|
1
|
Wolfgang CL, Herman JM, Laheru DA, Klein
AP, Erdek MA, Fishman EK and Hruban RH: Recent progress in
pancreatic cancer. CA Cancer J Clin. 63:318–348. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Andersen DK, Korc M, Petersen GM, Eibl G,
Li D, Rickels MR, Chari ST and Abbruzzese J: Diabetes,
pancreatogenic diabetes, and pancreatic cancer. Diabetes.
66:1103–1110. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
He H, Ke R, Lin H, Ying Y, Liu D and Luo
Z: Metformin, an old drug, brings a new era to cancer therapy.
Cancer J. 21:70–74. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Franciosi M, Lucisano G, Lapice E,
Strippoli GF, Pellegrini F and Nicolucci A: Metformin therapy and
risk of cancer in patients with type 2 diabetes: Systematic review.
PLoS One. 8:e715832013. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Zhang P, Li H, Tan X, Chen L and Wang S:
Association of metformin use with cancer incidence and mortality: A
meta-analysis. Cancer Epidemiol. 37:207–218. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bayraktar S, Hernadez-Aya LF, Lei X,
Meric-Bernstam F, Litton JK, Hsu L, Hortobagyi GN and
Gonzalez-Angulo AM: Effect of metformin on survival outcomes in
diabetic patients with triple receptor-negative breast cancer.
Cancer. 118:1202–1211. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Wan G, Sun X, Li F, Wang X, Li C, Li H, Yu
X and Cao F: Survival benefit of metformin adjuvant treatment for
pancreatic cancer patients: A systematic review and meta-analysis.
Cell Physiol Biochem. 49:837–847. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Broadhurst PJ and Hart AR: Metformin as an
adjunctive therapy for pancreatic cancer: A review of the
literature on its potential therapeutic use. Dig Dis Sci.
63:2840–2852. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Yang J and Weinberg RA:
Epithelial-mesenchymal transition: At the crossroads of development
and tumor metastasis. Dev Cell. 14:818–829. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lamouille S, Xu J and Derynck R: Molecular
mechanisms of epithelial-mesenchymal transition. Nat Rev Mol Cell
Biol. 15:178–196. 2014. View
Article : Google Scholar : PubMed/NCBI
|
|
11
|
Jie XX, Zhang XY and Xu CJ:
Epithelial-to-mesenchymal transition, circulating tumor cells and
cancer metastasis: Mechanisms and clinical applications.
Oncotarget. 8:81558–81571. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Okajima M, Kokura S, Ishikawa T, Mizushima
K, Tsuchiya R, Matsuyama T, Adachi S, Okayama T, Sakamoto N, Kamada
K, et al: Anoxia/reoxygenation induces epithelial-mesenchymal
transition in human colon cancer cell lines. Oncol Rep.
