|
1
|
Mohammed MS, Sendra S, Lloret J and Bosch
I: Systems and WBANs for Controlling Obesity. J Healthc Eng.
2018:15647482018. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kusminski CM, Bickel PE and Scherer PE:
Targeting adipose tissue in the treatment of obesity-associated
diabetes. Nat Rev Drug Discov. 15:639–660. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Abu-Farha M, Al-Mulla F, Thanaraj TA,
Kavalakatt S, Ali H, Abdul Ghani M and Abubaker J: Impact of
Diabetes in Patients Diagnosed With COVID-19. Front Immunol.
11:5768182020. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Goodman KE, Magder LS, Baghdadi JD,
Pineles L, Levine AR, Perencevich EN and Harris AD: Impact of sex
and metabolic comorbidities on coronavirus disease 2019 (COVID-19)
mortality risk across age groups: 66 646 inpatients across 613 U.S.
Hospitals. Clin Infect Dis. 73:e4113–e4123. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Piroth L, Cottenet J, Mariet AS, Bonniaud
P, Blot M, Tubert-Bitter P and Quantin C: Comparison of the
characteristics, morbidity, and mortality of COVID-19 and seasonal
influenza: A nationwide, population-based retrospective cohort
study. Lancet Respir Med. 9:251–259. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Ottaviani E, Malagoli D and Franceschi C:
The evolution of the adipose tissue: A neglected enigma. Gen Comp
Endocrinol. 174:1–4. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Unamuno X, Gomez-Ambrosi J, Rodriguez A,
Becerril S, Fruhbeck G and Catalan V: Adipokine dysregulation and
adipose tissue inflammation in human obesity. Eur J Clin Invest.
48:e129972018. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Burhans MS, Hagman DK, Kuzma JN, Schmidt
KA and Kratz M: Contribution of adipose tissue inflammation to the
development of type 2 diabetes Mellitus. Compr Physiol. 9:1–58.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Berg AH, Combs TP, Du X, Brownlee M and
Scherer PE: The adipocyte-secreted protein Acrp30 enhances hepatic
insulin action. Nat Med. 7:947–953. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yamauchi T, Kamon J, Ito Y, Tsuchida A,
Yokomizo T, Kita S, Sugiyama T, Miyagishi M, Hara K, Tsunoda M, et
al: Cloning of adiponectin receptors that mediate antidiabetic
metabolic effects. Nature. 423:762–769. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hefetz-Sela S and Scherer PE: Adipocytes:
Impact on tumor growth and potential sites for therapeutic
