Introduction
Breast cancer is currently the most common female
cancer. There are 183,000 new cases each year and 41,000 women
succumb to this disease in the USA in 2000 (1). In 85% of cases the tumor remains
localized and the treatment consists of surgery, radiotherapy ±
chemo and/or hormonotherapy. Despite this treatment, local or
distant relapses occur in approximately 40% of patients. Predictive
risk factors are being used to a greater extent to identify
subgroups of patients who will most likely benefit from adjuvant
treatment. The use of the St. Gallen guidelines (2) has led to the treatment of
approximately 50% of patients after surgery for early breast cancer
with anthracyclin-based chemotherapy sequenced with taxanes
(3). This probabilistic criterion
has resulted in many patients being submitted to aggressive
treatments.
Neoadjuvant chemotherapy is widely used in the
management of patients with locally advanced breast cancer. In
addition to increasing the rates of breast conservation, this
treatment strategy allows the use of pathologic response as an
early surrogate marker for overall survival. The uncertain benefit,
the toxicity of chemotherapy and the existence of alternative
treatments calls for the development of methods to select patients
most likely to benefit.
Using conventional two-dimensional electrophoresis
and mass spectrometry, we previously identified markers of
potential clinical interest in human breast cancer, such as the
molecular chaperone 14-3-3σ which is downregulated in breast cancer
cells as compared with normal breast epithelial cells (4). Surface-enhanced laser
desorption/ionization-time of flight (SELDI-TOF) mass spectrometry
(MS) coupled with appropriate bio-informatic tools have been used
to identify protein patterns related to various stages and types of
solid tumors and serum (5–12). This technology combines
chromatographic fractionation of the proteome using protein
biochips and TOF MS analysis that can be applied to various
clinical samples, such as serum and tissue (13); it allows relatively high-throughput
protein analysis of complex biological samples, with limited
preprocessing steps.
To date, most proteomic-based studies are largely
performed in vitro for the identification of differential
expression levels between parental and chemotherapy-resistant cell
sublines. Only a few small studies are based on fresh breast cancer
tissue samples (14,15) and plasma proteomic evaluations in
this situation have not yet been published.
Herein, we define plasma and tumor proteomic
profiles of primary breast cancer patients and provide evidence
that such an approach may have a significant impact in predicting
response to neoadjuvant chemotherapy. The primary objective of this
study was to define proteomic signatures correlated with a complete
pathological response after neoadjuvant chemotherapy. Secondary
objectives included the study of correlations between proteomic
signatures and nodal involvement, pathological subtypes, clinical
and ultrasound response and menopausal status.
Materials and methods
Patients
Main inclusion criteria were: female patients over
18 years of age, with a histologically proven breast
adenocarcinoma, eligible for neoadjuvant chemotherapy with
anthracyclines and taxanes with no previous chemotherapy for
malignant disease. Information and informed consent were obtained
according to the French law. Exclusion criteria were metastatic
disease, non-adenocarcinoma breast tumors, contraindication of
anthracyclines/taxanes, patient’s refusal of storage of blood and
tumor biopsy and inclusion in another clinical research study.
Treatment
The chemotherapy protocol included a sequence of
FEC100 (epirubicin, 100 mg/m2; cyclophosphamide, 500
mg/m2 and fluorouracil, 500 mg/m2) followed
by docetaxel, 100 mg/m2 on Day 1 every 3 weeks, provided
the neutrophil cell count was over 1,500/mm3. At the
beginning of the study, all patients received 4 cycles of each
regimen. After the publication of the results of the PACS 01
adjuvant trial (3), it was decided
to administer 3 courses of each for a total of 6.
Pathological analysis
The pathological diagnosis included the following
variables: histological type (essentially ductular or lobular),
histoprognostic grading, estradiol and progesterone receptor
status, HER2 positivity on immunohistochemistry or FISH, and Ki-67
hyperexpression. In triple-negative tumors (TNBC), the basal
phenotype was assessed by determining c-Kit and R EGF
hyperexpression.
Inprints of the frozen part of the tumor were
performed to be sure that the tissue extract proteomic analysis was
performed on tumor tissue. The pathological diagnosis, using the
same criteria, was also performed after surgery. The pathological
tumor and nodal responses were assessed according to Sataloff
(16) criteria.
Protein expression profiling
Tumor samples
All tumor samples were processed within 1 h after
collection and rapidly frozen at −80°C.
Plasma samples
Plasma (10 ml of blood) was obtained before the
initiation of neoadjuvant chemotherapy and processed within 1 h
after collection and frozen at −80°C.
Preparation of cytosols
The frozen tissues were weighed, then disrupted and
homogenized in 200 μl of 50 mM Tris-HCl buffer (pH 9.0) containing
7 M urea, 2 M thiourea, 2% CHAPS using a Potter Homogenizer and a
Rotor-Stator homogenizer (Ribolyser, Hybaid). The homogenate was
ultracentrifuged at 105,000 × g for 60 min at 4°C.