29:2311–2317. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wang Y, Wu Z and Hu L: The regulatory
effects of metformin on the [SNAIL/miR-34]:[ZEB/miR-200] system in
the epithelial-mesenchymal transition(EMT) for colorectal
cancer(CRC). Eur J Pharmacol. 834:45–53. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Valaee S, Yaghoobi MM and Shamsara M:
Metformin inhibits gastric cancer cells metastatic traits through
suppression of epithelial-mesenchymal transition in a
glucose-independent manner. PLoS One. 12:e01744862017. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tong D, Liu Q, Liu G, Xu J, Lan W, Jiang
Y, Xiao H, Zhang D and Jiang J: Metformin inhibits
castration-induced EMT in prostate cancer by repressing
COX2/PGE2/STAT3 axis. Cancer Lett. 389:23–32. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
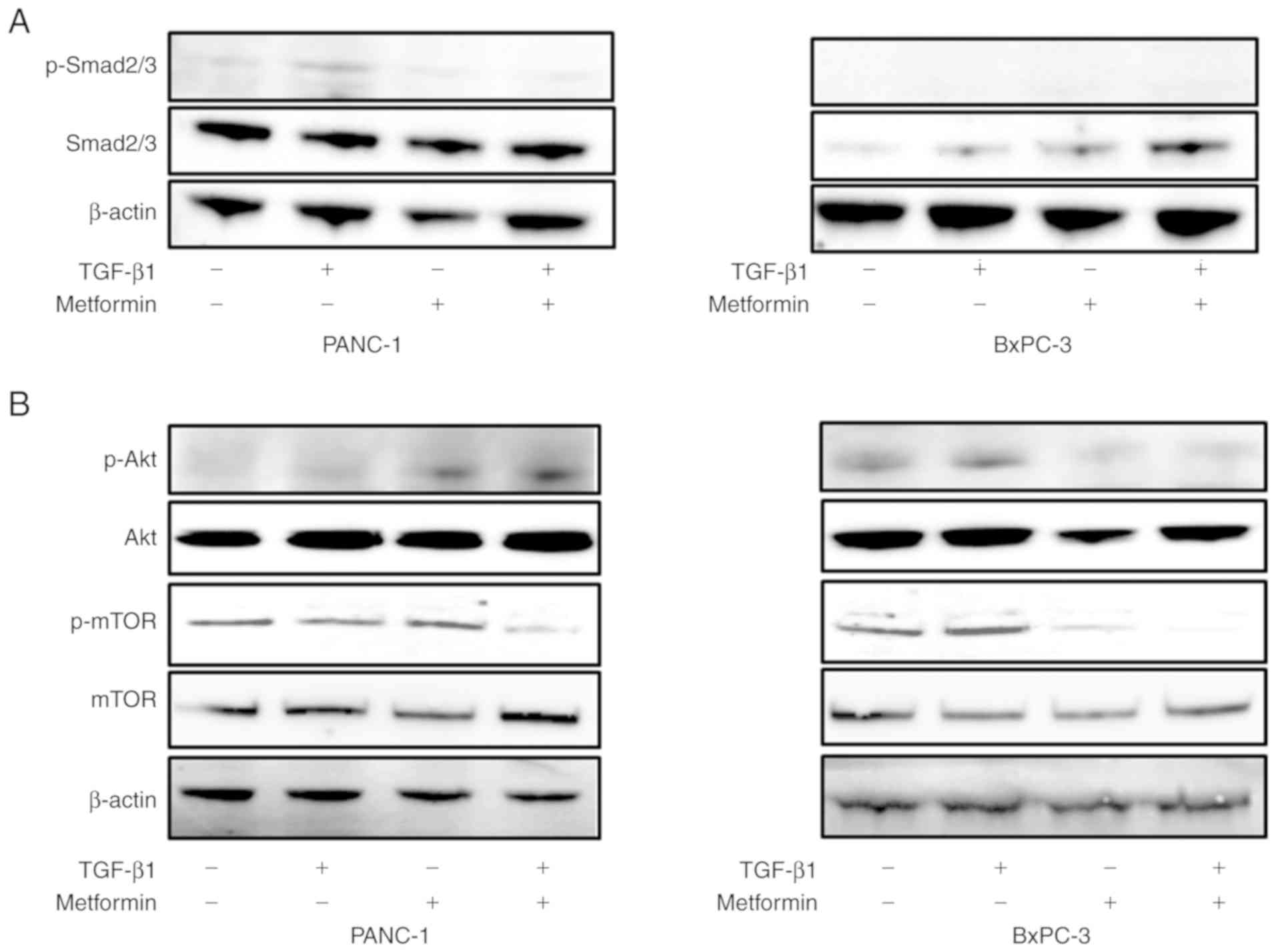
16
|
Song Y, Chen Y, Li Y, Lyu X, Cui J, Cheng
Y, Zhao L and Zhao G: Metformin inhibits TGF-beta1-induced
epithelial-to-mesenchymal transition-like process and stem-like
properties in GBM via AKT/mTOR/ZEB1 pathway. Oncotarget.
