable.
MAAN, ZOK, ZH, HAH, RMA and BMH wrote the
manuscript and designed the figures. AS and TA wrote the manuscript
and critically revised the paper. Data authentication is not
applicable. All authors read and approved the final manuscript.
Not applicable.
Not applicable.
The authors declare that they have no competing
interests.
|
1
|
Leaf C: Why we're losing the war on cancer
(and how to win it). Fortune. 149:76–82. 84–86. 882004.PubMed/NCBI
|
|
2
|
Debela DT, Muzazu SG, Heraro KD, Ndalama
MT, Mesele BW, Haile DC, Kitui SK and Manyazewal T: New approaches
and procedures for cancer treatment: Current perspectives. SAGE
Open Med. 9:205031212110343662021. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Ke X and Shen L: Molecular targeted
therapy of cancer: The progress and future prospect. Front
Laboratory Med. 1:69–75. 2017. View Article : Google Scholar
|
|
4
|
Liang XJ, Chen C, Zhao Y and Wang PC:
Circumventing tumor resistance to chemotherapy by nanotechnology.
Methods Mol Biol. 596:467–488. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Iyer AK, Khaled G, Fang J and Maeda H:
Exploiting the enhanced permeability and retention effect for tumor
targeting. Drug Discov Today. 11:812–818. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Szabo C: Gasotransmitters in cancer: From
pathophysiology to experimental therapy. Nat Rev Drug Discov.
15:185–203. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Xu W, Liu LZ, Loizidou M, Ahmed M and
Charles IG: The role of nitric oxide in cancer. Cell Res.
12:311–320. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ngowi EE, Afzal A, Sarfraz M, Khattak S,
Zaman SU, Khan NH, Li T, Jiang QY, Zhang X, Duan SF, et al: Role of
hydrogen sulfide donors in cancer development and progression. Int
J Biol Sci. 17:73–88. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hellmich MR and Szabo C: Hydrogen sulfide
and cancer. Handb Exp Pharmacol. 230:233–241. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wegiel B, Gallo D, Csizmadia E, Harris C,
Belcher J, Vercellotti GM, Penacho N, Seth P, Sukhatme V, Ahmed A,
et al: Carbon monoxide expedites metabolic exhaustion to inhibit
tumor growth. Cancer Res. 73:7009–7021. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Vannini F, Kashfi K and Nath N: The dual
role of iNOS in cancer. Redox Biol. 6:334–343. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Kashfi K: The dichotomous role of
H2S in cancer cell biology? Déjà vu all over again.
Biochem Pharmacol. 149:205–223. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Tien Vo TT, Vo QC, Tuan VP, Wee Y, Cheng
HC and Lee IT: The potentials of carbon monoxide-releasing
molecules in cancer treatment: An outlook from ROS biology and
medicine. Redox Biol. 46:1021242021. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Gensini GF, Conti AA and Lippi D: The
contributions of Paul Ehrlich to infectious disease. J Infection.
54:221–224. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Riddell S: The emperor of all maladies: A
biography of cancer. J Clin Invest. 121:52011. View Article : Google Scholar
|
|
16
|
Bosch F and Rosich L: The contributions of
Paul Ehrlich to pharmacology: A tribute on the occasion of the
centenary of his Nobel Prize. Pharmacology. 82:171–179. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Valent P, Groner B, Schumacher U,
Superti-Furga G, Busslinger M, Kralovics R, Zielinski C, Penninger
JM, Kerjaschki D, Stingl G, et al: Paul Ehrlich (1854–1915) and his
contributions to the foundation and birth of translational
medicine. J Innate Immun. 8:111–120. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Faguet GB: A brief history of cancer:
Age-old milestones underlying our current knowledge database. Int J
Cancer. 136:2022–2036. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Baselga J, Bhardwaj N, Cantley LC,
DeMatteo R, DuBois RN, Foti M, Gapstur SM, Hahn WC, Helman LJ,
Jensen RA, et al: AACR cancer progress report 2015. Clin Cancer
Res. 21 (Suppl 19):S1–S128. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Farber S and Diamond LK: Temporary
remissions in acute leukemia in children produced by folic acid
antagonist, 4-aminopteroyl-glutamic acid. N Engl J Med.
238:787–793. 1948. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kotecha RS, Gottardo NG, Kees UR and Cole
CH: The evolution of clinical trials for infant acute lymphoblastic
leukemia. Blood Cancer J. 4:e2002014. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kinjo J, Nakano D, Fujioka T and Okabe H:
Screening of promising chemotherapeutic candidates from plants
extracts. J Nat Med. 70:335–360. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Freireich EJ, Karon M and Frei III E:
Quadruple combination therapy (VAMP) for acute lymphocytic leukemia
of childhood. Proc Am Assoc Cancer Res. 5:201964.
|
|
24
|
Liebman HA, Hum GJ, Sheehan WW, Ryden VM
and Bateman JR: Randomized study for the treatment of adult
advanced Hodgkin's disease: Mechlorethamine, vincristine,
procarbazine, and prednisone (MOPP) versus lomustine, vinblastine,
and prednisone. Cancer Treat Rep. 67:413–419. 1983.PubMed/NCBI
|
|
25
|
Bonadonna G, Zucali R, Monfardini S, De
Lena M and Uslenghi C: Combination chemotherapy of Hodgkin's
disease with adriamycin, bleomycin, vinblastine, and imidazole
carboxamide versus MOPP. Cancer. 36:252–259. 1975. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Arruebo M, Vilaboa N, Sáez-Gutierrez B,
Lambea J, Tres A, Valladares M and González-Fernández A: Assessment
of the evolution of cancer treatment therapies. Cancers (Basel).
3:3279–3330. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Bonadonna G, Valagussa P, Moliterni A,
Zambetti M and Brambilla C: Adjuvant cyclophosphamide,
methotrexate, and fluorouracil in node-positive breast cancer: The
results of 20 years of follow-up. N Engl J Med. 332:901–906. 1995.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Fisher B, Sherman B, Rockette H, Redmond
C, Margolese R and Fisher ER: 1-phenylalanine mustard (L-PAM) in
the management of premenopausal patients with primary breast
cancer: lack of association of disease-free survival with
depression of ovarian function. National Surgical Adjuvant Project
for Breast and Bowel Cancers. Cancer. 44:847–857. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Early Breast Cancer Trialists'
Collaborative Group (EBCTCG), . Long-term outcomes for neoadjuvant
versus adjuvant chemotherapy in early breast cancer: Meta-analysis
of individual patient data from ten randomised trials. Lancet
Oncol. 19:27–39. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Mansoori B, Mohammadi A, Davudian S,
Shirjang S and Baradaran B: The different mechanisms of cancer drug
resistance: A Brief Review. Adv Pharm Bull. 7:339–348. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Roma-Rodrigues C, Mendes R, Baptista PV
and Fernandes AR: Targeting tumor microenvironment for cancer
therapy. Int J Mol Sci. 20:8402019. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Bagnyukova TV, Serebriiskii IG, Zhou Y,
Hopper-Borge EA, Golemis EA and Astsaturov I: Chemotherapy and
signaling: How can targeted therapies supercharge cytotoxic agents?
Cancer Biol Ther. 10:839–853. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Whiteside TL: The tumor microenvironment
and its role in promoting tumor growth. Oncogene. 27:5904–5912.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Alkasalias T, Moyano-Galceran L,
Arsenian-Henriksson M and Lehti K: Fibroblasts in the Tumor
Microenvironment: Shield or Spear? Int J Mol Sci. 19:15322018.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Klemm F and Joyce JA: Microenvironmental
regulation of therapeutic response in cancer. Trends Cell Biol.
25:198–213. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Vaupel P and Multhoff G:
Hypoxia-/HIF-1α-Driven factors of the tumor microenvironment
impeding antitumor immune responses and promoting malignant
progression. Adv Exp Med Biol. 1072:171–175. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Jing X, Yang F, Shao C, Wei K, Xie M, Shen
H and Shu Y: Role of hypoxia in cancer therapy by regulating the
tumor microenvironment. Mol Cancer. 18:1572019. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Luo W and Wang Y: Hypoxia mediates tumor
malignancy and therapy resistance. Adv Exp Med Biol. 1136:1–18.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Jarosz-Biej M, Smolarczyk R, Cichoń T and
Kułach N: Tumor Microenvironment as A ‘Game Changer’ in cancer
radiotherapy. Int J Mol Sci. 20:32122019. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Befani C and Liakos P: The role of
hypoxia-inducible factor-2 alpha in angiogenesis. J Cell Physiol.
233:9087–9098. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Senthebane DA, Rowe A, Thomford NE,
Shipanga H, Munro D, Mazeedi MAMA, Almazyadi HAM, Kallmeyer K,
Dandara C, Pepper MS, et al: The role of tumor microenvironment in
chemoresistance: to survive, keep your enemies closer. Int J Mol
Sci. 18:15862017. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Hass R, von der Ohe J and Ungefroren H:
Impact of the tumor microenvironment on tumor heterogeneity and
consequences for cancer cell plasticity and stemness. Cancers
(Basel). 12:37162020. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Vitale I, Manic G, Coussens LM, Kroemer G
and Galluzzi L: Macrophages and Metabolism in the Tumor
Microenvironment. Cell Metab. 30:36–50. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Bu L, Baba H, Yoshida N, Miyake K, Yasuda
T, Uchihara T, Tan P and Ishimoto T: Biological heterogeneity and
versatility of cancer-associated fibroblasts in the tumor
microenvironment. Oncogene. 38:4887–4901. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Wang R: The Evolution of Gasotransmitter
Biology and Medicine. Signal Transduction and the Gasotransmitters:
NO, CO, and H2S in Biology and Medicine. Wang R: Humana Press;
Totowa, NJ: pp. 3–31. 2004, View Article : Google Scholar
|
|
46
|
Andrew PJ and Mayer B: Enzymatic function
of nitric oxide synthases. Cardiovasc Res. 43:521–531. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Ryter SW and Choi AMK: Heme
oxygenase-1/carbon monoxide: From metabolism to molecular therapy.
Am J Respir Cell Mol Biol. 41:251–260. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Naik JS, O'Donaughy TL and Walker BR:
Endogenous carbon monoxide is an endothelial-derived vasodilator
factor in the mesenteric circulation. Am J Physiol Heart Circ
Physiol. 284:H838–H845. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Wang R: The gasotransmitter role of
hydrogen sulfide. Antioxid Redox Signal. 5:493–501. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Tang G, Wu L, Liang W and Wang R: Direct
stimulation of K(ATP) channels by exogenous and endogenous hydrogen
sulfide in vascular smooth muscle cells. Mol Pharmacol.
68:1757–1764. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Salihi A: Activation of inward rectifier
potassium channels in high salt impairment of hydrogen
sulfide-induced aortic relaxation in rats. Physiol Pharmacol.
19:263–273. 2016.
|
|
52
|
Wang L, Xie X, Ke B, Huang W, Jiang X and
He G: Recent advances on endogenous gasotransmitters in
inflammatory dermatological disorders. J Adv Res. (In Press).
|
|
53
|
West JB: Joseph Priestley, oxygen, and the
enlightenment. Am J Physiol Lung Cell Mol Physiol. 306:L111–L119.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Gruetter CA, Barry BK, McNamara DB,
Gruetter DY, Kadowitz PJ and Ignarro L: Relaxation of bovine
coronary artery and activation of coronary arterial guanylate
cyclase by nitric oxide, nitroprusside and a carcinogenic
nitrosoamine. J Cyclic Nucleotide Res. 5:211–224. 1979.PubMed/NCBI
|
|
55
|
Furchgott RF and Zawadzki JV: The
obligatory role of endothelial cells in the relaxation of arterial
smooth muscle by acetylcholine. Nature. 288:373–376. 1980.
View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Ignarro LJ, Buga GM, Wood KS, Byrns RE and
Chaudhuri G: Endothelium-derived relaxing factor produced and
released from artery and vein is nitric oxide. Proc Natl Acad Sci
USA. 84:9265–9269. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Palmer RM, Ferrige AG and Moncada S:
Nitric oxide release accounts for the biological activity of
endothelium-derived relaxing factor. Nature. 327:524–526. 1987.
View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Moncada S, Palmer RM and Higgs EA: The
discovery of nitric oxide as the endogenous nitrovasodilator.
Hypertension. 12:365–372. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Murad F, Mittal CK, Arnold WP, Katsuki S
and Kimura H: Guanylate cyclase: Activation by azide, nitro
compounds, nitric oxide, and hydroxyl radical and inhibition by
hemoglobin and myoglobin. Adv Cyclic Nucleotide Res. 9:145–158.
1978.PubMed/NCBI
|
|
60
|
Koshland DE Jr: The molecule of the year.
Science. 258:18611992. View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Marsh N and Marsh A: A short history of
nitroglycerine and nitric oxide in pharmacology and physiology.
Clin Exp Pharmacol Physiol. 27:313–319. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Xu WM and Liu LZ: Nitric Oxide: Nitric
oxide: From a mysterious labile factor to the molecule of the Nobel
Prize. Recent progress in nitric oxide research. Cell Res.
8:251–258. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Yetik-Anacak G and Catravas JD: Nitric
oxide and the endothelium: History and impact on cardiovascular
disease. Vascul Pharmacol. 45:268–276. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Kennedy J: Account of the phænomena
produced by a large quantity of nitric oxide of quicksilver,
swallowed by mistake; and of the means employed to counteract its
deleterious influence. Med Chir J Rev. 1:189–196. 1816.PubMed/NCBI
|
|
65
|
Thomsen LL, Lawton FG, Knowles RG, Beesley
JE, Riveros-Moreno V and Moncada S: Nitric oxide synthase activity
in human gynecological cancer. Cancer Res. 54:1352–1354.
1994.PubMed/NCBI
|
|
66
|
Hidy GM, Mueller PK, Altshuler SL, Chow JC
and Watson JG: Air quality measurements-From rubber bands to
tapping the rainbow. J Air Waste Manag Assoc. 67:637–668. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Kinnicutt LP and Sanford GR: The
iodometric determination of small quantities of carbon monoxide.
Public Health Pap Rep. 25:600–604. 1899.PubMed/NCBI
|
|
68
|
Luden G: THE carbon monoxide menace and
the cancer problem. Can Med Assoc J. 17:43–48. 1927.PubMed/NCBI
|
|
69
|
Roughton FJW: The Kinetics of Haemoglobin
V-The Combination of Carbon Monoxide with Reduced Haemoglobin. Proc
R Soc London Series B, Containing Papers Biol Character.
115:464–473. 1934. View Article : Google Scholar
|
|
70
|
Roughton FJW and Darling RC: The effect of
carbon monoxide on the oxyhemoglobin dissociation curve. Am J
Physiol Legacy Content. 141:17–31. 1944. View Article : Google Scholar
|
|
71
|
Roughton FJ: The equilibrium between
carbon monoxide and sheep haemoglobin at very high percentage
saturations. J Physiol. 126:359–383. 1954. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Sjostrand T: Endogenous formation of
carbon monoxide in man. Nature. 164:5801949. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Tenhunen R, Marver HS and Schmid R:
Microsomal heme oxygenase. Characterization of the enzyme. J Biol
Chem. 244:6388–6394. 1969. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Zhao Y, Biggs TD and Xian M: Hydrogen
sulfide (H2S) releasing agents: Chemistry and biological
applications. Chem Commun (Camb). 50:11788–11805. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Tanner FW: Studies on the bacterial
metabolism of sulfur: I. Formation of hydrogen sulfide from certain
sulfur compounds under aerobic conditions. J Bacteriol. 2:585–593.
1917. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Rose P, Moore PK, Ming SH, Nam OC,
Armstrong JS and Whiteman M: Hydrogen sulfide protects colon cancer
cells from chemopreventative agent beta-phenylethyl isothiocyanate
induced apoptosis. World J Gastroenterol. 11:3990–3997. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Wang R: Signaling pathways for the
vascular effects of hydrogen sulfide. Curr Opin Nephrol Hypertens.
20:107–112. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Housein Z, Kareem TS and Salihi A: In
vitro anticancer activity of hydrogen sulfide and nitric oxide
alongside nickel nanoparticle and novel mutations in their genes in
CRC patients. Sci Rep. 11:25362021. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Shen Y, Shen Z, Luo S, Guo W and Zhu YZ:
The cardioprotective effects of hydrogen sulfide in heart diseases:
From molecular mechanisms to therapeutic potential. Oxid Med Cell
Longev. 2015:9251672015. View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Coleman JW: Nitric oxide in immunity and
inflammation. Int Immunopharmacol. 1:1397–1406. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Esplugues JV: NO as a signalling molecule
in the nervous system. Br J Pharmacol. 135:1079–1095. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Sen S, Jensen K, Brennan K, Ramadoss S and
Chaudhuri G: Chapter 10-Chemoprotective and chemosensitizing
effects of nitric oxide and other biologically active gases in
breast cancer chemotherapy: Potential implications. Nitric Oxide
(Donor/Induced) in Chemosensitizing. Bonavida B: Academic Press;
pp. 169–178. 2017, View Article : Google Scholar
|
|
83
|
Choudhari SK, Chaudhary M, Bagde S,
Gadbail AR and Joshi V: Nitric oxide and cancer: A review. World J
Surg Oncol. 11:1182013. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Burke AJ, Sullivan FJ, Giles FJ and Glynn
SA: The yin and yang of nitric oxide in cancer progression.
Carcinogenesis. 34:503–512. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Ying L and Hofseth LJ: An Emerging role
for endothelial nitric oxide synthase in chronic inflammation and
cancer. Cancer Res. 67:1407–1410. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Tennyson Andrew G and Lippard Stephen J:
Generation, translocation, and action of nitric oxide in living
systems. Chem Biol. 18:1211–1220. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Grisham MB, Jourd'Heuil D and Wink DA:
Nitric oxide. I. Physiological chemistry of nitric oxide and its
metabolites: Implications in inflammation. Am J Physiol.
276:G315–G321. 1999.PubMed/NCBI
|
|
88
|
Subapriya R, Kumaraguruparan R,
Ramachandran CR and Nagini S: Oxidant-antioxidant status in
patients with oral squamous cell carcinomas at different intraoral
sites. Clin Biochem. 35:489–493. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Cheng H, Wang L, Mollica M, Re AT, Wu S
and Zuo L: Nitric oxide in cancer metastasis. Cancer Lett. 353:1–7.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Frérart F, Sonveaux P, Rath G, Smoos A,
Meqor A, Charlier N, Jordan BF, Saliez J, Noël A, Dessy C, et al:
The acidic tumor microenvironment promotes the reconversion of
nitrite into nitric oxide: Towards a new and safe radiosensitizing
strategy. Clin Cancer Res. 14:2768–2774. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Tanese K, Grimm EA and Ekmekcioglu S: The
role of melanoma tumor-derived nitric oxide in the tumor
inflammatory microenvironment: Its impact on the chemokine
expression profile, including suppression of CXCL10. Int J Cancer.
131:891–901. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Decker NK, Abdelmoneim SS, Yaqoob U,
Hendrickson H, Hormes J, Bentley M, Pitot H, Urrutia R, Gores GJ
and Shah VH: Nitric oxide regulates tumor cell cross-talk with
stromal cells in the tumor microenvironment of the liver. Am J
Pathol. 173:1002–1012. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
93
|
PeNarando J, Aranda E and RodrIguez-Ariza
A: Immunomodulatory roles of nitric oxide in cancer: Tumor
microenvironment says ‘NO’ to antitumor immune response. Transl
Res. 210:99–108. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Arora H, Panara K, Kuchakulla M,
Kulandavelu S, Burnstein KL, Schally AV, Hare JM and Ramasamy R:
Alterations of tumor microenvironment by nitric oxide impedes
castration-resistant prostate cancer growth. Proc Natl Acad Sci
USA. 115:11298–11303. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Yang G: Hydrogen sulfide in cell survival:
A double-edged sword. Exp Rev Clin Pharmacol. 4:33–47. 2011.
View Article : Google Scholar
|
|
96
|
Pei Y, Wu B, Cao Q, Wu L and Yang G:
Hydrogen sulfide mediates the anti-survival effect of sulforaphane
on human prostate cancer cells. Toxicol Appl Pharmacol.
257:420–428. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Bhattacharyya S, Saha S, Giri K, Lanza IR,
Nair KS, Jennings NB, Rodriguez-Aguayo C, Lopez-Berestein G, Basal
E, Weaver AL, et al: Cystathionine beta-synthase (CBS) contributes
to advanced ovarian cancer progression and drug resistance. PLoS
One. 8:e791672013. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Hellmich MR, Coletta C, Chao C and Szabo
C: The therapeutic potential of cystathionine β-synthetase/hydrogen
sulfide inhibition in cancer. Antioxid Redox Signal. 22:424–448.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Zhu H, Blake S, Chan KT, Pearson RB and
Kang J: Cystathionine β-synthase in physiology and cancer. Biomed
Res Int. 2018:32051252018. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Hellmich MR and Szabo C: Hydrogen sulfide
and cancer. Chemistry, Biochemistry and Pharmacology of Hydrogen
Sulfide. Springer; New York, NY: pp. 233–241. 2015, View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Sen N: Functional and molecular insights
of hydrogen sulfide signaling and protein sulfhydration. J Mol
Biol. 429:543–561. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Chattopadhyay M, Kodela R, Nath N,
Dastagirzada YM, Velázquez-Martínez CA, Boring D and Kashfi K:
Hydrogen sulfide-releasing NSAIDs inhibit the growth of human
cancer cells: A general property and evidence of a tissue
type-independent effect. Biochem Pharmacol. 83:715–722. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Szabo C, Ransy C, Módis K, Andriamihaja M,
Murghes B, Coletta C, Olah G, Yanagi K and Bouillaud F: Regulation
of mitochondrial bioenergetic function by hydrogen sulfide. Part I.