The protein concentration of the cytosols was
determined using the Quick Start Bradford Dye Reagent (Bio-Rad
Laboratories Inc., France) based on the method of Bradford
(17).
ProteinChip array analysis
Three types of ProteinChips (Bio-Rad Laboratories)
with a surface chemistry of hydrophobic (H50), cationic (CM10) and
metal affinity (IMAC-Cu) were tested to determine which might
provide the best plasma and tumor cytosol profiles.
Plasma samples were aliquoted (50 μl) and thawed at
−80°C. Each sample (10 μl) was denaturated by adding 90 μl of 50 mM
Tris-HCl buffer (pH 9.0) containing 7 M urea, 2 M thiourea and 2%
CHAPS [(3-cholamidopropyl)dimethylammonio]-propanesulfonic acid).
The mixture was vortex-mixed and shaken for 20 min at room
temperature. Tumor cytosols (100 μg proteins) were diluted in 200
μl of 50 mM Tris-HCl buffer pH 9.0 containing 7 M urea, 2 M
thiourea and 2% CHAPS.
The denatured plasma samples (20 μl) and the diluted
tumor cytosol samples (20 μl) were then diluted (1:10) with the
adequate binding buffer (acetonitrile 10 ml/l, trifluoroacetic acid
1 ml/l, NaCl 150 mM for H50, sodium acetate 100 mM pH 4.0 for CM10
and phosphate-buffer saline (PBS) pH 7.4 for IMAC-Cu). Then 100 μl
was spotted on the ProteinChip array in a 96-well bioprocessor
(Bio-Rad Laboratories). IMAC-Cu ProteinChips were precharged for
activation with 50 mM CuSO4 for 10 min according to the
manufacturer’s instructions (Bio-Rad Laboratories).
After the samples were allowed to bind at room
temperature for 45 min on a platform shaker (Heidolph Titramax
100), the arrays were washed twice with 200 μl adequate binding
buffer for 5 min, followed by two quick rinses with 200 μl
deionized water. After air-drying, 1 μl of saturated sinapinic acid
[5 mg dissolved in 400 μl of acetonitrile/trifluoroacetic acid
(50%/0.5%)] was applied twice to each spot, allowing the array
surface to air-dry 10 min between each application. Proteins bound
to the ProteinChips arrays were detected with the ProteinChip
System Series 4000 (Bio-Rad Laboratories).
Time of flight spectra were generated by averaging
530 laser shots collected at a laser intensity of 2,500 with a
focus mass of 7,000 (for 1,800–10,000 Da proteins), at a laser
intensity of 3,500 with a focus mass of 16,000 (for 10,000–20,000
Da proteins), and finally at a laser intensity of 5,000 with a
focus mass of 40,000 (for 20,000–150,000 Da proteins). External
mass calibration was performed using the All-In-One Peptide
molecular mass standard. Spectra analyses (peak detection, mass
calibration, baseline substraction and total ion current
normalization) were performed using Ciphergen ProteinChip Data
Manager DE Software 4.1.
Reproducibility was estimated using one pool of
plasma and one pool of tumor cytosols. The mean of the CV,
estimated on all the detected peaks both at each laser intensity
tested and on each type of ProteinChip array, ranged from 10 to
20%.
Statistical methods
Clinical and echographic assessments of tumor size,
node involvement and tissue diagnosis were recorded at baseline and
at the end of treatment. Patients with a pathological complete
response (pCR) were considered responders: tumor A (TA)/node A (NA)
or TA/NB. All other categories were considered non-responders.
On the basis of an expected pCR rate of 20%, the
inclusion of 100 breast cancer patients treated with neoadjuvant
chemotherapy allowed a 95% confidence interval width of ±8%.
Initial demographic and tumor characteristics for categorical
variables are presented as frequencies and percentages. Continuous
variables are presented as medians and range. For the receiver
operating characteristic curve (ROC) analyses, cytosol and plasma
variables were transformed to the logarithmic scale if deemed
necessary in order to stabilize the variance.
The search for candidate proteins was first
performed by univariate analysis using the non-parametric Wilcoxon
test comparing responders and non-responders. Multivariate analyses
using a generalized ROC criterion were then performed to obtain a
proteomic signature separately for cytosol and plasma and then in
combination (18). This technique
selects the variable combinations which maximize the area under the
curve (AUC). Each cytosol and plasma model was then validated
internally on 500 random samples with replacement on the whole
dataset. Logistic regression models were then applied selecting
variables according to the Akaike Information Criterion (AIC). The
percentage of times each variable was selected was extracted. Only
those variables which were selected in >80% of models were
retained. Results of statistical tests were considered significant
at the 5% level. The final model was adjusted for significant
clinical variables.