intervention. Pharmacol Ther. 138:197–210. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Igata M, Motoshima H, Tsuruzoe K, Kojima
K, Matsumura T, Kondo T, Taguchi T, Nakamaru K, Yano M, Kukidome D,
et al: Adenosine monophosphate-activated protein kinase suppresses
vascular smooth muscle cell proliferation through the inhibition of
cell cycle progression. Circ Res. 97:837–844. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Douros JD, Baltzegar DA, Reading BJ, Seale
AP, Lerner DT, Grau EG and Borski RJ: Leptin stimulates cellular
glycolysis through a STAT3 dependent mechanism in Tilapia. Front
Endocrinol (Lausanne). 9:4652018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
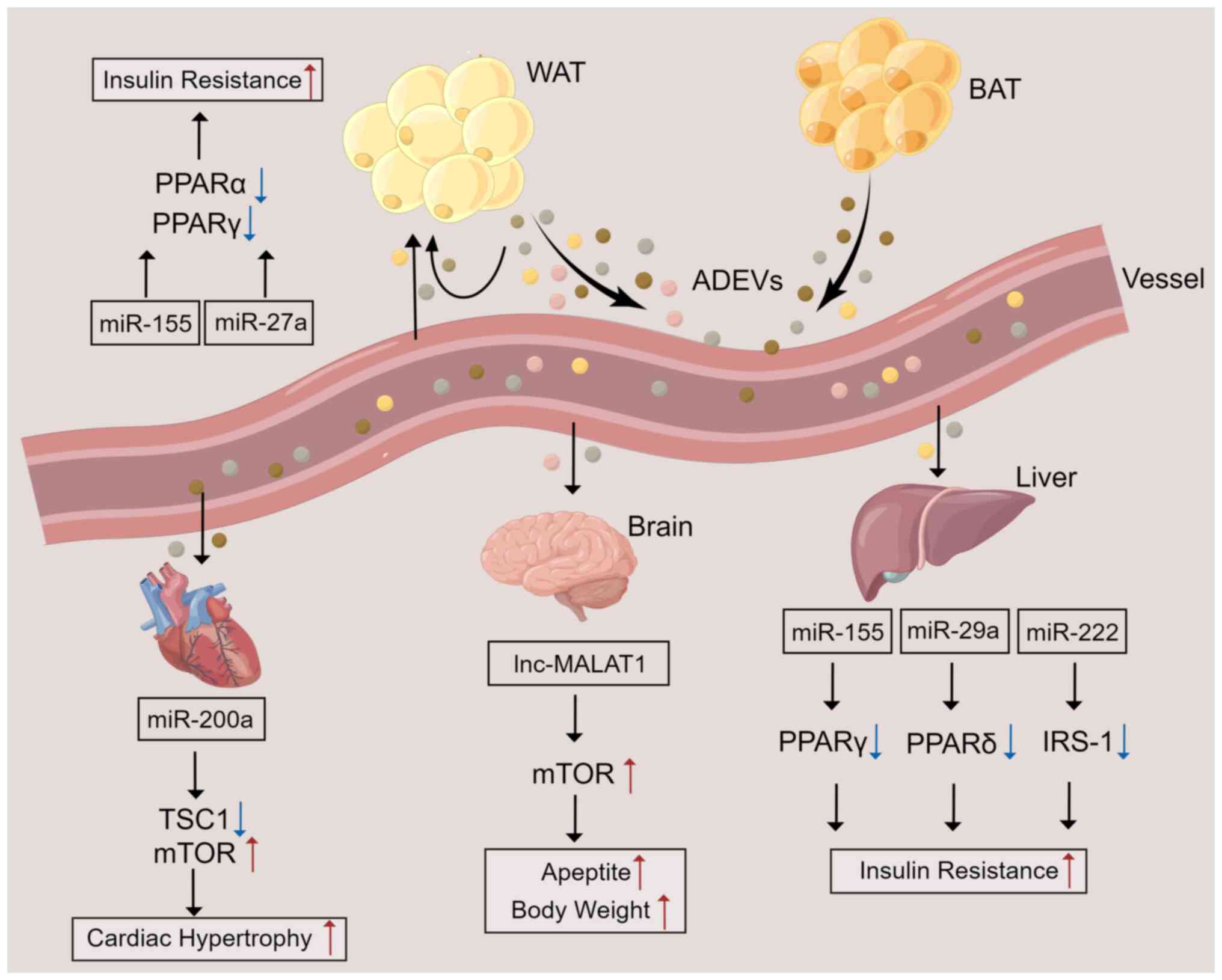
Huang Z and Xu A: Adipose extracellular
vesicles in intercellular and inter-organ crosstalk in metabolic
health and diseases. Front Immunol. 12:6086802021. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Padilla J, Vieira-Potter VJ, Jia G and
Sowers JR: Role of perivascular adipose tissue on vascular reactive
oxygen species in type 2 diabetes: A give-and-take relationship.
Diabetes. 64:1904–1906. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kern PA, Ranganathan S, Li C, Wood L and
Ranganathan G: Adipose tissue tumor necrosis factor and
interleukin-6 expression in human obesity and insulin resistance.
Am J Physiol Endocrinol Metab. 280:E745–E751. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
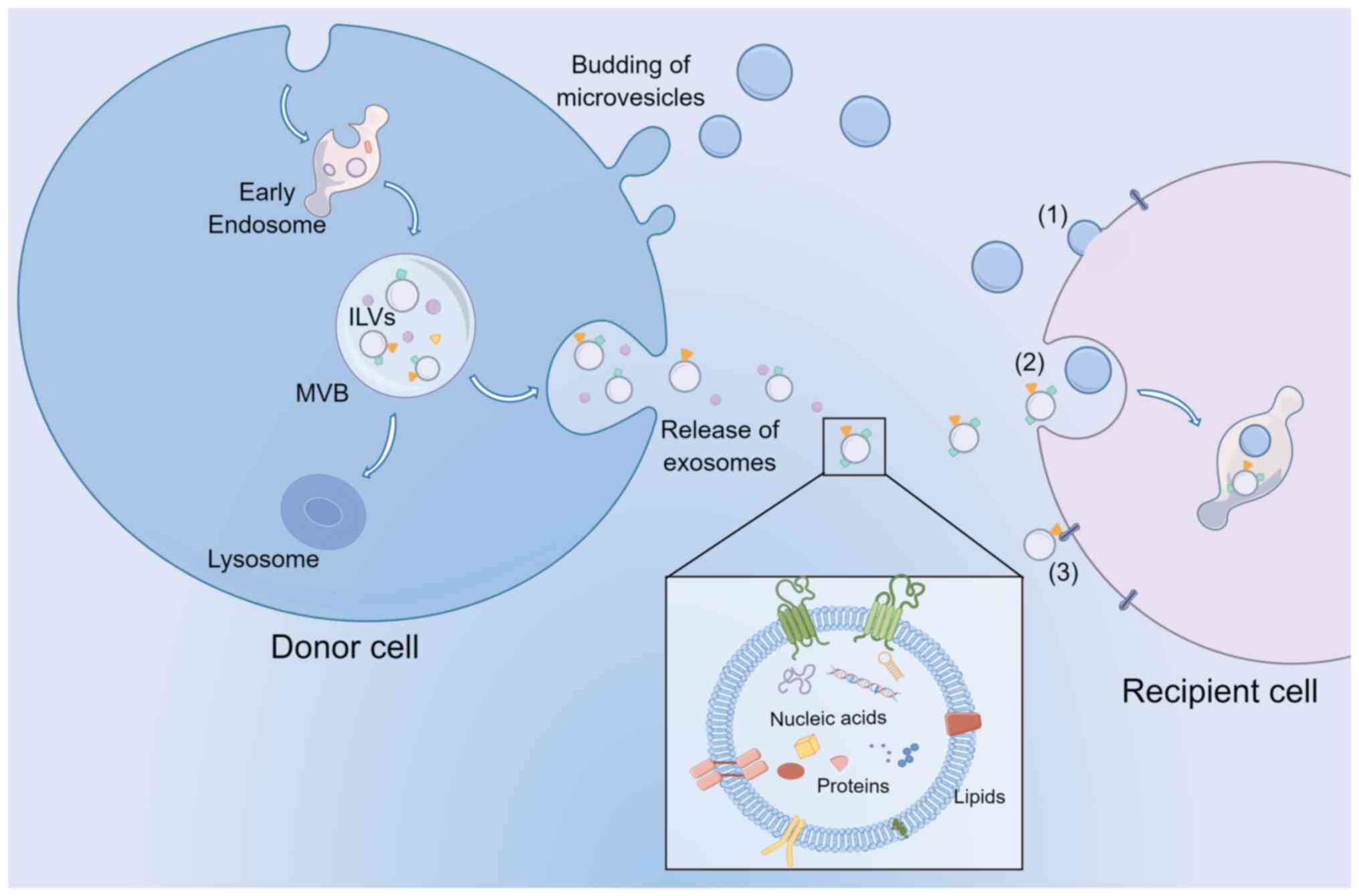
Keller S, Sanderson MP, Stoeck A and
Altevogt P: Exosomes: From biogenesis and secretion to biological
function. Immunol Lett. 107:102–108. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Thomou T, Mori MA, Dreyfuss JM, Konishi M,
Sakaguchi M, Wolfrum C, Rao TN, Winnay JN, Garcia-Martin R,
Grinspoon SK, et al: Adipose-derived circulating miRNAs regulate
gene expression in other tissues. Nature. 542:450–455. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Rome S, Blandin A and Le Lay S:
Adipocyte-Derived extracellular vesicles: State of the art. Int J
Mol Sci. 22:17882021. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Vidal M: Exosomes: Revisiting their role
as ‘garbage bags’. Traffic. 20:815–828. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
van der Pol E, Boing AN, Harrison P, Sturk
A and Nieuwland R: Classification, functions, and clinical
relevance of extracellular vesicles. Pharmacol Rev. 64:676–705.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Tricarico C, Clancy J and D'Souza-Schorey
C: Biology and biogenesis of shed microvesicles. Small GTPases.