9:7023–7035. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zhao Z, Cheng X, Wang Y, Han R, Li L,
Xiang T, He L, Long H, Zhu B and He Y: Metformin inhibits the
IL-6-induced epithelial-mesenchymal transition and lung
adenocarcinoma growth and metastasis. PLoS One. 9:e958842014.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Nakayama A, Ninomiya I, Harada S, Tsukada
T, Okamoto K, Nakanuma S, Sakai S, Makino I, Kinoshita J, Hayashi
H, et al: Metformin inhibits the radiation-induced invasive
phenotype of esophageal squamous cell carcinoma. Int J Oncol.
49:1890–1898. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Li NS, Zou JR, Lin H, Ke R, He XL, Xiao L,
Huang D, Luo L, Lv N and Luo Z: LKB1/AMPK inhibits TGF-β1
production and the TGF-beta signaling pathway in breast cancer
cells. Tumour Biol. 37:8249–8258. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Uchiyama K, Naito Y, Takagi T, Mizushima
K, Hayashi N, Harusato A, Hirata I, Omatsu T, Handa O, Ishikawa T,
et al: Carbon monoxide enhance colonic epithelial restitution via
FGF15 derived from colonic myofibroblasts. Biochem Biophys Res
Commun. 391:1122–1126. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kimura-Tsuchiya R, Ishikawa T, Kokura S,
Mizushima K, Adachi S, Okajima M, Matsuyama T, Okayama T, Sakamoto
N, Katada K, et al: The inhibitory effect of heat treatment against
epithelial-mesenchymal transition (EMT) in human pancreatic
adenocarcinoma cell lines. J Clin Biochem Nutr. 55:56–61. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
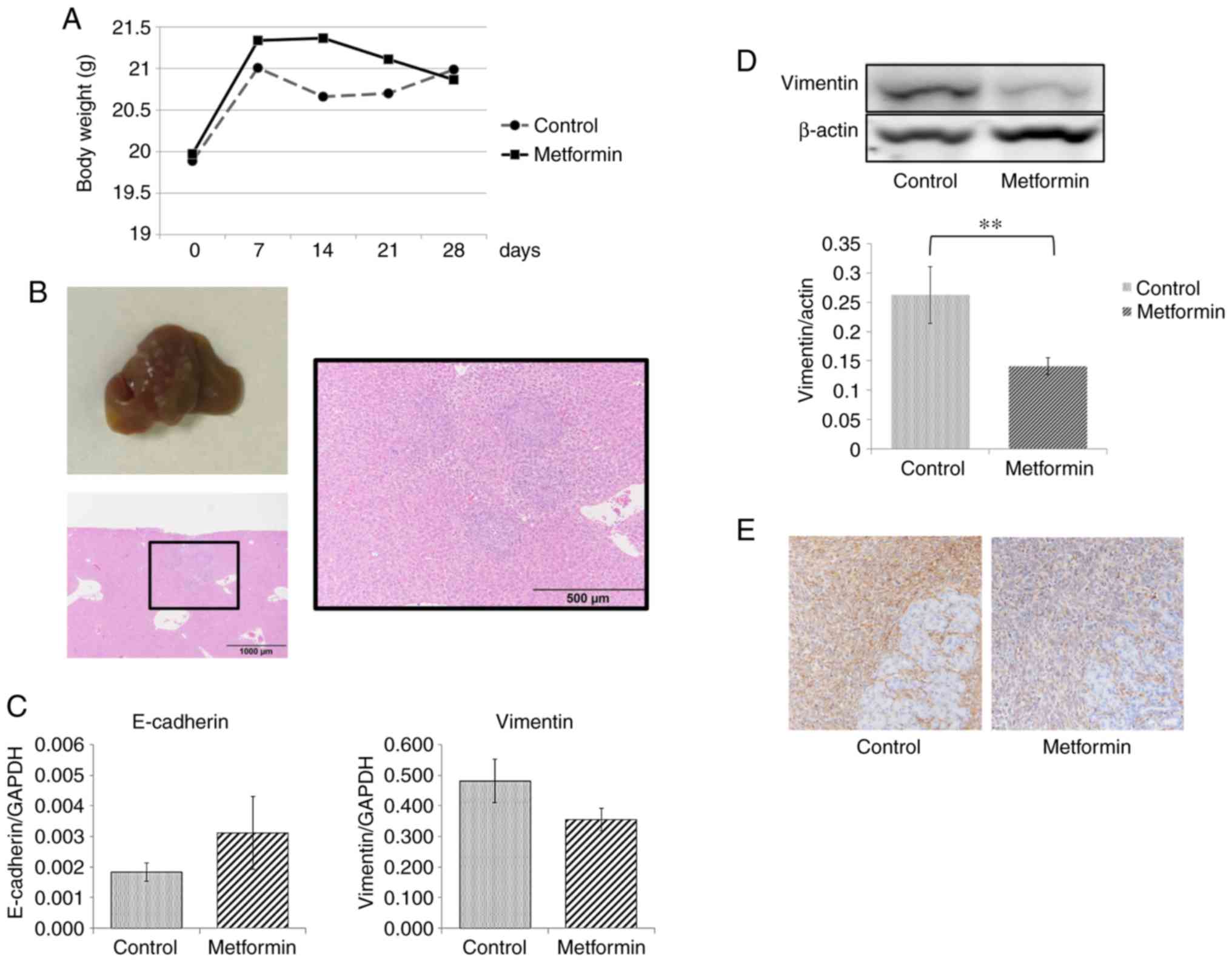
Hwang HK, Murakami T, Kiyuna T, Kim SH,
Lee SH, Kang CM, Hoffman RM and Bouvet M: Splenectomy is associated
