Introduction
Ultrasound technology has many applications for
diagnosis and therapy in medicine. Low-intensity ultrasound (LIUS)
has also been used to treat fractures. The LIUS protocol for
fracture consists of signals of 30 mW/cm2 spatial
average-temporal average (ISATA) intensity with a
frequency of 1.5 MHz in pulsed-wave mode (0.2-s burst sine waves
repeated at 1.0 kHz) for 20 min per day (1,2). The
ability of LIUS to promote fracture healing has been widely
investigated in both experimental vertebrate animal models
(3–6) and randomized clinical trials (7,8).
Fracture healing is a complex physiological process involving
various cell types. A number of in vitro studies have
clearly demonstrated LIUS-associated bone-formative responses in
cells related to fracture healing (9–21).
However, the mechanisms underlying the ability of bone cells to
detect and respond to LIUS irradiation remain poorly
understood.
To elucidate these mechanisms, we consider that
monitoring of the early cellular response to LIUS is crucial. The
combination of global-scale DNA microarray analysis and
bioinformatics analysis tools has provided a view of the gene
expression profiles, biological functions, and gene networks
relevant to the LIUS response of cells. Several groups have
reported that the gene expression patterns were affected within 3
to 24 h after LIUS-treatment in several cell types (18–23).
However, there has been no report about earlier changes in gene
expression profiles shortly after exposure of the cells to
LIUS.
Immediate-early genes (IEGs) were reported to be
induced within minutes after stimulation and have essential roles
in stress responses (24). Previous
findings indicated that FBJ osteosarcoma oncogene (Fos), a
well-characterized IEG, is induced by mechanical loadings including
LIUS (9–13). The Fos protein, a leucine
zipper-containing domain, heterodimerizes with the jun
proto-oncogene (Jun) protein to form the dimeric transcription
factor activator protein-1 (AP-1) (24), which plays an important role in bone
formation (25). More recently, we
showed that LIUS at an intensity of 25 mW/cm2
significantly and transiently increased the expression levels of 4
IEGs - Fos, early growth response 1 (Egr1),
Jun, and prostaglandin-endoperoxide synthase 2
(Ptgs2) - in mouse ST2 bone marrow stromal cells (BMSCs)
(13).
Here, to elucidate the early cellular response to
LIUS in cells, the early response genes elicited by LIUS
[ISATA, 25 mW/cm2 for 20 min with a
frequency of 1.11 MHz in a pulsed-wave mode (0.2-s burst sine waves
repeated at 1 kHz)] in mouse ST2 BMSCs were investigated using
GeneChip® oligonucleotide microarrays and computational
gene expression analysis tools.
Materials and methods
Cell culture
Mouse ST2 BMSCs (RCB0224) were obtained from the
RIKEN BRC through the National Bio-Resource Project of the Ministry
of Education, Culture, Sports, Science, and Technology of Japan
(MEXT). The cells were maintained in RPMI-1640 medium (Nacalai
Tesque, Inc.) supplemented with 10% fetal bovine serum
(Equitech-Bio, Inc.) at 37°C in humidified atmosphere of 95% air
with 5% CO2. For the LIUS experiments, the cells
(2×105 cells) were seeded on a 35-mm plastic culture
dish (Nippon Genetics Co., Ltd.) with 2 ml of culture medium and
cultured at 37°C for 24 h.
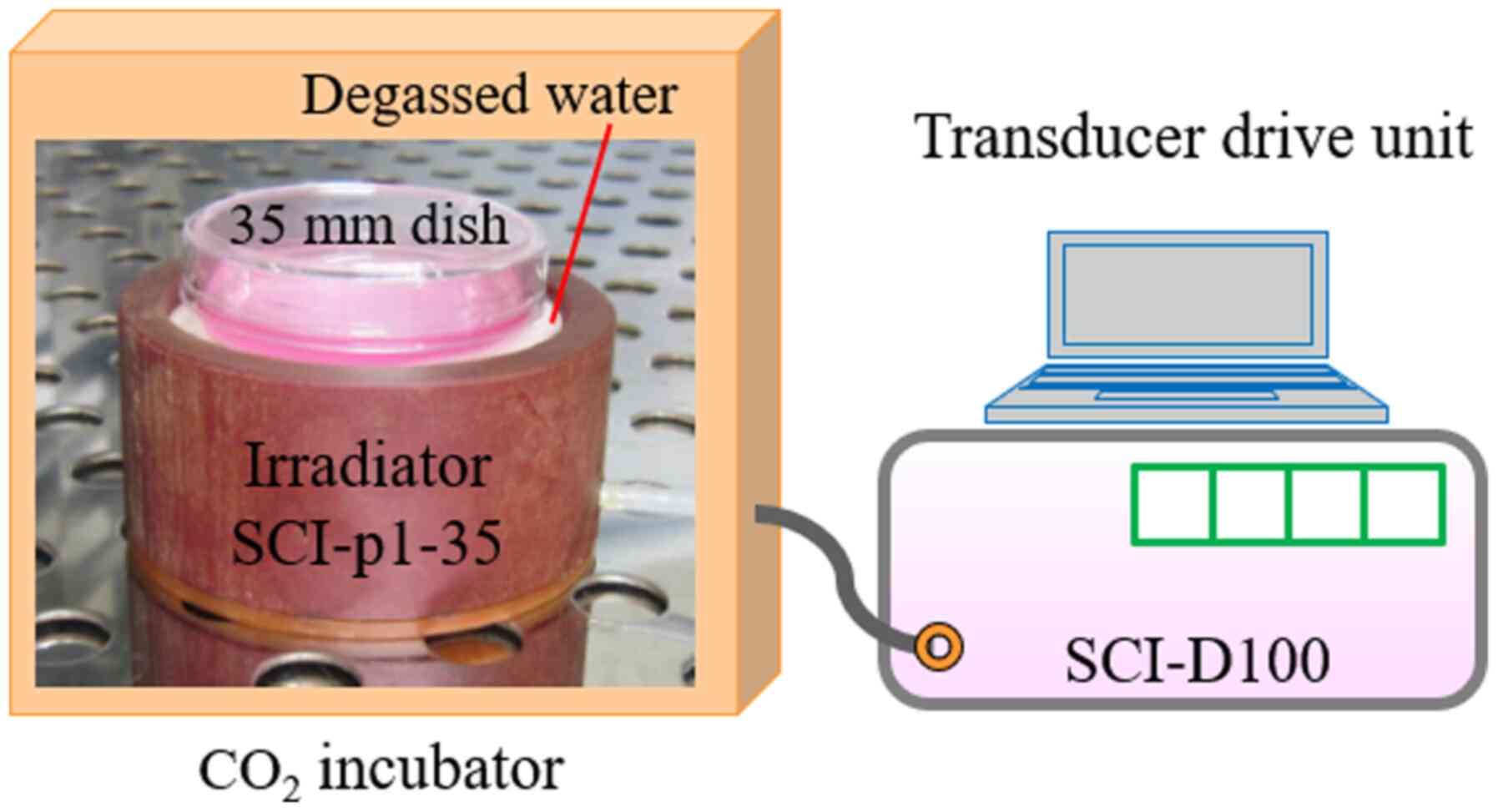
LIUS treatment
LIUS treatment was applied by an ultrasound
irradiating system, which consists of an irradiator SCI-p1-35
(Medical Ultrasound Co., Ltd.) with a ceramic transducer (28 mm
diameter, 2 mm thickness) and SCI-D100 driving equipment (Nepa Gene
Co., Ltd.). The LIUS signal had a ISATA of 25
mW/cm2, with a frequency of 1.11 MHz in a pulsed-wave
mode (0.2-s burst sine waves repeated at 1 kHz) (13). LIUS was transmitted through the
bottom of the culture dish in a CO2 incubator at 37°C
(Fig. 1). The cells were irradiated
with LIUS for 20 min, followed by incubation for 0, 0.5, 1, 3 or 24
h at 37°C. For heat treatment, cells were exposed to 38, 39, 40, 41
and 42°C for 20 min in a water bath. After heat treatment, the
cells were incubated for 0 or 0.5 h at 37°C. The temperature of the
culture medium was monitored with a digital thermometer (SK-1110,
Sato Keiryoki MFG Co., Ltd.) coupled to a type K thermocouple
sensor (SK-K020, Sato Keiryoki MFG Co., Ltd.) (13).
Morphological and cell growth
analyses
Cell morphology was observed using a phase-contrast
microscopy. For cell growth, Cell Count Reagent SF (Nacalai Tesque
Inc.), a water-soluble tetrazolium salt WST-8 based assay, was
used. Cells were incubated with WST-8 solution at 37°C. Thirty min
later, the produced formazan dye concentration was determined from
the absorbance at 450 nm (26).
Assay of alkaline phosphatase (ALP)
activity
Cellular material was placed into 50 mM Tris-HCl
buffer (pH 7.2) containing 0.01% Triton X-100 and homogenized by an
ultrasonic disruptor (UD-200, Tomy Co.). ALP activity of the cell
homogenate was measured by using a protocol supplied by Sigma
(Sigma-Aldrich; Merck KGaA). The absorbance at 405 nm was read on a
plate reader (13). The protein
concentration was determined with a bicinchoninic acid assay.
RNA isolation
Total RNA was isolated from cells using a
NucleoSpin® RNA Plus isolation kit (MACHEREY-NAGEL GmbH
& Co.) and treated with NucleoSpin® genomic DNA
removal column (MACHEREY-NAGEL GmbH & Co.) to remove residual
genomic DNA. The concentration of RNA was measured by spectroscopy
with an expected A260/A280 ratio close to 2. Qualitative assessment
of the RNA was also checked using a Bioanalyzer 2100 (Agilent
Technologies, Inc.). RNA samples (RNA integrity number values:
>9.5) were used (26).
Microarray gene expression and gene
network analyses
Microarray analysis was performed using a
GeneChip® system with a Mouse Genome 430 2.0 array
(Affymetrix, Inc.) spotted with 45,101 probe sets. Array samples
were prepared as described in the Affymetrix GeneChip®
Expression Technical Manual. Total RNA from three experiments was
pooled, and 500 ng of the RNA was used to synthesize cRNA with a
GeneChip® 3′ IVT Express Kit (Affymetrix, Inc.). The
array was hybridized with biotin-labeled cRNA at 45°C for 16 h.
After the treatment with phycoerythrin-labeled streptavidin, the
array was scanned using a prove array scanner (Affymetrix
GeneChip® Scanner 3000). The obtained hybridization
intensity data were further analyzed using GeneSpring®
GX (Agilent Technologies, Inc.) to extract the significant genes
and Ingenuity® Pathway Analysis tools (Tomy Digital
Biology, Co., Ltd.) to examine gene ontology, including biological
processes, cellular components, molecular functions, and gene
networks (21,27).
Real-time quantitative polymerase
chain reaction (qRT-PCR) assay
qRT-PCR was carried out on an Mx3005P real-time PCR
system (Agilent Technologies, Inc.) as described previously
(13). The specific primer and
probe sequences are listed in Table
I. β-actin (Actb) was used as an internal control.
 | Table I.Nucleotide sequences of the primer
pairs and a probe for target genes. |
Table I.