8:220–232. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Cai H, Reinisch K and Ferro-Novick S:
Coats, tethers, Rabs, and SNAREs work together to mediate the
intracellular destination of a transport vesicle. Dev Cell.
12:671–682. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Escola JM, Kleijmeer MJ, Stoorvogel W,
Griffith JM, Yoshie O and Geuze HJ: Selective enrichment of
tetraspan proteins on the internal vesicles of multivesicular
endosomes and on exosomes secreted by human B-lymphocytes. J Biol
Chem. 273:20121–20127. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Giebel B and Helmbrecht C: Methods to
Analyze EVs. Methods Mol Biol. 1545:1–20. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Wolf P: The nature and significance of
platelet products in human plasma. Br J Haematol. 13:269–288. 1967.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Al-Nedawi K, Meehan B, Micallef J, Lhotak
V, May L, Guha A and Rak J: Intercellular transfer of the oncogenic
receptor EGFRvIII by microvesicles derived from tumour cells. Nat
Cell Biol. 10:619–624. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Harding C, Heuser J and Stahl P:
Endocytosis and intracellular processing of transferrin and
colloidal gold-transferrin in rat reticulocytes: Demonstration of a
pathway for receptor shedding. Eur J Cell Biol. 35:256–263.
1984.PubMed/NCBI
|
|
29
|
Pan BT, Teng K, Wu C, Adam M and Johnstone
RM: Electron microscopic evidence for externalization of the
transferrin receptor in vesicular form in sheep reticulocytes. J
Cell Biol. 101:942–948. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Kalra H, Drummen GP and Mathivanan S:
Focus on extracellular vesicles: Introducing the next small big
thing. Int J Mol Sci. 17:1702016. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Minciacchi VR, Freeman MR and Di Vizio D:
Extracellular vesicles in cancer: Exosomes, microvesicles and the
emerging role of large oncosomes. Semin Cell Dev Biol. 40:41–51.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Raposo G and Stoorvogel W: Extracellular
vesicles: Exosomes, microvesicles, and friends. J Cell Biol.
200:373–383. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Mulcahy LA, Pink RC and Carter DR: Routes
and mechanisms of extracellular vesicle uptake. J Extracell
Vesicles. 3:2014. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Llorente A, Skotland T, Sylvanne T,
Kauhanen D, Rog T, Orlowski A, Vattulainen I, Ekroos K and Sandvig
K: Molecular lipidomics of exosomes released by PC-3 prostate
cancer cells. Biochim Biophys Acta. 1831:1302–1309. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Laulagnier K, Javalet C, Hemming FJ,
Chivet M, Lachenal G, Blot B, Chatellard C and Sadoul R: Amyloid
precursor protein products concentrate in a subset of exosomes
specifically endocytosed by neurons. Cell Mol Life Sci. 75:757–773.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Vargas A, Zhou S, Ethier-Chiasson M, Flipo
D, Lafond J, Gilbert C and Barbeau B: Syncytin proteins
incorporated in placenta exosomes are important for cell uptake and
show variation in abundance in serum exosomes from patients with
preeclampsia. FASEB J. 28:3703–3719. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Kamerkar S, LeBleu VS, Sugimoto H, Yang S,
Ruivo CF, Melo SA, Lee JJ and Kalluri R: Exosomes facilitate
therapeutic targeting of oncogenic KRAS in pancreatic cancer.
Nature. 546:498–503. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
van Niel G, D'Angelo G and Raposo G:
Shedding light on the cell biology of extracellular vesicles. Nat
Rev Mol Cell Biol. 19:213–228. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Jeppesen DK, Fenix AM, Franklin JL,
Higginbotham JN, Zhang Q, Zimmerman LJ, Liebler DC, Ping J, Liu Q,
Evans R, et al: Reassessment of exosome composition. Cell.
