Introduction
Biliary tract carcinomas (BTCs), which include
gallbladder carcinomas (GBCs) and cholangiocarcinomas (bile duct
cancer), are rapidly growing lethal tumors associated with the
digestive system (1). The 5-year
survival rate is <10% in patients with advanced or metastatic
BTCs (2). Since the current
treatments are minimally effective, a multi-omic approach combining
genomic, transcriptomic, and metabonomic landscapes would be
beneficial and could lead to improved treatments and possibly
earlier diagnosis.
At present, the concept of precision or personalized
medicine as a treatment strategy for many types of cancer has been
widely recognized (3). When utilizing
this type of treatment strategy, one or several actionable
mutations typically provide drug targets. Thus, appropriate
biopsies and technologies are required to identify relevant
biomarkers, such as single nucleotide variations (SNVs), insertion
and deletions (Indels), gene fusions, copy number variations
(CNVs), or aberrant expression (4).
Previous studies examining biliary tract tumors have utilized
genetic mutational profiling (5).
Moreover, in BTCs, gene mutations in ERBB2, PIK3CA, FGFR,
and IDH1 have been utilized as drug targets (6–9). However,
obtaining BTC tissue samples is challenging due to the anatomical
complexity of the biliary tract system. These tumors are typically
characterized by a small lesion size, potentially severe biliary
hemorrhaging, and a high perforation risk, which limits the use of
endoscopic retrograde cholangiopancreatography (ERCP) with
intraductal ultrasonography (IDUS)-guided fine needle aspiration. A
promising solution is the use of cell-free DNA (cfDNA), DNA
released by tumor and normal cells that could potentially be the
basis for liquid biopsies. This could provide tumor genomic
information in a less invasive way than the current methods
(10). Previous studies have revealed
that cfDNA can be utilized to identify actionable mutations and
predict therapeutic responses in non-small cell lung cancer (NSCLC)
(11–14). In the present study, bile cfDNA that
was obtained from BTC patients as a minimally invasive ‘liquid
biopsy’ method was subsequently examined using targeted deep
sequencing to identify somatic variants.
Materials and methods
Clinical specimens and data
collection
The present study was approved by the Ethics
Committee of the Shanghai Eastern Hepatobiliary Surgery Hospital,
Navy Military Medical University (Second Military Medical
University) (EHBHKY2018-K-003). Ten BTC patients, four with
gallbladder carcinomas and six with cholangiocarcinomas (Table I), were evaluated in the present
study. Each of the patients provided a bile sample and paired
formalin-fixed paraffin-embedded (FFPE) tumor tissue samples were
obtained from the clinical sample bank at the Department of Biliary
II, Shanghai Eastern Hepatobiliary Surgery Hospital, Navy Military
Medical University. The samples were collected from August 2017 to
March 2018. Patient status was confirmed by surgical pathology, and
FFPE specimens were reviewed by a pathologist to ensure a cancer
cell content ≥20%. All of the patients provided written informed
consent for the examination of their samples and the use of their
clinical data.
 | Table I.Characteristics of ten patients with
biliary tract cancer that received surgery. |
Table I.
Characteristics of ten patients with
biliary tract cancer that received surgery.
|
Characteristics | N |
|---|
| Age, median (range)
in years | 68 (44–74) |
| Sex |
|
|
Male | 4 |
|
Female | 6 |
| Cancer type |
|
|
Gallbladder carcinoma | 4 |
|
Cholangiocarcinomas | 6 |
| Incidence site |
|
|
Gallbladder | 4 |
|
Intrahepatic bile duct | 1 |
| Hilar
bile duct | 4 |
| Distal
bile duct | 1 |
| AJCC stage |
|
| I | 0 |
| II | 4 |
|
III | 3 |
| IV | 3 |
| Operation type |
|
| R0 | 8 |
| R1 | 1 |
| R2 | 1 |
| Gallbladder
stones |
|
|
Yes | 4 |
| No | 6 |
| Cholecystitis |
|
|
Yes | 4 |
| No | 6 |
| Method of obtaining
bile |
|
|
PTCD | 5 |
|
Operation | 5 |
| Location of
obtaining bile |
|
|
Gallbladder | 4 |
|
Intrahepatic bile duct | 1 |
| Hilar
bile duct | 4 |
| Distal
bile duct | 1 |
| AFP, median (range)
ng/ml | 3.4 (2.4–8.0) |
| CEA, median (range)
ng/ml | 4.5 (1.3–83.9) |
| CA19-9, median
(range) U/ml | 154.6
(8.8–1,000.0) |
| Total bilirubin,
median (range) µmol/l | 42.2
(8.8–305.6) |
DNA extraction from FFPE and bile
samples
To extract DNA from FFPE samples, 4-µm thick
sections were processed using a QIAamp DNA FFPE Tissue Kit (Qiagen)
according to the manufacturer's instructions. The DNA
concentrations were determined using a Qubit™ 3.0 Fluorometer
(Thermo Fisher Scientific, Inc.), and size distributions were
analyzed using LabChip GX Touch 24 nucleic acid analyzer
(PerkinElmer, Inc.). To obtain bile cfDNA, bile (3 ml) was
collected in 4 ml BD Vacutainer blood collection tubes (BD
Biosciences) and processed within 1 h after collection. First, the
bile samples were centrifuged at 1,600 × g for 15 min at room
temperature, and the supernatants were carefully transferred to new
2-ml tubes (Eppendorf). The samples were then centrifuged at 16,000
× g for 10 min at room temperature, and the supernatants were
collected and examined under a light microscope to ensure that
there were no residual cells or debris. Samples were then aliquoted
and stored at −80°C. Bile cfDNA was extracted using a QIAamp
Circulating Nucleic Acid kit (Qiagen) according to the
manufacturer's instructions. Bile cfDNA concentrations were
determined using a Qubit dsDNA HS Assay kit (Life Technologies;
Thermo Fisher Scientific, Inc.), and cfDNA size distributions were
analyzed by Agilent 2100 Bioanalyzer (Agilent Technologies,
Inc.).
Tumor tissue analysis by targeted deep
sequencing and variant calling
Tumor tissues from the 10 BTC patients were analyzed
utilizing a previously established targeted deep sequencing method
(15). Experimental procedures and
variant calling were performed as previously described, with 150
tumor-associated genes examined (Table
SI). This 150-gene list of targeted deep sequencing was
comprised of highly recurrent and known important regulatory genes
of biliary tract carcinoma, such as TP53, KRAS, NRAS, ERBB2,
ERBB3, CDKN2A, PIK3CA, NF1, among others. The cut-off of mutant
allele frequencies (MAFs) in tumor tissue was ≥0.01.
Bile cell-free DNA analysis by
targeted deep sequencing and variant calling
Bile cfDNA samples were evaluated using a previously
established targeted deep sequencing platform for cfDNA with a
unique identification (UID) indexed capturing-based sequencing
(UC-Seq) to establish a mutational profile (11). The same gene panel that was used for
the tumor samples was also utilized. Prior to sequencing, the bile
cfDNAs were fragmented into sizes ranging from 200 to 400 bp using
the Covaris S2 Sonolab (Covaris, Inc.), with the remaining
procedures and variant calling performed as previously described
(11). The cut-off of mutant allele
frequencies (MAFs) in bile cfDNA was ≥0.001.
Statistical analysis
A Fisher's exact test was used to assess the
significance and sensitivity differences for identifying mutations
within groups, such as the sample collection, cancer stage, and
tumor site. A P-value ≤0.05 was considered to indicate a
statistically significant difference.