Biochemical and physiological mechanisms. Br J Pharmacol.
171:2099–2122. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
Rose P, Moore PK and Zhu YZ:
H2S biosynthesis and catabolism: New insights from
molecular studies. Cell Mol Life Sci. 74:1391–1412. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Cao X, Ding L, Xie ZZ, Yang Y, Whiteman M,
Moore PK and Bian JS: A review of hydrogen sulfide synthesis,
metabolism, and measurement: Is modulation of hydrogen sulfide a
novel therapeutic for cancer? Antioxid Redox Signal. 31:1–38. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Giuffrè A, Tomé CS, Fernandes DGF, Zuhra K
and Vicente JB: Hydrogen sulfide metabolism and signaling in the
tumor microenvironment. Adv Exp Med Biol. 1219:335–353. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
107
|
Wang RH, Chu YH and Lin KT: The hidden
role of hydrogen sulfide metabolism in cancer. Int J Mol Sci.
22:65622021. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Watnick RS: The role of the tumor
microenvironment in regulating angiogenesis. Cold Spring Harb
Perspect Med. 2:a0066762012. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Zhou Y, Li XH, Zhang CC, Wang MJ, Xue WL,
Wu DD, Ma FF, Li WW, Tao BB and Zhu YC: Hydrogen sulfide promotes
angiogenesis by downregulating miR-640 via the VEGFR2/mTOR pathway.
Am J Physiol Cell Physiol. 310:C305–C317. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Wang M, Yan J, Cao X, Hua P and Li Z:
Hydrogen sulfide modulates epithelial-mesenchymal transition and
angiogenesis in non-small cell lung cancer via HIF-1α activation.
Biochem Pharmacol. 172:1137752020. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Szabo C and Hellmich MR: Endogenously
produced hydrogen sulfide supports tumor cell growth and
proliferation. Cell Cycle. 12:2915–2916. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Holwerda KM, Burke SD, Faas MM, Zsengeller
Z, Stillman IE, Kang PM, van Goor H, McCurley A, Jaffe IZ,
Karumanchi SA and Lely AT: Hydrogen sulfide attenuates
sFlt1-Induced hypertension and renal damage by upregulating
vascular endothelial growth factor. J Am Soc Nephrol. 25:717–725.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Szabo C, Coletta C, Chao C, Módis K,
Szczesny B, Papapetropoulos A and Hellmich MR: Tumor-derived
hydrogen sulfide, produced by cystathionine-β-synthase, stimulates
bioenergetics, cell proliferation, and angiogenesis in colon
cancer. Proc Natl Acad Sci USA. 110:12474–12479. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Liu D, Liu M, Wan Y, Zhou X, Yang S, An L,
Huang G and Tian Q: Remodeling endogenous H2S
microenvironment in colon cancer to enhance chemodynamic therapy.
Chem Engineering J. 422:1300982021. View Article : Google Scholar
|
|
115
|
Wan M, Liu Z, Li T, Chen H, Wang Q, Chen
T, Tao Y and Mao C: Zwitterion-Based hydrogen sulfide nanomotors
induce multiple acidosis in tumor cells by destroying tumor
metabolic symbiosis. Angew Chem Int Ed Engl. 60:16139–16148. 2021.
View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Li D, Xiong Q, Peng J, Hu B, Li W, Zhu Y
and Shen X: Hydrogen Sulfide Up-Regulates the expression of
ATP-Binding cassette transporter A1 via promoting nuclear
translocation of PPARα. Int J Mol Sci. 17:6352016. View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Schulze A and Harris AL: How cancer
metabolism is tuned for proliferation and vulnerable to disruption.
Nature. 491:3642012. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Lee ZW, Teo XY, Tay EY, Tan CH, Hagen T,
Moore PK and Deng LW: Utilizing hydrogen sulfide as a novel
anti-cancer agent by targeting cancer glycolysis and pH imbalance.
Br J Pharmacol. 171:4322–4336. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Niland S, Riscanevo AX and Eble JA: Matrix
metalloproteinases shape the tumor microenvironment in cancer
progression. Int J Mol Sci. 23:1462021. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Harjunpää H, Llort Asens M, Guenther C and
Fagerholm SC: Cell adhesion molecules and their roles and
regulation in the immune and tumor microenvironment. Front Immunol.
10:10782019. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Mao Y, Keller ET, Garfield DH, Shen K and
Wang J: Stromal cells in tumor microenvironment and breast cancer.
Cancer Metastasis Rev. 32:303–315. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Zhen Y, Pan W, Hu F, Wu H, Feng J, Zhang Y
and Chen J: Exogenous hydrogen sulfide exerts
proliferation/anti-apoptosis/angiogenesis/migration effects via
amplifying the activation of NF-κB pathway in PLC/PRF/5 hepatoma
cells. Int J Oncol. 46:2194–2204. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Li H, Xu F, Gao G, Gao X, Wu B, Zheng C,
Wang P, Li Z, Hua H and Li D: Hydrogen sulfide and its donors:
Novel antitumor and antimetastatic therapies for triple-negative
breast cancer. Redox Biol. 34:1015642020. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Wu D, Li M, Tian W, Wang S, Cui L, Li H,
Wang H, Ji A and Li Y: Hydrogen sulfide acts as a double-edged
sword in human hepatocellular carcinoma cells through
EGFR/ERK/MMP-2 and PTEN/AKT signaling pathways. Sci Rep.
7:51342017. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Wu D, Li J, Zhang Q, Tian W, Zhong P, Liu
Z, Wang H, Wang H, Ji A and Li Y: Exogenous hydrogen sulfide
regulates the growth of human thyroid carcinoma cells. Oxid Med
Cell Longev. 2019:69272982019. View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Zhang L, Qi Q, Yang J, Sun D, Li C, Xue Y,
Jiang Q, Tian Y, Xu C and Wang R: An anticancer role of hydrogen
sulfide in human gastric cancer cells. Oxid Med Cell Longev.
2015:6364102015. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Rose JJ, Wang L, Xu Q, McTiernan CF, Shiva
S, Tejero J and Gladwin MT: Carbon monoxide poisoning:
Pathogenesis, management, and future directions of therapy. Am J
Respir Crit Care Med. 195:596–606. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Motterlini R and Otterbein LE: The
therapeutic potential of carbon monoxide. Nat Rev Drug Discov.
9:728–743. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Wegiel B, Nemeth Z, Correa-Costa M, Bulmer
AC and Otterbein LE: Heme Oxygenase-1: A Metabolic Nike. Antioxid
Redox Signal. 20:1709–1722. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Ismailova A, Kuter D, Bohle DS and Butler
IS: An overview of the potential therapeutic applications of
CO-Releasing molecules. Bioinorg Chem Appl. 2018:85473642018.
View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Ji X, Damera K, Zheng Y, Yu B, Otterbein
LE and Wang B: Toward carbon monoxide-based therapeutics: Critical
drug delivery and developability issues. J Pharm Sci. 105:406–416.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
McCoubrey WK Jr, Huang T and Maines MD:
Isolation and characterization of a cDNA from the rat brain that
encodes hemoprotein heme oxygenase-3. Eur J Biochem. 247:725–732.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Otterbein LE, Soares MP, Yamashita K and
Bach FH: Heme oxygenase-1: Unleashing the protective properties of
heme. Trends Immunol. 24:449–455. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Ryter SW, Alam J and Choi AMK: Heme
Oxygenase-1/Carbon monoxide: From basic science to therapeutic
applications. Physiol Rev. 86:583–650. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Chen S, Wang X, Nisar MF, Lin M and Zhong
JL: Heme Oxygenases: Cellular multifunctional and protective
molecules against UV–Induced oxidative stress. Oxid Med Cell
Longev. 2019:54167282019. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Goebel U and Wollborn J: Carbon monoxide
in intensive care medicine-time to start the therapeutic
application? Intensive Care Med Exp. 8:22020. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Zuckerbraun BS, Chin BY, Bilban M, d'Avila
JC, Rao J, Billiar TR and Otterbein LE: Carbon monoxide signals via
inhibition of cytochrome c oxidase and generation of mitochondrial
reactive oxygen species. FASEB J. 21:1099–1106. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Chin BY, Jiang G, Wegiel B, Wang HJ,
Macdonald T, Zhang XC, Gallo D, Cszimadia E, Bach FH, Lee PJ and
Otterbein LE: Hypoxia-inducible factor 1alpha stabilization by
carbon monoxide results in cytoprotective preconditioning. Proc
Natl Acad Sci USA. 104:5109–5114. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Hanahan D and Weinberg RA: Hallmarks of
cancer: The next generation. Cell. 144:646–674. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Shefa U, Yeo SG, Kim MS, Song IO, Jung J,
Jeong NY and Huh Y: Role of gasotransmitters in oxidative stresses,
neuroinflammation, and neuronal repair. Biomed Res.
2017:16893412017.PubMed/NCBI
|
|
141
|
Yang C, Jeong S, Ku S, Lee K and Park MH:
Use of gasotransmitters for the controlled release of polymer-based
nitric oxide carriers in medical applications. J Control Release.
279:157–170. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Hassan AY, Maulood IM and Salihi A: The
vasodilatory mechanism of nitric oxide and hydrogen sulfide in the
human mesenteric artery in patients with colorectal cancer. Exp
Ther Med. 21:2142021. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Konovalova NP, Goncharova SA, Volkova LM,
Rajewskaya TA, Eremenko LT and Korolev AM: Nitric oxide donor
increases the efficiency of cytostatic therapy and retards the
development of drug resistance. Nitric Oxide. 8:59–64. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Weyerbrock A, Baumer B and Papazoglou A:
Growth inhibition and chemosensitization of exogenous nitric oxide
released from NONOates in glioma cells in vitro. J Neurosurg.
110:128–136. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
145
|
Wink DA, Cook JA, Christodoulou D, Krishna
MC, Pacelli R, Kim S, DeGraff W, Gamson J, Vodovotz Y, Russo A and
Mitchell JB: Nitric oxide and some nitric oxide donor compounds
enhance the cytotoxicity of cisplatin. Nitric Oxide. 1:88–94. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
146
|
Huerta-Yepez S, Vega M, Escoto-Chavez SE,
Murdock B, Sakai T, Baritaki S and Bonavida B: Nitric oxide
sensitizes tumor cells to TRAIL-induced apoptosis via inhibition of
the DR5 transcription repressor Yin Yang 1. Nitric Oxide. 20:39–52.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
147
|
Huerta S, Baay-Guzman G, Gonzalez-Bonilla
CR, Livingston EH, Huerta-Yepez S and Bonavida B: In vitro and in
vivo sensitization of SW620 metastatic colon cancer cells to
CDDP-induced apoptosis by the nitric oxide donor DETANONOate:
Involvement of AIF. Nitric Oxide. 20:182–194. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
148
|
Bratasz A, Selvendiran K, Wasowicz T,
Bobko A, Khramtsov VV, Ignarro LJ and Kuppusamy P: NCX-4040, a
nitric oxide-releasing aspirin, sensitizes drug-resistant human
ovarian xenograft tumors to cisplatin by depletion of cellular
thiols. J Transl Med. 6:92008. View Article : Google Scholar : PubMed/NCBI
|
|
149
|
Safdar S, Payne CA, Tu NH and Taite LJ:
Targeted nitric oxide delivery preferentially induces glioma cell
chemosensitivity via altered p53 and O(6)-methylguanine-DNA
methyltransferase activity. Biotechnol Bioengering. 110:1211–1220.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
150
|
Shami PJ, Saavedra JE, Wang LY, Bonifant
CL, Diwan BA, Singh SV, Gu Y, Fox SD, Buzard GS and Citro ML: JS-K,
a glutathione/glutathione S-transferase-activated nitric oxide
donor of the diazeniumdiolate class with potent antineoplastic
activity. Mol Cancer Ther. 2:409–417. 2003.PubMed/NCBI
|
|
151
|
Qiu M, Ke L, Zhang S, Zeng X, Fang Z and
Liu J: JS-K, a GST-activated nitric oxide donor prodrug, enhances
chemo-sensitivity in renal carcinoma cells and prevents cardiac
myocytes toxicity induced by Doxorubicin. Cancer Chemother
Pharmacol. 80:275–286. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
152
|
Laschak M, Spindler KD, Schrader AJ,
Hessenauer A, Streicher W, Schrader M and Cronauer MV: JS-K, a
glutathione/glutathione S-transferase-activated nitric oxide
releasing prodrug inhibits androgen receptor and WNT-signaling in
prostate cancer cells. BMC Cancer. 12:1302012. View Article : Google Scholar : PubMed/NCBI
|
|
153
|
Qiu M, Chen L, Tan G, Ke L, Zhang S, Chen
H and Liu J: A reactive oxygen species activation mechanism
contributes to JS-K-induced apoptosis in human bladder cancer
cells. Sci Rep. 5:151042015. View Article : Google Scholar : PubMed/NCBI
|
|
154
|
Riganti C, Doublier S, Costamagna C,
Aldieri E, Pescarmona G, Ghigo D and Bosia A: Activation of nuclear
factor-kappa B pathway by simvastatin and RhoA silencing increases
doxorubicin cytotoxicity in human colon cancer HT29 cells. Mol
Pharmacol. 74:476–484. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
155
|
De Boo S, Kopecka J, Brusa D, Gazzano E,
Matera L, Ghigo D, Bosia A and Riganti C: iNOS activity is
necessary for the cytotoxic and immunogenic effects of doxorubicin
in human colon cancer cells. Mol Cancer. 8:1082009. View Article : Google Scholar : PubMed/NCBI
|
|
156
|
Alimoradi H, Greish K, Barzegar-Fallah A,
Alshaibani L and Pittalà V: Nitric oxide-releasing nanoparticles
improve doxorubicin anticancer activity. Int J Nanomedicine.
13:7771–7787. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
157
|
Sung YC, Jin PR, Chu LA, Hsu FF, Wang MR,
Chang CC, Chiou SJ, Qiu JT, Gao DY, Lin CC, et al: Delivery of
nitric oxide with a nanocarrier promotes tumour vessel
normalization and potentiates anti-cancer therapies. Nat
Nanotechnol. 14:1160–1169. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
158
|
Pieretti JC, Pelegrino MT, Nascimento MHM,
Tortella GR, Rubilar O and Seabra AB: Small molecules for great
solutions: Can nitric oxide-releasing nanomaterials overcome drug
resistance in chemotherapy? Biochem Pharmacol. 176:1137402020.
View Article : Google Scholar : PubMed/NCBI
|
|
159
|
Yasuda H, Nakayama K, Watanabe M, Suzuki
S, Fuji H, Okinaga S, Kanda A, Zayasu K, Sasaki T, Asada M, et al:
Nitroglycerin treatment may enhance chemosensitivity to docetaxel
and carboplatin in patients with lung adenocarcinoma. Clin Cancer
Res. 12:6748–6757. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
160
|
Aalaei S, Mohammadzadeh M and Pazhang Y:
Synergistic induction of apoptosis in a cell model of human
leukemia K562 by nitroglycerine and valproic acid. EXCLI J.
18:619–630. 2019.PubMed/NCBI
|
|
161
|
Kaoud TS, Mohassab AM, Hassan HA, Yan C,
Van Ravenstein SX, Abdelhamid D, Dalby KN and Abdel-Aziz M:
NO-releasing STAT3 inhibitors suppress BRAF-mutant melanoma growth.
Eur J Med Chem. 186:1118852020. View Article : Google Scholar : PubMed/NCBI
|
|
162
|
Ishima Y, Kragh-Hansen U, Maruyama T and
Otagiri M: Poly-s-nitrosated albumin as a safe and effective
multifunctional antitumor agent: Characterization, biochemistry and
possible future therapeutic applications. Biomed Res Int.
2013:3538922013. View Article : Google Scholar : PubMed/NCBI
|
|
163
|
Ishima Y, Inoue A, Fang J, Kinoshita R,
Ikeda M, Watanabe H, Maeda H, Otagiri M and Maruyama T:
Poly-S-nitrosated human albumin enhances the antitumor and
antimetastasis effect of bevacizumab, partly by inhibiting
autophagy through the generation of nitric oxide. Cancer Sci.
106:194–200. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
164
|
Li L, Whiteman M, Guan YY, Neo KL, Cheng
Y, Lee SW, Zhao Y, Baskar R, Tan CH and Moore PK: Characterization
of a novel, water-soluble hydrogen sulfide-releasing molecule
(GYY4137): New insights into the biology of hydrogen sulfide.
Circulation. 117:2351–2360. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
165
|
Lee ZW, Zhou J, Chen CS, Zhao Y, Tan CH,
Li L, Moore PK and Deng LW: The slow-releasing hydrogen sulfide
donor, GYY4137, exhibits novel anti-cancer effects in vitro and in
vivo. PLoS One. 6:e210772011. View Article : Google Scholar : PubMed/NCBI
|
|
166
|
Nalli AD, Bhattacharya S, Wang H, Kendig
DM, Grider JR and Murthy KS: Augmentation of cGMP/PKG pathway and
colonic motility by hydrogen sulfide. Am J Physiol Gastrointest
Liver Physiol. 313:G330–G341. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
167
|
Liu B, Huang X, Li Y, Liao W, Li M, Liu Y,
He R, Feng D, Zhu R and Kurihara H: JS-K, a nitric oxide donor,
induces autophagy as a complementary mechanism inhibiting ovarian
cancer. BMC Cancer. 19:6452019. View Article : Google Scholar : PubMed/NCBI
|
|
168
|
Fonseca MD, Cunha FQ, Kashfi K and Cunha
TM: NOSH-aspirin (NBS-1120), a dual nitric oxide and hydrogen
sulfide-releasing hybrid, reduces inflammatory pain. Pharmacol Res
Perspect. 3:e001332015. View Article : Google Scholar : PubMed/NCBI
|
|
169
|
Rose P, Dymock BW and Moore PK: GYY4137, a
novel water-soluble, H2S-releasing molecule. Methods Enzymol.
554:143–167. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
170
|
Aaltoma SH, Lipponen PK and Kosma VM:
Inducible nitric oxide synthase (iNOS) expression and its
prognostic value in prostate cancer. Anticancer Res. 21:3101–3106.
2001.PubMed/NCBI
|
|
171
|
Aaltomaa SH, Lipponen PK, Viitanen J,
Kankkunen JP, Ala-Opas MY and Kosma VM: The prognostic value of
inducible nitric oxide synthase in local prostate cancer. BJU Int.
86:234–239. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
172
|
Bhowmick R and Girotti AW: Pro-survival
and pro-growth effects of stress-induced nitric oxide in a prostate
cancer photodynamic therapy model. Cancer Lett. 343:115–122. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
173
|
Coulter JA, Page NL, Worthington J, Robson
T, Hirst DG and McCarthy HO: Transcriptional regulation of
inducible nitric oxide synthase gene therapy: Targeting early stage
and advanced prostate cancer. J Gene Med. 12:755–765. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
174
|
Cronauer MV, Ince Y, Engers R, Rinnab L,
Weidemann W, Suschek CV, Burchardt M, Kleinert H, Wiedenmann J,
Sies H, et al: Nitric oxide-mediated inhibition of androgen
receptor activity: Possible implications for prostate cancer
progression. Oncogene. 26:1875–1884. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
175
|
Erlandsson A, Carlsson J, Andersson SO,
Vyas C, Wikström P, Andrén O, Davidsson S and Rider JR: High
inducible nitric oxide synthase in prostate tumor epithelium is
associated with lethal prostate cancer. Scand J Urol. 52:129–133.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
176
|
McCarthy HO, Coulter JA, Worthington J,
Robson T and Hirst DG: Human osteocalcin: A strong promoter for
nitric oxide synthase gene therapy, with specificity for hormone
refractory prostate cancer. J Gene Med. 9:511–520. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
177
|
Fahey JM and Girotti AW: Accelerated
migration and invasion of prostate cancer cells after a
photodynamic therapy-like challenge: Role of nitric oxide. Nitric
Oxide. 49:47–55. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
178
|
D'Este F, Della Pietra E, Badillo Pazmay
GV, Xodo LE and Rapozzi V: Role of nitric oxide in the response to
photooxidative stress in prostate cancer cells. Biochem Pharmacol.
182:1142052020. View Article : Google Scholar : PubMed/NCBI
|
|
179
|
Ryk C, de Verdier P, Montgomery E, Peter
Wiklund N, Wiklund F and Gronberg H: Polymorphisms in the
nitric-oxide synthase 2 gene and prostate cancer pathogenesis.
Redox Biol. 5:4192015. View Article : Google Scholar : PubMed/NCBI
|
|
180
|
Uotila P, Valve E, Martikainen P,
Nevalainen M, Nurmi M and Harkonen P: Increased expression of
cyclooxygenase-2 and nitric oxide synthase-2 in human prostate
cancer. Urol Res. 29:23–28. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
181
|
Abdelmagid SA, Rickard JA, McDonald WJ,
Thomas LN and Too CK: CAT-1-mediated arginine uptake and regulation
of nitric oxide synthases for the survival of human breast cancer
cell lines. J Cell Biochem. 112:1084–1092. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
182
|
Abdelmagid SA and Too CK: Prolactin and
estrogen up-regulate carboxypeptidase-d to promote nitric oxide
production and survival of mcf-7 breast cancer cells.
Endocrinology. 149:4821–4828. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
183
|
Ambs S and Glynn SA: Candidate pathways
linking inducible nitric oxide synthase to a basal-like
transcription pattern and tumor progression in human breast cancer.