177:428–445. e182019. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Corrado C, Raimondo S, Saieva L, Flugy AM,
De Leo G and Alessandro R: Exosome-mediated crosstalk between
chronic myelogenous leukemia cells and human bone marrow stromal
cells triggers an interleukin 8-dependent survival of leukemia
cells. Cancer Lett. 348:71–76. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Ailawadi S, Wang X, Gu H and Fan GC:
Pathologic function and therapeutic potential of exosomes in
cardiovascular disease. Biochim Biophys Acta. 1852:1–11. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
42
|
van Marken Lichtenbelt W: Brown adipose
tissue and the regulation of nonshivering thermogenesis. Curr Opin
Clin Nutr Metab Care. 15:547–552. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Lee YH, Kim SN, Kwon HJ and Granneman JG:
Metabolic heterogeneity of activated beige/brite adipocytes in
inguinal adipose tissue. Sci Rep. 7:397942017. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Keipert S and Jastroch M: Brite/beige fat
and UCP1 - is it thermogenesis? Biochim Biophys Acta.
1837:1075–1082. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Wang Z, Ning T, Song A, Rutter J, Wang QA
and Jiang L: Chronic cold exposure enhances glucose oxidation in
brown adipose tissue. EMBO Rep. 21:e500852020. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Shamsi BH, Ma C, Naqvi S and Xiao Y:
Effects of pioglitazone mediated activation of PPAR-ү on CIDEC and
obesity related changes in mice. PLoS One. 9:e1069922014.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Giampietro L, Gallorini M, De Filippis B,
Amoroso R, Cataldi A and di Giacomo V: PPAR-ү agonist GL516 reduces
oxidative stress and apoptosis occurrence in a rat astrocyte cell
line. Neurochem Int. 126:239–245. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Jung SM, Sanchez-Gurmaches J and Guertin
DA: Brown adipose tissue development and metabolism. Handb Exp
Pharmacol. 251:3–36. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Lau P, Tuong ZK, Wang SC, Fitzsimmons RL,
Goode JM, Thomas GP, Cowin GJ, Pearen MA, Mardon K, Stow JL and
Muscat GE: Roralpha deficiency and decreased adiposity are
associated with induction of thermogenic gene expression in
subcutaneous white adipose and brown adipose tissue. Am J Physiol
Endocrinol Metab. 308:E159–E171. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Wu J, Bostrom P, Sparks LM, Ye L, Choi JH,
Giang AH, Khandekar M, Virtanen KA, Nuutila P, Schaart G, et al:
Beige adipocytes are a distinct type of thermogenic fat cell in
mouse and human. Cell. 150:366–376. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Ikeda K, Maretich P and Kajimura S: The
common and distinct features of brown and beige adipocytes. Trends
Endocrinol Metab. 29:191–200. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Pinckard KM and Stanford KI: The
heartwarming effect of brown adipose tissue. Mol Pharmacol.
102:460–471. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Berbee JF, Boon MR, Khedoe PP, Bartelt A,
Schlein C, Worthmann A, Kooijman S, Hoeke G, Mol IM, John C, et al:
Brown fat activation reduces hypercholesterolaemia and protects
from atherosclerosis development. Nat Commun. 6:63562015.
View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Altshuler-Keylin S, Shinoda K, Hasegawa Y,
Ikeda K, Hong H, Kang Q, Yang Y, Perera RM, Debnath J and Kajimura
S: Beige adipocyte maintenance is regulated by autophagy-induced
mitochondrial clearance. Cell Metab. 24:402–419. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Rosen ED and Spiegelman BM: Adipocytes as
regulators of energy balance and glucose homeostasis. Nature.
444:847–853. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
56
|
Arner P: Regional adipocity in man. J
Endocrinol. 155:191–192. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
57
|
Chen SX, Zhang LJ and Gallo RL: Dermal
white adipose tissue: A newly recognized layer of skin innate
defense. J Invest Dermatol. 139:1002–1009. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
58
|
Zhang LJ, Guerrero-Juarez CF, Hata T,
Bapat SP, Ramos R, Plikus MV and Gallo RL: Innate immunity. Dermal
adipocytes protect against invasive Staphylococcus aureus skin
infection. Science. 347:67–71. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
59
|
Fruhbeck G: Overview of adipose tissue and
its role in obesity and metabolic disorders. Methods Mol Biol.
456:1–22. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
60
|
Salvador J, Silva C, Pujante P and
Fruhbeck G: Abdominal obesity: An indicator of cardiometabolic
risk. Endocrinol Nutr. 55:420–432. 2008.(In English, Spanish).
View Article : Google Scholar : PubMed/NCBI
|
|
61
|
Scheja L and Heeren J: The endocrine
function of adipose tissues in health and cardiometabolic disease.
Nat Rev Endocrinol. 15:507–524. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
62
|
Stern JH, Rutkowski JM and Scherer PE:
Adiponectin, leptin, and fatty acids in the maintenance of
metabolic homeostasis through adipose tissue crosstalk. Cell Metab.
23:770–784. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
63
|
Eto H, Suga H, Matsumoto D, Inoue K, Aoi
N, Kato H, Araki J and Yoshimura K: Characterization of structure
and cellular components of aspirated and excised adipose tissue.
Plast Reconstr Surg. 124:1087–1097. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
64
|
Zuk PA, Zhu M, Mizuno H, Huang J, Futrell
JW, Katz AJ, Benhaim P, Lorenz HP and Hedrick MH: Multilineage
cells from human adipose tissue: Implications for cell-based
therapies. Tissue Eng. 7:211–228. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
65
|
Brown JC, Shang H, Li Y, Yang N, Patel N
and Katz AJ: Isolation of adipose-derived stromal vascular fraction
cells using a novel point-of-care device: Cell characterization and
review of the literature. Tissue Eng Part C Methods. 23:125–135.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
66
|
Wu H and Ballantyne CM: Metabolic
inflammation and insulin resistance in obesity. Circ Res.