Results
Demographic and clinical
characteristics
One hundred and forty-nine breast cancer patients
were enrolled between February 2004 and January 2009 from 3
centers. A total of 8 patients were excluded: 4 were ineligible
(prior chemotherapy in one and metastatic disease in 3); and 4 were
non-evaluable (one patient was untreated, one patient received only
one cycle due to toxicity, one had no tumor nor blood plasma sample
and one patient developed a carcinomatous meningitis while
receiving neoadjuvant chemotherapy).
Clinical characteristics for the 141 patients
analyzed are presented in Table I.
Median age was 46 years (range, 26–74). Median tumor size was 40 mm
(range, 10–130). All patients received a minimum of three cycles of
chemotherapy. Overall, 82 (58%) patients received 3 cycles of FEC
and 3 cycles of docetaxel; 38 patients received eight cycles. The
reason for not receiving 6 or 8 cycles were side effects which
prevented the continuation of the same regimen.
 | Table ICharacteristics of the breast cancer
patients before chemotherapy. |
Table I
Characteristics of the breast cancer
patients before chemotherapy.
| Characteristics | n=141
n (%) |
|---|
| Site of tumor |
| Right | 76 (54) |
| Left | 65 (46) |
| Tumor stage |
| T1 | 9 (6) |
| T2 | 83 (59) |
| T3 | 30 (21) |
| T4 | 19 (14) |
| Nodal
involvement |
| N0 | 73 (52) |
| N1 | 62 (45) |
| N2 | 4 (3) |
| Missing | 2 |
| Histology |
| Ductal | 127 (90) |
| Lobular | 8 (6) |
| Other | 6 (4) |
| Missing | 2 |
| Differentiation |
| Well | 8 (7) |
| Medium | 33 (28) |
| Poor | 75 (65) |
| SBR grade |
| I | 10 (9) |
| II | 74 (67) |
| III | 26 (24) |
| NP | 17 |
| Missing | 15 |
| Hormone receptor
status |
| ER+
PR+ | 63 (45) |
| ER+
PR− | 23 (16) |
| ER−
PR+ | 3 (2) |
| ER−
PR− | 52 (37) |
| Ki-67 index |
| <15 | 10 (7) |
| ≥15 | 40 (93) |
| Missing | 91 |
Overall, 89 patients (63%) had conservative surgery,
and 136 (96%) had an axillary clearance; 98% of patients had
surgery within 6 weeks after the last chemotherapy cycle.
The pathological complete response rate according to
Sataloff was 18.8% (95% CI, 12.6–25.7). Negative hormone receptor
tumors showed a significantly higher pCR rate then positive ones.
In addition, in spite of many missing data for Ki-67, not a single
patient with Ki-67 <15% had a pCR (Table II).