Nucleotide sequences of the primer
pairs and a probe for target genes.
| Gene | Orientation | Nucleotide sequence
(position) | GenBank accession
no. |
|---|
| Actb | Sense |
ACCCTAAGGCCAACCGTGAA (441–460) | NM_007393 |
|
| Antisense |
TGTGGTACGACCAGAGGCATAC (556–535) |
|
| Bag3 | Sense |
CCAAATCGGGAGAAGCCGAAAC (1514–1535) | NM_013863 |
|
| Antisense |
TCGTCCTTCAGGGTCTACGGAA (1710–1689) |
|
| Bglap | Sense | GGCAATAAGGTAGTGAAC
(169–187) | NM_007541 |
|
| Antisense | GCCATACTGGTCTGATAG
(297–279) |
|
|
| Probe |
FAM-CGCTACCTTGGAGCCTCAGT-TAMRA
(196–216) |
|
| Dnajb1 | Sense |
AGATCTACAGCGGCTGTACC (678–697) | NM_018808 |
|
| Antisense |
AGCCCCTCTTCACTTCGATG (791–772) |
|
| Egr1 | Sense |
ATGAGCACCTGACCACAGAG (563–582) | NM_007913 |
|
| Antisense |
GAGGCAGAGGAAGACGATGA (830–811) |
|
| Fos | Sense |
TGCAAGATCCCCGATGACCT (749–768) | NM_010234 |
|
| Antisense |
TCAGCTCCACGTTGCTGATG (932–913) |
|
| Hspa1a | Sense |
GAACGCGCTCGAATCCTATG (1848–1867) | NM_010479 |
|
| Antisense |
GAGATGACCTCCTGGCACTT (1917–1899) |
|
| Hspb1 | Sense |
CTGGCAAGCACGAAGAAAGG (514–533) | NM_013560 |
|
| Antisense |
AGGGGATAGGGAAGAGGACA (629–610) |
|
| Ptgs2 | Sense |
TTCTCCCTGAAGCCGTACAC (1559–1578) | NM_011198 |
|
| Antisense |
GGCAGGGTACAGTTCCATGA (1669–1650) |
|
Separation of total cellular,
cytoplasmic and nuclear fractions
For separation of total cellular fraction, cells
were lysed with lysis buffer (50 mM NaCl, 1% Nonidet P-40 and 50 mM
Tris-HCl, pH 8.0) containing protease inhibitor cocktail (Nacalai
Tesque, Inc.). For separation of cytoplasmic and nuclear fractions,
cells were lysed in the fractionation buffer [phosphate-buffered
saline containing 0.1% Nonidet P-40 and the protease inhibitor
cocktail (Nacalai Tesque, Inc.)]and centrifuged at 15,000 × g for
10 sec at 4°C to obtain the cytosolic fraction (supernatants). The
insoluble pellets were resuspended in the fractionation buffer and
centrifuged at 15,000 × g for 10 sec at 4°C to obtain the nuclear
fraction (pellets). Either glyceraldehyde 3-phosphate dehydrogenase
(Gapdh) or fibrillarin (Fbl) was used as the cytoplasmic or nuclear
marker protein, respectively (26).
SDS-polyacrylamide gel electrophoresis
(PAGE) and Western blotting
SDS-PAGE and Western blotting were carried out
according to our previous reports (26). Proteins were detected using the
following primary antibodies: rabbit polyclonal anti-heat shock
transcription factor 1 (Hsf1) antibody (1:2,000 dilution, cat. no.
4356; Cell Signaling Technology, Inc.), mouse monoclonal anti-Gapdh
antibody (1:2,000 dilution, cat. no. 60004-1-Ig; Proteintech Group,
Inc.) and rabbit monoclonal anti-Fbl antibody (1:2,000 dilution,
cat. no. 2639; Cell Signaling Technology, Inc.). Secondary
fluorescent IRDye-conjugated anti-rabbit and anti-mouse antibodies
(1:10,000 dilution, LI-COR Biosciences) were also used.
Fluorescence images were acquired using an Odyssey Infrared Imager
(LI-COR Biosciences), and the band density was quantified using
Image Studio 5.1 software (LI-COR Biosciences).
Statistical analysis
Statistical analysis was performed using
KaleidaGraph version 4.1 software (Hulinks, Inc.). Data were
expressed as the means ± standard deviation (SD) of ≥3 repeated
experiments. Differences between groups were analyzed by ANOVA, and
correction for multiple comparisons was made using Tukey's post hoc
test. Comparisons between two groups were made by using Student's
t-test. Statistically significance was set at P-values
<0.05.
Results
Effects of LIUS on the morphology,
growth and ALP activity of ST2 BMSCs
ST2 BMSCs were exposed to a single LIUS irradiation
(25 mW/cm2 for 20 min) followed by culturing at 37°C for
24 h. Microscopic investigations demonstrated that ST2 BMSCs had a
fibroblast-like morphology. LIUS treatment did not change the ST2
morphology (Fig. S1). Moreover,
LIUS treatment did not affect cell growth or ALP activity, a marker
for osteoblast differentiation (Fig.
S2), as it did in our previous investigations (13).
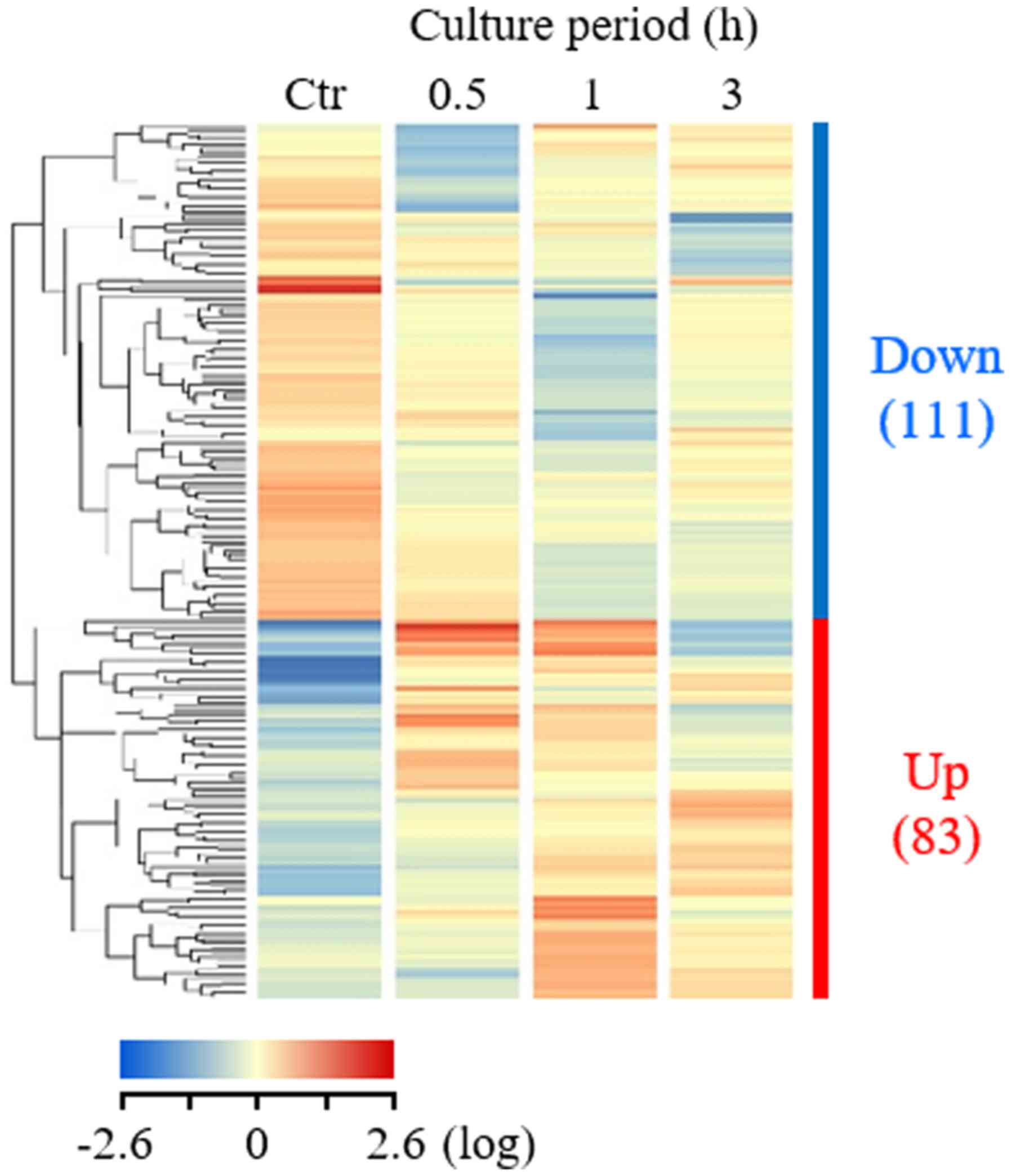
Gene expression analysis
After a single LIUS treatment, the cells were
cultured at 37°C for 0.5, 1, and 3 h. Global-scale gene expression
analysis was carried out using a GeneChip® Mouse Genome
430 2.0 oligonucleotide array. Of the 45,101 probe sets analyzed,
approximately 20,000 probe sets were significantly expressed in
either control or LIUS-treated cells. The complete lists of genes
from the ST2 cell samples have been deposited in the Gene
Expression Omnibus, a public database (accession number:
GSE135935). GeneSpring® software-based expression
analysis of cells exposed to LIUS demonstrated many probe sets that
were differentially regulated by a factor of 2.0 or greater. As
shown in a hierarchical clustering heatmap (Fig. 2), 83 and 111 probe sets were found
to be upregulated and downregulated, respectively, in ST2 cells
0.5, 1 and 3 h after LIUS treatment.