126:1549–1564. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
67
|
Hollenberg CH and Vost A: Regulation of
DNA synthesis in fat cells and stromal elements from rat adipose
tissue. J Clin Invest. 47:2485–2498. 1969. View Article : Google Scholar : PubMed/NCBI
|
|
68
|
Panina YA, Yakimov AS, Komleva YK, Morgun
AV, Lopatina OL, Malinovskaya NA, Shuvaev AN, Salmin VV,
Taranushenko TE and Salmina AB: Plasticity of adipose
tissue-derived stem cells and regulation of angiogenesis. Front
Physiol. 9:16562018. View Article : Google Scholar : PubMed/NCBI
|
|
69
|
Cao Y: Adipose tissue angiogenesis as a
therapeutic target for obesity and metabolic diseases. Nat Rev Drug
Discov. 9:107–115. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
70
|
Mahlakoiv T, Flamar AL, Johnston LK,
Moriyama S, Putzel GG, Bryce PJ and Artis D: Stromal cells maintain
immune cell homeostasis in adipose tissue via production of
interleukin-33. Sci Immunol. 4:eaax04162019. View Article : Google Scholar : PubMed/NCBI
|
|
71
|
Sun C, Berry WL and Olson LE: PDGFRα
controls the balance of stromal and adipogenic cells during adipose
tissue organogenesis. Development. 144:83–94. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
72
|
Mclaughlin T, Ackerman SE, Shen L and
Engleman E: Role of innate and adaptive immunity in
obesity-associated metabolic disease. J Clin Invest. 127:5–13.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
73
|
Rochette L, Mazini L, Malka G, Zeller M,
Cottin Y and Vergely C: The crosstalk of adipose-derived stem cells
(ADSC), oxidative stress, and inflammation in protective and
adaptive responses. Int J Mol Sci. 21:92622020. View Article : Google Scholar : PubMed/NCBI
|
|
74
|
Hui X, Zhang M, Gu P, Li K, Gao Y, Wu D,
Wang Y and Xu A: Adipocyte SIRT1 controls systemic insulin
sensitivity by modulating macrophages in adipose tissue. EMBO Rep.
18:645–657. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
75
|
Hotamisligil GS: Inflammation,
metaflammation and immunometabolic disorders. Nature. 542:177–185.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
76
|
Hotamisligil GS: Foundations of
immunometabolism and implications for metabolic health and disease.
Immunity. 47:406–420. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
77
|
Man K, Kutyavin VI and Chawla A: Tissue
immunometabolism: Development, physiology, and pathobiology. Cell
Metab. 25:11–26. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
78
|
Clement E, Lazar I, Attane C, Carrie L,
Dauvillier S, Ducoux-Petit M, Esteve D, Menneteau T, Moutahir M, Le
Gonidec S, et al: Adipocyte extracellular vesicles carry enzymes
and fatty acids that stimulate mitochondrial metabolism and
remodeling in tumor cells. EMBO J. 39:e1025252020. View Article : Google Scholar : PubMed/NCBI
|
|
79
|
Hartwig S, De Filippo E, Goddeke S, Knebel
B, Kotzka J, Al-Hasani H, Roden M, Lehr S and Sell H: Exosomal
proteins constitute an essential part of the human adipose tissue
secretome. Biochim Biophys Acta Proteins Proteom. 1867:1401722019.
View Article : Google Scholar : PubMed/NCBI
|
|
80
|
Valadi H, Ekstrom K, Bossios A, Sjostrand
M, Lee JJ and Lotvall JO: Exosome-mediated transfer of mRNAs and
microRNAs is a novel mechanism of genetic exchange between cells.
Nat Cell Biol. 9:654–659. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
81
|
Liu T, Sun YC, Cheng P and Shao HG:
Adipose tissue macrophage-derived exosomal miR-29a regulates
obesity-associated insulin resistance. Biochem Biophys Res Commun.
515:352–358. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
82
|
Geng L, Lam K and Xu A: The therapeutic
potential of FGF21 in metabolic diseases: From bench to clinic. Nat
Rev Endocrinol. 16:654–667. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
83
|
Gao J, Li X, Wang Y, Cao Y, Yao D, Sun L,
Qin L, Qiu H and Zhan X: Adipocyte-derived extracellular vesicles
modulate appetite and weight through mTOR signalling in the
hypothalamus. Acta Physiol (Oxf). 228:e133392020. View Article : Google Scholar : PubMed/NCBI
|
|
84
|
Lee JE, Moon PG, Lee IK and Baek MC:
Proteomic Analysis of extracellular vesicles released by adipocytes
of otsuka long-evans tokushima fatty (OLETF) Rats. Protein J.
34:220–235. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
85
|
Sano S, Izumi Y, Yamaguchi T, Yamazaki T,
Tanaka M, Shiota M, Osada-Oka M, Nakamura Y, Wei M, Wanibuchi H, et
al: Lipid synthesis is promoted by hypoxic adipocyte-derived
exosomes in 3T3-L1 cells. Biochem Biophys Res Commun. 445:327–333.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
86
|
Kranendonk ME, Visseren FL, van Balkom BW,
Nolte-'t Hoen EN, van Herwaarden JA, de Jager W, Schipper HS,
Brenkman AB, Verhaar MC, Wauben MH and Kalkhoven E: Human adipocyte
extracellular vesicles in reciprocal signaling between adipocytes
and macrophages. Obesity (Silver Spring). 22:1296–1308. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
87
|
Phoonsawat W, Aoki-Yoshida A, Tsuruta T
and Sonoyama K: Adiponectin is partially associated with exosomes
in mouse serum. Biochem Biophys Res Commun. 448:261–266. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
88
|
Crewe C and Scherer PE: Intercellular and
interorgan crosstalk through adipocyte extracellular vesicles. Rev
Endocr Metab Disord. 23:61–69. 2022. View Article : Google Scholar : PubMed/NCBI
|
|
89
|
Connolly KD, Wadey RM, Mathew D, Johnson
E, Rees DA and James PE: Evidence for adipocyte-derived
extracellular vesicles in the human circulation. Endocrinology.