Cell Cycle. 10:619–624. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
184
|
Alalami O and Martin JH: ZR-75-1 human
breast cancer cells: Expression of inducible nitric oxide synthase
and effect of tamoxifen and phorbol ester on nitric oxide
production. Cancer Lett. 123:99–105. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
185
|
Basudhar D, Somasundaram V, de Oliveira
GA, Kesarwala A, Heinecke JL, Cheng RY, Glynn SA, Ambs S, Wink DA
and Ridnour LA: Nitric oxide synthase-2-derived nitric oxide drives
multiple pathways of breast cancer progression. Antioxid Redox
Signal. 26:1044–1058. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
186
|
Bentrari F, Arnould L, Jackson AP, Jeannin
JF and Pance A: Progesterone enhances cytokine-stimulated nitric
oxide synthase II expression and cell death in human breast cancer
cells. Lab Invest. 85:624–632. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
187
|
Bing RJ, Miyataka M, Rich KA, Hanson N,
Wang X, Slosser HD and Shi SR: Nitric oxide, prostanoids,
cyclooxygenase, and angiogenesis in colon and breast cancer. Clin
Cancer Res. 7:3385–3392. 2001.PubMed/NCBI
|
|
188
|
Deepa M, Sureshkumar T, Satheeshkumar PK
and Priya S: Antioxidant rich Morus alba leaf extract induces
apoptosis in human colon and breast cancer cells by the
downregulation of nitric oxide produced by inducible nitric oxide
synthase. Nutr Cancer. 65:305–310. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
189
|
Duenas-Gonzalez A, Isales CM, del Mar
Abad-Hernandez M, Gonzalez-Sarmiento R, Sangueza O and
Rodriguez-Commes J: Expression of inducible nitric oxide synthase
in breast cancer correlates with metastatic disease. Mod Pathol.
10:645–649. 1997.PubMed/NCBI
|
|
190
|
Evig CB, Kelley EE, Weydert CJ, Chu Y,
Buettner GR and Burns CP: Endogenous production and exogenous
exposure to nitric oxide augment doxorubicin cytotoxicity for
breast cancer cells but not cardiac myoblasts. Nitric Oxide.
10:119–129. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
191
|
Flaherty RL, Intabli H, Falcinelli M,
Bucca G, Hesketh A, Patel BA, Allen MC, Smith CP and Flint MS:
Stress hormone-mediated acceleration of breast cancer metastasis is
halted by inhibition of nitric oxide synthase. Cancer letters.
459:59–71. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
192
|
Garrido P, Shalaby A, Walsh EM, Keane N,
Webber M, Keane MM, Sullivan FJ, Kerin MJ, Callagy G, Ryan AE and
Glynn SA: Impact of inducible nitric oxide synthase (iNOS)
expression on triple negative breast cancer outcome and activation
of EGFR and ERK signaling pathways. Oncotarget. 8:80568–80588.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
193
|
Hsu JT, Ying C and Chen CJ: Regulation of
inducible nitric oxide synthase by dietary phytoestrogen in MCF-7
human mammary cancer cells. Reprod Nutr Dev. 40:11–18. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
194
|
Kanugula AK, Gollavilli PN, Vasamsetti SB,
Karnewar S, Gopoju R, Ummanni R and Kotamraju S: Statin-induced
inhibition of breast cancer proliferation and invasion involves
attenuation of iron transport: Intermediacy of nitric oxide and
antioxidant defence mechanisms. FEBS J. 281:3719–3738. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
195
|
Kotamraju S, Williams CL and Kalyanaraman
B: Statin-induced breast cancer cell death: Role of inducible
nitric oxide and arginase-dependent pathways. Cancer Res.
67:7386–7394. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
196
|
López-Sánchez LM, Mena R, Guil-Luna S,
Mantrana A, Peñarando J, Toledano-Fonseca M, Conde F, De la
Haba-Rodríguez JR, Aranda E and Rodríguez-Ariza A: Nitric
oxide-targeted therapy inhibits stemness and increases the efficacy
of tamoxifen in estrogen receptor-positive breast cancer cells. Lab
Invest. 101:292–303. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
197
|
Loibl S, Buck A, Strank C, von Minckwitz
G, Roller M, Sinn HP, Schini-Kerth V, Solbach C, Strebhardt K and
Kaufmann M: The role of early expression of inducible nitric oxide
synthase in human breast cancer. Eur J Cancer. 41:265–271. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
198
|
Lahiri M and Martin JH: Reduced expression
of endothelial and inducible nitric oxide synthase in a multidrug
resistant variant of the MCF-7 human breast cancer cell line. Oncol
Rep. 12:1007–1011. 2004.PubMed/NCBI
|
|
199
|
Oktem G, Karabulut B, Selvi N, Sezgin C,
Sanli UA, Uslu R, Yurtseven ME and Omay SB: Differential effects of
doxorubicin and docetaxel on nitric oxide production and inducible
nitric oxide synthase expression in MCF-7 human breast cancer
cells. Oncol Res. 14:381–386. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
200
|
Martin JH, Alalami O and van den Berg HW:
Reduced expression of endothelial and inducible nitric oxide
synthase in a human breast cancer cell line which has acquired
estrogen independence. Cancer Lett. 144:65–74. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
201
|
Nafea H, Youness RA, Abou-Aisha K and Gad
MZ: LncRNA HEIH/miR-939-5p interplay modulates triple-negative
breast cancer progression through NOS2-induced nitric oxide
production. J Cell Physiol. 236:5362–5372. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
202
|
Oktem G, Bilir A, Selvi N, Yurtseven ME,
Vatansever S, Ates U, Uysal A and Omay SB: Chemotherapy influences
inducible nitric oxide synthase (iNOS) and endothelial nitric oxide
synthase (eNOS) activity on 3D breast cancer cell line. Oncol Res.
16:195–203. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
203
|
Zeybek ND, Inan S, Ekerbicer N, Vatansever
HS, Karakaya J and Muftuoglu SF: The effects of Gemcitabine and
Vinorelbine on inducible nitric oxide synthase (iNOS) and
endothelial nitric oxide synthase (eNOS) distribution of MCF-7
breast cancer cells. Acta Histochem. 113:62–67. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
204
|
Walsh EM, Keane MM, Wink DA, Callagy G and
Glynn SA: Review of triple negative breast cancer and the impact of
inducible nitric oxide synthase on tumor biology and patient
outcomes. Crit Rev Oncog. 21:333–351. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
205
|
Wink DA, Ridnour LA, Cheng R, Switzer CW,
Glynn S and Ambs S: The oncogenic properties of the redox
inflammatory protein inducible nitric oxide synthase in ER(−)
breast cancer. Redox Biol. 5:4132015. View Article : Google Scholar : PubMed/NCBI
|
|
206
|
Tschugguel W, Schneeberger C, Unfried G,
Czerwenka K, Weninger W, Mildner M, Gruber DM, Sator MO, Waldhör T
and Huber JC: Expression of inducible nitric oxide synthase in
human breast cancer depends on tumor grade. Breast Cancer Res
Treat. 56:145–151. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
207
|
Abadi AT and Kusters JG: Association of
inducible nitric oxide synthetase genotype and Helicobacter pylori
infection gastric cancer risk may be due to faulty primer design.
World J Gastroenterol. 19:429–430. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
208
|
Chen CN, Hsieh FJ, Cheng YM, Chang KJ and
Lee PH: Expression of inducible nitric oxide synthase and
cyclooxygenase-2 in angiogenesis and clinical outcome of human
gastric cancer. J Surg Oncol. 94:226–233. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
209
|
Doi C, Noguchi Y, Marat D, Saito A,
Fukuzawa K, Yoshikawa T, Tsuburaya A and Ito T: Expression of
nitric oxide synthase in gastric cancer. Cancer Lett. 144:161–167.
1999. View Article : Google Scholar : PubMed/NCBI
|
|
210
|
Goto T, Haruma K, Kitadai Y, Ito M,
Yoshihara M, Sumii K, Hayakawa N and Kajiyama G: Enhanced
expression of inducible nitric oxide synthase and nitrotyrosine in
gastric mucosa of gastric cancer patients. Clin Cancer Res.
5:1411–1415. 1999.PubMed/NCBI
|
|
211
|
Goto Y, Ando T, Naito M, Goto H and
Hamajima N: Inducible nitric oxide synthase polymorphism is
associated with the increased risk of differentiated gastric cancer
in a Japanese population. World J Gastroenterol. 12:6361–6365.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
212
|
Hirst D and Robson T: Nitric oxide in
cancer therapeutics: Interaction with cytotoxic chemotherapy. Curr
Pharm Des. 16:411–420. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
213
|
Hirahashi M, Koga Y, Kumagai R, Aishima S,
Taguchi K and Oda Y: Induced nitric oxide synthetase and
peroxiredoxin expression in intramucosal poorly differentiated
gastric cancer of young patients. Pathol Int. 64:155–163. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
214
|
Huang FY, Chan AO, Rashid A, Wong DK, Cho
CH and Yuen MF: Helicobacter pylori induces promoter methylation of
E-cadherin via interleukin-1β activation of nitric oxide production
in gastric cancer cells. Cancer. 118:4969–4980. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
215
|
Ikeguchi M, Ueta T and Kaibara N:
Expression of inducible nitric oxide synthase during
cisplatin-based chemotherapy for gastric cancer. In Vivo.
16:185–190. 2002.PubMed/NCBI
|
|
216
|
Jun Y, Fei G, Ebert MP and Malfertheiner
P: Expression of inducible nitric oxide synthase in human gastric
cancer. World J Gastroenterol. 5:430–431. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
217
|
Jung ID, Lee JS, Yun SY, Park CG, Han JW,
Lee HW and Lee HY: Doxorubicin inhibits the production of nitric
oxide by colorectal cancer cells. Arch Pharm Res. 25:691–696. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
218
|
Rafiei A, Hosseini V, Janbabai G, Fazli B,
Ajami A, Hosseini-Khah Z, Gilbreath J and Merrell DS: Inducible
nitric oxide synthetase genotype and helicobacter pylori infection
affect gastric cancer risk. World J Gastroenterol. 18:4917–4924.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
219
|
Rajnakova A, Moochhala S, Goh PM and Ngoi
S: Expression of nitric oxide synthase, cyclooxygenase, and p53 in
different stages of human gastric cancer. Cancer Lett. 172:177–185.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
220
|
Zhang W, He XJ, Ma YY, Wang HJ, Xia YJ,
Zhao ZS, Ye ZY and Tao HQ: Inducible nitric oxide synthase
expression correlates with angiogenesis, lymphangiogenesis, and
poor prognosis in gastric cancer patients. Hum Pathol.
42:1275–1282. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
221
|
Sawa T, Mounawar M, Tatemichi M, Gilibert
I, Katoh T and Ohshima H: Increased risk of gastric cancer in
Japanese subjects is associated with microsatellite polymorphisms
in the heme oxygenase-1 and the inducible nitric oxide synthase
gene promoters. Cancer Lett. 269:78–84. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
222
|
Shen J, Wang RT, Wang LW, Xu YC and Wang
XR: A novel genetic polymorphism of inducible nitric oxide synthase
is associated with an increased risk of gastric cancer. World J
Gastroenterol. 10:3278–3283. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
223
|
Son HJ, Kim YH, Park DI, Kim JJ, Rhee PL,
Paik SW, Choi KW, Song SY and Rhee JC: Interaction between
cyclooxygenase-2 and inducible nitric oxide synthase in gastric
cancer. J Clin Gastroenterol. 33:383–388. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
224
|
Song ZY, Wen SQ, Peng JP, Huang X and Qian
KD: Significance of vascular endothelial growth factor expression
and its correlation with inducible nitric oxide synthase in gastric
cancer. World J Gastroenterol. 10:1250–1255. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
225
|
Ambs S, Merriam WG, Bennett WP,
Felley-Bosco E, Ogunfusika MO, Oser SM, Klein S, Shields PG,
Billiar TR and Harris CC: Frequent nitric oxide synthase-2
expression in human colon adenomas: Implication for tumor
angiogenesis and colon cancer progression. Cancer Res. 58:334–341.
1998.PubMed/NCBI
|
|
226
|
Bocca C, Bozzo F, Bassignana A and
Miglietta A: Antiproliferative effect of a novel nitro-oxy
derivative of celecoxib in human colon cancer cells: Role of COX-2
and nitric oxide. Anticancer Res. 30:2659–2666. 2010.PubMed/NCBI
|
|
227
|
Dabrowska M, Uram L, Zielinski Z, Rode W
and Sikora E: Oxidative stress and inhibition of nitric oxide
generation underlie methotrexate-induced senescence in human colon
cancer cells. Mech Ageing Dev. 170:22–29. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
228
|
Narayanan BA, Narayanan NK, Desai D,
Pittman B and Reddy BS: Effects of a combination of docosahexaenoic
acid and 1,4-phenylene bis(methylene) selenocyanate on
cyclooxygenase 2, inducible nitric oxide synthase and beta-catenin
pathways in colon cancer cells. Carcinogenesis. 25:2443–2449. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
229
|
Narayanan BA, Narayanan NK, Simi B and
Reddy BS: Modulation of inducible nitric oxide synthase and related
proinflammatory genes by the omega-3 fatty acid docosahexaenoic
acid in human colon cancer cells. Cancer Res. 63:972–979.
2003.PubMed/NCBI
|
|
230
|
Kwak JY, Han MK, Choi KS, Park IH, Park
SY, Sohn MH, Kim UH, McGregor JR, Samlowski WE and Yim CY:
Cytokines secreted by lymphokine-activated killer cells induce
endogenous nitric oxide synthesis and apoptosis in DLD-1 colon
cancer cells. Cell Immunol. 203:84–94. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
231
|
Kapral M, Wawszczyk J, Sosnicki S and
Weglarz L: Down-regulation of inducible nitric oxide synthase
expression by inositol hexaphosphate in human colon cancer cells.
Acta Pol Pharm. 72:705–711. 2015.PubMed/NCBI
|
|
232
|
Puglisi MA, Cenciarelli C, Tesori V,
Cappellari M, Martini M, Di Francesco AM, Giorda E, Carsetti R,
Ricci-Vitiani L and Gasbarrini A: High nitric oxide production,
secondary to inducible nitric oxide synthase expression, is
essential for regulation of the tumour-initiating properties of
colon cancer stem cells. J Pathol. 236:479–490. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
233
|
Williams JL, Nath N, Chen J, Hundley TR,
Gao J, Kopelovich L, Kashfi K and Rigas B: Growth inhibition of
human colon cancer cells by nitric oxide (NO)-donating aspirin is
associated with cyclooxygenase-2 induction and beta-catenin/T-cell
factor signaling, nuclear factor-kappaB, and NO synthase 2
inhibition: Implications for chemoprevention. Cancer Res.
63:7613–7618. 2003.PubMed/NCBI
|
|
234
|
Tong X, Zheng S, Jin J, Zhu L, Lou Y and
Yao H: Triptolide inhibits cyclooxygenase-2 and inducible nitric
oxide synthase expression in human colon cancer and leukemia cells.
Acta Biochim Biophys Sin (Shanghai). 39:89–95. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
235
|
Sasahara Y, Mutoh M, Takahashi M, Fukuda
K, Tanaka N, Sugimura T and Wakabayashi K: Suppression of
promoter-dependent transcriptional activity of inducible nitric
oxide synthase by sodium butyrate in colon cancer cells. Cancer
Lett. 177:155–161. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
236
|
Shen X, Chen J, Qiu R, Fan X and Xin Y:
Effect of camptothecin on inducible nitric oxide synthase
expression in the colon cancer SW480 cell line. Oncol Lett.
10:3157–3160. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
237
|
Spiegel A, Hundley TR, Chen J, Ouyang N,
Liu X, Go MF, Tsioulias GJ, Kashfi K and Rigas B: NO-donating
aspirin inhibits both the expression and catalytic activity of
inducible nitric oxide synthase in HT-29 human colon cancer cells.
Biochem Pharmacol. 70:993–1000. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
238
|
Eijan AM, Piccardo I, Riveros MD, Sandes
EO, Porcella H, Jasnis MA, Sacerdote De Lustig E, Malagrino H,
Pasik L and Casabé AR: Nitric oxide in patients with transitional
bladder cancer. J Surg Oncol. 81:203–208. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
239
|
Hosseini A, Koskela LR, Ehren I,
Aguilar-Santelises M, Sirsjo A and Wiklund NP: Enhanced formation
of nitric oxide in bladder carcinoma in situ and in BCG treated
bladder cancer. Nitric Oxide. 15:337–343. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
240
|
Klotz T, Bloch W, Jacobs G, Niggemann S,
Engelmann U and Addicks K: Immunolocalization of inducible and
constitutive nitric oxide synthases in human bladder cancer.
Urology. 54:416–419. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
241
|
Koskela LR, Poljakovic M, Ehren I, Wiklund
NP and de Verdier PJ: Localization and expression of inducible
nitric oxide synthase in patients after BCG treatment for bladder
cancer. Nitric Oxide. 27:185–191. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
242
|
Langle YV, Balarino NP, Belgorosky D,
Cresta Morgado PD, Sandes EO, Marino L, Bilbao ER, Zambrano M,
Lodillinsky C and Eiján AM: Effect of nitric oxide inhibition in
Bacillus Calmette-Guerin bladder cancer treatment. Nitric Oxide.
98:50–59. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
243
|
Lin Z, Chen S, Ye C and Zhu S: Nitric
oxide synthase expression in human bladder cancer and its relation
to angiogenesis. Urol Res. 31:232–235. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
244
|
Ryk C, Steineck G, Wiklund NP, Nyberg T
and de Verdier PJ: The (CCTTT)n microsatellite polymorphism in the
nitric oxide synthase 2 gene may influence bladder cancer
pathogenesis. J Urol. 184:2150–2157. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
245
|
Ryk C, Wiklund NP, Nyberg T and De Verdier
PJ: Ser608Leu polymorphisms in the nitric oxide synthase-2 gene may
influence urinary bladder cancer pathogenesis. Scand J Urol
Nephrol. 45:319–325. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
246
|
Wolf H, Haeckel C and Roessner A:
Inducible nitric oxide synthase expression in human urinary bladder
cancer. Virchows Arch. 437:662–666. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
247
|
Sandes EO, Faletti AG, Riveros MD, Vidal
Mdel C, Gimenez L, Casabé AR and Eiján AM: Expression of inducible
nitric oxide synthase in tumoral and non-tumoral epithelia from
bladder cancer patients. Nitric Oxide. 12:39–45. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
248
|
Sandes EO, Lodillinsky C, Langle Y,
Belgorosky D, Marino L, Gimenez L, Casabé AR and Eiján AM:
Inducible nitric oxide synthase and PPARγ are involved in bladder
cancer progression. J Urol. 188:967–973. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
249
|
Ambs S and Harris CC: RESPONSE: Re:
Relationship between p53 mutations and inducible nitric oxide
synthase expression in human colorectal cancer. J Natl Cancer Inst.
91:1510–1511. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
250
|
Chung P, Cook T, Liu K, Vodovotz Y, Zamora
R, Finkelstein S, Billiar T and Blumberg D: Overexpression of the
human inducible nitric oxide synthase gene enhances
radiation-induced apoptosis in colorectal cancer cells via a
caspase-dependent mechanism. Nitric Oxide. 8:119–126. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
251
|
Cianchi F, Cortesini C, Fantappie O,
Messerini L, Sardi I, Lasagna N, Perna F, Fabbroni V, Di Felice A,
Perigli G, et al: Cyclooxygenase-2 activation mediates the
proangiogenic effect of nitric oxide in colorectal cancer. Clin
Cancer Res. 10:2694–2704. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
252
|
Cianchi F, Cortesini C, Fantappie O,
Messerini L, Schiavone N, Vannacci A, Nistri S, Sardi I, Baroni G,
Marzocca C, et al: Inducible nitric oxide synthase expression in
human colorectal cancer: Correlation with tumor angiogenesis. Am J
Pathol. 162:793–801. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
253
|
Fransen K, Elander N and Soderkvist P:
Nitric oxide synthase 2 (NOS2) promoter polymorphisms in colorectal
cancer. Cancer Lett. 225:99–103. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
254
|
Gallo O, Sardi I, Masini M and Franchi A:
Re: Relationship between p53 mutations and inducible nitric oxide
synthase expression in human colorectal cancer. J Natl Cancer Inst.
91:1509–1511. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
255
|
Ropponen KM, Kellokoski JK, Lipponen PK,
Eskelinen MJ, Alanne L, Alhava EM and Kosma VM: Expression of
inducible nitric oxide synthase in colorectal cancer and its
association with prognosis. Scand J Gastroenterol. 35:1204–1211.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
256
|
Zafirellis K, Zachaki A, Agrogiannis G and
Gravani K: Inducible nitric oxide synthase expression and its
prognostic significance in colorectal cancer. APMIS. 118:115–124.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
257
|
Wang Z, Cook T, Alber S, Liu K, Kovesdi I,
Watkins SK, Vodovotz Y, Billiar TR and Blumberg D: Adenoviral gene
transfer of the human inducible nitric oxide synthase gene enhances
the radiation response of human colorectal cancer associated with
alterations in tumor vascularity. Cancer Res. 64:1386–1395. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
258
|
Delarue FL, Taylor BS and Sebti SM: Ras
and RhoA suppress whereas RhoB enhances cytokine-induced
transcription of nitric oxide synthase-2 in human normal liver
AKN-1 cells and lung cancer A-549 cells. Oncogene. 20:6531–6537.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
259
|
Hu C, Li G and Wu E: A study on the
activity of nitric oxide in alveolar macrophages from patients with
lung cancer. Hunan Yi Ke Da Xue Xue Bao. 23:157–160. 1998.(In
Chinese). PubMed/NCBI
|
|
260
|
Li Y, Ma C, Shi X, Wen Z, Li D, Sun M and
Ding H: Effect of nitric oxide synthase on multiple drug resistance
is related to Wnt signaling in non-small cell lung cancer. Oncol
Rep. 32:1703–1708. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
261
|
Liu CY, Wang CH, Chen TC, Lin HC, Yu CT
and Kuo HP: Increased level of exhaled nitric oxide and
up-regulation of inducible nitric oxide synthase in patients with
primary lung cancer. Br J Cancer. 78:534–541. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
262
|
Liu CY, Wang YM, Wang CL, Feng PH, Ko HW,
Liu YH, Wu YC, Chu Y, Chung FT, Kuo CH, et al: Population
alterations of L-arginase- and inducible nitric oxide
synthase-expressed CD11b+/CD14-/CD15+/CD33+ myeloid-derived
suppressor cells and CD8+ T lymphocytes in patients with
advanced-stage non-small cell lung cancer. J Cancer Res Clin Oncol.