 | Table IIComplete pathological response
according to clinical variables. |
Table II
Complete pathological response
according to clinical variables.
|
Characteristics | Non-response
(n=114), n (%) | Response (n=27), n
(%) | P-value |
|---|
| Surgery |
| Conservative | 68 (60) | 21 (78) | 0.079 |
| Mastectomy | 46 (40) | 6 (22) | |
| Side |
| Right | 65 (57) | 11 (41) | 0.127 |
| Left | 49 (43) | 16 (59) | |
| Tumor stage |
| T1 | 7 (6) | 2 (7) | 0.783 |
| T2 | 66 (58) | 17 (63) | |
| T3 | 24 (21) | 6 (23) | |
| T4 | 17 (15) | 2 (7) | |
| Nodal
involvement |
| N0 | 59 (52) | 14 (56) | 0.700 |
| N+ | 55 (48) | 11 (44) | |
| SBR stage |
| I | 8 (9) | 2 (10) | 0.304 |
| II | 63 (70) | 10 (53) | |
| III | 19 (21) | 7 (37) | |
| ER status |
| Negative | 36 (32) | 18 (69) | 0.0004 |
| Positive | 78 (68) | 8 (31) | |
| PR status |
| Negative | 54 (47) | 20 (77) | 0.0064 |
| Positive | 60 (53) | 6 (23) | |
| HER2 status |
| Negative | 70 (75) | 16 (73) | 0.867 |
| Positive | 24 (25) | 6 (27) | |
| Ki-67 index |
| <15 | 10 (24) | 0 | 0.098 |
| ≥15 | 31 (76) | 9 (100) | |
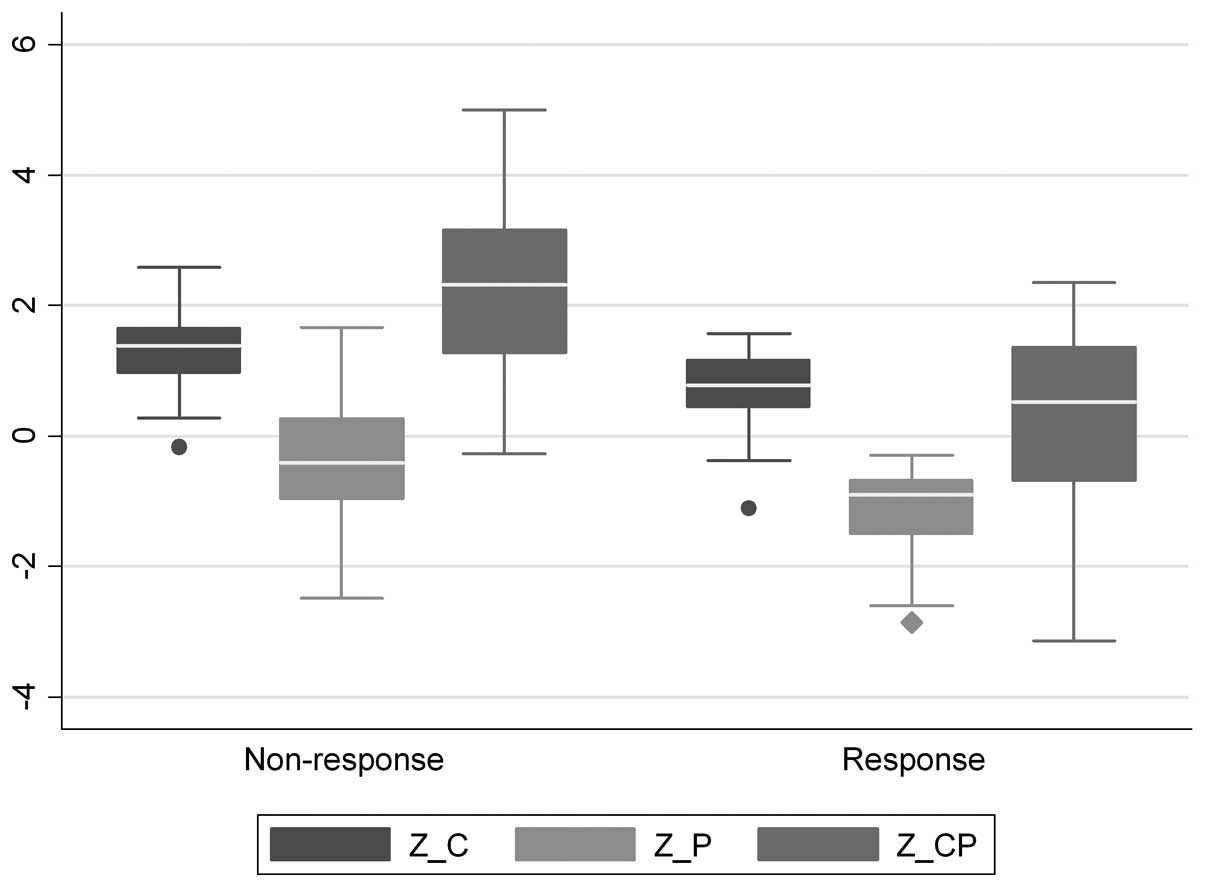
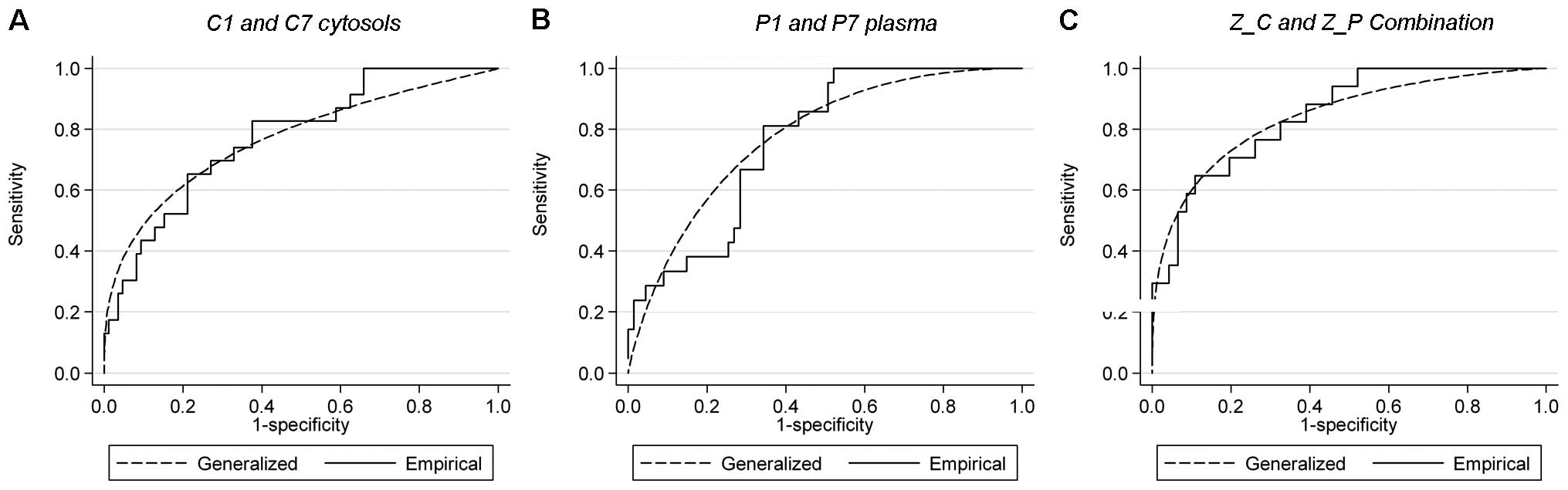
Cytosols
One hundred and eight patients (77%) were evaluable
for cytosol analysis. Using IMAC-Cu and H50 arrays, 150 and 131
different proteins were observed respectively and their levels were
statistically different between responders and non-responders for 4
proteins (IMAC-Cu) and for 2 proteins (H50), respectively. Using
CM10 pH4 arrays, 180 different proteins were observed. For 8
proteins, the levels were statistically different between
responders and non-responders (Table
III, Fig. 1). The generalized
ROC criterion identified cytosolic proteins C1, C7 and C8 as the
best three variables. However, only C1 and C7 were selected since
they were subsequently validated in 95.0 and 85.6% of models,
respectively. On the other hand, C8 was only present in 59.2% of
the models and was not retained. The AUC for log(C1) and log(C7)
was equal to AUC = 0.768 (95% CI, 0.623–0.858) (Fig. 2A).
 | Table IIIpCR according to the proteomic
analysis of the cytosols and the plasma. |
Table III
pCR according to the proteomic
analysis of the cytosols and the plasma.
| Non-response,
median (range) | Response, median
(range) | P-value |
|---|