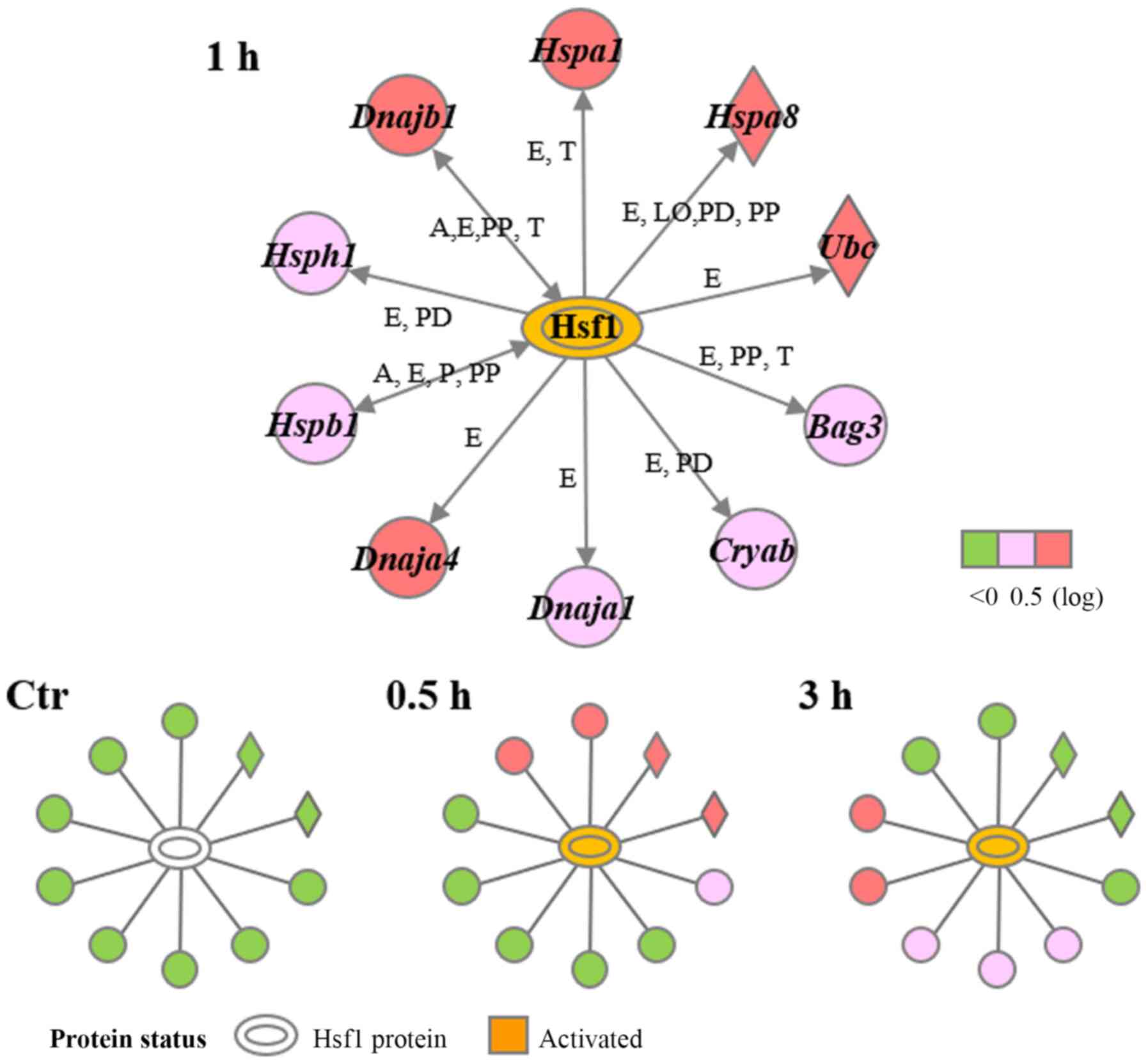
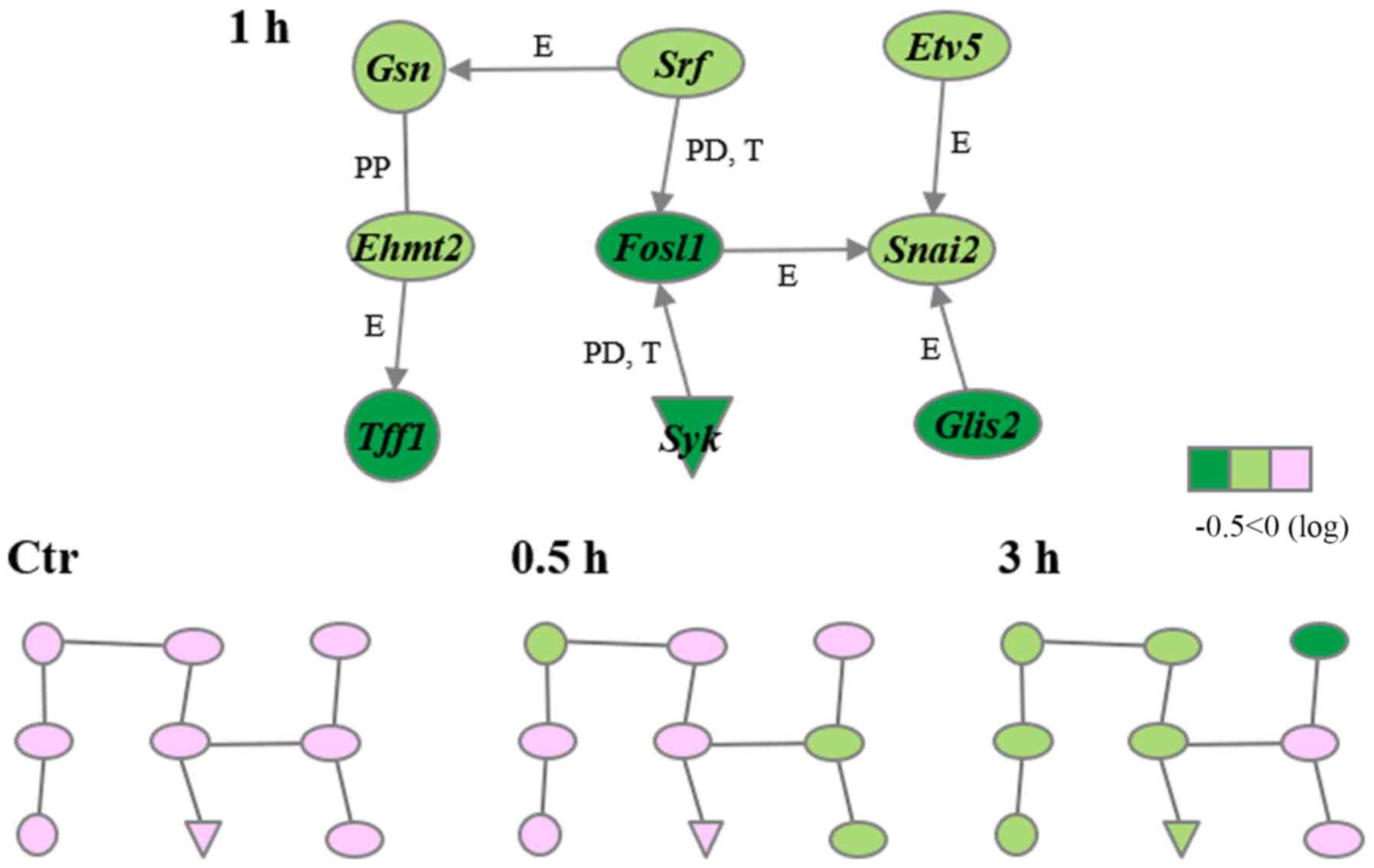
Biological function and gene network
analyses
Next, biological function and gene network analyses
were conducted by using the Ingenuity® Pathways
Knowledge Base. A total of 61 upregulated and 103 downregulated,
functionally annotated genes were identified in the 83 and 111
differentially expressed probe sets, respectively. The top 10
upregulated and top 10 downregulated genes are shown in Tables II and III, respectively. Moreover, 2
significant gene networks, labeled E (early-response) and H
(Hsf1-regulated), were identified from the upregulated genes
(Figs. 3 and 4), while a third network, labeled T
(transcription-related), was identified from the downregulated
genes (Fig. 5). Gene network E
included 11 genes - 3 IEGs (Fos, Egr1 and Ptgs2) plus
activating transcription factor 3 (Atf3), bone γ
carboxyglutamate protein (Bglap), dual specificity
phosphatase 1 (Dusp1), endothelin1 (Edn1),
fibromodulin (Fmod), gap junction protein, α 1
(Gja1), Kruppel-like factor 10 (Klf10) and
transcriptional repressor GATA binding 1 (Trps1) - and was
associated with the biological functions of differentiation of bone
cells, remodeling of bone, and ossification of bone (Fig. 3, Table
IV). Gene network H included 10 genes - 7 heat shock proteins
(HSPs) [DnaJ heat shock protein family (Hsp40) member A1
(Dnaja1), DnaJ heat shock protein family (Hsp40) member A4
(Dnaja4), DnaJ heat shock protein family (Hsp40) member B1
(Dnajb1), heat shock protein 1a/b (Hspa1), heat shock
protein 8 (Hspa8), heat shock protein 1 (Hspb1) and
heat shock 105kDa/110kDa protein 1 (Hsph1)] plus BAG
cochaperone 3 (Bag3), αB-crystallin (Cryab) and
ubiquitin C (Ubc) - and was associated with the biological
functions of protein folding, protein refolding, and apoptosis
(Fig. 4, Table IV). Ingenuity® pathway
analysis also indicated that the Hsf1 protein was predicted to be
activated at 0.5 to 3 h after LIUS stimulation (Fig. 4). In addition, we identified 9 genes
in gene network T - 6 transcription factors [euchromatic histone
lysine N-methyltransferase 2 (Ehmt2), ets variant 5
(Etv5), fos-like antigen 1 (Fosl1), GLIS family zinc
finger 2 (Glis2), snail family zinc finger 2 (Snai2)
and serum response factor (Srf)] plus gelsolin (Gsn),
spleen tyrosine kinase (Syk) and trefoil factor 1
(Tff1). This network was associated with the biological
functions of transcription, expression of RNA and activation of DNA
endogenous promoter (Fig. 5,
Table IV).
 | Figure 3.Early-response gene network.
Upregulated genes were analyzed using Ingenuity® Pathway
Analysis tools. The network is presented graphically as nodes
(genes) and edges (the biological relationships between the nodes).
Atf3, activating transcription factor 3; Bglap, bone
γ carboxyglutamate protein; Dusp1, dual specificity
phosphatase 1; Egr1, early growth response 1; Edn1,
endothelin 1; Fmod, fibromodulin; Fos, FBJ
osteosarcoma oncogene; Gja1, gap junction protein, α 1;
Klf10, Kruppel-like factor 10; Ptgs2,
prostaglandin-endoperoxide synthase 2; Trps1,
transcriptional repressor GATA binding 1. |
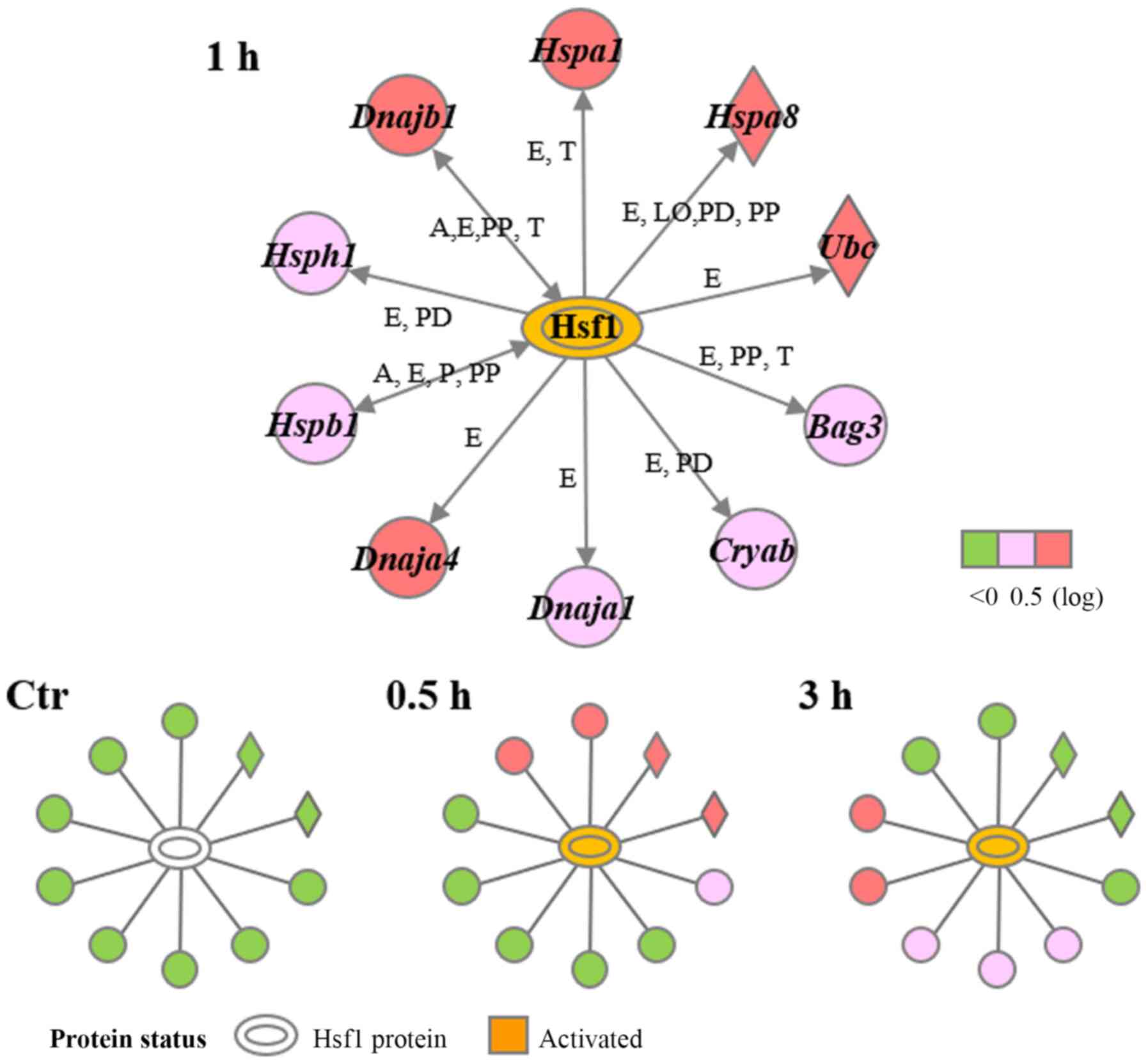 | Figure 4.Hsf1-regulated gene network.
Upregulated genes were analyzed using Ingenuity® Pathway
Analysis tools. The network is presented graphically as nodes
(genes) and edges (the biological relationships between the nodes).