136:35–45. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
263
|
Zhang J, Li B, Ding X, Sun M, Li H, Yang
M, Zhou C, Yu H, Liu H and Yu G: Genetic variants in inducible
nitric oxide synthase gene are associated with the risk of
radiation-induced lung injury in lung cancer patients receiving
definitive thoracic radiation. Radiother Oncol. 111:194–198. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
264
|
Ye S, Yang W, Wang Y, Ou W, Ma Q, Yu C,
Ren J, Zhong G, Shi H, Yuan Z, et al: Cationic liposome-mediated
nitric oxide synthase gene therapy enhances the antitumor effects
of cisplatin in lung cancer. Int J Mol Med. 31:33–42. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
265
|
Sim SH, Ahn YO, Yoon J, Kim TM, Lee SH,
Kim DW and Heo DS: Influence of chemotherapy on nitric oxide
synthase, indole-amine-2,3-dioxygenase and CD124 expression in
granulocytes and monocytes of non-small cell lung cancer. Cancer
Sci. 103:155–160. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
266
|
Franco L, Doria D, Bertazzoni E, Benini A
and Bassi C: Increased expression of inducible nitric oxide
synthase and cyclooxygenase-2 in pancreatic cancer. Prostaglandins
Other Lipid Mediat. 73:51–58. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
267
|
Kong G, Kim E, Kim W, Lee YW, Lee JK, Paik
SW, Rhee JC, Choi KW and Lee KT: Inducible nitric oxide synthase
(iNOS) immunoreactivity and its relationship to cell proliferation,
apoptosis, angiogenesis, clinicopathologic characteristics, and
patient survival in pancreatic cancer. Int J Pancreatol.
29:133–140. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
268
|
Kong G, Kim EK, Kim WS, Lee KT, Lee YW,
Lee JK, Paik SW and Rhee JC: Role of cyclooxygenase-2 and inducible
nitric oxide synthase in pancreatic cancer. J Gastroenterol
Hepatol. 17:914–921. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
269
|
Wang J, He P, Gaida M, Yang S, Schetter
AJ, Gaedcke J, Ghadimi BM, Ried T, Yfantis H, Lee D, et al:
Inducible nitric oxide synthase enhances disease aggressiveness in
pancreatic cancer. Oncotarget. 7:52993–53004. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
270
|
Vickers SM, MacMillan-Crow LA, Green M,
Ellis C and Thompson JA: Association of increased immunostaining
for inducible nitric oxide synthase and nitrotyrosine with
fibroblast growth factor transformation in pancreatic cancer. Arch
Surg. 134:245–251. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
271
|
Takahashi M, Kitahashi T, Ishigamori R,
Mutoh M, Komiya M, Sato H, Kamanaka Y, Naka M, Maruyama T, Sugimura
T and Wakabayashi K: Increased expression of inducible nitric oxide
synthase (iNOS) in N-nitrosobis(2-oxopropyl)amine-induced hamster
pancreatic carcinogenesis and prevention of cancer development by
ONO-1714, an iNOS inhibitor. Carcinogenesis. 29:1608–1613. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
272
|
Chen HH, Su WC, Chou CY, Guo HR, Ho SY,
Que J and Lee WY: Increased expression of nitric oxide synthase and
cyclooxygenase-2 is associated with poor survival in cervical
cancer treated with radiotherapy. Int J Radiat Oncol Biol Phys.
63:1093–1100. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
273
|
Dong J, Cheng M and Sun H: Function of
inducible nitric oxide synthase in the regulation of cervical
cancer cell proliferation and the expression of vascular
endothelial growth factor. Mol Med Rep. 9:583–589. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
274
|
Jiang N, Tian Z, Tang J, Ou R and Xu Y:
Granulocyte macrophage-colony stimulating factor (GM-CSF)
downregulates the expression of protumor factors cyclooxygenase-2
and inducible nitric oxide synthase in a GM-CSF
receptor-independent manner in cervical cancer cells. Mediators
Inflamm. 2015:6016042015. View Article : Google Scholar : PubMed/NCBI
|
|
275
|
Lee TS, Jeon YT, Kim JW, Park NH, Kang SB,
Lee HP and Song YS: Lack of association of the cyclooxygenase-2 and
inducible nitric oxide synthase gene polymorphism with risk of
cervical cancer in Korean population. Ann N Y Acad Sci.
1095:134–142. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
276
|
Ryu YK, Lee JW and Moon EY: Thymosin
beta-4, actin-sequestering protein regulates vascular endothelial
growth factor expression via hypoxia-inducible nitric oxide
production in HeLa cervical cancer cells. Biomol Ther (Seoul).
23:19–25. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
277
|
Sowjanya AP, Rao M, Vedantham H, Kalpana
B, Poli UR, Marks MA and Sujatha M: Correlation of plasma
nitrite/nitrate levels and inducible nitric oxide gene expression
among women with cervical abnormalities and cancer. Nitric Oxide.
52:21–28. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
278
|
Li L, Zhu L, Hao B, Gao W, Wang Q, Li K,
Wang M, Huang M, Liu Z, Yang Q, et al: iNOS-derived nitric oxide
promotes glycolysis by inducing pyruvate kinase M2 nuclear
translocation in ovarian cancer. Oncotarget. 8:33047–33063. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
279
|
Malone JM, Saed GM, Diamond MP, Sokol RJ
and Munkarah AR: The effects of the inhibition of inducible nitric
oxide synthase on angiogenesis of epithelial ovarian cancer. Am J
Obstet Gynecol. 194:1110–1118. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
280
|
Martins Filho A, Jammal MP, Cobo Ede C,
Silveira TP, Adad SJ, Murta EF and Nomelini RS: Correlation of
cytokines and inducible nitric oxide synthase expression with
prognostic factors in ovarian cancer. Immunol Lett. 158:195–199.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
281
|
Raspollini MR, Amunni G, Villanucci A,
Boddi V, Baroni G, Taddei A and Taddei GL: Expression of inducible
nitric oxide synthase and cyclooxygenase-2 in ovarian cancer:
Correlation with clinical outcome. Gynecol Oncol. 92:806–812. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
282
|
Zhao L, Yu C, Zhou S, Lau WB, Lau B, Luo
Z, Lin Q, Yang H, Xuan Y, Yi T, et al: Epigenetic repression of
PDZ-LIM domain-containing protein 2 promotes ovarian cancer via
NOS2-derived nitric oxide signaling. Oncotarget. 7:1408–1420. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
283
|
Xu L, Xie K and Fidler IJ: Therapy of
human ovarian cancer by transfection with the murine interferon
beta gene: Role of macrophage-inducible nitric oxide synthase. Hum
Gene Ther. 9:2699–2708. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
284
|
Trinh B, Ko SY, Haria D, Barengo N and
Naora H: The homeoprotein DLX4 controls inducible nitric oxide
synthase-mediated angiogenesis in ovarian cancer. Mol Cancer.
14:972015. View Article : Google Scholar : PubMed/NCBI
|
|
285
|
Sanhueza C, Araos J, Naranjo L, Barros E,
Toledo L, Subiabre M, Toledo F, Gutiérrez J, Chiarello DI, Pardo F,
et al: Are NHE1 and inducible nitric oxide synthase involved in
human ovarian cancer? Pharmacol Res. 105:183–185. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
286
|
Jayasurya A, Dheen ST, Yap WM, Tan NG, Ng
YK and Bay BH: Inducible nitric oxide synthase and bcl-2 expression
in nasopharyngeal cancer: Correlation with outcome of patients
after radiotherapy. Int J Radiat Oncol Biol Phys. 56:837–845. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
287
|
Lukes P, Pacova H, Kucera T, Vesely D,
Martinek J and Astl J: Expression of endothelial and inducible
nitric oxide synthase and caspase-3 in tonsillar cancer, chronic
tonsillitis and healthy tonsils. Folia Biol (Praha). 54:141–145.
2008.PubMed/NCBI
|
|
288
|
Soler MN, Bobe P, Benihoud K, Lemaire G,
Roos BA and Lausson S: Gene therapy of rat medullary thyroid cancer
by naked nitric oxide synthase II DNA injection. J Gene Med.
2:344–352. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
289
|
Rafa H, Benkhelifa S, AitYounes S, Saoula
H, Belhadef S, Belkhelfa M, Boukercha A, Toumi R, Soufli I, Moralès
O, et al: All-trans retinoic acid modulates TLR4/NF-κB signaling
pathway targeting TNF-α and nitric oxide synthase 2 expression in
colonic mucosa during ulcerative colitis and colitis associated
cancer. Mediators Inflamm. 2017:73532522017. View Article : Google Scholar : PubMed/NCBI
|
|
290
|
Amasyali AS, Kucukgergin C, Erdem S, Sanli
O, Seckin S and Nane I: Nitric oxide synthase (eNOS4a/b) gene
polymorphism is associated with tumor recurrence and progression in
superficial bladder cancer cases. J Urol. 188:2398–2403. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
291
|
Polat F, Diler SB, Azazi İ and Öden A:
T-786C, G894T, and intron 4 VNTR (4a/b) polymorphisms of the
endothelial nitric oxide synthase gene in bladder cancer cases.
Asian Pac J Cancer Prev. 16:2199–2202. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
292
|
Ryk C, Wiklund NP, Nyberg T and de Verdier
PJ: Polymorphisms in nitric-oxide synthase 3 may influence the risk
of urinary-bladder cancer. Nitric Oxide. 25:338–343. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
293
|
Abedinzadeh M, Dastgheib SA, Maleki H,
Heiranizadeh N, Zare M, Jafari-Nedooshan J, Kargar S and
Neamatzadeh H: Association of endothelial nitric oxide synthase
gene polymorphisms with susceptibility to prostate cancer: A
comprehensive systematic review and meta-analysis. Urol J.
17:329–337. 2020.PubMed/NCBI
|
|
294
|
Branković A, Brajušković G, Nikolić Z,
Vukotić V, Cerović S, Savić-Pavićević D and Romac S: Endothelial
nitric oxide synthase gene polymorphisms and prostate cancer risk
in Serbian population. Int J Exp Pathol. 94:355–361. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
295
|
Diler SB and Oden A: The T-786C, G894T,
and intron 4 VNTR (4a/b) polymorphisms of the endothelial nitric
oxide synthase gene in prostate cancer cases. Genetika. 52:249–254.
2016.PubMed/NCBI
|
|
296
|
Fu Q, Liu X, Liu Y, Yang J, Lv G and Dong
S: MicroRNA-335 and −543 suppress bone metastasis in prostate
cancer via targeting endothelial nitric oxide synthase. Int J Mol
Med. 36:1417–1425. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
297
|
Medeiros R, Morais A, Vasconcelos A, Costa
S, Carrilho S, Oliveira J and Lopes C: Endothelial nitric oxide
synthase gene polymorphisms and the shedding of circulating tumour
cells in the blood of prostate cancer patients. Cancer Lett.
189:85–90. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
298
|
Medeiros R, Morais A, Vasconcelos A, Costa
S, Pinto D, Oliveira J and Lopes C: Endothelial nitric oxide
synthase gene polymorphisms and genetic susceptibility to prostate
cancer. Eur J Cancer Prev. 11:343–350. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
299
|
Medeiros RM, Morais A, Vasconcelos A,
Costa S, Pinto D, Oliveira J, Ferreira P and Lopes C: Outcome in
prostate cancer: Association with endothelial nitric oxide synthase
Glu-Asp298 polymorphism at exon 7. Clin Cancer Res. 8:3433–3437.
2002.PubMed/NCBI
|
|
300
|
Nikolic ZZ, Pavicevic D, Romac SP and
Brajuskovic GN: Genetic variants within endothelial nitric oxide
synthase gene and prostate cancer: A meta-analysis. Clin Transl
Sci. 8:23–31. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
301
|
Marangoni K, Neves AF, Cardoso AM, Santos
WK, Faria PC and Goulart LR: The endothelial nitric oxide synthase
Glu-298-Asp polymorphism and its mRNA expression in the peripheral
blood of patients with prostate cancer and benign prostatic
hyperplasia. Cancer Detect Prev. 30:7–13. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
302
|
Polytarchou C, Hatziapostolou M, Poimenidi
E, Mikelis C, Papadopoulou A, Parthymou A and Papadimitriou E:
Nitric oxide stimulates migration of human endothelial and prostate
cancer cells through up-regulation of pleiotrophin expression and
its receptor protein tyrosine phosphatase beta/zeta. Int J Cancer.
124:1785–1793. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
303
|
Re A, Aiello A, Nanni S, Grasselli A,
Benvenuti V, Pantisano V, Strigari L, Colussi C, Ciccone S,
Mazzetti AP, et al: Silencing of GSTP1, a prostate cancer
prognostic gene, by the estrogen receptor-β and endothelial nitric
oxide synthase complex. Mol Endocrinol. 25:2003–2016. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
304
|
Re A, Colussi C, Nanni S, Aiello A, Bacci
L, Grassi C, Pontecorvi A and Farsetti A: Nucleoporin 153 regulates
estrogen-dependent nuclear translocation of endothelial nitric
oxide synthase and estrogen receptor beta in prostate cancer.
Oncotarget. 9:27985–27997. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
305
|
Ziaei SA, Samzadeh M, Jamaldini SH,
Afshari M, Haghdoost AA and Hasanzad M: Endothelial nitric oxide
synthase Glu298Asp polymorphism as a risk factor for prostate
cancer. Int J Biol Markers. 28:43–48. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
306
|
Zhao C, Yan W, Zu X, Chen M, Liu L, Zhao
S, Liu H, Hu X, Luo R, Xia Y and Qi L: Association between
endothelial nitric oxide synthase 894G>T polymorphism and
prostate cancer risk: A meta-analysis of literature studies. Tumour
Biol. 35:11727–11733. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
307
|
Yu S, Jia L, Zhang Y, Wu D, Xu Z, Ng CF,
To KK, Huang Y and Chan FL: Increased expression of activated
endothelial nitric oxide synthase contributes to antiandrogen
resistance in prostate cancer cells by suppressing androgen
receptor transactivation. Cancer Lett. 328:83–94. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
308
|
Wu JH, Yang K, Ma HS and Xu Y: Association
of endothelia nitric oxide synthase gene rs1799983 polymorphism
with susceptibility to prostate cancer: A meta-analysis. Tumour
Biol. 35:7057–7062. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
309
|
Safarinejad MR and Safarinejad S, Shafiei
N and Safarinejad S: Effects of the T-786C, G894T, and Intron 4
VNTR (4a/b) polymorphisms of the endothelial nitric oxide synthase
gene on the risk of prostate cancer. Urol Oncol. 31:1132–1140.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
310
|
Sanli O, Kucukgergin C, Gokpinar M, Tefik
T, Nane I and Seckin S: Despite the lack of association between
different genotypes and the presence of prostate cancer,
endothelial nitric oxide synthase a/b (eNOS4a/b) polymorphism may
be associated with advanced clinical stage and bone metastasis.
Urol Oncol. 29:183–188. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
311
|
Bayraktutan Z, Kiziltunc A, Bakan E and
Alp HH: Determination of endothelial nitric oxide synthase gene
polymorphism and plasma asymmetric dimethyl arginine concentrations
in patients with lung cancer. Eurasian J Med. 52:185–190. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
312
|
Cheon KT, Choi KH, Lee HB, Park SK, Rhee
YK and Lee YC: Gene polymorphisms of endothelial nitric oxide
synthase and angiotensin-converting enzyme in patients with lung
cancer. Lung. 178:351–360. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
313
|
Fujita S, Masago K, Hatachi Y, Fukuhara A,
Hata A, Kaji R, Kim YH, Mio T, Mishima M and Katakami N: Genetic
polymorphisms in the endothelial nitric oxide synthase gene
correlate with overall survival in advanced non-small-cell lung
cancer patients treated with platinum-based doublet chemotherapy.
BMC Med Genet. 11:1672010. View Article : Google Scholar : PubMed/NCBI
|
|
314
|
Kocer C, Benlier N, Balci SO, Pehlivan S,
Sanli M and Nacak M: The role of endothelial nitric oxide synthase
gene polymorphisms in patients with lung cancer. Clin Respir J.
14:948–955. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
315
|
Peddireddy V, Badabagni SP, Gundimeda SD
and Mundluru HP: Association of eNOS and ACE gene polymorphisms and
plasma nitric oxide with risk of non-small cell lung cancer in
South India. Clin Respir J. 12:207–217. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
316
|
Chen CH, Wu SH, Tseng YM, Hou MF, Tsai LY
and Tsai SM: Distinct role of endothelial nitric oxide synthase
gene polymorphisms from menopausal status in the patients with
sporadic breast cancer in Taiwan. Nitric Oxide. 72:1–6. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
317
|
Crucitta S, Restante G, Del Re M,
Bertolini I, Bona E, Rofi E, Fontanelli L, Gianfilippo G, Fogli S,
Stasi I, et al: Endothelial nitric oxide synthase c.-813C>T
predicts for proteinuria in metastatic breast cancer patients
treated with bevacizumab-based chemotherapy. Cancer Chemother
Pharmacol. 84:1219–1227. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
318
|
Basaran G, Turhal NS, Cabuk D, Yurt N,
Yurtseven G, Gumus M, Teomete M, Dane F and Yumuk PF: Weight gain
after adjuvant chemotherapy in patients with early breast cancer in
Istanbul Turkey. Med Oncol. 28:409–415. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
319
|
Hao Y, Montiel R and Huang Y: Endothelial
nitric oxide synthase (eNOS) 894 G>T polymorphism is associated
with breast cancer risk: A meta-analysis. Breast Cancer Res Treat.
124:809–813. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
320
|
Hefler LA, Grimm C, Lantzsch T, Lampe D,
Koelbl H, Lebrecht A, Heinze G, Tempfer C, Reinthaller A and
Zeillinger R: Polymorphisms of the endothelial nitric oxide
synthase gene in breast cancer. Breast Cancer Res Treat.
98:151–155. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
321
|
Kafousi M, Vrekoussis T, Tsentelierou E,
Pavlakis K, Navrozoglou I, Dousias V, Sanidas E, Tsiftsis D,
Georgoulias V and Stathopoulos EN: Immunohistochemical study of the
angiogenetic network of VEGF, HIF1α, VEGFR-2 and endothelial nitric
oxide synthase (eNOS) in human breast cancer. Pathol Oncol Res.
18:33–41. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
322
|
Loibl S, Bratengeier J, Farines V, von
Minckwitz G, Spänkuch B, Schini-Kerth V, Nepveu F, Strebhardt K and
Kaufmann M: Investigations on the inducible and endothelial nitric
oxide synthases in human breast cancer cell line MCF-7-estrogen has
an influence on e-NOS, but not on i-NOS. Pathol Res Pract. 202:1–7.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
323
|
Loibl S, Strank C, von Minckwitz G, Sinn
HP, Buck A, Solbach C, Strebhardt K and Kaufmann M:
Immunohistochemical evaluation of endothelial nitric oxide synthase
expression in primary breast cancer. Breast. 14:230–235. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
324
|
Lu J, Wei Q, Bondy ML, Yu TK, Li D,
Brewster A, Shete S, Sahin A, Meric-Bernstam F and Wang LE:
Promoter polymorphism (−786t>C) in the endothelial nitric oxide
synthase gene is associated with risk of sporadic breast cancer in
non-Hispanic white women age younger than 55 years. Cancer.
107:2245–2253. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
325
|
Mortensen K, Holck S, Christensen IJ,
Skouv J, Hougaard DM, Blom J and Larsson LI: Endothelial cell
nitric oxide synthase in peritumoral microvessels is a favorable
prognostic indicator in premenopausal breast cancer patients. Clin
Cancer Res. 5:1093–1097. 1999.PubMed/NCBI
|
|
326
|
Mortensen K, Skouv J, Hougaard DM and
Larsson LI: Endogenous endothelial cell nitric-oxide synthase
modulates apoptosis in cultured breast cancer cells and is
transcriptionally regulated by p53. J Biol Chemistry.
274:37679–37684. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
327
|
Martin JH, Begum S, Alalami O, Harrison A
and Scott KW: Endothelial nitric oxide synthase: Correlation with
histologic grade, lymph node status and estrogen receptor
expression in human breast cancer. Tumour Biol. 21:90–97. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
328
|
Ramírez-Patiño R, Figuera LE, Puebla-Pérez
AM, Delgado-Saucedo JI, Legazpí-Macias MM, Mariaud-Schmidt RP,
Ramos-Silva A, Gutiérrez-Hurtado IA, Gómez Flores-Ramos L,
Zúñiga-González GM and Gallegos-Arreola MP: Intron 4 VNTR (4a/b)
polymorphism of the endothelial nitric oxide synthase gene is
associated with breast cancer in Mexican women. J Korean Med Sci.