Results
Clinical information of BTC
patients
In the present study, 10 BTC patients (four males
and six females) with a median age of 68 years (range: 44–74) at
the time of diagnosis (Table I) were
examined. Four of the patients had gallbladder carcinomas and six
had bile duct cancer (one intrahepatic, four hilar, and one distal
cholangiocarcinoma). Based on the seventh edition of the American
Joint Committee on Cancer (AJCC) staging system for BTC (16), four (40%) patients had stage II, three
(30%) patients had stage III, and three (30%) patients had stage IV
(Table I). Four patients carried
gallbladder stones and cholecystitis, while the other six patients
did not. Percutaneous transhepatic cholangial drainage (PTCD) and
operation are regarded as two different methods of extracting the
bile. The origin of the obtained bile was respectively the
gallbladder (four patients), the intrahepatic bile duct (one
patient), the hilar bile duct (four patients) and the distal bile
duct (one patient). Out of the 10 patients with BTCs, eight
received a radical resection (R0), while the other two patients
underwent R1 and R2 resections.
Bile cfDNA fragment size
distributions
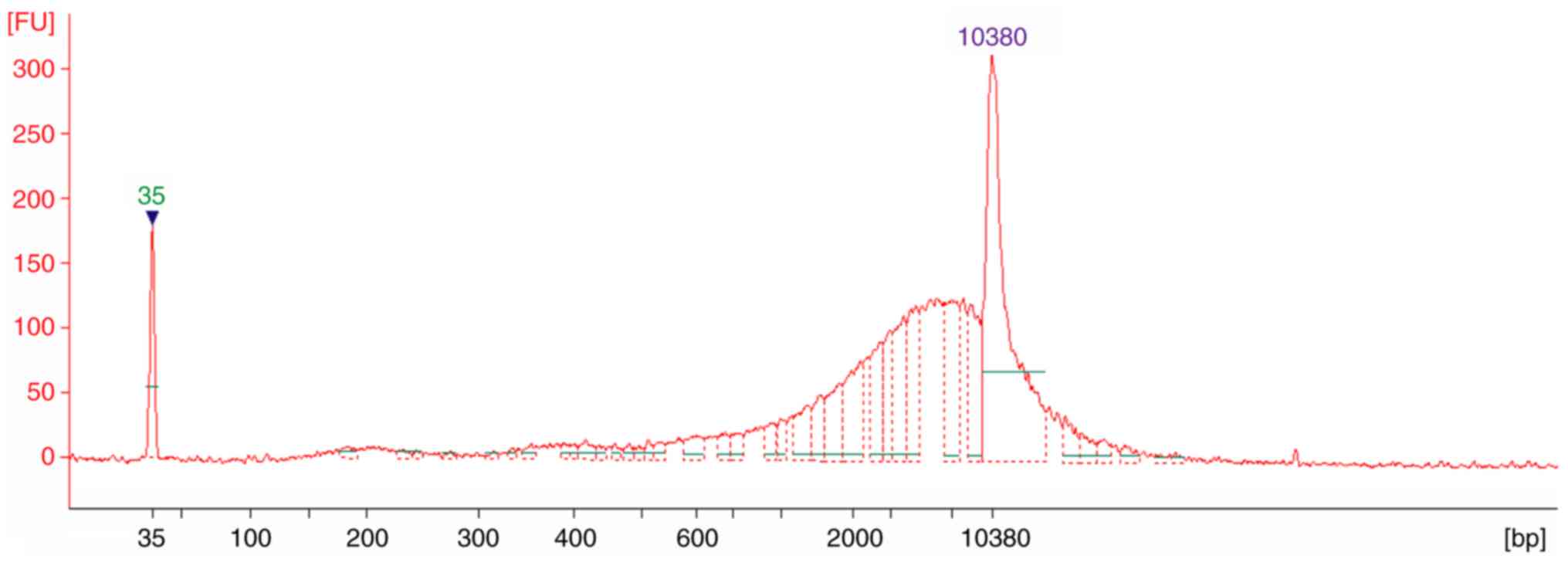
To examine the distributions of bile cfDNA
fragments, samples were analyzed using an Agilent 2100 Bioanalyzer.
The electropherograms revealed that all 10 of the samples had
similar distributions, which sheared to ~6,000 bp (Fig. 1). This result indicated that long DNA
fragments are more prevalent among bile cfDNAs, which is not
consistent with findings from plasma cfDNA (11).
BTC patient bile cfDNA mutational
profiles
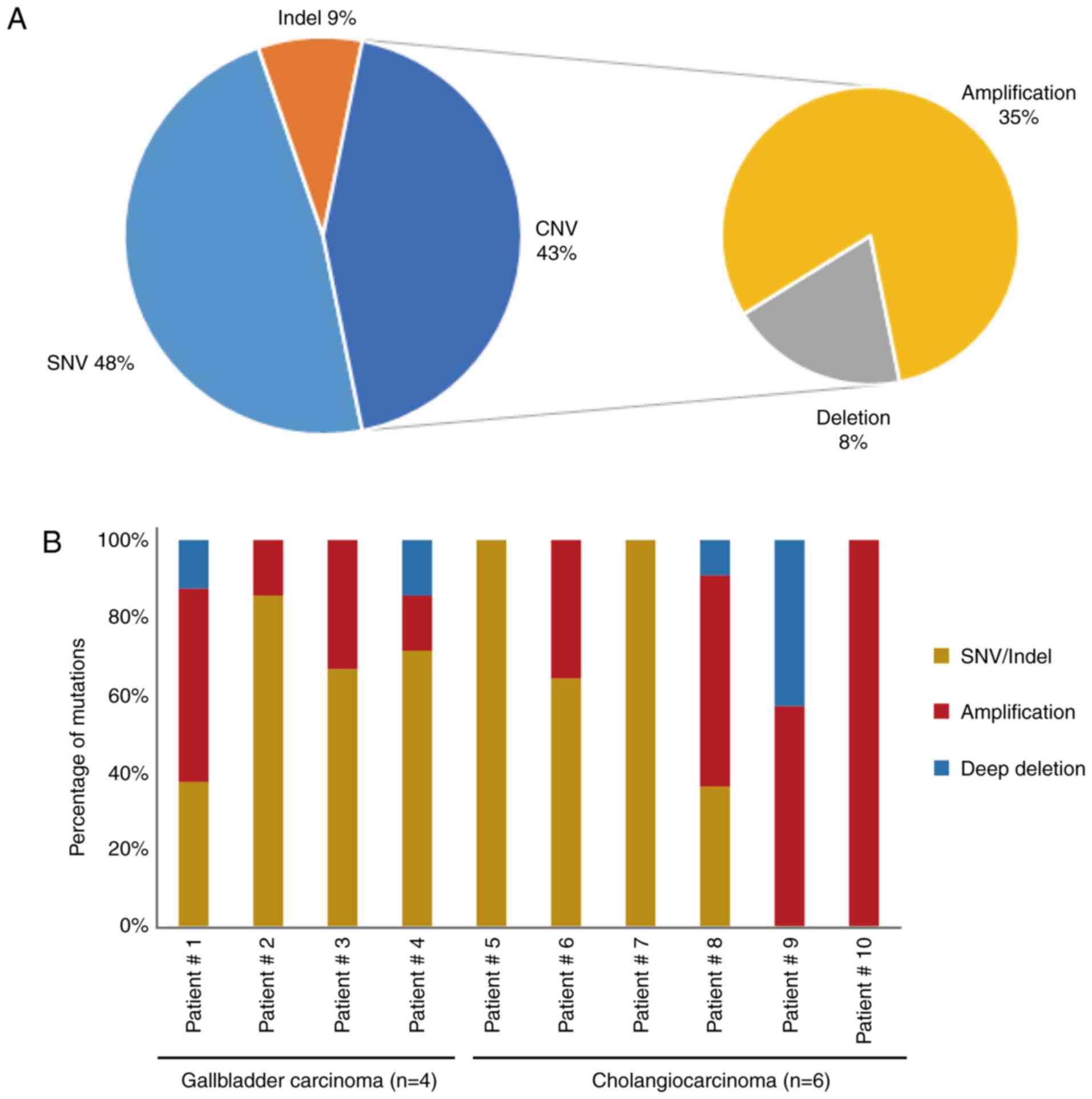
To explore the mutational landscape, the obtained
bile cfDNA was sequenced using targeted deep sequencing, which is
able to detect SNVs, Indels and CNVs concurrently, and a panel of
150 tumor-related genes was examined. The mean sequencing coverage
for the bile cfDNA was over 3,000× with barcodes (Table SII). A total of 71 unique somatic
mutations, including SNVs (48%), Indels (9%), CNVs (35%), and deep
deletions (8%), were revealed (Fig.