159:3259–3267. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
90
|
Lazar I, Clement E, Dauvillier S, Milhas
D, Ducoux-Petit M, Legonidec S, Moro C, Soldan V, Dalle S, Balor S,
et al: Adipocyte Exosomes Promote Melanoma Aggressiveness through
Fatty Acid Oxidation: A Novel Mechanism Linking Obesity and Cancer.
Cancer Res. 76:4051–4057. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
91
|
Ying W, Riopel M, Bandyopadhyay G, Dong Y,
Birmingham A, Seo JB, Ofrecio JM, Wollam J, Hernandez-Carretero A,
Fu W, et al: Adipose tissue macrophage-derived exosomal miRNAs Can
modulate in vivo and in vitro insulin sensitivity. Cell.
171:372–384.e12. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
92
|
Bassi EJ, Moraes-Vieira PM, Moreira-Sa CS,
Almeida DC, Vieira LM, Cunha CS, Hiyane MI, Basso AS, Pacheco-Silva
A and Camara NO: Immune regulatory properties of allogeneic
adipose-derived mesenchymal stem cells in the treatment of
experimental autoimmune diabetes. Diabetes. 61:2534–2545. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
93
|
Mizuno H, Tobita M and Uysal AC: Concise
review: Adipose-derived stem cells as a novel tool for future
regenerative medicine. Stem Cells. 30:804–810. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
94
|
Gonzalez MA, Gonzalez-Rey E, Rico L,
Buscher D and Delgado M: Adipose-derived mesenchymal stem cells
alleviate experimental colitis by inhibiting inflammatory and
autoimmune responses. Gastroenterology. 136:978–989. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
95
|
Garcia-Contreras M, Vera-Donoso CD,
Hernandez-Andreu JM, Garcia-Verdugo JM and Oltra E: Therapeutic
potential of human adipose-derived stem cells (ADSCs) from cancer
patients: A pilot study. PLoS One. 9:e1132882014. View Article : Google Scholar : PubMed/NCBI
|
|
96
|
Zhao H, Shang Q, Pan Z, Bai Y, Li Z, Zhang
H, Zhang Q, Guo C, Zhang L and Wang Q: Exosomes from
adipose-derived stem cells attenuate adipose inflammation and
obesity through polarizing M2 macrophages and beiging in white
adipose tissue. Diabetes. 67:235–247. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
97
|
Jung YJ, Kim HK, Cho Y, Choi JS, Woo CH,
Lee KS, Sul JH, Lee CM, Han J, Park JH, et al: Cell reprogramming
using extracellular vesicles from differentiating stem cells into
white/beige adipocytes. Sci Adv. 6:eaay67212020. View Article : Google Scholar : PubMed/NCBI
|
|
98
|
Fuster JJ, Ouchi N, Gokce N and Walsh K:
Obesity-Induced changes in adipose tissue microenvironment and
their impact on cardiovascular disease. Circ Res. 118:1786–1807.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
99
|
Zhao S, Kusminski CM and Scherer PE:
Adiponectin, leptin and cardiovascular disorders. Circ Res.
128:136–149. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
100
|
Weisberg SP, Hunter D, Huber R, Lemieux J,
Slaymaker S, Vaddi K, Charo I, Leibel RL and Ferrante AJ: CCR2
modulates inflammatory and metabolic effects of high-fat feeding. J
Clin Invest. 116:115–124. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
101
|
Lumeng CN, Bodzin JL and Saltiel AR:
Obesity induces a phenotypic switch in adipose tissue macrophage
polarization. J Clin Invest. 117:175–184. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
102
|
Deng ZB, Poliakov A, Hardy RW, Clements R,
Liu C, Liu Y, Wang J, Xiang X, Zhang S, Zhuang X, et al: Adipose
tissue exosome-like vesicles mediate activation of
macrophage-induced insulin resistance. Diabetes. 58:2498–2505.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
103
|
Pan Y, Hui X, Hoo RLC, Ye D, Chan CYC,
Feng T, Wang Y, Lam KSL and Xu A: Adipocyte-secreted exosomal
microRNA-34a inhibits M2 macrophage polarization to promote
obesity-induced adipose inflammation. J Clin Invest. 129:834–849.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
104
|
James DE, Stockli J and Birnbaum MJ: The
aetiology and molecular landscape of insulin resistance. Nat Rev
Mol Cell Biol. 22:751–771. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
105
|
Yu Y, Du H, Wei S, Feng L, Li J, Yao F,
Zhang M, Hatch GM and Chen L: Adipocyte-Derived exosomal MiR-27a
induces insulin resistance in skeletal muscle through repression of
PPARү. Theranostics. 8:2171–2188. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
106
|
Li D, Song H, Shuo L, Wang L, Xie P, Li W,
Liu J, Tong Y, Zhang CY, Jiang X, et al: Gonadal white adipose
tissue-derived exosomal MiR-222 promotes obesity-associated insulin
resistance. Aging (Albany NY). 12:22719–22743. 2020.PubMed/NCBI
|
|
107
|
Kranendonk ME, Visseren FL, van Herwaarden
JA, Nolte-'t Hoen EN, de Jager W, Wauben MH and Kalkhoven E: Effect
of extracellular vesicles of human adipose tissue on insulin
signaling in liver and muscle cells. Obesity (Silver Spring).