| Cytosols (protein
molecular weight, m/z) |
| C1
(3077) | 5.5
(1.1–83.2) | 3.1
(0.1–23.0) |
<0.0001 |
| C2 (4629) | 301.7
(6.6–749.7) | 164.7
(6.8–549.5) | 0.035 |
| C3 (44002) | 20.6
(0.1–58.1) | 14.0
(1.8–40.9) | 0.024 |
| C4 (116996) | 22.0
(0.1–71.3) | 13.1
(2.0–35.7) | 0.0116 |
| C5 (3556) | 6.9
(0.1–133.7) | 3.1 (0.6–51.8) | 0.009 |
| C6 (3348) | 53.0
(3.8–139.1) | 25.9
(2.8–149.9) | 0.056 |
| C7
(5071) | 2.9
(0.1–13.0) | 2.0
(0.6–3.9) | 0.006 |
| C8 (5793) | 0.17
(0.00–0.46) | 0.16
(0.05–0.23) | 0.022 |
| Z_C =
log(C1)+log(C7) | 1.39
(−0.16–2.59) | 0.77
(−1.11–1.57) | <0.00001 |
| Plasma (protein
molecular weight, m/z) |
| P1
(7948) | 5.4
(0.1–114.5) | 2.9
(0.1–19.9) | 0.022 |
| P2 (4752) | 5.0 (0.1–32) | 2.1 (0.1–11.1) | 0.036 |
| P3 (74986) | 16.0
(0.1–98.5) | 8.4 (0.1–31.5) | 0.0398 |
| P4 (89539) | 33.9
(9.9–172.7) | 17.7
(8.8–132.2) | 0.012 |
| P5 (116754) | 14.0
(1.5–59.7) | 8.3 (3.6–53.3) | 0.026 |
| P6 (115505) | 2.8 (0.4–13.8) | 4.1 (1.1–14.9) | 0.092 |
| P7
(101771) | 4.0
(0.2–11.0) | 5.5
(0.9–8.8) | 0.029 |
| P8 (8052) | 5.4 (2.6–9.4) | 6.4 (3.7–10.3) | 0.021 |
| P9 (7849) | 1.7 (0.7–3.9) | 2.3 (0.9–4.7) | 0.080 |
| P10 (7577) | 1.6 (0.1–4.7) | 2.4 (0.8–4.8) | 0.048 |
| P11 (100104) | 0.9 (0.1–3.7) | 1.4 (0.2–3.3) | 0.039 |
| P12 (43422) | 0.8 (0.1–2.9) | 1.3 (0.3–3.1) | 0.035 |
| Z_P =
log(P1)−2*log(P7) | −0.41
(−2.49–1.67) | −0.90
(−2.85–−0.29) | 0.0004 |
| Cytosol and
plasma |
| 2*Z_C + Z_P | 2.32
(−0.27–4.99) | 0.53
(−3.14–2.36) | <0.0001 |
Plasma
Eighty-eight (62%) patients were evaluable for
plasma analysis. Using CM10 pH4 and H50 arrays, 85 and 107
different proteins were observed, respectively, and their levels
were statistically different between responders and non-responders
for 2 proteins (CM10 pH4) and 6 proteins (H50). Using IMAC-Cu
arrays, 98 different proteins were observed. For 12 proteins, the
levels were statistically different between the two populations
(Table III, Fig. 1). The generalized ROC criterion
identified plasma proteins P1, P2 and P7 as the best three
variables. However, only P1 and P7 were selected since they were
validated in 94.8 and 97.6% of models respectively. On the other
hand, P2 was only present in 55.0% of the models and was not
retained. The AUC for log(P1) and log(P7) was equal to AUC = 0.774
(95% CI, 0.631–0.865) (Fig.