2A and Table II). Further
analysis of the gene mutational profiles revealed that in six of
the patients, SNVs and Indels accounted for more than half of the
mutations. In two of the bile cfDNA samples (Patients #5 and #7),
only SNVs and Indels were present; while in one sample (Patient
#10), only CNVs were present (Fig.
2B). Furthermore, the mutational profiles revealed that of the
SNV/Indel mutations, the highest variation was observed in
TP53 (70%), followed by KRAS (30%), NOTCH1
(20%), NOTCH2 (20%), and KMT2A (20%). Among the CNV
mutations, low recurrent amplified genes, such as CCNE1, ERBB2,
CDKN1B, ZNF217 and CDK6 were identified; with
CDKN2A revealing a deep deletion (Fig. 2C). Among these genes, NOTCH1,
NOTCH2, ERBB2 and CDK6 are of interest as potential drug
targets.
 | Table II.Mutations of bile cell-free DNA from
ten biliary tract cancer patients. |
Table II.
Mutations of bile cell-free DNA from
ten biliary tract cancer patients.
| Patient ID | SNV/Indel | CNV |
|---|
| Patient #1 | TP53 | p.Q38Pfs*5 | 0.498a | CDK12 | Gain |
|
| ERBB2 | p.D769Y | 0.004 | ERBB2 | Gain |
|
| PIK3CA | c.1665-1G>T | 0.004 | CCNE1 | Gain |
|
|
|
|
| CDKN2A | Loss |
|
|
|
|
| ZNF217 | Gain |
| Patient #2 | TP53 | p.C275F | 0.037 | FGFR2 | Gain |
|
| TP53 | p.P27Lfs*17 | 0.012 |
|
|
|
| ARID2 | p.Q794Cfs*45 | 0.014 |
|
|
|
| KRAS | p.A146V | 0.006 |
|
|
|
| TP53 | p.E180K | 0.022 |
|
|
|
| SETD2 | p.M118I | 0.015 |
|
|
| Patient #3 | TP53 | p.P151T | 0.022 | FLT1 | Gain |
|
| NOTCH2 | p.T235S | 0.011 |
|
|
| Patient #4 | TP53 | p.V157F | 0.062 | CCNE1 | Gain |
|
| FLT4 | p.A622T | 0.010 | CDKN2A | Loss |
|
| NOTCH1 | p.R1824Q | 0.492 |
|
|
|
| KMT2A | p.G3131S | 0.467 |
|
|
|
| NOTCH2 | p.R29Q | 0.028 |
|
|
| Patient #5 | TP53 | c.783-2_821del | 0.050 |
|
|
|
| CDKN2A | p.V82E | 0.169 |
|
|
|
| KRAS | p.I36M | 0.246 |
|
|
|
| IRS2 | p.Q1206R | 0.592 |
|
|
|
| EP300 | p.P881S | 0.423 |
|
|
|
| FAT1 | p.D850E | 0.129 |
|
|
| Patient #6 | TP53 | p.M237I | 0.760 | CDK6 | Gain |
|
| PDGFRA | p.L216I | 0.516 | MET | Gain |
|
| NF1 | p.E649* | 0.710 | BRAF | Gain |
|
| RNF43 | p.L706Cfs*20 | 0.471 | PIK3CA | Gain |
|
| FGFR3 | p.K413R | 0.320 | ALK | Gain |
|