A, activation; E, expression; LO, localization; P,
phosphorylation/dephosphorylation; PD, protein-DNA binding; PP,
protein-protein binding; T, transcription. Bag3, BAG
cochaperone 3; Cryab, αB-crystallin; Dnaja1, DnaJ
heat shock protein family (Hsp40) member A1; Dnaja4, DnaJ
heat shock protein family (Hsp40) member A4; Dnajb1, DnaJ
heat shock protein family (Hsp40) member B1; Hsf1, heat
shock transcription factor 1; Hspa1, heat shock protein
1a/b; Hspa8, heat shock protein 8; Hspb1, heat shock
protein 1; Hsph1, heat shock 105kDa/110kDa protein 1;
Ubc, ubiquitin C. |
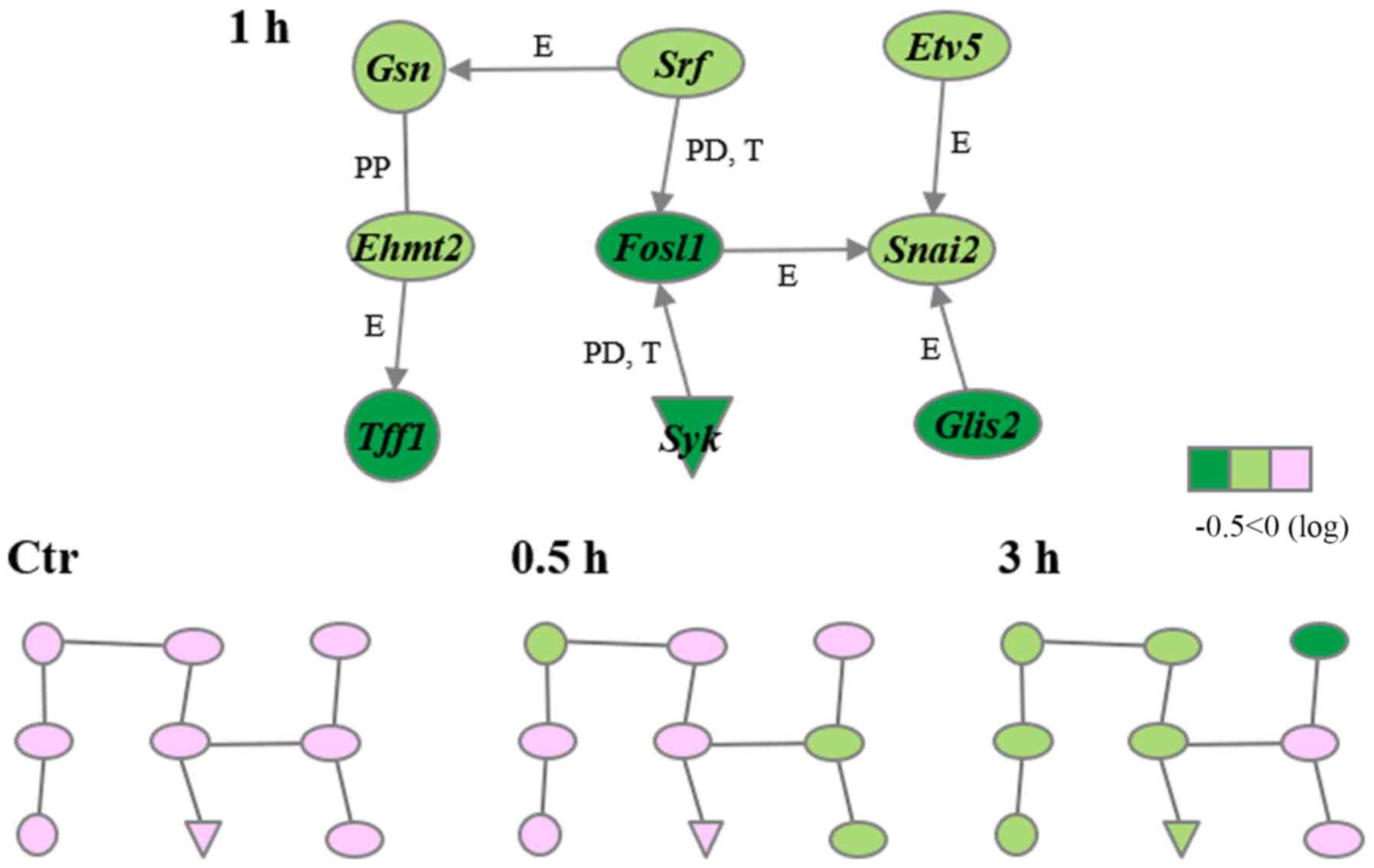 | Figure 5.Transcription-related gene network.
Downregulated genes were analyzed using Ingenuity®
Pathway Analysis tools. The network is presented graphically as
nodes (genes) and edges (the biological relationships between the
nodes). E, expression; PP, protein-protein binding; PD, protein-DNA
binding; T, transcription. Ehmt2, euchromatic histone lysine
N-methyltransferase 2; Etv5, ets variant 5; Fosl1,
fos-like antigen 1; Glis2, GLIS family zinc finger 2;
Gsn, gelsolin; Snai2, snail family zinc finger 2;
Srf, serum response factor; Syk, spleen tyrosine
kinase; Tff1, trefoil factor 1. |
 | Table II.Top 10 upregulated genes. |
Table II.
Top 10 upregulated genes.
|
| Fold-change |
|
|---|
|
|
|
|
|---|
| Gene symbol | 0.5 h | 1 h | 3 h | Description |
|---|
| Hspa1a | 73.0 | 102.6 | 14.5 | Heat shock protein
1A |
| Fos | 26.8 |
11.0 |
1.9 | FBJ osteosarcoma
oncogene |
| Hspa1b | 10.5 |
11.0 |
7.3 | Heat shock protein
1B |
| Egr1 | 10.0 |
5.6 |
1.5 | Early growth
response 1 |
| Hspb1 |
6.2 |
6.3 |
9.1 | Heat shock protein
1 |
| St3gal6 |
5.8 |
1.8 |
3.5 | ST3
beta-galactoside α-2,3-sialyltransferase 6 |
| Dnajb1 |
5.4 |
6.4 |
1.2 | DnaJ (Hsp40)
homolog, subfamily B, member 1 |
| Arc |
5.3 |
4.0 |
0.9 | Activity regulated
cytoskeletal-associated protein |
| Dnaja4 |
5.3 |
7.9 |
5.4 | DnaJ (Hsp40)
homolog, subfamily A, member 4 |
| Hspa8 |
5.1 |
2.6 |
0.7 | Heat shock protein
8 |
 | Table III.Top 10 downregulated genes. |
Table III.
Top 10 downregulated genes.
|
| Fold-change |
|
|---|
|
|
|
|
|---|
| Gene symbol | 0.5 h | 1 h | 3 h | Description |
|---|
| Ddah1 | 0.10 | 0.04 | 0.06 | Dimethylarginine
dimethylaminohydrolase 1 |
| Gsn | 0.13 | 0.15 | 0.11 | Gelsolin |
| Flnc | 0.18 | 0.18 | 0.60 | Filamin C, γ |
| Itgb1 | 0.19 | 0.18 | 0.30 | Integrin beta
1 |
| Ddx55 | 0.20 | 0.52 | 0.61 | DEAD
(Asp-Glu-Ala-Asp) box polypeptide 55 |
| Riok1 | 0.30 | 0.77 | 0.88 | RIO kinase 1 |
| Pcsk4 | 0.31 | 0.79 | 0.62 | Proprotein
convertase subtilisin/kexin type 4 |
| Cerk | 0.36 | 0.66 | 0.67 | Ceramide
kinase |
| Tbca | 0.36 | 0.64 | 0.84 | Tubulin cofactor
A |
| Nlgn2 | 0.37 | 0.38 | 0.50 | Neuroligin 2 |
 | Table IV.Biological functions in gene
networks. |
Table IV.
Biological functions in gene
networks.
| Name | P-value | Genes |
|---|
| Gene network E |
|
|
|
Differentiation of bone
cells |
2.83×10−8 | Bglap, Edn1,
Fos, Gja1, Klf10 and Ptgs2 |
|
Remodeling of bone |
5.19×10−10 | Bglap, Edn1,
Egr1, Fos, Gja1 and Ptgs2 |
|
Ossification of bone |
2.39×10−9 | Fmod, Gja1,
Klf10, Ptgs2 and Trps1 |
| Gene network H |
|
|
| Folding
of protein |
6.37×10−13 | Cryab, Dnaja1,
Dnaja4, Hspa8, Hspa1 and Hspb1 |
|
Refolding of protein |
3.56×10−11 | Dnaja1, Dnaja4,
Hspa8 and Hspa1 |
|
Apoptosis |
2.00×10−6 | Bag3, Cryab,
Dnaja1, Dnajb1, Hspa8, Hspa1, Hspb1, Hsph1 and Ube |
| Gene network T |
|
|
|
Transcription |
1.84×10−9 | Ehmt2, Etv5,
Fosl1, Glis2, Gsn, Snai2, Srf, Syk and Tff1 |
|
Expression of RNA |
3.70×10−9 | Ehmt2, Etv5,
Fosl1, Glis2, Gsn, Snai2, Srf, Syk and Tff1 |
|
Activation of DNA endogenous
promoter |
1.76×10−6 | Ehmt2, Etv5,
Fosl1, Glis2, Snai2a and Srf |
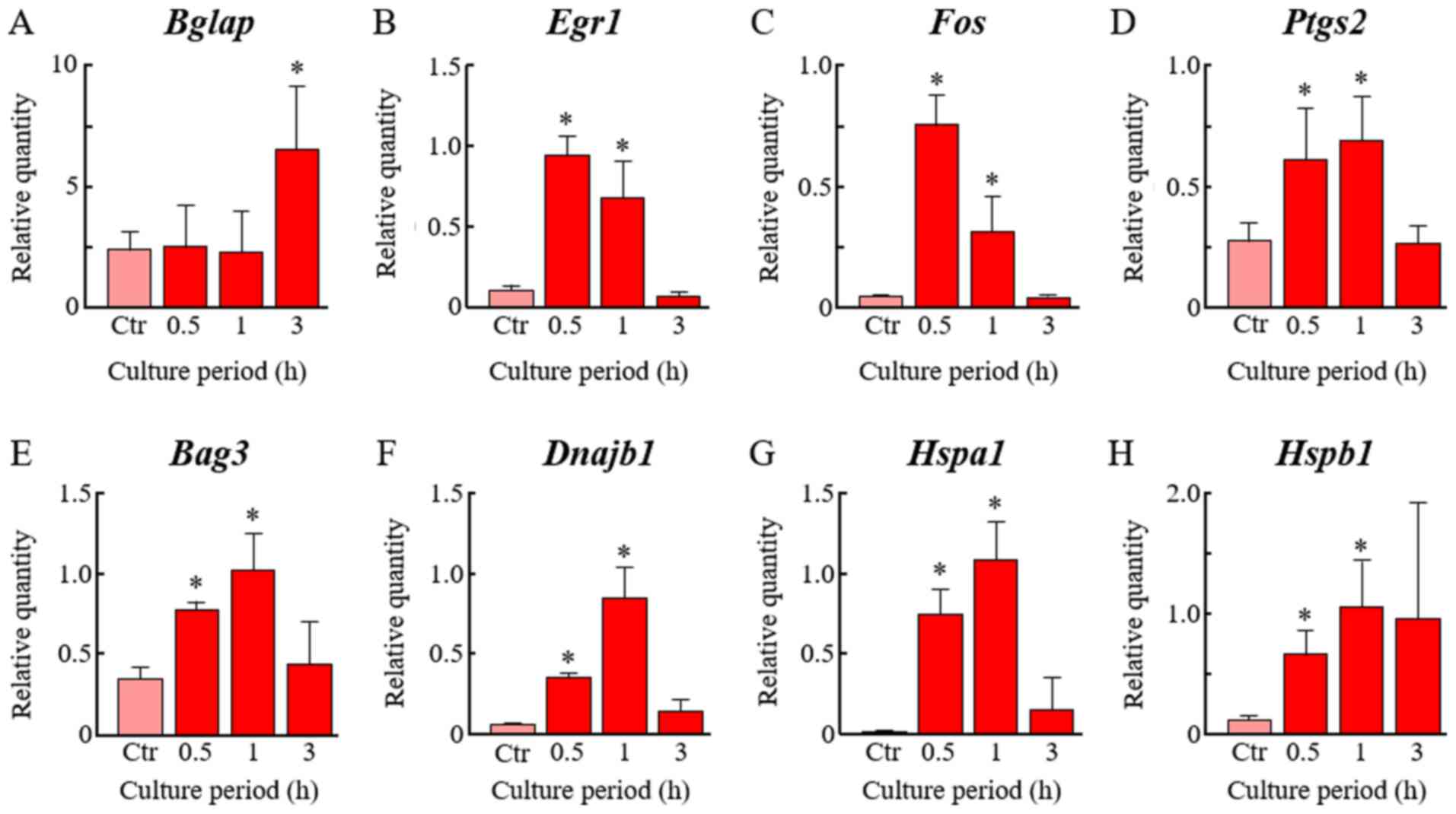
Verification of upregulated genes by
qRT-PCR assay
Eight upregulated genes were chosen: Bglap, Egr1,
Fos, and Ptgs2 from gene network E, and Bag3, Dnajb1,
Hspa1 and Hspb1 from gene network H. As shown in
Fig. 6, treatment of cells with
LIUS at 25 mW/cm2 for 20 min significantly elevated the
expression levels of all 8 genes. The expression levels peaked at
0.5–1.0 h after LIUS stimulation in 7 genes, i.e., Egr1, Fos,
Ptgs2, Bag3, Dnajb1, Hspa1 and Hspb1. On the other hand,
the peak expression level of Bglap was observed 3 h after
LIUS exposure (Fig. 6).