22:2216–2223. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
108
|
Gao X, Salomon C and Freeman DJ:
Extracellular vesicles from adipose tissue-A potential role in
obesity and type 2 diabetes? Front Endocrinol (Lausanne).
8:2022017. View Article : Google Scholar : PubMed/NCBI
|
|
109
|
Eguchi A, Lazic M, Armando AM, Phillips
SA, Katebian R, Maraka S, Quehenberger O, Sears DD and Feldstein
AE: Circulating adipocyte-derived extracellular vesicles are novel
markers of metabolic stress. J Mol Med (Berl). 94:1241–1253. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
110
|
Katayama M, Wiklander OPB, Fritz T,
Caidahl K, El-Andaloussi S, Zierath JR and Krook A: Circulating
exosomal miR-20b-5p is elevated in type 2 diabetes and could impair
insulin action in human skeletal muscle. Diabetes. 68:515–526.
2019. View Article : Google Scholar : PubMed/NCBI
|
|
111
|
Kranendonk ME, de Kleijn DP, Kalkhoven E,
Kanhai DA, Uiterwaal CS, van der Graaf Y, Pasterkamp G and Visseren
FL; SMART Study Group, : Extracellular vesicle markers in relation
to obesity and metabolic complications in patients with manifest
cardiovascular disease. Cardiovasc Diabetol. 13:372014. View Article : Google Scholar : PubMed/NCBI
|
|
112
|
Su S, Guntur AR, Nguyen DC, Fakory SS,
Doucette CC, Leech C, Lotana H, Kelley M, Kohli J, Martino J, et
al: A renewable source of human beige adipocytes for development of
therapies to treat metabolic Syndrome. Cell Rep. 25:3215–3228,e9.
2018. View Article : Google Scholar : PubMed/NCBI
|
|
113
|
Connolly KD, Rees DA and James PE: Role of
adipocyte-derived extracellular vesicles in vascular inflammation.
Free Radic Biol Med. 172:58–64. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
114
|
Dai W, Liu Z, Yang S and Kong J: Inflamed
adipose tissue: Therapeutic Targets for obesity-related endothelial
injury. Endocrinology. 164:bqad0942023. View Article : Google Scholar : PubMed/NCBI
|
|
115
|
Koenen M, Hill MA, Cohen P and Sowers JR:
Obesity, adipose tissue and vascular dysfunction. Circ Res.
128:951–968. 2021. View Article : Google Scholar : PubMed/NCBI
|
|
116
|
Xie Z, Wang X, Liu X, Du H, Sun C, Shao X,
Tian J, Gu X, Wang H, Tian J and Yu B: Adipose-Derived exosomes
exert proatherogenic effects by regulating macrophage foam cell
formation and polarization. J Am Heart Assoc. 7:e0074422018.
View Article : Google Scholar : PubMed/NCBI
|
|
117
|
Barberio MD, Kasselman LJ, Playford MP,
Epstein SB, Renna HA, Goldberg M, Deleon J, Voloshyna I, Barlev A,
Salama M, et al: Cholesterol efflux alterations in adolescent
obesity: Role of adipose-derived extracellular vesical microRNAs. J
Transl Med. 17:2322019. View Article : Google Scholar : PubMed/NCBI
|
|
118
|
Fleury A, Martinez MC and Le Lay S:
Extracellular vesicles as therapeutic tools in cardiovascular
diseases. Front Immunol. 5:3702014. View Article : Google Scholar : PubMed/NCBI
|
|
119
|
Wen Z, Li J, Fu Y, Zheng Y, Ma M and Wang
C: Hypertrophic adipocyte-derived exosomal miR-802-5p contributes
to insulin resistance in cardiac myocytes through targeting hSP60.
Obesity (Silver Spring). 28:1932–1940. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
120
|
Monteiro JP, Bennett M, Rodor J,
Caudrillier A, Ulitsky I and Baker AH: Endothelial function and
dysfunction in the cardiovascular system: The long non-coding road.
Cardiovasc Res. 115:1692–1704. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
121
|
Muller G: Microvesicles/exosomes as
potential novel biomarkers of metabolic diseases. Diabetes Metab
Syndr Obes. 5:247–282. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
122
|
Wadey RM, Connolly KD, Mathew D, Walters
G, Rees DA and James PE: Inflammatory adipocyte-derived
extracellular vesicles promote leukocyte attachment to vascular
endothelial cells. Atherosclerosis. 283:19–27. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
123
|
Fang X, Stroud MJ, Ouyang K, Fang L, Zhang
J, Dalton ND, Gu Y, Wu T, Peterson KL, Huang HD, et al:
Adipocyte-specific loss of PPARү attenuates cardiac hypertrophy.
JCI Insight. 1:e899082016. View Article : Google Scholar : PubMed/NCBI
|
|
124
|
Gan L, Xie D, Liu J, Bond LW, Christopher
TA, Lopez B, Zhang L, Gao E, Koch W, Ma XL and Wang Y: Small
extracellular microvesicles mediated pathological communications
between dysfunctional adipocytes and cardiomyocytes as a novel
mechanism exacerbating ischemia/reperfusion injury in diabetic
mice. Circulation. 141:968–983. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
125
|
Parekh N, Chandran U and Bandera EV:
Obesity in cancer survival. Annu Rev Nutr. 32:311–342. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
126
|
Dirat B, Bochet L, Dabek M, Daviaud D,
Dauvillier S, Majed B, Wang YY, Meulle A, Salles B, Le Gonidec S,
et al: Cancer-associated adipocytes exhibit an activated phenotype
and contribute to breast cancer invasion. Cancer Res. 71:2455–2465.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
127
|
Nieman KM, Kenny HA, Penicka CV, Ladanyi
A, Buell-Gutbrod R, Zillhardt MR, Romero IL, Carey MS, Mills GB,
Hotamisligil GS, et al: Adipocytes promote ovarian cancer
metastasis and provide energy for rapid tumor growth. Nat Med.