| FGFR1 | p.G35R | 0.109 |
|
|
|
| SPTA1 | p.N2076K | 0.107 |
|
|
|
| PIK3R1 | p.N564D | 0.034 |
|
|
|
| AR | p.K778M | 0.014 |
|
|
| Patient #7 | KRAS | p.G12D | 0.016 |
|
|
|
| ATM | p.A2626V | 0.012 |
|
|
|
| NOTCH1 | p.R592H | 0.486 |
|
|
|
| KMT2A | p.P658P | 0.483 |
|
|
|
| VEGFA | p.T8Rfs*78 | 0.385 |
|
|
| Patient #8 | TP53 | p.R248W | 0.533 | FGFR3 | Gain |
|
| TSC1 | p.R190H | 0.130 | VEGFA | Gain |
|
| ATR | p.M211I | 0.441 | MYC | Gain |
|
| BRCA1 | p.R762S | 0.197 | ERBB3 | Gain |
|
|
|
|
| CDKN1B | Gain |
|
|
|
|
| APC | Gain |
|
|
|
|
| ROS1 | Gain |
| Patient #9 |
|
|
| MRE11A | Gain |
|
|
|
|
| MTOR | Loss |
|
|
|
|
| CDKN2A | Loss |
|
|
|
|
| STK11 | Loss |
|
|
|
|
| ERBB2 | Gain |
|
|
|
|
| CCNE1 | Gain |
|
|
|
|
| CDK6 | Gain |
| Patient #10 |
|
|
| CDKN1B | Gain |
|
|
|
|
| CCNE1 | Gain |
|
|
|
|
| ZNF217 | Gain |
Concordance of mutations between tumor
tissue and bile
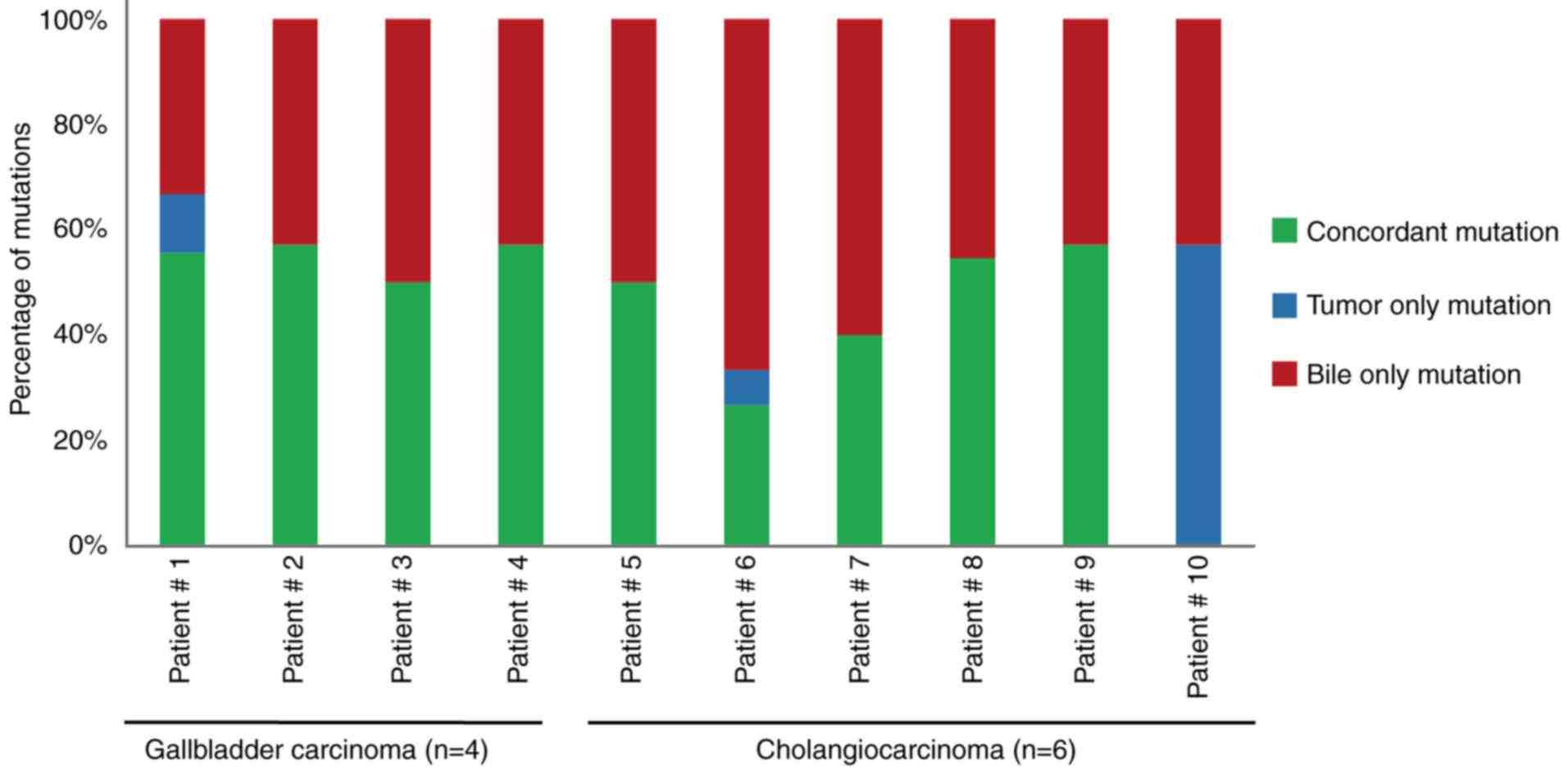
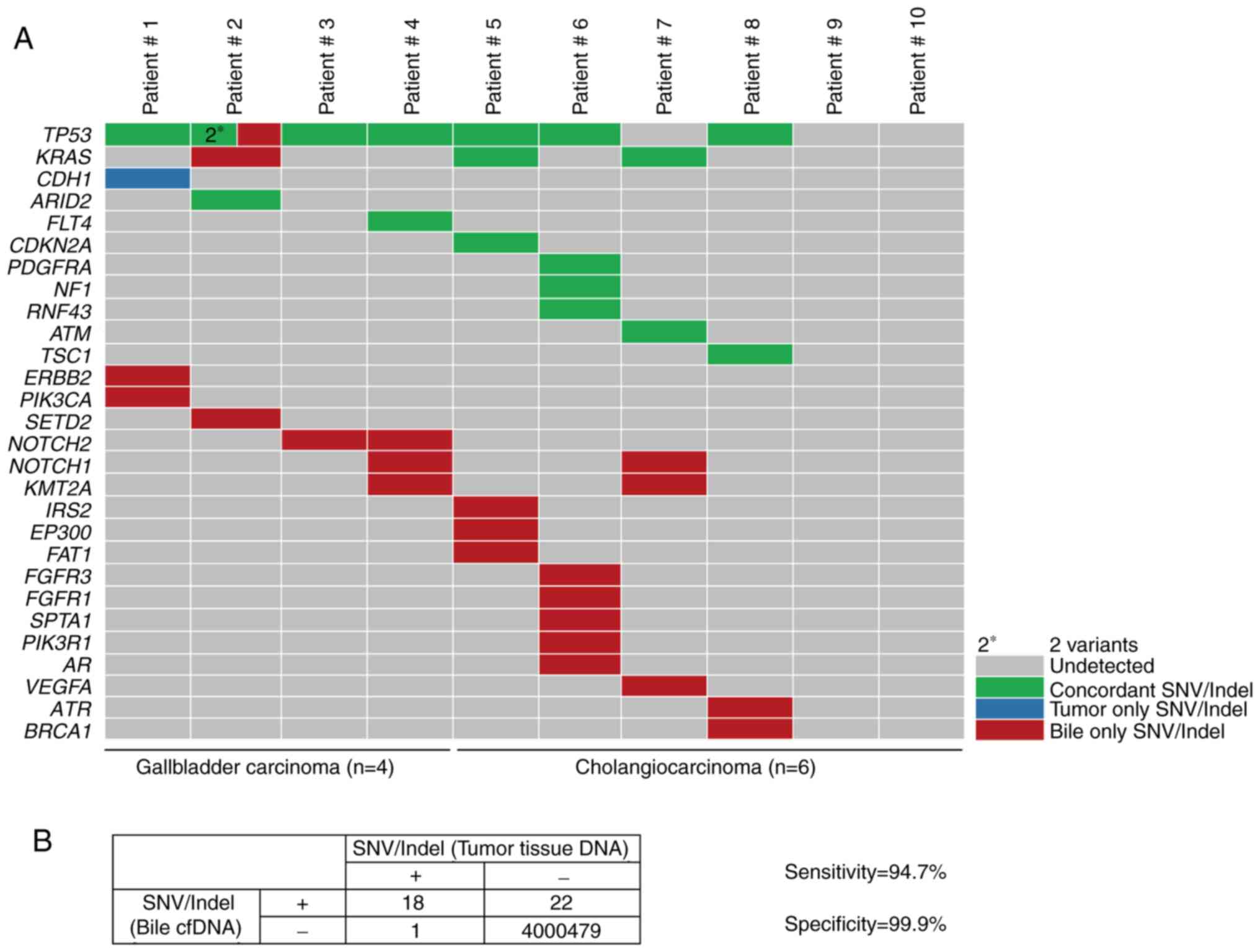
To assess the performance of the targeted deep
sequencing in detecting mutations in the bile cfDNA samples, the
findings were compared to the paired tumor tissue DNA findings. In
the tumor tissues, a total of 19 SNVs/Indels and 20 CNVs were
identified as a reference (Table
III). Mutational concordance percentages between paired bile
cfDNA and tumor tissue DNA samples are presented in Fig. 3. With the exception of Patient #10,
the other 9 BTC patients had concordant mutations. In seven
patients (70%, 7/10), >50% mutational concordance between the
bile cfDNA and tumor tissue DNA was revealed (Fig. 3). To further investigate the observed
SNVs/Indel mutational concordance, the paired bile and tumor
samples were further examined. Of the 19 variants detected in the
tumor samples, 18 were also detected in bile cfDNA (Fig. 4A). The only discordant mutated gene
was CDH1, whose allelic frequency was the lowest of all of
the tumor tissue SNVs. Moreover, when compared with the tumor
results, targeted deep sequencing of bile cfDNA revealed a high
sensitivity (94.7%) and specificity (99.9%; Fig. 4B).
 | Table III.Mutations of tumor tissue from ten
biliary tract cancer patients. |
Table III.