28:1587–1594. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
329
|
Zintzaras E, Grammatikou M, Kitsios GD,
Doxani C, Zdoukopoulos N, Papandreou C and Patrikidou A:
Polymorphisms of the endothelial nitric oxide synthase gene in
breast cancer: A genetic association study and meta-analysis. J Hum
Genet. 55:743–748. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
330
|
Zhang L, Zeng M and Fu BM: Inhibition of
endothelial nitric oxide synthase decreases breast cancer cell
MDA-MB-231 adhesion to intact microvessels under physiological
flows. Am J Physiol Heart Circ Physiol. 310:H1735–H1747. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
331
|
Carkic J, Nikolic N, Nisevic J, Lazarevic
M, Kuzmanovic-Pficer J, Jelovac D and Milasin J: Endothelial nitric
oxide synthase polymorphisms/haplotypes are strong modulators of
oral cancer risk in Serbian population. J Oral Sci. 62:322–326.
2020. View Article : Google Scholar : PubMed/NCBI
|
|
332
|
Karthik B, Shruthi DK, Singh J,
Tegginamani AS and Kudva S: Do tobacco stimulate the production of
nitric oxide by up regulation of inducible nitric oxide synthesis
in cancer: Immunohistochemical determination of inducible nitric
oxide synthesis in oral squamous cell carcinoma-a comparative study
in tobacco habituers and non-habituers. J Cancer Res Ther.
10:244–250. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
333
|
Chen Y, Li J, Guo Y and Guo XY: Nitric
oxide synthase 3 gene variants and colorectal cancer: A
meta-analysis. Asian Pac J Cancer Prev. 15:3811–3815. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
334
|
Mortensen K, Christensen IJ, Nielsen HJ,
Hansen U and Larsson LI: High expression of endothelial cell nitric
oxide synthase in peritumoral microvessels predicts increased
disease-free survival in colorectal cancer. Cancer Lett.
216:109–114. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
335
|
Peñarando J, López-Sánchez LM, Mena R,
Guil-Luna S, Conde F, Hernández V, Toledano M, Gudiño V, Raponi M,
Billard C, et al: A role for endothelial nitric oxide synthase in
intestinal stem cell proliferation and mesenchymal colorectal
cancer. BMC Biol. 16:32018. View Article : Google Scholar : PubMed/NCBI
|
|
336
|
Yeh CC, Santella RM, Hsieh LL, Sung FC and
Tang R: An intron 4 VNTR polymorphism of the endothelial nitric
oxide synthase gene is associated with early-onset colorectal
cancer. Int J Cancer. 124:1565–1571. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
337
|
Hefler LA, Ludwig E, Lampe D, Zeillinger
R, Leodolter S, Gitsch G, Koelbl H and Tempfer CB: Polymorphisms of
the endothelial nitric oxide synthase gene in ovarian cancer.
Gynecol Oncol. 86:134–137. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
338
|
Krishnaveni D, Amar Chand B, Shravan Kumar
P, Uma Devi M, Ramanna M, Jyothy A, Pratibha N, Balakrishna N and
Venkateshwari A: Association of endothelial nitric oxide synthase
gene T-786C promoter polymorphism with gastric cancer. World J
Gastrointest Oncol. 7:87–94. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
339
|
Wang L, Shi GG, Yao JC, Gong W, Wei D, Wu
TT, Ajani JA, Huang S and Xie K: Expression of endothelial nitric
oxide synthase correlates with the angiogenic phenotype of and
predicts poor prognosis in human gastric cancer. Gastric Cancer.
8:18–28. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
340
|
Tecder Ünal M, Karabulut HG, Gümüş-Akay G,
Dölen Y, Elhan A, Tükün A and Ünal AE: Endothelial nitric oxide
synthase gene polymorphism in gastric cancer. Turk J Gastroenterol.
21:338–344. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
341
|
de Fatima A, Zambuzzi WF, Modolo LV,
Tarsitano CA, Gadelha FR, Hyslop S, de Carvalho JE, Salgado I,
Ferreira CV and Pilli RA: Cytotoxicity of goniothalamin enantiomers
in renal cancer cells: Involvement of nitric oxide, apoptosis and
autophagy. Chem Biol Interact. 176:143–150. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
342
|
Hung WC, Wu TF, Ng SC, Lee YC, Shen HP,
Yang SF and Wang PH: Involvement of endothelial nitric oxide
synthase gene variants in the aggressiveness of uterine cervical
cancer. J Cancer. 10:2594–2600. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
343
|
Waheed S, Cheng RY, Casablanca Y, Maxwell
GL, Wink DA and Syed V: Nitric oxide donor DETA/NO inhibits the
growth of endometrial cancer cells by upregulating the expression
of RASSF1 and CDKN1A. Molecules. 24:37222019. View Article : Google Scholar : PubMed/NCBI
|
|
344
|
Riener EK, Hefler LA, Grimm C, Galid A,
Zeillinger R, Tong-Cacsire D, Gitsch G, Leodolter S and Tempfer CB:
Polymorphisms of the endothelial nitric oxide synthase gene in
women with vulvar cancer. Gynecol Oncol. 93:686–690. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
345
|
Wang J, Yang S, He P, Schetter AJ, Gaedcke
J, Ghadimi BM, Ried T, Yfantis HG, Lee DH, Gaida MM, et al:
Endothelial Nitric oxide synthase traffic inducer (NOSTRIN) is a
negative regulator of disease aggressiveness in pancreatic cancer.
Clin Cancer Res. 22:5992–6001. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
346
|
Yanar K, Cakatay U, Aydin S, Verim A,
Atukeren P, Özkan NE, Karatoprak K, Cebe T, Turan S, Ozkök E, et
al: Relation between endothelial nitric oxide synthase genotypes
and oxidative stress markers in larynx cancer. Oxid Med Cell
Longev. 2016:49850632016. View Article : Google Scholar : PubMed/NCBI
|
|
347
|
Chen C, Wang Y, Goh SS, Yang J, Lam DH,
Choudhury Y, Tay FC, Du S, Tan WK, Purwanti YI, et al: Inhibition
of neuronal nitric oxide synthase activity promotes migration of
human-induced pluripotent stem cell-derived neural stem cells
toward cancer cells. J Neurochem. 126:318–330. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
348
|
Karihtala P, Soini Y, Auvinen P, Tammi R,
Tammi M and Kosma VM: Hyaluronan in breast cancer: Correlations
with nitric oxide synthases and tyrosine nitrosylation. J Histochem
Cytochem. 55:1191–1198. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
349
|
Lewko B, Zółtowska A, Stepiński J,
Kamiński M, Skokowski J, Roszkiewicz A and Moszkowska G: Nitric
oxide synthase type 1 expression in human lung cancer and its
relation to p53. Med Sci Monit. 7:218–221. 2001.PubMed/NCBI
|
|
350
|
Ahmed HH, Metwally FM, Mahdy ES, Shosha WG
and Ramadan SS: Clinical value of serum hepatocyte growth factor,
B-cell lymphoma-2 and nitric oxide in primary breast cancer
patients. Eur Rev Med Pharmacol Sci. 16:958–965. 2012.PubMed/NCBI
|
|
351
|
Al Dhaheri Y, Attoub S, Arafat K, Abuqamar
S, Viallet J, Saleh A, Al Agha H, Eid A and Iratni R:
Anti-metastatic and anti-tumor growth effects of Origanum majorana
on highly metastatic human breast cancer cells: Inhibition of NFκB
signaling and reduction of nitric oxide production. PLoS One.
8:e688082013. View Article : Google Scholar : PubMed/NCBI
|
|
352
|
Avtandilyan N, Javrushyan H, Petrosyan G
and Trchounian A: The involvement of arginase and nitric oxide
synthase in breast cancer development: Arginase and NO Synthase as
therapeutic targets in cancer. Biomed Res Int. 2018:86969232018.
View Article : Google Scholar : PubMed/NCBI
|
|
353
|
Bani D, Masini E, Bello MG, Bigazzi M and
Sacchi TB: Relaxin activates the L-arginine-nitric oxide pathway in
human breast cancer cells. Cancer Res. 55:5272–5275.
1995.PubMed/NCBI
|
|
354
|
Avtandilyan N, Javrushyan H, Karapetyan A
and Trchounian A: RETRACTED ARTICLE: Inhibition of tumor
progression by NG-Nitro-L-arginine Methyl Ester in
7,12-dimethylbenz(a)anthracene induced breast cancer: Nitric oxide
synthase inhibition as an antitumor prevention. J Mammary Gland
Biol Neoplasia. 24:1992019. View Article : Google Scholar : PubMed/NCBI
|
|
355
|
Alagol H, Erdem E, Sancak B, Turkmen G,
Camlibel M and Bugdayci G: Nitric oxide biosynthesis and
malondialdehyde levels in advanced breast cancer. Aust N Z J Surg.
69:647–650. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
356
|
Bhattacharjee KG, Bhattacharyya M, Halder
UC, Jana P and Sinha AK: The ‘Cross Talk’ between the receptors of
insulin, estrogen and progesterone in neutrophils in the synthesis
of maspin through nitric oxide in breast cancer. Int J Biomed Sci.
8:129–139. 2012.PubMed/NCBI
|
|
357
|
Cendan JC, Souba WW, Copeland EM III and
Lind DS: Increased L-arginine transport in a nitric oxide-producing
metastatic colon cancer cell line. Ann Surg Oncol. 3:501–508. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
358
|
Cendan JC, Topping DL, Pruitt J, Snowdy S,
Copeland EM III and Lind DS: Inflammatory mediators stimulate
arginine transport and arginine-derived nitric oxide production in
a murine breast cancer cell line. J Surg Res. 60:284–288. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
359
|
Chakraborty S, Girish GV and Sinha AK:
Impaired binding of insulin to erythrocyte membrane receptor and
the activation of nitric oxide synthase by the hormone in human
breast cancer. J Cancer Res Clin Oncol. 130:294–300. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
360
|
Coskun U, Gunel N, Sancak B, Günel U, Onuk
E, Bayram O, Yílmaz E, Candan S and Ozkan S: Significance of serum
vascular endothelial growth factor, insulin-like growth factor-I
levels and nitric oxide activity in breast cancer patients. Breast.
12:104–110. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
361
|
Coskun U, Gunel N, Sancak B, Günel U, Onuk
E, Bayram O, Yílmaz E, Candan S and Ozkan S: WITHDRAWN:
Significance of serum vascular endothelial growth factor,
insulin-like growth factor-I levels and nitric oxide activity in
breast cancer patients. Breast. Aug 20–2008.doi:
10.1054/brst.2002.0483 (Epub ahead of print). PubMed/NCBI
|
|
362
|
Dave B, Granados-Principal S, Zhu R, Benz
S, Rabizadeh S, Soon-Shiong P, Yu KD, Shao Z, Li X, Gilcrease M, et
al: Targeting RPL39 and MLF2 reduces tumor initiation and
metastasis in breast cancer by inhibiting nitric oxide synthase
signaling. Proc Natl Acad Sci USA. 111:8838–8843. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
363
|
De Vitto H, Mendonca BS, Elseth KM, Onul
A, Xue J, Vesper BJ, Gallo CV, Rumjanek FD, Paradise WA and
Radosevich JA: Part III. Molecular changes induced by high nitric
oxide adaptation in human breast cancer cell line BT-20
(BT-20-HNO): A switch from aerobic to anaerobic metabolism. Tumour
Biol. 34:403–413. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
364
|
Deliconstantinos G, Villiotou V, Stavrides
JC, Salemes N and Gogas J: Nitric oxide and peroxynitrite
production by human erythrocytes: A causative factor of toxic
anemia in breast cancer patients. Anticancer Res. 15:1435–1446.
1995.PubMed/NCBI
|
|
365
|
Demircan B, Yucel B and Radosevich JA: DNA
methylation in human breast cancer cell lines adapted to high
nitric oxide. In Vivo. 34:169–176. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
366
|
Duan L, Danzer B, Levenson VV and Maki CG:
Critical roles for nitric oxide and ERK in the completion of
prosurvival autophagy in 4OHTAM-treated estrogen receptor-positive
breast cancer cells. Cancer Lett. 353:290–300. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
367
|
El Hasasna H, Saleh A, Al Samri H,
Athamneh K, Attoub S, Arafat K, Benhalilou N, Alyan S, Viallet J,
Al Dhaheri Y, et al: Rhus coriaria suppresses angiogenesis,
metastasis and tumor growth of breast cancer through inhibition of
STAT3, NFκB and nitric oxide pathways. Scic Rep. 6:211442016.
View Article : Google Scholar : PubMed/NCBI
|
|
368
|
Engelen M, Klimberg VS, Allasia A and
Deutz NEP: Major surgery diminishes systemic arginine availability
and suppresses nitric oxide response to feeding in patients with
early stage breast cancer. Clin Nutr. 37:1645–1653. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
369
|
Erbas H, Aydogdu N, Usta U and Erten O:
Protective role of carnitine in breast cancer via decreasing
arginase activity and increasing nitric oxide. Cell Biol Int.
31:1414–1419. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
370
|
Gaballah HE, Abdel Salam I, Abdel Wahab N
and Mansour OM: Plasma bcl-2 and nitric oxide: Possible prognostic
role in patients with metastatic breast cancer. Med Oncol.
18:171–178. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
371
|
Gajalakshmi P, Priya MK, Pradeep T, Behera
J, Muthumani K, Madhuwanti S, Saran U and Chatterjee S: Breast
cancer drugs dampen vascular functions by interfering with nitric
oxide signaling in endothelium. Toxicol Appl Pharmacol.
269:121–131. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
372
|
Ganguly Bhattacharjee K, Bhattacharyya M,
Halder UC, Jana P and Sinha AK: The role of neutrophil estrogen
receptor status on maspin synthesis via nitric oxide production in
human breast cancer. J Breast Cancer. 15:181–188. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
373
|
Ganguly Bhattacharjee K, Bhattacharyya M,
Halder UC, Jana P and Sinha AK: Effect of progesterone receptor
status on maspin synthesis via nitric oxide production in
neutrophils in human breast cancer. Breast Cancer. 21:605–613.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
374
|
Gaspari APS, da Silva RS, Carneiro ZA, de
Carvalho MR, Carvalho I, Pernomian L, Ferreira LP, Ramos LCB, de
Souza GA and Formiga ALB: Improving cytotoxicity against breast
cancer cells by using Mixed-Ligand Ruthenium(II) Complexes of
2,2′-Bipyridine, amino acid, and nitric oxide derivatives as
potential anticancer agents. Anticancer Agents Med Chem.
21:1602–1611. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
375
|
Guha M, Biswas J, Tirkey J and Sinha AK:
Impairment of stimulation by estrogen of insulin-activated nitric
oxide synthase in human breast cancer. Int J Cancer. 100:261–265.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
376
|
Günel N, Coskun U, Sancak B, Hasdemir O,
Sare M, Bayram O, Celenkoglu G and Ozkan S: Prognostic value of
serum IL-18 and nitric oxide activity in breast cancer patients at
operable stage. Am J Clin Oncol. 26:416–421. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
377
|
Kampa M, Hatzoglou A, Notas G, Niniraki M,
Kouroumalis E and Castanas E: Opioids are non-competitive
inhibitors of nitric oxide synthase in T47D human breast cancer
cells. Cell Death Differ. 8:943–952. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
378
|
Khalkhali-Ellis Z and Hendrix MJ: Nitric
oxide regulation of maspin expression in normal mammary epithelial
and breast cancer cells. Am J Pathol. 162:1411–1417. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
379
|
Konukoglu D, Turhan MS, Celik V and Turna
H: Relation of serum vascular endothelial growth factor as an
angiogenesis biomarker with nitric oxide & urokinase-type
plasminogen activator in breast cancer patients. Indian J Med Res.
125:747–751. 2007.PubMed/NCBI
|
|
380
|
Kumar S and Kashyap P: Antiproliferative
activity and nitric oxide production of a methanolic extract of
Fraxinus micrantha on Michigan Cancer Foundation-7 mammalian breast
carcinoma cell line. J Intercult Ethnopharmacol. 4:109–113. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
381
|
Lahiri M and Martin JH: Nitric oxide
decreases motility and increases adhesion in human breast cancer
cells. Oncol Rep. 21:275–281. 2009.PubMed/NCBI
|
|
382
|
Lee SY, Rim Y, McPherson DD, Huang SL and
Kim H: A novel liposomal nanomedicine for nitric oxide delivery and
breast cancer treatment. Biomed Mater Eng. 24:61–67.
2014.PubMed/NCBI
|
|
383
|
Hewala TI, Abd El-Moneim NA, Ebied SA,
Sheta MI, Soliman K and Abu-Elenean A: Diagnostic and prognostic
value of serum nitric oxide, tumor necrosis factor-alpha, basic
fibroblast growth factor and copper as angiogenic markers in
premenopausal breast cancer patients: A case-control study. Br J
Biomed Sci. 67:167–176. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
384
|
Finkelman BS, Putt M, Wang T, Wang L,
Narayan H, Domchek S, DeMichele A, Fox K, Matro J, Shah P, et al:
Arginine-nitric oxide metabolites and cardiac dysfunction in
patients with breast cancer. J Am Coll Cardiol. 70:152–162. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
385
|
Jadeski LC, Chakraborty C and Lala PK:
Role of nitric oxide in tumour progression with special reference
to a murine breast cancer model. Can J Physiol Pharmacol.
80:125–135. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
386
|
McCurdy MR, Wazni MW, Martinez J, McAleer
MF and Guerrero T: Exhaled nitric oxide predicts radiation
pneumonitis in esophageal and lung cancer patients receiving
thoracic radiation. Radiother Oncol. 101:443–448. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
387
|
Metwally FM, El-mezayen HA and Ahmed HH:
Significance of vascular endothelial growth factor, interleukin-18
and nitric oxide in patients with breast cancer: Correlation with
carbohydrate antigen 15.3. Med Oncol. 28 (Suppl 1):S15–S21. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
388
|
Mishra D, Patel V and Banerjee D: Nitric
Oxide and S-Nitrosylation in Cancers: Emphasis on breast cancer.
Breast Cancer (Auckl). 14:11782234198826882020.PubMed/NCBI
|
|
389
|
Nakamura Y, Yasuoka H, Tsujimoto M,
Yoshidome K, Nakahara M, Nakao K, Nakamura M and Kakudo K: Nitric
oxide in breast cancer: Induction of vascular endothelial growth
factor-C and correlation with metastasis and poor prognosis. Clin
Cancer Res. 12:1201–1207. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
390
|
Negroni MP, Fiszman GL, Azar ME, Morgado
CC, Español AJ, Pelegrina LT, de la Torre E and Sales ME:
Immunoglobulin G from breast cancer patients in stage I stimulates
muscarinic acetylcholine receptors in MCF7 cells and induces
proliferation. Participation of nitric oxide synthase-derived
nitric oxide. J Clin Immunol. 30:474–484. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
391
|
Martin JH, Alalami O and Yaqoob F:
Differential effects of retinoids on nitric oxide production by
promonocytic U937 cells and ZR-75-1 human breast cancer cells.
Oncol Rep. 7:219–223. 2000.PubMed/NCBI
|
|
392
|
Martin JH, Symonds A and Chohan S:
Down-regulation of nitric oxide production by droloxifene and
toremifene in human breast cancer cells. Oncol Rep. 10:979–984.
2003.PubMed/NCBI
|
|
393
|
Nath N, Chattopadhyay M, Rodes DB,
Nazarenko A, Kodela R and Kashfi K: Nitric Oxide-releasing aspirin
suppresses NF-κB signaling in estrogen receptor negative breast
cancer cells in vitro and in vivo. Molecules. 20:12481–12499. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
394
|
Pance A: Nitric oxide and hormones in
breast cancer: Allies or enemies? Future Oncol. 2:275–288. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
395
|
Parihar A, Parihar MS and Ghafourifar P:
Significance of mitochondrial calcium and nitric oxide for
apoptosis of human breast cancer cells induced by tamoxifen and
etoposide. Int J Mol Med. 21:317–324. 2008.PubMed/NCBI
|
|
396
|
Pervin S, Singh R and Chaudhuri G: Nitric
oxide-induced cytostasis and cell cycle arrest of a human breast
cancer cell line (MDA-MB-231): Potential role of cyclin D1. Proc
Natl Acad Sci USA. 98:3583–3588. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
397
|
Pervin S, Singh R and Chaudhuri G: Nitric
oxide, N omega-hydroxy-L-arginine and breast cancer. Nitric Oxide.
19:103–106. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
398
|
Pervin S, Singh R, Freije WA and Chaudhuri
G: MKP-1-induced dephosphorylation of extracellular
signal-regulated kinase is essential for triggering nitric
oxide-induced apoptosis in human breast cancer cell lines:
Implications in breast cancer. Cancer Res. 63:8853–8860.
2003.PubMed/NCBI
|
|
399
|
Pervin S, Singh R, Gau CL, Edamatsu H,
Tamanoi F and Chaudhuri G: Potentiation of nitric oxide-induced
apoptosis of MDA-MB-468 cells by farnesyltransferase inhibitor:
Implications in breast cancer. Cancer Res. 61:4701–4706.