2B).
Cytosol and plasma combination
In an effort to use both cytosol and plasma results
for constructing a combined proteomic signature, the weighted
combination variable Z = 2*Z_C + Z_P was generated from the integer
values of the coefficients estimated from the mROC analysis (1.088
and 0.509, respectively). The AUC for this combination was equal to
AUC = 0.843 (95% CI, 0.692–0.933) (Fig.
2C). Overall correct classification was 87.3% (Table IV). The proteomic signature
remained statistically significant when adjusted for hormone
receptor status. Moreover, in the population of patients with
positive Ki-67, the proteomic signature remained statistically
significant.
 | Table IVROC analysis of the cytosols and
plasma combination. |
Table IV
ROC analysis of the cytosols and
plasma combination.
| Term | Result |
|---|
| AUC (95% CI) | 0.84
(0.69–0.93) |
| Sensitivity
(%) | 89.1 |
| Specificity
(%) | 82.4 |
| Positive predictive
value (%) | 93.2 |
| Negative predictive
value (%) | 73.7 |
| Overall correct
classification (%) | 87.3 |
Due to missing data, only 63 (45%) samples could be
evaluated for the combination. However, no significant difference
in patient and tumor characteristics were noted for patients
included and excluded from the combination analysis (data not
shown).
Discussion
Our results showed that proteomic analysis in the
plasma, in the tumor and a combination of results in the plasma and
the tumor could differentiate complete pathological responders and
non-responders in breast cancer patients receiving neoadjuvant
chemotherapy. Two plasma and two cytosolic proteins were selected
and a combined plasma and tumor signature was generated. This
signature remained statistically significant when adjusted for
hormone receptor status and in Ki-67-positive patients.
Overall, the study population was similar to the
patient population of other neoadjuvant studies. Ninety-four
percent of patients had a tumor >2 cm (median tumor size, 4 cm).
Nearly half of them had positive axillary nodes. Only 61% of the
tumors had positive estradiol receptors and 47% were positive for
progesterone receptors. Twenty-four percent of tumors were grade 3
and the median value of Ki-67 was 30%. Twenty-five percent of
tumors were HER2-positive (either by immunohistochemistry or SISH).
This population had a high tumor burden and aggressive tumor.
SELDI-TOF MS profiling appears to be a promising
tool for diagnosis (6–7,11,19).
The use of such a technique in relation to therapeutic response
prediction has been limited (20).
In the present study, we used this technology on both plasma and
cytosols to predict the therapeutic response in a series of breast
cancer patients receiving neoadjuvant chemotherapy.
In both plasma and cytosols, the assays were
performed using three types of ProteinChip arrays (CM10 pH4,
IMAC-Cu and H50). In cytosols, CM10 pH4 ProteinChip arrays appeared
to be the best arrays to discriminate between responder and
non-responder patients, whereas IMAC-Cu array was the best
discriminator in plasma.
In the present study, no data was contained
concerning the characterization of the proteins of the established
signature. It is noteworthy that relevant biomarkers identified in
SELDI-TOF profiling studies are in most cases non-specific host
response-generated proteins at rather high levels (21). For example, in such studies,
haptoglobin, transferrin, or the C3A or C3B complement have been
evidenced. Furthermore, ubiquitin and ferritin light chain,
corresponding to the two peaks of interest, were evidenced using
SELDI-TOF-MS screening to identify differentially expressed
cytosolic proteins with a prognostic impact in node-negative breast
cancer patients with no relapse vs. patients with metastatic
relapse (22).
We demonstrated that plasma and tumor proteomic
profiles obtained prior to neoadjuvant chemotherapy in primary
breast cancer may predict a complete pathological response to
treatment. Comparable results were found by He et
al(15) in a smaller
population. In the entire group, a single peak at mass/charge ratio
(m/z) of 16,906 correctly separated 88.9% of the tumors with
pathological complete response and 91.7% of the resistant tumors.