Mutations of tumor tissue from ten
biliary tract cancer patients.
| Patient ID | SNV/Indel | CNV |
|---|
| Patient #1 | TP53 | p.Q38Pfs*5 | 0.30a | CDK12 | Gain |
|
| CDH1 | p.Q610* | 0.07 | ERBB2 | Gain |
|
|
|
|
| CCNE1 | Gain |
|
|
|
|
| CDKN2A | Loss |
| Patient #2 | TP53 | p.C275F | 0.22 | FGFR2 | Gain |
|
| TP53 | p.P27Lfs*17 | 0.10 |
|
|
|
| ARID2 | p.Q794Cfs*45 | 0.11 |
|
|
| Patient #3 | TP53 | p.P151T | 0.22 |
|
|
| Patient #4 | TP53 | p.V157F | 0.49 | CCNE1 | Gain |
|
| FLT4 | p.A622T | 0.21 | CDKN2A | Loss |
| Patient #5 | TP53 | c.783-2_821del | 0.07 |
|
|
|
| CDKN2A | p.V82E | 0.19 |
|
|
|
| KRAS | p.I36M | 0.35 |
|
|
| Patient #6 | TP53 | p.M237I | 0.08 | MSH6 | Loss |
|
| PDGFRA | p.L216I | 0.12 |
|
|
|
| NF1 | p.E649* | 0.08 |
|
|
|
| RNF43 | p.L706Cfs*20 | 0.07 |
|
|
| Patient #7 | KRAS | p.G12D | 0.19 |
|
|
|
| ATM | p.A2626V | 0.16 |
|
|
| Patient #8 | TP53 | p.R248W | 0.24 | FGFR3 | Gain |
|
| TSC1 | p.R190H | 0.23 | VEGFA | Gain |
|
|
|
|
| MYC | Gain |
|
|
|
|
| ERBB3 | Loss |
| Patient #9 |
|
|
| MRE11A | Gain |
|
|
|
|
| MTOR | Loss |
|
|
|
|
| CDKN2A | Loss |
|
|
|
|
| STK11 | Loss |
| Patient #10 |
|
|
| MTOR | Gain |
|
|
|
|
| SPEN | Gain |
|
|
|
|
| NOTCH1 | Gain |
|
|
|
|
| GNA11 | Gain |
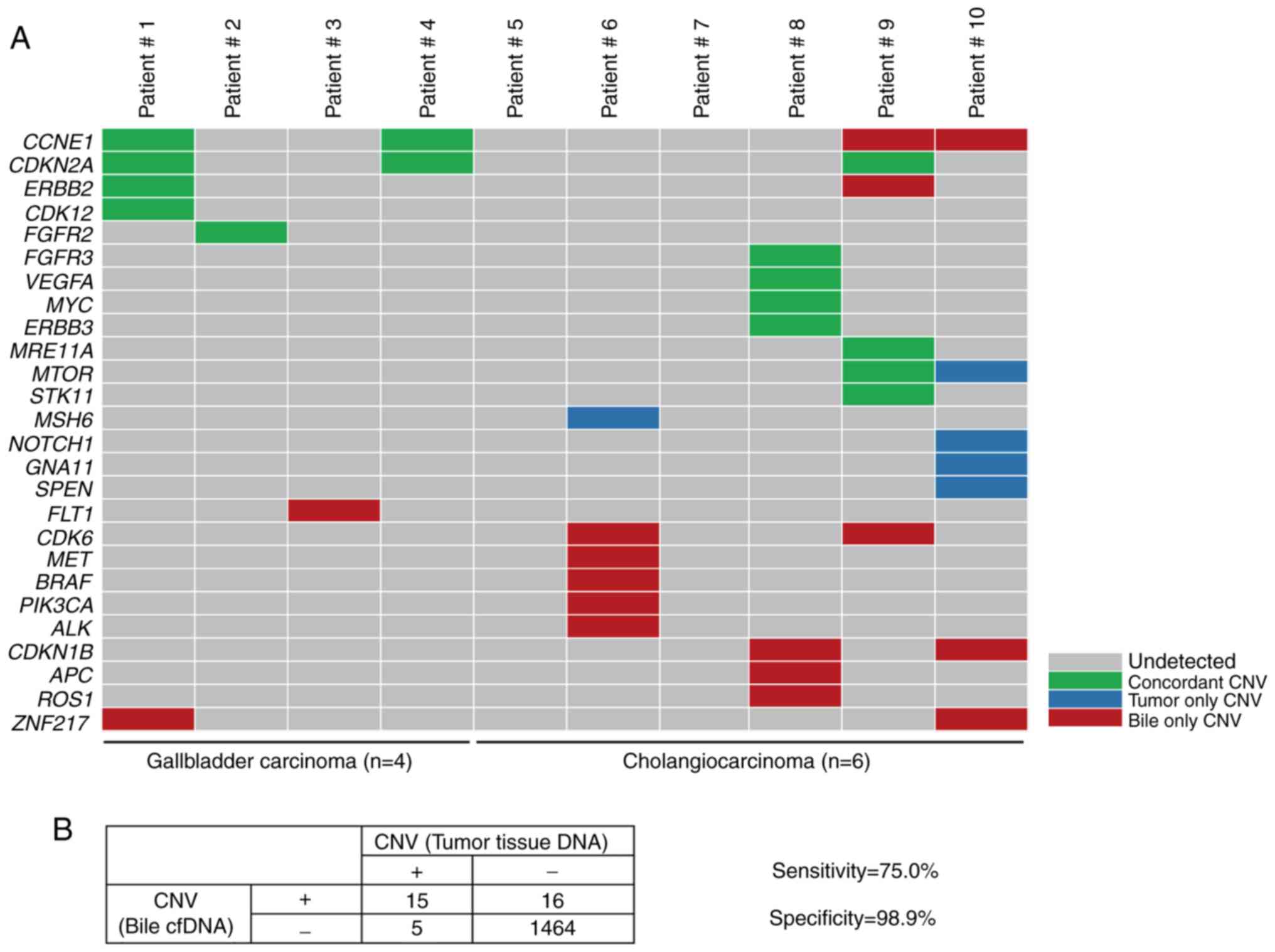
To further evaluate the capacity of targeted deep
sequencing to detect CNVs in bile cfDNA, the paired bile and tumor
samples were evaluated for concordance. Of the 20 CNVs identified
in the tumor tissue, 15 were also confirmed in bile cfDNA (Fig. 5A). The genes which were identified
with CNVs in bile cfDNA included CCNE1, ERBB2, FLT1, CDK6, MET,
PIK3CA and ROS1, with ERBB2, CDK6, MET, PIK3CA
and ROS1 being of interest as potential BTC therapeutic
targets. Furthermore, when compared to the tumor sample results,
targeted deep sequencing of bile cfDNA had a sensitivity of 75.0%
and specificity of 98.9% (Fig. 5B).
These results indicated that targeted deep sequencing of bile cfDNA
can confidently detect variance.