2001.PubMed/NCBI
|
|
400
|
Pervin S, Singh R, Hernandez E, Wu G and
Chaudhuri G: Nitric oxide in physiologic concentrations targets the
translational machinery to increase the proliferation of human
breast cancer cells: Involvement of mammalian target of
rapamycin/eIF4E pathway. Cancer Res. 67:289–299. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
401
|
Punathil T, Tollefsbol TO and Katiyar SK:
EGCG inhibits mammary cancer cell migration through inhibition of
nitric oxide synthase and guanylate cyclase. Biochem Biophys Res
Commun. 375:162–167. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
402
|
Radisavljevic Z: Inactivated tumor
suppressor Rb by nitric oxide promotes mitosis in human breast
cancer cells. J Cell Biochem. 92:1–5. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
403
|
Rashad YA, Elkhodary TR, El-Gayar AM and
Eissa LA: Evaluation of serum levels of HER2, MMP-9, Nitric Oxide,
and total antioxidant capacity in egyptian breast cancer patients:
Correlation with clinico-pathological parameters. Sci Pharm.
82:129–145. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
404
|
Ray GN, Shahid M and Husain SA: Effect of
nitric oxide and malondialdehyde on sister-chromatid exchanges in
breast cancer. Br J Biomed Sci. 58:169–176. 2001.PubMed/NCBI
|
|
405
|
Reveneau S, Arnould L, Jolimoy G, Hilpert
S, Lejeune P, Saint-Giorgio V, Belichard C and Jeannin JF: Nitric
oxide synthase in human breast cancer is associated with tumor
grade, proliferation rate, and expression of progesterone
receptors. Lab Invest. 79:1215–1225. 1999.PubMed/NCBI
|
|
406
|
Ridnour LA, Barasch KM, Windhausen AN,
Dorsey TH, Lizardo MM, Yfantis HG, Lee DH, Switzer CH, Cheng RY,
Heinecke JL, et al: Nitric oxide synthase and breast cancer: Role
of TIMP-1 in NO-mediated Akt activation. PLoS One. 7:e440812012.
View Article : Google Scholar : PubMed/NCBI
|
|
407
|
Zhu W, Yang B, Fu H, Ma L, Liu T, Chai R,
Zheng Z, Zhang Q and Li G: Flavone inhibits nitric oxide synthase
(NOS) activity, nitric oxide production and protein S-nitrosylation
in breast cancer cells. Biochem Biophys Res Commun. 458:590–595.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
408
|
Zheng X, Fernando V, Sharma V, Walia Y,
Letson J and Furuta S: Correction of arginine metabolism with
sepiapterin-the precursor of nitric oxide synthase cofactor
BH(4)-induces immunostimulatory-shift of breast cancer. Biochem
Pharmacol. 176:1138872020. View Article : Google Scholar : PubMed/NCBI
|
|
409
|
Zeillinger R, Tantscher E, Schneeberger C,
Tschugguel W, Eder S, Sliutz G and Huber JC: Simultaneous
expression of nitric oxide synthase and estrogen receptor in human
breast cancer cell lines. Breast Cancer Res Treat. 40:205–207.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
410
|
Wang HJ, Wei XF, Jiang YY, Huang H, Yang
Y, Fan SM, Zang LH, Tashiro S, Onodera S and Ikejima T: Silibinin
induces the generation of nitric oxide in human breast cancer MCF-7
cells. Free Radic Res. 44:577–584. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
411
|
Thamrongwittawatpong L, Sirivatanauksorn
Y, Batten JJ, Williamson RC, Kakkar AK and Mathie RT: The effect of
N(G)-monomethyl-L-arginine and tamoxifen on nitric oxide production
in breast cancer cells stimulated by oestrogen and progesterone.
Eur J Surg. 167:484–489. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
412
|
Toomey D, Condron C, Wu QD, Kay E, Harmey
J, Broe P, Kelly C and Bouchier-Hayes D: TGF-beta1 is elevated in
breast cancer tissue and regulates nitric oxide production from a
number of cellular sources during hypoxia re-oxygenation injury. Br
J Biomed Sci. 58:177–183. 2001.PubMed/NCBI
|
|
413
|
Salaroglio IC, Gazzano E, Abdullrahman A,
Mungo E, Castella B, Abd-Elrahman GEFA, Massaia M, Donadelli M,
Rubinstein M, Riganti C and Kopecka J: Increasing intratumor
C/EBP-β LIP and nitric oxide levels overcome resistance to
doxorubicin in triple negative breast cancer. J Exp Clin Cancer
Res. 37:2862018. View Article : Google Scholar : PubMed/NCBI
|
|
414
|
Sen S, Kawahara B and Chaudhuri G:
Mitochondrial-associated nitric oxide synthase activity inhibits
cytochrome c oxidase: Implications for breast cancer. Free Radic
Biol Med. 57:210–220. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
415
|
Sen S, Kawahara B, Fukuto J and Chaudhuri
G: Induction of a feed forward pro-apoptotic mechanistic loop by
nitric oxide in a human breast cancer model. PLoS One.
8:e705932013. View Article : Google Scholar : PubMed/NCBI
|
|
416
|
Shoulars K, Rodriguez MA, Thompson T, Turk
J, Crowley J and Markaverich BM: Regulation of the nitric oxide
pathway genes by tetrahydrofurandiols: Microarray analysis of MCF-7
human breast cancer cells. Cancer Lett. 264:265–273. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
417
|
Simeone AM, Broemeling LD, Rosenblum J and
Tari AM: HER2/neu reduces the apoptotic effects of
N-(4-hydroxyphenyl)retinamide (4-HPR) in breast cancer cells by
decreasing nitric oxide production. Oncogene. 22:6739–6747. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
418
|
Simeone AM, Ekmekcioglu S, Broemeling LD,
Grimm EA and Tari AM: A novel mechanism by which
N-(4-hydroxyphenyl)retinamide inhibits breast cancer cell growth:
The production of nitric oxide. Mol Cancer Ther. 1:1009–1017.
2002.PubMed/NCBI
|
|
419
|
Simeone AM, McMurtry V, Nieves-Alicea R,
Saavedra JE, Keefer LK, Johnson MM and Tari AM: TIMP-2 mediates the
anti-invasive effects of the nitric oxide-releasing prodrug JS-K in
breast cancer cells. Breast Cancer Res. 10:R442008. View Article : Google Scholar : PubMed/NCBI
|
|
420
|
Singh T and Katiyar SK: Honokiol, a
phytochemical from Magnolia spp., inhibits breast cancer cell
migration by targeting nitric oxide and cyclooxygenase-2. Int J
Oncol. 38:769–776. 2011.PubMed/NCBI
|
|
421
|
Smeda M, Kieronska A, Adamski MG,
Proniewski B, Sternak M, Mohaissen T, Przyborowski K, Derszniak K,
Kaczor D, Stojak M, et al: Nitric oxide deficiency and
endothelial-mesenchymal transition of pulmonary endothelium in the
progression of 4T1 metastatic breast cancer in mice. Breast Cancer
Res. 20:862018. View Article : Google Scholar : PubMed/NCBI
|
|
422
|
Song YK, Billiar TR and Lee YJ: Role of
galectin-3 in breast cancer metastasis: Involvement of nitric
oxide. Am J Pathol. 160:1069–1075. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
423
|
Switzer CH, Cheng RY, Ridnour LA, Glynn
SA, Ambs S and Wink DA: Ets-1 is a transcriptional mediator of
oncogenic nitric oxide signaling in estrogen receptor-negative
breast cancer. Breast Cancer Res. 14:R1252012. View Article : Google Scholar : PubMed/NCBI
|
|
424
|
Switzer CH, Glynn SA, Ridnour LA, Cheng
RY, Vitek MP, Ambs S and Wink DA: Nitric oxide and protein
phosphatase 2A provide novel therapeutic opportunities in
ER-negative breast cancer. Trends Pharmacol Sci. 32:644–651. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
425
|
Ai Y, Kang F, Huang Z, Xue X, Lai Y, Peng
S, Tian J and Zhang Y: Synthesis of CDDO-amino acid-nitric oxide
donor trihybrids as potential antitumor agents against both
drug-sensitive and drug-resistant colon cancer. J Med Chem.
58:2452–2464. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
426
|
Babykutty S, Suboj P, Srinivas P, Nair AS,
Chandramohan K and Gopala S: Insidious role of nitric oxide in
migration/invasion of colon cancer cells by upregulating MMP-2/9
via activation of cGMP-PKG-ERK signaling pathways. Clin Exp
Metastasis. 29:471–492. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
427
|
Bessa X, Elizalde JI, Mitjans F, Piñol V,
Miquel R, Panés J, Piulats J, Piqué JM and Castells A: Leukocyte
recruitment in colon cancer: Role of cell adhesion molecules,
nitric oxide, and transforming growth factor beta1.
Gastroenterology. 122:1122–1132. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
428
|
Chattopadhyay M, Kodela R, Olson KR and
Kashfi K: NOSH-aspirin (NBS-1120), a novel nitric oxide- and
hydrogen sulfide-releasing hybrid is a potent inhibitor of colon
cancer cell growth in vitro and in a xenograft mouse model. Biochem
Biophys Res Commun. 419:523–528. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
429
|
Edes K, Cassidy P, Shami PJ and Moos PJ:
JS-K, a nitric oxide prodrug, has enhanced cytotoxicity in colon
cancer cells with knockdown of thioredoxin reductase 1. PLoS One.
5:e87862010. View Article : Google Scholar : PubMed/NCBI
|
|
430
|
Ishikawa T, Yoshida N, Higashihara H,
Inoue M, Uchiyama K, Takagi T, Handa O, Kokura S, Naito Y, Okanoue
T and Yoshikawa T: Different effects of constitutive nitric oxide
synthase and heme oxygenase on pulmonary or liver metastasis of
colon cancer in mice. Clin Exp Metastasis. 20:445–450. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
431
|
Jarry A, Charrier L, Bou-Hanna C, Devilder
MC, Crussaire V, Denis MG, Vallette G and Laboisse CL: Position in
cell cycle controls the sensitivity of colon cancer cells to nitric
oxide-dependent programmed cell death. Cancer Res. 64:4227–4234.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
432
|
Jenkins DC, Charles IG, Baylis SA, Lelchuk
R, Radomski MW and Moncada S: Human colon cancer cell lines show a
diverse pattern of nitric oxide synthase gene expression and nitric
oxide generation. Br J Cancer. 70:847–849. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
433
|
Jeon HK, Choi SU and Jung NP: Association
of the ERK1/2 and p38 kinase pathways with nitric oxide-induced
apoptosis and cell cycle arrest in colon cancer cells. Cell Biol
Toxicol. 21:115–125. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
434
|
Kim MY: Sasa quelpaertensis Nakai extract
induces p53-independent apoptosis via the elevation of nitric oxide
production in human HCT116 colon cancer cells. Oncol Lett.
19:3027–3034. 2020.PubMed/NCBI
|
|
435
|
Kopecka J, Campia I, Brusa D, Doublier S,
Matera L, Ghigo D, Bosia A and Riganti C: Nitric oxide and
P-glycoprotein modulate the phagocytosis of colon cancer cells. J
Cell Mol Med. 15:1492–1504. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
436
|
Liu Q, Chan ST and Mahendran R: Nitric
oxide induces cyclooxygenase expression and inhibits cell growth in
colon cancer cell lines. Carcinogenesis. 24:637–642. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
437
|
Liu Q, Inoue H and Mahendran R:
Transcriptional regulation of the COX-2 expression by nitric oxide
in colon cancer cell lines. Oncol Rep. 19:269–274. 2008.PubMed/NCBI
|
|
438
|
Mojic M, Mijatovic S, Maksimovic-Ivanic D,
Miljkovic D, Stosic-Grujicic S, Stankovic M, Mangano K, Travali S,
Donia M, Fagone P, et al: Therapeutic potential of nitric
oxide-modified drugs in colon cancer cells. Mol Pharmacol.
82:700–710. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
439
|
Millet A, Bettaieb A, Renaud F, Prevotat
L, Hammann A, Solary E, Mignotte B and Jeannin JF: Influence of the
nitric oxide donor glyceryl trinitrate on apoptotic pathways in
human colon cancer cells. Gastroenterology. 123:235–246. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
440
|
Oláh G, Módis K, Törö G, Hellmich MR,
Szczesny B and Szabo C: Role of endogenous and exogenous nitric
oxide, carbon monoxide and hydrogen sulfide in HCT116 colon cancer
cell proliferation. Biochem Pharmacol. 149:186–204. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
441
|
Prevotat L, Filomenko R, Solary E, Jeannin
JF and Bettaieb A: Nitric oxide-induced down-regulation of
beta-catenin in colon cancer cells by a proteasome-independent
specific pathway. Gastroenterology. 131:1142–1152. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
442
|
Rao CV: Nitric oxide signaling in colon
cancer chemoprevention. Mutation Res. 555:107–119. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
443
|
Rao CV, Reddy BS, Steele VE, Wang CX, Liu
X, Ouyang N, Patlolla JM, Simi B, Kopelovich L and Rigas B: Nitric
oxide-releasing aspirin and indomethacin are potent inhibitors
against colon cancer in azoxymethane-treated rats: Effects on
molecular targets. Mol Cancer Ther. 5:1530–1538. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
444
|
Riganti C, Miraglia E, Viarisio D,
Costamagna C, Pescarmona G, Ghigo D and Bosia A: Nitric oxide
reverts the resistance to doxorubicin in human colon cancer cells
by inhibiting the drug efflux. Cancer Res. 65:516–525.
2005.PubMed/NCBI
|
|
445
|
Wang H and MacNaughton WK: Overexpressed
beta-catenin blocks nitric oxide-induced apoptosis in colonic
cancer cells. Cancer Res. 65:8604–8607. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
446
|
Xie J, Xia L, Xiang W, He W, Yin H, Wang
F, Gao T, Qi W, Yang Z, Yang X, et al: Metformin selectively
inhibits metastatic colorectal cancer with the KRAS mutation by
intracellular accumulation through silencing MATE1. Proc Natl Acad
Sci USA. 117:13012–13022. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
447
|
Wenzel U, Kuntz S, De Sousa UJ and Daniel
H: Nitric oxide suppresses apoptosis in human colon cancer cells by
scavenging mitochondrial superoxide anions. Int J Cancer.
106:666–675. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
448
|
Williams JL, Borgo S, Hasan I, Castillo E,
Traganos F and Rigas B: Nitric oxide-releasing nonsteroidal
anti-inflammatory drugs (NSAIDs) alter the kinetics of human colon
cancer cell lines more effectively than traditional NSAIDs:
Implications for colon cancer chemoprevention. Cancer Res.
61:3285–3289. 2001.PubMed/NCBI
|
|
449
|
Voss NCS, Kold-Petersen H and Boedtkjer E:
Enhanced nitric oxide signaling amplifies vasorelaxation of human
colon cancer feed arteries. Am J Physiol Heart Circ Physiol.
316:H245–H254. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
450
|
Tesei A, Rosetti M, Ulivi P, Fabbri F,
Medri L, Vannini I, Bolla M, Amadori D and Zoli W: Study of
molecular mechanisms of pro-apoptotic activity of NCX 4040, a novel
nitric oxide-releasing aspirin, in colon cancer cell lines. J
Transl Med. 5:522007. View Article : Google Scholar : PubMed/NCBI
|
|
451
|
Thomsen LL, Miles DW, Happerfield L,
Bobrow LG, Knowles RG and Moncada S: Nitric oxide synthase activity
in human breast cancer. Br J Cancer. 72:41–44. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
452
|
Stettner N, Rosen C, Bernshtein B,
Gur-Cohen S, Frug J, Silberman A, Sarver A, Carmel-Neiderman NN,
Eilam R, Biton I, et al: Induction of Nitric-Oxide metabolism in
enterocytes alleviates colitis and inflammation-associated colon
cancer. Cell Rep. 23:1962–1976. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
453
|
Ambs S, Bennett WP, Merriam WG, Ogunfusika
MO, Oser SM, Khan MA, Jones RT and Harris CC: Vascular endothelial
growth factor and nitric oxide synthase expression in human lung
cancer and the relation to p53. Br J Ccancer. 78:233–239. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
454
|
Cembrzynska-Nowak M, Bienkowska M and
Szklarz E: Exogenous interleukin 2 regulates interleukin 6 and
nitric oxide but not interferon gamma and tumor necrosis factor
alpha production in bronchoalveolar leukocytes from patients with
small cell lung cancer. Arch Immunol Ther Exp (Warsz). 46:367–374.
1998.PubMed/NCBI
|
|
455
|
Cembrzyńska-Nowak M, Bieńkowska M,
Weryńska B, Dyła T and Jankowska R: The contribution of endotoxins
present in the respiratory tract to overproduction of nitric oxide
associated with impaired interleukin 6 release in bronchoalveolar
leukocytes from lung cancer patients. Arch Immunol Ther Exp
(Warsz). 48:119–125. 2000.PubMed/NCBI
|
|
456
|
Chen Z, Huang KY, Ling Y, Goto M, Duan HQ,
Tong XH, Liu YL, Cheng YY, Morris-Natschke SL, Yang PC, et al:
Discovery of an Oleanolic Acid/Hederagenin-nitric oxide donor
hybrid as an EGFR tyrosine kinase inhibitor for non-small-cell lung
cancer. J Natural Prod. 82:3065–3073. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
457
|
Deliu Z, Tamas T, Chowdhury J, Aqil M,
Bassiony M and Radosevich JA: Expression of cross-tolerance to a
wide range of conditions in a human lung cancer cell line after
adaptation to nitric oxide. Tumour Biol. 39:10104283177237782017.
View Article : Google Scholar : PubMed/NCBI
|
|
458
|
Fu J, Han J, Meng T, Hu J and Yin J: Novel
α-ketoamide based diazeniumdiolates as hydrogen peroxide responsive
nitric oxide donors with anti-lung cancer activity. Chem Commun
(Camb). 55:12904–12907. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
459
|
Fujimoto H, Ando Y, Yamashita T, Terazaki
H, Tanaka Y, Sasaki J, Matsumoto M, Suga M and Ando M: Nitric oxide
synthase activity in human lung cancer. Jpn J Cancer Res.
88:1190–1198. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
460
|
Gao X, Xuan Y, Benner A, Anusruti A,
Brenner H and Schottker B: Nitric oxide metabolites and lung cancer
incidence: A matched case-control study nested in the ESTHER
cohort. Oxid Med Cell Longev. 2019:64709502019. View Article : Google Scholar : PubMed/NCBI
|
|
461
|
Hwang JH, Park SJ, Ko WG, Kang SM, Lee DB,
Bang J, Park BJ, Wee CB, Kim DJ, Jang IS and Ko JH: Cordycepin
induces human lung cancer cell apoptosis by inhibiting nitric oxide
mediated ERK/Slug signaling pathway. Am J Cancer Res. 7:417–432.
2017.PubMed/NCBI
|
|
462
|
Kaynar H, Meral M, Turhan H, Keles M,
Celik G and Akcay F: Glutathione peroxidase,
glutathione-S-transferase, catalase, xanthine oxidase, Cu-Zn
superoxide dismutase activities, total glutathione, nitric oxide,
and malondialdehyde levels in erythrocytes of patients with small
cell and non-small cell lung cancer. Cancer Lett. 227:133–139.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
463
|
Koizumi M, Yamazaki H, Toyokawa K,
Yoshioka Y, Suzuki G, Ito M, Shinkawa K, Nishino K, Watanabe Y,
Inoue T, et al: Influence of thoracic radiotherapy on exhaled
nitric oxide levels in patients with lung cancer. Jpn J Clin Oncol.
31:142–146. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
464
|
Munaweera I, Shi Y, Koneru B, Patel A,
Dang MH, Di Pasqua AJ and Balkus KJ Jr: Nitric oxide- and
cisplatin-releasing silica nanoparticles for use against non-small
cell lung cancer. J Inorg Biochem. 153:23–31. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
465
|
Maciag AE, Chakrapani H, Saavedra JE,
Morris NL, Holland RJ, Kosak KM, Shami PJ, Anderson LM and Keefer
LK: The nitric oxide prodrug JS-K is effective against
non-small-cell lung cancer cells in vitro and in vivo: Involvement
of reactive oxygen species. J Pharmacol Exp Ther. 336:313–320.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
466
|
Maiuthed A, Prakhongcheep O and
Chanvorachote P: Microarray-based analysis of genes, transcription
factors, and epigenetic modifications in lung cancer exposed to
nitric oxide. Cancer Genom Proteomics. 17:401–415. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
467
|
Lee JJ, Kwon HK, Lee DS, Lee SW, Lee KK,
Kim KJ and Kim JL: Mycelial extract of phellinus linteus induces
cell death in A549 lung cancer cells and elevation of nitric oxide
in raw 264.7 macrophage cells. Mycobiology. 34:143–147. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
468
|
Liaw YP, Ting TF, Ho CC and Chiou ZY: Cell
type specificity of lung cancer associated with nitric oxide. Sci
Total Environ. 408:4931–4934. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
469
|
Liu PF, Zhao DH, Qi Y, Wang JG, Zhao M,
Xiao K and Xie LX: The clinical value of exhaled nitric oxide in
patients with lung cancer. Clin Respir J. 12:23–30. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
470
|
Luanpitpong S and Chanvorachote P: Nitric
oxide and aggressive behavior of lung cancer cells. Anticancer Res.
35:4585–4592. 2015.PubMed/NCBI
|
|
471
|
Muto S, Takagi H, Owada Y, Inoue T,
Watanabe Y, Yamaura T, Fukuhara M, Okabe N, Matsumura Y, Hasegawa
T, et al: Serum nitric oxide as a predictive biomarker for
bevacizumab in non-small cell lung cancer patients. Anticancer Res.
37:3169–3174. 2017.PubMed/NCBI
|
|
472
|
Masri F: Role of nitric oxide and its
metabolites as potential markers in lung cancer. Ann Thorac Med.