These data suggest that breast cancer protein biomarkers may be
used to pre-select patients for optimal chemotherapeutic
treatments. Other studies have identified potential markers related
to neoadjuvant chemotherapy using SELDI-TOF MS by comparing the
proteomic profiles before and after treatment. Relatively few
changes were identified in plasma by Pusztai et al(23). They detected only a single
chemotherapy-inducible SELDI-MS peak [mass/charge ratio (m/z),
2790] that was induced by paclitaxel and, to a lesser extent, by
FAC chemotherapy. Recently, the intensities of eight different
protein peaks were demonstrated to be higher in breast cancer
tissue extracts after neoadjuvant chemotherapy than those before
neoadjuvant chemotherapy (24).
Although further experiments are needed to prove the reliability of
these eight proteins, these results will help in the establishment
of protein models based on drug resistance-related protein peaks to
screen whether a patient is suitable for adopting neoadjuvant
chemotherapy and to improve cancer treatment.
The pCR according to Sataloff (TA NA, TA, NB) was in
the lower range of the published results for anthracycline-taxane
combining regimens (25). One
reason for this relatively low rate could be the very restrictive
definition of the pCR related to the surgical specimen process for
pathological analysis as previously described (26). The prognostic factors of response
were ER (P=0.0004) and PR (P=0.006) negativity and Ki-67 above the
median value of 30% (P=0.003). No pCR was observed for Ki-67 below
15%. These factors have been previously reported in many
neoadjuvant studies (27).
Similarly, the pCR rate was higher in triple-negative tumors
(28) and in ductular than in
lobular cancer (29). Several
molecular signatures are being tested in the neoadjuvant setting
(30–33). However, the benefit of using genetic
predictors over usual pathological biomarkers is not clear. Our
study showed that a proteomic analysis of plasma and cytosol could
also predict pCR in breast cancer patients treated with FEC and
docetaxel. The role of a proteomic analysis in clinical practice
remains to be defined.
References
|
1
|
Greenlee RT, Murray T, Bolden S and Wingo
PA: Cancer statistics, 2000. CA Cancer J Clin. 50:7–33. 2000.
View Article : Google Scholar
|
|
2
|
Goldhirsch A, Wood WC, Gelber RD, Coates
AS, Thurlimann B and Senn HJ: Meeting highlights: updated
international expert consensus on the primary therapy of early
breast cancer. J Clin Oncol. 21:3357–3365. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Roche H, Fumoleau P, Spielman M, et al:
Sequential adjuvant epirubicin-based and docetaxel chemotherapy for
node-positive breast cancer patients: the FNCLCC PACS 01 Trial. J
Clin Oncol. 24:5664–5671. 2006. View Article : Google Scholar
|
|
4
|
Vercoutter-Edouart AS, Lemoine J, Le
Bourhis X, et al: Proteomic analysis reveals that 14-3-3sigma is
down-regulated in human breast cancer cells. Cancer Res. 61:76–80.
2001.PubMed/NCBI
|
|
5
|
Adam BL, Qu Y, Davis JW, et al: Serum
protein fingerprinting coupled with a pattern-matching algorithm
distinguishes prostate cancer from benign prostate hyperplasia and
healthy men. Cancer Res. 62:3609–3614. 2002.
|
|
6
|
Petricoin EF, Ardekani AM, Hitt BA, et al:
Use of proteomic patterns in serum to identify ovarian cancer.
Lancet. 359:572–577. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Petricoin EF III, Ornstein DK, Paweletz
CP, et al: Serum proteomic patterns for detection of prostate
cancer. J Natl Cancer Inst. 94:1576–1578. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Vlahou A, Laronga C, Wilson L, et al: A
novel approach toward development of a rapid blood test for breast
cancer. Clin Breast Cancer. 4:203–209. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Koopmann J, Zhang Z, White N, et al: Serum
diagnosis of pancreatic adenocarcinoma using surface-enhanced laser
desorption and ionization mass spectrometry. Clin Cancer Res.
10:860–868. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wadsworth JT, Somers KD, Cazares LH, et
al: Serum protein profiles to identify head and neck cancer. Clin
Cancer Res. 10:1625–1632. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Zhang Z, Bast RC Jr, Yu Y, et al: Three
biomarkers identified from serum proteomic analysis for the
detection of early stage ovarian cancer. Cancer Res. 64:5882–5890.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fung ET, Yip TT, Lomas L, et al:
Classification of cancer types by measuring variants of host
response proteins using SELDI serum assays. Int J Cancer.
115:783–789. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Fung ET, Thulasiraman V, Weinberger SR and
Dalmasso EA: Protein biochips for differential profiling. Curr Opin
Biotechnol. 12:65–69. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hodgkinson VC, Eagle GL, Drew PJ, Lind MJ
and Cawkwell L: Biomarkers of chemotherapy resistance in breast
cancer identified by proteomics: current status. Cancer Lett.