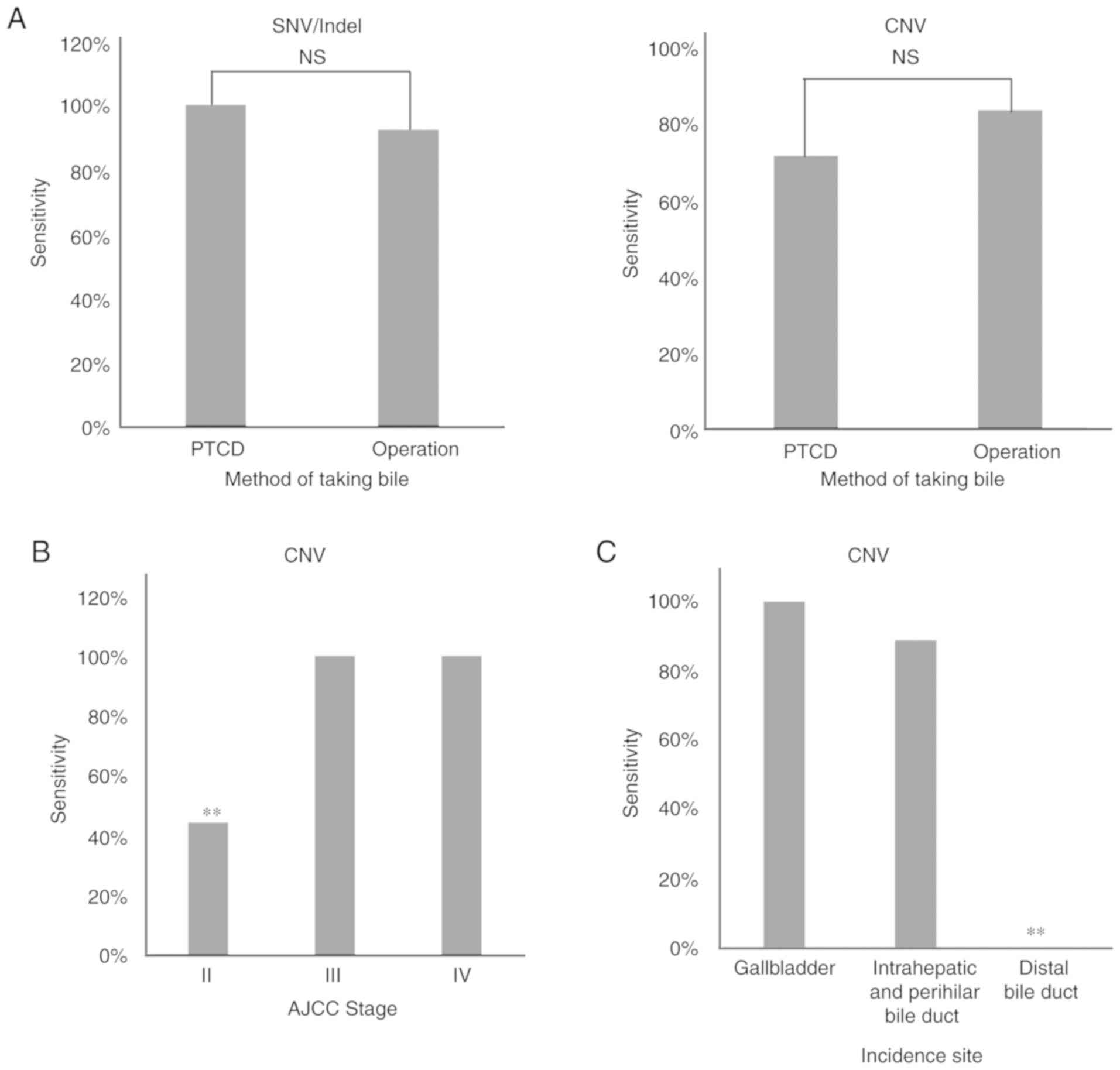
Effects of various clinical conditions
on the detection of mutations in bile cfDNA
To further evaluate the use of bile cfDNA, the
methods of obtaining bile (namely percutaneous transhepatic
cholangial drainage (PTCD) or operation) and the tumor stage or
incidence site were examined to determine if variant detection
sensitivity is impacted. In five of the patients, bile was obtained
using PTCD, while in the other five it was obtained by operation
(Table I). When examining the
detected SNV/Indels and CNVs, no significant difference in
sensitivity was noted between the PTCD and operation methods
(P>0.00 and P>0.00; Fig. 6A).
Next, any potential effects on sensitivity due to tumor stage or
incidence site were evaluated. The results revealed that AJCC stage
II had a significantly decreased sensitivity in CNV detection when
compared with other tumor stages (P<0.05), as did having an
incidence site of the distal bile duct (P<0.05; Fig. 6B). These findings indicated that the
sensitivity of tumor-matched mutation detection in bile cfDNA can
be affected by tumor stage and incidence site.
Discussion
Despite a real unmet need for improved BTC therapies
(17), clinical efforts to develop
genotype-specific targeted therapies have largely failed due to a
lack of reliable, safe, and reproducible genomic analyses. Current
approaches rely on obtaining a tumor mutational profile that can
then be utilized to predict sensitivity or resistance to particular
therapies (18). However, tissue
sampling in BTC patients is challenging due to the anatomical
complexity of the biliary tract system (19), with many patients at an advanced stage
losing the opportunity to receive personalized targeted therapy.
Herein, for the first time, the integral mutational landscape of
bile cfDNA was examined in 10 BTC patients. The examination of
these bile cfDNA samples with targeted deep sequencing revealed a
high sensitivity and specificity in detecting SNVs/Indels (94.7 and
99.9%, respectively) and CNVs (75.0 and 98.9%, respectively).
Overall, this study provides a promising liquid biopsy method for
evaluating clinical BTC patient samples.
Previous studies have reported that plasma cfDNA has
a higher proportion of small fragments, with sizes between 150 to
200 bp, in many types of tumors or cancer cell lines (11,20).
However, DNA fragment sizes in bile cfDNAs from BTC patients had
not been elucidated until now. Herein, bile cfDNA was revealed to
be composed of predominantly long DNA fragments, which was not
consistent with the findings in plasma cfDNA. These differences may
be attributed to DNA restriction endonuclease variety or activity
differences between the bile and plasma.
The landscape of BTC has been reported in several
previous studies using whole exome sequencing and whole genome
sequencing (21–24). The most recurrently mutated genes were
TP53, CDKN2A/B, KRAS, ARID1A, and IDH1 in
intrahepatic cholangiocarcinoma (ICC); KRAS, TP53, CDKN2A/B,
and SMAD4 in extrahepatic cholangiocarcinoma; and TP53,
CDKN2A/B, ARID1A, and ERBB2 in gallbladder cancer
(25).
Ras/phosphatidylinositol-4,5-bisphosphate 3-kinase signaling,
p53/cell cycle signaling, and transforming growth factor-β/Smad
signaling are substantially affected in ICC (26), while ErbB signaling is the most
extensively mutated pathway in gallbladder cancer samples (22). In the present study, similar to
previous research of tumor tissue, mutated TP53, KRAS, CDKN2A,
PIK3CA, and ERBB2 were also detected in bile cfDNA.
NOTCH1, and NOTCH2 mutations were recurrent in bile
cfDNA from BTC patients, which was not observed in previous
studies.
In a previous study examining SNVs in GBCs, bile
containing cfDNA was revealed to have a high concordance rate
(87.5%) with tumor tissues (19).
Considering the anatomical complexity of the biliary tract system
(27), patients not only with GBC,
but also cholangiocarcinomas with different incidence sites, were
evaluated in this cohort. In addition to SNVs, gene mutations such
as Indels and CNVs were also profiled. This study found a high
concordance between bile cfDNA and tumor tissues when examining
SNVs/Indels, but a high concordance was also found when identifying
CNVs, which has not been previously reported. Of the identified
CNVs, ERBB2, CDK6, MET, PIK3CA, and ROS1 are of
interest as potential BTC therapeutic targets. These results
support that targeted deep sequencing with barcodes can effectively
isolate somatic mutations in bile cfDNA from BTC patients.
Percutaneous transhepatic cholangial drainage (PTCD)
has been revealed to be one of the most important treatments for
benign and malignant obstructive jaundice (28–30).