5:123–127. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
473
|
Masri FA, Comhair SA, Koeck T, Xu W,
Janocha A, Ghosh S, Dweik RA, Golish J, Kinter M, Stuehr DJ, et al:
Abnormalities in nitric oxide and its derivatives in lung cancer.
Am J Respir Crit Care Med. 172:597–605. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
474
|
Matsunaga T, Yamaji Y, Tomokuni T, Morita
H, Morikawa Y, Suzuki A, Yonezawa A, Endo S, Ikari A, Iguchi K, et
al: Nitric oxide confers cisplatin resistance in human lung cancer
cells through upregulation of aldo-keto reductase 1B10 and
proteasome. Free Radical Res. 48:1371–1385. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
475
|
Powan P and Chanvorachote P: Nitric oxide
mediates cell aggregation and mesenchymal to epithelial transition
in anoikis-resistant lung cancer cells. Mol Cell Biochem.
393:237–245. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
476
|
Punathil T and Katiyar SK: Inhibition of
non-small cell lung cancer cell migration by grape seed
proanthocyanidins is mediated through the inhibition of nitric
oxide, guanylate cyclase, and ERK1/2. Mol Carcinog. 48:232–242.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
477
|
Zhou J, Zhu Q and Yao H: Chemotherapy of
non-small-cell lung cancer (NSCLC) and changes in serum sAPO-1/Fas
and nitric oxide (NO) levels. Zhonghua Zhong Liu Za Zhi.
22:225–227. 2000.(In Chinese). PubMed/NCBI
|
|
478
|
Zhou H, Dong Y, Ma X, Xu J and Xu S:
Development of a novel truncated deguelin derivative possessing
nitric oxide donor as a potential anti-lung cancer agent.
Fitoterapia. 146:1046702020. View Article : Google Scholar : PubMed/NCBI
|
|
479
|
Zhang L, Liu J, Wang X, Li Z, Zhang X, Cao
P, She X, Dai Q, Tang J and Liu Z: Upregulation of cytoskeleton
protein and extracellular matrix protein induced by stromal-derived
nitric oxide promotes lung cancer invasion and metastasis. Curr Mol
Med. 14:762–771. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
480
|
Yongsanguanchai N, Pongrakhananon V,
Mutirangura A, Rojanasakul Y and Chanvorachote P: Nitric oxide
induces cancer stem cell-like phenotypes in human lung cancer
cells. Am J Physiol Cell Physiol. 308:C89–C100. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
481
|
Wongvaranon P, Pongrakhananon V, Chunhacha
P and Chanvorachote P: Acquired resistance to chemotherapy in lung
cancer cells mediated by prolonged nitric oxide exposure.
Anticancer Res. 33:5433–5444. 2013.PubMed/NCBI
|
|
482
|
Saisongkorh V, Maiuthed A and
Chanvorachote P: Nitric oxide increases the migratory activity of
non-small cell lung cancer cells via AKT-mediated integrin αv and
β1 upregulation. Cell Oncol (Dordr). 39:449–462. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
483
|
Saleem W, Suzuki Y, Mobaraki A, Yoshida Y,
Noda S, Saitoh JI and Nakano T: Reduction of nitric oxide level
enhances the radiosensitivity of hypoxic non-small cell lung
cancer. Cancer Sci. 102:2150–2156. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
484
|
Sanuphan A, Chunhacha P, Pongrakhananon V
and Chanvorachote P: Long-term nitric oxide exposure enhances lung
cancer cell migration. Biomed Res Int. 2013:1869722013. View Article : Google Scholar : PubMed/NCBI
|
|
485
|
Sanuphan A, Chunhacha P, Pongrakhananon V
and Chanvorachote P: Corrigendum to ‘Long-term nitric oxide
exposure enhances lung cancer cell migration’. Biomed Res Int.
2015:3106362015. View Article : Google Scholar : PubMed/NCBI
|
|
486
|
Su X, Takahashi A, Guo G, Mori E, Okamoto
N, Ohnishi K, Iwasaki T and Ohnishi T: Biphasic effects of nitric
oxide radicals on radiation-induced lethality and chromosome
aberrations in human lung cancer cells carrying different p53 gene
status. Int J Radiat Oncol Biol Phys. 77:559–565. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
487
|
Suzuki Y, Inui N, Karayama M, Imokawa S,
Yamada T, Yokomura K, Asada K, Kusagaya H, Kaida Y, Matsuda H, et
al: Effect of PD-1 inhibitor on exhaled nitric oxide and pulmonary
function in non-small cell lung cancer patients with and without
COPD. Int J Chron Obstruct Pulmon Dis. 14:1867–1877. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
488
|
Szejniuk WM, Nielsen MS, Brønnum D,
Takács-Szabó Z, Weinreich UM, Pilegaard Thomsen L, Bøgsted M,
Jensen I, McCulloch T, Falkmer UG, et al: Fractional exhaled nitric
oxide as a potential biomarker for radiation pneumonitis in
patients with non-small cell lung cancer: A pilot study. Clin
Transl Radiat Oncol. 19:103–109. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
489
|
Arif M, Vedamurthy BM, Choudhari R, Ostwal
YB, Mantelingu K, Kodaganur GS and Kundu TK: Nitric oxide-mediated
histone hyperacetylation in oral cancer: Target for a water-soluble
HAT inhibitor, CTK7A. Chem Biol. 17:903–913. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
490
|
Beevi SS, Rasheed AM and Geetha A:
Evaluation of oxidative stress and nitric oxide levels in patients
with oral cavity cancer. Jpn J Clin Oncol. 34:379–385. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
491
|
Korde Choudhari S, Sridharan G, Gadbail A
and Poornima V: Nitric oxide and oral cancer: A review. Oral Oncol.
48:475–483. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
492
|
Patel JB, Shah FD, Shukla SN, Shah PM and
Patel PS: Role of nitric oxide and antioxidant enzymes in the
pathogenesis of oral cancer. J Cancer Res Ther. 5:247–253. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
493
|
Brankovic B, Stanojevic G, Stojanovic I,
Veljkovic A, Kocic G, Janosevic P, Nestorovic M, Petrovic D,
Djindjic B, Pavlovic D and Krivokapic Z: Nitric oxide synthesis
modulation-a possible diagnostic and therapeutic target in
colorectal cancer. J BUON. 22:162–169. 2017.PubMed/NCBI
|
|
494
|
El-Mezayen HA, Toson el SA, Darwish H and
El-Badry E: Discriminant function based on parameters of hyaluronic
acid metabolism and nitric oxide to differentiate metastatic from
non-metastatic colorectal cancer patients. Tumour Biol.
33:995–1004. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
495
|
Gao Y, Zhou S, Pang L, Yang J, Li HJ, Huo
X and Qian SY: Celastrol suppresses nitric oxide synthases and the
angiogenesis pathway in colorectal cancer. Free Radic Res.
53:324–334. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
496
|
Gao Y, Zhou S, Xu Y, Sheng S, Qian SY and
Huo X: Nitric oxide synthase inhibitors 1400W and L-NIO inhibit
angiogenesis pathway of colorectal cancer. Nitric Oxide. 83:33–39.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
497
|
Jiang H, Verovski VN, Leonard W, Law KL,
Vermeersch M, Storme G, Van den Berge D, Gevaert T, Sermeus A and
De Ridder M: Hepatocytes determine the hypoxic microenvironment and
radiosensitivity of colorectal cancer cells through production of
nitric oxide that targets mitochondrial respiration. Int J Radiat
Oncol Biol Phys. 85:820–827. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
498
|
Krzystek-Korpacka M, Szczęśniak-Sięga B,
Szczuka I, Fortuna P, Zawadzki M, Kubiak A, Mierzchała-Pasierb M,
Fleszar MG, Lewandowski Ł, Serek P, et al: L-Arginine/Nitric oxide
pathway is altered in colorectal cancer and can be modulated by
novel derivatives from oxicam class of non-steroidal
anti-inflammatory drugs. Cancers (Basel). 12:25942020. View Article : Google Scholar : PubMed/NCBI
|
|
499
|
Liu Y, Borchert GL and Phang JM: Polyoma
enhancer activator 3, an ets transcription factor, mediates the
induction of cyclooxygenase-2 by nitric oxide in colorectal cancer
cells. J Biol Chemistry. 279:18694–18700. 2004. View Article : Google Scholar
|
|
500
|
McIlhatton MA, Tyler J, Burkholder S,
Ruschoff J, Rigas B, Kopelovich L and Fishel R: Nitric
oxide-donating aspirin derivatives suppress microsatellite
instability in mismatch repair-deficient and hereditary
nonpolyposis colorectal cancer cells. Cancer Res. 67:10966–10975.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
501
|
Moochhala S, Chhatwal VJ, Chan ST, Ngoi
SS, Chia YW and Rauff A: Nitric oxide synthase activity and
expression in human colorectal cancer. Carcinogenesis.
17:1171–1174. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
502
|
Muscat JE, Dyer AM, Rosenbaum RE and Rigas
B: Nitric oxide-releasing medications and colorectal cancer risk:
The framingham study. Anticancer Res. 25:4471–4474. 2005.PubMed/NCBI
|
|
503
|
Mandal P: Molecular signature of nitric
oxide on major cancer hallmarks of colorectal carcinoma.
Inflammopharmacology. 26:331–336. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
504
|
Yagihashi N, Kasajima H, Sugai S,
Matsumoto K, Ebina Y, Morita T, Murakami T and Yagihashi S:
Increased in situ expression of nitric oxide synthase in human
colorectal cancer. Virchows Archiv. 436:109–114. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
505
|
Yu LB, Dong XS, Sun WZ, Zhao DL and Yang
Y: Effect of a nitric oxide synthase inhibitor NG-nitro-L-arginine
methyl ester on invasion of human colorectal cancer cell line
SL-174T. World J Gastroenterol. 11:6385–6388. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
506
|
Wei B, Wei HB, Qi CL, Han XY and Wang TB:
Effect of a selective inducible nitric oxide synthase inhibitor on
cell growth in human colorectal cancer Lovo cell line. Zhonghua Wei
Chang Wai Ke Za Zhi. 11:280–283. 2008.(In Chinese). PubMed/NCBI
|
|
507
|
Siedlar M, Mytar B, Hyszko M and Zembala
M: Involvement of protein kinases in signalling for nitric oxide
(NO) and tumour necrosis factor alpha (TNF) production by monocytes
stimulated with colorectal DeTa cancer cells: The lack of evidence
for the role of TNF in the regulation of NO production. Immunol
Lett. 65:189–195. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
508
|
Atala A: Re: Alterations of tumor
microenvironment by nitric oxide impedes castration-resistant
prostate cancer growth. J Urol. 202:35–36. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
509
|
Dillioglugil MO, Mekik H, Muezzinoglu B,
Ozkan TA, Demir CG and Dillioglugil O: Blood and tissue nitric
oxide and malondialdehyde are prognostic indicators of localized
prostate cancer. Int Urol Nephrol. 44:1691–1696. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
510
|
Della Pietra E, Simonella F, Bonavida B,
Xodo LE and Rapozzi V: Repeated sub-optimal photodynamic treatments
with pheophorbide a induce an epithelial mesenchymal transition in
prostate cancer cells via nitric oxide. Nitric Oxide. 45:43–53.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
511
|
Huh J, Liepins A, Zielonka J,
Andrekopoulos C, Kalyanaraman B and Sorokin A: Cyclooxygenase 2
rescues LNCaP prostate cancer cells from sanguinarine-induced
apoptosis by a mechanism involving inhibition of nitric oxide
synthase activity. Cancer Res. 66:3726–3736. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
512
|
Lee KM, Kang D, Park SK, Berndt SI, Reding
D, Chatterjee N, Chanock S, Huang WY and Hayes RB: Nitric oxide
synthase gene polymorphisms and prostate cancer risk.
Carcinogenesis. 30:621–625. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
513
|
Rezakhani L, Khazaei MR, Ghanbari A and
Khazaei M: Crab shell extract induces prostate cancer cell line
(LNcap) apoptosis and decreases nitric oxide secretion. Cell J.
19:231–237. 2017.PubMed/NCBI
|
|
514
|
Royle JS, Ross JA, Ansell I, Bollina P,
Tulloch DN and Habib FK: Nitric oxide donating nonsteroidal
anti-inflammatory drugs induce apoptosis in human prostate cancer
cell systems and human prostatic stroma via caspase-3. J Urol.
172:338–344. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
515
|
Wang D, Lu S and Dong Z: Regulation of
TGF-beta1 gene transcription in human prostate cancer cells by
nitric oxide. Prostate. 67:1825–1833. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
516
|
Tan G, Qiu M, Chen L, Zhang S, Ke L and
Liu J: JS-K, a nitric oxide pro-drug, regulates growth and
apoptosis through the ubiquitin-proteasome pathway in prostate
cancer cells. BMC Cancer. 17:3762017. View Article : Google Scholar : PubMed/NCBI
|
|
517
|
Thomas LN, Morehouse TJ and Too CK:
Testosterone and prolactin increase carboxypeptidase-D and nitric
oxide levels to promote survival of prostate cancer cells.
Prostate. 72:450–460. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
518
|
Siemens DR, Heaton JP, Adams MA, Kawakami
J and Graham CH: Phase II study of nitric oxide donor for men with
increasing prostate-specific antigen level after surgery or
radiotherapy for prostate cancer. Urology. 74:878–883. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
519
|
Soni Y, Softness K, Arora H and Ramasamy
R: The Yin yang role of nitric oxide in prostate cancer. Am J Mens
Health. 14:15579883209031912020. View Article : Google Scholar : PubMed/NCBI
|
|
520
|
Caneba CA, Yang L, Baddour J, Curtis R,
Win J, Hartig S, Marini J and Nagrath D: Nitric oxide is a positive
regulator of the Warburg effect in ovarian cancer cells. Cell Death
Dis. 5:e13022014. View Article : Google Scholar : PubMed/NCBI
|
|
521
|
El-Sehemy A, Chang AC, Azad AK, Gupta N,
Xu Z, Steed H, Karsan A and Fu Y: Notch activation augments nitric
oxide/soluble guanylyl cyclase signaling in immortalized ovarian
surface epithelial cells and ovarian cancer cells. Cell Signal.
25:2780–2787. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
522
|
El-Sehemy A, Postovit LM and Fu Y: Nitric
oxide signaling in human ovarian cancer: A potential therapeutic
target. Nitric Oxide. 54:30–37. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
523
|
Kielbik M, Klink M, Brzezinska M, Szulc I
and Sulowska Z: Nitric oxide donors: Spermine/NO and
diethylenetriamine/NO induce ovarian cancer cell death and affect
STAT3 and AKT signaling proteins. Nitric Oxide. 35:93–109. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
524
|
Leung EL, Fraser M, Fiscus RR and Tsang
BK: Cisplatin alters nitric oxide synthase levels in human ovarian
cancer cells: Involvement in p53 regulation and cisplatin
resistance. Br J Cancer. 98:1803–1809. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
525
|
Thomsen LL, Sargent JM, Williamson CJ and
Elgie AW: Nitric oxide synthase activity in fresh cells from
ovarian tumour tissue: Relationship of enzyme activity with
clinical parameters of patients with ovarian cancer. Biochem
Pharmacol. 56:1365–1370. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
526
|
Salimian Rizi B, Caneba C, Nowicka A,
Nabiyar AW, Liu X, Chen K, Klopp A and Nagrath D: Nitric oxide
mediates metabolic coupling of omentum-derived adipose stroma to
ovarian and endometrial cancer cells. Cancer Res. 75:456–471. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
527
|
Stevens EV, Carpenter AW, Shin JH, Liu J,
Der CJ and Schoenfisch MH: Nitric oxide-releasing silica
nanoparticle inhibition of ovarian cancer cell growth. Mol Pharm.
7:775–785. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
528
|
Camp ER, Yang A, Liu W, Fan F, Somcio R,
Hicklin DJ and Ellis LM: Roles of nitric oxide synthase inhibition
and vascular endothelial growth factor receptor-2 inhibition on
vascular morphology and function in an in vivo model of pancreatic
cancer. Clin Cancer Res. 12:2628–2633. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
529
|
Chen X, Jia F, Li Y, Deng Y, Huang Y, Liu
W, Jin Q and Ji J: Nitric oxide-induced stromal depletion for
improved nanoparticle penetration in pancreatic cancer treatment.
Biomaterials. 246:1199992020. View Article : Google Scholar : PubMed/NCBI
|
|
530
|
Fujita M, Imadome K, Endo S, Shoji Y,
Yamada S and Imai T: Nitric oxide increases the invasion of
pancreatic cancer cells via activation of the PI3K-AKT and RhoA
pathways after carbon ion irradiation. FEBS Lett. 588:3240–3250.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
531
|
Fujita M, Somasundaram V, Basudhar D,
Cheng RYS, Ridnour LA, Higuchi H, Imadome K, No JH, Bharadwaj G and
Wink DA: Role of nitric oxide in pancreatic cancer cells exhibiting
the invasive phenotype. Redox Biol. 22:1011582019. View Article : Google Scholar : PubMed/NCBI
|
|
532
|
Zhou H, Huang L, Sun Y and Rigas B: Nitric
oxide-donating aspirin inhibits the growth of pancreatic cancer
cells through redox-dependent signaling. Cancer Lett. 273:292–299.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
533
|
Wang B, Wei D, Crum VE, Richardson EL,
Xiong HH, Luo Y, Huang S, Abbruzzese JL and Xie K: A novel model
system for studying the double-edged roles of nitric oxide
production in pancreatic cancer growth and metastasis. Oncogene.
22:1771–1782. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
534
|
Wang L and Xie K: Nitric oxide and
pancreatic cancer pathogenesis, prevention, and treatment. Curr
Pharm Design. 16:421–427. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
535
|
Thomas WJ, Thomas DL, Knezetic JA and
Adrian TE: The role of oxygen-derived free radicals and nitric
oxide in cytokine-induced antiproliferation of pancreatic cancer
cells. Pancreas. 24:161–168. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
536
|
Stewart GD, Nanda J, Katz E, Bowman KJ,
Christie JG, Brown DJ, McLaren DB, Riddick AC, Ross JA, Jones GD
and Habib FK: DNA strand breaks and hypoxia response inhibition
mediate the radiosensitisation effect of nitric oxide donors on
prostate cancer under varying oxygen conditions. Biochem Pharmacol.
81:203–210. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
537
|
Sugita H, Kaneki M, Furuhashi S, Hirota M,
Takamori H and Baba H: Nitric oxide inhibits the proliferation and
invasion of pancreatic cancer cells through degradation of insulin
receptor substrate-1 protein. Mol Cancer Res. 8:1152–1163. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
538
|
Caygill CP, Royston C, Charlett A, Wall
CM, Gatenby PA, Ramus JR, Watson A, Winslet M, Hourigan CS and Dev
Bardhan K: Barrett's, blood groups and progression to oesophageal
cancer: Is nitric oxide the link? Eur J Gastroenterol Hepatol.
23:801–806. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
539
|
Sun GG, Hu WN, Zhang J, Li CL and Yang CR:
Effect of nitric oxide on esophageal cancer cell line TE-1. Chin
Med Sci J. 28:44–49. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
540
|
Gecit I, Aslan M, Gunes M, Pirincci N,
Esen R, Demir H and Ceylan K: Serum prolidase activity, oxidative
stress, and nitric oxide levels in patients with bladder cancer. J
Cancer Res Clin Oncol. 138:739–743. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
541
|
Gecit İ, Eryılmaz R, Kavak S, Meral İ,
Demir H, Pirinççi N, Güneş M and Taken K: The prolidase activity,
oxidative stress, and nitric oxide levels of bladder tissues with
or without tumor in patients with bladder cancer. J Membr Biol.
250:455–459. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
542
|
Jansson OT, Morcos E, Brundin L, Lundberg
JO, Adolfsson J, Söderhäll M and Wiklund NP: The role of nitric
oxide in bacillus Calmette-Guerin mediated anti-tumour effects in
human bladder cancer. Br J Cancer. 78:588–592. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
543
|
Kilic S, Bayraktar N, Beytur A, Ergin H,
Bayraktar M and Egri M: Can the levels of nitric oxide in the
urine, serum and tumor tissue be putative markers for bladder
cancer? Int J Urol. 13:1079–1085. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
544
|
Khalifa A, Eissa S and Aziz A:
Determination of cytosolic citrulline and nitrate as indicators of
nitric oxide in bladder cancer: Possible association with basic
fibroblast growth factor. Clin Biochem. 32:635–638. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
545
|
Morcos E, Jansson OT, Adolfsson J, Kratz G
and Wiklund NP: Endogenously formed nitric oxide modulates cell
growth in bladder cancer cell lines. Urology. 53:1252–1257. 1999.
View Article : Google Scholar : PubMed/NCBI
|
|
546
|
Wang Z, Fu S, Chen Y and Qin D: Modulation
of nitric oxide on lymphokine-activated killer cells in patients
with bladder cancer. Chin Med Sci J. 16:2132001.PubMed/NCBI
|
|
547
|
Thiel T, Ryk C, Chatzakos V, Hallén
Grufman K, Bavand-Chobot N, Flygare J, Wiklund NP and de Verdier
PJ: Secondary stimulation from Bacillus Calmette-Guerin induced
macrophages induce nitric oxide independent cell-death in bladder
cancer cells. Cancer Lett. 348:119–125. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
548
|
Saygili EI, Akcay T, Dincer Y, Obek C,
Kural AR and Cakalir C: Methylguanine DNA methyl transferase
activities, glutathione s transferase and nitric oxide in bladder
cancer patients. Cancer Invest. 24:256–260. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
549
|
Bakan E, Taysi S, Polat MF, Dalga S,
Umudum Z, Bakan N and Gumus M: Nitric oxide levels and lipid
peroxidation in plasma of patients with gastric cancer. Jap J Clin
Oncol. 32:162–166. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
550
|
Dincer Y, Akcay T, Tortum OB and Dogusoy
G: Nitric oxide and antioxidant defense in patients with gastric
cancer. Dig Dis Sci. 51:1367–1370. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
551
|
Holian O, Wahid S, Atten MJ and Attar BM:
Inhibition of gastric cancer cell proliferation by resveratrol:
Role of nitric oxide. Am J Physiol Gastrointest Liver Physiol.