with an aggressive tumor growth pattern and altered host immunity
in an orthotopic syngeneic murine pancreatic cancer model.
Oncotarget. 8:88827–88834. 2017. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Li D, Yeung SC, Hassan MM, Konopleva M and
Abbruzzese JL: Antidiabetic therapies affect risk of pancreatic
cancer. Gastroenterology. 137:482–488. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Shi Y, He Z, Jia Z and Xu C: Inhibitory
effect of metformin combined with gemcitabine on pancreatic cancer
cells in vitro and in vivo. Mol Med Rep.
14:2921–2928. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kisfalvi K, Moro A, Sinnett-Smith J, Eibl
G and Rozengurt E: Metformin inhibits the growth of human
pancreatic cancer xenografts. Pancreas. 42:781–785. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Algire C, Amrein L, Bazile M, David S,
Zakikhani M and Pollak M: Diet and tumor LKB1 expression interact
to determine sensitivity to anti-neoplastic effects of metformin in
vivo. Oncogene. 30:1174–1182. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Jalving M, Gietema JA, Lefrandt JD, de
Jong S, Reyners AK, Gans RO and de Vries EG: Metformin: Taking away
the candy for cancer? Eur J Cancer. 46:2369–2380. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Schneider MB, Matsuzaki H, Haorah J,
Ulrich A, Standop J, Ding XZ, Adrian TE and Pour PM: Prevention of
pancreatic cancer induction in hamsters by metformin.
Gastroenterology. 120:1263–1270. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Muniraj T and Chari ST: Diabetes and
pancreatic cancer. Minerva Gastroenterol Dietol. 58:331–345.