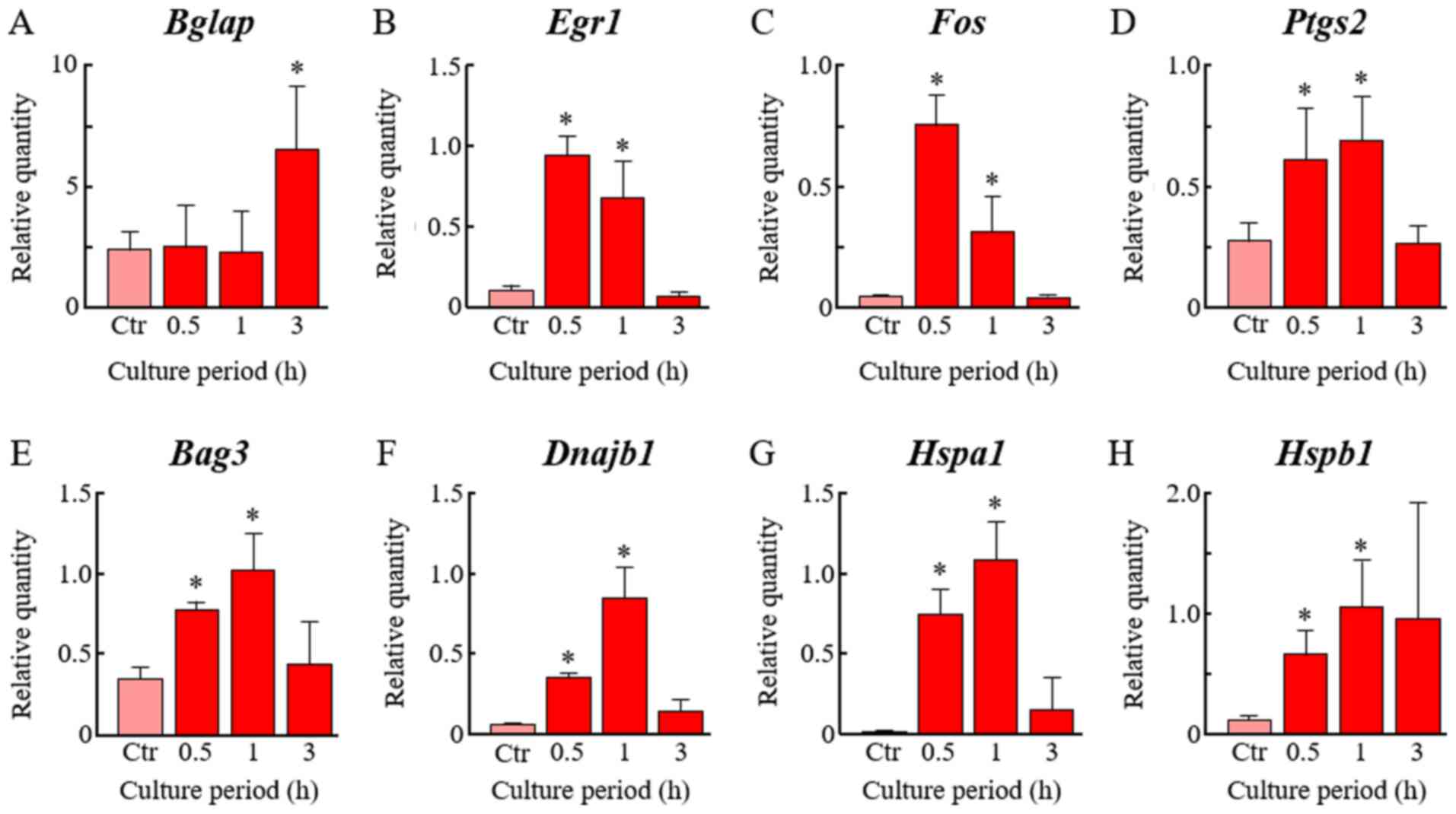 | Figure 6.Verification of the upregulated genes
determined via RT-qPCR. After treatment with low-intensity
ultrasound at 25 mW/cm2 for 20 min, cells were cultured
for 0.5, 1 or 3 h at 37°C. RT-qPCR was performed with specific
primers for (A) Bglap, (B) Egr1, (C) Fos, (D)
Ptgs2, (E) Bag3, (F) Dnajb1, (G) Hspa1
and (H) Hspb1. Levels were normalized to that of Actb.
Non-treated cells were served as the Ctr. Data are presented as the
mean ± SD (n=4). *P<0.05 vs. the Ctr group. RT-qPCR, reverse
transcription-quantitative PCR; Ctr, control. Bglap, bone γ
carboxyglutamate protein; Egr1, early growth response 1;
Fos, FBJ osteosarcoma oncogene; Ptgs2,
prostaglandin-endoperoxide synthase 2; Bag3, BAG cochaperone
3; Dnajb1, DnaJ heat shock protein family (Hsp40) member B1;
Hspa1, heat shock protein 1a/b; Hspb1, heat shock
protein 1. |
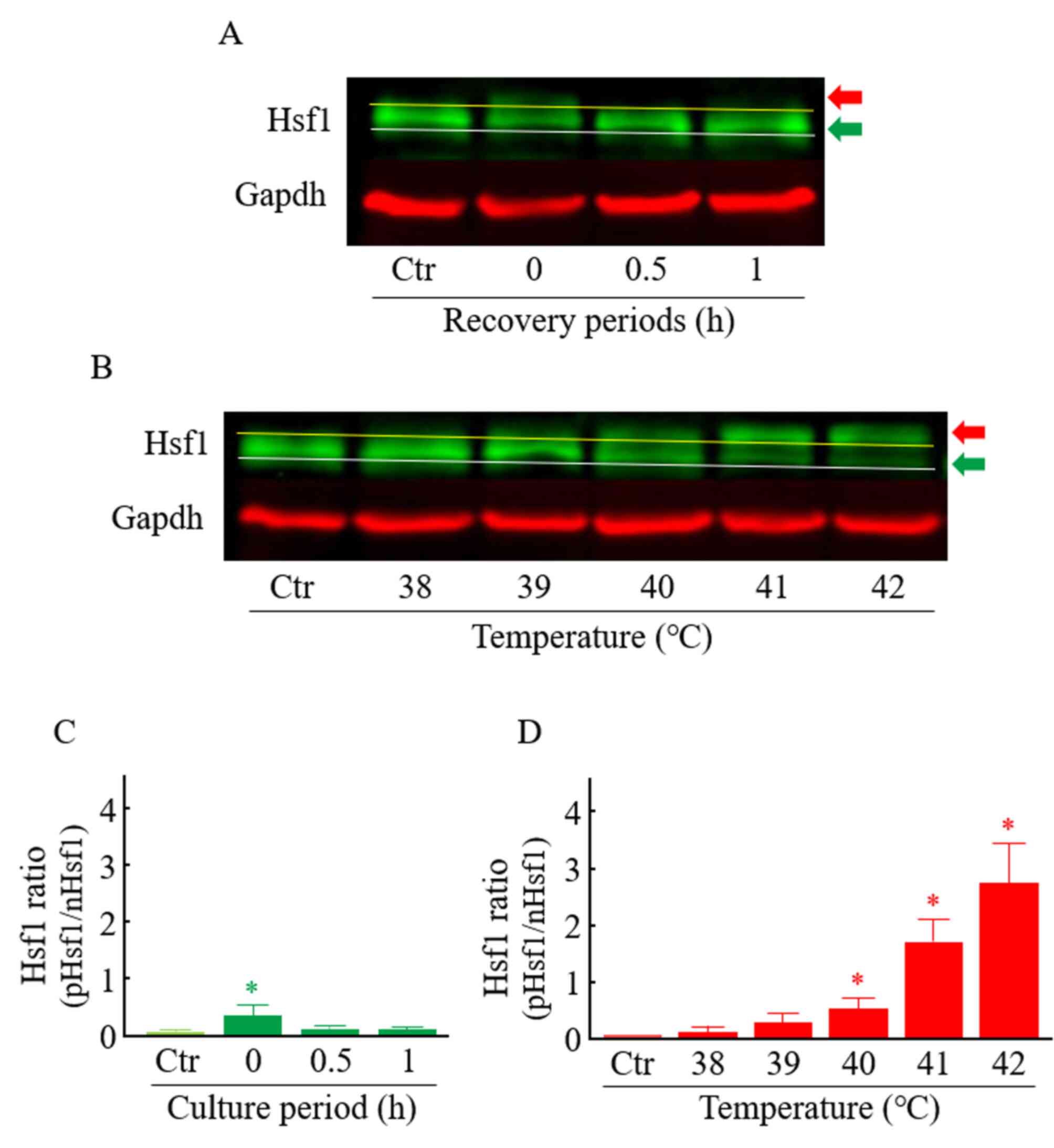
Effects of LIUS on the Hsf1
activation
Under heat-stress conditions, the induction of HSPs
principally occurs through the activation of Hsf1. It is well known
that the mobility shift and nuclear translocation of Hsf1 due to
its phosphorylation indicates activation of the molecule (28). Here, LIUS (25 mW/cm2 for
20 min) induced the temperature rise of the culture medium from
35.3±0.23°C (control) to 38.1±0.29°C (mean ± SD, n=4). Under
control conditions, the ratio of phosphorylated Hsf1 (mobility
shift of Hsf1) to non-phosphorylated Hsf1 was very low. On the
other hand, a slight but significant mobility shift of Hsf1 was
observed at 0 h after the LIUS treatment (Fig. 7A and C). Under heat-treated
conditions, the mobility shift of Hsf1 0 h after the heat exposure
was markedly and significantly increased in a temperature-dependent
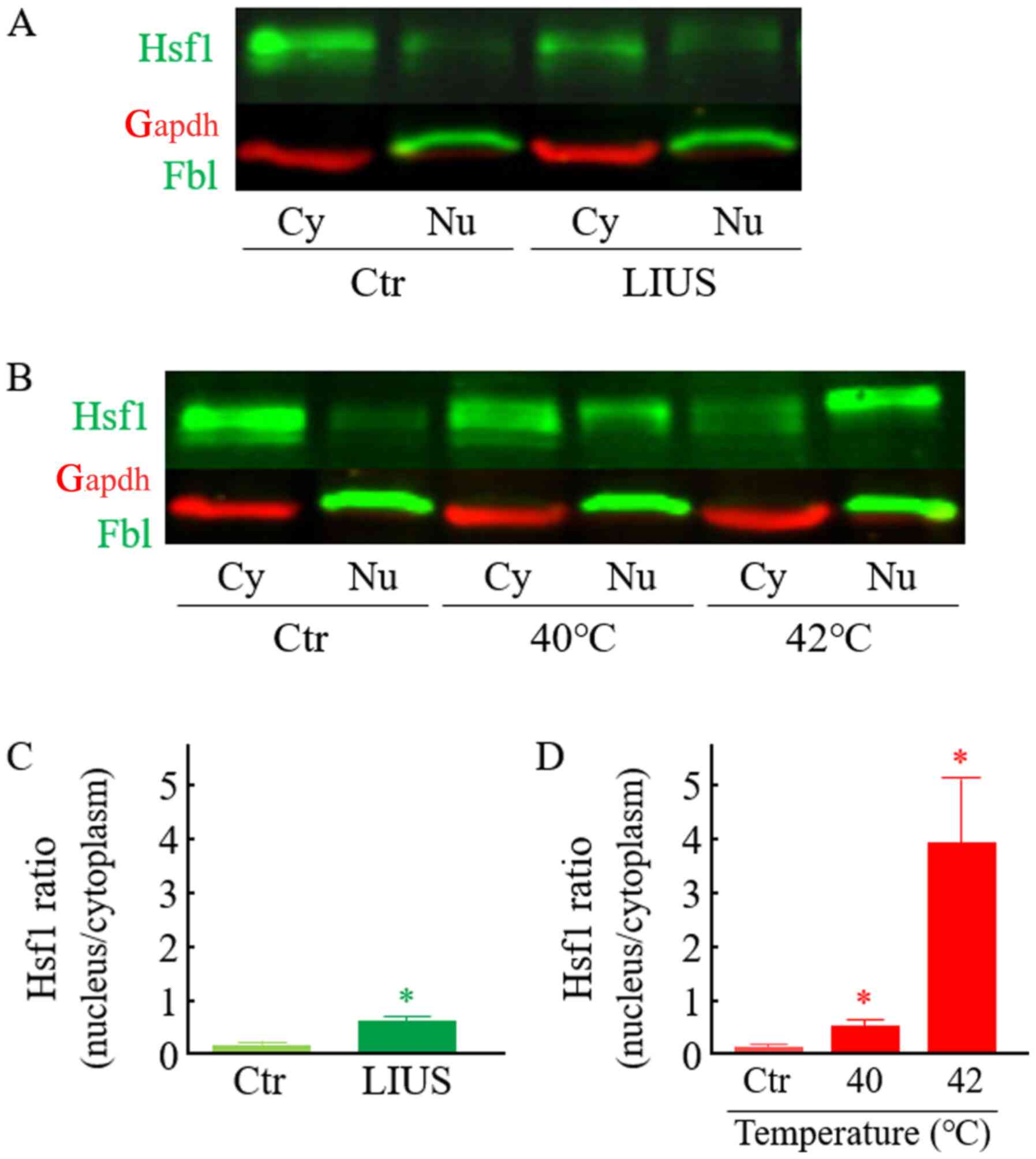
manner (Fig. 7B and D). As shown in
Fig. 8, Hsf1 was principally
localized in the cytosolic compartments in the control cells.