282:G809–G816. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
552
|
Eroğlu A, Demirci S, Ayyildiz A, Kocaoğlu
H, Akbulut H, Akgül H and Elhan HA: Serum concentrations of
vascular endothelial growth factor and nitrite as an estimate of in
vivo nitric oxide in patients with gastric cancer. Br J Cancer.
80:1630–1634. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
553
|
Koh E, Noh SH, Lee YD, Lee HY, Han JW, Lee
HW and Hong S: Differential expression of nitric oxide synthase in
human stomach cancer. Cancer Lett. 146:173–180. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
554
|
Oshima T, Imada T, Nagashima Y, Cho H,
Shiozawa M, Rino Y and Takanashi Y: Role of nitric oxide in human
gastric cancer cells treated with 5-fluorouracil. Oncol Rep.
8:847–849. 2001.PubMed/NCBI
|
|
555
|
Rajnakova A, Goh PM, Chan ST, Ngoi SS,
Alponat A and Moochhala S: Expression of differential nitric oxide
synthase isoforms in human normal gastric mucosa and gastric cancer
tissue. Carcinogenesis. 18:1841–1845. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
556
|
Yao X, Wu Y, Zhu M, Qian H and Chen Y:
Nitric oxide/cyclic guanosine monophosphate inducers sodium
nitroprusside and L-arginine inhibit the proliferation of gastric
cancer cells via the activation of type II cyclic guanosine
monophosphate-dependent protein kinase. Oncol Lett. 10:479–484.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
557
|
Sang J, Chen Y and Tao Y: Nitric oxide
inhibits gastric cancer cell growth through the modulation of the
Akt pathway. Mol Med Rep. 4:1163–1167. 2011.PubMed/NCBI
|
|
558
|
Sang JR, Chen YC, Shao GB and Huang XJ:
Effect of nitric oxide on the proliferation of AGS gastric cancer
cells. Chin J Cancer. 29:158–162. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
559
|
Li YH, Guo M, Shi SW, Zhang QL, Yang SP
and Liu JG: A ruthenium-nitrosyl-functionalized nanoplatform for
the targeting of liver cancer cells and NIR-light-controlled
delivery of nitric oxide combined with photothermal therapy. J
Mater Chem B. 5:7831–7838. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
560
|
Muntane J, De la Rosa AJ, Marin LM and
Padillo FJ: Nitric oxide and cell death in liver cancer cells.
Mitochondrion. 13:257–262. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
561
|
Sayed-Ahmad MM and Mohamad MA:
Contribution of nitric oxide and epidermal growth factor receptor
in anti-metastatic potential of paclitaxel in human liver cancer
cell (HebG2). J Egypt Natl Canc Inst. 17:35–41. 2005.PubMed/NCBI
|
|
562
|
Li J, Rao H, Jin C and Liu J: Involvement
of the Toll-like receptor/Nitric oxide signaling pathway in the
pathogenesis of cervical cancer caused by high-risk human
papillomavirus infection. Biomed Res Int.
2017:78302622017.PubMed/NCBI
|
|
563
|
Park IC, Woo SH, Park MJ, Lee HC, Lee SJ,
Hong YJ, Lee SH, Hong SI and Rhee CH: Ionizing radiation and nitric
oxide donor sensitize Fas-induced apoptosis via up-regulation of
Fas in human cervical cancer cells. Oncol Rep. 10:629–633.
2003.PubMed/NCBI
|
|
564
|
Wei XM, Wang Q, Gao SJ and Sui L:
Relationship between nitric oxide in cervical microenvironment and
different HPV types and effect on cervical cancer cells. Zhonghua
Fu Chan Ke Za Zhi. 46:260–265. 2011.(In Chinese). PubMed/NCBI
|
|
565
|
Sudhesh P, Tamilarasan K, Arumugam P and
Berchmans S: Nitric oxide releasing photoresponsive nanohybrids as
excellent therapeutic agent for cervical cancer cell lines. ACS
Appl Mater Interfaces. 5:8263–8266. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
566
|
Sundaram MK, Khan MA, Alalami U, Somvanshi
P, Bhardwaj T, Pramodh S, Raina R, Shekfeh Z, Haque S and Hussain
A: Phytochemicals induce apoptosis by modulation of nitric oxide
signaling pathway in cervical cancer cells. Eur Rev Med Pharmacol
Sci. 24:11827–11844. 2020.PubMed/NCBI
|
|
567
|
Menendez L, Juarez L, Garcia V, Hidalgo A
and Baamonde A: Involvement of nitric oxide in the inhibition of
bone cancer-induced hyperalgesia through the activation of
peripheral opioid receptors in mice. Neuropharmacology. 53:71–80.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
568
|
Yang Y, Zhang J, Liu Y, Zheng Y, Bo J,
Zhou X, Wang J and Ma Z: Role of nitric oxide synthase in the
development of bone cancer pain and effect of L-NMMA. Mol Med Rep.
13:1220–1226. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
569
|
Giusti M, Valenti S, Guazzini B, Molinari
E, Cavallero D, Augeri C and Minuto F: Circulating nitric oxide is
modulated by recombinant human TSH administration during monitoring
of thyroid cancer remnant. J Endocrinol Invest. 26:1192–1197. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
570
|
Ragot T, Provost C, Prignon A, Cohen R,
Lepoivre M and Lausson S: Apoptosis induction by combination of
drugs or a conjugated molecule associating non-steroidal
anti-inflammatory and nitric oxide donor effects in medullary
thyroid cancer models: Implication of the tumor suppressor p73.
Thyroid Res. 8:132015. View Article : Google Scholar : PubMed/NCBI
|
|
571
|
Gallo O, Masini E, Morbidelli L, Franchi
A, Fini-Storchi I, Vergari WA and Ziche M: Role of nitric oxide in
angiogenesis and tumor progression in head and neck cancer. J Natl
Cancer Inst. 90:587–596. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
572
|
Kawakami K, Kawakami M and Puri RK: Nitric
oxide accelerates interleukin-13 cytotoxin-mediated regression in
head and neck cancer animal model. Clin Cancer Res. 10:5264–5270.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
573
|
Wu HL, Chu YH, Tai YH, Tsou MY, Wu CH, Lo
WL, Tai SK, Yeh CC and Lu CC: Stage-dependent angiopoietin-Tie2 and
nitric oxide signaling of erythrocytes in response to surgical
trauma in head and neck cancer. World J Surg Oncol. 18:2092020.
View Article : Google Scholar : PubMed/NCBI
|
|
574
|
Utispan K and Koontongkaew S: High nitric
oxide adaptation in isogenic primary and metastatic head and neck
cancer cells. Anticancer Res. 40:2657–2665. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
575
|
Taysi S, Uslu C, Akcay F and Sutbeyaz MY:
Malondialdehyde and nitric oxide levels in the plasma of patients
with advanced laryngeal cancer. Surg Today. 33:651–654. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
576
|
Sanhueza C, Araos J, Naranjo L, Barros E,
Subiabre M, Toledo F, Gutiérrez J, Chiarello DI, Pardo F, Leiva A
and Sobrevia L: Nitric oxide and pH modulation in gynaecological
cancer. J Cell Mol Med. 20:2223–2230. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
577
|
Chattopadhyay M, Kodela R, Nath N,
Barsegian A, Boring D and Kashfi K: Hydrogen sulfide-releasing
aspirin suppresses NF-κB signaling in estrogen receptor negative
breast cancer cells in vitro and in vivo. Biochem Pharmacol.
83:723–732. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
578
|
Dong Q, Yang B, Han JG, Zhang MM, Liu W,
Zhang X, Yu HL, Liu ZG, Zhang SH, Li T, et al: A novel hydrogen
sulfide-releasing donor, HA-ADT, suppresses the growth of human
breast cancer cells through inhibiting the PI3K/AKT/mTOR and
Ras/Raf/MEK/ERK signaling pathways. Cancer Lett. 455:60–72. 2019.
View Article : Google Scholar : PubMed/NCBI
|
|
579
|
Li Y, Zhou J, Wang L and Xie Z: Endogenous
hydrogen sulfide-triggered MOF-based nanoenzyme for synergic cancer
therapy. ACS Appl Mater Interfaces. 12:30213–30220. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
580
|
Lv M, Li Y, Ji MH, Zhuang M and Tang JH:
Inhibition of invasion and epithelial-mesenchymal transition of
human breast cancer cells by hydrogen sulfide through decreased
phospho-p38 expression. Mol Med Rep. 10:341–346. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
581
|
Choi KS, Song H, Kim EH, Choi JH, Hong H,
Han YM and Hahm KB: Inhibition of Hydrogen Sulfide-induced
angiogenesis and inflammation in vascular endothelial cells:
Potential mechanisms of gastric cancer prevention by korean red
ginseng. J Ginseng Res. 36:135–145. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
582
|
Kawahara Y, Hirashita Y, Tamura C, Kudo Y,
Sakai K, Togo K, Fukuda K, Matsunari O, Okamoto K, Ogawa R, et al:
Helicobacter pylori infection modulates endogenous hydrogen
sulfide production in gastric cancer AGS cells. Helicobacter.
25:e127322020. View Article : Google Scholar : PubMed/NCBI
|
|
583
|
Sekiguchi F, Sekimoto T, Ogura A and
Kawabata A: Endogenous hydrogen sulfide enhances cell proliferation
of human gastric cancer AGS cells. Biol Pharm Bull. 39:887–890.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
584
|
Wang R, Tao B, Fan Q, Wang S, Chen L,
Zhang J, Hao Y, Dong S, Wang Z, Wang W, et al: Fatty-acid receptor
CD36 functions as a hydrogen sulfide-targeted receptor with its
Cys333-Cys272 disulfide bond serving as a specific molecular switch
to accelerate gastric cancer metastasis. EBioMedicine. 45:108–123.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
585
|
Ye F, Li X, Sun K, Xu W, Shi H, Bian J, Lu
R and Ye Y: Inhibition of endogenous hydrogen sulfide biosynthesis
enhances the anti-cancer effect of 3,3′-diindolylmethane in human
gastric cancer cells. Life Sci. 261:1183482020. View Article : Google Scholar : PubMed/NCBI
|
|
586
|
Chen S, Yue T, Huang Z, Zhu J, Bu D, Wang
X, Pan Y, Liu Y and Wang P: Inhibition of hydrogen sulfide
synthesis reverses acquired resistance to 5-FU through
miR-215-5p-EREG/TYMS axis in colon cancer cells. Cancer Lett.
466:49–60. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
587
|
Cai WJ, Wang MJ, Ju LH, Wang C and Zhu YC:
Hydrogen sulfide induces human colon cancer cell proliferation:
Role of Akt, ERK and p21. Cell Biol Int. 34:565–572. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
588
|
Hale VL, Jeraldo P, Mundy M, Yao J, Keeney
G, Scott N, Cheek EH, Davidson J, Greene M, Martinez C, et al:
Synthesis of multi-omic data and community metabolic models reveals
insights into the role of hydrogen sulfide in colon cancer.
Methods. 149:59–68. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
589
|
Hong M, Tang X and He K: Effect of
hydrogen sulfide on human colon cancer SW480 cell proliferation and
migration in vitro. Nan Fang Yi Ke Da Xue Xue Bao. 34:699–703.
2014.(In Chinese). PubMed/NCBI
|
|
590
|
Kodela R, Nath N, Chattopadhyay M, Nesbitt
DE, Velázquez-Martínez CA and Kashfi K: Hydrogen sulfide-releasing
naproxen suppresses colon cancer cell growth and inhibits NF-κB
signaling. Drug Design Dev Ther. 9:4873–4882. 2015.PubMed/NCBI
|
|
591
|
Chen S, Wang P and Liu Y: Research
progress of the association of hydrogen sulfide with colorectal
cancer and its associated anti-tumor drugs. Zhonghua Wei Chang Wai
Ke Za Zhi. 20:834–840. 2017.(In Chinese). PubMed/NCBI
|
|
592
|
Elsheikh W, Blackler RW, Flannigan KL and
Wallace JL: Enhanced chemopreventive effects of a hydrogen
sulfide-releasing anti-inflammatory drug (ATB-346) in experimental
colorectal cancer. Nitric Oxide. 41:131–137. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
593
|
Faris P, Ferulli F, Vismara M, Tanzi M,
Negri S, Rumolo A, Lefkimmiatis K, Maestri M, Shekha M, Pedrazzoli
P, et al: Hydrogen Sulfide-evoked intracellular Ca2+
signals in primary cultures of metastatic colorectal cancer cells.
Cancers (Basel). 12:33382020. View Article : Google Scholar : PubMed/NCBI
|
|
594
|
Malagrinò F, Zuhra K, Mascolo L,
Mastronicola D, Vicente JB, Forte E and Giuffrè A: Hydrogen sulfide
oxidation: Adaptive changes in mitochondria of SW480 colorectal
cancer cells upon exposure to hypoxia. Oxid Med Cell Longev.
2019:81029362019. View Article : Google Scholar : PubMed/NCBI
|
|
595
|
Sakuma S, Minamino S, Takase M, Ishiyama
Y, Hosokura H, Kohda T, Ikeda Y and Fujimoto Y: Hydrogen sulfide
donor GYY4137 suppresses proliferation of human colorectal cancer
Caco-2 cells by inducing both cell cycle arrest and cell death.
Heliyon. 5:e022442019. View Article : Google Scholar : PubMed/NCBI
|
|
596
|
Liu H, Chang J, Zhao Z, Li Y and Hou J:
Effects of exogenous hydrogen sulfide on the proliferation and
invasion of human Bladder cancer cells. J Cancer Res Ther.
13:829–832. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
597
|
Liu M, Wu L, Montaut S and Yang G:
Hydrogen sulfide signaling axis as a target for prostate cancer
therapeutics. Prostate Cancer. 2016:81085492016. View Article : Google Scholar : PubMed/NCBI
|
|
598
|
Zhang S, Bian H, Li X, Wu H, Bi Q, Yan Y
and Wang Y: Hydrogen sulfide promotes cell proliferation of oral
cancer through activation of the COX2/AKT/ERK1/2 axis. Oncol Rep.
35:2825–2832. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
599
|
Zhuang L, Li K, Wang G, Shou T, Gao C, Mao
Y, Bao M and Zhao M: Preconditioning with hydrogen sulfide prevents
bone cancer pain in rats through a proliferator-activated receptor
gamma/p38/Jun N-terminal kinase pathway. Exp Biol Med (Maywood).
243:57–65. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
600
|
Xu Y, Ma N, Wei P, Zeng Z and Meng J:
Expression of hydrogen sulfide synthases and Hh signaling pathway
components correlate with the clinicopathological characteristics
of papillary thyroid cancer patients. Int J Clin Exp Pathol.
11:1818–1824. 2018.PubMed/NCBI
|
|
601
|
Huang CC, Ho CH, Chen YC, Hsu CC, Lin HJ,
Tian YF, Wang JJ and Guo HR: Impact of carbon monoxide poisoning on
the risk of breast cancer. Sci Rep. 10:204502020. View Article : Google Scholar : PubMed/NCBI
|
|
602
|
Kawahara B, Moller T, Hu-Moore K,
Carrington S, Faull KF, Sen S and Mascharak PK: Attenuation of
antioxidant capacity in human breast cancer cells by carbon
monoxide through inhibition of cystathionine β-synthase activity:
Implications in chemotherapeutic drug sensitivity. J Med Chem.
60:8000–8010. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
603
|
Kim DH, Yoon HJ, Cha YN and Surh YJ: Role
of heme oxygenase-1 and its reaction product, carbon monoxide, in
manifestation of breast cancer stem cell-like properties: Notch-1
as a putative target. Free Radical Res. 52:1336–1347. 2018.
View Article : Google Scholar : PubMed/NCBI
|
|
604
|
Kourti M, Westwell A, Jiang W and Cai J:
Repurposing old carbon monoxide-releasing molecules towards the
anti-angiogenic therapy of triple-negative breast cancer.
Oncotarget. 10:1132–1148. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
605
|
Lee WY, Chen YC, Shih CM, Lin CM, Cheng
CH, Chen KC and Lin CW: The induction of heme oxygenase-1
suppresses heat shock protein 90 and the proliferation of human
breast cancer cells through its byproduct carbon monoxide. Toxicol
Appl Pharmacol. 274:55–62. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
606
|
Kawahara B, Gao L, Cohn W, Whitelegge JP,
Sen S, Janzen C and Mascharak PK: Diminished viability of human
ovarian cancer cells by antigen-specific delivery of carbon
monoxide with a family of photoactivatable antibody-photoCORM
conjugates. Chem Sci. 11:467–473. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
607
|
Kawahara B, Ramadoss S, Chaudhuri G,
Janzen C, Sen S and Mascharak PK: Carbon monoxide sensitizes
cisplatin-resistant ovarian cancer cell lines toward cisplatin via
attenuation of levels of glutathione and nuclear metallothionein. J
Inorganic Biochem. 191:29–39. 2019. View Article : Google Scholar
|
|
608
|
Khasag N, Sakiyama S, Toba H, Yoshida M,
Nakagawa Y, Takizawa H, Kawakami Y, Kenzaki K, Ali AH, Kondo K and
Tangoku A: Monitoring of exhaled carbon monoxide and carbon dioxide
during lung cancer operation. Eur J Cardiothorac Surg. 45:531–536.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
609
|
Liptay MJ, Basu S, Hoaglin MC, Freedman N,
Faber LP, Warren WH, Hammoud ZT and Kim AW: Diffusion lung capacity
for carbon monoxide (DLCO) is an independent prognostic factor for
long-term survival after curative lung resection for cancer. J Surg
Oncol. 100:703–707. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
610
|
Nemeth Z, Csizmadia E, Vikstrom L, Li M,
Bisht K, Feizi A, Otterbein S, Zuckerbraun B, Costa DB, Pandolfi
PP, et al: Alterations of tumor microenvironment by carbon monoxide
impedes lung cancer growth. Oncotarget. 7:23919–23932. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
611
|
Shao L, Gu YY, Jiang CH, Liu CY, Lv LP,
Liu JN and Zou Y: Carbon monoxide releasing molecule-2 suppresses
proliferation, migration, invasion, and promotes apoptosis in
non-small cell lung cancer Calu-3 cells. Eur Rev Med Pharmacol Sci.
22:1948–1957. 2018.PubMed/NCBI
|
|
612
|
Shirabe T, Mawatari S and Kuroiwa Y:
Autopsy case of carbon monoxide poisoning at the Miike Coal Mine
explosion-a case of lung cancer with the fatal outcome in 3 years
and 4 months. Shinkei Kenkyu No Shimpo. 14:321–326. 1970.PubMed/NCBI
|
|
613
|
Zarogoulidis P, Kerenidi T, Huang H,
Kontakiotis T, Tremma O, Porpodis K, Kalianos A, Rapti A, Foroulis
C, Zissimopoulos A, et al: Six minute walking test and carbon
monoxide diffusing capacity for non-small cell lung cancer: Easy
performed tests in every day practice. J Thorac Dis. 4:569–576.
2012.PubMed/NCBI
|
|
614
|
Lian S, Xia Y, Ung TT, Khoi PN, Yoon HJ,
Kim NH, Kim KK and Jung YD: Carbon monoxide releasing molecule-2
ameliorates IL-1β-induced IL-8 in human gastric cancer cells.
Toxicology. 361–362. 24–38. 2016.PubMed/NCBI
|
|
615
|
Lv C, Su Q, Fang J and Yin H:
Styrene-maleic acid copolymer-encapsulated carbon monoxide
releasing molecule-2 (SMA/CORM-2) suppresses proliferation,
migration and invasion of colorectal cancer cells in vitro and in
vivo. Biochem Biophys Res Commun. 520:320–326. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
616
|
Yin H, Fang J, Liao L, Maeda H and Su Q:
Upregulation of heme oxygenase-1 in colorectal cancer patients with
increased circulation carbon monoxide levels, potentially affects
chemotherapeutic sensitivity. BMC Cancer. 14:4362014. View Article : Google Scholar : PubMed/NCBI
|
|
617
|
Nitta S, Kawai K, Nagumo Y, Ikeda A,
Kandori S, Kojima T and Nishiyama H: Impact of hemoglobin levels on
hemoglobin-adjusted carbon monoxide diffusion capacity after
chemotherapy for testicular cancer. Jpn J Clin Oncol. 49:1151–1156.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
618
|
van Osch FHM, Pauwels CGGM, Jochems SHJ,
Fayokun R, James ND, Wallace DMA, Cheng KK, Bryan RT, van Schooten
FJ and Zeegers MP: Tar, nicotine and carbon monoxide yield of UK
cigarettes and the risk of non-muscle-invasive and muscle-invasive
bladder cancer. Eur J Cancer Prev. 28:40–44. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
619
|
Vítek L, Gbelcová H, Muchová L, Váňová K,
Zelenka J, Koníčková R, Suk J, Zadinova M, Knejzlík Z, Ahmad S, et
al: Antiproliferative effects of carbon monoxide on pancreatic
cancer. Dig Liver Dis. 46:369–375. 2014. View Article : Google Scholar : PubMed/NCBI
|