Therefore, PTCD and operation were used as two different methods
for obtaining bile in this study. Variant detection sensitivities
were compared between the two methods and no significant difference
was noted when detecting SNV/Indel or CNV mutations. These results
suggest that bile cfDNA could serve as a clinically applicable
liquid biopsy by means of PTCD. Retrograde endoscopy is one of the
main means of minimally invasive treatment of
cholangiopancreatography (31).
Inhepatobiliary pancreatic surgery, retrograde endoscopy is often
recommended for cholangiocarcinoma. The effect of endoscopic bile
extraction is a future study we plan to carry out.
Notably, several clinical features have been
revealed to have a marked influence on variant detection
sensitivity in bile cfDNA when compared with tumor tissues. In our
previous study, lung cancer patients with different tumor stages
exhibited a significant difference in mutational concordance
between plasma cfDNA and tumor tissues (11). Additionally, tumor stage has been
revealed to affect gene mutation detection in cfDNA (32,33).
Herein, AJCC stage II was revealed to significantly decrease the
sensitivity when detecting CNVs in bile cfDNA compared with other
tumor stages (P<0.05). While these findings indicate that tumor
stage can potentially affect CNV detection, the sample size
examined herein was small and this issue should be further examined
with a larger sample size in the future. Next, any potential
effects on CNV detection associated with tumor incidence site were
examined. The results revealed that the distal bile duct
significantly decreases the CNV detection sensitivity when compared
with other incidence sites. Thus, these findings demonstrated that
tumor stage and incidence site can impact variant detection
sensitivity in bile cfDNA samples.
In conclusion, the present study revealed that long
DNA fragments are prevalent in bile cfDNA samples and that targeted
deep sequencing can reproducibly identify somatic variants in BTC
bile cfDNA samples. Obtaining bile cfDNA, which is considered a
minimally invasive liquid biopsy, and utilizing targeted deep
sequencing has the following unique advantages: i) In BTC patients,
bile is commonly drained using PTCD, thus bile samples can be
obtained without additional trauma; ii) due to tumor heterogeneity,
the information obtained from bile cfDNA is more comprehensive in
comparison to a needle biopsy; iii) targeted deep sequencing of
bile cfDNA samples is feasible, accurate, and sensitive in
mutational variants, thus enabling a more personalized targeted
therapeutic approach; and iv) bile cfDNA may provide a means to
identify benign and malignant diseases or judge tumor recurrence in
the future.
Supplementary Material
Supporting Data
Acknowledgments
The authors would like to thank Jing Ma, Zuo Zhang,
Dalei Wang, Chang Jiang, Yun Wang and Chao Sun for their assistance
in data collection and analysis for this study. Additionally, the
authors would like to thank all of the patients and their families
for their support of this study.
Funding
The present study was funded by the Youth Fund of
Shanghai Municipal Health Planning Commission (20144Y0164).
Availability of data and materials
The datasets generated and/or analyzed during the
present study are available from the corresponding author on
reasonable request.
Authors' contributions
NS designed the bile extraction study, contributed
to data interpretation and wrote the manuscript. DZ designed the
extraction of bile cell-free DNA (cfDNA) and wrote the manuscript.
LYi performed the bile extraction from gallbladder carcinoma
patients using operation and interpreted the data. YQ collected the
bile samples by means of percutaneous transhepatic cholangial
drainage (PTCD) and contributed to data interpretation. JL
collected the tumor tissue from gallbladder carcinoma patients and
contributed to data interpretation. WY performed the separation and
storage of bile samples and collected the clinical information. XF
performed the collection and isolation of patients' blood and
interpreted the data. BZ performed the extraction of genomic DNA
and contributed to data interpretation. XX established the
methodology of extracting the bile cfDNA and interpreted the data.
AD performed bile cfDNA extraction and contributed to data
interpretation. ZC performed the quality control analyses on bile
cfDNA extraction and interpreted the data. XW performed the
construction of sequencing library and contributed to data
interpretation. XC performed the analyses on the SNV/Indel of bile
cfDNA and tumor tissue samples, contributed to data interpretation
and wrote the manuscript. TZ analyzed the clinical information of
patients and contributed to data interpretation. ZZ analyzed the
copy number variation of bile cfDNA and tumor tissue samples and
contributed to data interpretation. LYu performed the targeted deep
sequencing of bile cfDNA and interpreted the data. HQ performed the
the analyses on sensitivity and specificity of bile cfDNA in
detecting the mutations and data interpretation. ZF performed the
targeted deep sequencing of DNA from tumor tissues and contributed
to data interpretation. JYL discussed the hypothesis and
contributed to data interpretation. YL collected the tumor tissue
samples from cholangiocarcinoma patients and interpreted the data.
LX led the consistency analyses on mutations bewteen bile cfDNA and
tumor tissue DNA and contributed to data interpretation. BY
collected the bile samples from cholangiocarcinoma patients and
interpreted the data. FL conceived the study, led the project and
wrote the manuscript. YZ conceived the study and participated in
its design and coordination. All of the authors have read and
approved the final version of the manuscript and agree to be
accountable for all aspects of the research in ensuring that the
accuracy or integrity of any part of the work are appropriately
investigated and resolved.
Ethics approval and consent to
participate
Bile and tumor tissue samples were collected with
ethics approval obtained from the Eastern Hepatobiliary Surgery
Hospital (EHBHKY2018-K-003). Informed consent was obtained from the
patients for the examination of their samples and the use of their
clinical data.
Patient consent for publication
Not applicable.
Competing interests
All of the authors affiliated to 3D Medicines, Inc.
are current or former employees. No potential competing interests
were disclosed by the other authors.
Glossary
Abbreviations
Abbreviations:
|
BTC
|
biliary tract cancer
|
|
GBC
|
gallbladder carcinoma
|
|
cfDNA
|
cell-free DNA
|
|
SNV
|
single nucleotide variations
|
|
Indel
|
insertion and deletion
|
|
CNV
|
copy number variation
|
|
FFPE
|
formalin-fixed paraffin-embedded
|
|
PTCD
|
percutaneous transhepatic cholangial
drainage
|
References
|
1
|
Augustine MM and Fong Y: Epidemiology and
risk factors of biliary tract and primary liver tumors. Surg Oncol
Clin N Am. 23:171–188. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Marcano-Bonilla L, Mohamed EA, Mounajjed T
and Roberts LR: Biliary tract cancers: Epidemiology, molecular
pathogenesis and genetic risk associations. Chin Clin Oncol.
5:612016. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Streeter OE Jr, Beron PJ and Iyer PN:
Precision medicine: Genomic profiles to individualize therapy.
Otolaryngol Clin North Am. 50:765–773. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Hirsch FR, Scagliotti GV, Mulshine JL,
Kwon R, Curran W Jr, Wu YL and Paz-Ares L: Lung cancer: Current
therapies and new targeted treatments. Lancet. 389:299–311. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Nakamura H, Arai Y, Totoki Y, Shirota T,
Elzawahry A, Kato M, Hama N, Hosoda F, Urushidate T and Ohashi S:
Genomic spectra of biliary tract cancer. Nat Genet. 47:1003–1010.
2015. View
Article : Google Scholar : PubMed/NCBI
|
|
6
|
Nam AR, Kim JW, Cha Y, Ha H, Park JE, Bang
JH, Jin MH, Lee KH, Kim TY and Han SW: Therapeutic implication of
HER2 in advanced biliary tract cancer. Oncotarget. 7:58007–58021.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sakamoto Y, Yamagishi S, Tanizawa Y,
Tajimi M, Okusaka T and Ojima H: PI3K-mTOR pathway identified as a
potential therapeutic target in biliary tract cancer using a newly
established patient-derived cell panel assay. Jpn J Clin Oncol.