Treatment of cells with LIUS significantly induced the nuclear
localization of Hsf1 (Fig. 8A and
C). This translocation was comparable to that in the cells
treated with heat at 40°C for 20 min. On the other hand, the ratio
of nucleus Hsf1 to cytoplasm Hsf1 was dramatically elevated in the
cells treated with heat at 42°C for 20 min (Fig. 8A and D). These data suggested that
Hsf1 is activated in the cells treated with LIUS.
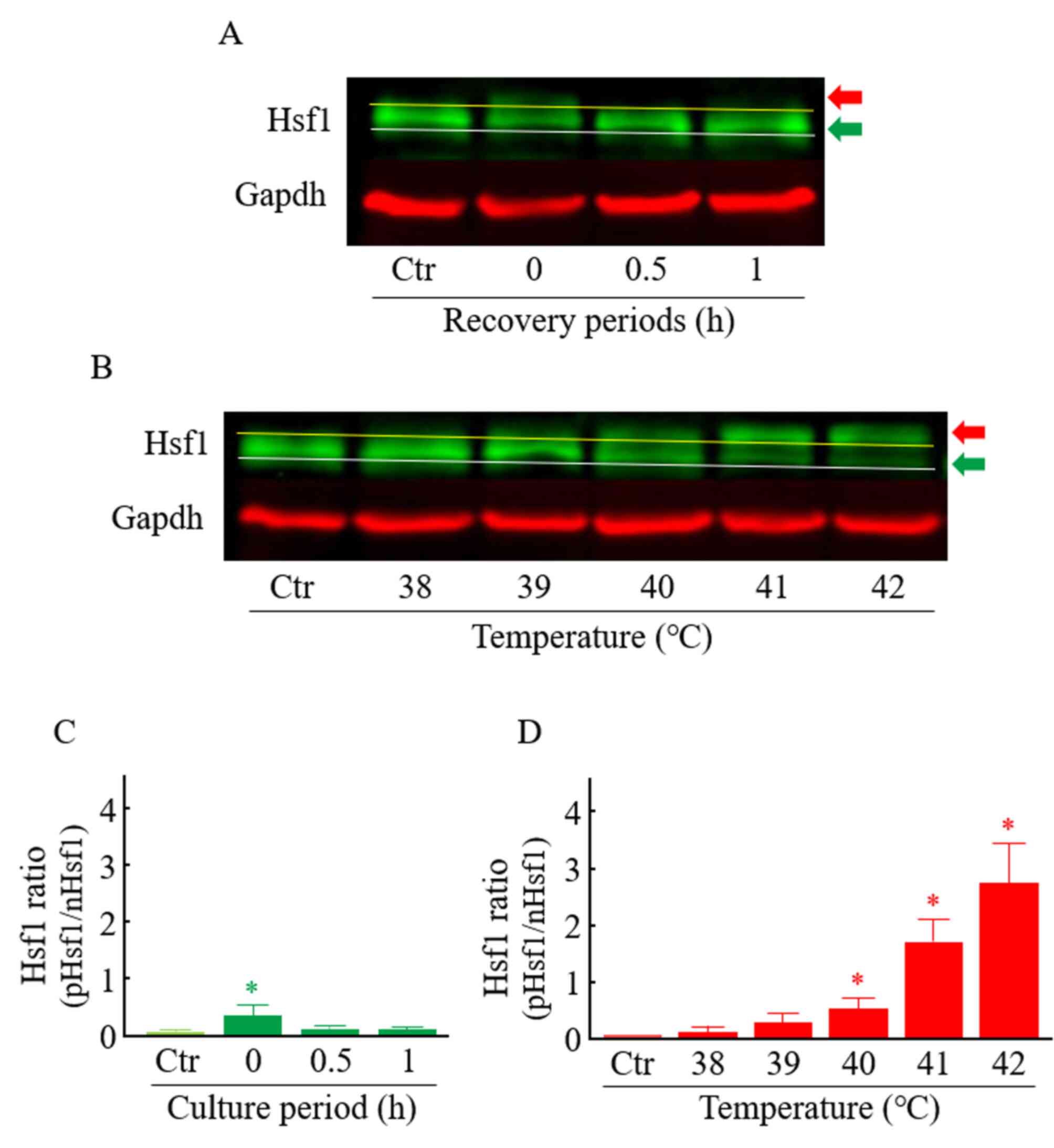 | Figure 7.Effects of LIUS and heat on the
activation of Hsf1 in ST2 cells. Cells were exposed to LIUS (25
mW/cm2) or heat (38, 39, 40, 41 or 42°C) for 20 min, and
cultured at 37°C. (A and C) Cells were harvested 0, 0.5 or 1 h
after LIUS exposure. (B and D) Cells were harvested immediately
after heat exposure. Western blotting was carried out using
specific primary antibodies against Hsf1 and Gapdh. Each Hsf1 band
density was quantified, and the ratio (phosphorylated Hsf1 to
non-phosphorylated Hsf1) was calculated. Gapdh served as a loading
control. Green arrow indicates nHsf1. Red arrow indicates pHsf1.
Data are presented as the mean ± SD (n=4–6). *P<0.05 vs. the Ctr
group. LIUS, low-intensity ultrasound; Ctr, control; Hsf1, heat
shock transcription factor 1; p, phosphorylated; n,
non-phosphorylated; Gapdh, glyceraldehyde 3-phosphate
dehydrogenase. |
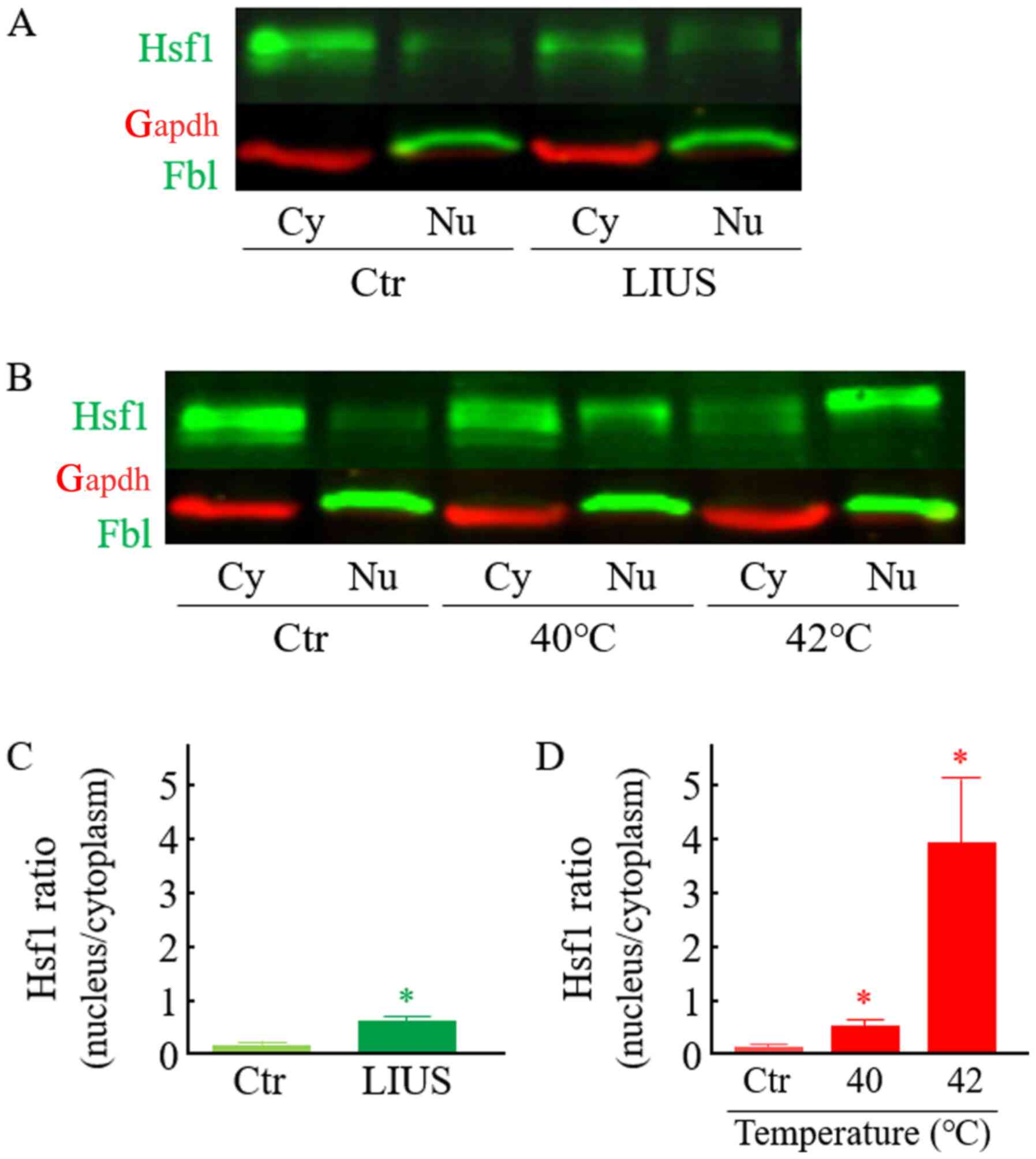 | Figure 8.Effect of LIUS and heat on the
intracellular localization of Hsf1 in ST2 cells. Cells were exposed
to (A and C) LIUS (25 mW/cm2) or (B and D) heat (40 or
42°C) for 20 min. Immediately after stress treatment, cells were
harvested. Either the cytoplasmic or nuclear fraction was
separated. Western blotting was carried out using specific primary
antibodies against Hsf1, Gapdh and Fbl. (C and D) Each band density
of Hsf1 was quantified, and the ratio (nucleus to cytoplasm) was
calculated. Gapdh and Fbl served as marker proteins for the
cytoplasm and nucleus, respectively. Data are presented as the mean
± SD (n=4). *P<0.05 vs. the Ctr group. LIUS, low-intensity
ultrasound; Hsf1, heat shock transcription factor 1; Fbl,
fibrillarin; Ctr, control; Cy, cytoplasm; Nu, nucleus; Gapdh,
glyceraldehyde 3-phosphate dehydrogenase. |
Discussion
LIUS has clear clinical potential for bone fracture
healing. However, the molecular mechanisms underlying the ability
of bone cells to detect LIUS stimulation have not been well
understood. Here, when we used our developed irradiating system
(13) to apply a single LIUS
irradiation at an ISATA of 25 mW/cm2
for 20 min, which is approximately equivalent to the clinical
condition (30 mW/cm2 for 20 min) (1,2), we
identified many differentially expressed genes and 3 unique gene
networks in LIUS-treated mouse ST2 BMSCs. To our knowledge, this is
the first report to identify changes in cellular gene expression as
an early cellular response to LIUS.