2012.PubMed/NCBI
|
|
30
|
Yue W, Yang CS, DiPaola RS and Tan XL:
Repurposing of metformin and aspirin by targeting AMPK-mTOR and
inflammation for pancreatic cancer prevention and treatment. Cancer
Prev Res (Phila). 7:388–397. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Ben Sahra I, Laurent K, Loubat A,
Giorgetti-Peraldi S, Colosetti P, Auberger P, Tanti JF, Le
Marchand-Brustel Y and Bost F: The antidiabetic drug metformin
exerts an antitumoral effect in vitro and in vivo through a
decrease of cyclin D1 level. Oncogene. 27:3576–3586. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Lund SS, Tarnow L, Stehouwer CD,
Schalkwijk CG, Teerlink T, Gram J, Winther K, Frandsen M, Smidt UM,
Pedersen O, et al: Impact of metformin versus repaglinide on
non-glycaemic cardiovascular risk markers related to inflammation
and endothelial dysfunction in non-obese patients with type 2
diabetes. Eur J Endocrinol. 158:631–641. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Buzzai M, Jones RG, Amaravadi RK, Lum JJ,
DeBerardinis RJ, Zhao F, Viollet B and Thompson CB: Systemic
treatment with the antidiabetic drug metformin selectively impairs
p53-deficient tumor cell growth. Cancer Res. 67:6745–6752. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Zhang YE: Non-Smad pathways in TGF-beta
signaling. Cell Res. 19:128–139. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Hoot KE, Lighthall J, Han G, Lu SL, Li A,
Ju W, Kulesz-Martin M, Bottinger E and Wang XJ:
Keratinocyte-specific Smad2 ablation results in increased
epithelial-mesenchymal transition during skin cancer formation and
progression. J Clin Invest. 118:2722–2732. 2008.PubMed/NCBI
|
|
36
|
Lamouille S and Derynck R: Cell size and
invasion in TGF-beta-induced epithelial to mesenchymal transition
is regulated by activation of the mTOR pathway. J Cell Biol.
178:437–451. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Lamouille S, Connolly E, Smyth JW, Akhurst
RJ and Derynck R: TGF-β-induced activation of mTOR complex 2 drives
epithelial-mesenchymal transition and cell invasion. J Cell Sci.
125:1259–1273. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Julien S, Puig I, Caretti E, Bonaventure
J, Nelles L, van Roy F, Dargemont C, de Herreros AG, Bellacosa A
and Larue L: Activation of NF-kappaB by Akt upregulates Snail
expression and induces epithelium mesenchyme transition. Oncogene.
26:7445–7456. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Shin HS, Ko J, Kim DA, Ryu ES, Ryu HM,
Park SH, Kim YL, Oh ES and Kang DH: Metformin ameliorates the
phenotype transition of peritoneal mesothelial cells and peritoneal
fibrosis via a modulation of oxidative stress. Sci Rep. 7:56902017.
View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Thakur S, Viswanadhapalli S, Kopp JB, Shi
Q, Barnes JL, Block K, Gorin Y and Abboud HE: Activation of
AMP-activated protein kinase prevents TGF-β1-induced
epithelial-mesenchymal transition and myofibroblast activation. Am
J Pathol. 185:2168–2180. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Duan W, Qian W, Zhou C, Cao J, Qin T, Xiao
Y, Cheng L, Li J, Chen K, Li X, et al: Metformin suppresses the
invasive ability of pancreatic cancer cells by blocking autocrine
TGF-β1 signaling. Oncol Rep. 40:1495–1502. 2018.PubMed/NCBI
|
|
42
|
Tan XL, Bhattacharyya KK, Dutta SK, Bamlet
WR, Rabe KG, Wang E, Smyrk TC, Oberg AL, Petersen GM and
Mukhopadhyay D: Metformin suppresses pancreatic tumor growth with
inhibition of NFkappaB/STAT3 inflammatory signaling. Pancreas.
44:636–647. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Odawara M, Kawamori R, Tajima N, Iwamoto
Y, Kageyama S, Yodo Y, Ueki F and Hotta N: Long-term treatment
study of global standard dose metformin in Japanese patients with
type 2 diabetes mellitus. Diabetol Int. 8:286–295. 2017. View Article : Google Scholar : PubMed/NCBI
|