294:13–24. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
He J, Shen D, Chung DU, Saxton RE,
Whitelegge JP, Faull KF and Chang HR: Tumor proteomic profiling
predicts the susceptibility of breast cancer to chemotherapy. Int J
Oncol. 35:683–692. 2009.PubMed/NCBI
|
|
16
|
Sataloff DM, Mason BA, Prestipino AJ,
Seinige VL, Lieber CP and Baloch Z: Pathologic response to
induction chemotherapy in locally advanced carcinoma of the breast:
a determinant of outcome. J Am Coll Surg. 180:297–306.
1995.PubMed/NCBI
|
|
17
|
Bradford MM: Rapid and sensitive method
for the quantitation of microgram quantities of protein utilizing
the principle of protein-dye binding. Anal Biochem. 72:248–254.
1976. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kramar A, Farraggi D, Fortuné A and Reiser
B: mROC: a computer program for combining tumour markers in
predicting disease states. Comput Methods Programs Biomed.
66:199–207. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kozak KR, Amneus MW, Pusey SM, et al:
Identification of biomarkers for ovarian cancer using strong
anion-exchange ProteinChips: potential use in diagnosis and
prognosis. Proc Natl Acad Sci USA. 100:12343–12348. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Gonçalves A, Esterni B, Bertucci F, et al:
Postoperative serum proteomic profiles may predict metastatic
relapse in high-riskprimary breast cancer patients receiving
adjuvant chemotherapy. Oncogene. 25:981–989. 2006.PubMed/NCBI
|
|
21
|
Diamandis EP: Analysis of serum proteomic
patterns for early cancer diagnosis: drawing attention to potential
problems. J Natl Cancer Inst. 96:353–356. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Ricolleau G, Charbonnel C, Lodé L, et al:
Surface-enhanced laser desorption/ionization time of flight mass
spectrometry protein profiling identifies ubiquitin and ferritin
light chain as prognostic biomarkers in node-negative breast cancer
tumors. Proteomics. 6:1963–1975. 2006. View Article : Google Scholar
|
|
23
|
Pusztai L, Gregory BW, Baggerly KA, et al:
Pharmacoproteomic analysis of prechemotherapy and postchemotherapy
plasma samples from patients receiving neoadjuvant or adjuvant
chemotherapy for breast carcinoma. Cancer. 100:1814–1822. 2004.
View Article : Google Scholar
|
|
24
|
Zhang K, Yuan K, Wu H, et al:
Identification of potential markers related to neoadjuvant
chemotherapy sensitivity of breast cancer by SELDI-TOF MS. Appl
Biochem Biotechnol. 166:753–763. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Dang CT and Hudis C: Preoperative
chemotherapy for operable breast cancer. Diseases of the Breast.
Harris JR, Lippman ME, Morrow M and Osborne CK:
WoltersKluwer/Lippincott Williams &Williams; Philadelphia: pp.
715–723. 2010
|
|
26
|
Mailliez A, Baranzelli MC, Giard S, et al:
Is there a reliable method to assess the complete pathologic
response on the tumor after neo-adjuvant chemotherapy in
inflammatory breast cancer toward recommendations for the
pathologic process? Experience in 56 patients treated in a single
institution. Breast J. 16:464–471. 2010. View Article : Google Scholar
|
|
27
|
Penault-Llorca F, Abrial C, Raolelfils I,
et al: Changes and predictive and prognostic value of the mitotic
index, Ki-67, cyclin D1, and cyclo-oxygenase-2 in 710 operable
breast cancer patients treated with neoadjuvant chemotherapy.
Oncologist. 13:1235–1245. 2008. View Article : Google Scholar
|
|
28
|
Liedtke C, Mazouni C, Hess KR, et al:
Response to neoadjuvant therapy and long-term survival in patients
with triple-negative breast cancer. J Clin Oncol. 26:1275–1281.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Katz A, Saad ED, Porter P and Pusztai L:
Primary systemic chemotherapy of invasive lobular carcinoma of the
breast. Lancet Oncol. 8:55–62. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Liedtke C, Hatzis C, Symmans WF, et al:
Genomic grade index is associated with response to chemotherapy in
patients with breast cancer. J Clin Oncol. 27:3185–3191. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Straver ME, Glas AM, Hannemann J, et al:
The 70-gene signature as a response predictor for neoadjuvant
chemotherapy in breast cancer. Breast Cancer Res Treat.
119:551–558. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Tabchy A, Valero V, Vidaurre T, et al:
Evaluation of a 30-gene paclitaxel, fluorouracil, doxorubicin, and
cyclophosphamide chemotherapy response predictor in a multicenter
randomized trial in breast cancer. Clin Cancer Res. 16:5351–5361.
2010. View Article : Google Scholar
|
|
33
|
Lee JK, Coutant C, Kim YC, et al:
Prospective comparison of clinical and genomic multivariate
predictors of response to neoadjuvant chemotherapy in breast
cancer. Clin Cancer Res. 16:711–718. 2010. View Article : Google Scholar : PubMed/NCBI
|