48:396–399. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Rizvi S, Yamada D, Hirsova P, Bronk SF,
Werneburg NW, Krishnan A, Salim W, Zhang L, Trushina E, Truty MJ
and Gores GJ: A hippo and fibroblast growth factor receptor
autocrine pathway in cholangiocarcinoma. J Biol Chem.
291:8031–8047. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Saha SK, Gordan JD, Kleinstiver BP, Vu P,
Najem MS, Yeo JC, Shi L, Kato Y, Levin RS, Webber JT, et al:
Isocitrate dehydrogenase mutations confer dasatinib
hypersensitivity and SRC dependence in intrahepatic
cholangiocarcinoma. Cancer Discov. 6:727–739. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Wan JCM, Massie C, Garcia-Corbacho J,
Mouliere F, Brenton JD, Caldas C, Pacey S, Baird R and Rosenfeld N:
Liquid biopsies come of age: Towards implementation of circulating
tumour DNA. Nat Rev Cancer. 17:223–238. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Yang N, Li Y, Liu Z, Qin H, Du D, Cao X,
Cao X, Li J, Li D, Jiang B, et al: The characteristics of ctDNA
reveal the high complexity in matching the corresponding tumor
tissues. BMC Cancer. 18:3192018. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Siravegna G, Marsoni S, Siena S and
Bardelli A: Integrating liquid biopsies into the management of
cancer. Nat Rev Clin Oncol. 14:531–548. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jiang T, Ren S and Zhou C: Role of
circulating-tumor DNA analysis in non-small cell lung cancer. Lung
Cancer. 90:128–134. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Jiang T, Li X, Wang J, Su C, Han W, Zhao
C, Wu F, Gao G, Li W, Chen X, et al: Mutational landscape of cfDNA
identifies distinct molecular features associated with therapeutic
response to first-line platinum-based doublet chemotherapy in
patients with advanced NSCLC. Theranostics. 7:4753–4762. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Su D, Zhang D, Chen K, Lu J, Wu J, Cao X,
Ying L, Jin Q, Ye Y, Xie Z, et al: High performance of targeted
next generation sequencing on variance detection in clinical tumor
specimens in comparison with current conventional methods. J Exp
Clin Cancer Res. 36:1212017. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Watanabe H, Okada M, Kaji Y, Satouchi M,
Sato Y, Yamabe Y, Onaya H, Endo M, Sone M and Arai Y: New response
evaluation criteria in solid tumours-revised RECIST guideline
(version 1.1). Gan To Kagaku Ryoho. 36:2495–2501. 2009.(In
Japanese). PubMed/NCBI
|
|
17
|
Ribiere SC, Léandri C, Guillaumot MA,
Brezault C and Coriat R: Therapeutic advances in the management of
biliary tract carcinoma. Presse Med. 47:419–422. 2018.(In French).
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Zill OA, Greene C, Sebisanovic D, Siew LM,
Leng J, Vu M, Hendifar AE, Wang Z, Atreya CE, Kelley RK, et al:
Cell-free DNA next-generation sequencing in pancreatobiliary
carcinomas. Cancer Discov. 5:1040–1048. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kinugasa H, Nouso K, Ako S, Dohi C,
Matsushita H, Matsumoto K, Kato H and Okada H: Liquid biopsy of
bile for the molecular diagnosis of gallbladder cancer. Cancer Biol
Ther. 19:934–938. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Underhill HR, Kitzman JO, Hellwig S,
Welker NC, Daza R, Baker DN, Gligorich KM, Rostomily RC, Bronner MP
and Shendure J: Fragment length of circulating tumor DNA. PLoS
Genet. 12:e10061622016. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Xie D, Ren Z, Fan J and Gao Q: Genetic
profiling of intrahepatic cholangiocarcinoma and its clinical
implication in targeted therapy. Am J Cancer Res. 6:577–586.
2016.PubMed/NCBI
|
|
22
|
Li M, Zhang Z, Li X, Ye J, Wu X, Tan Z,
Liu C, Shen B, Wang XA, Wu W, et al: Whole-exome and targeted gene
sequencing of gallbladder carcinoma identifies recurrent mutations
in the ErbB pathway. Nat Genet. 46:872–876. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Oliveira DV, Zhang S, Chen X, Calvisi DF
and Andersen JB: Molecular profiling of intrahepatic
cholangiocarcinoma: The search for new therapeutic targets. Expert
Rev Gastroenterol Hepatol. 11:349–356. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Lee H and Ross JS: The potential role of
comprehensive genomic profiling to guide targeted therapy for
patients with biliary cancer. Therap Adv Gastroenterol. 10:507–520.
2017. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Javle M, Bekaii-Saab T, Jain A, Wang Y,
Kelley RK, Wang K, Kang HC, Catenacci D, Ali S, Krishnan S, et al:
Biliary cancer: Utility of next-generation sequencing for clinical
management. Cancer. 122:3838–3847. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Zou S, Li J, Zhou H, Frech C, Jiang X, Chu
JS, Zhao X, Li Y, Li Q, Wang H, et al: Mutational landscape of
intrahepatic cholangiocarcinoma. Nat Commun. 5:56962014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Chandra A, Gupta V, Rahul R, Kumar M and
Maurya A: Intraoperative ultrasonography of the biliary tract using
saline as a contrast agent: A fast and accurate technique to
identify complex biliary anatomy. Can J Surg. 60:316–322. 2017.
View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Cao H, Liu J, Li T, Cao G, Xu G, Zhai S,
Xue J, Wang Z, Shi S and Bai W: Interventional therapy for the
treatment of severe hemobilia after percutaneous transhepatic
cholangial drainage: A case series. Int Surg. 98:223–228. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Jin H, Pang Q, Liu H, Li Z, Wang Y, Lu Y,
Zhou L, Pan H and Huang W: Prognostic value of inflammation-based
markers in patients with recurrent malignant obstructive jaundice
treated by reimplantation of biliary metal stents: A retrospective
observational study. Medicine (Baltimore). 96:e58952017. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Li X, Yu J, Liang P, Yu X, Cheng Z, Han Z,
Duan S and Zheng J: Ultrasound-guided percutaneous microwave
ablation assisted by three-dimensional visualization operative
treatment planning system and percutaneous transhepatic cholangial
drainage with intraductal chilled saline perfusion for larger
hepatic hilum hepatocellular (D ≥ 3 cm): Preliminary results.
Oncotarget. 8:79742–79749. 2017.PubMed/NCBI
|
|
31
|
Njei B, McCarty TR, Varadarajulu S and
Navaneethan U: Systematic review with meta-analysis: endoscopic
retrograde cholangiopancreatography-based modalities for the
diagnosis of cholangiocarcinoma in primary sclerosing cholangitis.
Aliment Pharmacol Ther. 44:1139–1151. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Newman AM, Bratman SV, To J, Wynne JF,
Eclov NC, Modlin LA, Liu CL, Neal JW, Wakelee HA, Merritt RE, et
al: An ultrasensitive method for quantitating circulating tumor DNA
with broad patient coverage. Nat Med. 20:548–554. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Li J, Dittmar RL, Xia S, Zhang H, Du M,
Huang CC, Druliner BR, Boardman L and Wang L: Cell-free DNA copy
number variations in plasma from colorectal cancer patients. Mol
Oncol. 11:1099–1111. 2017. View Article : Google Scholar : PubMed/NCBI
|