In the present study, a number of genes (61
upregulated and 103 downregulated) that responded to LIUS at an
early time point (0.5 to 3 h) were found to be differentially
expressed. Of these 164 genes, the expression levels of 3 genes
(Bag3, Dnajb1 and Hspa1) and 4 genes [pentraxin
related gene (Ptx3), Gja1, integrin beta 1
(Itgb1) and methionine aminopeptidase 2 (Metap2)]
were reported to be affected 3 h after LIUS at 300
mW/cm2 for 1 min in human leukemia Molt-4 (22) or lymphoma U937 cells (23), respectively. Except for these 7
genes, however, none of the genes identified here were reported in
previous microarray investigations in which the gene expression
patterns were monitored 3–24 h after LIUS (30–300
mW/cm2) in several cell types (18–23).
Particularly noteworthy in this study was the
detection of gene network E, which contained 3 IEGs, i.e., Fos,
Egr1, and Ptgs2, that were found to be associated mainly
with the biological functions of bone physiology. IEGs respond to a
wide variety of stresses, including LIUS (9–14). In
our previous study, qRT-PCR analysis confirmed the up-regulation of
the transient expression of these 3 IEGs in LIUS-treated ST2 cells
(13). Fos, Egr1, and Ptgs2
proteins are reported to have essential roles in bone formation
(25,29–31).
Our results showed that network E also included Bglap
(32), Edn1 (33) and Gja1 (34), which are known to be involved in the
differentiation of bone cells. It is thus intriguing that
interactions have been reported between Fos on the one hand
and Bglap (35), Edn1
(36), Gja1 (37) or Ptgs2 (38) on the other.
In this study, gene network H containing
Hsf1-regulated genes - 7 HSP genes (39,40),
Bag3 (39), Cryab
(41) and Ubc (42) - was obtained from up-regulated genes
and was associated principally with the biological functions of
protein folding and apoptosis. The products translated from these
genes are known to exert chaperonic and anti-apoptotic activity
(39,40). To our surprise,
Ingenuity® pathway analysis indicated that the Hsf1
protein was activated at 0.5 to 3 h after LIUS stimulation
(Fig. 4). We confirmed the
transient activation of the Hsf1 protein by using Western blot
analysis (Figs. 7 and 8). Under our experimental conditions, the
medium temperature was increased from 35.3°C (control) to 38.1°C in
LIUS-treated cells (25 mW/cm2, 20 min). On the other
hand, our previous study showed that heat treatment of the cells at
38°C for 20 min did not affect Fos expression (13). Zhang et al (16) previously reported that upregulation
of the Hsp70 protein was observed in the human adipose-derived
cells treated with LIUS at 30 mW/cm2 for 30 min, and the
temperature in the medium increased from 37°C to 40°C during the
LIUS exposure. Very weak but nonetheless significant heat-inducible
heat shock element-binding activity of Hsf1 has been reported in
cells incubated at 39°C for 20 min (43). Our previous paper also clearly
indicated a transient activation of Hsf1 at 0.5–1 h after mild
hyperthermia treatment (41°C, for 30 min) in human lymphoma U937
cells (44). It is well known that
Hsf1 can be activated by a wide variety of stressors, such as
oxidative stress, heavy metals, toxins, and bacterial infections,
in addition to heat (39). In
addition, under nonthermal-LIUS conditions (300 mW/cm2
for 1 min; temperature rise in medium: 0.3°C), the expression of
HSP genes increased significantly in human leukemia Molt-4 cells
(22). We considered that the
induction of genes such as HSPs in gene network H may have been
attributable, at least in part, to the activation of Hsf1 by the
slight rise in temperature.
In the present study, LIUS decreased the expression
levels of many genes. Previous findings demonstrated that heat
activates the transcription of HSPs coincident with a bulk decrease
in mRNA and protein syntheses, and this overall reprogramming of
gene expression permits the selective synthesis of HSPs in
mammalian cells (45). In the
present study, we detected gene network T, which contained many
transcription factors in down-regulated genes. Functional analysis
using the Ingenuity® Pathways Knowledge Base
demonstrated that this network was associated with the biological
functions of gene expression. For example, Etv5 (46), Fosl1 (47), Glis2 (48) and Srf (49) proteins increase the transcription of
promoters by RNA polymerase II complex.
In conclusion, LIUS as shown to elicit gene
expression even after short application in mouse ST2 BMSCs. The
present results provide a basis for elucidation of the detailed
molecular mechanisms underlying the cellular effects of LIUS.
However, the biological roles of genes induced by LIUS in either
cell or animal models remain a subject for further investigation.
Therapeutic LIUS has been used to enhance bone healing caused by
fracture in humans (1,2). The effects and possible advantages of
ultrasound have been a subject of increasing interest in other
fields of medicine as well, including oncology, surgery, gene
therapy and regenerative medicine (50–56).
Therefore, genetic effects should also be considered to be a factor
in these other fields.
Supplementary Material
Supporting Data
Acknowledgements
Not applicable.
Funding
The present study was supported by JSPS KAKENHI
(grant nos. 17K01353, 20K12619 and 20K06718).
Availability of data and materials
The datasets used and/or analyzed during the current
study are available from the corresponding author on reasonable
request.
Authors' contributions
YT and TM designed the experiments and wrote the
paper. YT, TM, HH, NS, YF, TH, RN, JH and NH performed the
experiments. YT, HH and TM analyzed the data. All authors read and
approved the final manuscript.
Ethics approval and consent to
participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing
interests.
Glossary
Abbreviations
Abbreviations:
|
Actb
|
β-actin
|
|
ALP
|
alkaline phosphatase
|
|
AP-1
|
activator protein-1
|
|
Atf3
|
activating transcription factor 3
|
|
Bag3
|
BAG cochaperone 3
|
|
BMSCs
|
bone marrow stromal cells
|
|
Bglap
|
bone γ carboxyglutamate protein
|
|
Cryab
|
αB-crystallin
|
|
Dnaja1
|
DnaJ heat shock protein family
(Hsp40) member A1
|
|
Dnaja4
|
DnaJ heat shock protein family
(Hsp40) member A4
|
|
Dnajb1
|
DnaJ heat shock protein family
(Hsp40) member B1
|
|
Dusp1
|
dual specificity phosphatase 1
|
|
Edn1
|
endothelin 1
|
|
Egr1
|
early growth response 1
|
|
Ehmt2
|
euchromatic histone lysine
N-methyltransferase 2
|
|
Etv5
|
ets variant 5
|
|
Fbl
|
fibrillarin
|
|
Fmod
|
fibromodulin
|
|
Fos
|
FBJ osteosarcoma oncogene
|
|
Fosl1
|
fos-like antigen 1
|
|
Gapdh
|
glyceraldehyde 3-phosphate
dehydrogenase
|
|
Gja1
|
gap junction protein, α 1
|
|
Glis2
|
GLIS family zinc finger 2
|
|
Gsn
|
gelsolin
|
|
Hsf1
|
heat shock transcription factor 1
|
|
Hspa1
|
heat shock protein 1a/b
|
|
Hspa8
|
heat shock protein 8
|
|
Hspb1
|
heat shock protein 1
|
|
Hsph1
|
heat shock 105kDa/110kDa protein
1
|
|
HSPs
|
heat shock proteins
|
|
IEGs
|
immediate-early genes
|
|
ISATA
|
spatial-average temporal-average
|
|
Itgb1
|
integrin beta 1
|
|
Jun
|
jun proto-oncogene
|
|
Klf10
|
Kruppel-like factor 10
|
|
LIUS
|
low-intensity ultrasound
|
|
Metap2
|
methionine aminopeptidase 2
|
|
PAGE
|
polyacrylamide gel
electrophoresis
|
|
Ptgs2
|
prostaglandin-endoperoxide synthase
2
|
|
Ptx3
|
pentraxin related gene
|
|
RT-qPCR
|
reverse transcription-quantitative
polymerase chain reaction
|
|
SD
|
standard deviation
|
|
Snai2
|
snail family zinc finger 2
|
|
Srf
|
serum response factor
|
|
Syk
|
spleen tyrosine kinase
|
|
Tff1
|
trefoil factor 1
|
|
Trps1
|
transcriptional repressor GATA
binding 1
|
|
Ubc
|
ubiquitin C
|
References
|
1
|
Padilla F, Puts R, Vico L and Raum K:
Stimulation of bone repair with ultrasound: A review of the
possible mechanic effects. Ultrasonics. 54:1125–1145. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Harrison A, Lin S, Pounder N and
Mikuni-Takagaki Y: Mode & mechanism of low intensity pulsed
ultrasound (LIPUS) in fracture repair. Ultrasonics. 70:45–52. 2016.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Duarte LR: The stimulation of bone growth
by ultrasound. Arch Orthop Trauma Surg. 101:153–159. 1983.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Azuma Y, Ito M, Harada Y, Takagi H, Ohta T
and Jingushi S: Low-intensity pulsed ultrasound accelerates rat
femoral fracture healing by acting on the various cellular
reactions in the fracture callus. J Bone Miner Res. 16:671–680.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hidaka K, Mikuni-Takagaki Y,
Wada-Takahashi S, Saita M, Kawamata R, Sato T, Kawata A, Miyamoto
C, Maehata Y, Watabe H, et al: Low intensity pulsed ultrasound
prevents development of bisphosphonate related osteonecrosis of the
jaw like pathophysiology in a rat model. Ultrasound Med Biol.
45:1721–1732. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Sun L, Sun S, Zhao X, Zhang J, Guo J, Tang
L and Ta D: Inhibition of myostatin signal pathway may be involved
in low-intensity pulsed ultrasound promoting bone healing. J Med
Ultrason (2001). 46:377–388. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Heckman JD, Ryaby JP, McCabe J, Frey JJ
and Kilcoyne RF: Acceleration of tibial fracture-healing by
non-invasive, low-intensity pulsed ultrasound. J Bone Joint Surg
Am. 76:26–34. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kristiansen TK, Ryaby JP, McCabe J, Frey
JJ and Roe LR: Accelerated healing of distal radial fractures with
the use of specific, low-intensity ultrasound. A multicenter,
prospective, randomized, double-blind, placebo-controlled study. J
Bone Joint Surg Am. 79:961–973. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Naruse K, Mikuni-Takagaki Y, Azuma Y, Ito
M, Oota T, Kameyama K and Itoman M: Anabolic response of mouse
bone-marrow-derived stromal cell clone ST2 cells to low-intensity
pulsed ultrasound. Biochem Biophys Res Commun. 268:216–220. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Naruse K, Miyauchi A, Itoman M and
Mikuni-Takagaki Y: Distinct anabolic response of osteoblast to
low-intensity pulsed ultrasound. J Bone Miner Res. 18:360–369.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Sena K, Leven RM, Mazhar K, Sumner DR and
Virdi AS: Early gene response to low-intensity pulsed ultrasound in
rat osteoblastic cells. Ultrasound Med Biol. 31:703–708. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Louw TM, Budhiraja G, Viljoen HJ and
Subramanian A: Mechanotransduction of ultrasound is frequency
dependent below the cavitation threshold. Ultrasound Med Biol.