17:1498–1503. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
128
|
Wang J, Wu Y, Guo J, Fei X, Yu L and Ma S:
Adipocyte-derived exosomes promote lung cancer metastasis by
increasing MMP9 activity via transferring MMP3 to lung cancer
cells. Oncotarget. 8:81880–81891. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
129
|
Wang Y, Chu Y, Li K, Zhang G, Guo Z, Wu X,
Qiu C, Li Y, Wan X, Sui J, et al: Exosomes secreted by
adipose-derived mesenchymal stem cells foster metastasis and
osteosarcoma proliferation by increasing COLGALT2 expression. Front
Cell Dev Biol. 8:3532020. View Article : Google Scholar : PubMed/NCBI
|
|
130
|
Gangadaran P, Rajendran RL, Oh JM, Oh EJ,
Hong CM, Chung HY, Lee J and Ahn BC: Identification of angiogenic
cargo in extracellular vesicles secreted from human adipose
tissue-derived stem cells and induction of angiogenesis in vitro
and in vivo. Pharmaceutics. 13:4952021. View Article : Google Scholar : PubMed/NCBI
|
|
131
|
Khanh VC, Fukushige M, Moriguchi K,
Yamashita T, Osaka M, Hiramatsu Y and Ohneda O: Type 2 diabetes
mellitus induced paracrine effects on breast cancer metastasis
through extracellular vesicles derived from human mesenchymal stem
cells. Stem Cells Dev. 29:1382–1394. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
132
|
Mattiske S, Suetani RJ, Neilsen PM and
Callen DF: The oncogenic role of miR-155 in breast cancer. Cancer
Epidemiol Biomarkers Prev. 21:1236–1243. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
133
|
Balaban S, Shearer RF, Lee LS, van
Geldermalsen M, Schreuder M, Shtein HC, Cairns R, Thomas KC,
Fazakerley DJ, Grewal T, et al: Adipocyte lipolysis links obesity
to breast cancer growth: Adipocyte-derived fatty acids drive breast
cancer cell proliferation and migration. Cancer Metab. 5:12017.
View Article : Google Scholar : PubMed/NCBI
|
|
134
|
Kuo CY and Ann DK: When fats commit
crimes: Fatty acid metabolism, cancer stemness and therapeutic
resistance. Cancer Commun (Lond). 38:472018. View Article : Google Scholar : PubMed/NCBI
|
|
135
|
Zhuang X, Xiang X, Grizzle W, Sun D, Zhang
S, Axtell RC, Ju S, Mu J, Zhang L, Steinman L, et al: Treatment of
brain inflammatory diseases by delivering exosome encapsulated
anti-inflammatory drugs from the nasal region to the brain. Mol
Ther. 19:1769–1779. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
136
|
Hardy J: Amyloid, the presenilins and
Alzheimer's disease. Trends Neurosci. 20:154–159. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
137
|
Selkoe DJ: The cell biology of
beta-amyloid precursor protein and presenilin in Alzheimer's
disease. Trends Cell Biol. 8:447–453. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
138
|
Katsuda T, Tsuchiya R, Kosaka N, Yoshioka
Y, Takagaki K, Oki K, Takeshita F, Sakai Y, Kuroda M and Ochiya T:
Human adipose tissue-derived mesenchymal stem cells secrete
functional neprilysin-bound exosomes. Sci Rep. 3:11972013.
View Article : Google Scholar : PubMed/NCBI
|
|
139
|
Garcia-Contreras M and Thakor AS: Human
adipose tissue-derived mesenchymal stem cells and their
extracellular vesicles modulate lipopolysaccharide activated human
microglia. Cell Death Discov. 7:982021. View Article : Google Scholar : PubMed/NCBI
|
|
140
|
Geng W, Tang H, Luo S, Lv Y, Liang D, Kang
X and Hong W: Exosomes from miRNA-126-modified ADSCs promotes
functional recovery after stroke in rats by improving neurogenesis
and suppressing microglia activation. Am J Transl Res. 11:780–792.
2019.PubMed/NCBI
|
|
141
|
Jiang M, Wang H, Jin M, Yang X, Ji H,
Jiang Y, Zhang H, Wu F, Wu G, Lai X, et al: Exosomes from
MiR-30d-5p-ADSCs reverse acute ischemic stroke-induced,
autophagy-mediated brain injury by promoting M2
microglial/macrophage polarization. Cell Physiol Biochem.
47:864–878. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
142
|
Takahashi Y and Takakura Y: Extracellular
vesicle-based therapeutics: Extracellular vesicles as therapeutic
targets and agents. Pharmacol Ther. 242:1083522023. View Article : Google Scholar : PubMed/NCBI
|
|
143
|
Greening DW, Xu R, Ale A, Hagemeyer CE and
Chen W: Extracellular vesicles as next generation
immunotherapeutics. Semin Cancer Biol. 90:73–100. 2023. View Article : Google Scholar : PubMed/NCBI
|
|
144
|
Kwan HY, Chen M, Xu K and Chen B: The
impact of obesity on adipocyte-derived extracellular vesicles. Cell
Mol Life Sci. 78:7275–7288. 2021. View Article : Google Scholar : PubMed/NCBI
|