39:1303–1319. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Tabuchi Y, Hasegawa H, Suzuki N, Furusawa
Y, Hirano T, Nagaoka R, Takeuchi SI, Shiiba M and Mochizuki T:
Low-intensity pulsed ultrasound promotes the expression of
immediate-early genes in mouse ST2 bone marrow stromal cells. J Med
Ultrason (2001). 47:193–201. 2020. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tang CH, Yang RS, Huang TH, Lu DY, Chuang
WJ, Huang TF and Fu WM: Ultrasound stimulates cyclooxygenase-2
expression and increases bone formation through integrin, focal
adhesion kinase, phosphatidylinositol 3-kinase, and Akt pathway in
osteoblasts. Mol Pharmacol. 69:2047–2057. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Costa V, Carina V, Fontana S, De Luca A,
Monteleone F, Pagani S, Sartori M, Setti S, Faldini C, Alessandro
R, et al: Osteogenic commitment and differentiation of human
mesenchymal stem cells by low-intensity pulsed ultrasound
stimulation. J Cell Physiol. 233:1558–1573. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Zhang Z, Ma Y, Guo S, He Y, Bai G and
Zhang W: Low-intensity pulsed ultrasound stimulation facilitates in
vitro osteogenic differentiation of human adipose-derived stem
cells via up-regulation of heat shock protein (HSP)70, HSP90, and
bone morphogenetic protein (BMP) signaling pathway. Biosci Rep.
38:BSR201800872018. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Su Z, Xu T, Wang Y, Guo X, Tu J, Zhang D,
Kong X, Sheng Y and Sun W: Low intensity pulsed ultrasound promotes
apoptosis and inhibits angiogenesis via p38 signaling mediated
endoplasmic reticulum stress in human endothelial cells. Mol Med
Rep. 19:4645–4654. 2019.PubMed/NCBI
|
|
18
|
Leskinen JJ, Karjalainen HM, Olkku A,
Hynynen K, Mahonen A and Lammi MJ: Genome-wide microarray analysis
of MG-63 osteoblastic cells exposed to ultrasound. Biorheology.
45:345–354. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Kobayashi Y, Sakai D, Iwashina T, Iwabuchi
S and Mochida J: Low-intensity pulsed ultrasound stimulates cell
proliferation, proteoglycan synthesis and expression of growth
factor-related genes in human nucleus pulposus cell line. Eur Cell
Mater. 17:15–22. 2009.PubMed/NCBI
|
|
20
|
Lu H, Qin L, Lee K, Cheung W, Chan K and
Leung K: Identification of genes responsive to low-intensity pulsed
ultrasound stimulations. Biochem Biophys Res Commun. 378:569–573.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Tabuchi Y, Sugahara Y, Ikegame M, Suzuki
N, Kitamura K and Kondo T: Genes responsive to low-intensity pulsed
ultrasound in MC3T3-E1 preosteoblast cells. Int J Mol Sci.
14:22721–22740. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Tabuchi Y, Ando H, Takasaki I, Feril LB
Jr, Zhao QL, Ogawa R, Kudo N, Tachibana K and Kondo T:
Identification of genes responsive to low intensity pulsed
ultrasound in a human leukemia cell line Molt-4. Cancer Lett.
246:149–156. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Tabuchi Y, Takasaki I, Zhao QL, Wada S,
Hori T, Feril LB Jr, Tachibana K, Nomura T and Kondo T: Genetic
networks responsive to low-intensity pulsed ultrasound in human
lymphoma U937 cells. Cancer Lett. 270:286–294. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Bahrami S and Drabløs F: Gene regulation
in the immediate-early response process. Adv Biol Regul. 62:37–49.
2016. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Wagner EF and Eferl R: Fos/AP-1 proteins
in bone and the immune system. Immunol Rev. 208:126–140. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Tabuchi Y, Maekawa K, Torigoe M, Furusawa
Y, Hirano T, Minagawa S, Yunoki T and Hayashi A: HIKESHI silencing
can enhance mild hyperthermia sensitivity in human oral squamous
cell carcinoma HSC-3 cells. Int J Mol Med. 46:58–66. 2020.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Furusawa Y, Yamamoto T, Hattori A, Suzuki
N, Hirayama J, Sekiguchi T and Tabuchi Y: De novo transcriptome
analysis and gene expression profiling of fish scales isolated from
Carassius auratus during space flight: Impact of melatonin
on gene expression in response to space radiation. Mol Med Rep.
22:2627–2636. 2020.PubMed/NCBI
|
|
28
|
Sarge KD, Murphy SP and Morimoto RI:
Activation of heat shock gene transcription by heat shock factor 1
involves oligomerization, acquisition of DNA-binding activity, and
nuclear localization and can occur in the absence of stress. Mol
Cell Biol. 13:1392–1407. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Cenci S, Weitzmann MN, Gentile MA, Aisa MC
and Pacifici R: M-CSF neutralization and egr-1 deficiency prevent
ovariectomy-induced bone loss. J Clin Invest. 105:1279–1287. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Demiralp B, Chen HL, Koh AJ, Keller ET and
McCauley LK: Anabolic actions of parathyroid hormone during bone
growth are dependent on c-fos. Endocrinology. 143:4038–4047. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Choudhary S, Halbout P, Alander C, Raisz L
and Pilbeam C: Strontium ranelate promotes osteoblastic
differentiation and mineralization of murine bone marrow stromal
cells: Involvement of prostaglandins. J Bone Miner Res.
22:1002–1010. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Paredes R, Arriagada G, Cruzat F, Villagra
A, Olate J, Zaidi K, van Wijnen A, Lian JB, Stein GS, Stein JL, et
al: Bone-specific transcription factor Runx2 interacts with the
1alpha,25-dihydroxyvitamin D3 receptor to up-regulate rat
osteocalcin gene expression in osteoblastic cells. Mol Cell Biol.
24:8847–8861. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Salama M, Andrukhova O, Jaksch P, Taghavi
S, Kelpetko W, Dekan G and Aharinejad S: Endothelin-1 governs
proliferation and migration of bronchoalveolar lavage-derived lung
mesenchymal stem cells in bronchiolitis obliterans syndrome.
Transplantation. 92:155–162. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Hashida Y, Nakahama K, Shimizu K, Akiyama
M, Harada K and Morita I: Communication-dependent mineralization of
osteoblasts via gap junctions. Bone. 61:19–26. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Owen TA, Bortell R, Yocum SA, Smock SL,
Zhang M, Abate C, Shalhoub V, Aronin N, Wright KL and van Wijnen
AJ: Coordinate occupancy of AP-1 sites in the vitamin D-responsive
and CCAAT box elements by Fos-Jun in the osteocalcin gene: Model
for phenotype suppression of transcription. Proc Natl Acad Sci USA.
87:9990–9994. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Rodríguez-Pascual F, Redondo-Horcajo M and
Lamas S: Functional cooperation between Smad proteins and activator
protein-1 regulates transforming growth factor-beta-mediated
induction of endothelin-1 expression. Circ Res. 92:1288–1295. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
37
|
Johnston IM, Spence HJ, Winnie JN, McGarry
L, Vass JK, Meagher L, Stapleton G and Ozanne BW: Regulation of a
multigenic invasion programme by the transcription factor, AP-1:
Re-expression of a down-regulated gene, TSC-36, inhibits invasion.
Oncogene. 19:5348–5358. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
38
|
Subbaramaiah K and Dannenberg AJ:
Cyclooxygenase-2 transcription is regulated by human papillomavirus
16 E6 and E7 oncoproteins: Evidence of a corepressor/coactivator
exchange. Cancer Res. 67:3976–3985. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Barna J, Csermely P and Vellai T: Roles of
heat shock factor 1 beyond the heat shock response. Cell Mol Life
Sci. 75:2897–2916. 2018. View Article : Google Scholar : PubMed/NCBI
|
|
40
|
Richter K, Haslbeck M and Buchner J: The
heat shock response: Life on the verge of death. Mol Cell.
40:253–266. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
41
|
Hayashida N, Fujimoto M, Tan K, Prakasam
R, Shinkawa T, Li L, Ichikawa H, Takii R and Nakai A: Heat shock
factor 1 ameliorates proteotoxicity in cooperation with the
transcription factor NFAT. EMBO J. 29:3459–3469. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
42
|
Le Masson F, Razak Z, Kaigo M, Audouard C,
Charry C, Cooke H, Westwood JT and Christians ES: Identification of
heat shock factor 1 molecular and cellular targets during embryonic
and adult female meiosis. Mol Cell Biol. 31:3410–3423. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Tanabe M, Nakai A, Kawazoe Y and Nagata K:
Different thresholds in the responses of two heat shock
transcription factors, HSF1 and HSF3. J Biol Chem. 272:15389–15395.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
44
|
Tabuchi Y, Takasaki I, Wada S, Zhao QL,
Hori T, Nomura T, Ohtsuka K and Kondo T: Genes and genetic networks
responsive to mild hyperthermia in human lymphoma U937 cells. Int J
Hyperthermia. 24:613–622. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Spriggs KA, Bushell M and Willis AE:
Translational regulation of gene expression during conditions of
cell stress. Mol Cell. 40:228–237. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
46
|
Degerny C, Monte D, Beaudoin C, Jaffray E,
Portois L, Hay RT, de Launoit Y and Baert JL: SUMO modification of
the Ets-related transcription factor ERM inhibits its
transcriptional activity. J Biol Chem. 280:24330–24338. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Finzer P, Soto U, Delius H, Patzelt A, Coy
JF, Poustka A, zur Hausen H and Rösl F: Differential
transcriptional regulation of the monocyte-chemoattractant
protein-1 (MCP-1) gene in tumorigenic and non-tumorigenic HPV 18
positive cells: The role of the chromatin structure and AP-1
composition. Oncogene. 19:3235–3244. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Vasanth S, ZeRuth G, Kang HS and Jetten
AM: Identification of nuclear localization, DNA binding, and
transactivating mechanisms of Kruppel-like zinc finger protein
Gli-similar 2 (Glis2). J Biol Chem. 286:4749–4759. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
49
|
Cordes KR, Sheehy NT, White MP, Berry EC,
Morton SU, Muth AN, Lee TH, Miano JM, Ivey KN and Srivastava D:
miR-145 and miR-143 regulate smooth muscle cell fate and
plasticity. Nature. 460:705–710. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
50
|
Sirsi SR and Borden MA: Advances in
ultrasound mediated gene therapy using microbubble contrast agents.
Theranostics. 2:1208–1222. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
51
|
Maloney E and Hwang JH: Emerging HIFU
applications in cancer therapy. Int J Hyperthermia. 31:302–309.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Boissenot T, Bordat A, Fattal E and Tsapis
N: Ultrasound-triggered drug delivery for cancer treatment using
drug delivery systems: From theoretical considerations to practical
applications. J Control Release. 241:144–163. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
53
|
Lafond M, Yoshizawa S and Umemura SI:
Sonodynamic therapy: Advances and challenges in clinical
translation. J Ultrasound Med. 38:567–580. 2019. View Article : Google Scholar : PubMed/NCBI
|
|
54
|
Mikolajczyk A, Khosrawipour T, Kulas J,
Migdal P, Arafkas M, Nicpon J and Khosrawipour V: The structural
effect of high intensity ultrasound on peritoneal tissue: A
potential vehicle for targeting peritoneal metastases. BMC Cancer.
20:4812020. View Article : Google Scholar : PubMed/NCBI
|
|
55
|
Xia C, Zeng H and Zheng Y: Low-intensity
ultrasound enhances the antitumor effects of doxorubicin on
hepatocellular carcinoma cells through the ROS-miR-21-PTEN axis.
Mol Med Rep. 21:989–998. 2020.PubMed/NCBI
|
|
56
|
de Lucas B, Pérez LM, Bernal A and Gálvez
BG: Ultrasound therapy: Experiences and perspectives for
regenerative medicine. Genes (Basel). 11:E10862020. View Article : Google Scholar : PubMed/NCBI
|